Abstract
The purpose of this study was to estimate the current economic burden of osteoporosis in South Korea using national claim data of the Korean National Health Insurance Service (KNHIS) from 2008 to 2011. Patients aged 50 years or older were identified from KNHIS nationwide database for all records of outpatient visits or hospital admissions. Healthcare costs for osteoporotic patients included direct medical costs for hospitalization, outpatient care, and prescription drugs for the year after discharge. Healthcare costs were estimated based on the perspective of KNHIS, and calculated using a bottom-up approach. Between 2008 and 2011, total healthcare costs for osteoporotic patients increased from 3976 million USD to 5126 million USD, with an annual increase of 9.2% which accounted for one-sixth (16.7%) of national healthcare expenditure. Healthcare cost for hospitalization was the highest ($1903 million, 40.0% of total healthcare cost), followed by cost for outpatient care ($1474 million, 31.0%) and cost for prescription drugs ($1379 million, 29.0%). Although total healthcare cost for osteoporotic men was 6 times lower than that for osteoporotic women, the cost per person was 1.5 times higher than that for women. Total healthcare cost for osteoporotic patients without fractures was higher than that for osteoporotic patients with fractures. However, cost per person was the opposite. Osteoporosis entails substantial epidemiologic and economic burden in South Korea. This study provides information about the total healthcare burden, which could be important when determining what attention and awareness osteoporosis should be given in the public health system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis has become a common musculoskeletal disease worldwide due to increased number of elderly population. The prevalence of osteoporosis in the United States and United Kingdom has been reported to be between 13 and 30% [1,2,3]. Osteoporotic fracture is one of the most significant medical burdens of public healthcare organizations in societies worldwide [4].The incidence of osteoporotic fractures is still increasing in most countries [5,6,7], although stabilization and even reduction are registered in some countries [8,9,10].
Recent reports in South Korea have shown that incidences of osteoporosis and osteoporotic fractures are increasing more than those in other countries [6, 11,12,13,14]. South Korea became an aging society (elderly population ≥7% of the total population) in 2000. It has been predicted that South Korea will become an aged society (elderly population ≥14% of the total population) by 2018 and a super-aged society (elderly population ≥20% of the total population) by 2026 [15]. Economic burdens of osteoporosis and osteoporotic fractures in South Korea are also expected to rise significantly in the future.
Along with epidemiological statistics, data on cost of illness are useful for decision making. They provide information to rank priorities. They also support both political process and management functions at different levels of healthcare organizations [16]. The impact of osteoporosis on morbidity and mortality has been reported to be far greater than that of many other high-profile conditions, including breast and colorectal cancers [17].
Healthcare cost of osteoporosis is available for other countries [18]. However, to the best of our knowledge, there has been no report about the economic burden of osteoporosis in South Korea using nationwide database.
Therefore, the purpose of this study was to estimate the current economic burden of osteoporosis in South Korea using national claim data of the Korean National Health Insurance Service (KNHIS) from 2008 to 2011.
Materials and Methods
Data Subjects
Patients aged 50 years or older were identified from KNHIS nationwide database between 2008 and 2011. Korean National Health Insurance (KNHI) program covers 100% of the population for all services except cosmetic surgery or services due to traffic accidents. All clinics and hospitals submit patient data, including diagnosis and medical costs for claims according to international classification of diseases, 10th revision (ICD-10). The KNHIS database offers advantage to study osteoporosis and osteoporotic fractures because it does not include high-energy injuries such as traffic or industrial accidents. In addition, the KNHIS database contains all information about patients and their diseases. These data have been used in many epidemiologic studies in South Korea [6, 11,12,13, 19].
