Abstract
Astrocytes release biologically active substances that cause inflammation in neurodegenerative diseases. The present study investigated the effects of two flavonoids (apigenin and luteolin) on the production of IL-31 and IL-33 in lipopolysaccharide (LPS)-activated astrocytes. Cell viability was investigated using EZ-Cytox assay, mRNA expressions of IL-31 and IL-33 were analyzed by RT-PCR, protein expressions were analyzed by western blot, and cytokine secretion was analyzed by ELISA. Apigenin and luteolin prevented astrocyte activation and inhibited mRNA and protein expression and secretion of IL-31 and IL-33 in the LPS-treated astrocytes. Apigenin’s suppression of ERK, NF-κB, and STAT3 activations was responsible for the inhibition of IL-31 and IL-33, while luteolin’s suppression of JNK, p38, ERK, NF-κB, and STAT3 activations was responsible for the inhibition of IL-31 in the astrocytes. Also, luteolin’s suppression of ERK, NF-κB, and STAT3 activations inhibited IL-33 production in the activated astrocytes. In addition, apigenin and luteolin also prevented the translocation of activated STAT3 and NF-κB to the nucleus of the activated astrocytes and subsequently affected their DNA binding activities. The results suggest that apigenin and luteolin may have potentials as neuroprotective agents for the treatment of diseases involving astrocyte activation and detrimental production of IL-31 and IL-33.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Astrocytes constitute the most abundant cell population in the central nervous system (CNS) [1]. Like other cells of the CNS, astrocytes can release several biologically active substances capable of stimulating other cells [1, 2]. Under inflammatory conditions, astrocytes are said to be activated to produce pro-inflammatory mediators like TNF-α and IL-1β [3]. In neurological diseases such as multiple sclerosis, Alzheimer’s disease, Parkinson’s disease, and HIV-1-associated dementia (HAD), activated astrocytes activate NF-κB and STAT3 pathways to release pro-inflammatory cytokines and chemokines that induce cellular damage in the brain [4, 5]. Recently, astrocytes have been said to be new players in chronic itch in atopic dermatitis but what biologically active substances they release to induce chronic itch in atopic dermatitis is still unknown [6]. IL-31 is a recently discovered cytokine with structural similarities with cytokines of the IL-6 family. IL-31 is thought to be one of the sole mediators of pruritus in atopic dermatitis [7]. Besides the role of IL-31 in pruritus, high levels of IL-31 have also been detected in tissues and serum of patients with Crohn’s disease, asthma, and rhinitis. [8, 9]. IL-33 is also a newly described cytokine that is structurally similar to cytokines of the IL-1 family [10]. Studies show that IL-33 is involved in the pathophysiology of the CNS as it is induced in astrocytes to produce innate type 2 immune responses and pro-inflammatory cytokines [11]. IL-33 also polarizes T helper cells towards Th2 cell lineage and drives the production of pro-inflammatory cytokines, chemokines, and Th2-associated cytokines in mast cells, natural killer cells, and dendritic cells [12]. This thus suggests that IL-33 might play a role in allergic inflammatory diseases including atopic dermatitis. Interesting IL-33 receptors have been detected in the dorsal root ganglion neurons and injection of IL-33 rapidly induced pruritus (a symptom of atopic dermatitis) via the ST2 receptor in a histamine-independent fashion. This study thus suggests an important link between IL-33 and pruritus in atopic dermatitis and makes IL-33 a promising drug target [13]. Considering the fact that activated astrocytes secrete IL-33 and play a role in the pathophysiology of several diseases, it is worthy to investigate further biologically active substances released by these activated astrocytes and to find agents that will inhibit the release of these substances. Glucocorticoids are well-known robust anti-inflammatory drugs used for the treatment of several chronic inflammatory and immune diseases as they decreased the production of inflammatory cytokines [14]. Despite these, treatment with glucocorticoids poses a variety of side effects such as acne, Cushing’s syndrome, and heart disease and has been shown to act as a pro-inflammatory agent in the PNS and CNS [15, 16]. Thus, the need for alternative therapy for targeting CNS-related inflammation cannot be outlooked. Certain naturally occurring flavonoids are capable of modulating the nervous system function through restoration of the injured brain and improvement of cognitive performance and behavior [17].
Luteolin and apigenin are naturally occurring flavones in the class of flavonoids with potent antioxidant and anti-inflammatory activities [18,19,20]. Luteolin inhibited the release of histamine and prostaglandins in human mast cells and also prevented vascular endothelial growth factor release from mast cells and activated T cells [21, 22]. Luteolin also protected blood-brain barrier function by preserving trans-endothelial electrical resistance and relieving aggravated permeability in a human BBB model [23]. Apigenin is a known inhibitor of CK2, ERK1/2, and cyclooxygenase-2 (COX-2) expression and has been shown to suppress the production of IL-1β, TNF-α, IL-6, and IL-31 by downregulating NF-κB in vitro and in vivo [24,25,26,27,28]. Apigenin has also demonstrated neuroprotective potentials against AD pathogenesis in a human disease model [29]. Interestingly, both apigenin and luteolin cross the blood-brain barrier, thus stressing the importance of these compounds as promising novel therapeutics for neuro-inflammation [30, 31].
Despite the promising therapeutic potentials of apigenin and luteolin in brain diseases, no studies have investigated the effects of these two compounds on astrocyte activation vis-à-vis IL-31 and IL-33 production. In this study, we aimed to investigate the effects of apigenin and luteolin in LPS-stimulated astrocytes vis-à-vis IL-31 and IL-33 production, and to reveal their molecular mechanism of action.
