Abstract
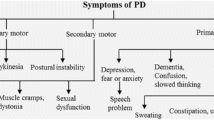
Parkinson's disease (PD) is associated with dopamine depletion in the striatum owing to the selective and progressive loss of the nigrostriatal dopaminergic neurons, which results in motor dysfunction and secondary clinical manifestations. The dopamine level in the striatum is preserved because of the innervation of the substantia nigra (SN) dopaminergic neurons into it. Therefore, protection of the SN neurons is crucial for maintaining the dopamine level in the striatum and for ensuring the desired motor coordination. Several strategies have been devised to protect the degenerating dopaminergic neurons or to restore the dopamine levels for treating PD. Most of the methods focus exclusively on preventing cell body death in the neurons. Although advances have been made in understanding the disease, the search for disease-modifying drugs is an ongoing process. The present review describes the evidence from studies involving patients with PD as well as PD models that axon terminals are highly vulnerable to exogenous and endogenous insults and degenerate at the early stage of the disease. Impairment of mitochondrial dynamics, Ca2+ homeostasis, axonal transport, and loss of plasticity of axon terminals appear before the neuronal degeneration in PD. Furthermore, distortion of synaptic morphology and reduction of postsynaptic dendritic spines are the neuropathological hallmarks of early-stage disease. Thus, the review proposes a shift in focus from discerning the mechanism of neuronal cell body loss and targeting it to an entirely different approach of preventing axonal degeneration. The review also suggests appropriate strategies to prevent the loss of synaptic terminals, which could induce regrowth of the axon and its auxiliary fibers and might offer relief from the symptomatic features of PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson's disease (PD) is a basal ganglia disorder caused by progressive and selective degeneration of the neurons. This degeneration consequently depletes the dopamine levels in the striatum, which results in motor dysfunction and loss of cognitive functions in late-stage PD. Dopamine is a neurotransmitter that regulates the fine motor activities, higher cognitive functions, and feelings of pleasure and rewards. Moreover, dopamine is the metabolic precursor of norepinephrine, another crucial neurotransmitter in the brain. Dopamine is also involved in controlling synaptic transmission, axonal excitability, and dendritic integration [1]. This catecholamine is metabolized and stored in the specialized tyrosine hydroxylase (TH)-positive nerve cells, the dopaminergic neurons. A set of identically derived dopaminergic projections forms a dopaminergic pathway, and each pathway innervates into a specific region of the brain. The mammalian brain consists of various major and minor dopaminergic pathways [1, 2]. Among the 10 different pathways, only four are prominent. The nigrostriatal, mesolimbic, mesocortical, and tuberoinfundibular pathways are the key pathways, and in PD pathology, the degeneration selectively occurs in the nigrostriatal system. The soma or cell bodies of the nigrostriatal dopaminergic neurons are embedded in the substantia nigra (SN), and the axons are innervated into the striatum. Thus, the idiopathic loss of SN neurons depletes the striatal dopamine level.
Numerous studies on genetics, post-mortem human brain, and animal and cellular models have revealed the role of redundant proteins, damaged mitochondria, apoptosis, autophagy, and neuroinflammation in disease pathogenesis [3,4,5]. However, these cellular pathologies are also common to other neurodegenerative diseases [6, 7]. Moreover, the enhanced susceptibility of the SN dopaminergic neurons to endogenous insults is not well understood. It has been opined that selective SN neuronal death could be due to Lewy body (LB) toxicity [8]. LBs are heterogenous protein aggregates rich in fibrillar α-synuclein and ubiquitinated proteins. Nonetheless, cytoskeletal and neuronal synaptic vesicle trafficking proteins are also present in the LBs formed in the degenerating nigral neurons and astrocytes [9]. Researchers have accepted the role of LB toxicity in early-onset PD after the publication of reports on genetic predisposition in genes (SNCA) encoding α-synuclein. This theory gained even more attention when aberrant α-synuclein-mediated PD pathology was found to be disseminated in the healthy dopaminergic neuronal graft through synaptic leakage [10]. Since α-synuclein is a synaptic protein and is abundant near the terminals, the extensive axonal arborization of the nigrostriatal neuron increases the α-synuclein levels and, therefore, enhances its susceptibility to degeneration.
The SN dopaminergic neurons are long, thin, and unmyelinated and have an extensive arborized axon and a high synapse to neuronal soma ratio. This unique cellular architecture of the SN dopaminergic neurons differentiates them from other dopamine-containing neurons, including those in the ventral tegmental area (VTA) [8, 11]. The high density of synapses connected to a neuron's cell body demands increased energy for proper functioning. Simultaneously, the narrow width of the axon and the associated terminals allows a controlled supply of mitochondria, several essential proteins, and vesicular structures to the presynaptic terminals through axonal trafficking [12, 13]. Therefore, the SN neuron's demand–supply equilibrium remains at the edge, and the bioenergetic demand is considerably high at the synaptic site [14]. To match the elevated bioenergetic demand at the synapse, mitochondrial dynamics, anterograde transportation, and its biogenesis increase in the SN neurons [15,16,17]. The mitochondria present in the neurons govern several neurophysiological processes, including the active axonal trafficking of cargos, mobilization of synaptic vesicles, calcium ion (Ca2+) homeostasis, and neurotransmission. Dysregulation of the mitochondrial dynamics disturbs several intraneuronal functions [18,19,20]. Moreover, the elevated bioenergy at the synaptic terminal results in enhanced oxidative stress and dopamine oxidation in the neuron if the delicate supply-chain equilibrium is disturbed [13]. The dysregulation of the mitochondrial dynamics leads to protein accumulation, excessive Ca2+ release into the cytosol, and disturbance of synaptic events [13, 19]. Furthermore, the high cytosolic level of free Ca2+, which is caused by the low intrinsic calcium buffering capacity of the SN neuron, is equally responsible for its preferential vulnerability [8]. Thus, the cellular architecture and the neurophysiology of the PD-related dopaminergic neurons are the reasons for the increased vulnerability.
Notwithstanding the several advances in understanding PD, including pathogenesis, selective histological loss, and the complex interplay of genetic and environmental factors, the specific cause for disease onset and progression at the cellular level remains unknown. Most of the recent investigations have focused on pathogenesis, alteration in dopaminergic neuron counts, and experimental therapeutics. However, the search for a permanent cure for the disease is not yet over. The impairment of axonal trafficking, mitochondrial dynamics, synaptic protein expression, neuronal excitability, Ca2+ homeostasis, synaptic integrity, and increased cytosolic dopamine level in the synaptic terminals, which have been reviewed here, point to the involvement of axon terminal loss before the degeneration of dopaminergic soma. However, the role of axon terminals and the initiation of the degeneration cascade at the cellular level of a dopaminergic neuron remain undeciphered. In this review, we have explored the cause of axonal degeneration and the role of impaired synaptic terminals in retrograde neurodegeneration that occurs in PD. Furthermore, we have suggested that future research should delve into the mechanism of preventing the degeneration of dopaminergic axons and their auxiliary terminals, which is likely to aid in restoring the dopamine level in the striatum and alleviate the motor complications in patients with PD.
Selective Vulnerability: Cellular Architecture and Neurotransmitter
The axon fiber of the SN dopaminergic neurons is thin, unmyelinated, and extensively ramified, with millions of synapses in the striatum (Figs. 2 and 3) [8]. The dense arborized axon terminals demand an excessive amount of energy for maintenance of their basal functions and survival. Furthermore, preservation of membrane potential, spreading of the action potential throughout the axolemma, release of dopamine from the synapses, and synaptic transmission of neural information create additional bioenergetic demands [11, 14]. The extreme demand for energy in the diffused neuronal extremities is met by densely packed mitochondria in the dopaminergic axon [12], and the regular supply of the mitochondria—as per the demand—in the neuronal extremities maintains their density therein. The increased density of the mitochondria in the neuron’s thin axon and the extremities helps cope with the tight energy budget [8]. However, because of either endogenous or exogenous insults, an imbalance in the demand and supply equilibrium of energy in the axons halts the energy-driven neuronal events and leads to dopaminergic neurodegeneration [21, 22]. Thus, the SN dopaminergic neuron's cellular morphology and mitochondrial homeostasis are peerless and contribute to its preferential vulnerability. One of the reasons for the sudden failure in the energy balance and the irreversible increase in anomalies in the SN neurons is their limited reserve capacity and the slow anterograde transportation of mitochondria to the site of need [13, 23, 24]. Therefore, in idiopathic PD and in several models of Parkinsonism, mitochondrial dysfunction is critical and is the reason for the selective degeneration [22, 25,26,27,28]. However, in addition to the SN axon terminals, mitochondrial dysfunction is also evident in the cholinergic neurons of the pedunculopontine nucleus, hippocampal nucleus, and the prefrontal cortex of the brain in patients with PD; furthermore, mitochondrial dysfunction has been reported in the unaffected regions of the brain, such as the cerebellar cortex and dentate nucleus [29,30,31].
