Abstract
Purpose
The potential of aerosol phage therapy for treating lung infections has been demonstrated in animal models and clinical studies. This work compared the performance of two dry powder formation techniques, spray freeze drying (SFD) and spray drying (SD), in producing inhalable phage powders.
Method
A Pseudomonas podoviridae phage, PEV2, was incorporated into multi-component formulation systems consisting of trehalose, mannitol and L-leucine (F1 = 60:20:20 and F2 = 40:40:20). The phage titer loss after the SFD and SD processes and in vitro aerosol performance of the produced powders were assessed.
Results
A significant titer loss (~2 log) was noted for droplet generation using an ultrasonic nozzle employed in the SFD method, but the conventional two-fluid nozzle used in the SD method was less destructive for the phage (~0.75 log loss). The phage were more vulnerable during the evaporative drying process (~0.75 log further loss) compared with the freeze drying step, which caused negligible phage loss. In vitro aerosol performance showed that the SFD powders (~80% phage recovery) provided better phage protection than the SD powders (~20% phage recovery) during the aerosolization process. Despite this, higher total lung doses were obtained for the SD formulations (SD-F1 = 13.1 ± 1.7 × 104 pfu and SD-F2 = 11.0 ± 1.4 × 104 pfu) than from their counterpart SFD formulations (SFD-F1 = 8.3 ± 1.8 × 104 pfu and SFD-F2 = 2.1 ± 0.3 × 104 pfu).
Conclusion
Overall, the SD method caused less phage reduction during the powder formation process and the resulted powders achieved better aerosol performance for PEV2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infectious respiratory diseases are among the most communicable of all diseases. They are also becoming increasingly lethal due to the increased emergence of bacterial resistance against most antibiotics (1,2). In particular, Pseudomonas aeruginosa, Staphylocccus aureus and Burkholderia cepacia complex, the major pathogens identified in chronically infected cystic fibrosis (CF) patients, lead to elevated morbidity and mortality risk (3,4). Although antibiotics remain an effective means of treating bacterial lung infections (5–7), the alarming rise of multidrug-resistant (MDR) bacteria and the slow development of new antibacterial compounds have highlighted the need for alternative therapies (4,8).
Bacteriophages (phages) are viruses that infect and replicate inside bacterial hosts, causing bacteriolysis. Phage therapy was discovered and proposed to treat human bacterial infection in the early 1920s. Early success of the phage therapy led to the development of many commercial phage preparations in the 1920s and 1930s, but its efficacy remained questionable as the understanding of the phage biology was very limited during that time (9). Due to the advent of antibiotics in the 1940s, it was largely forgotten after a short period of development in Western medicine. On the other hand, it continues to be refined and is widely used in the former Soviet Union and Eastern Europe to this day to treat patients, with the Eliava Institute in Tbilisi (Georgia) as one of the key centers (9–12). Debarbieux et al. (13) highlighted three main characteristics that distinguish phage therapy from antibiotic therapy: i) phages multiply at the infection site; ii) they typically have a narrow host range infecting only a specific bacterium, whereas antibiotics often eradicate a broad spectrum of bacteria; and iii) they can adapt to resistant bacteria. To help combat the rapid dissemination of MDR bacteria, the concept of phages for therapeutic use has been slowly re-introduced to the Western world. Recently, a number of in vitro infection models (14,15), animal models (16–18) and clinical evidence (11,12,19–22) have shown the potential of phage therapy in the clearance of MDR bacteria, suggesting it as a highly effective alternative to traditional antibiotics. In addition to using phages as an independent means to treat antibiotic-resistant bacterial infections, combining phage with traditional antibiotic therapies to enhance treatment outcomes has also been proposed (23,24).
Despite a large number of novel phages having been isolated and characterized to target broad-spectrum antimicrobial resistance of P. aeruginosa and B. cenocepacia (25), the route of delivery could be critical for successful application of phage therapy to treat respiratory infections. Pulmonary delivery of phages may be an efficacious administration route as phages are delivered directly to the site of infection, circumventing clearance effects caused by the human immune and reticulo-endothelial systems. Most phage research for respiratory infections in the past has been confined to liquid aerosols using intranasal instillation (13,16,17,26) and nebulization (12,27,28). Few studies have examined formulating phages into inhalable dry powder form for ease of storage, transport and administration (29–32).
With the right choice of excipients, freeze drying has been demonstrated to be an excellent technique in stabilizing phages in the solid state for long-term storage (33–35). Golshahi et al. (29) successfully produced respirable phage powder by micronizing a lyophilized lactose/lactoferrin (60:40 w/w) matrix containing phages KS4-M or ΦKZ (targeting P. aeruginosa and B. cepacia complex) using a mixer mill. This powder preparation process resulted in only a 1–2 log titer loss and the powders had reasonable in vitro aerosol performance, with a fine particle fraction of ~33%. Later, Matinkhoo et al. (30) demonstrated the feasibility of spray drying (SD), a widely used technique to produce fine drug particles for pulmonary delivery, as a single-step method to produce phage powders. Multi-component excipient systems consisting of trehalose, leucine and a third excipient, either a surfactant or casein sodium salt, were used to stabilize KS4-M, KS14 and cocktails of phages ΦKZ/D3 and ΦKZ/D3/ KS4-M in powder form. Due to the low outlet temperature (40–45°C), only 0.4–0.8 log titer loss was noted after the spray drying process. An in vitro lung dose of up to 82.7% was reported for these powders. The suitability of spray drying for producing inhalable powders containing phages (a podovirus phage LUZ19 against Pseudomonas strains or a myovirus Romulus phage against Staphylocccus strains) were also reported by Vandenheuvel et al. (31). The susceptibility of phages to the powder production method was phage dependent—whereas LUZ19 suffered less than 1 log titer loss, more than 2.5 log titer reduction was noted for Romulus. They also reported that trehalose was more efficient in preventing phages from inactivation during the production process, compared with lactose and dextran 35. Their subsequent study (32), however, highlighted the importance of suitable storage conditions in preserving the stability of phages embedded in the spray dried trehalose powders.
