Abstract
Alzheimer’s disease (AD), a neurodegenerative disorder exhibiting a gradual decline in cognitive function, is characterized by the presence of neuritic plaques composed of neurofibrillary tangles and amyloid-β (Aβ) peptide. Available drugs for AD therapy have small effect sizes and do not alter disease progression. Several studies have been shown that resveratrol is associated with anti-amyloidogenic properties, but therapeutic application of its beneficial effects is limited. Here we compared the neuroprotective effects of free resveratrol treatment with those of resveratrol-loaded lipid-core nanocapsule treatment against intracerebroventricular injection of Aβ1-42 in rats. Animals received a single intracerebroventricular injection of Aβ1-42 (2 nmol), and 1 day after Aβ infusion, they were administered either free resveratrol (RSV) or resveratrol-loaded lipid-core nanocapsules (5 mg/kg, each 12 h, intraperitoneally), for 14 days. Aβ1-42-infused animals showed a significant impairment on learning memory ability, which was paralleled by a significant decrease in hippocampal synaptophysin levels. Furthermore, animals exhibited activated astrocytes and microglial cells, as well as disturbance in c-Jun N-terminal kinase (JNK) and glycogen synthase kinase-3β (GSK-3β) activation, beyond destabilization of β-catenin levels. Our results clearly show that by using lipid-core nanocapsules, resveratrol was able to rescue the deleterious effects of Aβ1-42 while treatment with RSV presented only partial beneficial effects. These findings might be explained by the robust increase of resveratrol concentration in the brain tissue achieved by lipid-core nanocapsules. Our data not only confirm the potential of resveratrol in treating AD but also offer an effective way to improve the efficiency of resveratrol through the use of nanodrug delivery systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is an aged-related neurodegenerative disease clinically characterized by progressive cognitive decline associated with progressive memory loss, spatial disorientation, and impairment in activities of daily living throughout the disease course. The major neuropathological lesions of AD include intracellular neurofibrillary tangles, which are paired helical filaments of hyperphosphorylated tau proteins, extracellular deposits of fibrillar amyloid-β (Aβ) peptide in senile plaques, and the build-up of soluble Aβ oligomers [1, 2]. The deposition of Aβ in brain areas involved in cognitive functions is assumed to initiate an array of molecular and cellular cascades that eventually lead to synaptic dysfunction, synaptic loss, and neuronal death [3]. However, mechanistic molecular processes that link Aβ and neurodegeneration remain to be firmly established. Genetic factors which present as dominant mutations account for the few cases of family-oriented early onset AD.
Available drugs for AD therapy have small effect sizes and do not alter disease progression. Given the current absence of disease-modifying treatments, there has been growing interest in the identification of effective strategies for the prevention of AD. Furthermore, the presence of a blood–brain barrier (BBB) presents a huge challenge for effective entry of the majority of drugs and, thus, severely restricts the therapy of many diseases affecting the central nervous systems (CNS), including AD. Since the majority of drugs and large molecular weight particulate agents do not readily permeate into brain parenchyma, one of the most significant challenges facing CNS drug development is the availability of effective brain drug targeting technology [4]. Therefore, the application of technological advances in neurological research is expected to have a major impact leading to the development of newer therapeutic modalities [5]. Nanotechnology is at the core of biotechnology and it is likely to play a significant role in this regard. In this way, nanoparticles have become an important area of research in the field of drug delivery because they have the ability to deliver a wide range of drugs to various areas of the body for a sustained period of time [6].
Nanoparticles are polymeric particles made of natural or synthetic polymers ranging size from 1 to 1,000 nm [7]. The drugs may be dissolved into the nanoparticles, entrapped, encapsulated, and/or adsorbed or attached. Several authors have delivered a variety of drugs using nanoparticles as carriers (reviewed by [6]). Furthermore, the development of new practical treatment modalities for the therapy of neurodegenerative diseases is currently a highly active area of research [5], and the literature suggests that novel nanoparticles could be used as potential drug carriers across the BBB [5, 8–10]. The mechanisms of encapsulation and release of several drugs from nanoparticulated systems have been extensively studied by our group [11–14]. Moreover, we have already shown that lipid-core nanocapsules were able to deliver drugs into the brain in rats [15–17].
Epidemiological studies have suggested that moderate wine intake reduces the risk of developing AD [18–20]. Resveratrol (3,5,4′-trihydroxystilbene) is a non-flavonoid polyphenolic compound that occurs in abundance in grapes, red wine, and other foods that are commonly consumed as part of the human diet, and it is suspected to afford antioxidant and neuroprotective properties and therefore to contribute to the beneficial effect of wine consumption on the neurodegenerative process [21, 22]. Resveratrol presents a wide range of pharmacological properties including inhibition of oxidation of human low-density lipoprotein, suppression of cyclooxygenase-2 and inducible nitric oxide syntase (iNOS) activities, and anti-inflammatory and antioxidant effects [23]. Recently, it has been shown that this polyphenol is associated with anti-amyloidogenic properties in vitro and in vivo [20, 24–26]. Furthermore, resveratrol presents chemopreventive effects [27] and increases the activity of SIRT, a member of the sirtuin family of nicotinamide adenine dinucleotide-dependent deacetylases [28, 29], resulting in improved cellular stress resistance and longevity [30].
However, the therapeutic application of these beneficial effects of resveratrol remains very limited due to its poor solubility, photosensitivity, short biological half-life, and rapid metabolism and elimination, meaning very low bioavailability [23, 31]. The extensive metabolism of resveratrol leads to the formation of various glucuronide and sulfate conjugates of unknown potential biological activities. In this way, the development of the therapeutic potential of resveratrol can only be applied in vivo if the limitations tied to its bioavailability can be overcome. In this context, an increasing number of recent studies have aimed at designing novel resveratrol formulations to overcome these limitations (reviewed in [32]). Recently, we developed a resveratrol-loaded lipid-core nanocapsule formulation in an attempt to stabilize the drug, preserve its biological activities, and improve its bioavailability. Additionally, we found that healthy rats treated with these lipid-core nanocapsules showed significantly higher concentrations of resveratrol in the brain when compared to rats treated with free resveratrol even after gavage administration [16].
Although many studies have reported the protective effects of resveratrol against Aβ, the mechanisms underlying these neuroprotective effects still remain to be determined. Thereby, the present study evaluated the ability of resveratrol to protect against Aβ1-42-induced synaptotoxicity and memory impairment and investigated some underlying mechanisms. Furthermore, we compared the neuroprotective effects of free resveratrol treatment to the effects displayed by resveratrol-loaded lipid-core nanocapsule treatment against intracerebroventricular injection of Aβ1-42 in rats.
Materials and Methods
Preparation of Lipid-Core Nanocapsules
Lipid-core nanocapsule suspensions were prepared by interfacial deposition of the polymer as previously described [16, 33]. At 40 °C, trans-resveratrol (0.05 g) (Gerbras, Anápolis, GO, Brazil), poly(ε-caprolactone) (0.50 g) (MW = 65,000, Aldrich, Strasbourg, France), capric/caprylic triglyceride (1.650 mL) (Delaware, Porto Alegre, Brazil), and sorbitan monostearate (0.19 g) (Sigma Chemical Co., St. Louis, MO, USA) were dissolved in acetone (135 mL) (Merck, Darmstadt, Germany). In a separate flask, polysorbate 80 (0.19 g) (Delaware) was added to 265 mL of water (MilliQ®). The organic solution was injected into the aqueous phase under magnetic stirring at room temperature. After 10 min, the acetone was evaporated and the suspensions were concentrated under reduced pressure at 40 °C. The final volume was adjusted to 50 mL (MilliQ® water). A control formulation (load-off lipid-core nanocapsules—LNC) was prepared, as described above, without trans-resveratrol.
Physicochemical Characterization of the Formulations
The pH values of the suspensions were determined using a potentiometer B-474 (Micronal, Brazil). Mean diameters (z-average), polydispersity index, and zeta potential were measured at 25 °C using a Zetasizer®nano-ZS ZEN 3600 model (Nanoseries, Malvern, UK), after diluting the samples with MilliQ® water or with 0.01 mol/L NaCl aqueous solution, respectively. To avoid any sample selection, only the dilution media was filtered (Millipore® 0.45 μm) prior to analysis. Measurements were carried out using three different batches for each formulation in triplicate to assure accuracy. The size and polydispersity indexes were calculated using the software (Dispersion Technology Software—DTS Nano—Version 5.02, Malvern) provided by the manufacturer (Malvern Instruments Ltd).
