Abstract
Resveratrol, a phytoalexin found in grapes and wine, exhibits antioxidant, anti-inflammatory, anti-aging and antitumor activities. Resveratrol also protects neurons and astrocytes in several neurological disease models. Astrocytes are responsible for modulating neurotransmitter systems, synaptic information, ionic homeostasis, energy metabolism, antioxidant defense and inflammatory response. In previous work, we showed that resveratrol modulates important glial functions, including glutamate uptake, glutamine synthetase activity, glutathione (GSH) levels and inflammatory response. Furthermore, astrocytes express toll-like receptors that specifically recognize lipopolysaccharide (LPS), which has been widely used to study experimentally inflammatory response. In this sense, LPS may stimulate pro-inflammatory cytokines release and oxidative stress. Moreover, there is interplay between these signals through signaling pathways such as NFκB, HO-1 and MAPK. Thus, here, we evaluated the effects of resveratrol on LPS-stimulated inflammatory response in hippocampal primary astrocyte cultures and the putative role of HO-1, p38 and ERK pathways in the protective effect of resveratrol. LPS increased the levels of TNF-α, IL-1β, IL-6 and IL-18 and resveratrol prevented these effects. Resveratrol also prevented the oxidative and nitrosative stress induced by LPS as well as the decrease in GSH content. Additionally, we demonstrated the involvement of NFκB, HO-1, p38 and ERK signaling pathways in the protective effect of resveratrol, providing the first mechanistic explanation for these effects in hippocampal astrocytes. Our findings reinforce the neuroprotective effects of resveratrol, which are mainly associated with anti-inflammatory and antioxidant activities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Astrocytes, the more versatile cells in the central nervous system (CNS), have a fundamental role in normal brain development and function [1, 2]. Astrocytes contribute to maintenance of synaptic information processing and ionic homeostasis; regulate energy metabolism and release of neurotrophic factors; modulate the biosynthesis and release of antioxidant defenses and the main anti- and proinflammatory cytokines [2–8]. Although immune responses in the CNS are mainly attributed to microglia, due to the capacity of these cells to present antigens, astrocytes express toll-like receptors (TLR) and build up responses to immune triggers by releasing proinflammatory molecules [9, 10].
Lipopolysaccharide (LPS) is the main component of outer membrane of gran-negative bacteria and has been widely used to study experimentally inflammatory response, including in the CNS [11, 12]. In this sense, astrocytes have TLR4, which belongs to TLR family receptors, and specifically recognizes LPS [12, 13]. The exposure to LPS can lead to release of proinflammatory cytokines and it in turn activate the transcription factor NFκB, nitric oxide (NO) release and overproduction of reactive oxygen species (ROS) [11, 14]. Furthermore, there is a close relationship between oxidative stress and inflammation, including in the pathogenesis of neurodegenerative diseases. Particularly in astrocytes, the depletion of glutathione (GSH) content exacerbates the inflammatory response [15].
LPS activates mitogen-activated protein kinases (MAPK), such as p38 and ERK (extracellular signal-regulated kinase), in astrocytes and both exert influence on the transcriptional activity of NFκB [9]. The MAPK superfamily of enzymes is a critical component of a central switchboard that coordinates incoming signals generated by a variety of extracellular and intracellular mediators [16–18]. Specific phosphorylation and activation of enzymes in the MAPK module transmits the signal down the cascade, resulting in phosphorylation of many proteins with substantial regulatory functions throughout the cell, including other protein kinases, transcription factors, cytoskeletal proteins and other enzymes [18].
Resveratrol (3,5,4′-trihidroxy-trans-stilbene) is a polyphenol found in a variety of dietary sources including grapes, peanuts and wine, predominately red wine [19–21]. Numerous studies ranging from cell cultures to animal models have demonstrated that resveratrol exhibits antioxidant, anti-inflammatory, anti-aging and antitumor activities [22–30]. Resveratrol also protects neurons and astrocytes in several neurological disease models, such as epilepsy, stroke, Alzheimer’s and Parkinson’s diseases [31–36]. Our group has shown that resveratrol modulates important glial functions, including glutamate uptake, glutamine synthetase (GS) activity, GSH levels and inflammatory response [22, 24, 37–40]. Recently, we also demonstrated the age-related antioxidant and anti-inflammatory effects of resveratrol in hippocampal astrocytes from adult and aged Wistar rats [29]. Although there is increasing evidence for the protective effects of resveratrol on CNS, the mechanisms of these effects are not fully understood.
In this sense, heme oxygenase 1 (HO-1) has been reported as a potential intracellular pathway by which resveratrol can provide protection against stressful conditions, such as oxidative stress, inflammation, hypoxia and neurodegeneration [22, 34]. Recently, we reported that resveratrol protects astroglial cells against oxidative stress through HO-1. HO is the sole physiological pathway of heme degradation and, consequently, plays a critical role in the regulation of cellular heme-dependent enzyme levels, degrading heme into the antioxidants biliverdin and bilirubin [41]. This enzyme presents three isoforms: the inducible HO-1, the constitutive HO-2 and the not catalytically active HO-3 [42, 43]. Although initial interest in HO-1 focused on its role in heme metabolism, recent studies demonstrating that HO-1 is highly related to oxidative stress, generating renewed interest in the regulation and function of HO-1 [41]. HO-1 counteracts NO toxicity by inhibiting inducible nitric oxide synthase (iNOS) activity. Furthermore, HO-1 is able to inhibit the NFκB translocation from the cytoplasm to the nucleus [44].
