Abstract
Study objective
This burden-of-illness study on osteoporosis was performed with the main goal to estimate the economic implications of osteoporosis for the Slovenian healthcare system.
Methods
A variety of sources was used to quantify the utilization of resources in 2003, and the appropriate unit costs were assigned to the identified resources.
Main outcome measures
The study included all direct and indirect costs that arise from treatment of osteoporosis and consequent hip, spine and wrist fractures in total Slovene postmenopausal population in 2003.
Results
We estimated the total burden of postmenopausal osteoporosis in Slovenia for 2003 to be over SIT 7.55 billion (approximately €31.5 million); among that, 45% or SIT 3.39 billion (€14.2 million) belong to drug expenditures for osteoporosis treatment and prevention; 29% or SIT 2.2 billion (€9.2 million) include indirect costs for osteoporosis morbidity and mortality, and 26% or SIT 1.95 billion (€8.1 million) belong to direct costs for treatment, hospitalization, and rehabilitation of osteoporotic fractures. Total costs on osteoporotic fractures were however subject to an approximation due to the expert panel-based estimate of proportion of osteoporosis-caused fractures and the limited data on resource utilization for fracture treatment.
Conclusion
Osteoporosis is a costly disease with a significant burden to society and needs to be viewed as an important problem with a complex long-term impact.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis, a disease characterized by low bone mass and microarchitectural deterioration of bone tissue leading to enhanced bone fragility and a consequent increase in fracture risk [1], is a serious problem to society because of its huge prevalence in an ageing population, and the enormous costs required for treating this condition and its consequences, i.e. fractures.
Osteoporosis and the subsequent fractures are associated with significant economic costs relating to hospitalization, outpatient care, long-term care, disability and premature death [2].
It is of concern that the worldwide health and economic burden of osteoporosis is likely to increase in the future, as improvements in life expectancy will lead to growing population of elderly people with a high risk of fracture [2].
Given the potentially huge impact on society of osteoporosis and the fractures associated with it, it is of primary importance to assess the burden of this disorder in countries around the world [2]. Estimating the burden of a specific disease is usually undertaken by means of a cost-of-illness (or burden-of-illness) study to convey the financial aspect of the disease of interest. This calculation includes the costs of providing care for the illness (including drug therapy), the value of the lost productivity, and the monetary cost to society of premature death [3]. Thus, the total direct medical costs of treating osteoporosis, the number of deaths, hospitalizations, lost days from work, etc., are the variables of interest in a burden of illness analysis conducted on osteoporosis. Cost estimations of fracture include hospital costs and charges, pharmacotherapy costs, physician and patient visits, nursing home care, rehabilitation, durable medical equipment, special transportation, social workers and etc [4]. In addition, the impact of indirect costs for osteoporosis, such as those for patient and caregiver lost time from work, decline of productivity, substantial invalidity and mortality of hip fracture, is substantial from societal perspective.
Health-care expenditures attribu
table to osteoporosis and fractures are estimated and reported in many studies worldwide. However, due to difference in national settings that exist throughout the world (e.g. different healthcare systems, different methods of pricing and reimbursement, different types and qualities of data and statistical systems, etc.), results of the burden-of-illness studies vary considerably among countries and comparison between them may be difficult. Health care expenditures attributable to osteoporotic fractures in 1995 in the US were reported to be $13,8 billion [5]; only in California, osteoporosis accounted for over $2,4 billion in direct health care costs in 1998, and over $4 million in lost productivity resulting from premature death [6]. In the UK, the annual estimated cost for all fractures is £942 million [7]. Osteoporosis has also been shown to result in significant costs in other countries; in New Zealand, the first-year total direct costs associated with osteoporotic hip fractures were estimated at around $NZ 41.7 million [8]; in Canada, fractures of the hip, wrist and vertebrae account for up to 1 billion $Can in costs to the Canadian healthcare system [9].
To date, there have been no previous burden-of-osteoporosis studies in Slovenia. Therefore, our burden-of-illness study on osteoporosis was performed with the main goal to estimate the economic implications of osteoporosis for the Slovenian healthcare system. Given our limited knowledge of the extent to which osteoporosis affects the population, the estimation on the magnitude of burden of osteoporosis was based mainly on data for resource use and incidence of osteoporotic fractures.