Apart from the elevated mitochondrial density in the SN dopaminergic terminals, which engenders more risk, an important cause for the retrograde degeneration of the neurons is the presence of the neurotransmitter dopamine. The nascent neurotransmitter molecules are synthesized in the cytosol of the neuron. Dopamine synthesis, which occurs in two steps, is catalyzed by TH and aromatic amino acid decarboxylase (AADC) to generate L-dihydroxyphenylalanine (L-DOPA) and dopamine, respectively. L-DOPA, produced from the TH-catalyzed reaction in the presence of oxygen, serves as a substrate for AADC that forms dopamine upon decarboxylation in the cytosol [32,33,34]. Both enzymes (TH and AADC) bind to the synaptic vesicular membrane-localized vesicular monoaminergic transporter-2 (VMAT-2) protein and form a complex. Additionally, the dopamine molecules in the synaptic cleft are taken up into the cytosol through dopamine transporters (DATs) localized in the membranes of the axon terminals [35, 36]. Under normal circumstances, dopamine in the cytosol is recurrently pumped into the monoaminergic vesicles and stored therein. The translocation of dopamine into these acidic vesicles is VMAT-2-mediated and helps store dopamine in the axon terminals for future use and prevents the rapid conversion and depletion of the neurotransmitter in the cytosol [32, 37, 38]. If, somehow, dopamine fails to pass into the acidic lumen of the monoaminergic vesicles, it undergoes degradation in the cytosol and the levels of its metabolites increase.
In the axoplasm, monoamine oxidase (MAO) and catechol ortho-methyltransferase (COMT) catalyze the catabolism of dopamine. The MAO is a flavin adenine dinucleotide (FAD)-containing flavoenzyme present in the outer membrane of the mitochondria [39]. The enzyme converts the cytosolic dopamine into 3,4-dihydoxyphenylacetaldehyde and enhances oxidative stress because the oxidative deamination reaction generates hydrogen peroxide (H2O2). Furthermore, 3,4-dihydoxyphenylacetaldehyde is oxidized to form 3,4-dihydroxyphenylacetic acid (DOPAC) in the presence of aldehyde dehydrogenase. COMT methylates DOPAC and produces homovanillic acid (HVA). However, COMT can also directly methylate dopamine to produce 3-methoxytyramine (3-MT), which is also degraded to HVA in the presence of MAO and aldehyde dehydrogenase [32]. Also, the cytosolic dopamine is oxidized to dopamine o-quinone and further undergoes cyclization to form aminochrome and neuromelanin at physiological pH, which results in the production of reactive oxygen species (ROS). However, the end product of dopamine catabolism, neuromelanin, is neuroprotective [37, 40], and its presence is relatively higher in the SN neurons than in the VTA subtype. The augmented expression of neuromelanin in the neuron indicates increased dopamine oxidation in its cytoplasm. Thus, the resultant intermediate products and the ROS generated during the reaction cascade pose a significant risk to the neuron (Fig. 1). Reports have shown an increased level of oxidative stress and dopamine catabolites in the brain of patients with idiopathic PD and in animal models of PD [41, 42]. The dopamine catabolites enhance metabolic dysfunction as well as mitochondrial and lysosomal impairment [43].
Dopamine metabolism: In the presence of tyrosine hydroxylase (TH) and aromatic amino acid decarboxylase (AADC) enzymes, amino acid tyrosine is converted to dopamine, the neurotransmitter. An intermediate L-Dopa is also synthesized in the enzyme-catalyzed reactions in the axoplasm (cytoplasm of the axon). The degradation of dopamine in the cytosol is preserved by vesicular monoaminergic transporter-2 (VMAT-2) mediated transportation into the monoaminergic vesicles, the vesicle with low pH inside. The catabolism of dopamine in relatively alkaline pH of the cytosol is catalyzed by the mitochondrial monoamine oxidase (MAO), and cytosol localized catechol methyl-ortho-transferase (COMT) enzymes to form several intermediate metabolites and reactive oxygen species (ROS) molecules. Dopamine is also oxidized directly through different cascades to generate dopamine-O-quinone, aminochrome, neuromelanin, and ROS (All chemical structures were drawn using CambridgeSoft ChemDraw, RRID:SCR_016768) [32, 37, 39, 40, 42]
Impaired Axonal Transport in PD
Axonal transport is a process in the axoplasm that is responsible for the movement and distribution of essential biomolecules and organelles to and from its nerve endings. This transport maintains the equilibrium in the supply and demand of vital organelles, such as mitochondria, and several proteins and vesicles, including synaptic vesicles, in the neuron's cell body and axon terminals. Thus, the event is crucial for the proper functioning of the neuron and is equally essential for its growth and survival. The cytoskeletal and motor proteins facilitate the continuous anterograde and retrograde trafficking of cargos in the functional neuron to accomplish efficient axonal transport. In dopaminergic neurons, morphology-regulating actin and tubulin are the major cytoskeletal proteins that form “tracks” for cargo transportation [44,45,46] and kinesin and dynein are the motor proteins that assist in the anterograde and retrograde trafficking, respectively, of several proteins, vesicular structures, mitochondria, and other organelles (Fig. 2) [47, 48]. Studies have established that altered levels of these proteins in the dopaminergic neurons cause the dysregulation of axonal transport. This dysregulation leads to neuronal dystrophy, which is characterized by bulging neurites, loss of presynaptic terminals, deficit in synaptic function, abnormal protein accumulation in the neurites, defective mitochondrial dynamics, and dysregulated homeostasis long before the dopaminergic neurodegeneration [10, 44].
Axonal trafficking in the functional dopaminergic neuron [A] and in degenerating neuron in PD [B]. The cytoskeleton proteins (actin and tubulin) form “tracks” to transport proteins and organelles to and from the neuron's cell body. The kinesin and the dynein are two motor proteins for anterograde and retrograde trafficking, respectively. Impaired axonal transport in PD is marked by a higher ratio of obstructed protein inclusion and dysfunctional mitochondria in the deteriorating dopaminergic neurons. Failure in the trafficking of essential proteins, mitochondria, lysosomes and vesicular structures at the distal ends causes retrograde axonal loss (All structures are made with Inkscape Software, RRID:SCR_014479) [10, 45,46,47,48,49, 53]
Several reports have shown that axonal transport is significantly impaired in sporadic PD and that it precedes the early decline in dopaminergic neurons [49, 50]. A similar finding has also suggested impaired axonal transport, which leads to early degeneration in a retrograde manner in familial PD [10] and toxin-based PD models [51, 52]. Alterations in the expressions of motor proteins (kinesin and dynein) and cytoskeletal protein (tubulin) impair the axonal transport [46, 49, 53]. Disruption of the anterograde trafficking of the mitochondria into the axonal projections as per their energy demand results in energy deficit and the loss of synapses [10]. The exact reason for the onset of impairment in axonal trafficking is yet unknown; however, a few PD-related proteins (DJ-1, leucine-rich repeat kinase-2 (LRRK-2), and α-synuclein) have been linked to the process of axonal transport, and mutations in the corresponding genes cause axonal transport abruption [10, 46]. Moreover, hyperserotonergic neurotransmission, a state of neuropathology in the brain of patients with PD, also disrupts the regular axonal transportation in the dopaminergic neuron because serotonin plays an inhibitory role in axonal growth and regeneration [54].
Defective Mitochondrial Dynamics in the Axon
The SN dopaminergic neurons are top-to-toe energy-demanding cells. The neurons require energy for axonal transport and synaptic release and for maintaining basal cell functions, growth, and survival. The unique morphology of the SN neurons—dense axon terminal arborization with millions of synaptic contacts—requires additional energy when compared with the less vulnerable VTA dopaminergic neurons to maintain their synaptic events and adequate axonal transport as per the demand. The elevated bioenergetic demand is fulfilled by transporting more mitochondria to the axon terminals. In the dopaminergic neuron, the mitochondria perform many intraneuronal functions such as Ca2+ buffering, dopamine synthesis and degradation, neurotransmitter translocation, synaptic vesicle mobilization, and bidirectional axonal transport [48, 55, 56]. However, the narrow axonal width of the SN neurons imposes cytoplasmic space restrictions and controls the motility of the trafficking mitochondria [12]. Therefore, in the SN neurons, mitochondrial homeostasis is at the edge. However, the dynamic properties of the mitochondria, such as fission, fusion, trafficking, biogenesis, and degradation, are significantly higher in the SN neurons than in the VTA counterpart for maintaining their health [12, 57]. A disruption in any of these dynamic mitochondrial events disturbs the others and is associated with mitochondrial dysfunction, a critical pathology reported in PD [27, 48, 58].