In spite of the neurotoxic actions of LPS and the well-known role of hippocampus on brain plasticity as well as the plethora of functions of resveratrol in glial cells, including antioxidant and anti-inflammatory activities, the aim of this investigation was examine the effects of resveratrol on LPS-stimulated neurotoxicity in hippocampal primary astrocyte cultures and the putative roles of HO-1, p38 and ERK in the protective effect of resveratrol. Thus, in this study, we measured cytokines release (TNF-α, IL-1β, IL-6, IL-10 and IL-18), NFκB activation, ROS production, NO levels and GSH content.
Materials and Methods
Chemicals
Dulbecco’s Modified Eagle’s Medium/F12 (DMEM/F12), other materials for cell cultures and NFkB p65 ELISA were purchased from Gibco/Invitrogen (Carlsbad, CA, USA). Resveratrol, LPS, 2′-7′-dichorofluorescein diacetate (DCFH-DA), propidium iodide (PI), MTT Formazan, GSH Standard Stock Solution, o-phthaldialdehyde, ZnPP IX, SB203580 and PD98059 were obtained from Sigma-Aldrich (St. Louis, MO, USA). TNF-α ELISA was purchased from PeproTech (Rocky Hill, NJ, USA). IL-1β, IL-6, IL-10 and IL-18 were purchased from eBioscience (USA). All other chemicals were purchased from common commercial suppliers.
Animals
Newborn male Wistar rats were obtained from our breeding colony (Department of Biochemistry, UFRGS, Porto Alegre, Brazil), maintained under controlled environment (12 h light/12 h dark cycle; 22 ± 1 °C; ad libitum access to food and water). All animal experiments were performed in accordance with the NIH Guide for the Care and Use of Laboratory Animals and were approved by the Federal University of Rio Grande do Sul Animal Care and Use Committee (process number 27543).
Primary Hippocampal Astrocyte Cultures
This protocol was in accordance with Bellaver et al. [45]. Briefly, the newborn male Wistar rats hippocampi were aseptically removed from cerebral hemispheres. The tissue was enzymatic (with trypsin 0.05 %) and mechanically dissociated, and then centrifuged at 100 g for 5 min. The cells were resuspended in Hanks’ balanced salt solution (HBSS) containing DNase (0.003 %) and left for decantation for 20 min. The supernatant was collected and centrifuged for 7 min (400 g). The cells from supernatant were resuspended in DMEM/F12 [10 % FBS, 15 mM HEPES, 14.3 mM NaHCO3, 1 % fungizone and 0.04 % gentamicin], plated in 6- or 24-well plates pre-coated with poly-l-lysine at a density of 3–5 × 105 cells/cm2. The cells were cultured at 37 °C in atmosphere with 5 % of CO2. The first medium exchange occurred 24 h after obtaining the culture. The medium change occurred once every 2 days during the 1st week and once every 4 days in the 2nd week.
Resveratrol and LPS Treatments
After cells reached confluence, the culture medium was removed and the cells were incubated in the presence of resveratrol (100 μM) for 1 h at 37 °C in atmosphere with 5 % of CO2 in serum-free DMEM/F12. Subsequently, 10 μg/ml LPS was added for 3 h in the presence or absence of resveratrol (100 μM). To study the role of HO-1, p38 MAPK and ERK signaling pathways in the effects of resveratrol on LPS-induced inflammatory response, we co-incubated with resveratrol: (1) ZnPP IX (10 μM), a HO-1 inhibitor, (2) SB203580 (5 μM), a p38 MAPK inhibitor and (3) PD98059 (5 μM), a ERK inhibitor.
TNF-α Measurement
The TNF-α assay was carried out in an extracellular medium, using a rat TNF-α ELISA. The results are expressed as the percentage of the control levels.
IL-1β, IL-6, IL-10 and IL-18 Measurements
The levels of interleukins were carried out in an extracellular medium, using ELISA kits for IL-1β, IL-6, IL-10 and IL-18 from eBioscience (USA). The results are expressed as the percentage of the control levels.
Nuclear Factor-kB Levels
The levels of NF-kB p65 in the nuclear fraction, which had been isolated from lysed cells by centrifugation, were measured using an ELISA commercial kit from Invitrogen (USA). The results are expressed as percentages relative to the control levels.
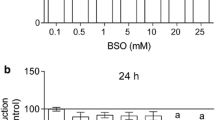
Cell Viability and Membrane Integrity
Cell viability was determined using a MTT Formazan assay (activity of mitochondrial dehydrogenases). MTT was added to the medium at a concentration of 50 µg/mL and cells were incubated for 30 min at 37 °C in an atmosphere with 5 % of CO2 [46]. Subsequently, the medium was removed and the MTT crystals were dissolved in dimethylsulfoxide. Absorbance values were measured at 560 and 650 nm. The results are expressed as percentages relative to the control conditions. For PI incorporation assay (membrane integrity), 7.5 μM PI was added, and cells were incubated for 30 min at 37 °C in an atmosphere with 5 % of CO2. The optical density of fluorescent nuclei (labeled with PI), used to indicate a loss in membrane integrity, was determined with Optiquant software (Packard Instrument Company). Density values obtained are expressed as a percentage of the control condition.
DCFH Oxidation
Intracellular ROS levels were detected using DCFH-DA. DCFH-DA was added to the medium at a concentration of 10 µM and cells were incubated for 30 min at 37 °C. Following DCFH-DA exposure, the cells were scraped into phosphate-buffered saline with 0.2 % Triton X-100. The fluorescence was measured in a plate reader (Spectra Max GEMINI XPS, Molecular Devices, USA) with excitation at 485 nm and emission at 520 nm [37]. The results are expressed as percentages relative to the control conditions.