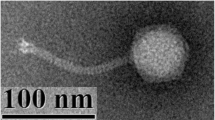
Thus, while dry powder phage formulations have been processed successfully by spray drying, the powder performance appears to be highly dependent on the phage type, formulation excipients and their concentrations, and production process. Recently, porous particles prepared by a spray freeze drying (SFD) technique have been demonstrated to be capable of delivering nanoparticles to the lungs (36). As reported therapeutic phages are generally in the nanosize range (~100 nm), SFD can potentially be used to carry and stabilize phages in an aerosol formulation. This study, therefore, compared the suitability of spray drying and spray freeze drying techniques in formulating phages into inhalable dry powders. Multi-component excipient systems composed of different ratio of trehalose, mannitol and leucine were used as the bulking and stabilizing agents. The stability of phage after the powder production process and the in vitro aerosol performance of the formulation were both assessed.
Materials and Methods
Materials
An N4-type, lytic podovirus bacteriophage, PEV2, active against P. aeruginosa was supplied by AmpliPhi Biosciences AU at a titer of 2.2 × 109 pfu/ml, stored in salt-magnesium buffer (SMB, 5.2 g/l sodium chloride, 2 g/l magnesium sulfate, 6.35 g/l Tris–HCl, 1.18 g/l Tris base and 0.01% gelatin solution, with pH adjusted to 7.5) and it was used here without further purification. The Kutter lab originally isolated it by enrichment from the sewage treatment plant in Olympia, WA, USA, using P. aeruginosa dog-ear strain PAV237 (37). Its molecular and physiological characteristics have been documented in Ceyssens et al. (37). PEV2 was used in this study because it has been shown to efficiently infect P. aeruginosa strains isolated from CF patients, under aerobic, anaerobic and biofilm conditions (14,37). The powder matrix systems were composed of different amounts of D-(+)-Trehalose dihydrate (Sigma–Aldrich, NSW, Australia), mannitol (Rocquette Frères, Lestrem, France) and L-leucine (Sigma–Aldrich, NSW, Australia). Table I shows the composition and the preparation method of the four formulations prepared in the present study.
Spray Freeze Drying
A volume of 50 ml sugar and amino acid mixture solution at a total solid concentration of 2 wt% was prepared with pH adjusted to 7–7.5 using 1 M hydrochloric acid and 1 M sodium hydroxide. Then 0.5 ml phage suspension (titer = 2.2 × 109 pfu/ml) was added to the sugar mixture, resulting in 100 times titer dilution. The phage viability in the sugar solution before spray freeze drying was confirmed with plaque assay (38). The phage containing mixture was then fed via a digitally controlled syringe pump at 1 ml/min into a 48 kHz ultrasonic nozzle (Sono-Tek Corp., NY, USA). A small amount of the sprayed droplets (~0.5 ml) were collected to examine the damaging effect of the spraying process on the phage titer. Then the atomized droplets were collected in a 250 ml beaker filled with liquid nitrogen. Excess liquid nitrogen was allowed to boil off and the frozen droplets were lyophilized at −30°C for 24 h and then at 25°C for 48 h in a freeze drier (Christ Alpha 1–4 LOC-1 M, Martin Christ, Osterode am Harz, Germany). The SFD powders were collected inside a relative humidity controlled chamber (RH < 20%) and stored in a desiccator at 4°C before being used.
Spray Drying
The phage and excipient mixtures were prepared as above and spray dried using a Büchi 290 spray dryer coupled with a conventional two-fluid nozzle for droplet atomization. The mixture was fed at a flow rate of 1.8 ml/min and atomized with compressed dry air at 742 l/h, and a small sample of the atomized droplets was collected to confirm the phage titer. Then the spray drier was run at an aspiration rate of 35 m3/h and inlet temperature of 60°C. The outlet temperature was recorded to be 40–45°C. Low outlet temperatures were used to minimize phage inactivation during the drying process (39). The SD powders were collected inside a relative humidity controlled chamber (RH < 20%) and stored in a desiccator at 4°C before use.
Phage Viability Test
The concentration of viable phage in the solution and powder samples was determined by the Miles-Misra surface droplet technique (38). Phage containing powders were dissolved in SMB to give a concentration of 50 mg/ml. Serial dilutions of the solution samples were performed by adding 20 μl sample to 180 μl SMB. A volume of 200 μl host bacteria containing ~2 × 109 colony forming units (cfu) was mixed with 5 ml molten soft agar (0.4% Amyl agar, 48°C). The mixture was overlayed onto a solidified NB agar plate made of 1.5% Amyl agar and Nutrient Broth. Then, 10 μL of diluted phage samples were dropped onto the agar lawn and left to air dry for 20 min, and the plates were incubated overnight at 37°C. Samples that gave rise to 3–30 plaque forming units were use to determined the phage titer.
Powder Characterization
Scanning Electron Microscopy (SEM)
Morphologies of the SFD and SD powders were obtained using a field emission scanning electron microscope (SEM) (Zeiss Ultra Plus, Carl Zeiss NTS GmbH, Oberkochen, Germany) at 5 kV. The samples were prepared on carbon tape and sputter coated with approximately 15 nm of gold using a K550X sputter coater (Quorum Emitech, Kent, UK) before imaging.
X-ray Diffraction (XRD)
The crystallinity of the produced powders was examined using an X-ray diffractometer (Model D5000; Siemens, Munich, Germany) under ambient conditions. Samples were spread on glass slides and subjected to Cu Kα radiation at 30 mA and 40 kV. The scattered intensity was collected by a detector for a 2θ range of 5–40° at an angular increment rate of 0.04° 2θ / s.
Dynamic Vapor Sorption (DVS)
The moisture sorption profiles of the SFD and SD samples were analyzed using a DVS instrument (DVS-Intrinsic, Surface Measurement Systems, London, UK). Each sample (5 ± 1 mg) was subjected to a dual moisture ramping cycle of 0 to 90% relative humidity (RH) at a step increase of 10% RH. Equilibrium moisture content at each RH was defined as dm/dt of 0.02% per minute.
Differential Scanning Calorimetry (DSC) and Thermogravimetric Analysis (TGA)
The thermal properties of the powders were analyzed using a differential scanning calorimeter and thermogravimetric analysis (Mettler Toledo, Greifensee, Switzerland). For DSC measurement, each sample (5 ± 1 mg) was weighed in an aluminium crucible which was then crimped to a perforated lid and heated from 30 to 300°C at a rate of 10°C/min under 250 cm3/min nitrogen purge. For TGA measurement each sample (5 ± 1 mg) was weighed in an alumina crucible and heated from 30 to 400°C at a rate of 10°C/min with dynamic nitrogen flow. The data was analyzed using STARe software (V.9.0x; Mettler Toledo, Greifensee, Switzerland).
In Vitro Aerosol Performance
The aerosol performance of the produced powders was assessed by dispersing 20 mg of powder into a Multi-stage Liquid Impinger (MSLI) using an Osmohaler™ at 100 l/min for 2.4 s. A Next Generation Impactor was not used because the silicon grease (Slipicone®; DC Products, VIC, Australia) that is generally used to minimize particle bounce was found to inactivate the PEV2 phage. The damaging effect of silicon grease was also reported in Dixit et al. (40). Size 3 hydroxypropyl methylcellulose (HPMC) capsules (Capsugel, NSW, Australia) were used for powder loading. While one capsule was used for the SD powder, SFD powders were loaded into four capsules due to its low powder density. Due to the high hygroscopicity of some formulations, all capsule filling was done in a humidity controlled (~17%) box. All dispersion experiments were conducted in triplicate at RH = 50 ± 5% and 20 ± 5°C. Preliminary experiments showed that the PEV2 phage was not very stable in deionized water, as is true for most phage. However, the presence of SMB had a significant impact on the chemical assay of trehalose and mannitol using High Performance Liquid Chromatography (HPLC). Therefore, separate dispersions were performed with SMB and pure water as the collecting solvent to determine the deposition profiles of the phage and the sugar excipients, respectively. The lower cutoff diameters of the MSLI stages 1–4 at 100 l/min are 10.1, 5.3, 2.4 and 1.32 μm, calculated with the adjustment equations given in Appendix XII C of the British Pharmacopoeia. The fine particle fraction (FPF) was defined as the mass fraction of particles ≤5.0 μm with respect to the recovered dose. The cumulative fraction of particles with aerodynamic diameter ≤5.0 μm, corresponding to the FPF, was determined by interpolation.
Chemical Assay
The deposition of trehalose and mannitol at the capsule, inhaler, adaptor and each part of the MSLI was determined using a HPLC system (Model LC-20; Shimadzu, Japan) using RI detection. The configuration consisted of a CBM-20A controller, LC-20AT pump, RID-10A RI detector, SIL-20A HT auto-sampler, and LCSolution software. An amino acid column (Phenomenex Luna NH2, 5 μm, 100 Å, 250 × 4.6 mm) was used. The mobile phase was a mixture of water (30%) and acetonitrile (70%). The solvent peak of pure water was found to overlap with the trehalose and mannitol peaks, so the 300 μl dispersion samples were mixed with 700 μl acetonitrile before HPLC analysis. The calibration curves for trehalose and mannitol were linear in the concentration range of 0.05–1 mg/mL (R2 = 0.999, n = 3). However, some samples were below the detection limit after the dilution with acetonitrile. Therefore, the dispersion samples were concentrated by evaporating 1.5 ml dispersion samples inside a 60°C oven overnight and reconstituting the dried powder in 300 μl deionized water before adding 700 μl acetonitrile for HPLC analysis.
Results and Discussion
Phage Viability
The viability of the PEV2 phage after each processing step during powder production was examined and the reduction in titer is shown in Fig. 1. When the phage suspension was mixed with the excipient solution (before spraying), ~0.5 log titer loss was noted for all formulations. The change in the ionic strength due to the dilution of the phage storage buffer (100 times dilution) could be responsible for the phage inactivation.
The ultrasonic nozzle employs high frequency (48 kHz in the present study) vibration to break liquid into small droplets of narrow size distribution; the two-fluid nozzle atomizes liquid droplets due to high frictional shearing forces between the liquid surface and the high velocity air. In general, PEV2 phage was more susceptible to the high vibration energy compared with the high shearing forces during the atomization step. The titer loss after the ultrasonic nozzle spraying was ~2 log, while only a ~0.75 log reduction was noted for the phage solution after spraying with the two-fluid nozzle. The titer loss was found to be independent of the formulation compositions for both droplet generation methods.
In the spray freeze drying technique, the atomized droplets fell into liquid nitrogen and froze instantly. The collected frozen droplets were subsequently dried under vacuum, where both frozen and non-frozen bound water were removed through sublimation to generate porous dry particles. When considering the drying process only, spray drying caused more phage damaged compared with the freeze drying. The total titer reduction in SFD formulation, however, was higher than the SD formulation, which was due to a much higher titer loss in the spraying process using the ultrasonic nozzle in SFD. The sprayed formulations SFD-F1 and SFD-F2 showed negligible difference in the titer before and after the lyophilization process (Fig. 1), suggesting that phage activity was preserved well by these excipient systems during the freeze drying step. In fact, the excellent capability of trehalose in preserving the activity of protein during freeze drying has been documented (41). In contrast to freeze drying, significant titer reduction was observed after the spray drying with an inlet temperature of 60°C (outlet temperature ranged 40–45°C), regardless of the formulation compositions. The higher titer loss was presumably due to heat, but there were potentially other confounding factors such as heating and aspiration rates.
Overall, the spray drying method produced powders with higher phage viability than the ultrasonic spray freeze drying technique. Whether spray drying remains a superior approach in producing phage powder in comparison with nontraditional approaches to spray freeze drying, such as atmospheric spray freeze drying (42,43), is a topic for future work.
Powder Characterization
Figure 2 shows the SEM images of the produced SFD and SD powders. The SFD particles (left panel) were spherical in shape and had a geometric diameter of ~30 μm, which corresponded to the initial droplet size generated by the ultrasonic nozzle. As water was removed by sublimation during the freeze drying process, the SFD particles were highly porous. From Fig. 2, it is clear that most SFD-F1 particles lost their porous structure and shrank, and the surface became quite smooth. Similar results were reported in Sonner et al. (44), who showed that SFD trehalose particles were highly hygroscopic and SFD mannitol particles were non-hygroscopic. With reduced trehalose content, SFD-F2 (40%) maintained their porous nature well. The SD particles were in principle spherical with two distinct particle sizes—some were 2 μm in diameter and some were sub-micron. Significant particle merging was observed in SD-F1 due to the high trehalose content (60%). The results also suggested that the amount of leucine (20%) may not be sufficient to form a crystalline shell to protect the amorphous trehalose (45). The degree of particle merging was significantly reduced as the mannitol content (40%) increased because of the crystalline nature of SD mannitol.
While trehalose powders prepared by spray drying and freeze drying techniques are dominantly amorphous (46), mannitol is generally crystalline (36). Feng et al. (45) showed the formation of a crystalline leucine shell when trehalose was co-spray dried with (≥25%) leucine. Figure 3 shows the X-ray diffraction patterns for the trehalose-mannitol-leucine in SFD and SD samples. All formulations demonstrated a partially crystalline and amorphous structure. Comparing with the SD formulations, more and stronger crystalline peaks were observed in the SFD counterparts. It was noted that the SFD samples became sticky during the sample preparation step. As seen in Fig. 2, the SFD powders were porous in structure. The enhanced specific surface area could increase the rate of moisture sorption and cause recrystallization of the trehalose component during the measurement, accounting for the stronger crystallinity. Vandenheuvel et al. (32) reported that high humidity (54% RH) could cause crystallization of the spray dried trehalose powder matrix.
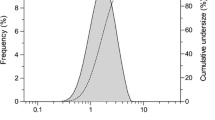
Dynamic vapor sorption (DVS) is a useful technique to determine the critical relative humidity storage condition of an amorphous or partially amorphous material to prevent storage above the glass transition temperature or a water-induced crystallization at a particular temperature. When a material undergoes an amorphous to crystalline transition, the water sorption capacity typically decreases drastically and results in an overall mass loss due to desorption of excess water during re-crystallization (47). Figure 4 shows the DVS weight change profiles of the SD and SFD powders as the relative humidity increased from 0 to 90% at room temperature. The adsorption profiles of both SD and SFD formulations clearly demonstrated the sorption characteristics of crystallization. The onset relative humidity for the crystallization process was found to decrease with increasing trehalose content. Despite the powder preparation, formulations with 60% trehalose absorbed more water for relative humidity below 80%. From the results, a relative humidity below 20% would be recommended for handling and storage of the phage powders.
The thermal behavior of phage loaded SFD and SD powders obtained by DSC and TGA analysis is shown in Fig. 5. Formulations containing 60% trehalose (SFD-F1 and SD-F1) showed glass transition temperature (Tg) of trehalose at ~80°C (Fig. 5a). If there is amorphous mannitol presented in the powder matrix, the Tg for the powder mixture is expected to decrease with decreasing trehalose content, as mannitol has a much lower Tg than trehalose (48). In this study, as the trehalose content decreased in the formulations, it became very difficult to identify the glass transition in the DSC trace (Fig. 5a). Chen et al. (49) showed that the glass transition temperature of a mixture of trehalose and hydroxyethyl starch, which is similar to mannitol in that it did not show a Tg in the studied temperature range, became questionable around a trehalose content of ~40%. A modulated DSC measurement is recommended for more accurate measurement of the Tg in these samples.
All SFD formulations had a small endothermic and an exothermic transition event at 150–158°C, followed by a large endothermic melting peak at 166°C (Fig. 5a). This is a characteristic transition of the δ form of mannitol to the thermodynamically more stable α and β polymorphs (50). Similar results for SFD mannitol were reported previously (36). Such transitions were not detected in the DSC traces for the SD formulations, indicating the absence of δ polymorph. Instead, only a large endothermic peak was noted at 130–180°C for SD-F2, corresponding to the melting of α or β mannitol. This peak vanished in SD-F1, which could be attributed to the lower mannitol content (20%).
There was an endothermic peak observed at 210–260°C for all formulations. Lähdea et al. (51) reported that the sublimation point of leucine (~200°C) was lower than its boiling point (~295°C). In addition, the peak height was relatively similar among all formulations, for which only the leucine content was kept constant (20%). Therefore, this peak was very likely accounted by the sublimation of leucine and corresponding to the TGA data (Fig. 5b).
There was an endothermic peak around 270–290°C, and the heat flow decreased with decreasing trehalose content. According to the TGA curves (Fig. 5b), the components in the powder formulation start decomposition around 250°C. Hence, this peak could be attributed to the onset of decomposition or oxidation of trehalose.
In-Vitro Aerosol Performance
The deposition profiles, total mass recovery and FPF of trehalose and viable phage of the SFD and SD formulations are depicted in Fig. 6. Mannitol, the other sugar excipient, shared similar deposition profiles to those of trehalose (data not shown). The total mass recovery (77–93%) for sugar was similar for all SFD (Fig. 6a) and SD (Fig. 6b) formulations. In contrast, the total recovery of viable phage was markedly different between the SFD (88–97%) and the SD (23–25%) formulations. The results suggested that large porous particles provided better protection for the phages during the dispersion, which could be due to their distribution within the particles. During the spray freeze drying process, the atomized droplets were frozen immediately in the liquid nitrogen. As a result, the phages had no time to redistribute themselves and were expected to be uniformly distributed within the particles. On the other hand, water within the atomized droplets gradually evaporated to form solid particles during the spray drying process. Therefore, components within the droplets may have enough time to redistribute within the particles, with the distribution depending on their material properties and the processing parameters (52). As mentioned above, phage particles (~100 nm) are essentially composed of a stable protein capsule enclosing a single molecule of DNA, and tend to reside at the surface of the particle matrices during the drying process (53,54). During the dispersion process, phages covering the particle surface might be inactivated upon impaction with the interior wall of the OsmohalerTM DPI, resulting in a low phage recovery (~20%). The results also suggest the amount of leucine added to the formulations might not be sufficient to form a crystalline shell to protect the phages.
The distribution profiles, total mass recovery and FPF of trehalose and viable phage of the (a) SFD and (b) SD formulations. Data presented as mean ± one standard deviation (n = 3). All formulations were dispersed at 100 L/min for 2.4 s using the Osmohaler™. The aerodynamic cutoff diameter of each stage is quoted in parentheses.
In general, the dispersion profiles of the phage samples were consistent with the sugar for SFD-F1. As seen in Fig. 2, most SFD-F1 particles had lost the porous structure, resulting in the majority of the trehalose depositing on higher stages (Stage 1 and 2) of the MSLI and hence a low FPF value (17%, Fig. 6a). On the other hand, the porous SFD-F2 particles dispersed well, with most powders depositing at the lower stages of the MSLI and having reasonable high FPF for the sugar (65%) and the phage (44%). The FPF of sugar was much higher than that of the phage for SFD-F2 because a significant amount of sugar was deposited in the filter stage, but no phages were detected there. It was also noted that the phages had higher depositions on the device and the throat than sugar at these positions.
All SD powders had a significantly higher deposition of viable phage than the sugar in the capsule and device. This could be due to the preferential adherence of phage onto the HPMC capsule wall. While more sugar was deposited on the throat and the upper stages of the MSLI (S1 and S2), similar sugar and phage depositions were noted for the lower stages of the MSLI (S3, S4 and filter stage). This resulted in similar FPF values between the sugar and phage for both SD formulations.
The phage loading in the capsules and the in vitro total lung dose of phage after dispersing with an Osmohaler™ at 100 l/min for 2.4 s are shown in Fig. 7. The total lung dose was determined as the amount of phage embedded in particles smaller than 5 μm i.e. the FPF. Though the FPF for SFD-F1 was only 17%, the total lung dose of viable phage was 8.3 ± 1.8 × 104 pfu, higher than SFD-F2 (2.1 ± 0.3 × 104 pfu). This is because SFD-F1 provided better preservation of phages, as seen in Fig. 1. The total lung doses for the SD formulations (SD-F1 = 13.1 ± 1.7 × 104 pfu and SD-F2 = 11.0 ± 1.4 × 104 pfu) were all higher than the corresponding SFD formulations, despite their higher titer loss (low phage recovery) during the dispersion process (Fig. 6).
Theoretically, only a small amount of phage should be needed to eradicate the target bacteria as phage is capable of self-replication in situ. However, the importance of phage titer for successful application of phage therapy has been demonstrated in animal models (13,17,55). Soohill (55) showed a dose of 1.2 × 107 pseudomonas phage could protect 50% of the mice which were infected with five times of the lethal dose (5LD50 = 1 × 108) of a strain of P. aeruginosa. Debarbieux and coworkers (13,17) reported similar results. They noted a >40% survival rate when infected mice (3 × 106 cfu of P. aeruginosa) treated with a single intranasal dose of 3 × 106 phages, whereas 100% of the animal given 3 × 108 phage were protected (17). In their follow up study (13), they showed that mice treated with phage in a phage-to-bacterium ratio of 1 : 10 died within 5 days of inoculation with P. aeruginosa of 1 × 107 cfu, while those treated with higher phage-to-bacterium ratios (1 : 1 and 10 : 1) survived until the end of the experiment (12 days). The lung dose achievable by powders produced in the present study (in the order of 105) is much lower than the doses used in these animal studies, but the delivery efficiency in the latter studies was not reported. The prediction of actual phage titer in airway surface liquid is highly complex, depending on regional deposition of the phage particles in the lungs (and particularly, within the vicinity of the targeted tissues) which is beyond the scope of the study. Nonetheless, further work on using a higher starting titer (before any process) and improving the process parameters to reduce titer loss in order to obtain a higher viable lung dose are worth exploring.
In term of pharmacokinetics, Payne et al. (56) suggested phage therapy can be classified into two categories: (1) ‘passive or inundative treatment’, where the phage density is high enough to remove a majority of target bacteria without requiring phage to replicate; (2) ‘active treatment’, where phage is increased to sufficient density by in situ replication to kill most of the bacteria. Therefore, a wide breadth of dosing ranges could be used during phage treatment, providing the minimum phage density that is necessary to achieve desired levels of bacterial eradication could be attained and then sustained (11). Based on calculation, Abeton suggested ~108 pfu/ml phage as the minimal effective phage density (57). For both safety and economic reasons, a standard approach towards phage therapy dosing should be the use of relatively low phage densities, with either repeated dosing or using greater phage densities when phage access to bacteria is limiting, rather than striving under all circumstances to inundate bacteria with substantial excesses of phages (>>108 pfu/ml) (58). In addition to dosing, timing of phage treatment could also be crucial for successful clinical outcomes (56). As both the replication and infection processes of bacteria and phage are density-dependent, phage administered too early may be loss from the body before it reaches the replication threshold. The optimal inoculation time will depend on particular phage-bacteria system (56). Further ex vivo and in vivo studies will be required to determine the suitable dose of the powder containing PEV2 phages, dosing frequency and timing of administration. Overall, the SD method has shown to be a better technique in producing dispersible PEV2 phage powder for pulmonary delivery compared with the ultrasonic SFD method.
Conclusion
SFD and SD powder processing techniques were employed to produce inhalable phage powders using various amounts of trehalose, mannitol and L-leucine as the powder matrices. The ability to formulate phages into powder form and potential to deliver phages to the lungs were assessed in vitro. A higher total phage loss was noted for the SFD powders (~2 log loss) due to the more destructive droplet generation process of the ultrasonic nozzle. Although the test PEV2 phage was more vulnerable to evaporative drying process, the SD powders had a slightly lower overall (droplet formation+drying) phage loss (1.5 log loss). All powders were partially crystalline and partially amorphous, with recrystallization taking place at high humidity conditions (>25%). During the aerosolization process, the SD powders loss of ~80% phage, was much higher than the SFD powders (~20% phage loss). Despite this, because of the lower powder loss during the powder production process, SD formulations achieved higher total lung dose (SD-F1 = 13.1 ± 1.7 × 104 pfu and SD-F2 = 11.0 ± 1.4 × 104 pfu) than their counterpart SFD formulations (SFD-F1 = 8.3 ± 1.8 × 104 pfu and SFD-F2 = 2.1 ± 0.3 × 104 pfu). In summary, the SD method produced more stable phage powder formulations and achieved better aerosol performance for the bacteriophage PEV2, and has the potential for providing viable phage for treating lung Pseudomonas infections.
Abbreviations
- CF:
-
Cystic fibrosis
- cfu:
-
Colony formation unit
- DSC:
-
Differential scanning calorimetry
- DVS:
-
Dynamic vapor sorption
- FPF:
-
Fine particle fraction
- HPLC:
-
High performance liquid chromatography
- HPMC:
-
Hydroxypropyl methylcellulose
- MDR:
-
Multidrug-resistant
- MSLI:
-
Multi-stage liquid impinger
- NB:
-
Nutrient broth
- pfu:
-
Plaque formation unit
- RH:
-
Relative humidity
- SD:
-
Spray drying
- SEM:
-
Scanning electron microscope
- SFD:
-
Spray freeze drying
- SMB:
-
Salt-magnesium buffer
- Tg :
-
Glass transition temperature
- TGA:
-
Thermogravimetric analysis
- XRD:
-
X-ray diffraction
References
Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2(1):25–32.
In: Foundation TAL, editor. The Australian Lung Foundation’s case statement: respiratory infectious disease burden in Australia. 2007.
Govan JRW, Deretic V. Microbial pathogenesis in cystic fibrosis: mucoid Pseudomonas aeruginosa and Burkholderia cepacia. Microbiol Rev. 1996;60(3):539–74.
Boucher HW, Talbot GH, Bradley JS, Edwards Jr JE, Gilbert D, Rice LB, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(1):1–12.
Li J, Nation RL, Turnidge JD, Milne RW, Coulthard K, Rayner CR, et al. Colistin: the re-emerging antibiotic for multidrug-resistant Gram-negative bacterial infections. Lancet Infect Dis. 2006;6(9):589–601.
Chmiel JF, Aksamit TR, Chotirmall SH, Dasenbrook EC, Elborn JS, LiPuma JJ, et al. Antibiotic management of lung infections in cystic fibrosis. I. The microbiome, methicillin-resistant Staphylococcus aureus, gram-negative bacteria, and multiple infections. Ann Am Thorac Soc. 2014;11(7):1120–9.
Hoiby N. Recent advances in the treatment of Pseudomonas aeruginosa infections in cystic fibrosis. Bmc Med. 2011;9:32.
Nordmann P, Naas T, Fortineau N, Poirel L. Superbugs in the coming new decade; multidrug resistance and prospects for treatment of Staphylococcus aureus, Enterococcus spp. and Pseudomonas aeruginosa in 2010. Curr Opin Microbiol. 2007;10(5):436–40.
Hoe S, Semler DD, Goudie AD, Lynch KH, Matinkhoo S, Finlay WH, et al. Respirable bacteriophages for the treatment of bacterial lung infections. J Aerosol Med Pulm Drug Deliv. 2013;26(6):317–35.
Sulakvelidze A, Alavidze Z, Morris JG. Bacteriophage therapy. Antimicrob Agents Chemother. 2001;45(3):649–59.
Kutter E, De Vos D, Gvasalia G, Alavidze Z, Gogokhia L, Kuhl S, et al. Phage therapy in clinical practice: treatment of human infections. Curr Pharm Biotechnol. 2010;11(1):69–86.
Kutateladze M, Adamia R. Phage therapy experience at the Eliava Institute. Med Mal Infect. 2008;38(8):426–30.
Debarbieux L, Leduc D, Maura D, Morello E, Criscuolo A, Grossi O, et al. Bacteriophages can treat and prevent Pseudomonas aeruginosa lung infections. J Infect Dis. 2010;201(7):1096–104.
Essoh C, Blouin Y, Loukou G, Cablanmian A, Lathro S, Kutter E, et al. The susceptibility of Pseudomonas aeruginosa strains from cystic fibrosis patients to bacteriophages. Plos One. 2013;8(4).
Larche J, Pouillot F, Essoh C, Libisch B, Straut M, Lee JC, et al. Rapid identification of international multidrug-resistant Pseudomonas aeruginosa clones by multiple-locus variable number of tandem repeats analysis and investigation of their susceptibility to lytic bacteriophages. Antimicrob Agents Chemother. 2012;56(12):6175–80.
Semler DD, Goudie AD, Finlay WH, Dennis JJ. Aerosol phage therapy efficacy in Burkholderia cepacia Complex respiratory infections. Antimicrob Agents Chemother. 2014;58(7):4005–13.
Morello E, Saussereau E, Maura D, Huerre M, Touqui L, Debarbieux L. Pulmonary bacteriophage therapy on Pseudomonas aeruginosa cystic fibrosis strains: first steps towards treatment and prevention. Plos One. 2011;6(2), e16963.
Alemayehu D, Casey PG, McAuliffe O, Guinane CM, Martin JG, Shanahan F, et al. Bacteriophages phi MR299-2 and phi NH-4 can eliminate Pseudomonas aeruginosa in the murine lung and on cystic fibrosis lung airway cells. Mbio. 2012;3(2), e00029.
Wright A, Hawkins CH, Anggard EE, Harper DR. A controlled clinical trial of a therapeutic bacteriophage preparation in chronic otitis due to antibiotic-resistant Pseudomonas aeruginosa; a preliminary report of efficacy, in Clin Otolaryngol. 2009;349–357.
Khawaldeh A, Morales S, Dillon B, Alavidze Z, Ginn AN, Thomas L, et al. Bacteriophage therapy for refractory Pseudomonas aeruginosa urinary tract infection. J Med Microbiol. 2011;60(11):1697–700.
Kutter E, Borysowski J, Miedzybrodzki R, Gorski A, Weber-Dabrowska B, Kutateladze M, et al. Clinical phage therapy. In: Borysowski J, Miedzybrodzki R, Gorski A, editors. Therapy: current research and applications. Caister Academic Press; 2014. p. 257–88.
Keen EC, Adhya SL. Phage therapy: current research and applications. Clin Infect Dis Off Publ Infect Dis Soc Am. 2015;61(1):141–2.
Kutateladze M, Adamia R. Bacteriophages as potential new therapeutics to replace or supplement antibiotics. Trends Biotechnol. 2010;28(12):591–5.
Semler DD, Lyunch KH, Dennis JJ. The promise of bacteriophage therapy for Burkholderia cepacia complex respiratory infections. Frontiers in cellular and infection microbiology, 2012. 1. UNSP 27.
Ackermann HW. 5500 phages examined in the electron microscope. Arch Virol. 2007;152(2):227–43.
Carmody LA, Gill JJ, Summer EJ, Sajjan US, Gonzalez CF, Young RF, et al. Efficacy of bacteriophage therapy in a model of Burkholderia cenocepacia pulmonary infection. J Infect Dis. 2010;201(2):264–71.
Golshahi L, Seed KD, Dennis JJ, Finlay WH. Toward modern inhalational bacteriophage therapy: nebulization of bacteriophages of Burkholderia cepacia Complex. J Aerosol Med Pulm Drug Deliv. 2008;21(4):351–9.
Sahota JS, Smith CM, Radhakrishnan P, Winstanley C, Goderdzishvili M, Chanishvili N, et al. Bacteriophage delivery by nebulization and efficacy against phenotypically diverse Pseudomonas aeruginosa from cystic fibrosis patients. J Aerosol Med Pulm Drug Deliv. 2015;28(5):353–60.
Golshahi L, Lynch KH, Dennis JJ, Finlay WH. In vitro lung delivery of bacteriophages KS4-M and Theta KZ using dry powder inhalers for treatment of Burkholderia cepacia complex and Pseudomonas aeruginosa infections in cystic fibrosis. J Appl Microbiol. 2011;110(1):106–17.
Matinkhoo S, Lynch KH, Dennis JJ, Finlay WH, Vehring R. Spray-dried respirable powders containing bacteriophages for the treatment of pulmonary infections. J Pharm Sci. 2011;100(12):5197–205.
Vandenheuvel D, Singh A, Vandersteegen K, Klumpp J, Lavigne R, Van den Mooter G. Feasibility of spray drying bacteriophages into respirable powders to combat pulmonary bacterial infections. Eur J Pharm Biopharm. 2013;84(3):578–82.
Vandenheuvel D, Meeus J, Lavigne R, Van den Mooter G. Instability of bacteriophages in spray-dried trehalose powders is caused by crystallization of the matrix. Int J Pharm. 2014;472(1–2):202–5.
