Abstract
Glutathione (GSH) is an important antioxidant found abundantly and synthesized intracellularly in the cytosol in a tightly regulated fashion. It has diverse physiological functions, including protection against reactive oxygen species and nitrogen species, antioxidant defense as well as maintenance of cellular thiol status. The human brain due to the high oxygen consumption is extremely susceptible to the generation of reactive oxygen species. GSH plays a paramount role in brain antioxidant defense, maintaining redox homeostasis. The depletion of brain GSH has also been observed from both autopsies as well as in vivo MRS studies with aging and varied neurological disorders (Alzheimer’s disease, Parkinson’s disease, etc.). Therefore, GSH enrichment using supplementation is a promising avenue in the therapeutic development for these neurological disorders. This review will enrich the information on the importance of GSH synthesis, metabolism, functions, compartmentation and inter-organ transport, structural conformations and its quantitation via different techniques. The transportation of GSH in the brain via different interventional routes and its potential role in the development of therapeutic strategies for various brain disorders is also addressed. Very recent study found significant improvement of behavioral deficits including cognitive decline, depressive-like behaviors, in APP (NL−G-F/NL−G-FG-) mice due to oral GSH administration. This animal model study put an emergent need to complete GSH supplementation trial in MCI and AD patients for cognitive improvement as proposed earlier.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glutathione (GSH, γ-glutamyl-cysteinyl-glycine) is an intracellular linear tripeptide comprising of glutamic acid (Glu), cysteine (Cys) and glycine (Gly) amino acids present ubiquitously in all mammalian cells [1]. The presence of the sulfhydryl (SH) group of Cys moiety, renders GSH a potent antioxidant property by interacting with reactive oxygen species /reactive nitrogen species (ROS/RNS) [2, 3]. Upon reduction, GSH forms two molecules which dimerize by disulfide linkage to form oxidized glutathione disulfide (GSSG) [2]. The reduced (GSH) and oxidized disulfide form (GSSG) are interconvertible, with reduced GSH being present as the predominant form [4]. GSH acts in coordination with other redox-active compounds like nicotinamide adenosine diphosphate (NADPH) to regulate and maintain cellular redox status [5]. Glutathione’s mechanism of action involves enzyme glutathione peroxidase (GPx) and glutathione reductase (GR), where GPx is responsible for the conversion of GSH to oxidized form GSSG and GR reduces GSSG back to GSH [6, 7]. The GSH–GSSG cycle inside the cell is primarily involved in the detoxification of hydrogen peroxide (H2O2) to water and oxygen. Additional functions of GSH involve (i) maintenance of antioxidant defense (ii) cellular redox status (iii) detoxification of xenobiotics (iv) Cys reservoir (v) maturation of iron–sulfur (Fe–S) cluster proteins (vi) storage and transport of nitric oxide (NO) [8,9,10].
The profound role of GSH in the brain as a detoxifying agent is critically important because of its higher vulnerability towards oxidative stress (OS), as it utilizes 20% of the O2 consumed by the body whereas constitutes only 2% of body weight [11]. GSH is also involved in other cellular processes such as neuroinflammation and ferroptosis, which brings the attention of pharmacologists pertaining to medical interventions for therapeutic benefits. The depleted levels of GSH trigger ROS generation implicated in the cell death causing various neurological diseases like Alzheimer’s disease (AD), Parkinson’s disease (PD) and multiple sclerosis (MS) [12,13,14,15,16].
Various autopsy as well as in vivo studies indicated that GSH level varies across different brain regions and also with different neurological diseases [14, 17,18,19,20,21]. Several autopsy studies showed that the GSH levels were found to be decreased in the AD brain in comparison to the healthy controls (HC) [17, 18]. A post-mortem analysis of Mild cognitive impairment (MCI) brain samples showed a significant reduction in hippocampal (HP) GSH level [19]. To detect the brain GSH in vivo MEscher GArwood-Point RESolved Spectroscopy (MEGA-PRESS) technique is preferred due to several clinical applications [20,21,22,23,24,25]. Similarly from the in vivo MRS study, GSH levels were reported to be statistically significant in different brain regions like frontal cortex (FC) and HP among MCI and AD patients [14, 20]. The GSH exists in two conformations as extended and in the closed form [22, 23, 26]. Structural aspects of GSH have also clinically indicated from a very recently published in vivo study, which showed that closed GSH conformer was depleted in the anterior cingulate cortex (ACC) and posterior cingulate cortex (PCC) regions, therefore, suggested to be a potential biomarker for AD [21].
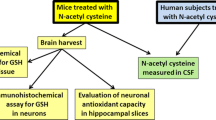
In order to replenish the brain antioxidant defense homeostasis, GSH or N-acetyl cysteine (NAC) as a supplement were reported to be beneficial in modulating GSH levels as suggested in different clinical trials [27,28,29,30,31,32,33,34]. The intervention of supplements to the brain were reported via different modes of delivery like intranasal, intravenous, sublingual and subcutaneous mode, in healthy as well as individuals suffering from neurological disorders [28, 31,32,33, 35,36,37,38,39,40,41,42].
Several studies were found which were focused on varied aspects of GSH such as structure, synthesis, functions, and its use in therapeutic practice. In order to accumulate all the information pertaining to GSH, we present this detailed review article with a focus on GSH biosynthesis, regulation, functions, and metabolism. The GSH in vivo detection and conformational states are also presented in this review. The compartmentalization, Inter-organ transfer and GSH transport to the brain via blood brain barrier (BBB) and its importance in various brain disorders are also discussed. GSH deficiency, therefore, plays a crucial role in aging as well as the pathogenesis of many neurological diseases. Based on these mechanisms and functions mentioned, some potential approaches for supplementation and its therapeutic benefits are also discussed. The review therefore also concentrates on various clinical supplementation studies with the intention to enrich the master antioxidant GSH in the brain. This review presents a critical discussion of the applications of GSH and approaches toward clinical intervention studies of various neurological diseases.
GSH-Biosynthesis, Regulation and Metabolism
GSH is found in the cytosol of all mammalian tissues in the range of 1 to 10 mM concentration [43]. GSH is synthesized using constituent amino acids i.e., Glu, Cys, and Gly in two steps where Glu and Cys combine to form γ-Glu-Cys in the presence of enzyme glutamate cysteine ligase (GCL, EC 6.3.2.2), which further combines with Gly in the presence of GS (Glutathione synthetase; EC 6.3.2.3) to synthesize GSH (Fig. 1) [4]. GCL enzyme is a heterodimer composed of two subunits i.e., catalytically active heavy subunit as GCLC (73 kDa), and light modifier subunit as GCLM (30 kDa). GCLC functions as a substrate-binding unit whereas the GCLM modulates the binding affinity of GCLC by altering the Km value. GS is a homodimer (52 kDa) comprising of two identical subunits [44]. GSH possesses a unique peptide bond formed by the γ-carboxyl group of N-terminal glutamate with the Cys residue. This specific peptide linkage protects GSH from being cleaved by most peptidases which hydrolyze at the α-carboxyl peptide bond of N-terminal amino acids. GSH is cleaved only at the outer surfaces of tissues containing γ-glutamyl transferase (γ-GT) whereas, it remains relatively stable inside the cell [45]. GSH is synthesized in all cell types with the maximum amount of GSH synthesized and exported from the liver. The source of substrates required for GSH synthesis varies between different cell types. Thus, alterations in the GSH plasma level may not reflect changes in GSH synthesis in a specific cell [46]. The whole blood (mainly red blood cells) may contribute approximately 10% of the complete GSH synthesis in humans [47, 48]. A decline in the amount of GCL and GS has been reported to result in the reduction of GSH levels in red blood cells of AD patients [49].
Synthesis of GSH. GSH synthesis is a two-step process where Glu, Cys, and Gly are catalyzed in the presence of enzymes GCL and GS. The figure was designed using BioRender with information taken from existing literature [4]
GSH synthesis regulation occurs (a) via non-allosteric feedback competitive inhibition where GSH (Ki = 2.3 mM) binds with glutamate thus, preventing glutamate from binding to Cys, (b) via the availability of its precursor l-cysteine [43, 50,51,52,53]. The availability of Cys is known to be affected by certain factors like diet and amino acid uptake. The hepatocellular level of Cys is regulated via electroneutral sodium/amino acid co-transporters (ASC) system and cysteine glutamate exchanger (Xc−) as well as the trans-sulfuration pathway [52, 54]. Other major determinants in the regulation of the rate of GSH synthesis are enzymes GCL and GS. Changes in GCL subunits (GCLC and GCLM) occurring at the transcriptional and post-transcriptional level has been extensively studied [55,56,57]. The post-transcriptional regulation of GCLC involves mRNA stabilization/destabilization of certain signaling molecules (PI3K/AKT/p70S6K) activated by insulin [58]. Unlike GCL, regulation by enzyme GS has been unexplored and overlooked and requires further research to reach conclusive inference.
GSH acts as an antioxidant in two ways as (i) it directly reacts non-enzymatically with free radicals such as superoxide radical (O2.−), NO, or hydroxyl ion (OH−) [59,60,61,62] and (ii) indirectly functions as a reducing agent by donating an electron to H2O2 for its reduction to water and O2 in the presence of GPx enzyme [63, 64]. GPx (EC 1.11.1.9) exists in two forms i.e., selenium-dependent and selenium independent. Four seleno-cysteine-containing isozymes of GPx reported to date are GPx 1, 2, 3 and 4 [65]. Now, GSH is reported to be extensively used as a co-substrate by GPx reducing H2O2 to water and O2 molecules and conversion of lipid hydroperoxides (LOOH) into organic peroxides (ROOH) producing GSSG [7]. GSSG formed further follows two fate (i) gets reduced back to GSH by GR [6] (ii) excreted outside the cell. GR (EC 1.8.1.7) functions as dimeric disulfide oxidoreductase which acts by transferring an electron from NADPH to GSSG, thereby regenerating GSH [66].
Functions of GSH
The OS in the biological process occurs as a result of the excessive production of free radicals. Oxidative stressors such as ROS are derived from a series of univalent reduction of O2 molecules produced as a result of aerobic respiration and substrate oxidation. ROS are involved in various biological processes such as cell growth, cell signaling, immune responses [67,68,69]. Excessive ROS production is known to damage the cellular system by oxidation of major biomolecules (lipids, proteins, and nucleic acids) [70,71,72,73]. Mitochondria being the most redox-active cell organelle produces mitochondrial ROS in the form of O2.−, hydroxyl radical (·OH) and H2O2 [74,75,76,77].