Nitrite Levels
NO levels were determined by measuring the amount of nitrite (a stable oxidation product of NO), as indicated by the Griess reaction. The Griess reagent was prepared by mixing equal volumes of 1 % sulfanilamide in 0.5 M HCl and 0.1 % N-(1-naphthyl) ethylenediamine in deionized water. Briefly, the Griess reagent was added directly to the cell culture, which was incubated in the dark for 15 min, at 22 °C [47]. Samples were analyzed at 550 nm on a microplate spectrophotometer. Nitrite concentrations were calculated using a standard curve prepared with concentrations of sodium nitrite ranging from 0 to 50 µM. The results are expressed as percentages relative to the control conditions.
Glutathione (GSH) Levels
GSH levels were assessed as described previously [48]. Cell lysate suspended in a sodium phosphate buffer with 140 mM KCl was diluted with a 100 mM sodium phosphate buffer (pH 8.0) containing 5 mM EDTA, and the protein was precipitated with 1.7 % meta-phosphoric acid. The supernatant was assayed with o-phthaldialdehyde (at a concentration of 1 mg/mL methanol) at 22 °C for 15 min. Fluorescence was measured using excitation and emission wavelengths of 350 and 420 nm, respectively. A calibration curve was performed with standard GSH solutions at concentrations ranging from 0 to 500 µM. GSH concentrations were calculated as nmol/mg protein. The results are expressed as percentages relative to the control conditions.
Protein Determination
Protein content was measured using Lowry’s method with bovine serum albumin as a standard [49].
Statistical Analyses
Data are presented as mean ± S.E.M. Each experiment was performed in triplicate from at least four independent hippocampal astrocyte cultures. Differences among groups were statistically analyzed using two-way analysis of variance (ANOVA), followed by Tukey’s test. Values of P < 0.05 were considered significant and a indicates differences from control conditions and b differences from LPS. All analyses were performed using the Statistical Package for the Social Sciences (SPSS) software.
Results
LPS can stimulate inflammatory response and, in this sense, we measured the levels of classical proinflammatory cytokines. LPS increased three times the release of TNF-α from astrocytes compared to control conditions (Fig. 1a) and also induced significant increase of IL-1β (96 %), IL-6 (55 %) and IL-18 (80 %), Fig. 1b, c, d, respectively. Resveratrol significantly prevented these effects, repressing partially the release of TNF-α, IL-1β, IL-6 and IL-18. Resveratrol per se did not affect the proinflammatory cytokines levels. Additionally, we measured the anti-inflammatory cytokine IL-10 levels (Fig. 1e). Interestingly, resveratrol alone increased IL-10 levels (23 %). LPS did not significantly affect IL-10 levels compared to control and resveratrol did not maintained the augmentation of IL-10 under LPS challenge. When cells were incubated with HO-1 inhibitor (ZnPP IX), all effects of resveratrol were blocked. However, the inhibition of p38 and ERK activities with SB203580 and PD98059, respectively, attenuated LPS-induced TNF-α and IL-1β levels. Resveratrol strongly increased the effects of these inhibitors.
Effects of resveratrol on cytokines release. Cells were incubated for 1 h with 100 µM resveratrol (RSV), followed by the addition of 10 μg/ml LPS for 3 h in serum-free DMEM/F12. 10 μM ZnPP IX, a HO-1 inhibitor; 5 μM SB203580, a p38 inhibitor and 5 μM PD98059, an ERK inhibitor were co-incubated with resveratrol. Cytokines levels were measured as described in the “Materials and Methods” section. Data represent the mean ± S.E.M of four independent experimental determinations performed in triplicate and differences among groups were statistically analyzed using two-way ANOVA, followed by Tukey’s test. Values of P < 0.05 were considered significant. a indicates differences from control conditions and b differences from LPS challenge
Regarding to cellular viability, the cytotoxicity of resveratrol and/or LPS in hippocampal astrocytes was evaluated by PI incorporation and MTT reduction. Resveratrol and/or LPS did not affect membrane integrity and cell viability (data not shown).
To elucidate the possible mechanism of resveratrol on the inhibition of inflammatory response, we determined the NFκB activation. LPS increased NFκB p65 nuclear levels by 70 % (Fig. 2). Resveratrol decreased the levels of NFκB from 170 to 110 %. This effect was dependent of HO-1, which is upstream of NFκB. SB203580 and PD98059 inhibitors blocked the transcriptional activity of NFκB and resveratrol increased the effects of these inhibitors on NFκB p65 levels. Resveratrol alone did not stimulate the NFκB activation.
Resveratrol prevented the LPS-stimulated NFκB activation. Cells were incubated for 1 h with 100 µM resveratrol (RSV), followed by the addition of 10 μg/ml LPS for 3 h in serum-free DMEM/F12. 10 μM ZnPP IX or 5 μM SB203580 or 5 μM PD98059 were co-incubated with resveratrol. NFkB levels were measured as described in the “Materials and Methods” section. Data represent the mean ± S.E.M of four independent experimental determinations performed in triplicate and differences among groups were statistically analyzed using two-way ANOVA, followed by Tukey’s test. Values of P < 0.05 were considered significant. a indicates differences from control conditions and b differences from LPS
The production of ROS was measured using DCFH oxidation. The ROS levels increased 60 % following LPS exposure (Fig. 3a). Resveratrol prevented this effect, decreasing ROS levels from 160 to 103 %. The NO production was measured by the formation of nitrite (Fig. 3b). The treatment of astrocytes with LPS caused a significant increase in NO levels (65 %) compared to control conditions. Resveratrol totally inhibited the LPS-induced production of NO. In the presence of HO-1 inhibitor, resveratrol did not prevent the ROS nor NO overproduction induced by LPS in astrocytes.
