Abstract
The lectin, concanavalin A (Con A), is the most extensively investigated member of the lectin family of plant proteins, but its effects on cortical neurons and astrocytes are poorly understood. In cultured cortical neurons and astrocytes, Con A exhibited dose-dependent neurotoxicity, but this was not observed in astrocytes. Similarly, in the cortical areas of rat brains, intracranial administration of Con A caused neuronal but no astrocyte damage. Methyl-α-d-mannopyranoside, a competitor of Con A, blocked Con A-induced cell death, whereas AMPA/KA receptor antagonists showed partial blocking effects. Furthermore, the mRNA levels of TNF-α, IL-1β, and IL-6 were elevated in astrocytes and cortical neurons treated with Con A. Intracellular reactive oxygen species (ROS) levels were increased in Con A-treated cortical neurons, and N-acetyl-cysteine (NAC, an antioxidant) and diphenyleneiodonium (DPI, a NADPH oxidase inhibitor) reduced intracellular ROS accumulation. Likewise, AG556 (a TNF-α inhibitor) and AG82 (a tyrosine kinase inhibitor) both reduced Con A-induced intracellular ROS accumulation. Furthermore, Con A-induced tyrosine phosphorylation was decreased by NAC and by AG556. Taken together, Con A-induced apoptosis in cortical neurons occurred as a sequel to Con A binding to neuronal glycoproteins and intracellular ROS accumulation. Interestingly, Con A-induced cellular damage was observed in cortical neurons but not in astrocytes or microglia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many plant lectins are capable of binding to the carbohydrate moieties of complex glycoconjugates without altering the covalent structures of recognized glycosyl ligands [1]. Concanavalin A (Con A) is a lectin that consists of four subunits of protein molecules, which can cross-link cell surface glycoproteins containing α-d-mannopyranosyl or α-d-glucopyranosyl residues [2]. Lectins induce apoptosis in a wide variety of cell types, and experimental studies have shown Con A-induced acute hepatitis in murine models resembles viral or autoimmune hepatitis in man. Con A has also been reported to trigger in vitro cellular processes, such as, cytokine secretion, nitric oxide production, and T-lymphocyte activation [3, 4], and has been used in models of acute liver injury [5, 6]. Con A induces liver injury by activating type 1 and type 2 TNF-α receptors (TNFR), and TNFR2 is important for Con A-induced JNK activation, as mice lacking JNK2 were found to be highly resistant to Con A-induced apoptotic and necrotic cell death in liver [7]. Con A-induced hepatotoxicity is commonly associated with releases of tumor necrosis factor α (TNF-α) and interleukin 1β (IL-1β) and reactive oxygen species (ROS) generation, which ultimately results in cellular apoptosis and autophagy [8].
Con A has been reported to induce membrane type-1 matrix metalloproteinase (MT1-MMP) over-expression in brain cancer via an inhibitory kappa B kinase (IKK)/nuclear factor kappa B (NF-κB)-dependent pathway, and Con A-induced MT1-MMP expression has been linked with cyclooxygenase-2 (COX-2) up-regulation and cancer cell death via endoplasmic reticulum (ER) stress signaling in glioblastoma cells [2, 9]. Moreover, several cell lines treated with Con A have exhibited tyrosine phosphorylations of major intracellular proteins, including protein-zero related (PZR) cell surface molecules [10], and Con A has been shown to selectively block kainate receptor (KAR) desensitization and to markedly increase KAR-mediated neurotoxicity [11]. Recently, we reported that Con A-mediated NMDA receptor subunit modulation in cultured cortical cells was associated with α-amino-3-hydroxy-5-methyl-isoxazole-4-propionate (AMPA) receptor activation [12]. Considering the roles played by ROS generation and tyrosine kinase activation in neuronal death [13,14,15], we asked whether Con A-induced neuronal apoptosis might occur via ROS generation and tyrosine kinase activation. To investigate the toxicity of Con A in neuronal systems, it was treated to cultured neuronal cells and directly injected into rat frontal cortices.
Materials and Methods
Chemicals
Con A (Type IV salt free), methyl-α-d-mannopyranoside (M-α-MP), L-glutamine, glucose, HEPES, poly-d-lysine, dimethyl sulfoxide (DMSO), N-acetyl cysteine (NAC), diphenyleneiodonium chloride (DPI), AG556 (a TNF-α inhibitor), AG82 (a tyrosine kinase inhibitor), and H2DCF-DA were obtained from Sigma-Aldrich (St. Louis, MO). Horse serum, fetal bovine serum (FBS), Eagle’s minimal essential media (MEM) and Dulbecco`s modified eagle medium (DMEM) were purchased from Hyclone (Logan, Utah, USA). Antibodies were obtained from Cell Signaling Technology®, 6-cyano-7-nitroquinoxaline-2,3-dione (CNQX), 2,3-dihydroxy-6-nitro-7-sulfamoyl-benzo[f] quinoxaline-2,3-dione (NBQX), and 1-(4-aminophenyl)-4-methyl-7,8-methylenedioxy-5H-2,3-benzodiazepine (GYKI524666) were purchased from Calbiochem (La Jolla, CA, USA).