Analytical Procedure
Resveratrol was analyzed by high-performance liquid chromatography (HPLC) at 306 nm. The content (total concentration) of resveratrol in the formulations (100 μL) was determined after dissolving the lipid-core nanocapsules containing resveratrol into acetonitrile (10 mL) (Tedia Company Inc., OH, USA) and filtering (Millipore® 0.45 μm) for analysis. The system consisted of a UV–Vis detector, pump and auto-injector S200 Perkin-Elmer (PerkinElmer Instruments, Norwalk, CT, USA), and a Shim-pack CLC-C8 (M) column (150 mm, 4.6 mm, 5 μm, Shimadzu Corporation, Japan) with a guard column. The mobile phase was prepared by using Milli-Q® water and HPLC grade acetonitrile and consisted of acetonitrile/water (40:60 v/v) with a pH of 3.0 ± 0.5 corrected with 10 % (v/v) orthophosphoric acid. The isocratic flow rate of the mobile phase was 1.2 mL/min and the retention time of resveratrol was 3.45 min. The HPLC method was validated presenting linearity between 2.5 and 17.5 μg/mL (r > 0.9999), inter- and intraday variability lower than 2.0 %, and accuracy from 96.19 to 97.21 %. The encapsulation efficiency was determined by ultrafiltration–centrifugation technique (Ultrafree-MC 10,000 MW, Millipore), at 15,300×g for 10 min. The associated resveratrol within the nanocapsules was calculated from the difference between the total and the free drug concentrations determined in the nanocapsule suspension and in the ultrafiltrate, respectively.
Peptide Preparation
The Aβ1-42 peptide (Bachem Americas Inc. Torrance, CA, USA) or the inactive control Aβ42-1 peptide (American Peptide Co., Sunnyvale, CA, USA) was dissolved in sterilized bi-distilled water with 0.1 % ammonium hydroxide (Merck) at a concentration of 1 mg/mL and stored at −20 °C. Aliquots of Aβ peptides were allowed to aggregate by incubation at 37 °C for 72 h before in vivo infusion.
Animals
Male adult Wistar rats (300–350 g) were obtained from in-house breeding colonies at the Departamento de Bioquímica, Universidade Federal do Rio Grande do Sul (UFRGS, Porto Alegre, Brazil). Animals were housed in cages under optimum light conditions (12:12 h light–dark cycle), temperature (22 ± 1 °C), and humidity (50 to 60 %), with food and water provided ad libitum. All procedures used in the present study followed the “Principles of Laboratory Animal Care” from NIH publication No. 85–23 and were approved by the local Ethics Committee on the Use of Animals (CEP-UFRGS, protocol number 2007977). All efforts were made to minimize the number of animals and their suffering.
Surgical Procedure
Animals were anesthetized with Equithesin (3.5 mL/kg intraperitoneally—i.p.) and placed in a stereotaxic frame. After sterilized using standard procedures, a middle sagittal incision was made in the scalp. Bilateral holes were drilled in the skull using a dental drill over the lateral ventricles. Injection coordinates were chosen according to the atlas of Paxinos and Watson [34]: 0.8 mm posterior to bregma, 1.5 mm lateral to the saggital suture, and 3.5 mm beneath the surface of brain. Rats received a single infusion of 5 μL into each lateral ventricle of Aβ1-42 or Aβ42-1 (total of 2 nmol in 10 μL). Controls animals received bilateral intracerebroventricular (i.c.v.) injections of equal volume of bi-distilled water with 0.1 % ammonium hydroxide. Microinjections were performed using a 10-μL Hamilton syringe fitted with a 26-gauge needle. All infusions were made at a rate of 1 μL/min over a period of 5 min. At the end of infusion, the needle was left in place for an additional 3–5 min before being slowly withdrawn to allow diffusion from the tip and prevent reflux of the solution. After the injection, the scalp was sutured and the animals were allowed to recover from the anesthesia on a heating pad to maintain body temperature at 37.5 ± 0.5 °C. The animals were submitted to behavioral tasks 2 weeks after Aβ injection.
Drug Administration
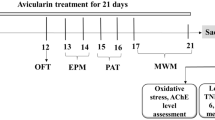
The experimental schedule is shown in Fig. 1. One day after the surgical procedure, the animals were randomly divided into eight groups. Control animals infused i.c.v. with water plus 0.1 % ammonium hydroxide (Aβ-vehicle) were split into the following three groups: (1) untreated (control group), (2) treated with free resveratrol (RSV group), and (3) treated with resveratrol-loaded lipid-core nanocapsules (RSV-LNC). Animals infused i.c.v. with Aβ1-42 were divided into the following groups: (4) untreated (Aβ group), (5) treated with ethanol 50 % (Aβ EtOH group), (6) treated with load-off lipid-core nanocapsules (Aβ LNC group), (7) treated with free resveratrol (Aβ RSV group), and (8) treated with resveratrol-loaded lipid-core nanocapsules (Aβ RSV-LNC group). Animals injected with Aβ42-1 received no treatment and completed behavioral tasks 2 weeks after Aβ injection.
Free resveratrol (RSV) was dissolved in ethanol 50 % (EtOH) at a concentration of 1 mg/mL. This solution was freshly made up for each administration, and lipid-core nanocapsules containing resveratrol (RSV-LNC) suspended in MilliQ® water were prepared as described above. Daily, doses reaching 10 mg/kg/day of RSV and RSV-LNC, divided in two administrations of 5 mg/kg each 12 h, were administered i.p. to the animals for 14 consecutives days. Similarly, vehicle-treated groups (EtOH 50 % and LNC, respectively) with identical volumes to those treated with RSV or RSV-LNC were run in parallel in rats infused with Aβ. The behavior tests were started on day 13 after Aβ infusion and were carried out sequentially.
Behavioral Analysis
Spontaneous Alternation. Hippocampal-dependent memory performance was assessed by measuring spontaneous alternation performance during 8 min in the Y-maze test, which evaluates cognitive searching behavior, although it does not allow isolating memory performance (reviewed in [35]). Spontaneous alternation behavior is considered to reflect spatial working memory, which is a form of short-term memory. The experimental apparatus used in the present study consisted of three arms (40 cm long, 25 cm high, and 10 cm wide, labeled A, B, and C) constructed of plywood and painted black with an equilateral triangular central area. This apparatus was used in a testing room with constant illumination. Each rat was placed at the end of one arm and allowed to move freely through the apparatus for 8 min. Behavior was recorded by a video camera mounted vertically above the test arena for later analysis using a video-tracking software (ANY-maze®, Stoelting Co., USA). The number of arm choices and pattern of choices were recorded for each animal. An arm entry was counted when the hind paws of the rat were completely within the arm. Spontaneous alternation behavior was defined as entry into all three arms on consecutive choices in overlapping triplet sets (i.e., ABC, BCA, CBA). The percentage of alternation was calculated as [total alternations / (total arm entries − 2) × 100].
Novel Object Recognition Task. The object recognition task was performed following recently reviewed guidelines [36]. This task is based on the spontaneous tendency of rodents to explore novel objects [37]. The task was performed in an apparatus made of wood covered with impermeable Formica (dimensions, 40 × 50 × 50 cm) that had black floor and walls. The apparatus was used in a testing room with a constant illumination. The objects used in this test all had similar textures, colors, and sizes, but had different shapes. Objects were placed near the two corners at either end of one side of the apparatus. The objects chosen were two cuboid glass blocks, a cylindrical bottle filled with water, and a dodecahedron-shaped block. These objects were heavy enough to prevent the rats from moving them. A day before the tests, rats were submitted to a habituation session in which they were allowed to explore the apparatus for 5 min without objects. On the following day, rats were acclimated in the testing room during 1 h before the beginning of the sessions. First, rats completed a training session (24 h after habituation) that consisted of leaving the animals in the apparatus containing two identical objects (A and A1). After training, rats were placed in their home cages for 3 h. The testing session to evaluate short-term recognition memory was performed 3 h after the training session. Rats were once again allowed to explore the apparatus, but during this session, the apparatus contained two dissimilar objects: the familiar object from the training session and a novel one (A and B, respectively). Long-term recognition memory was evaluated 24 h after the training session and a different pair of dissimilar objects (a familiar and a novel one, A and C, respectively) were presented. In all sessions, each rat was always placed in the apparatus facing the wall and allowed to explore the objects for 5 min, after which the rat was returned to its home cage. Behavior was recorded by a video camera mounted vertically above the test arena and analyzed using appropriated video-tracking software (ANY-maze®). Each animal underwent three trials, including the training and two test sessions. The animals started to explore the objects 1 min after they had been placed in the apparatus. The percentage of time spent exploring the novel object was calculated as a function of the total amount of time spent exploring both objects during testing [time spent with novel object / (time spent with novel object + time spent with familiar object)]. A higher percentage of time spent exploring the novel object was considered to be an index of enhanced cognitive performance (recognition index). Between trials, the objects were cleaned with 10 % ethanol solution. Active exploration was defined by directing the nose to the object at a distance of no more than 2 cm and/or touching the object with the nose or forepaws. Sitting on the object was not considered exploratory behavior.