Method
For evaluation of the financial burden of osteoporosis in Slovenia, we followed the methodological concepts about cost evaluation when conducting burden-of-osteoporosis studies recommended in the reference literature [2]: the resource utilization was quantified and unit costs were assigned to the identified resources. The study was performed from the broadest, societal perspective and included all direct and indirect costs that arise from osteoporosis and consequent hip, spine and wrist fractures in total Slovene postmenopausal population in 2003.
Measuring of resource utilization
Identifying the resource utilization included healthcare resources used for the treatment and management of osteoporosis and fractures due to osteoporosis. Utilization of drug treatments was evaluated on the basis of annual pharmacoepidemiology data (2003) on prescription of drugs aimed at prevention and treatment of osteoporosis, provided by the Slovenian National Health Institute – IVZ [10]. We considered the following regimens: bisphosphonates (etidronate and alendronate); synthetic salmon calcitonin; hormone replacement therapy; raloxifene; vitamin D and calcium. We considered only the quantities of osteoporotic regimens prescribed exclusively to postmenopausal women for both the prevention and treatment of osteoporosis. Healthcare resources utilization in terms of fractures and their consequences were determined on the basis of the total number of hospitalized and ambulatory treated hip, spine and wrist fractures in postmenopausal women in Slovenia for 2003, provided by IVZ [11]. The total number of hospitalizations and ambulatory treatments; average length of stay in hospital; total number of cases/days treated in hospital and ambulatory rehabilitation and average length of stay; the total number of deaths because of fracture; and the total number of absentees from work due to a fracture were collected for the following ICD-10 diagnosis: hip fractures, vertebral fractures, and wrist fractures. When estimating the occurrence of fractures, it is important to keep in mind that the skeletal fragility that results from osteoporosis is not always the underlying cause of a fracture event. The number of fractures was estimated from databases of IVZ using the above mentioned diagnostic codes, but those codes do not indicate which fractures are osteoporotic in nature. Therefore, we estimated the proportion of fractures, which could be attributable to osteoporosis, using the existing site-, gender- and age-specific attribution rates of an expert panel consensus, derived by Melton et al. [12].
Valuation of costs
Costs of treating osteoporosis and its consequences were valued by assigning the appropriate cost unit to each resource utilization item as identified above; i.e. related to drug treatments, fractures and their impact. All calculated costs are given in Slovenian tolars-SIT (1€ = 239.64 SIT, National Bank of Slovenia fixed conversion rate for Euro (€) takeover and access to Euro zone); main results on costs are also presented in Euros (€).
Direct costs of treating osteoporosis and fractures included pharmacotherapy costs, acute costs of hospitalization and/or ambulatory treatment of hip, spine and wrist fractures, and costs for ambulatory and hospital rehabilitation due to fractures. The wholesale prices of all therapeutic regimens prescribed and used for treatment of osteoporosis were provided from the ZZZS (National Slovenian Healthcare Insurance Fund) data [13]; VAT (value added tax) and pharmacy issue expenses were added. Estimation of the costs for primary care and specialist’s visits for osteoporosis in Slovenia is limited and complicated by the fact that there are no ambulatory data available by diagnosis, in this case for osteoporosis. Therefore, our burden-of-osteoporosis analysis included only those direct costs that are related to pharmacotherapy prescriptions, and costs of treating osteoporosis fractures, for which the costs of primary care are already considered, and not costs for preventive primary care visits.
The costs for osteoporotic hip, spine and wrist fracture per patient were calculated as follows: acute costs for treating hip, spine and wrist fracture in hospital or ambulance were pooled from a previous study conducted in the General Hospital Maribor [14], which based its calculation on estimation on the average length of stay and potential complications, which are dependent on the age of the patient, especially for hip fracture, so different average values about all ages were obtained. It is important to note that it is very difficult to assess the real value of direct hospitalization costs of osteoporotic fractures in Slovenia, because there is no specific price valuation mechanism for various procedures associated with some condition. Thus, hospitalization daily costs in Slovenia are charged on the basis of estimation of overall charge per one day spent in hospital, regardless of therapy and diagnosis, which already includes also the costs for surgery, pharmacotherapy and all additional costs [13].