Animals and Cell Culture
Cerebral cortices were removed from the brain of 15.5 days old ICR fetal mice for neuronal culture. Male Sprague–Dawley rats (260–280 g) were obtained from Daehan Biolink (Eumsung, Korea). Rats (3–4 per group) were kept under standard conditions; at 24 ± 3 °C under a 12 h light/dark cycle with free access to rodent chow and water. All procedures involving rats were performed according to the guidelines issued by the Animal Care and Use Committee of the School of Medicine, Ewha Womans University in South Korea.
The neocortices of fetal mice were triturated and plated on 24 well plates (~106 cells/culture well) pre-coated with 100 µg/mL poly–D–lysine and 4 μg/mL laminin, and cultured in MEM (supplemented with horse serum (5%), FBS (5%), 2 mM glutamine, and 20 mM glucose). Cultures were maintained at 37 °C in a humidified 5% CO2 atmosphere. After 6 days in vitro (DIV), the medium was changed to plating medium containing 10 μM cytosine arabinoside but not FBS. Media were changed twice weekly. To assess cell condition, mixed cortical cell cultures containing neurons and glia (DIV 12–14) were exposed to Con A in horse serum free culture medium. Cell morphologies of degenerating neurons were observed under a phase contrast microscope every 24 h after exposing cells to Con A.
Primary astrocytes and microglia were prepared from 1-day-old Sprague–Dawley rats. Cortices were triturated into single cells in MEM containing 10% FBS, and then plated into 75 cm2 T-flasks for 10–14 days. To prepare pure astrocytes, microglia were removed from T-flasks by mild shaking and remaining astrocytes were sub-cultured twice for experiments. Astrocyte purity was confirmed by staining for astrocyte-specific glial fibrillary acidic protein (GFAP, Chemicon), and was usually >99%. Detached microglia were used for co-culture experiments. The enriched microglia used were >95% pure as assessed by immunocytochemical staining for the microglia-specific marker, CR3 complement receptor, which was detected using OX-42 antibody (Serotec, UK).
Measurement of Cell Viability
Cell counts and viabilities were assessed using WST–1 reagent (Roche, Indianapolis, IN, USA). Cells were incubated with WST–1 at a dilution of 1:10 in original conditioned media at 37 °C for 2 h. After washing with medium, cells were collected and lysed. Relative amounts formazan produced by metabolically active cells were assessed indirectly by measuring absorbance at 450 nm.
Intracranial Con A Injection and Immunohistochemistry
Rats (260–280 g) were implanted with guide cannula for intracranial injection. Briefly, a rat was anesthetized with an intramuscular injection of ketamine (50 mg/kg) and xylazine (1 mg/kg), before standard stereotaxic surgery was performed on a Kopf stereotaxic frame. A 21-gauge stainless steel cannula was implanted in the frontal cortex (ML: 0.7 mm; AP: 3.2 mm; and DV: −2.3 mm); bregma was chosen as the stereotaxic reference point. The cannula was inserted into cortex and anchored in place with rapid-setting dental acrylic (Lang Dental Mfg. Co., Chicago, IL, USA) and to the skull by a plastic protective cap. Prior to microinjection, saline or Con A was filtered through a 0.2 µm sterile syringe filter and then infused using a 6-cm long PE-60 polyethylene tube connected to a Hamilton syringe. Con A (5 µl; 50 or 100 ng/µl) was microinfused over 10 min. The syringe was left in place for 5 min after injection completion to prevent diffusion up the cannula, and was then removed when a clean stylet was inserted into the cannula.