Western Blotting Assay
In order to evaluate any cell signaling disturbances triggered by i.c.v. injection of Aβ1-42 as well as resveratrol treatment, animals were killed by a lethal dosage of anesthesia following completion of the behavioral tasks and blood samples were collected by cardiac puncture. The brain was rapidly removed from the skull, and the hippocampus was dissected on dry ice. The hippocampi were then homogenized in ice-cold lysis buffer (4 % sodium dodecyl sulfate [SDS], 2 mM EDTA, 50 mM Tris) containing a protease inhibitor cocktail. The homogenates were denatured for 5 min at 100 °C, and then centrifuged at 10,000×g for 30 min. The supernatant containing the cytosolic fraction was collected, the protein concentration was determined [38], and β-mercaptoethanol was added to a final concentration of 5 %. Equal amounts of proteins were resolved (50 μg per lane) on 10 % SDS-PAGE. After electrophoresis, proteins were electro-transferred to nitrocellulose membranes (Hybond™ ECL™ nitrocellulose membrane, Amersham Biosciences, Freiburg, Germany) using a semi-dry transfer apparatus (Bio-Rad, Trans-Blot SD, Hercules, CA, USA). Membranes were incubated for 60 min at 4 °C in blocking solution (Tris-buffered saline containing 5 % non-fat milk and 0.1 % Tween-20, pH 7.4) and further incubated with the appropriate primary antibody dissolved in the blocking solution overnight at 4 °C. The primary antibodies against the following proteins were used: anti-phospho-β-catenin [pSer45] (1:1,000, Sigma Chemical Co.), anti-β-catenin (1:4,000, Sigma Chemical Co.), anti-glial fibrillary acidic protein (GFAP, 1:3,000, Sigma Chemical Co.), anti-phospho GSK-3β [pSer9] (1:1,000, Cell Signaling Technology, Beverly, MA, USA), anti-GSK-3β (1:1,000, Cell Signaling Technology), anti-phospho JNK1/2 [pTpY183/185] (pJNK, 1:1,000, Invitrogen, Grand Island, NY, USA), anti-JNK1/2 (1:500, Invitrogen), anti-synaptophysin (1:3,000, Millipore®, Bradford, MA, USA), and anti-β-actin (1:2,000, Sigma Chemical Co.). After washing, the membranes were incubated with adjusted secondary antibodies coupled to horseradish peroxidase (1:1,000, Amersham Pharmacia Biotech Piscataway, NJ, USA) for 2 h. The immunocomplexes were visualized by using Western blot detection SuperSignal West Pico chemiluminescent reagent (Pierce, Rockford, IL, USA). Band density measurements were performed by using Optiquant software (Packard Instrument). For each experiment, the test groups were compared to the control group not infused with Aβ.
Isolectin B4 (IB4) Reactivity
In an attempt to evaluate the activation of microglial cells after Aβ i.c.v. injection, we analyzed the IB4 (Sigma Chemical Co.) reactivity. Proteins (25 μg per line) were resolved on 8 % SDS-PAGE and electro-transferred to nitrocellulose membranes as described for the Western blotting assay. Membranes were incubated overnight at 4 °C in albumin solution (5 % albumin and 2 % Tween-20 in PBS, pH 7.4). After washing, IB4 peroxidase conjugate was incubated in PBS containing 0.05 % Tween-20 overnight in a final concentration of 0.250 μg/mL. Chemioluminescence was detected by Western blot detection SuperSignal West Pico chemiluminescent reagent (Pierce) using X-ray films (Kodak X-Omat, Rochester, NY, USA).
HPLC Analysis of Resveratrol Levels in the Brain
In order to determine the levels of resveratrol in the cerebral tissue, HPLC analysis was performed as has been described and validated previously [16]. Briefly, 1 h after the last i.p. injection, one group of animals was killed by a lethal dosage of anesthesia and blood samples were collected by cardiac puncture. The animals were perfused (0.9 % NaCl) to flush blood from the vascular system, the brain was weighed, and the hemispheres were separated. The right hemisphere was minced with scissors and placed in a homogenizer vessel; 5 mL of acetonitrile was added and tissues were subsequently homogenized. The homogenized samples were transferred to 50 mL conical glass tubes and vortexed for 5 min prior to centrifugation at 2,800×g for 30 min at 4 °C. The supernatant was placed into a clean tube, filtered (Millipore® 0.45 μm) and placed in a sealed amber vial for HPLC analysis. The injection volume used was 20 μL for all samples. The quantity of resveratrol was calculated by comparing the peak area ratio from tissue samples of treated animals with those of the corresponding concentration standards of trans-resveratrol in acetonitrile injected directly into the HPLC system.
Measurement of Hepatic Enzymes in Serum
In an attempt to evaluate whether treatments caused hepatic toxicity, the serum levels of hepatic enzymes were evaluated at the end of the treatments. The blood samples collected by cardiac puncture were analyzed by activities of hepatic enzymes γ-glutamyltransferase, alanine aminotransferase (ALT) and aspartate aminotransferase (AST), which were used as markers of metabolic and tissue toxicity. These experiments were performed in a LabMax 240 analyzer (Labtest Diagnostica, Brazil).
Data Analysis
All experiments were carried out at least in triplicate except for behavioral tests. The results are presented as the mean ± SD of 7 to 15 animals per group. The statistical comparisons of the data were performed by two-way analysis of variance (ANOVA) followed by Bonferroni post hoc test using GraphPad Prism software version 5.01 (GraphPad Software Inc., La Jolla, CA, USA). A p value lower than 0.05 (p < 0.05) was considered significant.
Results
Physicochemical Characterization of Lipid-Core Nanocapsules
The lipid-core nanocapsule formulations were prepared by interfacial polymer deposition and did not require subsequent purification. Resveratrol-loaded lipid-core nanocapsules (RSV-LNC) and load-off lipid-core nanocapsules (LNC) displayed macroscopic homogeneous features, appearing such as bluish-white opalescent liquids. After preparation, the RSV-LNC showed a mean particle size of 249 ± 5 nm, polydispersity index of 0.12 ± 0.05, zeta potential of −14 ± 1.8 mV, and pH of 5.5 ± 0.2. Similar results were obtained for LNC with 233 ± 4 nm, 0.15 ± 0.03, −13.6 ± 2.5 mV, and 5.2 ± 0.3, for particle size, polydispersity index, zeta potential, and pH values, respectively. The suspensions showed stable monomodal size distributions and polydispersity indexes lower than 0.15, indicating narrow size distributions. Resveratrol content was 0.964 ± 0.037 mg/mL and the encapsulation efficiency was 99.89 ± 1.3 % for all batches [16].
Effects of Resveratrol on Aβ1-42-Induced Memory Impairments
Since AD is characterized clinically by a progressive decline in learning and memory processes, spontaneous alternation and novel object recognition tasks were used to investigate behavioral impairments involved in Aβ-induced cognitive decline 14 days after rats were infused with Aβ1-42. Furthermore, we compared the effects of treatment with free resveratrol (RSV) to those of resveratrol-loaded lipid-core nanocapsules (RSV-LNC) against Aβ-induced toxicity. We observed that 2 weeks after a single i.c.v. infusion of 2 nmol of Aβ1-42, the rats displayed a decrease of spontaneous alternation in the Y-maze (Fig. 2). In order to evaluate the effects of resveratrol, animals were treated daily with 10 mg/kg of RSV or RSV-LNC for 14 days. As shown in Fig. 2, RSV treatment failed to increase the spontaneous alternation behavior in Aβ-infused rats. However, it is important to note that the treatment with RSV-LNC, at the same dosage, significantly attenuated this impairment triggered by Aβ1-42 (p < 0.001). The number of arm entries did not differ among all groups (data not shown), indicating that changes in alternation behavior were not due to generalized exploratory, locomotor, or motivational effects. Next, we evaluated the effects of Aβ1-42 infusion as well as RSV and RSV-LNC treatments on recognition memory by submitting the animals to a novel object recognition task. As seen in Fig. 3b, when the animals were placed in the arena 3 h after the first exploration period (training session, Fig. 3a), Aβ-infused rats were not able to discriminate between the familiar and novel objects, as indicated by similar exploration times for both objects (Fig. 3b). Treatment with 10 mg/kg of RSV did not improve short-term recognition memory. However, discrimination was restored by treating animals with the same dosage of RSV-LNC (p < 0.001; Fig. 3b). Similar results were found when long-term recognition memory was evaluated (p < 0.001; Fig. 3c), indicating that only rats treated with RSV-LNC were able to distinguish between familiar and new objects following Aβ infusion. Animals i.c.v. infused with water plus 0.1 % ammonium hydroxide (Aβ-vehicle) were treated with RSV or RSV-LNC at the same schedule in order to test for possible intrinsic toxicity. These animals showed no impairment in either the spontaneous alternation task or the recognition memory task when compared to control animals. Treatment with vehicle (EtOH 50 % or LNC, respectively) had no effects on the spontaneous alternation and recognition memory impairments triggered by Aβ (Fig. 3c). Animals i.c.v. infused with Aβ42-1 had no differences in the spontaneous alternation and memory recognition tasks (data not shown).