Operational Definition of Osteoporosis
Osteoporosis was identified from the algorithm used in previous reports [6, 11,12,13,14]. Briefly, at least one of the following criteria was needed to be included as an osteoporotic patient: (1) prescription of exclusive medications for osteoporosis treatment (bisphosphonate, selective estrogen receptor modifier, vitamin K2, calcitonin, ipriflavone), (2) international classification of diseases (ICD) diagnostic code of osteoporosis (ICD-10 codes M80–M82) and prescription of medications related to osteoporosis (hormones, calcium, vitamin D, oxymetholone), (3) >50 years old with an osteoporosis diagnosis, (4) past prescription history of medications for treating osteoporosis and/or past medical history suggestive of secondary osteoporosis with middle age (males: 50–69 years, females: 50–64 years), and (5) osteoporotic fractures with selected ICD-10 codes for hip (ICD-10 codes: S72.0, S72.1) and procedures associated with hip fractures, spine (S22.0, S22.1, S32.0, M48.4, and M48.5), distal radius (S52.5 and S52.6), and humerus (S42.2 and S42.3).
Resource of Healthcare Costs
From 2008 to the end of 2011, direct healthcare costs were estimated based on the perspective of KNHIS. Because there is only one insurance system in South Korea, KNHIS claims data are representatives of national medical care costs covered by the Korean medical insurance program. When clinics and hospitals manage insured patients, they request reimbursement of medical costs from the KNHIS at the end of each month. However, KNHI-claims data do not include non-covered costs such as costs of assistive devices or caregivers.
Total healthcare costs were calculated from 2008 to the end of 2011 using a bottom-up approach. Claims amounts for the first visit and follow-up treatments for 1 year were tallied for each patient. Healthcare costs of osteoporosis were expenditures that patients with osteoporosis spent on medical procedures and services performed in hospitals or clinics each year. These included costs for hospitalization, outpatient care, and prescription drugs. Costs per person were calculated as total costs divided by the total number of patients.
All costs were first calculated in Korean currency (KRW). They were then converted to US dollars (USD) using the average conversion rate of 1107 KRW per one USD in 2011 (http://ecos.bok.or.kr/).
The study protocol was approved by NHIS Institutional Review Board (approval number: NHIS-2015-4-001).
Results
Proportion of Osteoporosis
Between 2008 and 2011, the total number of osteoporosis among Koreans ≥50 years of age increased from 1,406,802 in 2008 to 1,868,601 in 2011, with an annual increase of 10% (Table 1). The incidence of osteoporosis increased from 10,589/100,000 in 2008 to 12,504/100,000 in 2011, with an annual increase of 4.9%. The proportion of osteoporosis increased from 10.9% in 2008 to 12.5% in 2011 in the general population. Total number of osteoporotic fractures accounted for 8.8% of osteoporosis in the study period. The incidence of osteoporotic fractures increased from 1127/100,000 in 2008 to 1295/100,000 in 2011, with an annual increase of 9.4% (Table 1).
Healthcare Costs for Osteoporotic Patients (Table 2)
Between 2008 and 2011, total healthcare costs for osteoporotic patients increased from 3976 million USD to 5126 million USD, with an annual increase of 9.2% which accounted for one-sixth (16.7%) of national healthcare expenditure.
Based on resource data of osteoporotic patients during the study period, healthcare cost for hospitalization was the highest ($1903 million, 40.0% of total healthcare cost), followed by cost for outpatient care ($1474 million, 31.0%) and cost for prescription drugs ($1379 million, 29.0%) (Table 3). Total healthcare cost during the study period was increased by 33.5% for osteoporotic men (553 million to 738 million USD). It was increased by 28.2% for osteoporotic women (3,423 million to 4387 million USD).
Although total healthcare cost for osteoporotic men was 6 times lower than that for osteoporotic women ($675 million USD for men and $4080 million USD for women), the cost per person for men was 1.5 times higher than that for women ($4043 USD for men and $2705 USD for women).
According to age, total healthcare cost and cost per person were the highest in the 70s. According to insurance type in South Korea, total healthcare cost of health insurance system ($3982 million USD) was 4.5 times higher than that of medical aid system ($863 million USD). However, the cost per person was 1.8 times higher in the medical aid system ($2612 USD in health insurance and $4580 USD in medical aid). Total healthcare cost was the highest for clinic. However, cost per person was the highest for tertiary hospital.
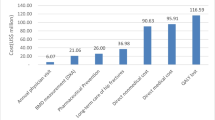
According to the presence of fractures, total healthcare cost for osteoporotic patients without fractures was higher than that for osteoporotic patients with fractures. However, cost per person was the opposite (Fig. 1).