Mitochondrial complex I (∼ 1 MDa), comprising of 45 polypeptides in mammals, is the entry point of electrons from NADH into the electron transport chain (ETC). Electrons released from NADH are accepted by the flavin mononucleotide (FMN) cofactor, which then passes the electrons through a chain of Fe–S clusters to the ubiquinone (Q) reduction site. During these events, NADH is oxidized to NAD+, FMN is reduced to FMNH2 and Q is reduced to ubiquinol (QH2) [78, 79]. Large amounts of O2.− (by univalent reduction of O2) generation have been reported in isolated mitochondria via two modes of operations: mode 1, when NADH is abundantly present (high NADH/NAD+ ratio) and mode 2, when there is a large proton-motive force (∆p) and reduced Q pool. Thus, the kinetics and thermodynamics factors favoring the interaction of potent one-electron donors with O2 controls the mitochondrial ROS production [80]. The predominant site of O2.− production in both the modes is in complex I, thus making it a major source of O2.− production within the mitochondria [81,82,83,84]. The mechanism of O2.− production in two modes are different as the production of O2.− in mode 1 occurs during the reduction of FMN to FMNH2 in the presence of abundant NADH whereas, the mode 2 involves O2.− production via reverse ETC where electrons are forced back from QH2 to complex I [85]. Under some conditions, when the build-up of NADH and Q coincides with a large ∆p, both modes operate simultaneously. Mitochondrial complex III (∼ 240 kDa monomer) accepts electrons from Q pool and reduces cytochrome-c. The complex III has been regarded as a source of O2.− within mitochondria for a long period of time [86, 87]
The superoxide dismutase (SOD) neutralizes O2.− into H2O2 which follows three fates (i) it is reduced by Fe2+ (normally present in cells) which donates an electron to produce ·OH, OH− and Fe3+ in Fenton’s reaction. An ·OH is a highly reactive molecule with high oxidizing ability. It oxidizes cellular components such as proteins, lipids and DNA by removal of an electron (associated with H atom) (ii) it combines with O2.− to generate OH−, ·OH and O2 in Haber Weiss’s reaction, (iii) H2O2 is neutralized to H2O and O2 in a reaction catalyzed by inter-conversion of GSH to GSSG via GPx. The ROS production within the mitochondria results in oxidative damage to mitochondrial lipid membrane, proteins, DNA and ATP synthesizing ability. The mitochondrial ROS also causes derangement in the majority of cellular metabolic functions including the citric acid cycle, urea cycle, amino acid metabolism, haem synthesis, Fe–S center assembly and fatty acid oxidation. The mitochondrial oxidative damage may also result in the release of intermembrane space proteins such as cytochrome-c in cytosol leading to activation of the cellular apoptotic machinery. Consequently, mitochondrial oxidative damage contributes to a wide variety of pathologies [88]. The detailed mechanism of free radical generation and fate of H2O2 are illustrated in Fig. 2.
Schematic view of ROS production and antioxidant defense system in mitochondria. NADH generated by the citric acid cycle inside the cell serves as an electron donor. During electron transport chain (ETC), electrons are passed through mitochondrial complexes “down the line”. Two electrons removed from NADH are accepted by an FMN cofactor in Complex I. During this phase, NADH+ H+ is oxidized to NAD+ by reducing FMN to FMNH2. The electrons from FMNH2 are passed further through Fe–S clusters to Q reduction site where Q is reduced to QH2. Complex II catalyzes the oxidation of succinate to fumarate and electrons gained during this reaction are accepted by FAD and passed further via a chain of Fe–S clusters to Q. During these chains of events FAD is reduced to FADH2 and Q is reduced to QH2. Complex III accepts electrons from QH2 which are transferred one by one in a complex process called the Q-cycle onto another electron carrier, cytochrome-c. Reduced cytochrome-c further gets oxidized by complex IV i.e. cytochrome-c oxidase to reduce oxygen to water. The proton-motive force (∆p) generated in the form of H+ ions finally leads to ATP synthesis via complex V i.e. ATP synthase, thereby completing the electron transport chain. However, some electrons can escape the respiratory chain (complex I and complex III processes) and combine with O2 to form O2.−. The superoxide dismutase (SOD) present inside mitochondria reduces O2.− to H2O2 which follows three fates where, (i) it is reduced by Fe2+ to produce ·OH, OH− and Fe3+ in Fenton’s reaction. (ii) it combines with O2.− to generate OH−, ·OH, and O2 in Haber Weiss’s reaction, (iii) it is converted to H2O and O2, catalyzed by inter-conversion of GSH to GSSG via GPx. The figure was designed using BioRender with information taken from existing literature [64, 74, 76, 77, 88, 89]
To maintain redox homeostasis, the cellular system possesses an antioxidant defense system as a counteractive mechanism which includes various antioxidants such as SOD, catalase, vitamin C, vitamin E, and GSH. Catalase is predominantly found in peroxisomes but its mitochondrial expression shows antioxidative effectiveness to be dependent upon the oxidant and the site of ROS production. The absence of catalase inside the mitochondria increases its vulnerability towards OS generation [90, 91]. GSH is mainly responsible for protection against ROS and RNS however other important functions include maintenance of redox status, detoxification of xenobiotics, regulation of cellular events including gene expression, DNA and protein synthesis, apoptosis, signal transduction, protein glutathionylation, cytokine production and immune response [8,9,10]. The specialized structural, biochemical and biophysical properties and its ability to synthesize independently determine its potential functions as a primary antioxidant [92, 93].
GSH donates an electron to form two glutathione-thiyl radicals (GS*), which further combine to form GSSG. The antioxidant function of GSH involves catalytic oxidation of thiol group of its Cys moiety in the presence of GPx to produce GSSG which in turn is reduced to GSH in the presence of GR. The detoxification of H2O2 to water and O2 molecules is catalyzed by the conversion of GSH to GSSG via GPx [64, 94]. NO produced from l-arginine by nitric oxide synthase (NOS), is a reactive gaseous free radical known to react with O2.− and cause nitrosative stress inside the cell by forming nitroxyl radicals (HNO), nitric oxides (NO2, N2O4, N2O3), peroxynitrite (ONOO−) and S-nitrosothiols (RSNO) [95]. These nitric oxide radicals generated are neutralized to S-nitroso glutathione (GSNO) by GSH thereby reducing nitrosative stress [96, 97]. GSH is also involved in the conversion of LOOH into lipid hydroxides (LOH), protein oxidant (P-SOH) into glutathionylated protein, and also helps in DNA repair (Fig. 3) [10, 94, 98, 99]. GSH also aids in the storage of Cys molecules as reactive Cys undergoes rapid autoxidation to form Cystine. Cystine produces toxic O2 radicals, therefore GSH act as a carrier and scavenger for the transport of Cys molecule [100].
Involvement of GSH in cellular detoxification. GSH conversion to GSSH releases an H+ moiety which is utilized for neutralization of oxidants such as (i) H2O2, (ii) NO·, (iii) LOOH and (iv) P-SOH into their less toxic forms i.e. H2O, GSNO, LOH, PS-SG respectively, (v) GSH is also involved in nucleic acid repair. The figure was designed using BioRender with information taken from existing literature [10, 94, 96,97,98,99]
Studies have also reported that GSH is primarily responsible for detoxification of xenobiotics, either directly by conjugating or acting as a substrate in conjugation reactions. Total antioxidant capacity levels were decreased on chronic exposure to xenobiotics like alcohol, explicating the fact that chronic exposure to xenobiotics leads to lipid peroxidation, depletion of cytosolic GSH stores and mitochondrial damage [101]. The transcriptional control involved behind the detoxification of xenobiotics is nuclear factor erythroid 2-related factor 2 (Nrf2)/Kelch like ECH associated protein 1 (Keap1) system [102]. GSH, being involved in detoxification could be an effective therapeutic strategy to decrease the toxic effects of xenobiotics inside the body.
GSH plays another important function, where it is involved in the maintenance of metal homeostasis. The redox-active metals like iron, copper, and chromium, undergo redox cycling and cause OS directly via Fenton’s reaction. Redox-inactive metals such as lead, cadmium, mercury, cobalt, and arsenic exhaust cell’s SH reserves and are indirectly involved in ROS formation [103, 104]. Redox-active metals cause cellular damage via production of ROS i.e., ·OH, O2.− and H2O2 (Fig. 2). The mechanism of redox-active metal-induced oxidative damage is extensively studied whereas the mechanism of redox inactive metals remains elusive and feasibly involves increased lipid peroxidation, alteration in thiol status and DNA damage [105, 106]. Metal induced toxicity and interactions with cellular aggregates have also been associated with neurodegenerative disorders such as AD [107, 108]. The role of GSH in the neutralization of redox-active metal like copper and iron is well documented where GSH is believed to be responsible for their mobilization, transport, and delivery to specific target molecules [109, 110]. The involvement of GSH in the maturation of Fe–S cluster proteins is also reported [111, 112].
GSH is also known to be involved in the maintenance of optimal cytokine levels. Pro-inflammatory cytokines i.e., tumor necrosis factor-α (TNF-α), Interleukin-1β (IL-1β) and IL-6 gene expression were increased due to GSH depletion, which further led to check the expression of anti-inflammatory cytokines i.e., IL-10. The levels of IL-10 remained unaltered elucidating the fact that GSH depletion leads to stimulation of pro-inflammatory cytokines and not anti-inflammatory cytokines [113, 114]. This GSH homeostasis alteration is resulted due to upregulation in nuclear factor kappa light chain enhancer of activated B cells (NFκβ) and c-Jun N-terminal kinase (JNK) signaling pathway which could be the plausible apoptotic pathway towards neuronal cell death [115, 116].
The balance of the GSH/GSSG ratio is crucial for the maintenance of redox status and cell survival [117, 118]. Starvation induced OS resulted in decreased GSH and shift towards more oxidizing conditions which further potentiated autophagy [119]. GSH reduction was observed in response to the treatment of tetrahydrobiopterin (BH4; an OS inducer) via activation of p38MAPK/p53 signaling cascade of apoptosis [120]. GSH depletion due to increased OS resulted in GPx4 inhibition that potentiated iron-induced cell death (ferroptosis) [121,122,123]. Overall the above-reported evidences suggest the involvement of GSH in various cell death pathways i.e. autophagy, apoptosis, and ferroptosis. Autophagy and apoptosis involve common inducing conditions (starvation) with autophagy underlying the first cell response (survival) before proceeding to apoptosis. GSH function in cellular detoxification is illustrated in Fig. 3.
Compartmentalization and Inter-Organ Transport of GSH
GSH pool is compartmentalized in different intracellular organelles like cytoplasm, mitochondria, endoplasmic reticulum (ER), and nucleus. GSH synthesized in the cytosol, is transported and distributed for its utilization in different organelles where it is involved in the regulation of cellular redox status. The reduced form of GSH is prominent in all the organelles except ER. In ER, GSSG serves as an oxidizing equivalent for the production of nascent polypeptides conformation by intramolecular disulfide bond formation between Cys residues [124,125,126,127]. In the nucleus, GSH plays a crucial role in maintaining the redox status of sulphydryl groups of proteins involved in DNA synthesis and repair. In addition, GSH also reduces ribonucleotides to give deoxyribonucleotides [125]. Due to the fact that mitochondria have a pivotal role in programmed cell death (apoptosis) and are the site of extensive ROS production, it constitutes 10–15% of total cellular GSH [128]. The inner mitochondrial membrane is rich in a specific phospholipid, cardiolipin which provides stability and fluidity to the membrane. Cardiolipin is associated with cytochrome-c at the inner mitochondrial membrane. The mitochondrial GSH (mGSH) protects cardiolipin from oxidative damage thus prevents the inner membrane from destabilization and dissociation of cytochrome-c. ROS generation results in an increase in internal membrane permeability for calcium ions which triggers apoptosis [45]. Thus, mGSH plays an important role here by preventing apoptosis which is triggered by the release of cytochrome-c from the inner mitochondrial membrane. Hence, reduction in mGSH has been associated with various diseases such as diabetes mellitus, liver cirrhosis, neurological diseases like AD and PD [17, 129,130,131].