Effect of free resveratrol (RSV) and resveratrol-loaded lipid-core nanocapsules (RSV-LNC) on spontaneous alternation behavior. Rats were injected (2 nmol, i.c.v.) with Aβ1-42 or Aβ-vehicle and daily administered with RSV or RSV-LNC (10 mg/kg, i.p.), starting 1 day after Aβ1-42 injection, and maintained for 14 days. Spontaneous alternation behavior during 8 min session in the Y-maze task was measured after 14 days of treatment. Columns indicate mean ± SD, n = 8–12 animals in each experimental group. *p < 0.05, significant differences between the indicated columns (two-way ANOVA followed by Bonferroni post hoc test)
Effect of free resveratrol (RSV) and resveratrol-loaded lipid-core nanocapsules (RSV-LNC) on the novel object recognition memory. Rats were injected (2 nmol, i.c.v.) with Aβ1-42 or Aβ-vehicle and daily administered with RSV or RSV-LNC (10 mg/kg, i.p.), starting 1 day after Aβ1-42 injection, and maintained for 14 days. Graphics show object recognition index during 5 min in the training session (a), short-term memory test session performed 3 h after training (b), and long-term memory test session performed 24 h after training session (c). Columns indicate mean ± SD, n = 8–12 animals in each experimental group. ***p < 0.001, significant differences between familiar and new object for each group (two-way ANOVA followed by Bonferroni post hoc test)
Resveratrol Decreases Synaptotoxicity Triggered by Aβ
To evaluate the synaptic integrity in our treatment groups, we performed Western blotting analysis for the presynaptic protein synaptophysin (a specific presynaptic marker). A significant reduction in synaptophysin levels was found in Aβ1-42-infused rats 15 days after i.c.v. injection (p < 0.05), suggesting that some form of synaptic dysfunction had been induced (Fig. 4). Consistent with the behavioral results, only treatment with RSV-LNC was able to block the decrease in synaptophysin levels following Aβ1-42 infusion (p < 0.05; Fig. 4). Animals i.c.v. infused with Aβ-vehicle were treated with RSV or RSV-LNC, at the same schedule. Those animals showed no alteration in the synaptophysin levels when compared to control animals, excluding possible intrinsic synaptotoxicity of resveratrol. Treatment with vehicle (EtOH 50 % or LNC, respectively) had no effects on the decreased synaptophysin levels triggered by Aβ (Fig. 4).
Aβ1-42 injection causes synaptotoxicity, which is reduced by resveratrol-loaded lipid-core nanocapsules treatment. Western blot analysis for synaptophysin and β-actin protein (loading control) was performed in the hippocampus of animals after being injected with Aβ1-42 (2 nmol, i.c.v.) and treated by 14 days with free resveratrol (RSV) or resveratrol-loaded lipid-core nanocapsules (RSV-LNC) (10 mg/kg, i.p.), starting 1 day after Aβ injection. Graphic shows representative quantification of synaptophysin immunocontent normalized to β-actin protein (loading control). The values represent synaptophysin level expressed as the average percentage increase (mean ± SD) over basal levels, n = 5–8 animals in each experimental group. *p < 0.05, significant differences between the indicated columns (two-way ANOVA followed by Bonferroni post hoc test)
Effect of Resveratrol on Glial and Microglial Activation Triggered by Aβ
Astrogliosis and microglial activation are some of the earliest pathological hallmarks of AD and may occur in response to the increasing number of degenerating neurons, or to the accumulation of Aβ. The reactivity for IB4 was increased in the hippocampi of Aβ1-42-infused rats, meaning microglial activation and treatment with RSV-LNC allowed that resveratrol reduced activated microglia (Fig. 5a). Similarly, the results showed that Aβ infusion caused a highly significant increase in activated astrocytes, as seen by increased GFAP immunocontent (Fig. 5b). In the same way, while RSV was ineffective at blocking astrocytes activation, RSV-LNC treatment significantly decreased the levels of GFAP immunocontent (p < 0.01; Fig. 5b). Animals i.c.v. infused with Aβ-vehicle were treated with RSV or RSV-LNC at the same schedule and showed no alteration in the activation of astrocytes and microglia compared to control animals. Treatment with vehicle (EtOH 50 % or LNC, respectively) had no effects on the activation of astrocytes and microglia triggered by Aβ (Fig. 5a, b).
Resveratrol-loaded lipid-core nanocapsules treatment reduces astrocyte and microglial activation in the hippocampus after i.c.v. injection of Aβ1-42. Representative image showing Isolectin B4 (IB4) reactivity (a) and GFAP (b) in the hippocampus 15 days after i.c.v. injection of Aβ1-42 (2 nmol) and treatment with free resveratrol (RSV) or resveratrol-loaded lipid-core nanocapsules (RSV-LNC) (10 mg/kg, i.p.). Graphic shows representative quantification of GFAP immunocontent normalized to β-actin protein (loading control) (b). The values represent GFAP level expressed as the average percentage increase (mean ± SD) over basal levels, n = 5–8 animals in each experimental group. #p < 0.05, significantly different from all control groups; **p < 0.01, significantly different from the groups Aβ1-42 and Aβ1-42 treated with vehicles (two-way ANOVA followed by Bonferroni post hoc test)
Signaling Pathways Involved in the Neuroprotection Afforded by Resveratrol Treatment on Neurotoxicity Triggered by Aβ
In order to clarify the neuroprotective effects of resveratrol, we attempted to outline some intracellular events triggered after i.c.v. Aβ1-42 injection. Therefore, we next tested the possible requirement of JNK activation in our AD paradigm. As shown in Fig. 6a, basal level of activated JNK was detected in the hippocampus; however, an evident increase in JNK phosphorylation was observed following Aβ1-42 injection (p < 0.001). Again, only RSV-LNC was capable of blocking JNK activation (p < 0.001), although RSV treatment showed a slight tendency to decrease JNK phosphorylation (Fig. 6a). We have shown in a previous study that the GSK-3β signaling pathway plays a key role in the neuroprotective effect of resveratrol on injuries induced by oxygen–glucose deprivation [39]. Thus, we evaluated whether GSK-3β could be involved in the Aβ1-42-induced toxicity. As seen in Fig. 6b, while Aβ1-42 induced activation of GSK-3β, an increase in phosphorylation/inactivation of GSK-3β was noticed after both RSV and RSV-LNC treatment (p < 0.001). Several studies have implicated the involvement of Wnt/β-catenin pathway on toxicity triggered by Aβ [40–42]. In this way, because GSK-3β is a major player in Wnt/β-catenin signaling and because it is well established that regulation of β-catenin stability is a crucial control mechanism in Wnt signaling, we investigated the effect of resveratrol in this cascade pathway. To determine whether Aβ1-42 altered the stability of β-catenin, we analyzed cytoplasm β-catenin levels, as well as phophorylated β-catenin levels by Western blotting. Rats infused with Aβ1-42 displayed increased phosphorylated β-catenin (p < 0.01) and reduced cytoplasm β-catenin levels (p < 0.01; Fig. 6c and d, respectively). Treatment with both RSV and RSV-LNC was able to decrease the β-catenin phosphorylation and rescue cytoplasm β-catenin levels (p < 0.05; Fig. 6c and d, respectively). Animals i.c.v. infused with Aβ-vehicle were treated with RSV or RSV-LNC at the same schedule and showed no alterations in cell signaling compared to control animals. Treatment with vehicles (EtOH 50 % or LNC, respectively) had no protective effects on the cell signaling disturbances triggered by Aβ (Fig. 6a–d).