Rehabilitation costs were estimated on the basis of the IVZ data on average length of rehabilitation, the number of patients using rehabilitation service because of hip, spine or wrist fracture, and the average costs per one day spent in a rehabilitation center (ZZZS estimation). The costs of rehabilitation were calculated as follows: the cost per day on hospital rehabilitation (SIT 38 682) was multiplied with the average length of stay on rehabilitation for hip fracture and spine fracture [11]. Under the assumption that wrist fractures are treated on ambulatory rehabilitation, the cost per day on ambulatory rehabilitation (SIT 5 217) was multiplied with the average length of ambulatory rehabilitation for wrist fracture [13]. Rehabilitation costs were estimated on the basis of the IVZ data on average length of rehabilitation, the number of patients using rehabilitation service because of hip, spine or wrist fracture, and the average costs per one day spent in a rehabilitation center (ZZZS estimation).
Indirect costs of treating osteoporosis included morbidity and mortality costs due to complications of osteoporosis and fractures, which result in loses to the patients and the society. Indirect costs were calculated on the basis of the human capital approach methodology, which estimates the value of potentially lost production (or the potentially lost income) as a consequence of disease [15].
Morbidity costs were calculated as follows: the total number of women/days and the average length of absentees due to hip, wrist and spine fracture in 2003 was estimated from the IVZ source [11], and the total number of days lost was multiplied for the value of cost per one lost day, calculated on the basis of the average monthly gross salary in Slovenia in 2003 (SIT 214 561) divided by the average of working days in a month (22), which gives the daily lost of incomes due to work absenteeism (SIT 9752,77 per day for 1 active woman) [16]. The average lengths of absenteeism from work per one woman due to hip, spine and wrist fracture were pooled from the IVZ data [11], and are as follows: hip fracture = 171,8 days; spine fracture = 100,2 days; wrist fracture = 68,2 days, respectively. Indirect morbidity costs were considered only for the active working age group, i.e. women ages 50–64, considering the fact that the average time of retirement in Slovenia is approximately 60 years.
Mortality costs were calculated on the basis of premature deaths due to osteoporosis which resulted with loses to society. The estimated costs are the product of the number of deaths and the expected value of an individual’s future earnings, with age and potential time of retirement taken into account. The calculation method considered the following: life expectancy for different age groups taken from the IVZ data [11]; the changing pattern of earnings at successive ages: average monthly incomes in Slovenia-pooled from the National statistics data, 2003 [16] for salary and pension, assuming that the average time of retirement for women in Slovenia is 60 years; total number of woman’s deaths due to hip, spine or wrist fracture in Slovenia for 2003–IVZ [11]; and the appropriate discounting rate of 5% used to convert the future lifetime earnings into their present value.
Results
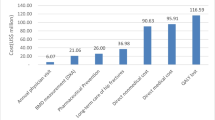
In 2003, there were 1354 hip fractures, 3129 spine fractures and 1789 wrist fractures due to osteoporosis in the total postmenopausal population of women in Slovenia. Most of the hip fractures (39%) occurred in women aged 75–84; most of the wrist fractures (78%) occurred in women aged 50–74; 34% and 32% of the estimated spine fractures were in women aged 50–64 and 75–84, respectively (Table 1). Total hospitalization costs for fractures amounted to SIT 1 282 777 990 (€5 352 938); of which, SIT 852 254 331 for hip fractures, SIT 375 367 000 for spine fractures and SIT 55 156 659 for wrist fractures. Total rehabilitation costs were estimated to be SIT 669 927 710 (€2 795 558), of which, SIT 549 555 176 for hip fractures, SIT 119 527 380 for spine fractures and SIT 845 154 for wrist fractures (Tables 1, 2).
The sum of estimated total direct costs of all osteoporotic fractures in women in 2003 (Table 2) was SIT 1 952 705 700 (€8 148 496), of which, 72% belonged to hip fractures, 25% to spine fractures and 3% to wrist fractures. The costs of hospitalization for hip fractures were greater than any other costs, followed by rehabilitation costs for hip fractures. The costs of wrist fractures were incomparable to either hip or spine fracture costs.