GSH is secreted in high concentrations which are translocated from hepatocytes into bile canalicular spaces and plasma [132, 133]. It is hydrolyzed into its constituent amino acids (i.e. Glu, Cys and Gly) in bile spaces where it is captured by hepatocytes to resynthesize GSH. The plasma GSH level is relatively low (22–27 µM), apparently due to its fast utilization by tissues having γ-GT enzyme located on the external surface of some tissues [134]. The highest amount of γ-GT activity is found in the kidney thus, kidney is the major organ for the extraction of GSH from plasma. The GSH translocation to extracellular spaces is an important factor for cellular GSH turnover. GSH from plasma is extracted by kidneys where it is hydrolyzed into its constituent amino acids by membranous enzymes (γ-GT) and peptidases. Renal tubular cells also secrete GSH into the tubular lumen where it is hydrolyzed into its constituent amino acids. These amino acids are taken up by renal tubular cells to resynthesize GSH. These constituent amino acids are also transferred to plasma from where they are translocated to the liver and small intestine through Na-dependent amino acid transporters for GSH synthesis. The GSH synthesized in intestinal epithelial cells is degraded and the constituents amino acids are taken up by the liver to restore GSH [135, 136]. While in the brain, the GSH is translocated from the plasma via the BBB [137]. The concentration of GSH varies in different tissues. Liver and small intestine contain highest concentration of GSH in body ranging from 1 to 6 mM [43], followed by kidney (2–5 mM) [138], brain (2–3 mM) [139], blood (~ 1 mM) [140, 141], and lung epithelial cells (0.42 mM) [142]. The combination of secretion, hydrolysis, and restoration of GSH and translocation of its constituent amino acids constitutes (i) Hepato-renal cycle (ii) Entero-hepatic cycle (iii) Intra-renal cycle and (iv) Intra-hepatic cycle, as illustrated in Fig. 4.
Inter-organ GSH transport. GSH is secreted from hepatocytes into empty spaces and bile canalicular spaces. This GSH is degraded in kidneys by membranous γ-GT and other peptidases. GSH from the liver is also transferred to the small intestine where it is hydrolyzed to its constituent amino acids on the brush border membrane. The resulting amino acids are taken up by intestinal epithelial cells by Na dependent transporters and transferred to plasma from where they are transferred back to the liver for its regeneration. GSH is translocated from plasma to the brain via the BBB. The figure was designed using BioRender with information taken from existing literature [136]
GSH in the Brain
Biosynthesis
The brain constitutes only 2% of the bodyweight but utilizes 20% of the O2 used by the whole body. Due to the high O2 utilization and poor antioxidant status, the brain is highly susceptible to OS [11]. Amongst the major central nervous system (CNS) cells, the concentration of GSH is highest in astrocytes followed by neurons [143,144,145,146]. GSH is synthesized as de novo in astrocyte using its constituent amino acids Glu, Cys and Gly. The GSH synthesized in an astrocyte is transported to extracellular space via multiple drug resistance protein 1 (MRP1) where it is hydrolyzed into CysGly and γ-GluX moieties by enzyme γ-GT [147,148,149]. The CysGly moiety is cleaved into Cys and Gly via neuronal ectopeptidase aminopeptidase which is transported to neuron via excitatory amino acid carrier 1 (EAAC1) and glycine transporter (GlyT2) respectively [149,150,151,152,153,154,155]. The Cys and Gly combine with Glu (provided by glutamate-glutamine cycle operating between astrocytes and neurons) to synthesize GSH [156] (Fig. 5). Due to the major role played in the synthesis and transport of GSH precursors, astrocyte act as a neuroprotector against OS and neurodegeneration [157].
GSH synthesis in CNS. GSH is exported from the astrocyte through MRP1 and is catabolized by the ectozyme γ-GT to provide CysGly and γ-GluX. The resulting amino acids are further catabolized by aminopeptidase into Cys and Gly and are taken up by the neuron via EAAC1 and GlyT2 respectively. In the neuron, Cys and Gly are combined with Glu (provided by glutamate-glutamine cycle) to synthesize GSH. The figure was designed using BioRender with information taken from existing literature [149, 153]
Route and Transport Across BBB
BBB formed by the blood vascular endothelial cell lines the cerebral microvessels and is required to control the brain microenvironment by separating the blood from the brain. Various molecules are transported through BBB via different routes [158, 159]. Paracellular transport through tight junctions is responsible for the transport of simple water-soluble molecules, while other lipid-soluble substances like steroids and alcohol are transported passively via diffusion. Other molecules such as amino acids and glucose are transported via solute carrier-mediated transport based on concentration gradient with the use of ATP as an energy source. GSH is a tripeptide known to cross the BBB through Na-dependent GSH transporter, which belongs to the solute carrier family [137]. Other routes like receptor-mediated transcytosis, adsorptive-mediated transcytosis are responsible for the transport of macromolecules and charged molecules with characteristic receptor-ligand interaction and electrostatic properties respectively (Fig. 6) [160]. The efflux transporters are also present for the extrusion of drugs outside the brain [161].
Routes of transport across the blood brain barrier (BBB): (i) Several simple water molecules pass the BBB through paracellular transport (ii) Certain other compounds like lipid molecules pass passively via diffusion. (iii) Solute carrier transporters are involved in energy mediated active transport of certain molecules like glucose, amino acids, and nucleosides. (iv) Receptor-mediated transcytosis requires the receptor binding of ligand and can transport various molecules like peptides and proteins across the BBB. (v) Adsorptive-mediated transcytosis involves the transfer of charged molecules like cationic peptide to cross the barrier via electrostatic interactions. (vi) Efflux transporter is responsible for the extrusion of drugs out of the brain. The figure was designed using BioRender with information taken from existing literature [158]
Based on the previous studies on GSH uptake by endothelial cells in rat and bovine brain led to experiments of GSH uptake in human cerebrovascular endothelial cells and fetal human embryonic cells. Na dependent GSH transporters are reported to be localized in the lumen of endothelial cells [162,163,164]. This Na-dependent GSH transporter was shown to be bidirectional. Uptake of GSH by astrocytes was also checked which elucidated the presence of Na dependent GSH transporters in both astrocytes and brain endothelial cells. Once it reaches to astrocytes, GSH takes its path until it reaches neuron via carrier-mediated transporters (Fig. 7) [137].
GSH transport across the blood brain barrier (BBB): GSH uptake from the blood (luminal side) to the brain (abluminal side) is mediated via Na dependent GSH transporter localized at the luminal membrane. This GSH from abluminal side en-route astrocyte via Na dependent GSH transporter, which is effluxed through carrier-mediated transporter to neuron. The figure was designed using BioRender with information taken from existing literature [137]
Biophysical, Chemical and Conformational Characteristics of GSH
The physical and chemical properties of GSH are enlisted as—molecular weight 307 g/mol, intermediate molecular flexibility with nine rotatable bonds, the lipophilicity of—6.4; and molecular topological surface area of 160 Å [93]. Nuclear magnetic resonance (NMR) and molecular dynamic studies have reported that GSH exists in two interconvertible conformations “extended” and “folded” (closed) forms, though in aqueous solution it remains typically in “extended” form [26]. Under physiological conditions, the conformational distribution and hydrogen-bonding network plays a crucial role in GSH functioning. Due to the presence of Cys molecule, the GSH is considered to be very sensitive to the surrounding environment. The analysis of NMR spectra obtained in the inert environment reported that GSH exists mainly in closed conformation which is identified by the presence of Cys Hβ peak at 2.79 ppm while the GSH also exists as extended conformation, identified by the presence of Cys Hβ peak at 2.95 ppm [22, 23, 26]. Very recently, for the first time, study reported alterations of in vivo GSH closed conformers among normal, MCI and AD brain using the MEGA-PRESS pulse sequence [21] (Fig. 8).
Structure of GSH and its conformations: a GSH structure and its two confirmations i.e., closed and extended. b NMR experiment results depicting the Cys-Hβ peak of GSH at 2.79 ppm for closed and 2.95 ppm for extended conformer. NMR spectra of GSH within two different environments (i) without oxygenated environment and (ii) completely oxygenated environment. c In vivo (human brain) MRS data were processed using in-house developed MATLAB based MRS signal processing and analysis toolbox, KALPANA. [165]. Necessary permissions were taken to reproduce GSH structure and the NMR spectra from the publishers—Elsevier [14], IOS Press [23] FEBS [166], Springer [26] and Frontiers [167]
Brain GSH Quantification
Differences in GSH content between brain regions may reflect variations in the availability of GSH for vital cellular functions. The highest concentration of GSH is observed in the cortex followed by HP, cerebellum, striatum and substantia nigra (SN) [168, 169]. GSH metabolism-related disorders in the brain are highly correlated with an increased level of OS due to ROS generation [170]. Thus, to develop a clear understanding, accurate estimation of GSH content in the brain is necessary with clinical significance. GSH measurement in autopsy brain was performed by various methods such as high-performance liquid chromatography with UV detection and spectroscopic technique for evaluation of the oxidative product of 5,5′-Dithio-bis (2-nitrobenzoic acid) [171, 172]. However, the in vivo detection of GSH in the human brain is performed by proton magnetic resonance spectroscopy (1H MRS).
Autopsy Studies
GSH levels in the cingulate cortex region of autopsy brain samples (N = 10) were found to be decreased in the AD brain in comparison to the HC, whereas no significant changes in GSH levels were observed in the PD brain [17]. In another study, prefrontal cortex regions obtained from autopsy brain tissues of non-cognitively impaired (N = 10), MCI (N = 8), mild/moderate AD (N = 4), and late-stage AD (N = 9) patients were assessed for GSH levels and significantly decreased GSH levels were reported in post mitochondrial supernatant, mitochondria, and synaptosomal fractions in MCI, AD and late AD samples in comparison to controls [18]. A study investigated GSH in HP (N = 6), from post-mortem autopsy brain of MCI patients, showed that GSH was significantly decreased in HP in comparison to HC samples [19].
In Vivo Studies Using MRS
In order to detect the GSH in vivo in various brain regions, special pulse sequence MEGA-PRESS is considered as a selective and confirmatory method of choice [14, 23, 32, 173]. This technique has several clinical applications, as it is useful in understanding various neurological disease processes [20,21,22,23,24,25]. The multi-centric study from our laboratory confirmed the existence of two GSH conformers (extended and closed) as illustrated in (Fig. 9a) [23]. Additionally, a very recent study from our laboratory also for the first time showed the clinical importance of GSH and reported that the closed GSH conformer is depleted in ACC and PCC regions and therefore suggested to be a potential biomarker for AD [21]. In our earlier in vivo MRS study, the GSH levels were reported to be statistically significant in the right and left FC region among AD female and male (F/M-7/7) patients as compared to healthy young female and male (F/M-20/25) controls respectively [20]. Another study conducted to detect GSH concentrations in different brain regions like the HP (right and left regions) suggested that MCI (N = 22) and AD (N = 21) patients had significantly decreased GSH levels when compared to healthy old control (N = 21) [14] (Fig. 9b).

The figure reproduced with permission from IOS Press [23]. b Box plot representation of GSH concentrations in the right hippocampus (RH) and left hippocampus (LH) regions among HC (green), MCI (blue) and AD (red) subjects. A significant reduction was observed in the RH and LH regions of AD and MCI patients in comparison with HC. All significant values were set at p < 0.05 (*p < 0.05, **p < 0.01, ***p < 0.001). Necessary permissions were taken to reproduce the figure from the publisher—Elsevier [14] (Color figure online)
GSH detection via MRS. a Quantitation of GSH peaks using MRS from healthy subjects (voxel size = 3.5 × 3.5 × 3.5 cm3 on the left parietal cortex). The MEGA-ON and MEGA-OFF excitation pulse positions are (I) 4.40 ppm and 5.00 ppm, (II) 4.56 ppm and 5.00 ppm, respectively. These were processed using in-house developed MATLAB based MRS signal processing and analysis toolbox, KALPANA [165] to get Cys Hβ peak of extended (2.95 ppm) and closed form (2.80 ppm) of GSH.