MATERIALS AND METHODS
Materials
Murine astrocytes (C8-D1A) were procured from ATCC, Manassas, VA, USA. Dulbecco’s modified Eagle medium (DMEM) with 110 mg/mL sodium pyruvate and fetal bovine serum (FBS), horse serum (HS), and penicillin/streptomycin were procured from Gibco, Grand Island, NY, USA. Apigenin and luteolin (≥ 98%, HPLC) were procured from ChemFaces, Wuhan, China. EZ-Cytox reagent and EZ-western Lumi Pico Alpha were purchased from DoGenBio, Seoul, South Korea. Ribospin II extraction kit was purchased from GeneAll Biotechnology, Seoul, South Korea. ReverTra Ace® qPCR RT Master Mix with gDNA Remover and SYBR Premix Ex Taq™ were procured from Toyobo, Osaka, Japan, and Takara Bio, Nojihigashi, Japan, respectively. Radio-immunoprecipitation assay buffer (RIPA buffer), NE-PER™ nuclear/cytoplasmic extraction reagent, and enzyme-linked immunosorbent assay (ELISA) kits for IL-31 and IL-33 were purchased from Thermo Scientific, Rockford, IL, USA. Bradford’s assay reagent was purchased from Bio-Rad Laboratories, Hercules, CA, USA. 5× SDS-PAGE loading buffer was purchased from Biosesang, Seongnam, South Korea. Polyvinylidene fluoride membrane was purchased from Millipore, MA, USA. Lipopolysaccharides (LPS); dimethyl sulfoxide (DMSO); and inhibitors of p65, p38, ERK, and JNK were purchased from Sigma-Aldrich, St. Louis, MO, USA. Antibodies for p-JNK, JNK, p-NF-κB, p65, p-IκB-α, IκB-α, p-ERK, ERK p38, and p38 were purchased from Santa Cruz Biotechnology, Santa Cruz, CA, USA. Antibodies for IL-31 and actin were purchased from Abcam, Cambridge, UK, and Biosciences, Franklin Lakes, NJ, USA, respectively. Antibodies for IL-33 and GFAP were purchased from Invitrogen, Carlsbad, CA, USA. Anti-lamin B1, p-STAT3, STAT3, and horseradish peroxidase (HRP)-IgG secondary antibodies were purchased from Cell Signaling Technology, Danvers, MA, USA. DNA binding ELISA kits for NF-κB and STAT3 activation assays were purchased from Active Motif, Carlsbad, CA, USA. All other reagents, especially for western blot assay, were purchased from Bio-Rad, Bioseseang, or Millipore.
Cell Culture and Treatment
Astrocytes (5 × 104 cells/mL) were cultured in DMEM supplemented with 1% penicillin/streptomycin antibiotics, 10% FBS, and 5% HS in 125 × 25 mm or 90 × 20 mm cell culture dishes in an incubator with a temperature of 37 °C and a humidified atmosphere of 5% CO2. The astrocytes were cultured to 80% confluence and pretreated with 30 μM and 60 μM of apigenin or luteolin for 1 h before the astrocytes were stimulated with 2 μg/mL of LPS. After stimulation with LPS, the astrocytes were incubated for either 24 h, 12 h, 3 h, or 30 min depending on the experiment to be carried out. Astrocytes without apigenin or luteolin pretreatment and stimulation and astrocytes without apigenin or luteolin pretreatment but stimulated with LPS were cultured in parallel as negative and positive controls.
Cell Viability
For astrocyte viability studies, the astrocytes (3 × 104 cells/mL) were cultured in a 6-well cell culture plate for 16 h and then incubated in 0–100 μM of apigenin or luteolin for 24 h. After 24 h, 0.01 mL of EZ-Cytox reagent was added to each well and incubated for 4 h. The astrocyte viability in each well was monitored by measuring the absorbance in each well at 450 nm with a microplate reader (Tecan, Männedorf, Switzerland). The absorbance correlated with the number of live astrocytes.
ELISA
For ELISA, the cell culture supernatants (0.05 mL) from astrocytes treated with or without luteolin or apigenin and stimulated with LPS for 24 h were used. The amount of IL-31 and IL-33 secreted from astrocytes was measured with the ELISA kits according to the manufacturer’s instructions.
Whole-Cell Protein Extraction
Whole-cell protein extraction was performed on astrocytes treated with or without luteolin or apigenin and stimulated with or without LPS for 12 h or 30 min. The extraction was done using RIPA buffer according to the manufacturer’s instruction. In brief, astrocytes were rinsed in ice-cold PBS and detach from the culture dish. The astrocytes were pelleted by centrifugation at 2500×g for 5 min in 1.5-mL Eppendorf tubes. RIPA buffer (0.1 mL) containing protease and phosphatase inhibitors was added to the pelleted cells and mixed to suspend the cells. Next, the tubes were kept on ice and vortexed at 5-min interval for a total of 15 min. Then, the mixture was centrifuged at 14,000×g for 15 min to pellet the cell debris. The supernatant from each tube was transferred to new tubes and kept at − 80 °C for analysis.
Nuclear Protein Extraction
Nuclear protein extraction was performed on astrocytes treated with or without luteolin or apigenin and stimulated with or without LPS for 30 min. The extraction was done using NE-PER nuclear and cytoplasmic extraction kit according to the manufacturer’s instruction. In brief, the astrocytes were rinsed in ice-cold PBS and harvested with trypsin-EDTA centrifugation at 500×g for 5 min in 1.5-mL Eppendorf tubes. The astrocytes were washed in PBS and pelleted by centrifugation at 500×g for 5 min. CER I solution (0.1 mL) containing protease and phosphatase inhibitors was added to the pelleted astrocytes and the tubes were vortexed vigorously and kept on ice for 10 min. Then, CER II (0.011 mL) solution was added to the tubes, vortexed, and incubated for a minute on ice. Next, the tubes were vortexed and centrifuged for 5 min at 14,000×g. After centrifugation, the supernatant in the tube containing cytoplasmic proteins was immediately transferred to new pre-chilled tubes and stored at − 80 °C. Insoluble pellets of each tube containing the nuclei were suspended in ice-cold NER solution (0.05 mL) containing protease and phosphatase inhibitors. The tubes were kept on ice and vortexed at 10-min interval for 40 min. After that, the tubes were centrifuged for 10 min at 14,000×g. The supernatant containing the nuclear protein fractions was immediately transferred to new pre-chilled tubes and stored at − 80 °C for analysis. The purity of the nuclear extract was demonstrated by the absence of actin in the nuclear extract upon western blot analysis.