Experimental studies have suggested that several endogenous and exogenous insults influence the defective mitochondrial dynamic processes in the axon terminals during early-stage PD [59,60,61]. For being functional, neurons depend on the regular supply and distribution of functional mitochondria in their axon and terminals. Simultaneously, the dysfunctional mitochondria need to be eliminated from the synaptic terminals for their ultimate degradation via mitophagy [62, 63]. The equilibrium between the supply of healthy mitochondria and the clearance of aberrant mitochondria is crucial for maintaining the morphology, plasticity, and functionality of the synapses. Several experimental and idiopathic PD studies have stated that defects in the mitochondrial dynamics appear early, well before neurodegeneration [27, 28, 64]. In familial PD cases, mutations in a few genes associated with disease onset have been linked to the mitochondria and have been shown to play a crucial role in regulating the mitochondrial dynamics in the neurons [61, 65]. Defects in the dynamics distort the synapse morphology and reduce the postsynaptic dendritic spines, which lead to a loss of plasticity [55, 66]. Moreover, abnormal mitochondrial dynamics cause cyclic oxidative stress, increased energy demand at the synaptic contact, and dysregulated Ca2+ buffering at the synaptic site. These events culminate in the untimely degeneration of the dopaminergic neurons originating from their synaptic sites [24, 61].
Early Impairment of Synaptic Homeostasis
The synapses are often distantly located from the cell body of the neurons owing to axonal extension. Synapse is the functional junction and comprises the presynaptic bouton, which contains neurotransmitters packaged in vesicles, and the postsynaptic neuronal membrane, which consists of target receptors that bind the released neurotransmitters to exchange the presynaptic neural information. Between them, there is a synaptic cleft that isolates and holds the presynaptic and postsynaptic components. The homeostasis and sustained functionality of the neuronal synapses, including the SN dopaminergic neurons, depend on several synaptic proteins residing in the presynaptic boutons, mitochondrial influx and elevated bioenergetics in the presynaptic boutons that fuel effective and sustained neurotransmission, and the postsynaptic membrane-receptor proteins that bind the neurotransmitter and transmit the neural information to the postsynaptic neurons.
A study has established the loss of synaptic sites and its association with the onset of motor symptoms in PD [67]. A similar study has suggested that synaptic decay and loss of auxiliary axonal fibers in the striatum occur earlier than the degeneration of the cell bodies in the nigral compartment. Thus, the demise of the synaptic terminals occurs before that of the cell bodies in the SN dopaminergic neurons [68, 69]. However, the reason behind the early loss of synaptic terminals in PD is largely obscure.
The presynaptic boutons contain several proteins called synaptic proteins, which are involved in maintaining the survivability, plasticity, and functionality of the synapse. Members of these proteins also regulate vesicular packaging and exocytosis of the neurotransmitters. In the SN dopaminergic neurons, members of the synaptic protein family belong to both types, i.e., membrane-bound and soluble cytosolic proteins (Table 1) [70,71,72]. These proteins regulate the Ca2+ level, dopamine release, growth and alignment of the dendrites, synaptic density, and the plasticity of the synapses [70]. Impairment in the genes encoding the synaptic proteins and their abnormal expression cause synaptic dysfunction in PD-linked dopaminergic neurons. The abnormal expression of the synaptic proteins alters neurotransmission and results in synaptic dysfunction but does not necessarily lead to synaptic degeneration (Fig. 3). However, abnormalities in a few synaptic proteins and/or genes encoding them, including α-synuclein, LRRK-2, auxilin, synaptojanin-1 (Synj-1), and endophilin A1, have been linked to Parkinsonism [70, 73, 74]. Moreover, elevated levels of the synaptic proteins neurogranin and the 25-kDa synaptosomal-associated protein (SNAP25) have been observed in the cerebrospinal fluid of patients with PD [75].
Presynaptic homeostasis in the functional dopaminergic neuron [A] and presynaptic impairment in PD [B]. The presynaptic bouton of an operational dopaminergic neuron shows a proper morphology and consists of abundant mitochondria, functional lysosomes and synaptic vesicles packed with neurotransmitters [A]. Early synaptic alteration in PD is marked with a change in the morphology of the bouton, increased cytosolic dopamine, protein inclusion/aggregates, dysfunctional mitochondria and lysosomes and reduction in the synaptic structures in the presynaptic bouton [B] (All structures are made with Inkscape Software, RRID:SCR_014479) [10, 53, 78,79,80,81, 128]
The exact mechanism of synaptic dysfunction, which is caused by abnormalities in the proteins and leads to synaptic loss, is an enigmatic question. The autopsy of PD-affected brains has revealed aggregates of α-synuclein, a protein involved in regulating the synaptic functions [71], in the presynaptic terminals [76]. Such reports are also standard in experimental studies [77]. The aberrant α-synuclein is propagated intercellularly to neighboring neurons, which results in the transfection of the deleterious cascade in a prion-like manner. The presence of the pathological α-synuclein in deteriorating neurons and ingrafted tissues received by patients with PD supports the prion hypothesis of disease spread [78,79,80]. The aberrant α-synuclein impairs the dopamine release [79], abruptly snares the essential cellular components at an inappropriate location, including the mitochondria and lysosomes, and obstructs the normal axonal trafficking [10, 53]. Furthermore, the protein binds to other presynaptic proteins such as cysteine-string protein α (CSP α)—a protein involved in maintaining synaptic integrity—and heat shock protein cognate 70 (Hsc 70)—a chaperone protein for α-synuclein turnover—thereby hindering their functions [81].
Breakdown of Ca2+ Homeostasis in the Axon Terminals
The abundance and homeostasis of Ca2+ in the cytoplasm of dopaminergic neurons are vital for the function and survival of these neurons. Ca2+ regulates many physiological processes, including membrane excitability, dopamine release, and synaptic plasticity [82]. The divalent cation is pumped into the cytosol from intracellular and extracellular sources in a nigrostriatal dopaminergic neuron. The central intracellular Ca2+ reserve is the endoplasmic reticulum (ER), and the opening of voltage-gated Ca2+-channel (Cav) proteins, which are located on the ER membrane, releases these cations into the cytoplasm. Simultaneously, Ca2+ from the extracellular source enters through the Cav proteins situated on the axonal membrane [83, 84]. However, the dopaminergic neuron's action potential modulates the Ca2+ influx into the cytosol from its reservoirs, i.e., the intracellular and the extracellular sources. The Ca2+ entry, its cytosolic oscillation, and the electric activity of the neuron play a decisive role in dopamine release within the dorsal striatum. Additionally, the secondary messenger molecule maintains the basal dopamine levels for the next neurotransmission cycle [85].
The SN neuron has a unique slow and broad action potential that maximizes the Ca2+ entry into the cytoplasm from its reserves [8]. The additional feature of the SN dopaminergic neuron that distinguishes it from the other neuronal types is its low intrinsic calcium buffering ability. The inflow of Ca2+, when released from the reserves, floods the nearby cytosol. Therefore, calcium-binding proteins in the neuron, such as calbindin, interact with the available free cytosolic Ca2+ and rapidly buffer the situation until the surplus Ca2+ is instead pumped back into the reservoirs [86]. In the SN neurons, the presence of the calcium buffering protein is low. Thus, the surplus free Ca2+ interacts with other proteins, alters the cytosolic pH, and inhibits the cellular functions. Furthermore, the Cav aligned to the plasma membrane of the SN neurons allows more Ca2+ to enter the cytosol than the Cav of the VTA neurons [87, 88]. Ca2+ long-lasting presence in the cytosol synergizes with the PD-linked risk factors including ageing, environmental agents, and genetics, and induces mitochondrial dysfunction, which leads to oxidative stress [89]. A report has suggested imbalance in Cav activity in the dopaminergic terminals of PD models [90] and altered expression of Cav and calcium-binding proteins in early- and late-stage PD, which establishes the key role of calcium ions in the disease [91, 92]. The aberrant α-synuclein in the presynaptic terminals of the degenerating neurons causes dysregulation of Ca2+ and also induces Ca2+-mediated neuronal death [93]. Gene mutations and abnormal expressions of PD-associated proteins also dysregulate the homeostasis of Ca2+, the secondary signaling molecule [94, 95].
Relevance of Axonal Degeneration in PD
The dopaminergic neurons of the nigrostriatal pathway connect the SN nucleus to the striatum compartment, the pathway which is defective in PD. Of course, both SN and striatal tissue deteriorate as the disease progresses, but from where does the degeneration initiate? Does the neuronal soma of the SN neuron degenerate before losing its extended axon and arborized terminals, or does the dysfunction begin in the axon terminals/axon and propagate in a retrograde manner? Many believe that the degeneration co-occurs in the SN dopaminergic soma and axon terminals, whereas others are unclear of the degeneration pattern. Thus, the underlying facts are yet to be established.