Three days after Con A infusion, rats were anesthetized with ether and hearts were perfused with 0.05 M PBS. Brains were removed, fixed in 4%-paraformaldehyde (in 0.1 M phosphate buffer), and cryoprotected by infiltration using increasing concentrations of sucrose (10–30%), frozen in freezing medium. Coronal sections (20 μm thick) were prepared using a cryostat (LEICA CM 3000), and collected on gelatin-coated slides. Antigen retrieval from tissue sections was performed with sodium acetate and this was followed by immersion in 0.3% hydrogen peroxide (in PBS) for 20 min at room temperature. Slides were then preincubated with 10% normal horse serum (Vector Laboratory) for 1 h and incubated with mouse anti-MAP2 (6 μg/ml, Upstate) and mouse anti-GFAP antibody (1:800, Chemicon) overnight at 4 °C. A second slide of an adjacent brain section was incubated with either Alexa 488- or Alexa 555-conjugated secondary antibodies for 1 h at room temperature. In addition, appropriate controls not incubated with primary antibodies were included. After counterstaining with Hoechst 33,342, tissue sections were mounted with ProLong Gold antifade reagent and coverslipped. Finally, stained slides were visualized under an epifluorescence microscope. The immuno-positive cells were measured and the numbers of particle (pixel) at certain area (100 µm2) were calculated using analysis software (Soft Image Systems, Munster, Germany).
Immunoblot Analysis
After incubation with ConA, neuronal cells were washed twice with cold PBS, lysed in ice-cold modified lysis buffer (150 mM NaCl, 50 mM Tris, 1 mM EDTA, 0.01% Triton X-100, and protease inhibitor pH 8.0) and centrifuged at 12,000 rpm for 5 min. Cells were aliquoted and stored at -70 °C until required. Protein concentrations were determined using the bicinchoninic acid (BCA) assay (Rockford, IL, USA). Unlike the Bradford and Lowry assay, the BCA assay features a relatively small protein-to protein variation [16]. Samples were incubated at 60 °C for 15 min to ensure the lowest protein-to-protein variation. Proteins were loaded and separated by SDS-polyacrylamide gel electrophoresis and transferred to polyvinylidene difluoride (PVDF) membranes, which were blocked with 5% non-fat dry milk in TBST solution. Blots were then incubated with antibodies for anti-MAP2, anti-GFAP, anti-phosphotyrosine, 4G10 (Upstate, USA), phosphorylated or total forms of ERK1/2, p38 MAPK, JNK, Bcl-xL, and cleaved caspase-3 (Cell Signaling Technology, MA, USA). After washing with TBST, HRP-conjugated secondary antibodies (Cell Signaling Technology) were applied and blots were developed using an enhanced chemiluminescence detection kit (Amersham Biosciences, Piscataway, NJ, USA).
Reverse Transcription Polymerase Chain Reaction (RT-PCR)
Total RNA was isolated from cortical neurons and astrocytes using TRIzol (Invitrogen, Carlsbad, CA, USA), according to the manufacturer’s instructions. For cDNA synthesis, 2 µg of total RNA was reverse-transcribed using the SuperScript First-Strand Synthesis System (Invitrogen, Carlsbad, CA, USA). cDNA was amplified by RT-PCR using rat primers for inducible nitric oxide synthase (iNOS), IL-1β, IL-6, TNF-α, gp91-phox, p22-phox, p40-phox, p47-phox, p67-phox, and β-actin, which was used as a loading control. PCR products were separated by 1% agarose gel electrophoresis and stained with ethidium bromide.
Measurement of Intracellular ROS
Intracellular ROS accumulation was measured using the oxidant-sensing fluorescent probe dichlorodihydro-fluorescein diacetate (H2DCF-DA). Cortical cultures were incubated with 30 μM H2DCF-DA in HBSS buffer for 1 h at 37 °C and then treated with Con A. DCF fluorescence intensities were measured at excitation and emission wavelengths of 485 and 535 nm, respectively, using a fluorescence plate reader (Molecular Devices, CA, and USA).
Statistical Analysis
Results are expressed as means ± SEMs. Group comparisons were performed using the one-tailed unpaired t-test or analysis of variance (ANOVA) followed by the post hoc t-test. Statistical significance was accepted for p values of <0.05 or <0.01, as indicated.
Results
Con A Induced Neuronal Cell Death and Astrocyte Activation In Vitro
Con A (1, 10, 100 μg/ml) had a cytotoxic effect on cortical neurons, as demonstrated by a reduction in cell viability of 70% and 50% (p < 0.01) at concentrations of 10 and 100 μg/ml, respectively (Fig. 1a). In addition, MAP2 (microtubule associated protein 2) expression was strongly suppressed by Con A treatment in neuronal cells (Fig. 1b, c), but its toxic effect on astrocytes was minimal, for example, GFAP expression was not changed (Fig. 1b, c).