Western Blot
Whole-cell-extracted proteins and nuclear extracts from each sample were subjected to western blot analysis. The protein concentration was measured using Bradford’s reagent. Thirty micrograms of protein from each sample was diluted in 5× SDS-PAGE loading buffer and resolved on a 12% or 20% SDS-PAGE. The resolved proteins were transferred onto a polyvinylidene fluoride membranes at 100 V for 1 h. Following the transfer, the membranes were incubated in 5% BSA to block non-specific binding during subsequent immunostaining. Then, the membranes were incubated overnight at 4 °C with either antibody for p-JNK, p-STAT3, p-NF-κB, p-IκB-α, p-ERK, p-p38, GFAP, IL-33, or IL-31. After washing of the membranes, they were incubated with corresponding HRP-conjugated secondary antibodies for 2 h at room temperature. After washing, the membranes were then exposed to the EZ-western Lumi Pico Alpha chemiluminescence reagent and visualized on an ultraviolet detection imaging system (Alliance version 15.11; UVITEC, Cambridge, UK). After detection, the antibodies on the membranes were stripped in stripping buffer and incubated with either antibody for JNK, NF-κB, STAT3, IκB-α, ERK, p38, tubulin, actin, or lamin B1. The immunostaining procedure was repeated as described. The band densities were determined using ImageJ analysis software program.
Real-time RT-PCR
Astrocytes treated with or without luteolin and apigenin and stimulated with or without LPS for 3 h were used for real-time PCR analysis. The Ribospin II extraction kit was used to extract and purify total RNA from the astrocytes according to the manufacturer’s instructions. The RNA extract was stored at − 20 °C for analysis. One microgram of the total RNA from each sample was utilized to prepare cDNA using a ReverTra Ace® qPCR RT Master Mix with gDNA remover kit according to the manufacturer’s instructions. The thermal cycler use for the cDNA synthesis was a T100TM Bio-Rad thermal cycler. Real-time PCR was performed using the Thermal Cycler Dice Real-Time System III and lite (Takara). The reaction mixture consisted of 0.0125 mL of TB Green Premix Ex Taq, 0.002 mL of forward and reverse primers, 0.002 mL of cDNA, and 0.0085 mL of distilled water. Amplification was done using the following primers: GAPDH forward: 5′GGC TAC ACT GAG GAC CAG GT3′, reverse: 5′TCC ACC ACC CTG TTG CTG TA3′; IL-31 forward: 5′CCT ACC CTG GTG CGT CTT TG3′, reverse: 5′CTG ACA TCC CAG ATG CCT GC3′; and IL-33 forward: 5′TTG GCT TAC GAT GTT G GA3′, reverse: 5′ACT GTG GTG CCT GCT CTT CT3′. The thermal profile consisted of an initial denaturation at 95 °C for 5 min, followed by 40 cycles of 95 °C for 30 s. This was followed by annealing at 62 °C for 30 s. All samples were run in triplicate and the expression levels were normalized with GAPDH using a 2− ΔΔCt comparative method.
NF-κB and STAT Transcriptional Activity Assay
The NF-κB activation assay kit and STAT3 activation kit were used to perform the NF-κB DNA and STAT3 DNA binding activity according to the manufacturer’s guidelines with little modification.
The aforementioned nuclear extract was used for this experiment. Briefly, 0.02 mL of 10 μg of nuclear extract was mixed with 0.03 mL of complete binding buffer in the well plates containing NF-κB and STAT3 DNA targets. The plate was incubated for 1 h at room temperature with mild agitation. After the washing step, 0.1 mL of diluted NF-κB or STAT3 antibodies that recognize only epitopes of p65 and STAT3 (respectively) that are bound to DNA in the wells was added to each well. Following incubation for 1 h at room temperature, the wells were washed and 0.1 mL of diluted HRP–conjugated antibodies was added to each well. The plates were subsequently incubated for 1 h at room temperature and washed, and 0.1 mL of developing solution was put into the wells for 10 min. The reaction was stopped by adding 0.1 mL of stop solution. The absorbance was read at 450 nm and this absorbance corresponded with the DNA binding activities.
Statistical Analysis
All data were obtained from three independent experiments unless stated otherwise. Data analysis was done using SPSS statistics program (version 22 SPSS Inc., Chicago, IL, USA). The data are presented as mean ± SD. Differences between the variables were analyzed using a one-way analysis of variance with Duncan’s post hoc tests. Statistical significance was set at a p value of less than 0.05.
RESULTS
Cell Viability of Astrocytes
Changes in the cell viability of astrocytes following treatment with apigenin and luteolin were investigated using the EZ cell viability assay. As shown in Fig. 1a, we found that astrocytes treated with up to 100 μM of luteolin were still 100% viable at the end of the incubation period while astrocytes treated with apigenin retained their viability with up to 60 μM of apigenin treatment. Treatment with apigenin greater than 60 μM appeared to have significant toxicity to the astrocytes. In addition, the DMSO concentrations used to dissolve apigenin and luteolin were lower than 0.2% v/v and did not interfere with the viability of the astrocytes (data not shown). Based on these results, a concentration of 30 μM and 60 μM of apigenin or luteolin was used in all subsequent experiments.