Studies have indicated that the motor deficits are visible in PD only after approximately 70% of the striatal dopamine has been depleted [25, 41]; hence, the demise of the presynaptic terminals governing the neurotransmitter release must begin much earlier than the appearance of the disease symptoms. Therefore, the loss of striatal axon terminals outweighs the loss of cell bodies of the SN dopaminergic neurons during the disease progression because the axon terminals participate earlier in the degenerative cascade [68]. Furthermore, the flaws in the presynaptic terminals of the degenerating neurons confirm the prior involvement of the axon terminals during progressive degeneration. The presynaptic terminals become a damping corner of aberrant proteins, damaged mitochondria, and dysregulated Ca2+ [24]. The accumulation of aberrant proteins and the breakdown of the synaptic bioenergetics—due to defective mitochondria—hinder the transmission of impulses from the neuron's functional junction. These aberrations need to be urgently cleared form the deteriorating neuron to be revived and regain its functionality. However, the central clearance machinery for defective proteins and organelles exists in the neuron's cell body, and the defective axon trafficking of the deteriorating neurons obstructs the retrograde cargo transportation. In addition, dopaminergic neurons are post-mitotic cells that forever remain in their resting phase (G0 phase) and never redistribute their damaged proteins and organelles to the daughter cells [96]. Thus, in the absence of redispersal and proper trafficking, these abnormalities remain intracellularly in millions of tiny presynaptic axon terminals and cell bodies and are disproportionately overshared in the axon terminals when compared with the cell body of the neurons. Moreover, the terminals exhibit synaptic density and structural alterations, which is yet another link to disease progression [69]. Apart from PD, chronic exposure to various psychostimulant addictions also impairs the dopaminergic terminals. These addictive drugs increase cytosolic dopamine levels, block DAT reuptake, modulate neuronal firing, alter neurotransmission, and induce changes in synaptic morphology [97,98,99].
Thus, the axonal projections, not the cell bodies, are the initial players in the SN dopaminergic neurodegeneration; subsequently, their loss, which propagates toward the cell body, leads to the appearance and progression of clinical manifestations. Unfortunately, very few studies have reported the axonal origin of the dopaminergic neurons' disintegration in PD [3, 62, 100, 101]. If loss of axon terminals occurs early in PD and is responsible for the progression of the motor symptoms, targeting the cell bodies for a neuroprotective approach is non-directional. However, despite the mounting evidence for the predominant role of the axon terminals in PD, to date, researchers have rarely studied the axons and the cell body of a neuron separately and have continued to focus on the death of the entire neuron structure. The strategy to cure the disease has been to either target the neuronal soma or replace the defective ones with exogenous healthy neurons. Similarly, experimental strategies for neuroprotection have focused on preventing the demise of the cell bodies and not axonal loss. Until now, the protective strategies have revolved around targeting different pathways of programmed cell death, but the apoptotic mechanism of cell death is applied only in the neuronal soma. The mechanism of axonal degeneration is utterly different from programmed cell death, and much of the degenerative cascade is indescribable [3]. Investigating the pathological changes only in neuronal soma could well be the reason for our failure in developing clinical neuroprotective and restorative therapeutics despite experimental successes.
The Future Perspective of Axon Neurobiology
The proper functioning of the nigrostriatal system depends on the structurally polarized SN dopaminergic neuron. In the polarized architecture, the soma overshares the cellular machinery for its maintenance. Simultaneously, the axon projections rely on bidirectional axonal transport for their survival and for maintaining their functionality. Unfortunately, in PD, the axonal trafficking in the related neurons deteriorates with the progression of the disease. The progressive deterioration in bidirectional trafficking is due to the gradual accumulation of redundant proteins and damaged organelles. At the initial stage of the disease, neuronal debris is formed at the synaptic site but is successively accumulated in the axon and cell body because of the obstruction of axonal trafficking, retardation in the clearance machinery, and advancement of the disease. Thus, unlike other cell types, the neuron's architectural components—neuronal soma and axon projections—should be studied separately and the neuropathological changes should be classified discretely in the ramified terminals and soma of the degenerating PD-related neurons. The neurobiological alterations should be separately measured per unit area/volume in both the neuronal compartments. Designing such studies could help investigate the comparative alterations in the soma and terminals and identify early-stage PD biomarkers residing at or near the synaptic sites and causing synaptic dysfunction. Furthermore, spatial autophagy in the terminals and synaptic sites, which involve synaptic proteins, could be induced to digest the synaptic junks locally before they exponentially multiply in the axon and hinder the axonal transport [102,103,104]. Since dopaminergic neurons are non-dividing cells, correcting the neuronal aberrations and digesting the cellular debris through site-specific autophagy, particularly at an early stage, are the sole strategies available.
Although neuronal soma restoration is crucial for axonal growth, maintenance, and survival, it is not sufficient to prevent the clinical progression of PD. Ignoring the axons' decisive relevance in formulating neuroprotective strategies could be due to the obstacles in the experimental demonstration of axons and their auxiliary fibers in the brain tissue. Studying axons requires high-quality tissue preservation and special techniques. However, if studying axonal destruction, regrowth, and anatomical organization becomes feasible in the future with advanced techniques, attempts to develop therapeutic strategies by correcting the synaptic autophagy at the pre-symptomatic stage may be more effective. Moreover, while the lost neuronal tissues are replaced by the exogenous implant in the grafting technique, in the new approach, the surviving neurons can be stimulated to regrow their axons and the associated auxiliary fibers for proper anatomical arrangement and reintegration into the surviving circuitry. Thus, if the approach for correcting the spatial clearance machinery of the axon terminals to design neuroprotective and restorative drugs could be made feasible in the future, it could offer a better direction in devising novel therapeutic strategies for PD.
References
Tritsch NX, Sabatini BL (2012) Dopaminergic modulation of synaptic transmission in cortex and striatum. Neuron 76(1):33–50. https://doi.org/10.1016/j.neuron.2012.09.023
Ayano G (2016) Dopamine: receptors, functions, synthesis, pathways, locations and mental disorders: review of literatures. J Ment Disord Treat 2(2):120. https://doi.org/10.4172/2471-271x.1000120
Tagliaferro P, Burke RE (2016) Retrograde axonal degeneration in Parkinson disease. J Parkinsons Dis 6(1):1–15. https://doi.org/10.3233/jpd-150769