Discussion
South Korea is an aging country. It will become an aged country in the near future. Hence, it is necessary to know the economic impact of osteoporosis on health systems as well as the epidemiology of these events. Many studies have reported the incidence of osteoporosis locally or nationally in South Korea. However, no study has reported the economic burden of osteoporosis in South Korea. The present study determined the economic burden of osteoporosis in South Korea for 2008 to 2011. In the present study, total healthcare cost for osteoporotic patients increased from 3976 million USD to 5126 million USD, with an annual increase of 9.2%. Such costs accounted for one-sixth (16.7%) of national healthcare expenditure in the study period. To the best of our knowledge, this is the first study that analyzes nationwide healthcare costs for osteoporotic patients in South Korea.
Many countries have reported that the economic burden of osteoporosis is an important issue for their health systems [20,21,22,23,24,25,26,27,28,29]. In the USA, direct medical expenditure on osteoporosis in 1995 was estimated at 13.8 billion USD [18]. A recent study has shown that the financial burden of osteoporosis has increased, with annual direct medical cost estimated at 17 to 20 billion USD [21]. In Germany, total direct cost attributable to osteoporosis was €5.4 billion in 2003. In that year, cost for osteoporotic patients accounted for 3.5% of all healthcare expenditure of social and private health insurance [20]. In Mexico, direct medical cost for osteopenia and osteoporosis besides cost due to medical care of fragility fractures was 411.1 million USD in 2010 [25]. In Canada, the overall cost of osteoporosis among Canadians aged 50 years and over was over 2.3 billion USD in 2010 for the base case analysis, when outpatient care, prescription drugs, and indirect costs were added [23]. However, current burden of osteoporosis is doubled ($4.6 billion) compared to their previous estimate ($2.3 billion) due to improved data capture of multiple encounters and services associated with fractures [24].
Several studies have shown that the economic burden of osteoporosis has increased over time [25, 26, 29]. In Mexico, the total healthcare cost was predicted to be 19.2% higher in 2015 than that in 2010. In a span of 10 years (2010–2020), the economic burden has been projected to increase by 41.7% [25]. In Switzerland, the cost of osteoporosis was estimated to increase from CHF 2.1 billion in 2010 to CHF 2.6 billion in 2025, corresponding to an increase of 29%. Costs for women and men would increase by 23 and 44%, respectively. The increase for men was estimated to be particularly higher than that for women (39 vs. 20%) [29]. In New Zealand, costs of treatment and management of osteoporosis were expected to increase to over $NZ 391 million in 2013 and $NZ 458 million in 2010 [26]. In the present study, total healthcare costs increased 28.9% (from 3976 million USD in 2008 to 5126 million USD in 2011). This means that the increment in total healthcare cost might be due to increase in aging population.
There are various reports about the expense of osteoporosis in different countries. Clark et al. have reported that the mean healthcare cost is larger for women than that for men in Mexico [3]. In addition, the mean healthcare cost for older patients (90 years and over) is higher than that for other age groups (80–89, 70–79, and <70 years) in Mexico [30]. Moraes et al. have reported that those aged 80–89 years in Brazil have the highest expenses over their study period [31]. Their average expenses are approximately 4 times higher compared to the average expenditure for those aged 60–69 years [31]. In the present study, healthcare cost per person was continuously increased with age. It was the highest for those in their 70s.
In the present study, although total healthcare cost for osteoporotic men was 6 times lower than that for osteoporotic women ($675 million USD for men and $4080 million USD for women), the cost per person was 1.5 times higher for men than that for women. Moraes et al. have verified that women are more often in need of osteoporosis-related procedures compared to men, thus presenting higher expenses from an overall point of view. However, when adjusting the total expenditure by quantity, they observed that men had higher average cost per procedure. This could be due to the higher frequency of men requiring more complex procedures. This might indicate a possible delay for men to start treatment or search for medical care when they are in advanced stages of the disease [32, 33].