Effects of apigenin and luteolin on astrocyte cell viability and activation. a Astrocytes (3 × 104 cells/mL) were cultured and treated with apigenin or luteolin (0 to 100 μM) for 24 h before cell viability studies were performed. Results are shown as mean ± SD of four different experiments. b Astrocytes (3 × 104 cells/mL) were cultured and treated with apigenin or luteolin (30 and 60 μM) before the cells were stimulated with LPS for 30 min. The expression level of glial fibrillary acidic protein (GFAP) was investigated via western blot assay. c ImageJ analysis software was used to analyze the densities of each band with respect to actin. Results are shown as mean ± SD of three different experiments. a Asterisk (*) indicates a significant difference compared to the non-treated samples for bars with the same color: p < 0.05. c Asterisk (*) indicates a significant difference at *p < 0.05 compared to the LPS-only treated cells for bars with the same color. Hash (#) indicates a significant difference at #p < 0.05 for bars with different colors within the same treatment concentration.
Luteolin and Apigenin Suppressed the Activation of Astrocytes by LPS
The suppression of astrocyte activation by apigenin and luteolin was investigated. As shown in Fig. 1 b and c, GFAP, a marker of astrocyte activation, was significantly expressed when astrocytes were incubated with LPS for 30 min. However, the expression of the GFAP was significantly decreased in a concentration-dependent manner when the cells were pretreated with apigenin or luteolin before stimulation with LPS. Luteolin prevented astrocyte activation more than apigenin. Collectively, the results show that apigenin and luteolin significantly prevented the activation of astrocytes by LPS.
Luteolin and Apigenin Prevented IL-31 and IL-33 mRNA Expression in Astrocytes
The suppression of IL-31 and IL-33 mRNA expressions in astrocytes by apigenin and luteolin was investigated. As shown in Fig. 2, when astrocytes were incubated with LPS for 3 h, there was a significant increase in IL-31 mRNA (Fig. 2a) and IL-33 mRNA (Fig. 2b) expressions. However, when the cells were pretreated with apigenin or luteolin, the expression of IL-31 and IL-33 mRNAs was significantly suppressed. No significant difference between apigenin and luteolin treatment was observed at 30-μM concentration, but at 60-μM concentration, luteolin significantly suppressed IL-31 mRNA expression more than apigenin. Similar results were obtained for IL-33 mRNA expression at 30-μM concentration, but at 60-μM concentration, apigenin significantly suppressed IL-33 mRNA expression more than luteolin. These results collectively demonstrate that luteolin and apigenin also affected IL-31 and IL-33 mRNA expression in astrocytes.
Effects of apigenin and luteolin on IL-31 (a) and IL-33 (b) mRNA expressions. Astrocytes (5 × 104 cells/mL) were cultured and treated with apigenin or luteolin (30 and 60 μM) before the cells were stimulated with LPS for 3 h. The mRNA expression levels of IL-31 and IL-33 were investigated via quantitative real-time PCR analysis. Results are shown as mean ± SD (n = 3). Asterisk (*) indicates a significant difference at *p < 0.05 compared to the LPS-only treated cells for bars with the same color. Hash (#) indicates a significant difference at #p < 0.05 for bars with different colors within the same treatment concentration.
Luteolin and Apigenin Prevented IL-31 and IL-33 Protein Expression in Astrocytes
The suppression of IL-31 and IL-33 mRNA by apigenin and luteolin pushed us to investigate whether apigenin and luteolin could also affect the expression of IL-31 and IL-33 proteins in the astrocytes. The astrocytes were cultured and pretreated with apigenin or luteolin before stimulation with LPS for 12 h. The expression status of IL-31 and IL-33 was measured by western blot. The results, as shown in Fig. 3, revealed that LPS significantly increased the expression state of IL-31 (Fig. 3a) and IL-33 (Fig. 3b). Pretreatment with apigenin or luteolin significantly decreased IL-31 and IL-33 expression in a dose-dependent manner. Luteolin suppressed the expression of IL-31 more than apigenin at both concentrations (Fig. 3c). On the other hand, no difference was found between the suppression of IL-33 by apigenin and luteolin at 30 μM but at 60 μM, luteolin was found to suppress IL-33 expression more than apigenin (Fig. 3d). Collectively, these results demonstrate that luteolin and apigenin also affected IL-31 and IL-33 expression at the protein levels.
Effects of apigenin and luteolin on IL-31 (a) and IL-33 (b) protein expression in astrocytes. Astrocytes (5 × 104 cells/mL) were cultured and treated with apigenin or luteolin (30 and 60 μM) before the cells were stimulated with LPS for 12 h. The protein expression levels of IL-31 and IL-33 were investigated via western blot assay. ImageJ analysis software was used to analyze the densities of each band with respect to actin (c, d). Results are shown as mean ± SD of three different experiments. The asterisk (*) indicates a significant difference at *p < 0.05 compared to the LPS-only treated cells for bars with the same color. The hash (#) indicates a significant difference at #p < 0.05 for bars with different colors within the same treatment concentration.
Luteolin and Apigenin Inhibited the Secretion of IL-31 and IL-33 in Astrocytes
The fact that apigenin and luteolin inhibited the expression of IL-31 and IL-33 proteins in the astrocytes motivated us to investigate the secretion of IL-31 and IL-33 by astrocytes stimulated with LPS. To achieve this, the astrocytes were cultured and pretreated with apigenin or luteolin before stimulation with LPS for 24 h. The concentrations of IL-31 and IL-33 in the cell culture media were measured by the ELISA technique. The results revealed that LPS stimulation significantly increased the secretion of IL-31 and IL-33 by the astrocytes (Fig. 4). However, when the cells were pretreated with apigenin or luteolin, before stimulation, the secretion of IL-31 (Fig. 4a) and IL-33 (Fig. 4b) was significantly suppressed in a concentration-dependent fashion. Luteolin significantly inhibited IL-31 and IL-33 secretion more than apigenin at both concentrations. This result collectively indicates that luteolin and apigenin affected the secretion of IL-31 and IL-33 in LPS-stimulated astrocytes.
Effects of apigenin and luteolin on IL-31 (a) and IL-33 (b) secretion from astrocytes. Astrocytes (5 × 104 cells/mL) were cultured and treated with apigenin or luteolin (30 and 60 μM) before the cells were stimulated with LPS for 24 h. The cell media was collected for IL-31 and IL-33 measurements by the ELISA kits. Results are shown as mean ± SD of three different experiments. The asterisk (*) indicates a significant difference at *p < 0.05 compared to the LPS-only treated cells for bars with the same color. The hash (#) indicates a significant difference at #p < 0.05 for bars with different colors within the same treatment concentration.
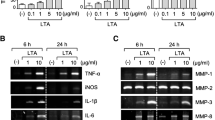
Luteolin and Apigenin Inhibited MAPK, NF-κB, and STAT3 Signal Pathways in Stimulated Astrocytes
The effects of luteolin and apigenin revealed above on the expression and production of IL-31 and IL-33 in stimulated astrocytes pushed us to investigate the effects of these two compounds on cell signaling proteins responsible for transcription of most cytokines in cells. We cultured the astrocytes and pretreated the cells with apigenin or luteolin before stimulation of the cells with LPS for 30 min. The phosphorylation statuses of key kinases in the NF-κB, STAT3, and MAPK signal pathways were investigated using western blot. In the MAPK pathway, stimulation of the astrocytes with LPS resulted in an increased ratio of phosphorylated versus non-phosphorylated forms of ERK, JNK, and p38. Apigenin significantly inhibited phosphorylation of ERK at doses of 30 μM and 60 μM, but did not affect phosphorylation levels of JNK and p38. Luteolin significantly inhibited phosphorylation of ERK, JNK, and p38 at doses of 30 μM and 60 μM (Fig. 5a, b). As concerning NF-κB-related signaling proteins, stimulation of the astrocytes with LPS resulted in an increased ratio of phosphorylated versus non-phosphorylated forms of IκB and p65. Apigenin and luteolin significantly inhibited phosphorylation of IκB and p65 at doses of 30 μM and 60 μM (Fig. 5c, d). For the JAK/STAT3 pathway, stimulation of the astrocytes with LPS resulted in an increased ratio of phosphorylated versus non-phosphorylated STAT3. Apigenin and luteolin also significantly inhibited phosphorylated STAT3 at doses of 30 μM and 60 μM (Fig. 5c, d). Further analysis of nuclear extracts revealed that apigenin and luteolin also dose-dependently blocked the translocation of phosphorylated p65 and phosphorylated STAT3 to the nucleus (Fig. 7a, b). The data suggest that apigenin and luteolin effectively suppressed the activation of MAPK, NF-κB, and STAT3 signaling in response to LPS.
Effects of apigenin and luteolin on MAPK, NF-κB, and STAT3 signal pathways in stimulated astrocytes. Astrocytes (5 × 104 cells/mL) were cultured and treated with apigenin or luteolin (a–d) before the cells were stimulated with LPS for 30 min. The protein expression levels of cell signaling kinases were investigated via western blot assay (a, c). ImageJ analysis software was used to analyze the densities of each band with respect to actin (b, d). Results are shown as mean ± SD of three different experiments. The asterisk (*) indicates a significant difference at *p < 0.05 compared to the LPS-only treated cells for bars with the same color.
Signaling Pathways Associated with the Effects of Apigenin and Luteolin on LPS-Induced IL-31 and IL-33 Expressions in Astrocytes
To further examine the mechanisms involved in the regulation of LPS-stimulated production of IL-31 and IL-33 in astrocytes, we added potent pharmacological inhibitors of JNK, ERK, p38, p65, and STAT3 to cultured astrocytes at non-cytotoxic concentrations and stimulated the astrocytes with LPS for 3 h to examine the mRNA expression of IL-31 and IL-33. According to the results reported in Fig. 6, the known inhibitors of ERK, p38, JNK, and p65 significantly suppressed the IL-31 mRNA while the known inhibitors of ERK, p65, and STAT3 significantly suppressed the IL-33 mRNA expression in the astrocytes. The findings indicate that ERK, p38, JNK, and p65, but not STAT3, might mediate the production of IL-31 while ERK, p65, and STAT3 might mediate the expression of IL-33 in astrocytes. Also, the suppression of ERK, p65, and STAT3 by apigenin and the suppression of ERK, JNK, p38, p65, and STAT3 by luteolin may be responsible for the inhibition of IL-31 and IL-33 in LPS-stimulated astrocytes.
Effects of ERK, p38, JNK, and NF-κB inhibitors on MAPK, NF-κB, and STAT3 signal pathways in stimulated astrocytes. Astrocytes (5 × 104 cells/mL) were cultured and treated with potent inhibitors of ERK, p38, JNK, NF-κB, or STAT3 before the cells were stimulated with LPS for 3 h. The mRNA expression levels of IL-31 and IL-33 were investigated via quantitative real-time PCR analysis. Results are shown as mean ± SD of three different experiments. The asterisk (*) indicates a significant difference at *p < 0.05 compared to the LPS-only treated cells for bars with the same color.
Luteolin Suppressed NF-κB DNA Binding Activity in IL-33-Stimulated HMC-1
Finally, we investigated if apigenin and luteolin affected the binding of NF-κB and STAT3 to their respective consensus-binding sites on a DNA molecule. To achieve this, astrocytes were cultured and pretreated with apigenin or luteolin before stimulation with LPS for 30 min to measure the DNA binding activities of activated NF-κB and STAT3 in the nuclear extract by ELISA technique. As reported in Fig. 7c, stimulation of the astrocytes resulted in a significant increase in the NF-κB and STAT3 binding to the immobilized NF-κB and STAT3 consensus-binding site in the wells. Apigenin and luteolin at a concentration of 60 μM suppressed the NF-κB and STAT3 activation by decreasing the binding of activated NF-κB and STAT3 to their respective consensus-binding site. These results thus demonstrate that apigenin and luteolin prevented the activation of NF-κB and STAT3 in activated astrocytes.
Effects of apigenin and luteolin on NF-κB, and STAT3 nuclear translocation and DNA binding. Astrocytes (5 × 104 cells/mL) were cultured and treated with apigenin or luteolin before the cells were stimulated with LPS for 30 min. The protein expression levels of activated NF-κB and STAT3 were investigated via western blot assay (a). ImageJ analysis software was used to analyze the densities of each band with respect to lamin B1 (b). The DNA binding activities of activated NF-κB and STAT3 were evaluated in the nuclear extracts using the ELISA-based method (c). Results are shown as mean ± SD of three different experiments. The asterisk (*) indicates a significant difference at *p < 0.05 compared to the LPS-only treated cells for bars with the same color.
DISCUSSION
Previous studies have reported on the anti-inflammatory and neuroprotective effects of apigenin and luteolin [29, 32]. However, whether apigenin and luteolin inhibit the production of IL-31 and IL-33 in LPS-activated astrocytes is not known. In the present study, we reported on the production of IL-31 in astrocytes and the effects of apigenin and luteolin on IL-31 and IL-33 production in astrocytes stimulated by LPS. We provided evidence that apigenin and luteolin also inhibit the expression of IL-31 and IL-33 in astrocytes.
Firstly, we investigated the activation of astrocytes by LPS and studied the effects of apigenin and luteolin treatment on astrocyte activation. We found that LPS stimulated the activation of astrocytes as upregulated GFAP expression was found in the LPS-treated astrocytes more than in the normal cells. We also found that both apigenin and luteolin suppressed the expression of the GFAP, thus implying an inhibition of astrocyte activation. While some activated astrocytes can promote neuronal survival, repair tissue, and reconstruct damaged blood-brain barriers, some activated astrocytes can cause adverse effects such as neuronal deaths and chronic pains by releasing signaling molecules [33]. Spinal cord reactive astrocytes have also been suggested as new players in chronic itch but what biologically active substances they release to mediate itch is still largely unknown although TLR4 receptors and STAT3 have been reported to be widely activated in reactive astrocytes [6]. Thus, inhibiting astrocyte activation in the diseased state is necessary for the treatment of several brain diseases including itch, spinal cord injury, Parkinson’s disease, and other neuro-inflammatory diseases [6, 34, 35]. Our data provide important clues of the inhibition of astrocyte activation by apigenin and luteolin that can be considered as therapeutic options for the regulation of astrocyte activations in diseases involving the CNS.
Next, we investigated if the activated astrocyte produces IL-31 and IL-33, two important cytokines implicated in the pathology of some diseases in the CNS. Although no study has reported on the production of IL-31 in the CNS, IL-31 receptors have widely been detected in the spinal cord and brain tissues and are thought to be responsible for the itch in atopic dermatitis. IL-33, on the other hand, has been widely studied to be produced by glial cells and is involved in the pathogenesis of neurodegenerative diseases. Thus, inhibiting the production of these cytokines in the CNS can be beneficial for the treatment or prevention of CNS-related diseases. Our study reviewed for the first time the mRNA expression and production of IL-31 in astrocytes and suggests that the production of IL-31 in the CNS might directly play a role in stimulating other cells of the CNS to induce itch as widely reported. This hypothesis needs to be considered as a major issue for future investigation. We also revealed that the two flavonoids—apigenin and luteolin—inhibited the production of IL-31 and IL-33 in activated astrocytes, an effect that started at least with the inhibition of their gene expression that subsequently affected their protein expressions and secretion from the astrocytes. The suppression of these cytokines by apigenin and luteolin may contribute to the prevention and treatment of CNS-related diseases involving IL-31 and IL-33. The data also adds more evidence about the neuroprotective action of apigenin and luteolin reported in other studies [25, 32, 36, 37].
Finally, we investigated the effects of apigenin and luteolin on some signaling pathways responsible for the production of several cytokines and inflammatory mediators in an attempt to understand the molecular mechanism of action these two flavonoids have in inhibiting IL-31 and IL-33 production in LPS-activated astrocytes. We reported that apigenin inhibited the phosphorylation activation of ERK while luteolin inhibited the activation of JNK, ERK, and p38 in the MAPK signaling pathways. In the NF-κB and STAT3 signaling pathways, we reported that both flavonoids inhibited the activation of IκB, NF-κB, and STAT3 in activated astrocytes. Further findings using potent inhibitors of the MAPK, NF-κB, and STAT3 signaling pathways revealed that ERK, p38, NF-κB, and STAT3 activations were responsible for the production of IL-31 in the LPS-stimulated astrocytes while ERK, NF-κB, and STAT3 activations signaled for the production of IL-33 in the activated astrocytes. The report implies that apigenin’s suppression of ERK, NF-κB, and STAT3 activations was responsible for the inhibition of IL-31 and IL-33 while luteolin’s suppression of JNK, p38, ERK, NF-κB, and STAT3 activations was responsible for the inhibition of IL-31 in the astrocytes. Also, luteolin’s suppression of ERK, NF-κB, and STAT3 activations inhibited IL-33 production in the activated astrocytes. Further investigation also revealed that both apigenin and luteolin suppressed the nuclear translocation and subsequent DNA binding activities of activated NF-κB and STAT3. The data offer insights into the potential mechanisms of action of the two flavonoids in inhibiting the production of IL-31 and IL-33 in LPS-stimulated astrocytes, tracing their action right down to the DNA level where transcription factors bind to the promoter regions of DNA to regulate the transcription of related genes. However, this may not be the initial site of action of the two flavonoids as the inhibition of the activations of upstream signaling kinases could have initiated the effects seen at the DNA binding activity levels. This could be true, as several studies have reported that flavonoids inhibit the activation of other upstream kinases in the MAPK, NF-κB, and STAT3 signaling pathways [38, 39].
In conclusion, by interfering with MAPK, NF-κB, and STAT3 signaling pathways, apigenin and luteolin suppressed the production of IL-31 and IL-33 in LPS-activated astrocytes, suggesting possibilities of the two flavonoids being exploited as neuroprotective agents for the treatment of diseases involving astrocyte activation and detrimental production of IL-31 and IL-33. Further investigations will be required to ascertain these facts in vivo in animal models.
Data Availability Statement
The data used to support the findings of the study is included in the article, and the data are available from the corresponding author upon request.
References
Eroglu, C., and B.A. Barres. 2010. Regulation of synaptic connectivity by glia. Nature 468: 223–231.
Rowitch, D.H., and A.R. Kriegstein. 2010. Developmental genetics of vertebrate glial–cell specification. Nature 468: 214–222.
Deng, Y., D. Xie, M. Fang, G. Zhu, C. Chen, H. Zeng, J. Lu, and K. Charanjit. 2014. Astrocyte-derived proinflammatory cytokines induce hypomyelination in the periventricular white matter in the hypoxic neonatal brain. PLoS One 9: e87420.
González-Reyes, R.E., M.O. Nava-Mesa, K. Vargas-Sánchez, D. Ariza-Salamanca, and L. Mora-Muñoz. 2017. Involvement of astrocytes in Alzheimer’s disease from a neuroinflammatory and oxidative stress perspective. Frontiers in Molecular Neuroscience 10: 427.
Sofroniew, M.V., and H.V. Vinters. 2010. Astrocytes: biology and pathology. Acta Neuropathologica 119: 7–35.
Tsuda, M. 2017. Spinal dorsal horn astrocytes: new players in chronic itch. Allergology international : official journal of the Japanese Society of Allergology 66: 31–35.
Dillon, S.R., C. Sprecher, A. Hammond, J. Bilsborough, M. Rosenfeld-Franklin, S.R. Presnell, H.S. Haugen, M. Maurer, B. Harder, J. Johnston, S. Bort, S. Mudri, J.L. Kuijper, T. Bukowski, P. Shea, D.L. Dong, M. Dasovich, F.J. Grant, L. Lockwood, S.D. Levin, C. LeCiel, K. Waggie, H. Day, S. Topouzis, J. Kramer, R. Kuestner, Z. Chen, D. Foster, J. Parrish-Novak, and J.A. Gross. 2004. Interleukin 31, a cytokine produced by activated T cells, induces dermatitis in mice. Nature Immunology 5: 752–760.
Dambacher, J., F. Beigel, J. Seiderer, D. Haller, B. Göke, C.J. Auernhammer, and S. Brand. 2007. Interleukin 31 mediates MAP kinase and STAT1/3 activation in intestinal epithelial cells and its expression is upregulated in inflammatory bowel disease. Gut 56: 1257–1265.
Lei, Z., G. Liu, Q. Huang, M. Lv, R. Zu, G.-M. Zhang, Z.-H. Feng, and B. Huang. 2008. SCF and IL-31 rather than IL-17 and BAFF are potential indicators in patients with allergic asthma. Allergy 63: 327–332.
Schmitz, J., A. Owyang, E. Oldham, Y. Song, E. Murphy, T.K. McClanahan, G. Zurawski, M. Moshrefi, J. Qin, X. Li, D.M. Gorman, J.F. Bazan, and R.A. Kastelein. 2005. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity 23: 479–490.
Hudson, C.A., G.P. Christophi, R.C. Gruber, J.R. Wilmore, D.A. Lawrence, and P.T. Massa. 2008. Induction of IL-33 expression and activity in central nervous system glia. Journal of Leukocyte Biology 84: 631–643.
Yasuoka, S., J. Kawanokuchi, B. Parajuli, S. Jin, Y. Doi, M. Noda, Y. Sonobe, H. Takeuchi, T. Mizuno, and A. Suzumura. 2011. Production and functions of IL-33 in the central nervous system. Brain Research 1385: 8–17.
Liu, B., Y. Tai, S. Achanta, M.M. Kaelberer, A.I. Caceres, X. Shao, J. Fang, and S.-E. Jordt. 2016. IL-33/ST2 signaling excites sensory neurons and mediates itch response in a mouse model of poison ivy contact allergy. Proceedings of the National Academy of Sciences of the United States of America 113: E7572–E7579.
Barnes, P.J. 2011. Glucocorticosteroids: current and future directions. British Journal of Pharmacology 163: 29–43.
Ericson-Neilsen, W., and A.D. Kaye. 2014. Steroids: pharmacology, complications, and practice delivery issues. The Ochsner Journal 14: 203–207.
Sorrells, S.F., and R.M. Sapolsky. 2007. An inflammatory review of glucocorticoid actions in the CNS. Brain, Behavior, and Immunity 21: 259–272.
Matias, I., A.S. Buosi, and F.C.A. Gomes. 2016. Functions of flavonoids in the central nervous system: astrocytes as targets for natural compounds. Neurochemistry International 95: 85–91.
Middleton, E., C. Kandaswami, and T.C. Theoharides. 2000. The effects of plant flavonoids on mammalian cells: implications for inflammation, heart disease, and cancer. Pharmacological Reviews 52: 673–751.
García-Lafuente, A., E. Guillamón, A. Villares, M.A. Rostagno, and J.A. Martínez. Flavonoids as anti-inflammatory agents: implications in cancer and cardiovascular disease. Inflammation Research 58: 537–552.
Wang, S., M. Cao, S. Xu, J. Shi, X. Mao, X. Yao, and C. Liu. 2020. Luteolin alters macrophage polarization to inhibit inflammation. Inflammation 43: 95–108.
Asadi, S., B. Zhang, Z. Weng, A. Angelidou, D. Kempuraj, K.D. Alysandratos, and T.C. Theoharides. 2010. Luteolin and thiosalicylate inhibit HgCl(2) and thimerosal-induced VEGF release from human mast cells. International Journal of Immunopathology and Pharmacology 23: 1015–1020.
Kempuraj, D., M. Tagen, B.P. Iliopoulou, A. Clemons, M. Vasiadi, W. Boucher, M. House, A. Wolfberg, and T.C. Theoharides. Luteolin inhibits myelin basic protein-induced human mast cell activation and mast cell-dependent stimulation of Jurkat T cells. British Journal of Pharmacology 155: 1076–1084.
Zhang, J.-X., J.-G. Xing, L.-L. Wang, H.-L. Jiang, S.-L. Guo, and R. Liu. 2017. Luteolin inhibits fibrillary β-amyloid(1-40)-induced inflammation in a human blood-brain barrier model by suppressing the p38 MAPK-mediated NF-κB signaling pathways. Molecules 22: 334.
Sawatzky, D.A., D.A. Willoughby, P.R. Colville-Nash, and A.G. Rossi. 2006. The involvement of the apoptosis-modulating proteins ERK 1/2, Bcl-xL and Bax in the resolution of acute inflammation in vivo. The American Journal of Pathology 168: 33–41.
Salehi, B., A. Venditti, M. Sharifi-Rad, D. Kręgiel, J. Sharifi-Rad, A. Durazzo, M. Lucarini, A. Santini, E.B. Souto, E. Novellino, H. Antolak, E. Azzini, W.N. Setzer, and N. Martins. 2019. The therapeutic potential of apigenin. International Journal of Molecular Sciences 20: 1305.
Che, D.N., B.O. Cho, J.Y. Shin, H.J. Kang, J.-S. Kim, H. Oh, Y.-S. Kim, and S.I. Jang. 2019. Apigenin inhibits IL-31 cytokine in human mast cell and mouse skin tissues. Molecules 24: 1290.
Ghildiyal, R., and E. Sen. 2017. CK2 induced RIG-I drives metabolic adaptations in IFNγ-treated glioma cells. Cytokine 89: 219–228.
Dang, Y., Z. Li, Q. Wei, R. Zhang, H. Xue, and Y. Zhang. 2018. Protective effect of apigenin on acrylonitrile-induced inflammation and apoptosis in testicular cells via the NF-κB pathway in rats. Inflammation 41: 1448–1459.
Balez, R., N. Steiner, M. Engel, S.S. Muñoz, J.S. Lum, Y. Wu, D. Wang, P. Vallotton, P. Sachdev, M. O’Connor, K. Sidhu, G. Münch, and L. Ooi. 2016. Neuroprotective effects of apigenin against inflammation, neuronal excitability and apoptosis in an induced pluripotent stem cell model of Alzheimer’s disease. Scientific Reports 6: 31450.
Venigalla, M., S. Sonego, E. Gyengesi, and G. Münch. 2015. Curcumin and apigenin - novel and promising therapeutics against chronic neuroinflammation in Alzheimer’s disease. Neural Regeneration Research 10: 1181–1185.
Theoharides, T.C., D. Kempuraj, and B.P. Iliopoulou. 2007. Mast cells, T cells, and inhibition by luteolin: implications for the pathogenesis and treatment of multiple sclerosis. Advances in Experimental Medicine and Biology 601: 423–430.
Rezai-Zadeh, K., J. Ehrhart, Y. Bai, P.R. Sanberg, P. Bickford, J. Tan, and R.D. Shytle. 2008. Apigenin and luteolin modulate microglial activation via inhibition of STAT1-induced CD40 expression. Journal of Neuroinflammation 5: 41.
Li, T., X. Chen, C. Zhang, Y. Zhang, and W. Yao. 2019. An update on reactive astrocytes in chronic pain. Journal of Neuroinflammation 16: 140–140.
Li, G., Y. Cao, F. Shen, Y. Wang, L. Bai, W. Guo, Y. Bi, G. Lv, and Z. Fan. 2016. Mdivi-1 inhibits astrocyte activation and astroglial scar formation and enhances axonal regeneration after spinal cord injury in rats. Frontiers in Cellular Neuroscience 10: 241.
Lee, Y., S. Lee, S.-C. Chang, and J. Lee. 2019. Significant roles of neuroinflammation in Parkinson’s disease: therapeutic targets for PD prevention. Archives of Pharmacal Research 42: 416–425.
Guo, D.J., F. Li, P.H. Yu, and S.W. Chan. 2013. Neuroprotective effects of luteolin against apoptosis induced by 6-hydroxydopamine on rat pheochromocytoma PC12 cells. Pharmaceutical Biology 51: 190–196.
Fu, J., H. Sun, Y. Zhang, W. Xu, C. Wang, Y. Fang, and J. Zhao. 2018. Neuroprotective effects of luteolin against spinal cord ischemia-reperfusion injury by attenuation of oxidative stress, inflammation, and apoptosis. Journal of Medicinal Food 21: 13–20.
Hou, D.X., and T. Kumamoto. 2010. Flavonoids as protein kinase inhibitors for cancer chemoprevention: direct binding and molecular modeling. Antioxidants & Redox Signaling 13: 691–719.
Prasad, S., K. Phromnoi, V.R. Yadav, M.M. Chaturvedi, and B.B. Aggarwal. 2010. Targeting inflammatory pathways by flavonoids for prevention and treatment of cancer. Planta Medica 76: 1044–1063.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (NRF-2019R1F1A1060332).
Author information
Authors and Affiliations
Contributions
Seon Il Jang: conceptualization, methodology, resources, writing-review and editing, supervision. Byoung Ok Cho: methodology, writing-review and editing. Denis Nchang Che: methodology, investigation, and data analysis, writing-original draft. Ji-su Kim, Jae Young Shin, Hyun Ju Kang: validation and visualization.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethics Approval
Not applicable
Consent to Participate
Not applicable
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Che, D.N., Cho, B.O., Kim, Js. et al. Luteolin and Apigenin Attenuate LPS-Induced Astrocyte Activation and Cytokine Production by Targeting MAPK, STAT3, and NF-κB Signaling Pathways. Inflammation 43, 1716–1728 (2020). https://doi.org/10.1007/s10753-020-01245-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-020-01245-6