Effects of resveratrol on ROS production and nitrite levels. Cells were incubated for 1 h with 100 µM resveratrol (RSV), followed by the addition of 10 μg/ml LPS for 3 h in serum-free DMEM/F12. 10 μM ZnPP IX was coincubated with resveratrol. a ROS production and b nitrite levels were measured as described in the “Materials and Methods” section. Data represent the mean ± S.E.M of four independent experimental determinations performed in triplicate and differences among groups were statistically analyzed using two-way ANOVA, followed by Tukey’s test. Values of P < 0.05 were considered significant. a indicates differences from control conditions and b differences from LPS
As shown in Fig. 4, LPS decreased GSH levels (30 %) compared to control. Resveratrol prevented this effect. In addition, resveratrol alone increased GSH basal levels by about 20 %. The HO-1 inhibitor abolished the effect of resveratrol on GSH content.
Effects of resveratrol on GSH levels. Cells were incubated for 1 h with 100 µM resveratrol (RSV), followed by the addition of 10 μg/ml LPS for 3 h in serum-free DMEM/F12. 10 μM ZnPP IX was coincubated with resveratrol. GSH levels were measured as described in the “Materials and Methods” section. Data represent the mean ± S.E.M of three independent experimental determinations performed in triplicate and differences among groups were statistically analyzed using two-way ANOVA, followed by Tukey’s test. Values of P < 0.05 were considered significant. a indicates differences from control conditions and b differences from LPS
Discussion
The results of this study showed that resveratrol could protect hippocampal primary astrocytes from LPS-induced inflammatory response and oxidative stress. The effect of resveratrol seems to be mediated by HO-1 cascade, which is an upstream of NFκB, a transcription factor associated to inflammatory response and oxidative stress [44, 50]. Additionally, resveratrol increased the effects of p38 and ERK signaling pathways on the transcriptional activity of NFκB and, consequently, proinflammatory cytokines release after LPS challenge. Resveratrol emerges as an anti-inflammatory molecule, because inhibits the cascade of proinflammatory factors, including NO, iNOS, PGE2 and COX as well as inflammatory mediators, such as TNF-α and interleukins [11, 14, 24, 51]. In this sense, our results reinforce the role of resveratrol in the attenuation of inflammatory response in the CNS.
The effects of resveratrol in the CNS have been studied in a variety of pathological events, including stroke, Alzheimer’s and Parkinson’s diseases [21]. The pathophysiology of these disorders is complex and strongly associated to neuroinflammation. In this sense, astrocytes are thought of as active cells in the immune response, because they have TLR4 and secrete anti- and proinflammatory cytokines [8, 13]. Herein, after LPS challenge, we observed an increase in proinflammatory cytokines, such as TNF-α, IL-1β, IL-6 and IL-18, which are down-regulated by resveratrol.
TNF-α is synthesized mainly by microglia and astrocytes, and has several important functions in the CNS, including astrocytes activation [52]. TNF-α and IL-1β, classical proinflammatory cytokines, act since acute inflammatory response and are essential for the production of IL-6 [52]. This cytokine is also produced by microglia and astrocytes, and plays a pivotal role in pathological brain inflammation. Furthermore, IL-18 (a member of IL-1 superfamily) induces inflammatory process and is directly associated to neurodegenerative diseases [53, 54]. In addition, resveratrol per se modulated IL-10, an anti-inflammatory cytokine, capable to induce resistance against brain damage, such as ischemia and subsequent inflammation [55]. Moreover, the anti-inflammatory effect of IL-10 is related to inhibition of TNF-α secretion [56]. IL-10 is also capable to exert rapid neuroprotection through modulation of intracellular calcium and mediates delayed effects via NFκB [55, 57]. These events may explain the absence of changes in IL-10 after LPS exposure.
NFκB is considered the major inflammatory mediator in the CNS; however, its mechanism of activation and subsequent translocation into the nucleus are not completely understood [44, 50]. Concerning to resveratrol neuroprotection, this compound protected neurons against LPS-induced neuronal death via NFκB signaling pathway inhibition [58]. In this study, we reported that resveratrol was able to inhibit NFκB p65 nuclear levels and we also focused on testing a mechanistic hypothesis whether the attenuation of proinflammatory cytokines release by resveratrol was through HO-1 signaling, an upstream of NFκB. In this sense, the copresence of HO-1 inhibitor blocked the positive effects of resveratrol in hippocampal astrocytes. HO-1 has been proposed as a candidate by which resveratrol can induce neuroprotective effect and our previous data supported this theory. Increases in HO-1 activity are associated with protection against stressful conditions, such as oxidative stress, inflammation and hypoxia [22, 34].
MAPK pathway is associated to inflammatory response and oxidative stress and p38 MAPK controls the NFκB translocation [9]. Thus p38 presents an upstream action on LPS-induced cytokine release. p38 MAPK attenuation has been reported to contribute to neuroprotection and MAPK inhibitors have emerged as attractive anti-inflammatory drugs. In this sense, resveratrol increased the effect of MAPK inhibitor [59]. ERK1/2 pathway has also been implicated in the regulation of glial inflammatory response following an insult and is another upstream signal transduction of NFκB [24, 60]. Here, we demonstrated that resveratrol improved the action of MEK/ERK inhibitor, indicating that inactivation may represent a novel anti-inflammatory mechanism of resveratrol. Our findings are supported by Lee et al. [15, 60], who demonstrated that resveratrol protected hippocampal slice cultures via inhibition of ERK1/2 pathway.