Effect of resveratrol on JNK and GSK-3β activation and β-catenin destabilization triggered by Aβ1-42. Western blot analysis was performed in hippocampi of animals after being injected with Aβ1-42 (2 nmol, i.c.v.) and treated by 14 days with free resveratrol (RSV) or resveratrol-loaded lipid-core nanocapsules (RSV-LNC) (10 mg/kg, i.p.). a Representative Western blot and graphic showing quantification of ratio pJNK/JNK immunocontent normalized to β-actin protein (loading control). The values represent pJNK/JNK level expressed as the average percentage increase (mean ± SD) over basal levels, n = 5–8 animals in each experimental group. #p < 0.001, significantly different from all control groups; ***p < 0.001, significantly different from the groups Aβ1-42 and Aβ1-42 treated with vehicles. b Representative Western blot and graphic showing quantification of ratio pGSK-3β/GSK-3β immunocontent normalized to β-actin protein (loading control). The values represent pGSK-3β/GSK-3β level expressed as the average percentage increase (mean ± SD) over basal levels, n = 5–8 animals in each experimental group. ***p < 0.001, significant differences between the indicated columns. c Representative Western blot and graphic showing quantification of β-catenin phosphorylated at serine 45 immunocontent normalized to β-actin protein (loading control). The values are expressed as the average percentage increase (mean ± SD) over basal levels, n = 5–8 animals in each experimental group. #p < 0.01, significantly different from all groups; **p < 0.01, significantly different from the groups Aβ1-42 and Aβ1-42 treated with vehicles. d Representative Western blot and graphic showing quantification of β-catenin immunocontent normalized to β-actin protein (loading control). The values are expressed as the average percentage increase (mean ± SD) over basal levels, n = 5–8 animals in each experimental group. *p < 0.05, significant differences between the indicated columns. Two-way ANOVA followed by Bonferroni post hoc test
Lipid-Core Nanocapsules Increase Resveratrol Concentration in the Brain
Since drug-loaded lipid-core nanocapsule treatment displayed enhanced effectiveness of resveratrol against Aβ1-42-induced toxicity in rats, we hypothesized that the lipid-core nanocapsules facilitated these improvements by increasing the cerebral biodistribution of resveratrol. On this purpose, quantitative analyses were performed to assess the cerebral biodistribution of resveratrol administered via polymeric nanocapsules (RSV-LNC) compared to RSV after treatment using equal dosing (10 mg/kg/day, i.p.). As can be seen in Fig. 7, a significantly higher quantity of resveratrol was found in the brains of animals treated with RSV-LNC in comparison with animals treated with free resveratrol (p < 0.001).
Lipid-core nanocapsules improve the brain biodistribution of resveratrol. Brain amount of resveratrol was analyzed by HPLC in rats injected (2 nmol, i.c.v.) with Aβ1-42 or Aβ-vehicle and daily administered with RSV or RSV-LNC (10 mg/kg, i.p.) for 14 days, as described in “Materials and Methods” section. The values are depicted as mean ± SD of five animals per group. ***p < 0.001, significantly different between the indicated columns. Two-way ANOVA followed by Bonferroni post hoc test
Investigation of the Possible Side Effects of Resveratrol Treatment
Treatment with RSV or RSV-LNC (10 mg/kg/day, i.p.), as well as the vehicles EtOH 50 % and LNC, respectively, did not induce mortality or alter body weight within 14 days of treatment (data not shown). The activities of hepatic enzymes γ-glutamyltransferase, ALT, and AST were assessed in rat blood serum. None of the treated animals presented with significant alterations in the investigated enzymes, suggesting no hepatic alterations or metabolic toxicity in the animals in the tested conditions (data not shown). Further, none of the treated animals presented with alterations in hematological parameters (data not shown).
Discussion
In the current study, we demonstrate that a single intracerebroventricular injection of Aβ1-42 induces memory dysfunction which may be related to synaptic degeneration, a cardinal feature of early phases of AD. This Aβ disease model has been a useful complement to transgenic approaches to AD neuropathology in the development and evaluation of therapeutic approaches [43]. Notably, the memory dysfunction observed here appears to be related to synaptic dysfunction. This support the hypothesis that synaptic dysfunction induced by Aβ is the primary marker of AD and precedes neuronal death [3, 44, 45]. Furthermore, our results are suggestive that the physiological response to Aβ1-42 injection involves astroglial and microglial activation. Our data show that resveratrol protects from behavioral impairments, astrocyte and microglial activation, as well as cell signaling disturbances triggered by Aβ in vivo. Of high interest, by using lipid-core nanocapsules as a resveratrol carrier, we observed that dramatically higher intracerebral concentrations of resveratrol were achieved in those rats injected with Aβ1-42, culminating in a neuroprotective effect. This supports the notion that prevention of synaptic impairment may underlie the ability of resveratrol to prevent Aβ-induced memory dysfunction which can be a relevant strategy to the therapy of neurodegenerative process involved in AD.
Loss of memory and impairment of cognitive functions represent classical signs observed in AD patients [1]. Our experimental protocol (based on the i.c.v. injection of Aβ1-42 in rats) caused a significant decline in the spontaneous alternation and the object recognition memory, which are highly dependent of the hippocampal system [46]. Additionally, the i.c.v. infusion of Aβ42-1 did not affect either spontaneous alternation or the ability of animals in recognizing new objects, indicating that the observed behavioral impairments in Aβ1-42-exposed animals were dependent on the peptide sequence/structure. In an attempt to reduce the toxicity induced by Aβ1-42, we evaluated the effects of resveratrol, a natural polyphenolic compound in grapes, peanuts, and a variety of other foods [23].
Neuroprotective effects of resveratrol against memory impairments induced by Aβ remain to be established. Here, we have observed that treatment with 10 mg/kg/day of free resveratrol failed to improve the cognitive damage induced by i.c.v. Aβ injection. On the other hand, the lipid-core nanocapsule treatment at the same dosage robustly improved Aβ-induced memory impairment, with treated rats displaying performances equivalent to their control counterparts. Because RSV-LNC treatment was initiated after Aβ infusion, these data suggest that resveratrol not only prevented memory loss, but also restored the cognitive deficit. Resveratrol significantly improved the recognition index performance, indicating that RSV-LNC-treated rats were able to distinguish between the familiar and new objects. Thereby, we suppose that improvement in spontaneous alternation and recognition index performances of RSV-LNC-treated animals reflects the neuroprotective effect of resveratrol on hippocampal regions damaged by Aβ.
Synapse loss at specific encephalic structures of AD patients significantly correlates with the severity of their cognitive symptoms [47]. In our experimental model, i.c.v. Aβ1-42 injection caused a significant decrease in hippocampal levels of synaptophysin (a specific presynaptic marker). The decreased synaptophysin levels and the impaired spontaneous alternation and object recognition tasks in Aβ1-42-exposed rats greatly suggest a link between both events. The synaptotoxic effects of Aβ1-42 might be crucial in causing the observed memory deficits. Our results are in accordance with a previous work related to synaptic loss due to toxicity induced by i.c.v. injection of Aβ [48–50]. This hypothesis is reinforced by the effects of resveratrol against synaptotoxicity triggered by Aβ1-42, since resveratrol rescued synaptic changes as can be seen by increasing synaptophysin levels, the major synaptic vesicle protein.
Despite the fact that resveratrol has attracted considerable interest for its beneficial potentials for human health, its use is strongly limited by its low bioavailability, which is a barrier to the development of therapeutic applications. In recent years, an increasing number of studies have focused on novel formulation approaches to stabilize and protect resveratrol from degradation, increase its solubility in water in order to improve its bioavailability, achieve a sustained release, and ultimately target resveratrol to specific locations via multiparticulate forms and colloidal carriers (reviewed by [32]). In this context, we recently developed a lipid-core nanocapsule system containing resveratrol and reported that this formulation improves the brain biodistribution of resveratrol [16]. We have previously shown that the same lipid-core nanocapsules were able to deliver increased concentrations of indomethacin into rat brain, resulting in decreased tumor growth [15] and Aβ toxicity [17], improving its efficacy in experimental models of peripheral inflammation [51] as well as neuroinflammation induced by oxygen–glucose deprivation [52]. In accordance with our initial findings, a possible mechanism underlying the superior efficacy of treatment with RSV-LNC against Aβ-induced toxicity may include the enhanced brain biodistribution of resveratrol afforded by lipid-core nanocapsules.