In the present study, total healthcare cost for osteoporotic patients without fractures was higher than that for osteoporotic patients with fractures. However, the cost per person was opposite. This means that osteoporotic fractures should be prevented to decrease their economic burden in the public health system.
It is difficult to compare our results of direct costs to those of other studies in other countries due to differences in economic development, size of the economy, and types of health systems. In addition, different methodologies and years of publication make results non-comparable. Although international comparisons for total costs of osteoporosis are complicated by differences in age structures within a country and different health services provided by the society to people with osteoporosis, the conclusion from all international studies, including those from Sweden [34, 35], France [36], other countries [37, 38], and the current study, is that osteoporosis and related fractures are associated with significant healthcare costs, and reduction in the quality of life.
The cost-of-illness data are useful for decision making. They provide important information to rank priorities. They also support political process and management functions at different levels of healthcare organizations [16]. Johnell et al. have compared the total burden of osteoporosis in Europe to that of other chronic diseases [17]. They found that osteoporosis accounted for more disability-adjusted life-years lost than rheumatoid arthritis. However, it was less than osteoarthritis. With regard to neoplastic disorders, the burden of osteoporosis has been found to be greater than that of cancer at all sites except lung cancers [17].
This study has several limitations. First, the incidence of osteoporosis was not based on bone mineral density. The number was estimated based on claim data. We included prescriptions of osteoporosis or its related medication (vitamin K, calcitonin, ipriflavone, oxymetholone) as many as possible in order to extract accurate data regarding the number of osteoporotic patients from the KNHIS claimed database. In our previous study, these national claimed data have been validated against a cohort study in Korea, and found a sensitivity of 93% and a positive predicted value of 77.4% [39]. Second, only four major types of osteoporosis-related fractures were included in this study. Available evidence has suggested that the incidence of osteoporosis-related fractures can increase by about 10% if other types of fractures are included in the analysis [40]. Third, our cost estimation was conservative because indirect costs were not included in the analysis. Tarride et al. have reported that indirect cost due to osteoporosis accounts for 5% of the total cost in Canada [23]. Finally, the Korean government lowered the price of several anti-osteoporotic drugs up to 20% through efficient allocation and utilization of drugs in 2011. This might have caused the stabilization of cost in osteoporosis management in 2011 compared to previous cost (in 2010).
In conclusion, the present study investigated the economic burden of osteoporosis in South Korea based on national claim database. This study provides information about the total healthcare burden, which could be important when determining what attention and awareness osteoporosis should be given in the public health system.
References
Looker AC, Orwoll ES, Johnston CC Jr, Lindsay RL, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP (1997) Prevalence of low femoral bone density in older US adults from NHANES III. J Bone Miner Res 12:1761–1768
Kanis JA, Johnell O, Oden A, Jonsson B, De Laet C, Dawson A (2000) Risk of hip fracture according to the World Health Organization criteria for osteopenia and osteoporosis. Bone 27:585–590
Ballard PA, Purdie DW, Langton CM, Steel SA, Mussurakis S (1998) Prevalence of osteoporosis and related risk factors in UK women in the seventh decade: osteoporosis case finding by clinical referral criteria or predictive model? Osteoporos Int 8:535–539
Yoon HK, Park C, Jang S, Jang S, Lee YK, Ha YC (2011) Incidence and mortality following hip fracture in Korea. J Korean Med Sci 26:1087–1092
Chen IJ, Chiang CY, Li YH, Chang CH, Hu CC, Chen DW, Chang Y, Yang WE, Shih HN, Ueng SW, Hsieh PH (2015) Nationwide cohort study of hip fractures: time trends in the incidence rates and projections up to 2035. Osteoporos Int 26:681–688
Ha YC, Kim TY, Lee A, Lee YK, Kim HY, Kim JH, Park CM, Jang S (2016) Current trends and future projections of hip fracture in South Korea using nationwide claims data. Osteoporos Int 27:2603–2609
Wright NC, Saag KG, Curtis JR, Smith WK, Kilgore ML, Morrisey MA, Yun H, Zhang J, Delzell ES (2012) Recent trends in hip fracture rates by race/ethnicity among older US adults. J Bone Miner Res 27:2325–2332
Cassell E, Clapperton A (2013) A decreasing trend in fall-related hip fracture incidence in Victoria, Australia. Osteoporos Int 24:99–109
Korhonen N, Niemi S, Parkkari J, Sievanen H, Palvanen M, Kannus P (2013) Continuous decline in incidence of hip fracture: nationwide statistics from Finland between 1970 and 2010. Osteoporos Int 24:1599–1603
Maravic M, Taupin P, Landais P, Roux C (2011) Change in hip fracture incidence over the last 6 years in France. Osteoporos Int 22:797–801
Kim TY, Jang S, Park CM, Lee A, Lee YK, Kim HY, Cho EH, Ha YC (2016) Trends of incidence, mortality, and future projection of spinal fractures in Korea using nationwide claims data. J Korean Med Sci 31:801–805
Kwon GD, Jang S, Lee A, Park CM, Lee YK, Kim TY, Kim HY, Park EJ, Ha YC (2016) Incidence and mortality after distal radius fractures in adults aged 50 years and older in Korea. J Korean Med Sci 31:630–634
Park C, Jang S, Lee A, Kim HY, Lee YB, Kim TY, Ha YC (2015) Incidence and mortality after proximal humerus fractures over 50 years of age in South Korea: national claim data from 2008 to 2012. J Bone Metab 22:17–21
Choi HJ, Shin CS, Ha YC, Jang S, Jang S, Park C, Yoon HK, Lee SS (2012) Burden of osteoporosis in adults in Korea: a national health insurance database study. J Bone Miner Metab 30:54–58
Ha YC, Park YG, Nam KW, Kim SR (2015) Trend in hip fracture incidence and mortality in Korea: a prospective cohort study from 2002 to 2011. J Korean Med Sci 30:483–488
Tarricone R (2006) Cost-of-illness analysis: what room in health economics? Health Policy 77:51–63
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
WHO Scientific Group (2003) Prevention and management of osteoporosis. World Health Organ Tech Rep Ser 921:1–164
Kang HY, Yang KH, Kim YN, Moon SH, Choi WJ, Kang DR, Park SE (2010) Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health 10:230
Haussler B, Gothe H, Gol D, Glaeske G, Pientka L, Felsenberg D (2007) Epidemiology, treatment and costs of osteoporosis in Germany—the BoneEVA Study. Osteoporos Int 18:77–84
Becker DJ, Kilgore ML, Morrisey MA (2010) The societal burden of osteoporosis. Curr Rheumatol Rep 12:186–191
Blume SW, Curtis JR (2011) Medical costs of osteoporosis in the elderly Medicare population. Osteoporos Int 22:1835–1844
Tarride JE, Hopkins RB, Leslie WD, Morin S, Adachi JD, Papaioannou A, Bessette L, Brown JP, Goeree R (2012) The burden of illness of osteoporosis in Canada. Osteoporos Int 23:2591–2600
Hopkins RB, Burke N, Von Keyserlingk C, Leslie WD, Morin SN, Adachi JD, Papaioannou A, Bessette L, Brown JP, Pericleous L, Tarride J (2016) The current economic burden of illness of osteoporosis in Canada. Osteoporos Int 27:3023–3032
Carlos F, Clark P, Galindo-Suarez RM, Chico-Barba LG (2013) Health care costs of osteopenia, osteoporosis, and fragility fractures in Mexico. Arch Osteoporos 8:125
Brown P, McNeill R, Leung W, Radwan E, Willingale J (2011) Current and future economic burden of osteoporosis in New Zealand. Appl Health Econ Health Policy 9:111–123
Borgstrom F, Sobocki P, Strom O, Jonsson B (2007) The societal burden of osteoporosis in Sweden. Bone 40:1602–1609
Sambrook PN, Seeman E, Phillips SR, Ebeling PR, Osteoporosis A, National Prescribing S (2002) Preventing osteoporosis: outcomes of the Australian fracture prevention summit. Med J Aust 176(Suppl):S1–S16
Svedbom A, Ivergard M, Hernlund E, Rizzoli R, Kanis JA (2014) Epidemiology and economic burden of osteoporosis in Switzerland. Arch Osteoporos 9:187
Clark P, Carlos F, Barrera C, Guzman J, Maetzel A, Lavielle P, Ramirez E, Robinson V, Rodriguez-Cabrera R, Tamayo J, Tugwell P (2008) Direct costs of osteoporosis and hip fracture: an analysis for the Mexican healthcare system. Osteoporos Int 19:269–276
Moraes LF, Silva EN, Silva DA, Paula AP (2014) Expenditures on the treatment of osteoporosis in the elderly in Brazil (2008–2010): analysis of associated factors. Rev Bras Epidemiol 17:719–734
Gomes Fde F, Cherchiglia ML, Machado CD, Santos VC, Acurcio Fde A, Andrade EI (2014) Access to medium and high-complexity procedures in the Brazilian Unified National Health System: a matter of judicialization. Cad Saude Publica 30:31–43
Oliveira LG, Guimaraes ML (2010) Male Osteoporosis. Rev Bras Ortop 45:392–396
Zethraeus N, Borgstrom F, Strom O, Kanis JA, Jonsson B (2007) Cost-effectiveness of the treatment and prevention of osteoporosis—a review of the literature and a reference model. Osteoporos Int 18:9–23
Jonsson B, Christiansen C, Johnell O, Hedbrandt J (1995) Cost-effectiveness of fracture prevention in established osteoporosis. Osteoporos Int 5:136–142
Levy P, Levy E, Audran M, Cohen-Solal M, Fardellone P, Le Parc JM (2002) The cost of osteoporosis in men: the French situation. Bone 30:631–636
Finnern HW, Sykes DP (2003) The hospital cost of vertebral fractures in the EU: estimates using national datasets. Osteoporos Int 14:429–436
Schwenkglenks M, Lippuner K, Hauselmann HJ, Szucs TD (2005) A model of osteoporosis impact in Switzerland 2000–2020. Osteoporos Int 16:659–671
Kim SR, Ha YC, Kim JR, Kim R, Kim SY, Koo KH (2010) Incidence of hip fractures in Jeju Island, South Korea: a prospective study (2002–2006). Clin Orthop Surg 2:64–68
Kanis JA, Hans D, Cooper C, Baim S, Bilezikian JP, Binkley N, Cauley JA, Compston JE, Dawson-Hughes B, El-Hajj Fuleihan G, Johansson H, Leslie WD, Lewiecki EM, Luckey M, Oden A, Papapoulos SE, Poiana C, Rizzoli R, Wahl DA, McCloskey EV, Task Force of the FI (2011) Interpretation and use of FRAX in clinical practice. Osteoporos Int 22:2395–2411
Author information
Authors and Affiliations
Contributions
S. Jang and Y.-C. Ha designed the study. T.-Y. Kim and Y.-K. Lee prepared the first draft of the paper. T.-Y. Kim is a guarantor. H.-Y. Kim and Y.-C. Ha contributed to data collection. H.-Y. Kim, S. Jang, and T.-Y. Kim were responsible for statistical analysis of data. All authors revised the paper critically for intellectual content and approved the final version. All authors agree to be accountable for the work and ensure that any questions relating to the accuracy and integrity of the paper are investigated and properly resolved.
Corresponding author
Ethics declarations
Conflict of interest
Yong-Chan Ha, M.D., Ha-Young Kim, M.D., Sunmee Jang, PhD., Young-Kyun Lee, M.D., Tae-Young Kim, M.D. declare that they have no conflict of interest.
Human and Animal Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee as well as the 1964 Helsinki declaration and its later amendments or comparable ethical standards (IRB number: NHIS-2015-4-001).
Informed Consent
Informed consent was obtained from all individual participants included in this study.
Rights and permissions
About this article
Cite this article
Ha, YC., Kim, HY., Jang, S. et al. Economic Burden of Osteoporosis in South Korea: Claim Data of the National Health Insurance Service from 2008 to 2011. Calcif Tissue Int 101, 623–630 (2017). https://doi.org/10.1007/s00223-017-0320-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-017-0320-1