There is accumulating evidence that resveratrol decreases oxidative and nitrosative stress, including in inflammatory conditions [11, 61]. Although, the precise mechanisms by which resveratrol exerts its effects were not established, is possible that resveratrol may exert its effects by direct antioxidant/scavenger activity or may trigger molecular signaling through HO-1. In line with this, HO-1 is able to scavenge NO and block iNOS activity, to prevent further NO production. Additionally, proinflammatory cytokines release from LPS challenge may increase the levels of NO as well as NFκB activation levels stimulating NO production, which may mediate oxidative damage through NO/ROS overproduction [44, 61, 62]. Several reports indicate that resveratrol decreased iNOS expression and our recent publication showed that this effect was dependent of HO-1 pathway [21, 22, 32]. Thus, we demonstrated that resveratrol decreased NFκB levels via HO-1 signaling pathway and, consequently, this inhibition may be associated to attenuation in inflammatory response and oxidative stress.
As possible consequence of oxidative and nitrosative stress induced by LPS, we observed a decrease in GSH content. In addition, Lee et al. [15, 60] demonstrated that the depletion of GSH in glial cells induces inflammatory response. There is not a consensus whether inflammation induces oxidative stress or vice versa, since TLR4 cascade is involved in both events [63]. In this sense, ROS overproduction is able to increase TNF-α levels [64, 65]. Our results show that resveratrol prevented the LPS-induced GSH content decrease through HO-1. It is important to note that Nrf-2, a transcription factor, regulates HO-1 biosynthesis and also mediates neuroprotection modulating several detoxification genes that encode antioxidant proteins, such as GSH system [66, 67]. Resveratrol activates Nrf-2 and modulates direct or indirectly GSH in glial cells [43]. Moreover, astrocytes are the main supplier of GSH to the CNS [6]. Because the depletion of GSH can induce neuroinflammation and neurotoxicity [15], our results improve the knowledge about the neuroprotective action of resveratrol.
In summary, this report provides the first mechanistic explanation for the protective effect of resveratrol against LPS in hippocampal astrocytes. There is a close relationship between inflammatory response and antioxidant defense/oxidative stress, and HO-1 signaling pathway may control these events. Additionally, p38 and ERK were required for NFκB transcriptional activity as well as influenced the release of TNF-α and IL-1β after LPS exposure. Resveratrol was able to modulate NFκB, HO-1, p38 and ERK pathways. Thus, resveratrol emerging as an important focus for neuroprotection and our findings suggest that resveratrol may potentially be used as neuroprotective molecule, mainly by its antioxidant and anti-inflammatory effects.
References
Belanger M, Allaman I, Magistretti PJ (2011) Brain energy metabolism: focus on astrocyte-neuron metabolic cooperation. Cell Metab 14(6):724–738. doi:10.1016/j.cmet.2011.08.016
Maragakis NJ, Rothstein JD (2006) Mechanisms of disease: astrocytes in neurodegenerative disease. Nat Clin Pract Neurol 2(12):679–689. doi:10.1038/ncpneuro0355
He F, Sun YE (2007) Glial cells more than support cells? Int J Biochem Cell Biol 39(4):661–665. doi:10.1016/j.biocel.2006.10.022
Ransom BR, Ransom CB (2012) Astrocytes: multitalented stars of the central nervous system. Methods Mol Biol 814:3–7. doi:10.1007/978-1-61779-452-0_1
Parpura V, Heneka MT, Montana V, Oliet SH, Schousboe A, Haydon PG, Stout RF Jr, Spray DC, Reichenbach A, Pannicke T, Pekny M, Pekna M, Zorec R, Verkhratsky A (2012) Glial cells in (patho)physiology. J Neurochem 121(1):4–27. doi:10.1111/j.1471-4159.2012.07664.x
Hertz L, Zielke HR (2004) Astrocytic control of glutamatergic activity: astrocytes as stars of the show. Trends Neurosci 27(12):735–743. doi:10.1016/j.tins.2004.10.008
Allaman I, Belanger M, Magistretti PJ (2011) Astrocyte-neuron metabolic relationships: for better and for worse. Trends Neurosci 34(2):76–87. doi:10.1016/j.tins.2010.12.001
Farina C, Aloisi F, Meinl E (2007) Astrocytes are active players in cerebral innate immunity. Trends Immunol 28(3):138–145. doi:10.1016/j.it.2007.01.005
Gorina R, Font-Nieves M, Marquez-Kisinousky L, Santalucia T, Planas AM (2011) Astrocyte TLR4 activation induces a proinflammatory environment through the interplay between MyD88-dependent NFkappaB signaling, MAPK, and Jak1/Stat1 pathways. Glia 59(2):242–255. doi:10.1002/glia.21094
Rivest S (2009) Regulation of innate immune responses in the brain. Nat Rev Immunol 9(6):429–439. doi:10.1038/nri2565
Zong Y, Sun L, Liu B, Deng YS, Zhan D, Chen YL, He Y, Liu J, Zhang ZJ, Sun J, Lu D (2012) Resveratrol inhibits LPS-induced MAPKs activation via activation of the phosphatidylinositol 3-kinase pathway in murine RAW 264.7 macrophage cells. PLoS One 7(8):e44107. doi:10.1371/journal.pone.0044107
Guerra MC, Tortorelli LS, Galland F, Da Re C, Negri E, Engelke DS, Rodrigues L, Leite MC, Goncalves CA (2011) Lipopolysaccharide modulates astrocytic S100B secretion: a study in cerebrospinal fluid and astrocyte cultures from rats. J Neuroinflammation 8:128. doi:10.1186/1742-2094-8-128
Carpentier PA, Duncan DS, Miller SD (2008) Glial toll-like receptor signaling in central nervous system infection and autoimmunity. Brain Behav Immun 22(2):140–147. doi:10.1016/j.bbi.2007.08.011
Zhong LM, Zong Y, Sun L, Guo JZ, Zhang W, He Y, Song R, Wang WM, Xiao CJ, Lu D (2012) Resveratrol inhibits inflammatory responses via the mammalian target of rapamycin signaling pathway in cultured LPS-stimulated microglial cells. PLoS One 7(2):e32195. doi:10.1371/journal.pone.0032195
Lee M, Cho T, Jantaratnotai N, Wang YT, McGeer E, McGeer PL (2010) Depletion of GSH in glial cells induces neurotoxicity: relevance to aging and degenerative neurological diseases. FASEB J 24(7):2533–2545. doi:10.1096/fj.09-149997
Chang L, Karin M (2001) Mammalian MAP kinase signalling cascades. Nature 410(6824):37–40. doi:10.1038/35065000
Rigon AP, Cordova FM, Oliveira CS, Posser T, Costa AP, Silva IG, Santos DA, Rossi FM, Rocha JB, Leal RB (2008) Neurotoxicity of cadmium on immature hippocampus and a neuroprotective role for p38 MAPK. Neurotoxicology 29(4):727–734. doi:10.1016/j.neuro.2008.04.017
Bramanti V, Tomassoni D, Bronzi D, Grasso S, Curro M, Avitabile M, Li Volsi G, Renis M, Ientile R, Amenta F, Avola R (2010) Alpha-lipoic acid modulates GFAP, vimentin, nestin, cyclin D1 and MAP-kinase expression in astroglial cell cultures. Neurochem Res 35(12):2070–2077. doi:10.1007/s11064-010-0256-6
Baur JA, Sinclair DA (2006) Therapeutic potential of resveratrol: the in vivo evidence. Nat Rev Drug Discov 5(6):493–506. doi:10.1038/nrd2060
Fremont L (2000) Biological effects of resveratrol. Life Sci 66(8):663–673. doi:10.1016/S0024-3205(99)00410-5
Bastianetto S, Menard C, Quirion R (2014) Neuroprotective action of resveratrol. Biochim Biophys Acta. doi:10.1016/j.bbadis.2014.09.011
Quincozes-Santos A, Bobermin LD, Latini A, Wajner M, Souza DO, Goncalves CA, Gottfried C (2013) Resveratrol protects C6 astrocyte cell line against hydrogen peroxide-induced oxidative stress through heme oxygenase 1. PLoS One 8(5):e64372. doi:10.1371/journal.pone.0064372
Quincozes-Santos A, Gottfried C (2011) Resveratrol modulates astroglial functions: neuroprotective hypothesis. Ann N Y Acad Sci 1215:72–78. doi:10.1111/j.1749-6632.2010.05857.x
Bobermin LD, Quincozes-Santos A, Guerra MC, Leite MC, Souza DO, Goncalves CA, Gottfried C (2012) Resveratrol prevents ammonia toxicity in astroglial cells. PLoS One 7(12):e52164. doi:10.1371/journal.pone.0052164
Pervaiz S (2003) Resveratrol: from grapevines to mammalian biology. FASEB J 17(14):1975–1985. doi:10.1096/fj.03-0168rev
Delmas D, Jannin B, Latruffe N (2005) Resveratrol: preventing properties against vascular alterations and ageing. Mol Nutr Food Res 49(5):377–395. doi:10.1002/mnfr.200400098
Jang M, Cai L, Udeani GO, Slowing KV, Thomas CF, Beecher CW, Fong HH, Farnsworth NR, Kinghorn AD, Mehta RG, Moon RC, Pezzuto JM (1997) Cancer chemopreventive activity of resveratrol, a natural product derived from grapes. Science 275(5297):218–220. doi:10.1126/science.275.5297.218
Baur JA, Pearson KJ, Price NL, Jamieson HA, Lerin C, Kalra A, Prabhu VV, Allard JS, Lopez-Lluch G, Lewis K, Pistell PJ, Poosala S, Becker KG, Boss O, Gwinn D, Wang M, Ramaswamy S, Fishbein KW, Spencer RG, Lakatta EG, Le Couteur D, Shaw RJ, Navas P, Puigserver P, Ingram DK, de Cabo R, Sinclair DA (2006) Resveratrol improves health and survival of mice on a high-calorie diet. Nature 444(7117):337–342. doi:10.1038/nature05354
Bellaver B, de Souza DG, Souza DO, Quincozes-Santos A (2013) Resveratrol increases antioxidant defenses and decreases proinflammatory cytokines in hippocampal astrocyte cultures from newborn, adult and aged Wistar rats. Toxicol In Vitro 28(4):479–484. doi:10.1016/j.tiv.2014.01.006
Tiwari V, Chopra K (2011) Resveratrol prevents alcohol-induced cognitive deficits and brain damage by blocking inflammatory signaling and cell death cascade in neonatal rat brain. J Neurochem 117(4):678–690. doi:10.1111/j.1471-4159.2011.07236.x
Khan MM, Ahmad A, Ishrat T, Khan MB, Hoda MN, Khuwaja G, Raza SS, Khan A, Javed H, Vaibhav K, Islam F (2010) Resveratrol attenuates 6-hydroxydopamine-induced oxidative damage and dopamine depletion in rat model of Parkinson’s disease. Brain Res 1328:139–151. doi:10.1016/j.brainres.2010.02.031
Huang TC, Lu KT, Wo YY, Wu YJ, Yang YL (2011) Resveratrol protects rats from Abeta-induced neurotoxicity by the reduction of iNOS expression and lipid peroxidation. PLoS One 6(12):e29102. doi:10.1371/journal.pone.0029102
Wu Z, Xu Q, Zhang L, Kong D, Ma R, Wang L (2009) Protective effect of resveratrol against kainate-induced temporal lobe epilepsy in rats. Neurochem Res 34(8):1393–1400. doi:10.1007/s11064-009-9920-0
Sakata Y, Zhuang H, Kwansa H, Koehler RC, Dore S (2010) Resveratrol protects against experimental stroke: putative neuroprotective role of heme oxygenase 1. Exp Neurol 224(1):325–329. doi:10.1016/j.expneurol.2010.03.032
Frozza RL, Bernardi A, Hoppe JB, Meneghetti AB, Battastini AM, Pohlmann AR, Guterres SS, Salbego C (2013) Lipid-core nanocapsules improve the effects of resveratrol against Abeta-induced neuroinflammation. J Biomed Nanotechnol 9(12):2086–2104. doi:10.1166/jbn.2013.1709
Frozza RL, Bernardi A, Hoppe JB, Meneghetti AB, Matte A, Battastini AM, Pohlmann AR, Guterres SS, Salbego C (2013) Neuroprotective effects of resveratrol against Abeta administration in rats are improved by lipid-core nanocapsules. Mol Neurobiol 47(3):1066–1080. doi:10.1007/s12035-013-8401-2
Quincozes-Santos A, Nardin P, de Souza DF, Gelain DP, Moreira JC, Latini A, Goncalves CA, Gottfried C (2009) The janus face of resveratrol in astroglial cells. Neurotox Res 16(1):30–41. doi:10.1007/s12640-009-9042-0
dos Santos AQ, Nardin P, Funchal C, de Almeida LM, Jacques-Silva MC, Wofchuk ST, Goncalves CA, Gottfried C (2006) Resveratrol increases glutamate uptake and glutamine synthetase activity in C6 glioma cells. Arch Biochem Biophys 453(2):161–167. doi:10.1016/j.abb.2006.06.025
de Almeida LM, Pineiro CC, Leite MC, Brolese G, Tramontina F, Feoli AM, Gottfried C, Goncalves CA (2007) Resveratrol increases glutamate uptake, glutathione content, and S100B secretion in cortical astrocyte cultures. Cell Mol Neurobiol 27(5):661–668. doi:10.1007/s10571-007-9152-2
Vieira de Almeida LM, Pineiro CC, Leite MC, Brolese G, Leal RB, Gottfried C, Goncalves CA (2008) Protective effects of resveratrol on hydrogen peroxide induced toxicity in primary cortical astrocyte cultures. Neurochem Res 33(1):8–15. doi:10.1007/s11064-007-9399-5
Bramanti V, Tomassoni D, Grasso S, Bronzi D, Napoli M, Campisi A, Li Volti G, Ientile R, Amenta F, Avola R (2012) Cholinergic precursors modulate the expression of heme oxigenase-1, p21 during astroglial cell proliferation and differentiation in culture. Neurochem Res 37(12):2795–2804. doi:10.1007/s11064-012-0873-3
Dore S (2005) Unique properties of polyphenol stilbenes in the brain: more than direct antioxidant actions; gene/protein regulatory activity. Neurosignals 14(1–2):61–70. doi:10.1159/000085386
Calabrese V, Cornelius C, Mancuso C, Pennisi G, Calafato S, Bellia F, Bates TE, Giuffrida Stella AM, Schapira T, Dinkova Kostova AT, Rizzarelli E (2008) Cellular stress response: a novel target for chemoprevention and nutritional neuroprotection in aging, neurodegenerative disorders and longevity. Neurochem Res 33(12):2444–2471. doi:10.1007/s11064-008-9775-9
Wakabayashi N, Slocum SL, Skoko JJ, Shin S, Kensler TW (2010) When NRF2 talks, who’s listening? Antioxid Redox Signal 13(11):1649–1663. doi:10.1089/ars.2010.3216
Bellaver B, Souza DG, Souza DO, Quincozes-Santos A (2014) Resveratrol increases antioxidant defenses and decreases proinflammatory cytokines in hippocampal astrocyte cultures from newborn, adult and aged Wistar rats. Toxicol In Vitro 28(4):479–484. doi:10.1016/j.tiv.2014.01.006
Quincozes-Santos A, Bobermin LD, Souza DG, Bellaver B, Goncalves CA, Souza DO (2014) Guanosine protects C6 astroglial cells against azide-induced oxidative damage: a putative role of heme oxygenase 1. J Neurochem 130(1):61–74. doi:10.1111/jnc.12694
Quincozes-Santos A, Bobermin LD, de Souza DG, Bellaver B, Goncalves CA, Souza DO (2013) Gliopreventive effects of guanosine against glucose deprivation in vitro. Purinergic Signal. doi:10.1007/s11302-013-9377-0
Browne RW, Armstrong D (1998) Reduced glutathione and glutathione disulfide. Methods Mol Biol 108:347–352. doi:10.1385/0-89603-472-0:347
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193(1):265–275
Gloire G, Legrand-Poels S, Piette J (2006) NF-kappaB activation by reactive oxygen species: fifteen years later. Biochem Pharmacol 72(11):1493–1505. doi:10.1016/j.bcp.2006.04.011
Bi XL, Yang JY, Dong YX, Wang JM, Cui YH, Ikeshima T, Zhao YQ, Wu CF (2005) Resveratrol inhibits nitric oxide and TNF-alpha production by lipopolysaccharide-activated microglia. Int Immunopharmacol 5(1):185–193. doi:10.1016/j.intimp.2004.08.008