The cause–effect relationship between resveratrol concentration in the systemic bloodstream and its reported biological effects is still a conundrum. Despite oral absorption of resveratrol is high, it is rapidly metabolized. Indeed, the conjugated forms of resveratrol will be those that reach tissues where they could exert their possible biological effect, although the reported lower in vitro activity of the metabolites than resveratrol [53–55] may not necessarily reflect their in vivo function, since enzymes could convert the metabolites back to resveratrol in target organs [55]. Additionally, repeated or long-term dosing, which might result in saturation of metabolism, might lead to higher plasma and tissue levels of resveratrol [56]. Although we did not determine the levels of resveratrol in the bloodstream, our results suggest that nanocapsules are protecting resveratrol from intense metabolism which would be in the organism for a longer period of time leading to higher brain concentration. Likewise, we did not perform any experiments to directly verify that lipid-core nanocapsules became lodged in the brain. Thus, whether nanocapsules are able to cross the BBB remain to be determined, although some authors have already shown that the coating of nanocapsules with polysorbate 80 is essential for the delivery of drugs into the brain [57–59].
Synaptic loss and death of specific neurons population in AD are provoked by a cascade of multiple deleterious molecular and cellular events rather than a single pathogenic factor. One feature present in AD brain and analyzed in the present study is the presence of reactive astrocytes and activated microglial cells triggered by Aβ1-42, which plays a prominent role in the neurodegenerative process [60]. These cells normally provide tissue maintenance and immune surveillance of the brain, but as potent sources of proinflammatory cytokines and chemokines, astrocytes and microglia are pivotal in the progression of neurodegenerative processes including AD [61]. In fact, previous studies have shown that astrocytes and microglial cells are important mediators of Aβ-induced neurotoxicity becoming prominent sources of inflammatory mediators and reactive oxygen or nitrogen species [62, 63]. Our results clearly show that resveratrol was able to decrease both astrocyte and microglial activation induced by i.c.v. injection of Aβ1-42. Recently, using organotypic hippocampal culture exposed to Aβ1-42, we observed that resveratrol exhibited potent anti-inflammatory effects by decreasing cytokine release, reactive species formation, and glial activation, culminating in the prevention of cell death (unpublished data). In the same way, previous evidence suggests that the activation by phosphorylation of stress-activated protein JNK is closely associated with neural dysfunction in AD [48, 64]. Additionally, JNKs are reported to be involved in the enlargement of microglia, as well as in the induction of proinflammatory cytokine genes coding for TFN-α, IL-6, or MCP-1 in addition to COX-2 [65], suggesting that JNKs are relevant co-mediators of the activation of microglia. Further, activation of JNKs in the brain induced by Aβ leads to enhanced expression of iNOS, contributing to the neurodegenerative process and cognitive damage [48]. Recently, the fundamental role of JNK in the regulation of tau hyperphosphorylation, a hallmark of AD, has also been established [66]. In the present study, we demonstrate that Aβ triggers astrocyte activation and likely triggers microglial activation as well. The activation of these glial cells may have led to the release of inflammation factors culminating in the sustained JNK activation. The association of these events is closely related to memory dysfunction as described by Medeiros and collaborators [48]. Our results show that by using lipid-core nanocapsules, resveratrol was able to decrease reactive astrocytes and microglia as well as activate JNK. Therefore, we suggest that blocking this vicious cycle was correlated with the improvements of memory performance impaired by Aβ.
Activation of GSK-3β has been shown to be a key component in signaling pathways that underlie neurodegeneration [67]. GSK-3β activation is implicated in AD because it can increase Aβ production and neuroinflammation. In neurons, GSK-3β directly phosphorylates several microtubule-associated proteins (MAPs) such as tau, MAP-1B, and MAP-2B [68]. Another substrate of GSK-3β in vitro is β-catenin, a protein implicated in cell adhesion and in the Wnt signaling pathway, which is known to be involved in the control of tissue patterning, cell fate, cell proliferation, development of the vertebrate CNS, and synaptic regulation [69–71], beyond closely related in the degenerative process involved in Aβ-induced toxicity [40–42]. Free cytoplasmic β-catenin levels are strictly controlled by phosphorylation of NH2-terminal region. This reaction, which targets β-catenin to proteosome for ubiquitin-mediated degradation, requires association with several kinases including GSK-3β [72]. Consistent with the amyloid cascade hypothesis, we observed that Aβ induces a strong activation of GSK-3β, which may be involved in the increased levels of β-catenin phosphorylation and consequent β-catenin destabilization. Given that we have previously shown that resveratrol was able to increase phosphorylation/inactivation of GSK-3β in an in vitro model of oxygen–glucose deprivation [39], we sought to evaluate the effect of resveratrol against GSK-3β activation induced by Aβ. Although only RSV-LNC treatment was able to improve memory and synaptic damage, as well as astrocytes, microglial, and JNK activation induced by i.c.v. Aβ infusion, to our surprise, both RSV and RSV-LNC treatments were able to inhibit GSK-3β activity by serine 9 phosphorylation. This effect in turn led to a decrease of phosphorylation levels of β-catenin induced by Aβ, which contributed to the stabilization of β-catenin as evidenced by increased cytoplasmic levels of β-catenin, which may cause TCF-induced transcriptional activation and prevent Aβ toxicity. Despite the amount of resveratrol in the brain tissue was three times higher in animals treated with nanocapsules which decreases behavioral impairments and changes in the synaptic function and glial activation triggered by Aβ, likely a lower concentration of resveratrol may be effective in modulating both GSK-3β and β-catenin proteins explaining the similarity in results after RSV or RSV-LNC treatments.
Degradation of β-catenin is initiated upon amino-terminal serine/threonine phosphorylation, and GSK-3β appears to be a central player for ubiquitination-dependent proteolysis of β-catenin. Although GSK-3β phosphorylates β-catenin at serine 33/37, and this phosphorylation is critical for β-catenin recognition by ubiquitination apparatus, it has been recognized that β-catenin phosphorylation in vivo requires casein kinase Iα, which phosphorylates β-catenin at serine 45 and whose phosphorylation of β-catenin precedes and is obligatory for subsequent GSK-3β phosphorylation of β-catenin [72]. Thereby, our results show that resveratrol treatment was able to inhibit not only GSK-3β activation induced by Aβ1-42 but also phosphorylation of β-catenin at serine 45 stabilizing β-catenin levels, which might be related to the improvement of memory performance. In fact, recent studies concentrated on establishing the molecular complexity of Wnt/β-catenin signaling in neurons propose that inhibition of GSK-3β decreases Aβ neurotoxicity by reducing tau phosphorylation, increases β-catenin stabilization, and improves memory performance, suggesting that restoring β-catenin signaling may alleviate the underlying neuronal deficits in AD [73, 74].
Taking into account our results, a concern about the efficacy of resveratrol as an anti-Aβ drug remains to be determined; however, some studies have shown that resveratrol may binding to different assemblies of Aβ [75] and selectively remodels soluble oligomers and fibrils of Aβ [76], reduces plaque pathology in transgenic model of AD [25], as well as promotes clearance of Aβ through proteasome activation [24]. In our AD paradigm, the effects of resveratrol seem not to be directly linked to inhibition of Aβ aggregation, once Aβ i.c.v. injected was in the aggregated form. Although we have used insoluble amyloid fibrils, we do not exclude the presence of other Aβ assemblies in our Aβ preparation. Indeed, it appears unlikely that there are just one or two assembly forms of the peptide that induce neuronal dysfunction. Rather, various soluble oligomers of Aβ can likely bind to different components of neuronal and non-neuronal plasma membranes to induce complex patterns of synaptic dysfunction and network disorganization. These changes may in turn activate biochemical cascades causing neuronal dysfunction and ultimately cell death [77, 78], and our results show that the neuroprotective effects of resveratrol seem to be fair in these disturbed biochemical cascades triggered by Aβ.
In conclusion, the present findings reinforce and extend the notion of the hazardous effects of Aβ1-42 toward hippocampal synaptic homeostasis and cognitive performance. Furthermore, we show that resveratrol is able to counteract the behavioral and cell signaling impairments triggered by i.c.v. infusion of Aβ1-42. Moreover, this is the first report relating the ability of resveratrol to protect against synaptic degeneration induced by Aβ. Therefore, data from this study not only confirm the potential of resveratrol in treating the neurodegenerative process involved in AD but also offer an effective way to improve the biodistribution of resveratrol afforded by nanodrug delivery systems. Our results open the possibility that resveratrol could be a promising molecule for further pharmacological studies on the search for therapeutic strategies to treat or prevent AD.