Apart from neurodegenerative diseases, in vivo detection was also proven to be beneficial in epilepsy, schizophrenia, and MS [24, 25, 174]. A study conducted with the objective to measure GSH level in the parieto-occipital region in epilepsy patients showed that GSH/water ratio was significantly reduced as compared to HC [174, 175]. GSH levels quantified in the posterior medial FC of patients with schizophrenia (N = 20) showed a significant negative correlation between GSH levels and scale for assessment of negative symptoms total scores (r = − 0.68) and negative symptom subscore on Brief Psychiatric Rating Scale (r = − 0.60) [24]. Similar studies for GSH detection were conducted in the grey matter region in MS patients where a significant decrease in GSH concentration (2.4 ± 0.5 mM) was observed as compared to control (3.3 ± 0.1 mM). However, no significant difference in white matter was observed [25].
Supplementation for GSH Enrichment
To maintain the disturbed antioxidant defense homeostasis in the brain, certain antioxidants such as GSH, vitamin C, vitamin E, and NAC were provided as a supplement to healthy as well as patients with various neurological disorders [27,28,29,30, 34, 39, 176,177,178,179,180,181]. However, it has been reported that vitamin C and E are dependent on GSH for their regeneration [92]. Therefore, GSH and its precursors like NAC could be the potential therapeutic strategy in the form of supplements. NAC is a precursor to the amino acid L-cysteine and consequently the antioxidant GSH. NAC is also reported to be effective in crossing the BBB [182, 183]. The GSH level is replenished intracellularly by the intervention of Cys prodrug—NAC therefore is considered as a well-tolerated antidote for Cys/GSH deficiency [184]. The NAC promotes GSH biosynthesis, scavenges ROS, and upholds detoxification consequently effective in treating disease-associated OS [34, 178, 180, 185]. The reduced GSH levels were also responsible for increased OS in various neurodegenerative disorders like AD, PD, and ALS which further led to cellular death as reported in several studies [116, 129, 186, 187]. To prevent this pathology, exogenous GSH was delivered and the progression of disease was evaluated [31,32,33, 35]. This delivery of GSH or NAC for therapeutic application is accomplished via different modes of delivery which are discussed further in detail.
Modes of Delivery for GSH and NAC Supplementation to the Brain
The modes of GSH or NAC delivery to the brain are similar to any other drug such as oral, intravenous, intranasal, sublingual and intramuscular. Orally administered drugs are the most common which undergo the first-pass metabolism i.e., drugs are first absorbed in the gut, reach the liver via the hepatic portal vein and then enter the systemic circulation. The intestinal wall and liver consist of enzyme γ-GT which metabolizes GSH into its constituent amino acids thereby decreasing the systemic bioavailability of drugs [181]. There are different studies conducted with oral GSH supplementation in different doses and conditions [27, 29, 181, 188,189,190,191]. Similarly, the oral formulation for NAC was also evaluated [30, 34, 178,179,180]. While the intravenously administered drug is directly provided in the veins to reach the bloodstream [192]. Likewise, the administration of intranasal drug travels through fast axonal transport along with the perinuclear space surrounding the nerve cell via trigeminal and olfactory nerves to reach into the cerebrospinal fluid (CSF)/brain interstitial fluid through a transcellular pathway. This mode of transfer allows the direct transfer of drugs from an intranasal cavity to the brain by circumventing the BBB [193, 194]. Sublingually administered drug is absorbed in oral mucosa and reaches directly to the bloodstream through the ventral surface of the tongue [195]. Similarly, the intramuscularly administered drug is injected into the muscles from where it reaches the blood [196]. Several studies of GSH, as well as NAC supplementation in healthy as well as various disorders such as PD, amyotrophic lateral sclerosis (ALS), MS and autism spectrum disorder (ASD) through intranasal, intravenous, sublingual and subcutaneous mode, were also reported [28, 31,32,33, 35,36,37,38,39,40,41,42].
Clinical Trials Involving GSH and NAC Supplementation in Healthy Individuals
The supplementation of GSH or NAC was found to be beneficial among HC as evidenced in several clinical trials conducted with different outcome measures [27,28,29, 42, 181, 197]. A pilot randomized trial with oral liposomal GSH (500 and 1000 mg for 1 month) in HC (N = 12) has been reported to be effective in elevating GSH levels and improving the immune function and OS [29]. A trial conducted to determine the long-term effectiveness of oral GSH (250 and 1000 mg/day, 6 months) on body stores in healthy adults (N = 54), showed increased GSH levels in the blood after 1, 3 and 6 months vs baseline [27]. Another study conducted to compare the bioavailability, effect on OS markers and the safety of a sublingual form of GSH with two commonly used dietary supplements, NAC and oral GSH, where sublingual GSH (450 mg), Oral (450 mg) and NAC (200 mg) were provided for 3 weeks to 20 normal volunteers. Significant superiority of the sublingual form of GSH over the oral form, both in terms of bioavailability and positive effects on OS was observed [28]. In a randomized, double-blind, placebo-controlled clinical trial investigating effects of oral GSH supplementation (500 mg, for 4 weeks) on biomarkers of systemic OS in human volunteers (N = 40), no significant changes in total GSH and measures of GSH/GSSG ratio were observed [181].
Evidence of GSH and NAC Supplementation Trials in Various Neurological Disorders
Disturbance in the level of GSH or associated enzymes (GPx) are observed in different neurological disorders such as AD [14, 198], PD [15, 199], MS [200, 201], ASD [202], and ALS [203]. Therefore, providing GSH or NAC as a supplement reported being beneficial in modulating the brain GSH level as suggested in different clinical trials [30,31,32, 39, 42, 180, 197, 204, 205]. Different clinical trials involving GSH or NAC as an intervention are discussed further for AD, PD, MS, ASD and ALS diseases.
Alzheimer’s and Parkinson’s Disease
AD is a neurodegenerative disorder characterized by progressive memory loss, disorientation and pathological markers (senile plaques and neurofibrillary tangles) [206]. Similarly, PD is also a neurodegenerative disorder characterized by the loss of dopaminergic neurons affecting mobility and muscle control [207]. The increased OS and GSH reduction have been well found to be associated with these neurodegenerative disorders [208, 209]. Reduced levels of GSH was observed in regions susceptible to AD and PD like the HP, FC and SN [14, 15, 198, 199]. The study was performed to evaluate the intranasal GSH uptake in PD where 15 participants were involved in self-administration of GSH and results were observed after different time-periods. A significant increase in GSH concentration was observed after 45 min of GSH administration. This result demonstrates the plausible role of GSH in the therapeutics of PD [32]. To the best of our knowledge, no clinical trial was found to assess brain GSH levels in AD patients with the intervention of GSH.
Several trials with NAC supplements were reported in AD and PD patients. A double-blinded, multi-site, phase II study was conducted in 106 AD individuals randomized to oral nutraceutical formulation (folate, alpha-tocopherol, B12, S-adenosyl methionine, NAC, acetyl-l-carnitine) or placebo for 3 or 6 months. The active control showed significant improvement in cognitive performance and the Dementia Rating Scale [34]. Similarly, a placebo-controlled trial of 34 MCI patients, 600 mg of oral NAC (along with folate, alpha-tocopherol, vitamin B12, S-adenosyl methionine, and acetyl-l-carnitine) for 6 months was associated with improvement in dementia rating scale and preservation of executive function [40]. Another clinical trial specifically testing NAC in probable AD (N = 43) reported that oral NAC (50 mg/kg/day) failed to significantly improve MMSE scores in 6 months duration [179]. In another open-label 4-week prospective study with an oral NAC in PD (N = 5) and HC (N = 3), where brain GSH in the occipital cortex was measured using 1H MRS (3 and 7 T) before and after 28 days of 6000 mg NAC/day. Although peripheral antioxidant measures (catalase and GSH/GSSG) increased significantly, no significant increases in brain GSH were observed for the healthy and PD groups [180]. Another study with 3 PD, 3 Gaucher disease (GD) patients and 3 HC subjects observed that a single intravenous dose of NAC resulted in an increase of the blood GSH/GSSG ratio which was followed by an increase in brain GSH concentrations in all those subjects. No conclusive outcome was inferred due to the small sample size and study duration [39].
Multiple Sclerosis
MS is a chronic autoimmune, inflammatory neurological disease of CNS attacking myelinated axons (white matter) [210]. Enzymes like GPx and selenium were reported to be reduced in MS patients [200, 201]. Therefore, supplementation with selenium salts is being tested in a patient along with GSH, to check whether selenium treatment helps in the treatment of pathology. In a study, 18 MS patients were provided with 6 tablets of selenium (equivalent to 6 mg) for five weeks and GPx levels were monitored and quantified. GPx levels were increased significantly in the treatment group (10.4 ± 4.5 micro katal per gram (µkat/g) protein) as compared to control group (3.97 ± 2.09 µkat/g protein) [31].
Autism Spectrum Disorder
ASD is a set of neurodevelopmental disorders characterized by behavioral deficits and non-verbal interactions such as reduced eye contact, facial expression, and body gestures [211]. Children with autism were reported to be diagnosed with lower plasma GSH levels, therefore, the study was designed to check whether GSH supplementation increases the plasma GSH levels in autistic children [202]. The study was an eight-week, open-label trial using oral lipoceutical GSH (N = 13) or trans-dermal GSH (N = 13) in ASD children of 3 to 13 years of age. The oral treatment group showed significant increases in plasma reduced GSH, but not whole-blood GSH levels post supplementation [33].
Similarly, in a 12-week, double-blind, randomized, placebo-controlled study, autistic children (N = 33) were initiated 900 mg oral NAC daily for 4 weeks, then 900 mg twice daily for 4 weeks and 900 mg three times daily for 4 weeks. Significant improvements on the Aberrant Behavior Checklist irritability subscale, Repetitive Behavior Scale-Revised stereotypies measure, and Social Responsiveness Scale mannerisms scores. While no significant improvement in other subscales were reported [178]. Another 12-week randomized, double-blind, placebo-controlled trial of oral NAC with the target dose of 60 mg/kg/day in three divided doses in ASD youth (N = 31) found no statistically significant difference in Clinical Global Impression—Improvement scale but the GSH level in blood was significantly higher in the NAC group (p < 0.05). However, no significant difference in the GSH/GSSG ratio was observed [30].
Amyotrophic Lateral Sclerosis
ALS is a fatal motor neuron disorder characterized by progressive loss of the upper and lower motor neurons at the spinal or bulbar level [212]. Impairment of the antioxidant defense system could be the potential reason for the etiology, supported by the studies of the lowered activity of enzymes like GPx in blood and CSF of ALS patients [203]. Due to the reported observations of the lowering of antioxidant enzymes, GSH supplementation could be beneficial for the treatment of disease. A pilot trial of reduced GSH was conducted in 32 ALS patients for 6 months, where 600 mg dose of GSH was provided intramuscularly each day. No significant difference was observed between the treated ALS and control groups after GSH treatment [35].
Similar to GSH, a randomized, double-blind, placebo-controlled clinical trial to assess the effect of treatment with NAC was also conducted in ALS patients. A dose of 50 mg/kg per day subcutaneously for 12 months was provided and observed that NAC did not result in a major increase in 12-month survival or a reduction in disease progression [41].
Conclusion
GSH being a master antioxidant displays a remarkable metabolic and regulatory versatility. GSH plays a crucial role in various cellular processes including cell signaling, balance of thiol redox status and detoxification of xenobiotic. Moreover, studies so far elucidate the fact that dysregulation of GSH homeostasis due to increased OS, is involved in various neurological disorders like AD, PD, MS, autism, and ALS, etc. In this review article, we have addressed how GSH acts as a master antioxidant by casing all aspects like function, metabolism, compartmentalization, transport, and synthesis of tripeptide inside the cellular system. We also discussed GSH in vivo detection using advanced spectroscopy techniques. Delineating the therapeutic effectiveness of GSH and NAC as a supplement through various clinical trials will augment the understanding of the treatment of various neurological diseases. Upcoming GSH supplementation studies will be an important step towards clinical neuroscience research which in turn will be beneficial for a wide range of patients suffering from neurological illnesses.