Zhang J, Culp ML, Craver JG, Darley-Usmar V (2018) Mitochondrial function and autophagy: integrating proteotoxic, redox, and metabolic stress in Parkinson’s disease. J Neurochem 144:691–709. https://doi.org/10.1111/jnc.14308
McCormack A, Keating DJ, Chegeni N, Colella A, Wang JJ, Chataway T (2019) Abundance of synaptic vesicle-related proteins in alpha-synuclein-containing protein inclusions suggests a targeted formation mechanism. Neurotox Res 35(4):883–897. https://doi.org/10.1007/s12640-019-00014-0
Ghavami S, Shojaei S, Yeganeh B, Ande SR, Jangamreddy JR, Mehrpour M, Christoffersson J, Chaabane W, Moghadam AR, Kashani HH, Hashemi M, Owji AA, Łos MJ (2014) Autophagy and apoptosis dysfunction in neurodegenerative disorders. Prog Neurobiol 112:24–49. https://doi.org/10.1016/j.pneurobio.2013.10.004
Malik BR, Maddison DC, Smith GA, Peters OM (2019) Autophagic and endo-lysosomal dysfunction in neurodegenerative disease. Mol Brain 12(1):100. https://doi.org/10.1186/s13041-019-0504-x
Surmeier DJ (2018) Determinants of dopaminergic neuron loss in Parkinson’s disease. FEBS J 285(19):3657–3668. https://doi.org/10.1111/febs.14607
Voronkov DN, Salkov VN, Anufriev PL, Khudoerkov RM (2018) Lewy bodies in Parkinson’s disease: histological, immunohistochemical and interferometric examinations. Arkh Patol 80(4):9–13. https://doi.org/10.17116/patol20188049
Prots I, Grosch J, Brazdis RM, Simmnacher K, Veber V, Havlicek S, Hannappel C, Krach F, Krumbiegel M, Schütz O, Reis A, Wrasidlo W, Galasko DR, Groemer TW, Masliah E, Schlötzer-Schrehardt U, Xiang W, Winkler J, Winner B (2018) α-Synuclein oligomers induce early axonal dysfunction in human iPSC-based models of synucleinopathies. Proc Natl Acad Sci U S A 115(30):7813–7818. https://doi.org/10.1073/pnas.1713129115
Bolam JP, Pissadaki EK (2012) Living on the edge with too many mouths to feed: why dopamine neurons die. Mov Disord 27(12):1478–1483. https://doi.org/10.1002/mds.25135
Pacelli C, Giguère N, Bourque MJ, Lévesque M, Slack RS, Trudeau LÉ (2015) Elevated mitochondrial bioenergetics and axonal arborization size are key contributors to the vulnerability of dopamine neurons. Curr Biol 25(18):2349–2360. https://doi.org/10.1016/j.cub.2015.07.050
Franco-Iborra S, Perier C (2015) Neurodegeneration: the size takes it all. Curr Biol 25(18):R797–R800. https://doi.org/10.1016/j.cub.2015.07.062
Mamelak M (2018) Parkinson’s disease, the dopaminergic neuron and gammahydroxybutyrate. Neurol Ther 7(1):5–11. https://doi.org/10.1007/s40120-018-0091-2
Valdinocci D, Simões RF, Kovarova J, Cunha-Oliveira T, Neuzil J, Pountney DL (2019) Intracellular and intercellular mitochondrial dynamics in Parkinson’s disease. Front Neurosci 13:930. https://doi.org/10.3389/fnins.2019.00930
Guo W, Stoklund Dittlau K, Van Den Bosch L (2020) Axonal transport defects and neurodegeneration: molecular mechanisms and therapeutic implications. Semin Cell Dev Biol 99:133–150. https://doi.org/10.1016/j.semcdb.2019.07.010
Scorziello A, Borzacchiello D, Sisalli MJ, Di Martino R, Morelli M, Feliciello A (2020) Mitochondrial homeostasis and signaling in Parkinson’s disease. Front Aging Neurosci 12:100. https://doi.org/10.3389/fnagi.2020.00100
Vos M, Lauwers E, Verstreken P (2010) Synaptic mitochondria in synaptic transmission and organization of vesicle pools in health and disease. Front Synaptic Neurosci 2:139. https://doi.org/10.3389/fnsyn.2010.00139
Ludtmann MHR, Abramov AY (2018) Mitochondrial calcium imbalance in Parkinson’s disease. Neurosci Lett 663:86–90. https://doi.org/10.1016/j.neulet.2017.08.044
Reeve AK, Grady JP, Cosgrave EM, Bennison E, Chen C, Hepplewhite PD, Morris CM (2018) Mitochondrial dysfunction within the synapses of substantia nigra neurons in Parkinson’s disease. NPJ Parkinsons Dis 4(1):1–10. https://doi.org/10.1038/s41531-018-0044-6
Morais VA, Verstreken P, Roethig A, Smet J, Snellinx A, Vanbrabant M, Haddad D, Frezza C, Mandemakers W, Vogt-Weisenhorn D, Van Coster R, Wurst W, Scorrano L, De Strooper B (2009) Parkinson’s disease mutations in PINK1 result in decreased Complex I activity and deficient synaptic function. EMBO Mol Med 1(2):99–111. https://doi.org/10.1002/emmm.200900006
Dixit A, Srivastava G, Verma D, Mishra M, Singh PK, Prakash O (1832) Singh MP (2013) Minocycline, levodopa and MnTMPyP induced changes in the mitochondrial proteome profile of MPTP and Maneb and Paraquat mice models of Parkinson’s disease. Biochim Biophys Acta 8:1227–1240. https://doi.org/10.1016/j.bbadis.2013.03.019
Chen Y, Sheng ZH (2013) Kinesin-1-syntaphilin coupling mediates activity-dependent regulation of axonal mitochondrial transport. J Cell Biol 202(2):351–364. https://doi.org/10.1083/jcb.201302040
Chen C, Turnbull DM, Reeve AK (2019) Mitochondrial dysfunction in Parkinson’s disease—cause or consequence? Biology (Basel) 8(2):38. https://doi.org/10.3390/biology8020038
Agrawal S, Dixit A, Singh A, Tripathi P, Singh D, Patel DK, Singh MP (2015) Cyclosporine A and MnTMPyP alleviate α-synuclein expression and aggregation in cypermethrin-induced Parkinsonism. Mol Neurobiol 52(3):1619–1628. https://doi.org/10.1007/s12035-014-8954-8
ur Rasheed MS, Tripathi MK, Mishra AK, Shukla S, Singh MP, (2016) Resveratrol protects from toxin-induced parkinsonism: plethora of proofs hitherto petty translational value. Mol Neurobiol 53(5):2751–2760. https://doi.org/10.1007/s12035-015-9124-3
Podlesniy P, Puigròs M, Serra N, Fernández-Santiago R, Ezquerra M, Tolosa E, Trullas R (2019) Accumulation of mitochondrial 7S DNA in idiopathic and LRRK2 associated Parkinson’s disease. EBioMedicine 48:554–567. https://doi.org/10.1016/j.ebiom.2019.09.015
Dossi G, Squarcina L, Rango M (2019) In vivo mitochondrial function in idiopathic and genetic Parkinson’s disease. Metabolites 10(1):19. https://doi.org/10.3390/metabo10010019
Bury AG, Pyle A, Elson JL, Greaves L, Morris CM, Hudson G, Pienaar IS (2017) Mitochondrial DNA changes in pedunculopontine cholinergic neurons in Parkinson disease. Ann Neurol 82(6):1016–1021. https://doi.org/10.1002/ana.25099
Flønes IH, Fernandez-Vizarra E, Lykouri M, Brakedal B, Skeie GO, Miletic H, Lilleng PK, Alves G, Tysnes OB, Haugarvoll K, Dölle C, Zeviani M, Tzoulis C (2018) Neuronal complex I deficiency occurs throughout the Parkinson’s disease brain, but is not associated with neurodegeneration or mitochondrial DNA damage. Acta Neuropathol (Berl) 135(3):409–425. https://doi.org/10.1007/s00401-017-1794-7
Dixit A, Mehta R, Singh AK (2019) Proteomics in human Parkinson’s disease: present scenario and future directions. Cell Mol Neurobiol 39(7):901–915. https://doi.org/10.1007/s10571-019-00700-9
Segura-Aguilar J, Paris I, Muñoz P, Ferrari E, Zecca L, Zucca FA (2014) Protective and toxic roles of dopamine in Parkinson’s disease. J Neurochem 129(6):898–915. https://doi.org/10.1111/jnc.12686
Plotegher N, Berti G, Ferrari E, Tessari I, Zanetti M, Lunelli L, Greggio E, Bisaglia M, Veronesi M, Girotto S, Dalla Serra M, Perego C, Casella L, Bubacco L (2017) DOPAL derived alpha-synuclein oligomers impair synaptic vesicles physiological function. Sci Rep 7:40699. https://doi.org/10.1038/srep40699
Klein MO, Battagello DS, Cardoso AR, Hauser DN, Bittencourt JC, Correa RG (2019) Dopamine: functions, signaling, and association with neurological diseases. Cell Mol Neurobiol 39(1):31–59. https://doi.org/10.1007/s10571-018-0632-3
Nirenberg MJ, Vaughan RA, Uhl GR, Kuhar MJ, Pickel VM (1996) The dopamine transporter is localized to dendritic and axonal plasma membranes of nigrostriatal dopaminergic neurons. J Neurosci 16(2):436–447. https://doi.org/10.1523/jneurosci.16-02-00436.1996
Hersch SM, Yi H, Heilman CJ, Edwards RH, Levey AI (1997) Subcellular localization and molecular topology of the dopamine transporter in the striatum and substantia nigra. J Comp Neurol 388(2):211–227. https://doi.org/10.1002/(sici)1096-9861(19971117)388:2%3c211::aid-cne3%3e3.0.co;2-4
Segura-Aguilar J, Paris I (2014) Mechanisms of dopamine oxidation and parkinson's disease. In: Handbook of neurotoxicity, vol 2, pp 865–883. Springer, New York. https://doi.org/10.1007/978-1-4614-5836-4_16
German CL, Baladi MG, McFadden LM, Hanson GR, Fleckenstein AE (2015) Regulation of the dopamine and vesicular monoamine transporters: pharmacological targets and implications for disease. Pharmacol Rev 67(4):1005–1024. https://doi.org/10.1124/pr.114.010397
Castagnoli N, Petzer JP, Steyn S, Castagnoli K, Chen JF, Schwarzschild MA, Van Der Schyf CJ (2003) Monoamine oxidase B inhibition and neuroprotection: studies on selective adenosine A2A receptor antagonists. Neurology 61(11 SUPPL. 6):S62-68. https://doi.org/10.1212/01.wnl.0000095215.97585.59
Segura-Aguilar J (2017) On the role of endogenous neurotoxins and neuroprotection in Parkinson’s disease. Neural Regen Res 12(6):897–901. https://doi.org/10.4103/1673-5374.208560
Singh AK, Tiwari MN, Upadhyay G, Patel DK, Singh D, Prakash O, Singh MP (2012) Long term exposure to cypermethrin induces nigrostriatal dopaminergic neurodegeneration in adult rats: postnatal exposure enhances the susceptibility during adulthood. Neurobiol Aging 33(2):404–415. https://doi.org/10.1016/j.neurobiolaging.2010.02.018
Toulorge D, Schapira AHV, Hajj R (2016) Molecular changes in the postmortem parkinsonian brain. J Neurochem 139:27–58. https://doi.org/10.1111/jnc.13696
Burbulla LF, Song P, Mazzulli JR, Zampese E, Wong YC, Jeon S, Santos DP, Blanz J, Obermaier CD, Strojny C, Savas JN, Kiskinis E, Zhuang X, Krüger R, Surmeier DJ, Krainc D (2017) Dopamine oxidation mediates mitochondrial and lysosomal dysfunction in Parkinson’s disease. Science 357(6357):1255–1261. https://doi.org/10.1126/science.aam9080
Chung CY, Koprich JB, Siddiqi H, Isacson O (2009) Dynamic changes in presynaptic and axonal transport proteins combined with striatal neuroinflammation precede dopaminergic neuronal loss in a rat model of AAV α-synucleinopathy. J Neurosci 29(11):3365–3373. https://doi.org/10.1523/jneurosci.5427-08.2009
Pellegrini L, Wetzel A, Grannó S, Heaton G, Harvey K (2017) Back to the tubule: microtubule dynamics in Parkinson’s disease. Cell Mol Life Sci 74(3):409–434. https://doi.org/10.1007/s00018-016-2351-6
Cartelli D, Cappelletti G (2017) Microtubule destabilization paves the way to Parkinson’s disease. Mol Neurobiol 54:6762–6774. https://doi.org/10.1007/s12035-016-0188-5
Brady ST, Morfini GA (2017) Regulation of motor proteins, axonal transport deficits and adult-onset neurodegenerative diseases. Neurobiol Dis 105:273–282. https://doi.org/10.1016/j.nbd.2017.04.010
Panchal K, Tiwari AK (2021) Miro (Mitochondrial Rho GTPase), a key player of mitochondrial axonal transport and mitochondrial dynamics in neurodegenerative diseases. Mitochondrion 56:118–135. https://doi.org/10.1016/j.mito.2020.10.005
Chu Y, Morfini GA, Langhamer LB, He Y, Brady ST, Kordower JH (2012) Alterations in axonal transport motor proteins in sporadic and experimental Parkinson’s disease. Brain 135(7):2058–2073. https://doi.org/10.1093/brain/aws133
Kordower JH, Olanow CW, Dodiya HB, Chu Y, Beach TG, Adler CH, Halliday GM, Bartus RT (2013) Disease duration and the integrity of the nigrostriatal system in Parkinson’s disease. Brain 136(8):2419–2431. https://doi.org/10.1093/brain/awt192
Morfini GA, Burns M, Binder LI, Kanaan NM, Lapointe N, Bosco DA, Brown RH, Brown H, Tiwari A, Hayward L, Edgar J, Nave KA, Garberrn J, Atagi Y, Song Y, Pigino G, Brady ST (2009) Axonal transport defects in neurodegenerative diseases. J Neurosci 29(41):12776–12786. https://doi.org/10.1523/jneurosci.3463-09.2009
Morfini G, Pigino G, Opalach K, Serulle Y, Moreira JE, Sugimori M, Llinás RR, Brady ST (2007) 1-Methyl-4-phenylpyridinium affects fast axonal transport by activation of caspase and protein kinase C. Proc Natl Acad Sci U S A 104(7):2442–2447. https://doi.org/10.1073/pnas.0611231104
Prots I, Veber V, Brey S, Campioni S, Buder K, Riek R, Böhm KJ, Winner B (2013) α-Synuclein oligomers impair neuronal microtubule-kinesin interplay. J Biol Chem 288(30):21742–21754. https://doi.org/10.1074/jbc.M113.451815
da Cruz M-J (2019) Hyper-serotonergic state determines onset and progression of idiopathic Parkinson’s disease. Med Hypotheses 133:109399. https://doi.org/10.1016/j.mehy.2019.109399
Flippo KH, Strack S (2017) Mitochondrial dynamics in neuronal injury, development and plasticity. J Cell Sci 130(4):671–681. https://doi.org/10.1242/jcs.171017
Whitworth AJ, Pallanck LJ (2017) PINK1/Parkin mitophagy and neurodegeneration—what do we really know in vivo? Curr Opin Genet Dev 44:47–53. https://doi.org/10.1016/j.gde.2017.01.016
Haddad D, Nakamura K (2015) Understanding the susceptibility of dopamine neurons to mitochondrial stressors in Parkinson’s disease. FEBS Lett 589:3702–3713. https://doi.org/10.1016/j.febslet.2015.10.021
Podlesniy P, Vilas D, Taylor P, Shaw LM, Tolosa E, Trullas R (2016) Mitochondrial DNA in CSF distinguishes LRRK2 from idiopathic Parkinson’s disease. Neurobiol Dis 94:10–17. https://doi.org/10.1016/j.nbd.2016.05.019
Winklhofer KF (1802) Haass C (2010) Mitochondrial dysfunction in Parkinson’s disease. Biochim Biophys Acta 1:29–44. https://doi.org/10.1016/j.bbadis.2009.08.013
Lu X, Kim-Han JS, Harmon S, Sakiyama-Elbert SE, O’Malley KL (2014) The Parkinsonian mimetic, 6-OHDA, impairs axonal transport in dopaminergic axons. Mol Neurodegener 9(1):17. https://doi.org/10.1186/1750-1326-9-17
Pozo Devoto VM, Falzone TL (2017) Mitochondrial dynamics in Parkinson’s disease: a role for α-synuclein? Dis Model Mech 10(9):1075–1087. https://doi.org/10.1242/dmm.026294
Burke RE, O’Malley K (2013) Axon degeneration in Parkinson’s disease. Exp Neurol 246:72–83. https://doi.org/10.1016/j.expneurol.2012.01.011
Ashrafi G, Schlehe JS, LaVoie MJ, Schwarz TL (2014) Mitophagy of damaged mitochondria occurs locally in distal neuronal axons and requires PINK1 and Parkin. J Cell Biol 206(5):655–670. https://doi.org/10.1083/jcb.201401070
Trancikova A, Tsika E, Moore DJ (2012) Mitochondrial dysfunction in genetic animal models of Parkinson’s disease. Antioxid Redox Signal 16(9):896–919. https://doi.org/10.1089/ars.2011.4200
Park JS, Davis RL, Sue CM (2018) Mitochondrial dysfunction in Parkinson’s disease: new mechanistic insights and therapeutic perspectives. Curr Neurol Neurosci Rep 18(5):21. https://doi.org/10.1007/s11910-018-0829-3
Amorim IS, Graham LC, Carter RN, Morton NM, Hammachi F, Kunath T, Pennetta G, Carpanini SM, Manson JC, Lamont DJ, Wishart TM, Gillingwater TH (2017) Sideroflexin 3 is an α-synuclein-dependent mitochondrial protein that regulates synaptic morphology. J Cell Sci 130(2):325–331. https://doi.org/10.1242/jcs.194241
Mallet N, Delgado L, Chazalon M, Miguelez C, Baufreton J (2019) Cellular and synaptic dysfunctions in Parkinson’s disease: stepping out of the striatum. Cells 8(9):1005. https://doi.org/10.3390/cells8091005
Fazio P, Svenningsson P, Cselényi Z, Halldin C, Farde L, Varrone A (2018) Nigrostriatal dopamine transporter availability in early Parkinson’s disease. Mov Disord 33(4):592–599. https://doi.org/10.1002/mds.27316
Matuskey D, Tinaz S, Wilcox KC, Naganawa M, Toyonaga T, Dias M, Henry S, Pittman B, Ropchan J, Nabulsi N, Suridjan I, Comley RA, Huang Y, Finnema SJ, Carson RE (2020) Synaptic changes in Parkinson disease assessed with in vivo imaging. Ann Neurol 87(3):329–338. https://doi.org/10.1002/ana.25682
Pienaar IS, Burn D, Morris C, Dexter D (2012) Synaptic protein alterations in Parkinson’s disease. Mol Neurobiol 45(1):126–143. https://doi.org/10.1007/s12035-011-8226-9
Burré J (2015) The synaptic function of α-synuclein. J Parkinsons Dis 5:699–713. https://doi.org/10.3233/jpd-150642