References
Mattson MP (2004) Pathways towards and away from Alzheimer’s disease. Nature 430:631–639
Klein WL, Stine WB Jr, Teplow DB (2004) Small assemblies of unmodified amyloid beta-protein are the proximate neurotoxin in Alzheimer’s disease. Neurobiol Aging 25:569–580
Walsh DM, Selkoe DJ (2004) Deciphering the molecular basis of memory failure in Alzheimer’s disease. Neuron 44:181–193
Pardridge WM (2005) The blood–brain barrier: bottleneck in brain drug development. NeuroRx 2:3–14
Modi G, Pillay V, Choonara YE, Ndesendo VMK, du Toit LC, Naidoo D (2009) Nanotechnological applications for the treatment of neurodegenerative disorders. Progress Neurobiol 88:272–285
Hans ML, Lowman AM (2002) Biodegradable nanoparticles for drug delivery and targeting. Curr Opin Solid State Mater Sci 6:319–327
Soppimath KS, Aminabhavi TM, Kulkarni AR, Rudzinski WE (2001) Biodegradable polymeric nanoparticles as drug delivery devices. J Control Release 70:1–20
Zensi A, Begley D, Pontikis C, Legros C, Mihoreanu L, Wagner S, Büchel C, von Briesen H, Kreuter J (2009) Albumin nanoparticles targeted with Apo E enter the CNS by transcytosis and are delivered to neurons. J Control Release 137:78–86
Brasnjevic I, Steinbusch HWM, Schmitz C, Martinez-Martinez P (2009) Delivery of peptide and protein drugs over the blood–brain barrier. Progress Neurobiol 87:212–251
Wilson B, Samanta MK, Santhi K, Kumar KPS, Ramasamy M, Suresh B (2010) Chitosan nanoparticles as a new delivery system for the anti-Alzheimer drug tacrine. Nanomedicine 6:144–152
Guterres SS, Weiss V, de Luca Freitas L, Pohlmann AR (2000) Influence of benzyl benzoate as oil core on the physicochemical properties of spray-dried powders from polymeric nanocapsules containing indomethacin. Drug Deliv 7:195–199
Pohlmann AR, Soares LU, Cruz L, Da Silveira NP, Guterres SS (2004) Diffusion and mathematical modeling of release profiles from nanocarriers. Curr Drug Deliv 1:103–110
Beck RCR, Pohlmann AR, Hoffmeister C, Gallas MR, Collnot E, Schaefer UF, Guterres SS, Lehr CM (2007) Dexamethasone-loaded nanoparticle-coated microparticles: correlation between in vitro drug release and drug transport across Caco-2 cell monolayers. Eur J Pharm Biopharm 67:8–30
Pohlmann AR, Mezzalira G, Venturini C, Cruz L, Bernardi A, Jäger E, Battastini AMO, Silveira NP, Guterres SS (2008) Determining the simultaneous presence of drug nanocrystals in drug-loaded polymeric nanocapsule aqueous suspensions: a relation between light scattering and drug content. Int J Pharmac 359:288–293
Bernardi A, Braganhol E, Jäger E, Figueiró F, Edelweiss MI, Pohlmann AR, Guterres SS, Battastini AMO (2009) Indomethacin-loaded nanocapsules treatment reduces in vivo glioblastoma growth in a rat glioma model. Cancer Lett 281:53–63
Frozza RL, Bernardi A, Paese K, Hoppe JB, da Silva T, Battastini AMO, Pohlmann AR, Guterres SS, Salbego C (2010) Characterization of trans-resveratrol-loaded lipid-core nanocapsules and tissue distribution studies in rats. J Biomed Nanotechnol 6:694–703
Bernardi A, Frozza RL, Meneghetti A, Hoppe JB, Battastini AM, Pohlmann AR, Guterres SS, Salbego CG (2012) Indomethacin-loaded lipid-core nanocapsules reduce the damage triggered by Aβ1-42 in Alzheimer’s disease models. Int J Nanomedicine 7:4927–4942
Orgogozo JM, Dartigues JF, Lafont S, Letenneur L, Commenges D, Salomon R, Renaud S, Breteler MB (1997) Wine consumption and dementia in the elderly: a prospective community study in the Bordeaux area. Rev Neurol 153:185–192
Lindsay J, Laurin D, Verreault R, Hébert R, Helliwell B, Hill GB, McDowell I (2002) Risk factors for Alzheimer’s disease: a prospective analysis from the Canadian Study of Health and Aging. Am J Epidemiol 156:445–453
Vingtdeux V, Dreses-Werringloer U, Zhao H, Davies P, Marambaud P (2008) Therapeutic potential of resveratrol in Alzheimer's disease. BMC Neurosci 9(Suppl 2):S6, Review
Anekonda TS (2006) Resveratrol-A boon for treating Alzheimer's disease? Brain Res Rev 52:316–326
Harikumar KB, Aggarwal BB (2008) Resveratrol A multi-targeted agent for age-associated chronic diseases. Cell Cycle 8:1020–1035
Baur JA, Sinclair DA (2006) Therapeutic potential of resveratrol: the in vivo evidence. Nat Rev Drug Discov 5:493–506
Marambaud P, Zhao H, Davies P (2005) Resveratrol promotes clearance of Alzheimer's disease amyloid-beta peptides. J Biol Chem 280:37377–37382
Karuppagounder SS, Pinto JT, Xu H, Chen HL, Beal MF, Gibson GE (2009) Dietary supplementation with resveratrol reduces plaque pathology in a transgenic model of Alzheimer's disease. Neurochem Int 54:111–118
Vingtdeux V, Giliberto L, Zhao H, Chandakkar P, Wu Q, Simon JE, Janle EM, Lobo J, Ferruzzi MG, Davies P, Marambaud P (2010) AMP-activated protein kinase signaling activation by resveratrol modulates amyloid-beta peptide metabolism. J Biol Chem 285:9100–9113
Kundu JK, Surh Y-J (2008) Cancer chemopreventive and therapeutic potential of resveratrol: mechanistic perspectives. Cancer Lett 296:243–261
Knutson MD, Leeuwenburgh C (2008) Resveratrol and novel potent activators of SIRT1: effects on aging and age-related diseases. Nutr Rev 66:591–596
Albani D, Polito L, Forloni G (2010) Sirtuins as novel targets for Alzheimer's disease and other neurodegenerative disorders: experimental and genetic evidence. J Alzheimers Dis 19:11–26
Baur JA, Pearson KJ, Price NL, Jamieson HA, Lerin C, Kalra A, Prabhu VV, Allard JS, Lopez-Lluch G, Lewis K, Pistell PJ, Poosala S, Becker KG, Boss O, Gwinn D, Wang M, Ramaswamy S, Fishbein KW, Spencer RG, Lakatta EG, Le Couteur D, Shaw RJ, Navas P, Puigserver P, Ingram DK, de Cabo R, Sinclair DA (2006) Resveratrol improves health and survival of mice on a high-calorie diet. Nature 444:337–342
Wenzel E, Somoza V (2005) Metabolism and bioavailability of trans-resveratrol. Mol Nutr Food Res 49:472–481
Amri A, Chaumeil JC, Sfar S, Charrueau C (2012) Administration of resveratrol: what formulation solutions to bioavailability limitations? J Control Release 158:182–193
Jäger E, Venturini CG, Poletto FS, Colomé LM, Pohlmann JPU, Bernardi A, Battastini AMO, Guterres SS, Pohlmann AR (2009) Sustained release from lipid-core nanocapsules by varying the core viscosity and the particle surface area. J Biomed Nanotechnol 5:130–140
Paxinos G, Watson C (2005) The rat brain in stereotaxic coordinates, 5th edn. Elsevier Academic, San Diego
Huges RN (2004) The value of spontaneous alternation behavior (SAB) as a test of retention in pharmacological investigations of memory. Neurosci Biobehav Rev 28:497–505
Bevins RA, Besheer J (2006) Object recognition in rats and mice: a one-trial non-matching-to-sample learning task to study ‘recognition memory’. Nat Protocols 1:1306–1311
Ennaceur A, Delacour J (1988) A new one-trial test for neurobiological studies of memory in rats. 1. Behavioral data. Behav Brain Res 31:47–59
Peterson GL (1979) Review of the Folin-phenol protein quantification method of Lowry, Rosebrough, Farr and Randall. Anal Biochem 100:201–220
Zamin LL, Dillenburg-Pilla P, Argenta-Comiran R, Horn AP, Simão F, Nassif M, Gerhardt D, Frozza RL, Salbego C (2006) Protective effect of resveratrol against oxygen–glucose deprivation in organotypic hippocampal slice cultures: involvement of PI3-K pathway. Neurobiol Dis 24:170–182