Future Perspectives
GSH is a master antioxidant as it has a beneficial impact on substantially all organs of the living body including the brain. To the best of our knowledge, no phase III randomized controlled trial is existing for MCI or AD patients, wherein brain GSH level is monitored non-invasively with the GSH supplementation. Recent mouse model studies have concluded that behavioral deficits including cognitive decline, depressive-like behaviors, and anxiety-related behaviors observed in APP (NL−G-F/NL−G-FG-) mice were significantly improved by oral GSH administration [213]. This study has validated our ongoing work [14, 20, 21] and hypothesis that oral GSH supplementation [204] will like to have huge impact for possible cognitive improvement in MCI and AD patients subject to verification through an urgent clinical trail.
References
Townsend DM, Tew KD, Tapiero H (2003) The importance of glutathione in human disease. Biomed Pharm 57:145–155
Mailloux RJ, McBride SL, Harper M-E (2013) Unearthing the secrets of mitochondrial ROS and glutathione in bioenergetics. Trends Biochem Sci 38:592–602
Keszler A, Zhang Y, Hogg N (2010) Reaction between nitric oxide, glutathione, and oxygen in the presence and absence of protein: how are S-nitrosothiols formed? Free Radic Biol Med 48:55–64
Lu SC (2013) Glutathione synthesis. Biochem Biophys Acta 1830:3143–3153
Shen D, Dalton TP, Nebert DW, Shertzer HG (2005) Glutathione redox state regulates mitochondrial reactive oxygen production. J Biol Chem 280:25305–25312
Knollema S, Hom HW, Schirmer H, Korf J, Ter Horst GJ (1996) Immunolocalization of glutathione reductase in the murine brain. J Comp Neurol 373:157–172
Lubos E, Loscalzo J, Handy DE (2011) Glutathione peroxidase-1 in health and disease: from molecular mechanisms to therapeutic opportunities. Antioxid Redox Signal 15:1957–1997
Dringen R, Gutterer JM, Hirrlinger J (2000) Glutathione metabolism in brain metabolic interaction between astrocytes and neurons in the defense against reactive oxygen species. Eur J Biochem 267:4912–4916
Franco R, Schoneveld OJ, Pappa A, Panayiotidis MI (2007) The central role of glutathione in the pathophysiology of human diseases. Arch Physiol Biochem 113:234–258
Ghezzi P (2005) Regulation of protein function by glutathionylation. Free Radic Res 39:573–580
Clark DD, Sokoloff L (1999) Circulation and energy metabolism of the brain. Lippincott, Philadelphia
Choi I-Y, Lee S, Denney DR, Lynch SG (2011) Lower levels of glutathione in the brains of secondary progressive multiple sclerosis patients measured by 1H magnetic resonance chemical shift imaging at 3 T. Multiple Scler J 17:289–296
Lovell MA, Ehmann WD, Butler SM, Markesbery WR (1995) Elevated thiobarbituric acid-reactive substances and antioxidant enzyme activity in the brain in Alzheimer's disease. Neurology 45:1594–1601
Mandal PK, Saharan S, Tripathi M, Murari G (2015) Brain glutathione levels—a novel biomarker for mild cognitive impairment and Alzheimer’s disease. Biol Psychiatry 78:702–710
Pearce R, Owen A, Daniel S, Jenner P, Marsden C (1997) Alterations in the distribution of glutathione in the substantia nigra in Parkinson's disease. J Neural Transm 104:661–677
Saharan S, Mandal PK (2014) The emerging role of glutathione in Alzheimer's disease. J Alzheimer's Dis 40:519–529
Gu M, Owen AD, Toffa SE, Cooper JM, Dexter DT, Jenner P, Marsden CD, Schapira AH (1998) Mitochondrial function, GSH and iron in neurodegeneration and Lewy body diseases. J Neurol Sci 158:24–29
Ansari MA, Scheff SW (2010) Oxidative stress in the progression of Alzheimer disease in the frontal cortex. J Neuropathol Exp Neurol 69:155–167
Sultana R, Piroddi M, Galli F, Butterfield DA (2008) Protein levels and activity of some antioxidant enzymes in hippocampus of subjects with amnestic mild cognitive impairment. Neurochem Res 33:2540–2546
Mandal PK, Tripathi M, Sugunan S (2012) Brain oxidative stress: detection and mapping of anti-oxidant marker 'Glutathione' in different brain regions of healthy male/female, MCI and Alzheimer patients using non-invasive magnetic resonance spectroscopy. Biochem Biophys Res Commun 417:43–48
Shukla D, Mandal PK, Tripathi M, Vishwakarma G, Mishra R, Sandal K (2020) Quantitation of in vivo brain glutathione conformers in cingulate cortex among age-matched control, MCI, and AD patients using MEGA-PRESS. Hum Brain Mapp 41:194–217
Mandal PK, Shukla D, Govind V, Boulard Y, Ersland L (2017) Glutathione conformations and its implications for in vivo magnetic resonance spectroscopy. J Alzheimer’s Dis 59:537–541
Shukla D, Mandal PK, Ersland L, Gruner ER, Tripathi M, Raghunathan P, Sharma A, Chaithya GR, Punjabi K, Splaine C (2018) A Multi-center study on human brain glutathione conformation using magnetic resonance spectroscopy. J Alzheimer’s Dis 66:517–532
Matsuzawa D, Obata T, Shirayama Y, Nonaka H, Kanazawa Y, Yoshitome E, Takanashi J, Matsuda T, Shimizu E, Ikehira H, Iyo M, Hashimoto K (2008) Negative correlation between brain glutathione level and negative symptoms in schizophrenia: a 3T 1H-MRS study. PLoS ONE 3:e1944
Srinivasan R, Ratiney H, Hammond-Rosenbluth KE, Pelletier D, Nelson SJ (2010) MR spectroscopic imaging of glutathione in the white and gray matter at 7 T with an application to multiple sclerosis. Magn Reson Imaging 28:163–170
Zhang R, Wu W, Luo S (2011) Different behaviors of glutathione in aqueous and DMSO solutions: molecular dynamics simulation and NMR experimental study. J Solut Chem 40:1784–1795
Richie JP Jr, Nichenametla S, Neidig W, Calcagnotto A, Haley JS, Schell TD, Muscat JE (2015) Randomized controlled trial of oral glutathione supplementation on body stores of glutathione. Eur J Nutr 54:251–263
Schmitt B, Vicenzi M, Garrel C, Denis FM (2015) Effects of N-acetylcysteine, oral glutathione (GSH) and a novel sublingual form of GSH on oxidative stress markers: a comparative crossover study. Redox Biol 6:198–205
Sinha R, Sinha I, Calcagnotto A, Trushin N, Haley JS, Schell TD, Richie JP Jr (2018) Oral supplementation with liposomal glutathione elevates body stores of glutathione and markers of immune function. Eur J Clin Nutr 72:105–111
Wink LK, Adams R, Wang Z, Klaunig JE, Plawecki MH, Posey DJ, McDougle CJ, Erickson CA (2016) A randomized placebo-controlled pilot study of N-acetylcysteine in youth with autism spectrum disorder. Mol Autism 7:26
Mai J, Sorensen PS, Hansen JC (1990) High dose antioxidant supplementation to MS patients. Effects on glutathione peroxidase, clinical safety, and absorption of selenium. Biol Trace Elem Res 24:109–117
Mischley LK, Conley KE, Shankland EG, Kavanagh TJ, Rosenfeld ME, Duda JE, White CC, Wilbur TK, De La Torre PU, Padowski JM (2016) Central nervous system uptake of intranasal glutathione in Parkinson's disease. NPJ Parkinson's Dis 2:16001–16007
Kern JK, Geier DA, Adams JB, Garver CR, Audhya T, Geier MR (2011) A clinical trial of glutathione supplementation in autism spectrum disorders. Med Sci Monit 17:677–682
Remington R, Bechtel C, Larsen D, Samar A, Doshanjh L, Fishman P, Luo Y, Smyers K, Page R, Morrell C, Shea TB (2015) A phase II Randomized clinical trial of a nutritional formulation for cognition and mood in Alzheimer's disease. J Alzheimer’s Dis 45:395–405
Chio A, Cucatto A, Terreni AA, Schiffer D (1998) Reduced glutathione in amyotrophic lateral sclerosis: an open, crossover, randomized trial. Ital J Neurol Sci 19:363–366
Hauser RA, Lyons KE, McClain T, Carter S, Perlmutter D (2009) Randomized, double-blind, pilot evaluation of intravenous glutathione in Parkinson's disease. Mov Disord 24:979–983
Mischley LK, Lau RC, Shankland EG, Wilbur TK, Padowski JM (2017) Phase IIb study of intranasal glutathione in Parkinson's disease. J Parkinson’s Dis 7:289–299
Sechi G, Deledda MG, Bua G, Satta WM, Deiana GA, Pes GM, Rosati G (1996) Reduced intravenous glutathione in the treatment of early Parkinson's disease. Prog Neuropsychopharmacol Biol Psychiatry 20:1159–1170
Holmay MJ, Terpstra M, Coles LD, Mishra U, Ahlskog M, Oz G, Cloyd JC, Tuite PJ (2013) N-Acetylcysteine boosts brain and blood glutathione in Gaucher and Parkinson diseases. Clin Neuropharmacol 36:103–106
Remington R, Lortie JJ, Hoffmann H, Page R, Morrell C, Shea TB (2015) A nutritional formulation for cognitive performance in mild cognitive impairment: a placebo-controlled trial with an open-label extension. J Alzheimer’s Dis 48:591–595
Louwerse ES, Weverling GJ, Bossuyt PM, Meyjes FE, de Jong JM (1995) Randomized, double-blind, controlled trial of acetylcysteine in amyotrophic lateral sclerosis. Arch Neurol 52:559–564
Salamon S, Kramar B, Marolt TP, Poljsak B, Milisav I (2019) Medical and dietary uses of N-acetylcysteine. Antioxidants 8:111
Meister A, Anderson ME (1983) Glutathione. Annu Rev Biochem 52:711–760
Njalsson R, Norgren S, Larsson A, Huang CS, Anderson ME, Luo JL (2001) Cooperative binding of gamma-glutamyl substrate to human glutathione synthetase. Biochem Biophys Res Commun 289:80–84
Lushchak VI (2012) Glutathione homeostasis and functions: potential targets for medical interventions. J Amino Acids 2012:736–837
Bella DL, Hirschberger LL, Kwon YH, Stipanuk MH (2002) Cysteine metabolism in periportal and perivenous hepatocytes: perivenous cells have greater capacity for glutathione production and taurine synthesis but not for cysteine catabolism. Amino Acids 23:453–458
Reid M, Badaloo A, Forrester T, Morlese JF, Frazer M, Heird WC, Jahoor F (2000) In vivo rates of erythrocyte glutathione synthesis in children with severe protein-energy malnutrition. Am J Physiol Endocrinol Metab 278:E405–412
Lyons J, Rauh-Pfeiffer A, Yu YM, Lu XM, Zurakowski D, Tompkins RG, Ajami AM, Young VR, Castillo L (2000) Blood glutathione synthesis rates in healthy adults receiving a sulfur amino acid-free diet. Proc Natl Acad Sci USA 97:5071–5076
Liu H, Wang H, Shenvi S, Hagen TM, Liu RM (2004) Glutathione metabolism during aging and in Alzheimer disease. Ann N Y Acad Sci 1019:346–349
Richman PG, Meister A (1975) Regulation of gamma-glutamyl-cysteine synthetase by nonallosteric feedback inhibition by glutathione. J Biol Chem 250:1422–1426
Huang CS, Moore WR, Meister A (1988) On the active site thiol of gamma-glutamylcysteine synthetase: relationships to catalysis, inhibition, and regulation. Proc Natl Acad Sci USA 85:2464–2468
Bannai S, Tateishi N (1986) Role of membrane transport in metabolism and function of glutathione in mammals. J Membr Biol 89:1–8
Lu SC, Ge JL, Kuhlenkamp J, Kaplowitz N (1992) Insulin and glucocorticoid dependence of hepatic gamma-glutamylcysteine synthetase and glutathione synthesis in the rat. Studies in cultured hepatocytes and in vivo. J Clin Investig 90:524–532
Kilberg MS (1982) Amino acid transport in isolated rat hepatocytes. J Membr Biol 69:1–12
Mulcahy RT, Bailey HH, Gipp JJ (1995) Transfection of complementary DNAs for the heavy and light subunits of human gamma-glutamylcysteine synthetase results in an elevation of intracellular glutathione and resistance to melphalan. Can Res 55:4771–4775
Mulcahy RT, Gipp JJ (1995) Identification of a putative antioxidant response element in the 5'-flanking region of the human gamma-glutamylcysteine synthetase heavy subunit gene. Biochem Biophys Res Commun 209:227–233
Mulcahy RT, Untawale S, Gipp JJ (1994) Transcriptional up-regulation of gamma-glutamylcysteine synthetase gene expression in melphalan-resistant human prostate carcinoma cells. Mol Pharmacol 46:909–914
Kim SK, Woodcroft KJ, Khodadadeh SS, Novak RF (2004) Insulin signaling regulates gamma-glutamylcysteine ligase catalytic subunit expression in primary cultured rat hepatocytes. J Pharmacol Exp Ther 311:99–108
Clancy RM, Levartovsky D, Leszczynska-Piziak J, Yegudin J, Abramson SB (1994) Nitric oxide reacts with intracellular glutathione and activates the hexose monophosphate shunt in human neutrophils: evidence for S-nitrosoglutathione as a bioactive intermediary. Proc Natl Acad Sci USA 91:3680–3684
Lobo V, Patil A, Phatak A, Chandra N (2010) Free radicals, antioxidants and functional foods: impact on human health. Pharmacogn Rev 4:118–126
Singh SP, Wishnok JS, Keshive M, Deen WM, Tannenbaum SR (1996) The chemistry of the S-nitrosoglutathione/glutathione system. Proc Natl Acad Sci USA 93:14428–14433
Winterbourn CC, Metodiewa D (1994) The reaction of superoxide with reduced glutathione. Arch Biochem Biophys 314:284–290
Chance B, Sies H, Boveris A (1979) Hydroperoxide metabolism in mammalian organs. Physiol Rev 59:527–605
Ng CF, Schafer FQ, Buettner GR, Rodgers VG (2007) The rate of cellular hydrogen peroxide removal shows dependency on GSH: mathematical insight into in vivo H2O2 and GPx concentrations. Free Radic Res 41:1201–1211
Ursini F, Maiorino M, Brigelius-Flohe R, Aumann KD, Roveri A, Schomburg D, Flohe L (1995) Diversity of glutathione peroxidases. Methods Enzymol 252:38–53
Ulusu NN, Tandogan B (2007) Purification and kinetic properties of glutathione reductase from bovine liver. Mol Cell Biochem 303:45–51
Dasuri K, Zhang L, Keller JN (2013) Oxidative stress, neurodegeneration, and the balance of protein degradation and protein synthesis. Free Radic Biol Med 62:170–185
Fukai T, Ushio-Fukai M (2011) Superoxide dismutases: role in redox signaling, vascular function, and diseases. Antioxid Redox Signal 15:1583–1606
Ray PD, Huang B-W, Tsuji Y (2012) Reactive oxygen species (ROS) homeostasis and redox regulation in cellular signaling. Cell Signal 24:981–990
Finkel T (2003) Oxidant signals and oxidative stress. Curr Opin Cell Biol 15:247–254
Smythies J (1999) The neurotoxicity of glutamate, dopamine, iron and reactive oxygen species: functional interrelationships in health and disease: a review—discussion. Neurotox Res 1:27–39
Stone JR, Yang S (2006) Hydrogen peroxide: a signaling messenger. Antioxid Redox Signal 8:243–270
Wang X, Wang W, Li L, Perry G, Lee H-G, Zhu X (2014) Oxidative stress and mitochondrial dysfunction in Alzheimer's disease. Biochimica et Biophysica Acta (BBA) 1842:1240–1247
Wong HS, Dighe PA, Mezera V, Monternier PA, Brand MD (2017) Production of superoxide and hydrogen peroxide from specific mitochondrial sites under different bioenergetic conditions. J Biol Chem 292:16804–16809
Zorov DB, Filburn CR, Klotz LO, Zweier JL, Sollott SJ (2000) Reactive oxygen species (ROS)-induced ROS release: a new phenomenon accompanying induction of the mitochondrial permeability transition in cardiac myocytes. J Exp Med 192:1001–1014
Kehrer JP (2000) The Haber-Weiss reaction and mechanisms of toxicity. Toxicology 149:43–50
Thomas C, Mackey MM, Diaz AA, Cox DP (2009) Hydroxyl radical is produced via the Fenton reaction in submitochondrial particles under oxidative stress: implications for diseases associated with iron accumulation. Redox Rep 14:102–108
Sazanov LA (2007) Respiratory complex I: mechanistic and structural insights provided by the crystal structure of the hydrophilic domain. Biochemistry 46:2275–2288
Hirst J, Carroll J, Fearnley IM, Shannon RJ, Walker JE (2003) The nuclear encoded subunits of complex I from bovine heart mitochondria. Biochem Biophys Acta 1604:135–150
Sawyer DT, Valentine JS (1981) How super is superoxide? Acc Chem Res 14:393–400
Brand MD, Affourtit C, Esteves TC, Green K, Lambert AJ, Miwa S, Pakay JL, Parker N (2004) Mitochondrial superoxide: production, biological effects, and activation of uncoupling proteins. Free Radic Biol Med 37:755–767
Hirst J, King MS, Pryde KR (2008) The production of reactive oxygen species by complex I. Biochem Soc Trans 36:976–980
Andreyev AY, Kushnareva YE, Starkov AA (2005) Mitochondrial metabolism of reactive oxygen species. Biochem Biokhimiia 70:200–214
Adam-Vizi V, Chinopoulos C (2006) Bioenergetics and the formation of mitochondrial reactive oxygen species. Trends Pharmacol Sci 27:639–645
Chance B, Hollunger G (1961) The interaction of energy and electron transfer reactions in mitochondria. I. General properties and nature of the products of succinate-linked reduction of pyridine nucleotide. J Biol Chem 236:1534–1543
Turrens JF, Alexandre A, Lehninger AL (1985) Ubisemiquinone is the electron donor for superoxide formation by complex III of heart mitochondria. Arch Biochem Biophys 237:408–414
Cadenas E, Boveris A, Ragan CI, Stoppani AO (1977) Production of superoxide radicals and hydrogen peroxide by NADH-ubiquinone reductase and ubiquinol-cytochrome c reductase from beef-heart mitochondria. Arch Biochem Biophys 180:248–257
Murphy MP (2009) How mitochondria produce reactive oxygen species. Biochem J 417:1–13
Ramsay RR (2019) Electron carriers and energy conservation in mitochondrial respiration. ChemTexts 5:9
Bai J, Cederbaum AI (2001) Mitochondrial catalase and oxidative injury. Biol Signals Recept 10:189–199
Nandi A, Yan LJ, Jana CK, Das N (2019) Role of catalase in oxidative stress- and age-associated degenerative diseases. Oxid Med Cell Longev 2019:9613090
Szarka A, Tomasskovics B, Banhegyi G (2012) The ascorbate-glutathione-alpha-tocopherol triad in abiotic stress response. Int J Mol Sci 13:4458–4483
National Center for Biotechnology Information (2020) PubChem Database. Glutathione, CID=124886, https://pubchem.ncbi.nlm.nih.gov/compound/Glutathione. Accessed 12 Feb 2020
Ribas V, Garcia-Ruiz C, Fernandez-Checa JC (2014) Glutathione and mitochondria. Front Pharmacol 5:151
Stamler JS, Simon DI, Osborne JA, Mullins ME, Jaraki O, Michel T, Singel DJ, Loscalzo J (1992) S-nitrosylation of proteins with nitric oxide: synthesis and characterization of biologically active compounds. Proc Natl Acad Sci 89:444–448
Kolesnik B, Palten K, Schrammel A, Stessel H, Schmidt K, Mayer B, Gorren AC (2013) Efficient nitrosation of glutathione by nitric oxide. Free Radic Biol Med 63:51–64
Schrammel A, Gorren AC, Schmidt K, Pfeiffer S, Mayer B (2003) S-nitrosation of glutathione by nitric oxide, peroxynitrite, and (*)NO/O(2)(*-). Free Radic Biol Med 34:1078–1088
Chatterjee A (2013) Reduced glutathione: a radioprotector or a modulator of DNA-repair activity? Nutrients 5:525–542
Gaschler MM, Stockwell BR (2017) Lipid peroxidation in cell death. Biochem Biophys Res Commun 482:419–425
Wu G, Fang YZ, Yang S, Lupton JR, Turner ND (2004) Glutathione metabolism and its implications for health. J Nutr 134:489–492
Ferrari CK (2012) Effects of xenobiotics on total antioxidant capacity. Interdiscip Toxicol 5:117–122
Tonelli C, Chio IIC, Tuveson DA (2018) Transcriptional regulation by Nrf2. Antioxid Redox Signal 29:1727–1745
Liochev SI (1999) The mechanism of "Fenton-like" reactions and their importance for biological systems. A biologist's view. Met Ions Biol Syst 36:1–39
Stohs SJ, Bagchi D (1995) Oxidative mechanisms in the toxicity of metal ions. Free Radic Biol Med 18:321–336
Ercal N, Gurer-Orhan H, Aykin-Burns N (2001) Toxic metals and oxidative stress part I: mechanisms involved in metal-induced oxidative damage. Curr Top Med Chem 1:529–539
Valko M, Morris H, Cronin M (2005) Metals, toxicity and oxidative stress. Curr Med Chem 12:1161–1208
Arslan A, Tüzün FA, Tamer S, Demir H, Aycan A, Demir C, Tasin M, Gönüllü E (2016) Change of antioxidant enzyme activities, some metals and lipid peroxidation in Alzheimer’s disease. Acta MedicaMediterranea 32:1643–1649
Bush AI, Tanzi RE (2008) Therapeutics for Alzheimer's disease based on the metal hypothesis. Neurotherapeutics 5:421–432
Wang W, Ballatori N (1998) Endogenous glutathione conjugates: occurrence and biological functions. Pharmacol Rev 50:335–356
Sipos K, Lange H, Fekete Z, Ullmann P, Lill R, Kispal G (2002) Maturation of cytosolic iron-sulfur proteins requires glutathione. J Biol Chem 277:26944–26949
Couturier J, Przybyla-Toscano J, Roret T, Didierjean C, Rouhier N (2015) The roles of glutaredoxins ligating Fe-S clusters: sensing, transfer or repair functions? Biochem Biophys Acta 1853:1513–1527
Qi W, Li J, Chain CY, Pasquevich GA, Pasquevich AF, Cowan JA (2013) Glutathione-complexed iron-sulfur clusters. Reaction intermediates and evidence for a template effect promoting assembly and stability. Chem Commun 49:6313–6315