Con A had a cytotoxic effect in cortical neurons. Cultured cortical cells (1 × 106 cells per well) were treated with Con A (1, 10, 100 μg/ml) for 24 h and cell viabilities were determined using WST-1 (a). Con A-induced cytotoxicity was monitored using MAP2 protein expression in cortical neurons (b). Beta actin was also measured as an internal control. Con A-treated cortical neurons and pure astrocytes stained with MAP2 and GFAP, respectively (c). The one-tailed unpaired t-test was used for reasons of intergroup comparisons. Results are presented as the means ± standard errors of three independent experiments. *p < 0.05, **p < 0.01 versus vehicle treated controls
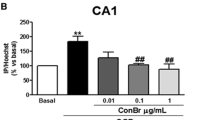
Intracranial Injection of Con A Detrimentally Affected Neurons But Not Astrocytes
At 3 days after injecting 5 μl of Con A (50 or 100 ng/μl) into cortical tissues in frontal cortices neuron dendrites were degraded as indicated by only faint MAP2 expression (Con A 50 ng/μl, p < 0.05; Con A 100 ng/μl, p < 0.01), whereas astrocyte activation was not changed; glial filaments and GFAP expression remained unchanged (Fig. 2).
Morphological abnormalities of neuronal cells in Con A treated rat brains. Con A (5 µl of 50 or 100 ng/µl) was directly injected into a frontal cortex over 10 min (0.5 µl/min). Neurons in cortical area were found to be damaged at 3 days post-injection. Sections were observed under a fluorescence microscope at 800× (a). MAP2 or GFAP immuno-positive cells in cortical tissues were measured. The numbers of particle (pixel) at the certain areas (100 µm2) were calculated using analysis software (Soft Image Systems, Munster, Germany). The one-tailed unpaired t-test was used for intergroup comparisons. *p < 0.05, **p < 0.01 versus saline controls (each group n = 5)
Pretreatment with Methyl α-d-Mannopyranoside Maintained the Viabilities of Con A-treated Neurons
We investigated the involvement of cross-linked cell surface glycoproteins containing α-d-mannopyranoside (M-α-MP) residue in Con A-induced neuronal death. M-α-MP, a competitor of Con A binding to carbohydrate chain of a protein, was used in the cell viability assay, which was conducted on mixed cortical neurons. One way ANOVA revealed a significant difference between the viabilities of cells treated with Con A or M-α-MP plus ConA (F3,11=57.36, p < 0.01). Pre-treatment with M-α-MP (10 mM) before ConA (10 µg/ml) maintained cell viability (p < 0.01) at the normal level (Fig. 3a). The relationship between activation of AMPA/KA receptor and Con A-induced cell death was investigated, as Con A has been reported to be an inhibitor of AMPA receptor desensitization [12]. We found Con A-induced cell death was not modulated by the AMPA/KA receptor antagonist, GYKI52466 (Fig. 3b), which suggested Con A-induced cell death occurred after its binding to neuronal glycoproteins.
Effects of methyl-α-d-mannopyranoside and AMPA/KA receptor antagonist on Con A-induced cell death. Cortical neurons (1 × 106 cells per well) were pretreated with methyl-α-d-mannopyranoside (M-α-MP) or GYKI524666 for 30 min, and then exposed for Con A (10 μg/ml) for 24 h. Cell viabilities were measured using WST-1. M-α-MP inhibited Con A-induced cell death (a), whereas the AMPA/KA receptor antagonist, GYKI524666 did not affect cell viability (b). Results are presented as the means ± standard errors of three independent experiments. Columns represent mean values and SEMs (n = 8–10). ANOVA was used to compare significance for M-a-Mp treatment, and the one-tailed unpaired t-test was used to compare significance for GYKI524666 treatment. *p < 0.05 versus Con A treated controls
Con A-Treated Cortical Neurons and Astrocytes Exhibited Elevated mRNA Expressions of Pro-Inflammatory Cytokines
Astrocytes and cortical neurons release cytokines during mechanical and ischemic injury [17]. Therefore, we examined whether Con A could induce inflammation in cultured cortical cells and astrocytes by investigating the gene expressions of proinflammatory cytokines. Expressions of TNF-α, IL-1β and IL-6 mRNAs were markedly and dose-dependently elevated in cortical neurons and astrocytes (Fig. 4a, b). Interestingly, although inducible nitric oxide synthase (iNOS) gene expression was pronounced in astrocytes, its expression was not observed in cortical neurons.
Effect of Con A on the expressions of iNOS and pro-inflammatory genes in cortical neurons and astrocytes. Cells were treated with Con A (1–100 μg/ml) for 24 h and total RNAs were extracted. Gene expression levels of iNOS and pro-inflammatory cytokines were determined by RT-PCR. iNOS, TNF-α, IL-1β and IL-6 mRNA expressions in cortical neurons (a) and astrocytes (b). Results are presented as the means ± standard errors of three independent experiments (c, d). The one-tailed unpaired t-test was used intergroup comparisons. *p < 0.01, **p < 0.01 versus treatment naïve controls
Intracellular ROS Generation and NADPH Oxidase Expression was Enhanced by Con A in Cortical Cells
It has been reported that activated astrocytes release intracellular ROS [18, 19]. Therefore, we evaluated ROS generation after Con A treatment (1–100 µg/ml) in cortical neurons, astrocytes, and microglia. ROS levels were markedly and dose-dependently increased in cortical neurons (p < 0.05, p < 0.01) but not in astrocytes or microglia (Fig. 5a). Although high concentrations (50, 100 µg/ml) of Con A significantly increased ROS levels in astrocytes.
ROS generation and NADPH oxidase gene expressions in Con A-treated cortical cells. Cortical neurons were incubated with H2DCF-DA for 1 h, treated with Con A (1–100 μg/ml) for 6 h, and ROS levels were measured (RFUs, relative fluorescence units) (a). Cells were treated with Con A for 24 h and the mRNA levels of NADPH oxidase subunits, gp91-phox, p22-phox, p40-phox, p47-phox, and p67-phox mRNA were determined by RT-PCR (b). Results are presented as the means ± standard errors of three independent experiments (c). The one-tailed unpaired t-test was used for intergroup comparisons. *p < 0.01, **p < 0.01 versus treatment naïve controls
Because NADPH oxidase directly contributes to oxidative stress by increasing the levels of ROS [20], we measured the mRNA expressions of NADPH oxidase gp91-phox, p22-phox, p40-phox, p47-phox and p67-phox in cortical cells treated with Con A (1-100 μg/ml). We found Con A at concentrations of 5 µg/ml upregulated the mRNA expressions of membrane and cytosolic subunits of NADPH oxidase (Fig. 5b, c).
Con A-Induced Intracellular ROS Generation and the Involvement of TNF-α and Tyrosine Kinase-Mediated Signaling
Con A has been reported to have mitogenic activities in various cells via receptor cross-linkages [10, 21]. Con A-induced ROS generation was investigated using, that is, M-α-MP, NAC (an antioxidant), and DPI (a NADPH oxidase inhibitor). One way ANOVA revealed that treatments with these agents ROS accumulation was decreased significantly {M-α-MP (F4,14 = 99.58, p < 0.01), NAC (F4,14 = 1531, p < 0.01), DPI (F4,14 = 18.95. p < 0.01), AG556 (F5,17 = 41.16, p < 0.01) and AG82 (F5,17 = 246.48, p < 0.01)}. Post hoc t-test analysis showed that pretreatment of cortical cells with NAC or DPI significantly inhibited ROS accumulation (p < 0.01) (Fig. 6b, c), whereas treatment with M-α-MP slightly suppressed ROS accumulation (p < 0.05) (Fig. 6a). Next, we investigated the signaling pathway responsible for Con A-induced ROS generation. Pretreatment of cortical neurons with TNF-α inhibitor (AG556) or tyrosine kinase inhibitor (AG82) significantly inhibited ROS generation in a dose-dependent manner (p < 0.05, p < 0.01) (Fig. 6d, e), indicating TNF-α and tyrosine kinase mediated signaling pathways participated in Con A-induced ROS generation in cortical neurons.
Effects of oxidative stress, TNF-α generation, and the activations of tyrosine kinases by ROS in Con A-treated cortical neurons. Cells were pretreated with the Con A competitor methyl-α-d-mannopyranoside (M-α-MP) (a), the anti-oxidant NAC (b), or the NADPH oxidase inhibitor DPI (c) for 30 min and then exposed for Con A (50 μg/ml) for 6 h. ROS generation (RFU) was assessed using H2DCF-DA on a fluorescence plate reader. Both AG556 (d) and AG82 (e) strongly suppressed ROS generation by Con A in cortical neurons. Results are presented as the means ± standard errors of three independent experiments. Column represent mean values and SEMs (n = 8–10) as determined by ANOVA. Comparisons were made using the one-tailed unpaired t-test. *p < 0.05, **p < 0.01 versus Con A only treated controls
Con A-Induced Apoptotic Cell Death and the Involvement of Caspase 3
To identify other signaling pathways involved in Con A-induced cell death in cortical neurons, we examined MAPK phosphorylation (of p38, ERK, and JNK) and the protein expressions of Bcl-2, procaspases and caspases in cortical cultures treated with Con A (1–100 μg/ml). Whereas phospho-p38 protein expression was significantly (p < 0.05) upregulated, the phosphorylations of ERK and JNK were unaltered (Fig. 7a). On the other hand, Con A downregulated the expressions of the anti-apoptotic proteins Bcl-xL and pro-caspase-3 and upregulated the expressions of cleaved caspase-3 (Fig. 7b, c).