Soukup SF, Vanhauwaert R, Verstreken P (2018) Parkinson’s disease: convergence on synaptic homeostasis. EMBO J 37(18):e98960. https://doi.org/10.15252/embj.201898960
Pan PY, Zhu Y, Shen Y, Yue Z (2019) Crosstalk between presynaptic trafficking and autophagy in Parkinson’s disease. Neurobiol Dis 122(2017):64–71. https://doi.org/10.1016/j.nbd.2018.04.020
Shimojo M, Madara J, Pankow S, Liu X, Yates J, Südhof TC, Maximov A (2019) Synaptotagmin-11 mediates a vesicle trafficking pathway that is essential for development and synaptic plasticity. Genes Dev 33(5–6):365–376. https://doi.org/10.1101/gad.320077.118
Bereczki E, Bogstedt A, Höglund K, Tsitsi P, Brodin L, Ballard C, Svenningsson P, Aarsland D (2017) Synaptic proteins in CSF relate to Parkinson’s disease stage markers. NPJ Parkinsons Dis 3(1):7. https://doi.org/10.1038/s41531-017-0008-2
Bridi JC, Hirth F (2018) Mechanisms of α-Synuclein induced synaptopathy in parkinson’s disease. Front Neurosci 12:80. https://doi.org/10.3389/fnins.2018.00080
Phan JA, Stokholm K, Zareba-Paslawska J, Jakobsen S, Vang K, Gjedde A, Landau AM, Romero-Ramos M (2017) Early synaptic dysfunction induced by α-synuclein in a rat model of Parkinson’s disease. Sci Rep 7(1):6363. https://doi.org/10.1038/s41598-017-06724-9
Visanji NP, Brooks PL, Hazrati LN, Lang AE (2014) The prion hypothesis in Parkinson’s disease: Braak to the future. Acta Neuropathol Commun 1:2. https://doi.org/10.1186/2051-5960-1-2
Longhena F, Faustini G, Missale C, Pizzi M, Spano P, Bellucci A (2017) The Contribution of α-synuclein spreading to Parkinson’s disease synaptopathy. Neural Plas 2017:5012129. https://doi.org/10.1155/2017/5012129
Ma J, Gao J, Wang J, Xie A (2019) Prion-like mechanisms in Parkinson’s disease. Front Neurosci 13:552. https://doi.org/10.3389/fnins.2019.00552
Gorenberg EL, Chandra SS (2017) The role of co-chaperones in synaptic proteostasis and neurodegenerative disease. Front Neurosci 11:248. https://doi.org/10.3389/fnins.2017.00248
Catoni C, Calì T, Brini M (2019) Calcium, dopamine and neuronal calcium sensor 1: their contribution to Parkinson’s disease. Front Mol Neurosci 12:55. https://doi.org/10.3389/fnmol.2019.00055
Surmeier DJ, Schumacker PT, Guzman JD, Ilijic E, Yang B, Zampese E (2017) Calcium and Parkinson’s disease. Biochem Biophys Res Commun 483(4):1013–1019. https://doi.org/10.1016/j.bbrc.2016.08.168
Benkert J, Hess S, Roy S, Beccano-Kelly D, Wiederspohn N, Duda J, Simons C, Patil K, Gaifullina A, Mannal N, Dragicevic E, Spaich D, Müller S, Nemeth J, Hollmann H, Deuter N, Mousba Y, Kubisch C, Poetschke C, Striessnig J, Pongs O, Schneider T, Wade-Martins R, Patel S, Parlato R, Frank T, Kloppenburg P, Liss B (2019) Cav2.3 channels contribute to dopaminergic neuron loss in a model of Parkinson’s disease. Nat Commun 10(1):5094. https://doi.org/10.1038/s41467-019-12834-x
Zaichick SV, McGrath KM, Caraveo G (2017) The role of Ca2+ signaling in Parkinson’s disease. Dis Model Mech 10(5):519–535. https://doi.org/10.1242/dmm.028738
Brimblecombe KR, Vietti-Michelina S, Platt NJ, Kastli R, Hnieno A, Gracie CJ, Cragg SJ (2019) Calbindin-D28K limits dopamine release in ventral but not dorsal striatum by regulating Ca2+ availability and dopamine transporter function. ACS Chem Neurosci 10(8):3419–3426. https://doi.org/10.1021/acschemneuro.9b00325
Leandrou E, Emmanouilidou E, Vekrellis K (2019) Voltage-gated calcium channels and α-synuclein: implications in Parkinson’s disease. Front Mol Neurosci 12:237. https://doi.org/10.3389/fnmol.2019.00237
Verma A, Ravindranath V (2020) CaV1.3 L-type calcium channels increase the vulnerability of substantia nigra dopaminergic neurons in MPTP mouse model of Parkinson’s disease. Front Aging Neurosci 11:382. https://doi.org/10.3389/fnagi.2019.00382
Surmeier DJ, Guzman JN, Sanchez-Padilla J, Schumacker PT (2011) The role of calcium and mitochondrial oxidant stress in the loss of substantia nigra pars compacta dopaminergic neurons in Parkinson’s disease. Neuroscience 198:221–231. https://doi.org/10.1016/j.neuroscience.2011.08.045
Sgobio C, Sun L, Ding J, Herms J, Lovinger DM, Cai H (2019) Unbalanced calcium channel activity underlies selective vulnerability of nigrostriatal dopaminergic terminals in Parkinsonian mice. Sci Rep 9(1):4857. https://doi.org/10.1038/s41598-019-41091-7
Hurley MJ, Brandon B, Gentleman SM, Dexter DT (2013) Parkinson’s disease is associated with altered expression of Ca V1 channels and calcium-binding proteins. Brain 136(7):2077–2097. https://doi.org/10.1093/brain/awt134
Betzer C, Jensen PH (2018) Reduced cytosolic calcium as an early decisive cellular state in Parkinson’s disease and synucleinopathies. Front Neurosci 12:819. https://doi.org/10.3389/fnins.2018.00819
Angelova PR, Ludtmann MHR, Horrocks MH, Negoda A, Cremades N, Klenerman D, Dobson CM, Wood NW, Pavlov EV, Gandhi S, Abramov AY (2016) Ca2+ is a key factor in α-synuclein-induced neurotoxicity. J Cell Sci 129(9):1792–1801. https://doi.org/10.1242/jcs.180737
Verma M, Wills Z, Chu CT (2018) Excitatory dendritic mitochondrial calcium toxicity: implications for Parkinson’s and other neurodegenerative diseases. Front Neurosci 12:523. https://doi.org/10.3389/fnins.2018.00523
Barazzuol L, Giamogante F, Brini M, Calì T (2020) PINK1/Parkin mediated mitophagy, Ca2+ signalling, and ER-mitochondria contacts in Parkinson’s disease. Int J Mol Sci 21:1772. https://doi.org/10.3390/ijms21051772
Lim J, Yue Z (2015) Neuronal aggregates: formation, clearance, and spreading. Dev Cell 32(4):491–501. https://doi.org/10.1016/j.devcel.2015.02.002
Sulzer D (2011) How addictive drugs disrupt presynaptic dopamine neurotransmission. Neuron 69(4):628–649. https://doi.org/10.1016/j.neuron.2011.02.010
Siciliano CA, Calipari ES, Ferris MJ, Jones SR (2015) Adaptations of presynaptic dopamine terminals induced by psychostimulant self-administration. ACS Chem Neurosci 6(1):27–36. https://doi.org/10.1021/cn5002705
Yorgason JT, Calipari ES, Ferris MJ, Karkhanis AN, Fordahl SC, Weiner JL, Jones SR (2016) Social isolation rearing increases dopamine uptake and psychostimulant potency in the striatum. Neuropharmacology 101:471–479. https://doi.org/10.1016/j.neuropharm.2015.10.025
Cheng HC, Ulane CM, Burke RE (2010) Clinical progression in Parkinson disease and the neurobiology of axons. Ann Neurol 67(6):715–725. https://doi.org/10.1002/ana.21995
Hasbani DM, O’Malley KL (2006) WldS mice are protected against the Parkinsonian mimetic MPTP. Exp Neurol 202(1):93–99. https://doi.org/10.1016/j.expneurol.2006.05.017
Murdoch JD, Rostosky CM, Gowrisankaran S, Arora AS, Soukup SF, Vidal R, Capece V, Freytag S, Fischer A, Verstreken P, Bonn S, Raimundo N, Milosevic I (2016) Endophilin—a deficiency induces the Foxo3a-Fbxo32 network in the brain and causes dysregulation of autophagy and the ubiquitin-proteasome system. Cell Rep 17(4):1071–1086. https://doi.org/10.1016/j.celrep.2016.09.058
Jin EJ, Kiral FR, Ozel MN, Burchardt LS, Osterland M, Epstein D, Wolfenberg H, Prohaska S, Hiesinger PR (2018) Live observation of two parallel membrane degradation pathways at axon terminals. Curr Biol 28 (7):1027–1038e1024. https://doi.org/10.1016/j.cub.2018.02.032
Stavoe AKH, Holzbaur ELF (2019) Autophagy in neurons. Annu Rev Cell Dev Biol 35:477–500. https://doi.org/10.1146/annurev-cellbio-100818-125242
Olgiati S, Thomas A, Quadri M, Breedveld GJ, Graafland J, Eussen H, Douben H, de Klein A, Onofrj M, Bonifati V (2015) Early-onset Parkinsonism caused by alpha-synuclein gene triplication: clinical and genetic findings in a novel family. Parkinsonism Relat Disord 21(8):981–986. https://doi.org/10.1016/j.parkreldis.2015.06.005
Lee S, Imai Y, Gehrke S, Liu S, Lu B (2012) The synaptic function of LRRK2. Biochem Soc Trans 40(5):1047–1051. https://doi.org/10.1042/bst20120113