Aguilera G, Colin-Gonzalez AL, Rangel-Lopez E, Chavarria A, Santamaria A (2018) Redox signaling, neuroinflammation, and neurodegeneration. Antioxid Redox Signal 28:1626–1651
Diaz-Hung ML, Yglesias-Rivera A, Hernandez-Zimbron LF, Orozco-Suarez S, Ruiz-Fuentes JL, Diaz-Garcia A, Leon-Martinez R, Blanco-Lezcano L, Pavon-Fuentes N, Lorigados-Pedre L (2016) Transient glutathione depletion in the substantia nigra compacta is associated with neuroinflammation in rats. Neuroscience 335:207–220
Mosley RL, Benner EJ, Kadiu I, Thomas M, Boska MD, Hasan K, Laurie C, Gendelman HE (2006) Neuroinflammation, oxidative stress and the pathogenesis of Parkinson’s disease. Clin Neurosci Res 6:261–281
Lee M, Cho T, Jantaratnotai N, Wang YT, McGeer E, McGeer PL (2010) Depletion of GSH in glial cells induces neurotoxicity: relevance to aging and degenerative neurological diseases. FASEB J 24:2533–2545
Jones DP (2006) Redefining oxidative stress. Antioxid Redox Signal 8:1865–1879
Schafer FQ, Buettner GR (2001) Redox environment of the cell as viewed through the redox state of the glutathione disulfide/glutathione couple. Free Radic Biol Med 30:1191–1212
Desideri E, Filomeni G, Ciriolo MR (2012) Glutathione participates in the modulation of starvation-induced autophagy in carcinoma cells. Autophagy 8:1769–1781
Cardaci S, Filomeni G, Rotilio G, Ciriolo MR (2010) p38(MAPK)/p53 signalling axis mediates neuronal apoptosis in response to tetrahydrobiopterin-induced oxidative stress and glucose uptake inhibition: implication for neurodegeneration. Biochem J 430:439–451
Lewerenz J, Ates G, Methner A, Conrad M, Maher P (2018) Oxytosis/ferroptosis-(Re-) emerging roles for oxidative stress-dependent non-apoptotic cell death in diseases of the central nervous system. Front Neurosci 12:214
Friedmann Angeli JP, Schneider M, Proneth B, Tyurina YY, Tyurin VA, Hammond VJ, Herbach N, Aichler M, Walch A, Eggenhofer E, Basavarajappa D, Radmark O, Kobayashi S, Seibt T, Beck H, Neff F, Esposito I, Wanke R, Forster H, Yefremova O, Heinrichmeyer M, Bornkamm GW, Geissler EK, Thomas SB, Stockwell BR, O'Donnell VB, Kagan VE, Schick JA, Conrad M (2014) Inactivation of the ferroptosis regulator Gpx4 triggers acute renal failure in mice. Nat Cell Biol 16:1180–1191
Dixon SJ, Stockwell BR (2014) The role of iron and reactive oxygen species in cell death. Nat Chem Biol 10:9–17
Hwang C, Sinskey AJ, Lodish HF (1992) Oxidized redox state of glutathione in the endoplasmic reticulum. Science 257:1496–1502
Holmgren A, Sengupta R (2010) The use of thiols by ribonucleotide reductase. Free Radic Biol Med 49:1617–1628
Cooper AJL, Pulsinelli WA, Duffy TE (1980) Glutathione and ascorbate during ischemia and postischemic reperfusion in rat brain. J Neurochemistry 35:1242–1245
Kumar C, Igbaria A, D'Autreaux B, Planson AG, Junot C, Godat E, Bachhawat AK, Delaunay-Moisan A, Toledano MB (2011) Glutathione revisited: a vital function in iron metabolism and ancillary role in thiol-redox control. EMBO J 30:2044–2056
Mari M, Morales A, Colell A, Garcia-Ruiz C, Kaplowitz N, Fernandez-Checa JC (2013) Mitochondrial glutathione: features, regulation and role in disease. Biochem Biophys Acta 1830:3317–3328
Schulz JB, Lindenau J, Seyfried J, Dichgans J (2000) Glutathione, oxidative stress and neurodegeneration. Eur J Biochem 267:4904–4911
Krahenbuhl S, Krahenbuhl-Glauser S, Stucki J, Gehr P, Reichen J (1992) Stereological and functional analysis of liver mitochondria from rats with secondary biliary cirrhosis: impaired mitochondrial metabolism and increased mitochondrial content per hepatocyte. Hepatology 15:1167–1172
Purucker E, Winograd R, Roeb E, Matern S (1998) Glutathione status in liver and plasma during development of biliary cirrhosis after bile duct ligation. Res Exp Med 198:167–174
Meister A, Tate SS (1976) Glutathione and related gamma-glutamyl compounds: biosynthesis and utilization. Annu Rev Biochem 45:559–604
Bartoli GM, Sies H (1978) Reduced and oxidized glutathione efflux from liver. FEBS Lett 86:89–91
Anderson ME, Meister A (1980) Dynamic state of glutathione in blood plasma. J Biol Chem 255:9530–9533
Griffith OW, Meister A (1979) Glutathione: interorgan translocation, turnover, and metabolism. Proc Natl Acad Sci USA 76:5606–5610
Inoue M (2016) Glutathionists in the battlefield of gamma-glutamyl cycle. Arch Biochem Biophys 595:61–63
Kannan R, Chakrabarti R, Tang D, Kim KJ, Kaplowitz N (2000) GSH transport in human cerebrovascular endothelial cells and human astrocytes: evidence for luminal localization of Na+-dependent GSH transport in HCEC. Brain Res 852:374–382
Lash LH (2005) Role of glutathione transport processes in kidney function. Toxicol Appl Pharmacol 204:329–342
Sun X, Shih AY, Johannssen HC, Erb H, Li P, Murphy TH (2006) Two-photon imaging of glutathione levels in intact brain indicates enhanced redox buffering in developing neurons and cells at the cerebrospinal fluid and blood-brain interface. J Biol Chem 281:17420–17431
Michelet F, Gueguen R, Leroy P, Wellman M, Nicolas A, Siest G (1995) Blood and plasma glutathione measured in healthy subjects by HPLC: relation to sex, aging, biological variables, and life habits. Clin Chem 41:1509–1517
Richie JP Jr, Skowronski L, Abraham P, Leutzinger Y (1996) Blood glutathione concentrations in a large-scale human study. Clin Chem 42:64–70
Cantin AM, North SL, Hubbard RC, Crystal RG (1987) Normal alveolar epithelial lining fluid contains high levels of glutathione. J Appl Physiol 63:152–157
Huang J, Philbert MA (1995) Distribution of glutathione and glutathione-related enzyme systems in mitochondria and cytosol of cultured cerebellar astrocytes and granule cells. Brain Res 680:16–22
Langeveld CH, Schepens E, Jongenelen CA, Stoof JC, Hjelle OP, Ottersen OP, Drukarch B (1996) Presence of glutathione immunoreactivity in cultured neurones and astrocytes. NeuroReport 7:1833–1836
Raps SP, Lai JC, Hertz L, Cooper AJ (1989) Glutathione is present in high concentrations in cultured astrocytes but not in cultured neurons. Brain Res 493:398–401
Rice ME, Russo-Menna I (1998) Differential compartmentalization of brain ascorbate and glutathione between neurons and glia. Neuroscience 82:1213–1223
Dringen R, Kranich O, Hamprecht B (1997) The γ-glutamyl transpeptidase inhibitor acivicin preserves glutathione released by astroglial cells in culture. Neurochem Res 22:727–733
Li X, Wallin C, Weber SG, Sandberg M (1999) Net efflux of cysteine, glutathione and related metabolites from rat hippocampal slices during oxygen/glucose deprivation: dependence on gamma-glutamyl transpeptidase. Brain Res 815:81–88
Rae CD, Williams SR (2017) Glutathione in the human brain: review of its roles and measurement by magnetic resonance spectroscopy. Anal Biochem 529:127–143
Aoyama K, Nakaki T (2013) Neuroprotective properties of the excitatory amino acid carrier 1 (EAAC1). Amino Acids 45:133–142
Aoyama K, Suh SW, Hamby AM, Liu J, Chan WY, Chen Y, Swanson RA (2006) Neuronal glutathione deficiency and age-dependent neurodegeneration in the EAAC1 deficient mouse. Nat Neurosci 9:119–126
Shashidharan P, Huntley GW, Murray JM, Buku A, Moran T, Walsh MJ, Morrison JH, Plaitakis A (1997) Immunohistochemical localization of the neuron-specific glutamate transporter EAAC1 (EAAT3) in rat brain and spinal cord revealed by a novel monoclonal antibody. Brain Res 773:139–148
Allaman I, Belanger M, Magistretti PJ (2011) Astrocyte-neuron metabolic relationships: for better and for worse. Trends Neurosci 34:76–87
Bradaia A, Schlichter R, Trouslard J (2004) Role of glial and neuronal glycine transporters in the control of glycinergic and glutamatergic synaptic transmission in lamina X of the rat spinal cord. J Physiol 559:169–186
Aoyama K, Watabe M, Nakaki T (2008) Regulation of neuronal glutathione synthesis. J Pharmacol Sci 108:227–238
Massucci FA, DiNuzzo M, Giove F, Maraviglia B, Castillo IP, Marinari E, De Martino A (2013) Energy metabolism and glutamate-glutamine cycle in the brain: a stoichiometric modeling perspective. BMC Syst Biol 7:103
Liu B, Teschemacher AG, Kasparov S (2017) Astroglia as a cellular target for neuroprotection and treatment of neuro-psychiatric disorders. Glia 65:1205–1226
Abbott NJ, Romero IA (1996) Transporting therapeutics across the blood-brain barrier. Mol Med Today 2:106–113
Abbott NJ, Ronnback L, Hansson E (2006) Astrocyte-endothelial interactions at the blood-brain barrier. Nat Rev Neurosci 7:41–53
Goti D, Hrzenjak A, Levak-Frank S, Frank S, van der Westhuyzen DR, Malle E, Sattler W (2001) Scavenger receptor class B, type I is expressed in porcine brain capillary endothelial cells and contributes to selective uptake of HDL-associated vitamin E. J Neurochem 76:498–508
Chen Y, Liu L (2012) Modern methods for delivery of drugs across the blood-brain barrier. Adv Drug Deliv Rev 64:640–665
Kannan R, Kuhlenkamp JF, Ookhtens M, Kaplowitz N (1992) Transport of glutathione at blood-brain barrier of the rat: inhibition by glutathione analogs and age-dependence. J Pharmacol Exp Ther 263:964–970
Kannan R, Mittur A, Bao Y, Tsuruo T, Kaplowitz N (1999) GSH transport in immortalized mouse brain endothelial cells: evidence for apical localization of a sodium-dependent GSH transporter. J Neurochem 73:390–399
Kannan R, Yi JR, Tang D, Li Y, Zlokovic BV, Kaplowitz N (1996) Evidence for the existence of a sodium-dependent glutathione (GSH) transporter. Expression of bovine brain capillary mRNA and size fractions in Xenopus laevis oocytes and dissociation from gamma-glutamyltranspeptidase and facilitative GSH transporters. J Biol Chem 271:9754–9758
Mandal PK, Shukla D (2020) KALPANA: advanced spectroscopic signal processing platform for improved accuracy to aid in early diagnosis of brain disorders in clinical setting. J Alzheimer’s Dis 75:22–28
Delalande O, Desvaux H, Godat E, Valleix A, Junot C, Labarre J, Boulard Y (2010) Cadmium-glutathione solution structures provide new insights into heavy metal detoxification. FEBS J 277:5086–5096
Mandal PK, Ersland L (2019) Editorial: Predictive imagable biomarkers for neurodegenerative and neurodevelopmental diseases. Front Neurol 10:583
Perry TL, Berry K, Hansen S, Diamond S, Mok C (1971) Regional distribution of amino acids in human brain obtained at autopsy. J Neurochem 18:513–519
Calabrese V, Scapagnini G, Ravagna A, Fariello RG, Giuffrida Stella AM, Abraham NG (2002) Regional distribution of heme oxygenase, HSP70, and glutathione in brain: relevance for endogenous oxidant/antioxidant balance and stress tolerance. J Neurosci Res 68:65–75
Gawryluk JW, Wang JF, Andreazza AC, Shao L, Young LT (2011) Decreased levels of glutathione, the major brain antioxidant, in post-mortem prefrontal cortex from patients with psychiatric disorders. Int J Neuropsychopharmacol 14:123–130
Harrison FE, Hosseini AH, Dawes SM, Weaver S, May JM (2009) Ascorbic acid attenuates scopolamine-induced spatial learning deficits in the water maze. Behav Brain Res 205:550–558
Rahman I, Kode A, Biswas SK (2006) Assay for quantitative determination of glutathione and glutathione disulfide levels using enzymatic recycling method. Nat Protoc 1:3159–3165
Tumati S, Opmeer EM, Marsman JC, Martens S, Reesink FE, De Deyn PP, Aleman A (2018) Lower choline and myo-inositol in temporo-parietal cortex is associated with apathy in amnestic MCI. Front Aging Neurosci 10:106
Frantseva MV, Velazquez JL, Hwang PA, Carlen PL (2000) Free radical production correlates with cell death in an in vitro model of epilepsy. Eur J Neurosci 12:1431–1439
Mueller SG, Trabesinger AH, Boesiger P, Wieser HG (2001) Brain glutathione levels in patients with epilepsy measured by in vivo (1)H-MRS. Neurology 57:1422–1427
Arlt S, Muller-Thomsen T, Beisiegel U, Kontush A (2012) Effect of one-year vitamin C- and E-supplementation on cerebrospinal fluid oxidation parameters and clinical course in Alzheimer's disease. Neurochem Res 37:2706–2714
Galasko DR, Peskind E, Clark CM, Quinn JF, Ringman JM, Jicha GA, Cotman C, Cottrell B, Montine TJ, Thomas RG, Aisen P, Alzheimer's Disease Cooperative S (2012) Antioxidants for Alzheimer disease: a randomized clinical trial with cerebrospinal fluid biomarker measures. Arch Neurol 69:836–841
Hardan AY, Fung LK, Libove RA, Obukhanych TV, Nair S, Herzenberg LA, Frazier TW, Tirouvanziam R (2012) A randomized controlled pilot trial of oral N-acetylcysteine in children with autism. Biol Psychiatry 71:956–961
Adair JC, Knoefel JE, Morgan N (2001) Controlled trial of N-acetylcysteine for patients with probable Alzheimer's disease. Neurology 57:1515–1517
Coles LD, Tuite PJ, Oz G, Mishra UR, Kartha RV, Sullivan KM, Cloyd JC, Terpstra M (2018) Repeated-dose oral N-acetylcysteine in Parkinson's disease: pharmacokinetics and effect on brain glutathione and oxidative stress. J Clin Pharmacol 58:158–167
Allen J, Bradley RD (2011) Effects of oral glutathione supplementation on systemic oxidative stress biomarkers in human volunteers. J Altern Complement Med 17:827–833
Farr SA, Poon HF, Dogrukol-Ak D, Drake J, Banks WA, Eyerman E, Butterfield DA, Morley JE (2003) The antioxidants alpha-lipoic acid and N-acetylcysteine reverse memory impairment and brain oxidative stress in aged SAMP8 mice. J Neurochem 84:1173–1183
Anderson ME, Luo JL (1998) Glutathione therapy: from prodrugs to genes. Semin Liver Dis 18:415–424
Atkuri KR, Mantovani JJ, Herzenberg LA, Herzenberg LA (2007) N-Acetylcysteine—a safe antidote for cysteine/glutathione deficiency. Curr Opin Pharmacol 7:355–359
Mokhtari V, Afsharian P, Shahhoseini M, Kalantar SM, Moini A (2017) A review on various uses of N-acetyl cysteine. Cell J 19:11–17
Bains JS, Shaw CA (1997) Neurodegenerative disorders in humans: the role of glutathione in oxidative stress-mediated neuronal death. Brain Res Brain Res Rev 25:335–358
Huang WJ, Zhang X, Chen WW (2016) Role of oxidative stress in Alzheimer's disease. Biomed Rep 4:519–522
Honda Y, Kessoku T, Sumida Y, Kobayashi T, Kato T, Ogawa Y, Tomeno W, Imajo K, Fujita K, Yoneda M, Kataoka K, Taguri M, Yamanaka T, Seko Y, Tanaka S, Saito S, Ono M, Oeda S, Eguchi Y, Aoi W, Sato K, Itoh Y, Nakajima A (2017) Efficacy of glutathione for the treatment of nonalcoholic fatty liver disease: an open-label, single-arm, multicenter, pilot study. BMC Gastroenterol 17:96
Kovacs-Nolan J, Rupa P, Matsui T, Tanaka M, Konishi T, Sauchi Y, Sato K, Ono S, Mine Y (2014) In vitro and ex vivo uptake of glutathione (GSH) across the intestinal epithelium and fate of oral GSH after in vivo supplementation. J Agric Food Chem 62:9499–9506
Weschawalit S, Thongthip S, Phutrakool P, Asawanonda P (2017) Glutathione and its antiaging and antimelanogenic effects. Clin Cosmet Investig Dermatol 10:147–153
Arjinpathana N, Asawanonda P (2012) Glutathione as an oral whitening agent: a randomized, double-blind, placebo-controlled study. J Dermatol Treat 23:97–102
Cleary M (1991) Peripheral intravenous cannulation. Aust Fam Phys 20:1285–1288
Djupesland PG, Messina JC, Mahmoud RA (2014) The nasal approach to delivering treatment for brain diseases: an anatomic, physiologic, and delivery technology overview. Ther Deliv 5:709–733
Illum L (2004) Is nose-to-brain transport of drugs in man a reality? J Pharm Pharmacol 56:3–17
Narang N, Sharma J (2011) Sublingual mucosa as a route for systemic drug delivery. Int J Pharm Pharm Sci 3:18–22
Cocoman A, Murray J (2008) Intramuscular injections: a review of best practice for mental health nurses. J Psychiatr Ment Health Nurs 15:424–434
Tardiolo G, Bramanti P, Mazzon E (2018) Overview on the effects of N-Acetylcysteine in neurodegenerative diseases. Molecules 23:3305
Marcus DL, Thomas C, Rodriguez C, Simberkoff K, Tsai JS, Strafaci JA, Freedman ML (1998) Increased peroxidation and reduced antioxidant enzyme activity in Alzheimer's disease. Exp Neurol 150:40–44
Sofic E, Lange KW, Jellinger K, Riederer P (1992) Reduced and oxidized glutathione in the substantia nigra of patients with Parkinson's disease. Neurosci Lett 142:128–130
Jensen GE, Clausen J (1984) Glutathione peroxidase and reductase, glucose-6-phosphate dehydrogenase and catalase activities in multiple sclerosis. J Neurol Sci 63:45–53
Jensen GE, Clausen J (1986) Glutathione peroxidase activity, associated enzymes and substrates in blood cells from patients with multiple sclerosis—effects of antioxidant supplementation. Acta Pharmacol Toxicol 59(Suppl 7):450–453
James SJ, Cutler P, Melnyk S, Jernigan S, Janak L, Gaylor DW, Neubrander JA (2004) Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. Am J Clin Nutr 80:1611–1617
Moumen R, Nouvelot A, Duval D, Lechevalier B, Viader F (1997) Plasma superoxide dismutase and glutathione peroxidase activity in sporadic amyotrophic lateral sclerosis. J Neurol Sci 151:35–39
Mandal PK, Shukla D, Tripathi M, Ersland L (2019) Cognitive Improvement with glutathione supplement in Alzheimer's disease: a way forward. J Alzheimer’s Dis 68:531–535
Pocernich CB, Butterfield DA (2012) Elevation of glutathione as a therapeutic strategy in Alzheimer disease. Biochem Biophys Acta 1822:625–630
Schachter AS, Davis KL (2000) Alzheimer's disease. Dialogues Clin Neurosci 2:91–100
DeMaagd G, Philip A (2015) Parkinson's disease and Its management: part 1: disease entity, risk factors, pathophysiology, clinical presentation, and diagnosis. P & T 40:504–532
Hwang O (2013) Role of oxidative stress in Parkinson's disease. Exp Neurobiol 22:11–17
Markesbery WR (1997) Oxidative stress hypothesis in Alzheimer's disease. Free Radic Biol Med 23:134–147
Calabresi PA (2004) Diagnosis and management of multiple sclerosis. Am Fam Phys 70:1935–1944
Park HR, Lee JM, Moon HE, Lee DS, Kim BN, Kim J, Kim DG, Paek SH (2016) A Short review on the current understanding of autism spectrum disorders. Exp Neurobiol 25:1–13
Rowland LP, Shneider NA (2001) Amyotrophic lateral sclerosis. N Engl J Med 344:1688–1700
Izumi H, Sato K, Kozima K, Sainto, T, Saido T, Fukunag, K (2020) Oral glutathione administration inhibits the oxidative stress and the inflammatory responses in AppNL−G-F/NL−G-F knock-in mice. Neuropharmacology 168:108026–108036
Acknowledgements
Dr. Pravat Kumar Mandal (Principal Investigator) is thankful to the Department of Biotechnology, Ministry of Science and Technology, Government of India (Award no. BT/PR7361/MED/30/953/2013), Indo-Australia Biotechnology Fund (Grant no. BT/Indo-Aus/10/31/2016) and Ministry of Electronics and Information Technology, Govt. of India (Grant No 4(5)2019 ITEA) for funding this project. Partial financial support from Tata Innovation Fellowship (No. BT/HRD/35/01/05/2014) awarded to Dr. Pravat Kumar Mandal from the Department of Biotechnology, Ministry of Science and Technology, Government of India is highly appreciated. We would also like to thank Dr. Deepika Shukla (Scientist, NINS laboratory) and Ms. Khushboo Punjabi (Ph. D scholar, NINS laboratory) for discussion as well as Ms. Kanika Sandal (R&D Engineer I, NINS laboratory) for her help in arranging the copyright permission from various publishers. Thanks to Ms. Shubhangi Tripathi for proof reading.
Author information
Authors and Affiliations
Contributions
Dr. PKM (Professor) conceptualized the research idea and was involved in writing the manuscript, figure preparation, critically reviewing and finalization of the manuscript. Ms. DD (R&D Engineer), Dr. KM (Research Associate) and Mr. RM (Clinical Coordinator) contributed equally to the literature search, critically reviewing the literature, writing and reviewing the manuscript as well as designing the figures.
Corresponding author
Ethics declarations
Conflict of interest
All the authors agree with the content of the article and declare no conflict of interest (personal, academic or financial) associated with this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dwivedi, D., Megha, K., Mishra, R. et al. Glutathione in Brain: Overview of Its Conformations, Functions, Biochemical Characteristics, Quantitation and Potential Therapeutic Role in Brain Disorders. Neurochem Res 45, 1461–1480 (2020). https://doi.org/10.1007/s11064-020-03030-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-020-03030-1