Con A induced neuronal apoptosis was associated with caspase activation. Cells were treated with Con A for 6 h and the protein expressions of p38, ERK1/2, and JNK (a), Bcl-xL (b), and cleaved caspase 3 (c) were measured. Results are presented as the means ± standard errors of three independent experiments. The analysis was performed using one-tailed unpaired t-test. *p < 0.05 versus treatment naïve controls
Discussion
The plant lectin concanavalin A (Con A) has a myriad biological effects. Con A exhibits a tetrameric conformation at physiological pH and may play important roles in cell adhesion, signal transduction, mitogenic stimulation, cytotoxic, and apoptotic mechanisms [22, 23]. Concanavalin A induces programmed cell death in neurons via signals emanating from the cross-linking of glycoprotein on neuronal membranes [24]. However, Con A-induced neuronal toxicity through inflammation-mediated ROS production and the activations of tyrosine kinases is poorly understood. Here, we found treatment with Con A led to toxicity in cortical neurons and enhanced the gene expressions of proinflammatory mediators, such as, IL-1β, IL-6, TNF-α, and NO. Con A-induced neuronal cell death, but not astrocyte death, in rat brain, indicating a cell-specific toxic effect, as has been previously reported [25, 26]. We observed Con A-induced ROS generation was significantly more elevated in neurons than in astrocytes or microglia in cultured cells, which suggests that ROS generation induced by cortical neurons probably caused the neuronal cell death observed, as has been previously reported [13]. In addition, we found ROS induction by Con A was significantly reduced by 20 mM M-α-MP, but not by 40 mM M-α-MP, which we speculate was due diminished membrane stability caused by osmolality changes. Con A-induced ROS generation was also inhibited by NAC (an anti-oxidant) and by TNF-α inhibitor (AG556), which suggests ROS generation induced by Con A initiated TNF-α and/or tyrosine kinase mediated signaling pathways that led to neuronal cell death [7, 14]. Given the role of MEK/ ERK pathway in Con A-induced autophagy in HeLa cells [27], we investigated changes in MAPK, Bcl-2 and caspase protein expressions during Con A-induced neuronal apoptosis. Con A-treatment led to up-regulations of the expressions of p38 MAPK and cleaved caspase 3 protein expressions and to the down regulation of Bcl-xL, indicating Con A-induced neuronal cell death also involve autophagic cell signaling pathways.
Activated astrocytes aggravate neurodegeneration by releasing proinflammatory mediators [28, 29] and they are also key players in glia-neuron complex interactions associated with neuroinflammation [29]. We surmise NO, TNF-α, IL-1β and IL-6 releases by Con A-activated astrocytes may exert neurotoxic effects that ultimately lead to neuronal cell death. The cytokine TNF-α is released by various cell types including neurons and can induce cellular responses, such as, inflammation and cell death [30, 31]. Furthermore, it has been reported Con A-mediated liver injury associated with ROS production and JNK activation is largely dependent on TNF-α [7]. Studies also indicate activated T-cells cause hepatocyte apoptosis mediated by the TNF-α signaling cascade via cell surface death receptors that activate caspase-8, caspase-3 and caspase-7 [5, 31]. Our observations suggest Con A-treated cortical cells may follow a similar scenario.
Protein tyrosine phosphorylation plays an important role in cellular metabolism [32,33,34]. Cytoplasmic tyrosine kinase activation and signaling induced by extracellular stimuli [35] have been reported to lead to cellular apoptosis. We observed Con A induced the tyrosine phosphorylation of proteins (100−75 kDa) in cortical cells, which might explain in part ROS generation and neuronal cell death (data not shown). This topic requires further study.
NADPH oxidase mediated ROS generation appears to be an initial “trigger” of neuronal apoptotic [36, 37]. Therefore, we speculated Con A-induced neuronal apoptosis might originate from the activation of NADPH oxidase and exacerbated by astrocyte-induced NO and proinflammatory cytokine production. Thus, Con A-induced ROS generation might be an immediate cause for neuronal toxicity. The over-expression of iNOS has also been documented to have hepatotoxic effects in a variety of animal models, including a murine Con A-induced hepatitis model [38], in which it was associated with NO release by neutrophils and monocytes [5] through the p38 MAPK pathway [1]. It appears reasonable to presume Con A-induced iNOS overexpression in astrocytes accompanied by NO release may further increase ROS generation.
The study indicates Con A induces ROS generation in cortical cells, and that subsequent TNF-α signaling and tyrosine kinase activation may interact and result in ROS accumulation, and thus, cortical neuron damage and death.
References
Kesherwani V, Sodhi A (2007) Differential activation of macrophages in vitro by lectin concanavalin A, Phytohemagglutinin and wheat germ agglutinin: production and regulation of nitric oxide. Nitric Oxide 16(2):294–305
Sina A, Proulx-Bonneau S, Roy A, Poliquin L, Cao J, Annabi B (2010) The lectin concanavalin-A signals MT1-MMP catalytic independent induction of COX-2 through an IKKgamma/NF-kappaB-dependent pathway. J Cell Commun Signal 4(1):31–38
Nanni SB, Pratt J, Beauchemin D, Haidara K, Annabi B (2016) Impact of concanavalin-A-mediated cytoskeleton disruption on low-density lipoprotein receptor-related protein-1 internalization and cell surface expression in glioblastomas. Biomark Cancer 8:77–87
Biswas R, Ghosh P, Banerjee N, Das JK, Sau T, Banerjee A, Roy S, Ganguly S, Chatterjee M, Mukherjee A, Giri AK (2008) Analysis of T-cell proliferation and cytokine secretion in the individuals exposed to arsenic. Hum Exp Toxicol 27(5):381–386
Ding JW, Wang K, Brems JJ, Gamelli RL (2004) Protection against concanavalin A-induced hepatocyte apoptosis by molsidomine is time-dependent. J Am Coll Surg 198(1):67–77
Liu T, Xia Y, Li J, Li S, Feng J, Wu L, Zhang R, Xu S, Cheng K, Zhou Y, Zhou S, Dai W, Chen K, Wang F, Lu J, Guo C (2016) Shikonin attenuates concanavalin A-induced acute liver injury in mice via inhibition of the JNK pathway. Mediators Inflamm 2748367:(10)
Maeda S, Chang L, Li ZW, Luo JL, Leffert H, Karin M (2003) IKKbeta is required for prevention of apoptosis mediated by cell-bound but not by circulating TNFalpha. Immunity 19(5):725–737
Chen K, Li J, Li S, Feng J, Wu L, Liu T, Zhang R, Xu S, Cheng K, Zhou Y, Zhou S, Wang F, Dai W, Xia Y, Lu J, Guo C (2016) 15d-PGJ2 alleviates ConA-induced acute liver injury in mice by up-regulating HO-1 and reducing hepatic cell autophagy. Biomed Pharmacother 80:183–192
Proulx-Bonneau S, Pratt J, Annabi B (2011) A role for MT1-MMP as a cell death sensor/effector through the regulation of endoplasmic reticulum stress in U87 glioblastoma cells. J Neurooncol 104(1):33–43
Zhao R, Guerrah A, Tang H, Zhao ZJ (2002) Cell surface glycoprotein PZR is a major mediator of concanavalin A-induced cell signaling. J Biol Chem 277(10):7882–7888
Benveniste M, Wilhelm J, Dingledine RJ, Mott DD (2010) Subunit-dependent modulation of kainate receptors by muscarinic acetylcholine receptors. Brain Res 17:61–69
Jang S, Yu JY, Ahn JH, Oh S (2016) Modulation of NMDA receptor subunits expression by concanavalin A. Neurochem Res 41(48):1887–1898. doi:10.1007/s11064-016-1900-6 doi
Wakatsuki S, Araki T (2016) NADPH oxidases promote apoptosis by activating ZNRF1 ubiquitin ligase in neurons treated with an exogenously applied oxidant. Commun Integr Biol 9(2):e1143575
Folch J, Petrov D, Ettcheto M, Abad S, Sanchez-Lopez E, Garcia ML, Olloquequi J, Beas-Zarate C, Auladell C, Camins A (2016) Current research therapeutic strategies for Alzheimer’s disease treatment. Neural Plast 2016:8501693. doi:10.1155/2016/8501693
Adam-Vizi V (2005) Production of reactive oxygen species in brain mitochondria: contribution by electron transport chain and non-electron transport chain sources. Antioxid Redox Signal 7(9–10):1140–1149
Noble JE, Knight AE, Reason AJ, Di Matola A, Bailey MJ (2007) A comparison of protein quantitation assays for biopharmaceutical applications. Mol Biotechnol 37(2):99–111
Lau LT, Yu AC (2001) Astrocytes produce and release interleukin-1, interleukin-6, tumor necrosis factor alpha and interferon-gamma following traumatic and metabolic injury. J Neurotrauma 18(3):351–359
Jian Z, Ding S, Deng H, Wang J, Yi W, Wang L, Zhu S, Gu L, Xiong X (2016) Probenecid protects against oxygen-glucose deprivation injury in primary astrocytes by regulating inflammasome activity. Brain Res 15:123–129
Olatunji OJ, Feng Y, Olatunji OO, Tang J, Ouyang Z, Su Z (2016) Cordycepin protects PC12 cells against 6-hydroxydopamine induced neurotoxicity via its antioxidant properties. Biomed Pharmacother 81:7–14
Lee HJ, Ban JY, Seong YH (2005) Blockade of 5-HT(3) receptor with MDL7222 and Y25130 reduces hydrogen peroxide-induced neurotoxicity in cultured rat cortical cells. Life Sci 78(3):294–300
Pani G, Colavitti R, Borrello S, Galeotti T (2000) Endogenous oxygen radicals modulate protein tyrosine phosphorylation and JNK-1 activation in lectin-stimulated thymocytes. Biochem J 1:173–181
Yue KT, MacDonald JF, Pekhletski R, Hampson DR (1995) Differential effects of lectins on recombinant glutamate receptors. Eur J Pharmacol 291(3):229–235
Kulkarni GV, Lee W, Seth A, McCulloch CA (1998) Role of mitochondrial membrane potential in concanavalin A-induced apoptosis in human fibroblasts. Exp Cell Res 245(1):170–178
Cribbs DH, Kreng VM, Anderson AJ, Cotman CW (1996) Cross-linking of concanavalin A receptors on cortical neurons induces programmed cell death. Neuroscience 75(1):173–185
Oh TH, Markelonis GJ, Von Visger JR, Baik B, Shipley MT (1995) Acidic pH rapidly increases immunoreactivity of glial fibrillary acidic protein in cultured astrocytes. Glia 13(4):319–322
Jang S, Lee JH, Choi KR, Kim D, Yoo HS, Oh S (2007) Cytochemical alterations in the rat retina by LPS administration. Neurochem Res 32(1):1–10
Roy B, Pattanaik AK, Das J, Bhutia SK, Behera B, Singh P, Maiti TK (2014) Role of PI3K/Akt/mTOR and MEK/ERK pathway in Concanavalin A induced autophagy in HeLa cells. Chem Biol Interact 210:96–102
Efremova L, Chovancova P, Adam M, Gutbier S, Schildknecht S, Leist M (2016) Switching from astrocytic neuroprotection to neurodegeneration by cytokine stimulation. Arch Toxicol 91:231–246
Gonzalez-Reyes RE, Graciela Rubiano M (2016) Astrocyte’s RAGE: more than just a question of mood. Cent Nerv Syst Agents Med Chem:[Epub ahead of print]
Rauert H, Stuhmer T, Bargou R, Wajant H, Siegmund D (2011) TNFR1 and TNFR2 regulate the extrinsic apoptotic pathway in myeloma cells by multiple mechanisms. Cell Death Dis 2(2):e194
Martin M, Wei H, Lu T (2016) Targeting microenvironment in cancer therapeutics. Oncotarget 7:52575. doi: 10.18632/oncotarget.9824
Hunter T (2009) Tyrosine phosphorylation: thirty years and counting. Curr Opin Cell Biol 21(2):140–146
Naudin C, Chevalier C, Roche S (2016) The role of small adaptor proteins in the control of oncogenic signalingr driven by tyrosine kinases in human cancer. Oncotarget 7(10):11033–11055
Thannickal VJ, Fanburg BL (2000) Reactive oxygen species in cell signaling. Am J Physiol Lung Cell Mol Physiol 279(6):L1005-L1028
Varoni EM, Lo Faro AF, Sharifi-Rad J, Iriti M (2016) Anticancer molecular mechanisms of resveratrol. Front Nutr 3:8
Choi SH, Lee DY, Kim SU, Jin BK (2005) Thrombin-induced oxidative stress contributes to the death of hippocampal neurons in vivo: role of microglial NADPH oxidase. J Neurosci 25(16):4082–4090
Tammariello SP, Quinn MT, Estus S (2000) NADPH oxidase contributes directly to oxidative stress and apoptosis in nerve growth factor-deprived sympathetic neurons. J Neurosci 20(1):RC53
Schwabe RF, Brenner DA (2006) Mechanisms of liver injury. I. TNF-alpha-induced liver injury: role of IKK, JNK, and ROS pathways. Am J Physiol Gastrointest Liver Physiol 290(4):G583-589
Acknowledgements
This research was supported by a National Research Foundation (NRF) grant funded by the Korea government (MIST) (MRC 2010-0027945).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jang, S., Yayeh, T., Leem, YH. et al. Concanavalin A Induces Cortical Neuron Apoptosis by Causing ROS Accumulation and Tyrosine Kinase Activation. Neurochem Res 42, 3504–3514 (2017). https://doi.org/10.1007/s11064-017-2398-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-017-2398-2