Table 3 shows the indirect morbidity costs due to osteoporotic fractures. These costs were considered only for the active working group of women, i.e. those aged 50–64, considering an average time of retirement of 60 years.
As this table illustrates, the greatest morbidity costs occurred with wrist fractures, as the most frequent in the given age group. Total morbidity costs of all fractures amounted to SIT 482 186 850 (€2 012 130).
Table 4 shows the indirect mortality costs due to osteoporotic fractures. The present value of lifetime earnings lost due to death for 1 woman ranged from SIT 25 655 969 for the age group 50–64, to SIT 12 202 994 (age group 65–74), SIT 8 694 451 (age group 75–84) to SIT 6 515 296 (age group over 85); differences between age groups were mainly due to difference in life-years lost per one death and different value of incomes between ages. Still, the value of total lifetime earnings lost per all deaths due to osteoporotic fractures (Table 4) was lowest for the age group 50–64 (SIT 359 183 570) and increased with age: SIT 317 277 840 (age group 65–74), SIT 443 417 000 (age group 75–84), and SIT 605 922 530 (age group over 85), as also the number of deaths increased with age. The value of total mortality costs for all deaths due to osteoporotic fractures amounted to SIT 1 725 800 940 (€7 201 640).
The total indirect costs amounted to over SIT 2 207 987 790 (€9 213 770); of which, SIT 482 186 850 (€2 012 130) were morbidity costs, and SIT 1 725 800 940 (€7 201 640) were mortality costs.
Our estimate on total prescription medication costs for prevention and treatment of postmenopausal osteoporosis in 2003 indicates that total SIT 3 392 339 929 (€14 155 984) were spent on drugs for osteoporosis in postmenopausal women in 2003. We took into account also supplemental therapies such as calcium and vitamin D for the reason that they are extensively prescribed for prevention of osteoporosis as additional supplements to therapy, and contribute to the real expenditures. The prescription costs excluding calcium and vitamin D amounted to total SIT 2 898 031 929. Bisphosphonates (SIT 1 923 423 000) and HRT (SIT 436 718 000) accounted for most of the drug expenditures, followed by calcitonin (SIT 403 530 000) and raloxifene (SIT 134 360 929).
Table 5 reveals the total costs of postmenopausal osteoporosis for Slovenia in 2003, which amounted SIT 7 553 033 419 (€31 518 250). Most of these costs, or SIT 3 392 339 929 (45%) were spent on drugs for prevention and treatment of osteoporosis; followed by SIT 2 207 987 790 (29%) accounted for indirect costs of osteoporotic fractures; and SIT 1 952 705 700 (26%) comprise the direct costs of all osteoporotic fractures in postmenopausal women.
Discussion
Burden-of-illness studies translate the adverse effects of osteoporosis into financial terms. Our burden-of-osteoporosis study was performed in order to estimate the total burden of osteoporosis and its consequences, and the impact on society. We estimated the total burden of postmenopausal osteoporosis in Slovenia for 2003 to be over SIT 7.55 billion (€31.5 million); among that, 45% or SIT 3.39 billion (€14.2 million) belongs to drug expenditures for osteoporosis treatment and prevention; 29% or SIT 2.2 billion (€9.2 million) includes indirect costs for osteoporosis morbidity and mortality, and 26% or SIT 1.95 billion (€8.1 million) belongs to direct costs for treatment, hospitalization, and rehabilitation of osteoporotic fractures. Total costs of postmenopausal osteoporosis comprise approximately 0.13% of the total Slovenian GDP (gross domestic product) in 2003 [17]. This justifies the need for considering osteoporosis as an important problem with a complex long-term impact. The society also faces substantial long-term consequences of osteoporosis in terms of productivity lost and premature deaths (29% of the total costs), besides the acute costs for treatment and hospitalization of fractures (26% of the total costs).
When analyzing the direct costs of osteoporotic fractures, it is obvious that hip fractures are the most devastating, and produce greatest hospitalization and rehabilitation costs: 72% of them belong to hip fractures, compared with 25% for spine and 3% for wrist fractures, respectively. The estimated average direct cost per hip fracture in Slovenia is around SIT 1,2 million (€5008 or US $6060), which is lower than in other developed countries. Reference data reveal that the costs per hip fracture vary substantially among countries: converted to the same currency-US $, from $6 407 in Australia, to $10 000 in The Netherlands [18], $27 014 in Sweden and $46 638 in Switzerland [19]. This is mostly due to the differences in healthcare service reimbursement and calculations; in Slovenia, all costs for drugs, surgery, additional services and etc. are included in the cost per day of hospitalization, which is not the case with many of reference countries.
Our estimates for direct costs of osteoporotic fractures reflect accurately the real situation with fractures; however, they have been subject to approximation, as the real number of fractures that are caused exclusively by osteoporosis cannot be precisely determined. An approach adopted widely is to consider low-energy fractures as being osteoporotic. This has the merit of recognizing the multifactorial causation of fracture [20]. Furthermore, on the basis of epidemiological data for fractures in Slovenia-IVZ [11], it is not possible to determine the cause of fracture coded by diagnosis, as no data of the underlying cause for fracture exist. For this reason, we decided to apply an expert panel consensus [12] results on the osteoporosis-attributable proportion of fractures by fracture site, age and gender. The estimated costs of osteoporosis-related fractures were based on the most reliable data available; nevertheless, the limitations mentioned above should be noted.
Osteoporosis is also associated with great indirect costs due to lost productivity from its subsequent morbidity and mortality: 53% or SIT 2 207 987 790 (€9 213 770) from the total 2003 burden of osteoporotic fractures belong to indirect costs. The human capital approach method [15] was used to calculate the indirect costs of osteoporosis; according to this approach, a person produces a stream of earnings that is valued at market earnings. Therefore, the indirect costs of osteoporosis may even be understated, as a relatively large number of elderly persons suffer from osteoporosis, and this method yields somewhat lower values for the elderly, because the value of human life is based on market earnings [6]. The estimates of the indirect costs of loss due to morbidity and mortality of osteoporotic fractures represent a more complete account of the economic impact of osteoporosis than is usually reported.
Other major categories of intangible costs, including pain and suffering related to osteoporosis, were omitted in our analysis, due to the difficulty of quantification. Several other costs were also excluded due to lack of data: non-medical costs, such as costs of transportation to and from healthcare centers, costs of extra household assistance required due to condition, costs of outpatient visits related to osteoporosis and nursing home costs. Therefore, the total costs of osteoporosis are even greater than that presented in our analysis.
The expenditures incurred from prescription drugs for osteoporosis treatment contribute in a great extent to the total burden of osteoporosis. The pharmaceutical expenditures take into account 45% (SIT 3 392 339 929) of total burden of osteoporosis in 2003 and are greater than direct costs of treating fractures. The usage of drugs for osteoporosis in Slovenia revealed rapid increases during the past few years, which inevitably led to greater costs and healthcare expenditures. Bisphosphonates (alendronate) and calcitonin account for most of these expenditures. Given their relatively high treatment costs, it is utterly important to ensure that all patients receive the proper treatment according to their age, fracture risk and characteristics. Literature reviews [21] suggest that all treatments are adjustable and cost-effective if targeted to a population at high-risk; population-wide public measures account only for cheapest agents, like calcium and vitamin D supplements for improving BMD in population as a whole. Therefore, it is very important to promote early detection of patients at high risk so that effective interventions can be targeted to high-risk population and implemented to prevent fractures and their negative outcomes.
The results of our cost-of-illness study are consistent with the findings of many international studies reported in the literature [5–9], and reveal the conclusion: osteoporosis represents a significant burden to society. However, direct comparing among countries cannot reflect the real burden of osteoporosis for a particular country due to substantial differences of healthcare systems and policies, data collecting and resource utilization measurement.
Cost-of-illness studies on osteoporosis are utilized to define the impact of osteoporosis on health and social service delivery systems and on productivity. They serve as a basis for policy and planning, and provide an economic basis for evaluation of interventions. Their use has varied over the years, but it is generally accepted that they are rather used to improve understanding of the clinical and economic implications of a disease, than for resource allocation [2]. However, although there are certainly some limitations on burden-of-illness studies, they are appropriate and important tool for a global approach to the problem of osteoporosis. The results of our analysis implying the significant burden of osteoporosis will therefore no doubt have implication on national healthcare fund policies and resource allocation planning, as well as on future studies on drug expenditures and utilization reviews.
Conclusion
Osteoporosis is a costly disease with a significant burden to society, as its total costs in 2003 comprised approximately 0.13% of the Slovenian GDP. This is however a rough estimation as the analysis was somewhat restricted due to deficient epidemiology data on proportion of osteoporotic fractures and per diem calculation on hospitalization costs. Given its complexity and long-term impact of its consequences, i.e. fractures, osteoporosis needs to be approached as an important problem that requires effective resource allocation to promote early detection of patients at high risk so that effective interventions can be targeted to high-risk population and implemented to prevent fractures and their negative outcomes.
References
WHO Study Group. Assessment of Fracture Risk and its Application to Screening for Postmenopausal Osteoporosis (1994) World Health Organization Technical Report Series 843:5–6
Sedrine W, Radican L, Reginster J-Y On conducting burden-of-osteoporosis studies: a review of the core concepts and practical issues. A study carried out under the auspices of a WHO Collaborating Center. Rheumatology 2001;40:7–14
Morrison A, Wertheimer AI Types of Pharmacoeconomic Evaluation. In: Morrison A, Wertheimer AI, editors. Pharmacoeconomics. A primer for the pharmaceutical industry. Philadelphia: Temple University; 2002
National Osteoporosis Foundation Status Report. Osteoporosis: review of the evidence for prevention, diagnosis and treatment and cost-effectiveness analysis. Osteoporosis International 1998; 8(S4):S1–S88
Ray N, Chan J, Thamer M et al. Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. Journal of Bone and Mineral Research 1997;12(1):24–35
Max W, Sinnot P, Kao C et al. The burden of osteoporosis in California, 1998. Osteoporosis International 2002;13:493–500
Dolan P, Torgerson DJ The cost of treating osteoporotic fractures in the United Kingdom female population. Osteoporosis International 1998;8:611–617
Lane A Direct costs of osteoporosis for New Zealand women. PharmacoEconomics 1996;9(3):231–245
Rosner A, Grima D, Torrance G et al. Cost effectiveness of multi-therapy treatment strategies in the prevention of vertebral fractures in postmenopausal women with osteoporosis. Pharmacoeconomics 1998;14(5):559–573
IVZ. Ambulantno predpisovanje zdravil v Sloveniji po ATC klasifikaciji v letu; 2003. Available via <http://www.ivz.si>
Inštitut za varovanje zdravja Republike Slovenije: Zdravstveni statistični letopis; 2003
Melton III L, Thamer M, Ray N et al. Fractures attributable to osteoporosis: report from the national osteoporosis foundation. Journal of Bone and Mineral Research 1997;12(1):16–23
http://www.zzzs.si
Ferk J Osteoporotični zlomi kolka, zapestja in hrbteničnega vretenca ter stroški zdravljenja Zdravniški Vestnik 2002;71:41–44
Koopmanschap AM, Rutten FH A practical guide for calculating indirect costs of disease. PharmacoEconomics 1996;10(5):460–466
www.gov.si/zrs/
http://www.stat.si
De Laet C, Van Hout B, Burger H et al Incremental cost of medical care after hip fracture and first vertebral fracture: The Rotterdam study. Osteoporosis International 1999;10(1):66–72
Vestergaard P, Rejnmark L, Mosekilde L Hip fracture prevention. Cost-effective strategies. Pharmacoeconomics 2001;19(5Pt1):449–468
Kanis J, Oden A, Johnell O et al The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporosis International 2001;12:417–427
Ankjaer-Jensen A, Johnell O Prevention of osteoporosis: cost-effectiveness of different pharmaceutical treatments. Osteoporosis International 1996;6:265–275
Acknowledgements
Biljana Dzajkovska wishes to thank the Slovenian Scientific Foundation for the given fellowship during the postgraduate studies. No sources of funding were used in the preparation of this paper.
Conflicts of Interest
The authors have no conflicts of interest that are directly relevant to the contents of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dzajkovska, B., Wertheimer, A.I. & Mrhar, A. The burden-of-illness study on osteoporosis in the Slovenian female population. Pharm World Sci 29, 404–411 (2007). https://doi.org/10.1007/s11096-007-9091-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-007-9091-5