Tanabe K, Matsushima-Nishiwaki R, Yamaguchi S, Iida H, Dohi S, Kozawa O (2010) Mechanisms of tumor necrosis factor-alpha-induced interleukin-6 synthesis in glioma cells. J Neuroinflammation 7:16. doi:10.1186/1742-2094-7-16
de Rivero Vaccari JP, Dietrich WD, Keane RW (2014) Activation and regulation of cellular inflammasomes: gaps in our knowledge for central nervous system injury. J Cereb Blood Flow Metab 34(3):369–375. doi:10.1038/jcbfm.2013.227
Bossu P, Ciaramella A, Salani F, Vanni D, Palladino I, Caltagirone C, Scapigliati G (2010) Interleukin-18, from neuroinflammation to Alzheimer’s disease. Curr Pharm Des 16(38):4213–4224. doi:10.2174/138161210794519147
Tukhovskaya EA, Turovsky EA, Turovskaya MV, Levin SG, Murashev AN, Zinchenko VP, Godukhin OV (2014) Anti-inflammatory cytokine interleukin-10 increases resistance to brain ischemia through modulation of ischemia-induced intracellular Ca(2)(+) response. Neurosci Lett 571:55–60. doi:10.1016/j.neulet.2014.04.046
Green HF, Nolan YM (2012) GSK-3 mediates the release of IL-1beta, TNF-alpha and IL-10 from cortical glia. Neurochem Int 61(5):666–671. doi:10.1016/j.neuint.2012.07.003
Hu D, Wan L, Chen M, Caudle Y, LeSage G, Li Q, Yin D (2014) Essential role of IL-10/STAT3 in chronic stress-induced immune suppression. Brain Behav Immun 36:118–127. doi:10.1016/j.bbi.2013.10.016
Zhang F, Shi JS, Zhou H, Wilson B, Hong JS, Gao HM (2010) Resveratrol protects dopamine neurons against lipopolysaccharide-induced neurotoxicity through its anti-inflammatory actions. Mol Pharmacol 78(3):466–477. doi:10.1124/mol.110.064535
Collino M, Aragno M, Mastrocola R, Benetti E, Gallicchio M, Dianzani C, Danni O, Thiemermann C, Fantozzi R (2006) Oxidative stress and inflammatory response evoked by transient cerebral ischemia/reperfusion: effects of the PPAR-alpha agonist WY14643. Free Radic Biol Med 41(4):579–589. doi:10.1016/j.freeradbiomed.2006.04.030
Lee EO, Park HJ, Kang JL, Kim HS, Chong YH (2010) Resveratrol reduces glutamate-mediated monocyte chemotactic protein-1 expression via inhibition of extracellular signal-regulated kinase 1/2 pathway in rat hippocampal slice cultures. J Neurochem 112(6):1477–1487. doi:10.1111/j.1471-4159.2009.06564.x
Lu X, Ma L, Ruan L, Kong Y, Mou H, Zhang Z, Wang Z, Wang JM, Le Y (2010) Resveratrol differentially modulates inflammatory responses of microglia and astrocytes. J Neuroinflammation 7:46. doi:10.1186/1742-2094-7-46
Kakita H, Aoyama M, Hussein MH, Kato S, Suzuki S, Ito T, Togari H, Asai K (2009) Diclofenac enhances proinflammatory cytokine-induced nitric oxide production through NF-kappaB signaling in cultured astrocytes. Toxicol Appl Pharmacol 238(1):56–63. doi:10.1016/j.taap.2009.04.014
Okun E, Griffioen KJ, Mattson MP (2011) Toll-like receptor signaling in neural plasticity and disease. Trends Neurosci 34(5):269–281. doi:10.1016/j.tins.2011.02.005
Shen HM, Pervaiz S (2006) TNF receptor superfamily-induced cell death: redox-dependent execution. FASEB J 20(10):1589–1598. doi:10.1111/j.1471-4159.2009.06564.x
Hamby ME, Gragnolati AR, Hewett SJ, Hewett JA (2008) TGF beta 1 and TNF alpha potentiate nitric oxide production in astrocyte cultures by recruiting distinct subpopulations of cells to express NOS-2. Neurochem Int 52(6):962–971. doi:10.1016/j.neuint.2007.10.010
Arredondo F, Echeverry C, Abin-Carriquiry JA, Blasina F, Antunez K, Jones DP, Go YM, Liang YL, Dajas F (2010) After cellular internalization, quercetin causes Nrf2 nuclear translocation, increases glutathione levels, and prevents neuronal death against an oxidative insult. Free Radic Biol Med 49(5):738–747. doi:10.1016/j.freeradbiomed.2010.05.020
Calkins MJ, Johnson DA, Townsend JA, Vargas MR, Dowell JA, Williamson TP, Kraft AD, Lee JM, Li J, Johnson JA (2009) The Nrf2/ARE pathway as a potential therapeutic target in neurodegenerative disease. Antioxid Redox Signal 11(3):497–508. doi:10.1089/ARS.2008.2242
Acknowledgments
This work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (FAPERGS), Financiadora de Estudos e Projetos (FINEP)—IBN Net (Instituto Brasileiro de Neurociências) 01.06.0842-00, Federal University of Rio Grande do Sul (UFRGS) and Instituto Nacional de Ciência e Tecnologia para Excitotoxicidade e Neuroproteção (INCTEN/CNPq), Brazil.
Conflict of interest
The authors declare there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bellaver, B., Souza, D.G., Bobermin, L.D. et al. Resveratrol Protects Hippocampal Astrocytes Against LPS-Induced Neurotoxicity Through HO-1, p38 and ERK Pathways. Neurochem Res 40, 1600–1608 (2015). https://doi.org/10.1007/s11064-015-1636-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-015-1636-8