Arranz AM, Delbroek L, van Kolen K, Guimarães MR, Mandemakers W, Daneels G, Matta S, Calafate S, Shaban H, Baatsen P, de Bock PJ, Gevaert K, Berghe PV, Verstreken P, de Strooper B, Moechars D (2015) LRRK2 functions in synaptic vesicle endocytosis through a kinase dependent mechanism. J Cell Sci 128(3):541–552. https://doi.org/10.1242/jcs.158196
Xiong Y, Dawson TM, Dawson VL (2017) Models of LRRK2-associated Parkinson’s disease. Adv Neurobiol 14:163–191. https://doi.org/10.1007/978-3-319-49969-7_9
Kuhlmann N, Milnerwood AJ (2020) A critical LRRK at the synapse? The neurobiological function and pathophysiological dysfunction of LRRK2. Front Mol Neurosci 13:153. https://doi.org/10.3389/fnmol.2020.00153
Cao M, Milosevic I, Giovedi S, De Camilli P (2014) Upregulation of Parkin in endophilin mutant mice. J Neurosci 34(49):16544–16549. https://doi.org/10.1523/jneurosci.1710-14.2014
Sassone J, Serratto GM, Valtorta F, Silani V, Passafaro M, Ciammola A (2017) The synaptic function of Parkin. Brain 140(9):2265–2272. https://doi.org/10.1093/brain/awx006
Lee W, Koh S, Hwang S, Kim SH (2018) Presynaptic dysfunction by familial factors in Parkinson disease. Int Neurourol J 22:S115–S121. https://doi.org/10.5213/inj.1836216.108
Williams ET, Chen X, Moore DJ (2017) VPS35, the retromer complex and Parkinson’s disease. J Parkinsons Dis 7(2):219–233. https://doi.org/10.3233/jpd-161020
Rahman AA, Morrison BE (2019) Contributions of VPS35 mutations to Parkinson’s disease. Neuroscience 401:1–10. https://doi.org/10.1016/j.neuroscience.2019.01.006
Eleuteri S, Albanese A (2019) VPS35-based approach: a potential innovative treatment in Parkinson’s disease. Front Neurol 10:1272. https://doi.org/10.3389/fneur.2019.01272
Stanic J, Mellone M, Napolitano F, Racca C, Zianni E, Minocci D, Ghiglieri V, Thiolat ML, Li Q, Longhi A, De Rosa A, Picconi B, Bezard E, Calabresi P, Di Luca M, Usiello A, Gardoni F (2017) Rabphilin 3A: a novel target for the treatment of levodopa-induced dyskinesias. Neurobiol Dis 108:54–64. https://doi.org/10.1016/j.nbd.2017.08.001
Shi MM, Shi CH, Xu YM (2017) Rab GTPases: the key players in the molecular pathway of Parkinson’s disease. Front Cell Neurosci 11:81. https://doi.org/10.3389/fncel.2017.00081
Lunati A, Lesage S, Brice A (2018) The genetic landscape of Parkinson’s disease. Rev Neurol (Paris) 174(9):628–643. https://doi.org/10.1016/j.neurol.2018.08.004
Singh PK, Muqit MMK (2020) Parkinson’s: a disease of aberrant vesicle trafficking. Annu Rev Cell Dev Biol 36:237–264. https://doi.org/10.1146/annurev-cellbio-100818-125512
Song L, He Y, Ou J, Zhao Y, Li R, Cheng J, Lin CH, Ho MS (2017) Auxilin underlies progressive locomotor deficits and dopaminergic neuron loss in a Drosophila model of Parkinson’s disease. Cell Rep 18(5):1132–1143. https://doi.org/10.1016/j.celrep.2017.01.005
Nguyen M, Krainc D (2018) LRRK2 phosphorylation of auxilin mediates synaptic defects in dopaminergic neurons from patients with Parkinson’s disease. Proc Natl Acad Sci U S A 115(21):5576–5581. https://doi.org/10.1073/pnas.1717590115
Roosen DA, Landeck N, Conti M, Smith N, Saez-Atienzar S, Ding J, Beilina A, Kumaran R, Kaganovich A, Du Hoffmann J (2019) Mutations in Auxilin cause parkinsonism via impaired clathrin-mediated trafficking at the Golgi apparatus and synapse. BioRxiv. https://doi.org/10.1101/830802
Fasano D, Parisi S, Pierantoni GM, De Rosa A, Picillo M, Amodio G, Pellecchia MT, Barone P, Moltedo O, Bonifati V, De Michele G, Nitsch L, Remondelli P, Criscuolo C, Paladino S (2018) Alteration of endosomal trafficking is associated with early-onset parkinsonism caused by SYNJ1 mutations. Cell Death Dis 9(3):1–15. https://doi.org/10.1038/s41419-018-0410-7
Cao M, Park D, Wu Y, De Camilli P (2020) Absence of Sac2/INPP5F enhances the phenotype of a Parkinson’s disease mutation of synaptojanin 1. Proc Natl Acad Sci U S A 117(22):12428–12434. https://doi.org/10.1073/pnas.2004335117
Nguyen M, Wong YC, Ysselstein D, Severino A, Krainc D (2019) Synaptic, mitochondrial, and lysosomal dysfunction in Parkinson’s disease. Trends Neurosci 42(2):140–149. https://doi.org/10.1016/j.tins.2018.11.001
Vidyadhara DJ, Lee JE, Chandra SS (2019) Role of the endolysosomal system in Parkinson’s disease. J Neurochem 150(5):487–506. https://doi.org/10.1111/jnc.14820
Agliardi C, Guerini FR, Zanzottera M, Riboldazzi G, Zangaglia R, Sturchio A, Casali C, Di Lorenzo C, Minafra B, Nemni R, Clerici M (2019) SNAP25 gene polymorphisms protect against Parkinson’s disease and modulate disease severity in patients. Mol Neurobiol 56(6):4455–4463. https://doi.org/10.1007/s12035-018-1386-0
Longhena F, Faustini G, Varanita T, Zaltieri M, Porrini V, Tessari I, Poliani PL, Missale C, Borroni B, Padovani A, Bubacco L, Pizzi M, Spano PF, Bellucci A (2018) Synapsin III is a key component of α-synuclein fibrils in Lewy bodies of PD brains. Brain Pathol 28(6):875–888. https://doi.org/10.1111/bpa.12587
Atias M, Tevet Y, Sun J, Stavsky A, Tal S, Kahn J, Roy S, Gitler D (2019) Synapsins regulate α-synuclein functions. Proc Natl Acad Sci U S A 166(23):11116–11118. https://doi.org/10.1073/pnas.1903054116
Cao M, Wu Y, Ashrafi G, McCartney AJ, Wheeler H, Bushong EA, Boassa D, Ellisman MH, Ryan TA, De Camilli P (2017) Parkinson sac domain mutation in synaptojanin 1 impairs clathrin uncoating at synapses and triggers dystrophic changes in dopaminergic axons. Neuron 93(4):882–896. https://doi.org/10.1016/j.neuron.2017.01.019
Bento CF, Ashkenazi A, Jimenez-Sanchez M, Rubinsztein DC (2016) The Parkinson’s disease-associated genes ATP13A2 and SYT11 regulate autophagy via a common pathway. Nat Commun 7(1):1–16. https://doi.org/10.1038/ncomms11803
Wang C, Kang X, Zhou L, Chai Z, Wu Q, Huang R, Xu H, Hu M, Sun X, Sun S, Li J, Jiao R, Zuo P, Zheng L, Yue Z, Zhou Z (2018) Synaptotagmin-11 is a critical mediator of Parkin-linked neurotoxicity and Parkinson’s disease-like pathology. Nat Commun 9(1):1–14. https://doi.org/10.1038/s41467-017-02593-y
Garcia-Reitböck P, Anichtchik O, Bellucci A, Iovino M, Ballini C, Fineberg E, Ghetti B, Della Corte L, Spano P, Tofaris GK, Goedert M, Spillantini MG (2010) SNARE protein redistribution and synaptic failure in a transgenic mouse model of Parkinson’s disease. Brain 133(7):2032–2044. https://doi.org/10.1093/brain/awq132
Ageta-Ishihara N, Yamakado H, Morita T, Hattori S, Takao K, Miyakawa T, Takahashi R, Kinoshita M (2013) Chronic overload of SEPT4, a parkin substrate that aggregates in Parkinson’s disease, causes behavioral alterations but not neurodegeneration in mice. Mol Brain 6:35. https://doi.org/10.1186/1756-6606-6-35
Sala G, Stefanoni G, Arosio A, Riva C, Melchionda L, Saracchi E, Fermi S, Brighina L, Ferrarese C (2014) Reduced expression of the chaperone-mediated autophagy carrier hsc70 protein in lymphomonocytes of patients with Parkinson’s disease. Brain Res 1546:46–52. https://doi.org/10.1016/j.brainres.2013.12.017
Sala G, Marinig D, Arosio A, Ferrarese C (2016) Role of chaperone-mediated autophagy dysfunctions in the pathogenesis of Parkinson’s disease. Front Mol Neurosci 9:157. https://doi.org/10.3389/fnmol.2016.00157
Acknowledgements
The authors sincerely acknowledge Government Shahid Gend Singh College, Charama, for providing facilities to Abhishek Kumar Mishra.
Author information
Authors and Affiliations
Contributions
AKM contributed to literature search, review design, manuscript preparation, and editing. AD contributed to manuscript preparation and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors in the manuscript declare that they do not have any conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mishra, A.K., Dixit, A. Dopaminergic Axons: Key Recitalists in Parkinson’s Disease. Neurochem Res 47, 234–248 (2022). https://doi.org/10.1007/s11064-021-03464-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-021-03464-1