Garrido JL, Godoy J, Alvarez A, Bronfman M, Inestrosa NC (2002) Protein kinase C inhibits amyloid β-peptide neurotoxicity by acting on members of the Wnt pathway. FASEB J 14:1982–1984
De Ferrari GV, Chacón MA, Barría MI, Garrido JL, Godoy JA, Olivares G, Reyes AE, Alvarez A, Bronfman M, Inestrosa NC (2003) Activation of Wnt signaling rescues neurodegeneration and behavioral impairments induced by β-amyloid fibrils. Mol Psychiatry 8:195–208
Li B, Zhong L, Yang X, Andersson T, Huang M, Tang S-J (2011) WNT5A signaling contributes to Aβ-induced neuroinflammation and neurotoxicity. PlosOne 6:1–10
Woodruff-Pak DS (2008) Animal models of Alzheimer’s disease: therapeutic implications. J Alzheimers Dis 15:507–521
Ferreira ST, Vieira MN, De Felice FG (2007) Soluble protein oligomers as emerging toxins in Alzheimer’s and others amyloid diseases. IUBMB Life 59:332–345
Knobloch M, Mansuy IM (2008) Dendritic spine loss and synaptic alterations in Alzheimer’s disease. Mol Neurobiol 37:73–82
Broadbent NJ, Gaskin S, Squire LR, Clark RE (2010) Object recognition memory and the rodent hippocampus. Learn Mem 17:5–11
Scheff SW, Price DA, Schmitt FA, Mufson EJ (2006) Hippocampal synaptic loss in early Alzheimer’s disease and mild cognitive impairment. Neurobiol Aging 27:1372–1384
Medeiros R, Prediger RDS, Passos GF, Pandolfo P, Duarte FS, Franco JL, Dafre AL, Di Giunta G, Figueiredo CP, Takahashi RN, Campos MM, Calixto JB (2007) Connecting TNF-α signaling pathways to iNOS expression in a mouse model of Alzheimer’s disease: relevance for the behavioral and synaptic deficits induced by amyloid β protein. J Neurosci 27:5394–5404
Canas PM, Porciúncula LO, Cunha GMA, Silva CG, Machado NJ, Oliveira JMA, Oliveira CR, Cunha RA (2009) Adenosine A2A receptor blockade prevents synaptotoxicity and memory dysfunction caused by β-amyloid peptides via p38 mitogen-activated protein kinase pathway. J Neurosci 29:14741–14751
Passos GF, Figueiredo CP, Prediger RDS, Pandolfo P, Duarte FS, Medeiros R, Calixto JB (2009) Role of the macrophage inflammatory protein-1α/CC chemokine receptor 5 signaling pathway in the neuroinflammatory response and cognitive deficits induced by β-amyloid peptide. Am J Pathol 175:1586–1597
Bernardi A, Zilberstein AC, Jäger E, Campos MM, Morrone FB, Calixto JB, Pohlmann AR, Guterres SS, Battastini AMO (2009) Effects of indomethacin-loaded nanocapsules in experimental model of inflammation in rats. Br J Pharmacol 158:1104–1111
Bernardi A, Frozza RL, Horn AP, Campos MM, Calixto JB, Salbego C, Pohlmann AR, Guterres SS, Battastini AMO (2010) Protective effects of indomethacin-loaded nanocapsules against oxygen–glucose deprivation in organotypic hippocampal slice cultures: involvement of neuroinflammation. Neurochem Int 57:629–636
Calamini B, Ratia K, Malkowski MG, Cuendet M, Pezzuto JM, Santarsiero BD, Mesecar AD (2010) Pleiotropic mechanisms facilitated by resveratrol and its metabolites. Biochem J 429(2):273–282
Hoshino J, Park EJ, Kondratyuk TP, Marler L, Pezzuto JM, van Breemen RB, Mo S, Li Y, Cushman M (2010) Selective synthesis and biological evaluation of sulfate-conjugated resveratrol metabolites. J Med Chem 53(13):5033–5043
Miksits M, Wlcek K, Svoboda M, Kunert O, Haslinger E, Thalhammer T, Szekeres T, Jäger W (2009) Antitumor activity of resveratrol and its sulfated metabolites against human breast cancer cells. Planta Med 75(11):1227–1230
Walle T (2011) Biovailability of resveratrol. Ann NY Acad Sci 1215:9–15
Kreuter J, Alyautdin RN, Kharkevich DA, Ivanov AA (1995) Passage of peptides through the blood–brain barrier with colloidal polymer particles (nanoparticles). Brain Res 674:171–174
Alyautdin RN, Petrov VE, Langer K, Berthold A, Kharkevich DA, Kreuter J (1997) Delivery of loperamide across the blood–brain barrier with polysorbate 80-coated poly(butylcyanoacrylate) nanoparticles. Pharm Res 14:325–328
Gulyaev AE, Gelperina SE, Skidan IN, Antropov AS, Kivman GY, Kreuter J (1999) Significant transport of doxorubicin into the brain with polysorbate 80-coated nanoparticles. Pharm Res 16:1564–1569
Lue L-F, Kuo Y-M, Beach T, Walker DG (2010) Microglia activation and anti-inflammatory regulation in Alzheimer’s disease. Mol Neurobiol 41:115–128
Hensley K (2010) Neuroinflammation in Alzheimer’s disease: mechanisms, pathologic consequences, and potential for therapeutic manipulation. J Alzheimers Dis 21:1–14
Garwood CJ, Pooler AM, Atherton J, Hanger DP, Noble W (2011) Astrocytes are important mediators of Aβ-induced neurotoxicity and tau phosphorylation in primary culture. Cell Death Dis 2:1–9
Capiralla H, Vingtdeux V, Zhao H, Sankowski R, Al-Abed Y, Davies P, Marambaud P (2011) Resveratrol mitigates lipopolysaccharide- and Aβ-mediated microglial inflammation by inhibiting the TLR4/NF-κB/STAT signaling cascade. J Neurochem 120:461–472
Mehan S, Meena H, Sharma D, Sankhla R (2011) JNK: a stress-activated protein kinase therapeutic strategies and involvement in Alzheimer’s and various neurodegenerative abnormalities. J Mol Neurosci 43:376–390
Waetzig V, Herdegen T (2004) Neurodegenerative and physiological actions of c-Jun N-terminal kinases in the mammalian brain. Neurosci Lett 361:64–67
Ploia C, Antoniou X, Sclip A, Grande V, Cardinetti D, Colombo A, Canu N, Benussi L, Ghidoni R, Forloni G, Borsello T (2011) JNK plays a key role in tau hyperphosphorylation in Alzheimer’s disease models. J Alzheimers Dis 26:315–329
Balaraman Y, Limaye AR, Levey AI, Srinivasan S (2006) Glycogen synthase kinase 3β and Alzheimer’s disease: pathophysiological and therapeutic significance. Cell Mol Life Sci 63:1226–1235
Hall AC, Lucas FR, Salinas PC (2000) Axonal remodeling and synaptic differentiation in the cerebellum is regulated by Wnt-7a signaling. Cell 100:525–535
Cadigan KM, Nusse R (1997) Wnt signaling: a common theme in animal development. Genes Dev 11:3286–3305
Lee SM, Tole S, Grove E, McMahon AP (2000) A local Wnt-3a signal is required for development of the mammalian hippocampus. Development 127:457–467
Galceran J, Miyashita-Lin EM, Devaney E, Rubenstein JL, Grosschedl R (2000) Hippocampus development and generation of dentate gyrus granule cells is regulated by LEF1. Development 127:469–482
Liu C, Li Y, Semenov M, Han C, Baeg C, Tan Y, Zhang Z, Lin X, He X (2002) Control of β-catenin phosphorylation/degradation by a dual-kinase mechanism. Cell 108:837–847
Inestrosa NC, Varela-Nallar L, Grabowski CP, Colombres M (2007) Synaptotoxicity in Alzheimer’s disease: the Wnt signaling pathway as a molecular target. IUBMB Life 59:316–321
Toledo EM, Inestrosa NC (2009) Activation of Wnt signaling by lithium and rosiglitazone reduced spatial memory impairment and neurodegeneration in brains of an APPswe/PSEN1DeltaE9 mouse model of Alzheimer’s disease. Mol Psychiatry 15:272–285
Ge J-F, Qiao J-P, Qi C-C, Wang C-W, Zhou J-N (2012) The binding of resveratrol to monomer and fibril amyloid beta. Neurochem Int 61:1192–1201
Ladiwala ARA, Lin JC, Bale SS, Marcelino-Cruz AM, Bhattacharya M, Dordick JS, Tessier PM (2010) Resveratrol selectively remodels soluble oligomers and fibrils of amyloid Aβ into off-pathway conformers. J Biol Chem 285:24228–24237
Selkoe DJ (2011) Resolving controversies on the path to Alzheimer’s therapeutics. