Abstract
Purpose
Previously, a respirable powder (RP) formulation of pirfenidone (PFD) was developed for reducing phototoxic risk; however, PFD-RP demonstrated unacceptable in vitro inhalation performance. The present study aimed to develop a new RP system of PFD with favorable inhalation properties by spray-drying method.
Methods
Spray-dried PFD (SD/PFD) was prepared by spray-drying with L-leucine, and the physicochemical properties and efficacy in an antigen-sensitized airway inflammation model were assessed. A pharmacokinetic study was also conducted after intratracheal and oral administration of PFD formulations.
Results
Regarding powder characterization, SD/PFD had dimpled surface with the mean diameter of 1.793 μm. In next generation impactor analysis, SD/PFD demonstrated high in vitro inhalation performance without the need of carrier particles, and the fine particle fraction of SD/PFD was calculated to be 62.4%. Insufflated SD/PFD (0.3 mg-PFD/rat) attenuated antigen-evoked inflammatory events in the lung, including infiltration of inflammatory cells and myeloperoxidase activity. Systemic exposure level of PFD after insufflation of SD/PFD at the pharmacologically effective dose was 600-fold lower than that after oral administration of PFD at the phototoxic dose.
Conclusion
SD/PFD would be suitable for inhalation, and the utilization of an RP system with SD/PFD would provide a safer medication compared with oral administration of PFD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pirfenidone (PFD), 5-methyl-1-phenylpyridin-2-one, has been shown to have anti-inflammatory and anti-fibrotic properties and to suppress the progression of fibrotic and inflammatory events in the lung, liver, and kidney in experimental animal models (1–4). Potential mechanisms for the suppression of fibrogenesis by PFD have been reported, including the regulation of inflammatory cytokines and growth factors, attenuation of fibroblast proliferation, and inhibition of collagen synthesis (5), and together, these functions may mediate the anti-fibrotic effect of PFD. In clinical settings, PFD is the first orally-administered agent (Esbriet® or Pirespa®) for treating idiopathic pulmonary fibrosis (IPF) in Europe, Japan, India, and China (1,6,7). On the other hand, orally-administered PFD often causes systemic side effects, such as phototoxic skin reactions, gastrointestinal discomfort, and liver dysfunction (6,8,9). In particular, the incidence of phototoxic skin reactions after oral administration of PFD was reported to be over 50% in clinical trial (8). The mechanism of PFD-induced phototoxicity was partially identified in the previous investigation (10) and was attributed to high skin exposure levels of PFD. The International Council on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) guideline S10 (11) describes distribution of a chemical to light-exposed tissues as a critical characteristic for induction of phototoxic events; therefore, modulating the dermal distribution of PFD would reduce the phototoxic risk of PFD in the skin.
Recently, several inhalable formulation systems have been developed for treating respiratory inflammation, and insufflated formulations have been shown to achieve a high lung concentration and low systemic exposure of the drug (12,13). Hence, use of an inhalation system would be a suitable approach for developing PFD medication with a wide safety margin. A respirable powder (RP) formulation of PFD (PFD-RP) was previously developed for reducing phototoxic risk of PFD (14). Insufflated PFD-RP (0.3 mg-PFD/rat) attenuated inflammatory events in an antigen-evoked lung inflammation model and exhibited dramatically lower systemic exposure and skin distribution compared with orally-administered PFD at a phototoxic dose. Although PFD-RP would be useful for treatment of IPF with low phototoxic risk, drawbacks remain regarding its inhalation properties. In the previous investigation, PFD was micronized by jet-milling system, and PFD-RP was prepared with the use of lactose carriers. PFD-RP demonstrated fine dispersion and aerosolization of the jet-milled PFD powders. However, in vitro inhalation performance of PFD-RP analyzed by cascade impactor was unacceptable because the calculated fine particle fraction (FPF) value of PFD-RP was 23.4%. The slightly larger particle size of the jet-milled PFD may result in low treatment efficacy in clinical use. The particle size of a drug influences lung deposition; thus, reducing the size of PFD microparticles may be an appropriate approach to optimize the inhalation performance of a respirable formulation of PFD.
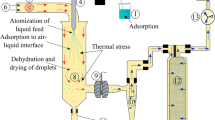
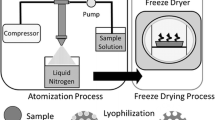
The spray-drying technique is widely used for preparing respirable microparticles with adequate inhalation properties (15,16), and this technology has been used for the production of inhalable dry powders for antibiotics (17–19), non-steroidal anti-inflammatory drugs (20), and immune suppressors (21). Therefore, the spray-drying technique may be suitable for preparing PFD microparticles with favorable inhalation performance. The aim of the present study was to produce a new inhalable powder formulation of PFD with favorable inhalation properties. Spray-dried PFD (SD/PFD) particles were obtained by spray-drying with L-leucine because the addition of L-leucine was shown to significantly increased FPF of a formulation with high dispersibility and flowability (22). The physicochemical characterization of SD/PFD was performed with respect to morphology, particle size distribution, and in vitro inhalation performance, and the pharmacological effects of insufflated SD/PFD were assessed using an experimental lung inflammation model. To verify the risk of side effects, the plasma concentration of PFD after intratracheal administration of SD/PFD was assessed by ultra-performance liquid chromatography equipped with electrospray ionization mass spectrometry (UPLC/ESI-MS), and the systemic exposure of PFD after intratracheal administration of SD/PFD was compared with that after oral administration of PFD at both non-phototoxic and phototoxic doses.
Materials and Methods
Chemicals
PFD was kindly provided by Shionogi (Osaka, Japan). L-leucine was purchased from Sigma–Aldrich (New South Wales, Australia). Ammonium acetate, antipyrine, and trypan blue were bought from Wako Pure Chemical Industries (Osaka, Japan). Aluminum hydroxide gel, horseradish peroxidase, lactose, ovalbumin (OVA), and sodium pentobarbital were purchased from Sigma-Aldrich (St. Louis, MO, USA). Acetonitrile and 3,3′,5,5′-tetramethylbenzidine (TMBZ) were obtained from Honeywell International (Morristown, NJ, USA) and Dojindo Laboratories (Kumamoto, Japan), respectively. All other regents were obtained from commercial sources.
Powder Preparation
PFD and L-leucine were dissolved in water containing 30% ethanol at a weight ratio of 90:10, with a total solid content of 10 mg/ml. SD/PFD was prepared by spray-drying of the solution using a Buchi 290 spray dryer under open-loop conditions using dehumidified air (Buchi Dehumidifier B-296) as the drying gas at a solution feed rate of 2 mL/min, aspiration rate of 38 m3/h, and atomization rate of 819 NL/h. The inlet and outlet temperatures were 60 and 43°C, respectively. Spray-dried powders were stored in a desiccator containing silica gel at 20 ± 3°C until used.
Scanning Electron Microscopy (SEM)
Representative scanning electron microscopic images of SD/PFD were taken using Hitachi S-4500 FESEM (Hitachi, Tokyo, Japan) with approximately 15 nm gold coating. For the scanning electron microscopic observation, SD/PFD was fixed on an aluminum sample holder using double-sided carbon sticky tape.
Particle Size Distribution
The particle size distribution of SD/PFD was measured by laser diffraction using a Mastersizer 2000 (Malvern Instruments, UK). The real and imaginary refractive indices were set to 1.59 and 0.1, respectively. The dispersant (air) refractive index was set to 1.000. The powders were dispersed through the measurement window with compressed air at 1 bar and 3.5 bar for the spray freeze dry and spray dry formulations, respectively, using a Scirocco 2000 dry powder module (Malvern Instruments, UK). All measurements were performed in triplicate. Size was expressed by the volume median diameter (VMD) and width was defined as [D(υ, 90)–D(υ, 10)]/ D(υ, 50), where D(υ, 10), D(υ, 50), and D(υ, 90) were the equivalent volume diameters at 10, 50, and 90% cumulative volumes, respectively.
In Vitro Inhalation Performance
The in vitro inhalation performance of SD/PFD was assessed by dispersing 5 mg of SD/PFD into a Next Generation Impactor (NGI) at 100 L/min for 2.4 s using an OsmohalerTM. Size 3 hydroxypropyl methylcellulose capsules (Capsugel, New South Wales, Australia) were used for powder loading. All dispersion experiments were conducted in triplicate (n = 3). The impactor stages were coated with silicon grease (Slipicone®; DC Products, Victoria, Australia) before testing to minimize particle bounce. After dispersion, the powder deposited on the capsule, inhaler, adaptor, and NGI stages were exhaustively washed with 3 ml 70% methanol–water mixture. Drug content at each location was quantified using a high performance liquid chromatography (HPLC) system from Shimadzu Corporation (Kyoto, Japan) and a NovaPak C18 column (4 μm, 3.9 × 150 mm; Waters, USA). The mobile phase was a mixture of methanol (50%) and water (50%, pH adjusted to 4.5 using orthophosphate acid). UV absorbance at a wavelength of 324 nm was used to detect PFD. The flow rate was 1 mL/min and the retention time for PFD was 2.5 min. The calibration curves were linear in the concentration range of 0.05–1 mg/mL (R2 = 0.999, n = 3).
The lower cutoff diameters of NGI stages 1–7 at 100 L/min were 6.12, 3.42, 2.18, 1.31, 0.72, 0.40, and 0.24 μm, calculated by adjustment equations given in Appendix XII C of the British Pharmacopoeia (2011). The emitted fraction (EF) was the total amount of powder that exited the inhaler with respect to the recovered dose. The FPF was defined as the mass fraction of particles ≤ 5.0 μm with respect to the emitted dose. The cumulative fraction of particles with aerodynamic diameter ≤ 5.0 μm, corresponding to the FPF, was determined by interpolation.
In Vivo Preparations
Male Sprague–Dawley rats at 9–12 weeks of age (260–470 g body weight) were purchased from SLC Inc. (Hamamatsu, Japan), housed in the laboratory with free access to food and water, and maintained under a 12-h dark/light cycle in a room with controlled temperature (24 ± 1°C) and humidity (55 ± 5%). All procedures performed in the present study were conducted according to the guidelines approved by the Institutional Animal Care and Ethical Committee of the University of Shizuoka.
In the present in vivo experiments, SD/PFD was blended with lactose (43–90 μm) because the amount of drug required for in vivo experiments was too little to handle. The ratio of SD/PFD to lactose was 3:50 (w/w). For pharmacological experiments, RP formulation of OVA (OVA-RP) was prepared as reported previously (23). OVA particles and erythritol were first ground to fine powders with a pestle and mortar and then milled with an A-O JET MILL (Seishin Enterprise, Tokyo, Japan) at a pusher nozzle pressure and grinding nozzle pressure of 6.0 and 5.5 MPa, respectively. The ratio of OVA to erythritol was 1:400 (w/w). Micronized OVA was decompounded with a 10-fold amount of erythritol carrier particles in a plastic bag for 3 min, and the obtained dry powders of OVA were stored in a vacuum desiccator until tested.
For evaluating pharmacological efficacy, experimental lung inflammation model rats were prepared in accordance with the previous report (23) (Supplementary Fig. 1). Briefly, rats were sensitized by intraperitoneal injection of 100 μg of OVA with 5 mg aluminum hydroxide gel on days 0, 7, and 14. Then, they were anesthetized with sodium pentobarbital (50 mg/kg, i.p.) and received intratracheal administration of OVA-RP (100 μg-OVA/rat) powder at 24 h after the last OVA sensitization. At 1 h before the OVA challenge, SD/PFD (0.3 mg-PFD/rat) or lactose as control-RP was administered via intratracheal insufflation using a PennCentury insufflation powder delivery device (DP-4, INA Research Inc., Nagoya, Japan). A bolus (2 mL) of air from an attached syringe was used to deliver the preloaded powder from the chamber of the insufflator into the airway of the rats. At 24 h after OVA challenge, rats were exsanguinated via the descending aorta under anesthesia with sodium pentobarbital, and the lungs were perfused with 30 mL of saline and removed. For pharmacokinetic analysis, rats were fasted for approximately 18 h before drug administration, and SD/PFD was administered via intratracheal insufflation. PFD dissolved in water containing 0.05% Tween 20 was orally administered to fasted rats (30 and 160 mg/kg).
Total Cell Counting in Bronchoalveolar Lavage Fluid
Bronchoalveolar lavage fluid (BALF) is widely used for the differential diagnosis or monitoring of lung inflammatory, and BALF cell patterns reflect inflammatory cell profiles in affected lung tissues (24). Total cell number in BALF also related to the number of inflammatory cells infiltrating in the rat lung (25); therefore, total cell counting in BALF was carried out in accordance with the previous report (14). The animals were euthanized at 24 h after OVA challenge, and BALF was immediately obtained by washing the lung via airways twice with 5 mL of phosphate buffered saline (PBS). Cells in BALF were isolated by centrifugation at 112 × g for 10 min. The isolated cells were re-suspended by adding 1 mL of PBS and stained by adding an equal amount of 0.2% trypan blue. The total cell number in BALF was counted using a Burker-Turk counting chamber.
Measurement of Myeloperoxidase Activity
Enzymatic detection of myeloperoxidase (MPO) in BALF was performed in accordance with a previous report (12,23). Briefly, assay mixtures consisted of 40 μL of H2O2 (final concentration: 0.3 mM) in 80 mM sodium phosphate buffer (pH5.4) and 50 μL of BALF sample. The reaction was initiated by addition of 10 μL of TMBZ (final concentration: 1.6 mM) in dimethyl sulfoxide at 37°C and stopped after 2 min by addition of 0.18 M H2SO4. Subsequently, optical density was determined at 450 nm. A titration curve of horseradish peroxidase was used for the calculation of MPO activity, which was expressed in arbitrary units. All samples were assayed in duplicate, and optical densities in all assays were measured using a SAFIRE microplate reader (TECAN, Männedorf, Switzerland).
Plasma Concentration of PFD After Intratracheal or Oral Administration
Blood samples were taken in a volume of 200 μL from the tail vein at the indicated time points (5, 15, 30, 45 min, 1, 2, 3, 4, and 6 h) after intratracheal administration of SD/PFD (0.3 mg-PFD/rat) or oral administration of PFD (30 and 160 mg/kg). The blood samples were centrifuged (10,000 × g, 10 min, 4°C) to prepare plasma samples, which were then kept frozen at below −20°C until analyzed. Plasma samples were deproteinized by the addition of acetonitrile (plasma:acetonitrile = 2:5), mixed, and centrifuged (2000 rpm, 1 min, 4°C). The supernatants were then filtered, and 50% acetonitrile solution containing antipyrine (5 μg/mL), an internal standard, was added for UPLC/ESI-MS analysis.
UPLC Analysis
The concentrations of PFD in the plasma were determined by UPLC/ESI-MS analysis. The UPLC/ESI-MS system consisted of a Waters Acquity UPLCTM system (Waters, Milford, MA, USA), which included a binary solvent manager, a sample manager, a column compartment, and a Micromass SQ detector connected with Waters Masslynx v 4.1. A Waters Acquity UPLCTM BEH C18 column (particle size: 1.7 μm, column size: ϕ2.1 × 50 mm; Waters) was used, and column temperature was maintained at 40°C. The standards and samples were separated using a gradient mobile phase consisting of Milli-Q containing 5 mM ammonium acetate (A) and methanol (B). The gradient condition of the mobile phase was 0–0.5 min, 75% A; 0.5–4 min, 75–40% A; 4–5 min, 5% A; 5–6 min, 75% A, and the flow rate was set at 0.25 mL/min. Analysis was carried out using SIR for specific m/z: 186 [M + 1]+ for PFD; and 189 [M + 1]+ for antipyrine (internal standard). The present UPLC-ESI/MS protocol for the determination of PFD was validated in terms of linearity, accuracy, and precision according to the ICH guidelines “Q2B Validation of Analytical Procedures: Methodology.”
Pharmacokinetic Analysis
Pharmacokinetic characterization in the plasma was performed by non-compartmental analysis as implemented in WinNonlin Professional Version 5.2 (Pharsight Corporation, Mountain View, CA, USA), and maximum concentration (C max), elimination half-life (t 1/2), area under concentration versus time curve (AUC0-inf), and mean residence time (MRT) were calculated based on the obtained plasma concentration-time curves.
Data Analysis
For statistical comparisons, one-way ANOVA with pairwise comparison by Fisher’s least significant difference test was used. A p value of less than 0.05 was considered significant for all analyses.
Results and Discussion
Physicochemical Properties of Spray-Dried Pirfenidone
Spray-drying of pharmaceuticals has been widely used as a powder manufacturing technology for producing inhalable dry powders due to its ability to modulate particle properties, including particle density, particle size, and surface morphology (26). The one-step process for preparing inhalable powders from solution, suspension, or emulsion is also an advantage of spray-drying technology. Hence, the spray-drying method was employed for preparing inhalable PFD particles. Dispersibility is also an important particle property for inhalable particles, and addition of excipients, including amino acids, lecithin, and magnesium stearate, has been used for improving dispersibility (27). In particular, L-leucine is widely used as a dispersiblity enhancer for preparing inhalable powders by spray-drying (26), and L-leucine was shown to significantly increased FPF of a formulation with high dispersibility and flowability compared with other amino acids (22). In this context, SD/PFD was prepared by spray-drying of a 30% ethanol solution containing PFD and L-leucine (9:1) in the present investigation, and the physicochemical properties of the resultant SD/PFD were assessed focusing on particle morphology, particle size, and in vitro inhalation performance.
The particle morphology of SD/PFD was observed by SEM, and the powders produced had corrugated surface (Fig. 1a). Addition of L-leucine resulted in spray-dried powders with dimpled surfaces, and the surface roughness of inhalable powders made a contribution to a reduction in aerodynamic diameter (22). Therefore, SD/PFD may have a favorable surface morphology for inhalation therapy. Particle size is a key particle property in defining the deposition pattern of drug particles delivered to the respiratory system using inhalers (28), and thus, the particle size distribution of the prepared SD/PFD powders was measured by laser diffraction analysis (Fig. 1b). The mean diameter and SPAN factor of the prepared SD/PFD particles were calculated to be 1.793 μm and 1.533, respectively. According to the previous report (29), inhaled powders with a diameter of around 1–5 μm are suitable for deposition in small airways and alveoli, and particles smaller than 3 μm, in particular, have a higher potential for reaching lower airways. Although particles with diameter of less than 0.5 μm can be inhaled into the deep lung, these particles are likely to be exhaled before deposition. Thus, the prepared SD/PFD powders have an optimal size distribution for pulmonary delivery, and inhalation of SD/PFD may have a high therapeutic potential for IPF. For further characterization, the in vitro inhalation performance of SD/PFD was examined using the NGI system with OsmohalerTM (Fig. 1c). From the deposition profile obtained from the NGI analysis, the emitted dose and FPF value of SD/PFD were calculated to be 73.3 and 62.4%, respectively. Interestingly, SD/PFD particles achieved a high FPF value without the need of carrier particles. In the previous investigation, PFD-RP was prepared with lactose carriers, and the FPF value of PFD-RP obtained from cascade impactor analysis was found to be 23.4% (14); therefore, SD/PFD would allow more efficient pulmonary delivery compared with PFD-RP by comparison of the FPF values, and SD/PFD may be made available as a carrier-free inhalable powder formulation for the treatment of IPF. In the development of RP systems, carrier particles, such as lactose and other sugars, are usually blended for improving the flowability and dispersibility of drug microparticles and nanoparticles (30); however, the drug loading amount is limited in carrier-blended RP systems because of the presence of excessive carrier particles (31,32). On the other hand, SD/PFD would achieve high drug loading amount due to the lack of carrier particle requirement for inhalation, possibly leading to better clinical outcomes.
In vitro particle characterization of SD/PFD. (a) A scanning electron microscopic image of SD/PFD. Bar represents 5 μm. (b) Particle size distribution of SD/PFD as determined by laser diffraction particle size analysis. Solid line, frequency; and dotted line, cumulative undersize fraction curve. (c) Deposition pattern of SD/PFD powders in the NGI. Data represent mean ± SD for three experiments. The number in parenthesis represents a cutoff diameter (μm) for each stage.
Anti-Inflammatory Effects in an Experimental Airway Inflammation Model
To clarify the therapeutic potential of SD/PFD, the anti-inflammatory effects of insufflated SD/PFD were evaluated in an antigen-evoked lung inflammation model (23). SD/PFD was intratracheally administered at 1 h before OVA-RP challenge, followed by collection of BALF for counting the number of inflammatory cells at 24 h after OVA-RP insufflation (Fig. 2a). SD/PFD at a dose of 0.3 mg-PFD/rat was employed for intratracheal administration because insufflated PFD-RP at 0.3 mg-PFD/rat or higher was reported to attenuate inflammatory events in the airway system (14). After intratracheal administration of OVA-RP, significant recruitment of inflammatory cells in BALF was observed as evidenced by approximately 4.8-fold increase of total cell number, mainly consisting of monocytes and neutrophils. On the other hand, recruitment of inflammatory cells in BALF in response to insufflated OVA-RP was significantly attenuated by pre-insufflation of SD/PFD (0.3 mg-PFD/rat) with approximately 83% reduction of infiltrated cells, and no significant differences were observed between non-sensitized and OVA-sensitized rats pretreated with SD/PFD. These results suggested that insufflated SD/PFD may have a therapeutic potential for airway inflammation.
Anti-inflammatory effects of insufflated SD/PFD in OVA-evoked airway inflammation model. At 24 h after the OVA challenge, (a) recruited inflammatory cells and (b) MPO activity in BALF were monitored with or without pre-insufflation of SD/PFD (0.3 mg-PFD/rat). Data represent mean ± SE for six experiments. *, P < 0.05 and **, P < 0.01 with respect to non-sensitized rats with insufflation of control-RP. ##, P < 0.01 with respect to OVA-sensitized rats with insufflation of control-RP.
In the OVA-evoked airway inflammation model, infiltration of neutrophils was observed as one of the main infiltrating inflammatory cells after OVA-RP challenge, consistent with the previous report (23). MPO is a pro-inflammatory and pro-oxidant enzyme, mainly released from activated neutrophils and macrophages (33); therefore, for further characterization of the anti-inflammatory effects of SD/PFD in the antigen-evoked asthma/COPD model, MPO activity in BALF was also investigated (Fig. 2b). OVA-RP challenge caused an approximate 2.5-fold elevation of MPO level in BALF, suggesting the development of pulmonary neutrophilia in OVA-sensitized rats. Pretreatment of SD/PFD tended to suppress the up-regulation of MPO activity in BALF caused by OVA-RP challenge, possibly indicating its potential for treatment of neutrophilia in the airway system. In the previous reports, an increase of neutrophils in bronchoalveolar lavage was observed in 70–90% of IPF patients (34), and neutrophilic inflammation was reported to be a pathogenic factor of IPF (35). Therefore, the use of an antigen-evoked asthma/COPD model would be adequate for evaluating the pharmacological efficacy of insufflated SD/PFD, and the present results suggest the topical therapeutic potential of SD/PFD against pulmonary inflammation in the early stages of IPF.
In the previous report, anti-inflammatory effects of orally-administered PFD at 30 mg/kg were confirmed in experimental models, including antigen-induced and LPS-induced acute inflammation models (36). On the other hand, a high anti-inflammatory effect was observed after pre-insufflation of SD/PFD at 0.3 mg-PFD/rat (approximately 1 mg-PFD/kg) in the present study, suggesting that SD/PFD may be effective at lower doses compared with orally-administered PFD. Although this comparison may not be appropriate due to the different experimental conditions, SD/PFD may achieve marked reductions in the pharmacologically effective dose of PFD for lung disease. Regarding treatment of pulmonary fibrosis, the pharmacologically effective dose of RP systems of PFD for treating pulmonary fibrosis is still unclear. In the previous investigation, fibrocyte accumulation in the lung was attenuated after oral administration of PFD at 300 mg/kg/day for 2 weeks in a bleomycin-induced pulmonary fibrosis model (37). Thus, the appropriate dosage of RP formulations of PFD for treatment of pulmonary fibrosis should be further investigated in pulmonary fibrosis models.
Pharmacokinetic Analysis of Pirfenidone After Oral or Intratracheal Administration
According to the in vivo pharmacological experiments, insufflated SD/PFD (0.3 mg-PFD/rat) achieved favorable anti-inflammatory outcomes in an antigen-evoked airway inflammation model; however, systemic exposure risk after insufflation of SD/PFD is still unclear. Hence, a pharmacokinetic study of PFD was conducted after intratracheal administration of SD/PFD at a pharmacologically effective dose (0.3 mg-PFD/rat) to investigate systemic exposure risk. In general, particle size reduction results in high membrane permeability and improved bioavailability (38). Additionally, permeability in the lung is higher than that in the intestine because the lung has a large surface area attributed to numerous alveoli and the thin layer of alveolar cells (39,40). The RP formulations of PFD was developed for reducing systemic exposure of PFD compared with oral administration of PFD, possibly leading to low toxicity risk (14); therefore, to investigate the toxicity risk of SD/PFD, a comparative pharmacokinetic study of PFD in rats was also performed after oral administration of PFD at non-phototoxic and phototoxic doses (30 and 160 mg/kg, respectively) (10). Plasma concentration-time curves of PFD were obtained by UPLC/ESI-MS analysis of samples taken after intratracheal and oral administration of PFD formulations (Fig. 3). The pharmacokinetic parameters of PFD were calculated on the basis of the plasma concentration-time profiles obtained (Table I). After intratracheal administration of SD/PFD (0.3 mg-PFD/rat), the plasma concentration reached C max within 5 min, as did orally-administered PFD (30 and 160 mg/kg). Plasma concentrations then rapidly decreased with a t 1/2 of approximately 0.3–0.5 h. According to the calculated C max and AUC0–inf in the plasma, the systemic exposure level of PFD after insufflation of SD/PFD at the pharmacologically effective dose was much lower than those after oral administration of PFD at both non-phototoxic and phototoxic doses. Compared with orally-administered PFD at the phototoxic dose, insufflated SD/PFD at the pharmacologically effective dose led to approximately 280- and 600-fold reductions in C max and AUC0–inf values, respectively. In addition, 42- and 52-fold differences in C max and AUC0–inf values, respectively, were still observed between insufflated SD/PFD at the pharmacologically effective dose and oral administration of PFD at the non-phototoxic dose. On the other hand, there were no differences in the duration of systemic exposure of PFD among the intratracheal and oral administrations of PFD formulations on the basis of the t 1/2 and MRT values. From these findings, compared with oral therapy of PFD for IPF, inhalation therapy with the use of SD/PFD would attenuate systemic exposure risk with improved photosafety of PFD.
Plasma concentration-time profiles of PFD after intratracheal administration of SD/PFD and oral administration of PFD in rats. ●, insufflated SD/PFD at a pharmacologically effective dose (0.3 mg-PFD/rat); △, orally-administered PFD at a phototoxic dose (160 mg/kg); and ▽, orally-administered PFD at a non-phototoxic dose (30 mg/kg). Each value represents mean ± SE for five rats.
In the previous investigation, insufflated PFD-RP at the pharmacologically effective dose indicated low systemic exposure levels, and deposition to UV-exposed tissues was reduced after insufflation of PFD-RP compared with orally-administered PFD at both non-phototoxic and phototoxic doses. Therefore, insufflated SD/PFD may similarly modurate deposition of PFD in light-exposed tissues due to its low systemic exposure. Furthermore, the limited systemic exposure after insufflation of RP formulations of PFD may attenuate other adverse effects induced by orally-administered PFD, including hepatic dysfunction and gastrointestinal discomfort. Thus, further investigations of RP formulation of PFD focusing on hepatotoxicity and gastrointestinal tract disturbance are warranted. Inhalation therapy with the use of RP systems for PFD would be an attractive alternative to current oral therapy of PFD for treating IPF.
Conclusion
A new RP system of PFD with favorable inhalation properties and lowered systemic exposure risk was developed using the spray-drying method. Prepared SD/PFD powder had favorable surface morphology and particle size distribution for inhalation, and the high in vitro inhalation performance of SD/PFD was observed without the need of carrier particles in NGI analysis. In the antigen-evoked airway inflammation model, insufflated SD/PFD attenuated inflammatory events in the lung after OVA-RP challenge. Regarding the pharmacokinetic behaviors, insufflation of SD/PFD at the pharmacologically effective dose reduced systemic exposure levels of PFD compared with orally-administered PFD at both non-phototoxic and phototoxic dose, suggesting a lowered risk of systemic side effects. From these findings, the RP system with the use of SD/PFD would allow effective treatment of IPF with a wide safety margin.
Abbreviations
- AUC0-inf :
-
Area under the concentration versus time curve
- BALF:
-
Bronchoalveolar lavage fluid
- C max :
-
Maximum concentration
- EF:
-
Emitted fraction
- FPF:
-
Fine particle fraction
- HPLC:
-
High performance liquid chromatography
- ICH:
-
The International Council on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for human use
- IPF:
-
Idiopathic pulmonary fibrosis
- MPO:
-
Myeloperoxidase
- MRT:
-
Mean residence time
- NGI:
-
Next generation impactor
- OVA:
-
Ovalbumin
- OVA-RP:
-
Respirable powder formulation of ovalbumin
- PBS:
-
Phosphate buffered saline
- PFD:
-
Pirfenidone
- PFD-RP:
-
Respirable powder formulation of pirfenidone
- RP:
-
Respirable powder
- SD/PFD:
-
Spray-dried pirfenidone
- SEM:
-
Scanning electron microscopy
- t 1/2 :
-
Elimination half-life
- TMBZ:
-
3,3′,5,5′-tetramethylbenzidine
- UPLC/ESI-MS:
-
Ultra-performance liquid chromatography equipped with electrospray ionization mass spectrometry
- VMD:
-
Volume median diameter
References
Schaefer CJ, Ruhrmund DW, Pan L, Seiwert SD, Kossen K. Antifibrotic activities of pirfenidone in animal models. Eur Respir Rev. 2011;20:85–97.
Iyer SN, Gurujeyalakshmi G, Giri SN. Effects of pirfenidone on transforming growth factor-beta gene expression at the transcriptional level in bleomycin hamster model of lung fibrosis. J Pharmacol Exp Ther. 1999;291:367–73.
Hisatomi K, Mukae H, Sakamoto N, Ishimatsu Y, Kakugawa T, Hara S, et al. Pirfenidone inhibits TGF-beta1-induced over-expression of collagen type I and heat shock protein 47 in A549 cells. BMC Pulm Med. 2012;12:24.
Lasky J. Pirfenidone. IDrugs. 2004;7:166–72.
Takeda Y, Tsujino K, Kijima T, Kumanogoh A. Efficacy and safety of pirfenidone for idiopathic pulmonary fibrosis. Patient Prefer Adher. 2014;8:361–70.
Hilberg O, Simonsen U, du Bois R, Bendstrup E. Pirfenidone: significant treatment effects in idiopathic pulmonary fibrosis. Clin Respir J. 2012;6:131–43.
Richeldi L, Yasothan U, Kirkpatrick P. Pirfenidone. Nat Rev Drug Discov. 2011;10:489–90.
Taniguchi H, Ebina M, Kondoh Y, Ogura T, Azuma A, Suga M, et al. Pirfenidone in idiopathic pulmonary fibrosis. Eur Respir J. 2010;35:821–9.
Carter NJ. Pirfenidone: in idiopathic pulmonary fibrosis. Drugs. 2011;71:1721–32.
Seto Y, Inoue R, Kato M, Yamada S, Onoue S. Photosafety assessments on pirfenidone: photochemical, photobiological, and pharmacokinetic characterization. J Photochem Photobiol B. 2013;120:44–51.
International Council on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH). ICH Guideline S10 Guidance on photosafety evaluation of pharmaceuticals. 2013.
Onoue S, Aoki Y, Kawabata Y, Matsui T, Yamamoto K, Sato H, et al. Development of inhalable nanocrystalline solid dispersion of tranilast for airway inflammatory diseases. J Pharm Sci. 2011;100:622–33.
Onoue S, Sato H, Kawabata Y, Mizumoto T, Hashimoto N, Yamada S. In vitro and in vivo characterization on amorphous solid dispersion of cyclosporine A for inhalation therapy. J Control Release. 2009;138:16–23.
Onoue S, Seto Y, Kato M, Aoki Y, Kojo Y, Yamada S. Inhalable powder formulation of pirfenidone with reduced phototoxic risk for treatment of pulmonary fibrosis. Pharm Res. 2013;30:1586–96.
Buttini F, Colombo P, Rossi A, Sonvico F, Colombo G. Particles and powders: tools of innovation for non-invasive drug administration. J Control Release. 2012;161:693–702.
Lin YW, Wong J, Qu L, Chan HK, Zhou QT. Powder production and particle engineering for dry powder inhaler formulations. Curr Pharm Des. 2015;21:3902–16.
Belotti S, Rossi A, Colombo P, Bettini R, Rekkas D, Politis S, et al. Spray-dried amikacin sulphate powder for inhalation in cystic fibrosis patients: the role of ethanol in particle formation. Eur J Pharm Biopharm. 2015;93:165–72.
Lee SH, Teo J, Heng D, Zhao Y, Ng WK, Chan HK, et al. A novel inhaled multi-pronged attack against respiratory bacteria. Eur J Pharm Sci. 2015;70:37–44.
Zhou QT, Morton DA, Yu HH, Jacob J, Wang J, Li J, et al. Colistin powders with high aerosolisation efficiency for respiratory infection: preparation and in vitro evaluation. J Pharm Sci. 2013;102:3736–47.
Aquino RP, Stigliani M, Del Gaudio P, Mencherini T, Sansone F, Russo P. Nanospray drying as a novel technique for the manufacturing of inhalable NSAID powders. Scientific World J. 2014;2014:838410.
Onoue S, Sato H, Ogawa K, Kojo Y, Aoki Y, Kawabata Y, et al. Inhalable dry-emulsion formulation of cyclosporine A with improved anti-inflammatory effects in experimental asthma/COPD-model rats. Eur J Pharm Biopharm. 2012;80:54–60.
Chew NY, Shekunov BY, Tong HH, Chow AH, Savage C, Wu J, et al. Effect of amino acids on the dispersion of disodium cromoglycate powders. J Pharm Sci. 2005;94:2289–300.
Misaka S, Sato H, Yamauchi Y, Onoue S, Yamada S. Novel dry powder formulation of ovalbumin for development of COPD-like animal model: physicochemical characterization and biomarker profiling in rats. Eur J Pharm Sci. 2009;37:469–76.
Costabel U, Guzman J. Bronchoalveolar lavage in interstitial lung disease. Curr Opin Pulm Med. 2001;7:255–61.
Misaka S, Aoki Y, Karaki S, Kuwahara A, Mizumoto T, Onoue S, et al. Inhalable powder formulation of a stabilized vasoactive intestinal peptide (VIP) derivative: anti-inflammatory effect in experimental asthmatic rats. Peptides. 2010;31:72–8.
Vehring R. Pharmaceutical particle engineering via spray drying. Pharm Res. 2008;25:999–1022.
Begat R, Price R, Harris H, Morton DAV, Staniforth JN. The influence of force control agents on the cohesive-adhesive balance in dry powder inhaler formulations. KONA. 2005;23:109–21.
Suarez S, Hickey AJ. Drug properties affecting aerosol behavior. Respir Care. 2000;45:652–66.
Labiris NR, Dolovich MB. Pulmonary drug delivery. part I: physiological factors affecting therapeutic effectiveness of aerosolized medications. Br J Clin Pharmacol. 2003;56:588–99.
Pilcer G, Amighi K. Formulation strategy and use of excipients in pulmonary drug delivery. Int J Pharm. 2010;392:1–19.
Healy AM, Amaro MI, Paluch KJ, Tajber L. Dry powders for oral inhalation free of lactose carrier particles. Adv Drug Deliv Rev. 2014;75:32–52.
Zhou QT, Leung SS, Tang P, Parumasivam T, Loh ZH, Chan HK. Inhaled formulations and pulmonary drug delivery systems for respiratory infections. Adv Drug Deliv Rev. 2015;85:83–99.
Winterbourn CC, Vissers MC, Kettle AJ. Myeloperoxidase. Curr Opin Hematol. 2000;7:53–8.
Pesci A, Ricchiuti E, Ruggiero R, De Micheli A. Bronchoalveolar lavage in idiopathic pulmonary fibrosis: what does it tell us? Respir Med. 2010;104 Suppl 1:S70–73.
Beeh KM, Beier J, Kornmann O, Buhl R. Neutrophilic inflammation in induced sputum of patients with idiopathic pulmonary fibrosis. Sarcoidosis Vasc Diffuse Lung Dis. 2003;20:138–43.
Spond J, Case N, Chapman RW, Crawley Y, Egan RW, Fine J, et al. Inhibition of experimental acute pulmonary inflammation by pirfenidone. Pulm Pharmacol Ther. 2003;16:207–14.
Inomata M, Kamio K, Azuma A, Matsuda K, Kokuho N, Miura Y, et al. Pirfenidone inhibits fibrocyte accumulation in the lungs in bleomycin-induced murine pulmonary fibrosis. Respir Res. 2014;15:16.
Onoue S, Yamada S, Chan HK. Nanodrugs: pharmacokinetics and safety. Int J Nanomed. 2014;9:1025–37.
Patton JS, Fishburn CS, Weers JG. The lungs as a portal of entry for systemic drug delivery. Proc Am Thorac Soc. 2004;1:338–44.
Patton JS, Byron PR. Inhaling medicines: delivering drugs to the body through the lungs. Nat Rev Drug Discov. 2007;6:67–74.
ACKNOWLEDGMENTS AND DISCLOSURES
This work was supported by Grant-in-Aid for Young Scientists (B) from the Ministry of Education, Science, Sports and Culture, Japan. Sharon Shui Yee Leung was supported by Faculty of Pharmacy postdoctoral fellowship at the University of Sydney.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
The timeline for the pharmacological experiment for evaluating the anti-inflammatory effects of insufflated SD/PFD. i.p.: intraperitoneal; and i.t.: intratracheal administration. (GIF 23 kb)
Rights and permissions
About this article
Cite this article
Seto, Y., Suzuki, G., Leung, S.S.Y. et al. Development of an Improved Inhalable Powder Formulation of Pirfenidone by Spray-Drying: In Vitro Characterization and Pharmacokinetic Profiling. Pharm Res 33, 1447–1455 (2016). https://doi.org/10.1007/s11095-016-1887-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-016-1887-3