Merabishvili M, Vervaet C, Pirnay J-P, De Vos D, Verbeken G, Mast J, et al. Stability of Staphylococcus aureus phage ISP after freeze-drying (Lyophilization). Plos One. 2013;8(7).
Ackermann HW, Tremblay D, Moineau S. Long-term bacteriophage preservation. World Fed Cult Collect Newsl. 2004;38:35–40.
Jepson CD, March JB. Bacteriophage lambda is a highly stable DNA vaccine delivery vehicle. Vaccine. 2004;22(19):2413–9.
D’Addio SM, Chan JGY, Kwok PCL, Benson BR, Prud’homme RK, Chan H-K. Aerosol delivery of nanoparticles in uniform mannitol carriers formulated by ultrasonic spray freeze drying. Pharm Res. 2013;30(11):2891–901.
Ceyssens P-J, Brabban A, Rogge L, Lewis MS, Pickard D, Goulding D, et al. Molecular and physiological analysis of three Pseudomonas aeruginosa phages belonging to the “N4-like viruses”. Virology. 2010;405(1):26–30.
Carlson K. Appendix. Working with bacteriophages: common techniques and methodological approaches. In: Kutter E, and Sulakvelidze A, editors. Bacteriophages: biology and applications. Boca Raton: CRC Press; 2005. p. 437–94.
Chopin MC. Resistance of 17 mesophilic lactic streptococcus bacteriophages to pasteurization and spray-drying. J Dairy Res. 1980;47(1):131–9.
Dixit N, Maloney KM, Kalonia DS. Protein-silicone oil interactions: comparative effect of nonionic surfactants on the interfacial behavior of a fusion protein. Pharm Res. 2013;30(7):1848–59.
Wang W. Lyophilization and development of solid protein pharmaceuticals. Int J Pharm. 2000;203(1–2):1–60.
Leuenberger H. Process of drying a particulate material and apparatus for implementing the process. 1987. US patent 4,608,764.
Wang ZL, Finlay WH, Peppler MS, Sweeney LG. Powder formation by atmospheric spray-freeze-drying. Powder Technol. 2006;170(1):45–52.
Sonner C, Maa YF, Lee G. Spray-freeze-drying for protein powder preparation: particle characterization and a case study with trypsinogen stability. J Pharm Sci. 2002;91(10):2122–39.
Feng AL, Boraey MA, Gwin MA, Finlay PR, Kuehl PJ, Vehring R. Mechanistic models facilitate efficient development of leucine containing microparticles for pulmonary drug delivery. Int J Pharm. 2011;409(1–2):156–63.
Surana R, Pyne A, Suryanarayanan R. Effect of preparation method on physical properties of amorphous trehalose. Pharm Res. 2004;21(7):1167–76.
Burnett DJ, Thielmann F, Booth J. Determining the critical relative humidity for moisture-induced phase transitions. Int J Pharm. 2004;287(1–2):123–33.
Kim AI, Akers MJ, Nail SL. The physical state of mannitol after freeze-drying: effects of mannitol concentration, freezing rate, and a noncrystallizing cosolute. J Pharm Sci. 1998;87(8):931–5.
Chen T, Bhowmick S, Sputtek A, Fowler A, Toner M. The glass transition temperature of mixtures of trehalose and hydroxyethyl starch. Cryobiology. 2002;44(3):301–6.
Burger A, Henck JO, Hetz S, Rollinger JM, Weissnicht AA, Stottner H. Energy/temperature diagram and compression behavior of the polymorphs of D-mannitol. J Pharm Sci. 2000;89(4):457–68.
Lahde A, Raula J, Malm J, Kauppinen EI, Karppinen M. Sublimation and vapour pressure estimation of L-leucine using thermogravimetric analysis. Thermochim Acta. 2009;482(1–2):17–20.
Vehring R. Pharmaceutical particle engineering via spray drying. Pharm Res. 2008;25(5):999–1022.
Maury M, Murphy K, Kumar S, Mauerer A, Lee G. Spray-drying of proteins: effects of sorbitol and trehalose on aggregation and FT-IR amide I spectrum of an immunoglobulin G. Eur J Pharm Biopharm. 2005;59(2):251–61.
Maa YF, Costantino HR, Nguyen PA, Hsu CC. The effect of operating and formulation variables on the morphology of spray-dried protein particles. Pharm Dev Technol. 1997;2(3):213–23.
Soothill JS. Treatment of experimental infections of mice with bacteriophages. J Med Microbiol. 1992;37(4):258–61.
Payne RJH, Jansen VAA. Pharmacokinetic principles of bacteriophage therapy. Clin Pharmacokinet. 2003;42(4):315–25.
Abedon ST. Phage therapy pharmacology: calculating phage dosing. Adv Appl Microbiol. 2011;77:1–40.
Curtright AJ, Abedon ST. Phage therapy: emergent property pharmacology. J Bioanal Biomed. 2011; S6, article 002.
ACKNOWLEDGMENTS AND DISCLOSURES
This work was financially supported by the Australian Research Council (Discovery Project DP150103953). Authors are grateful to Tony Smithyman of Special Phage Services for his valuable discussion and advice. Sharon Leung is a research fellow supported by the University of Sydney. Thaigarajan Parumasivam is a recipient of the Malaysian Government Scholarship. H-KC is funded by the National Institutes of Health (NIH Project no.1R21AI121627-01).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leung, S.S.Y., Parumasivam, T., Gao, F.G. et al. Production of Inhalation Phage Powders Using Spray Freeze Drying and Spray Drying Techniques for Treatment of Respiratory Infections. Pharm Res 33, 1486–1496 (2016). https://doi.org/10.1007/s11095-016-1892-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-016-1892-6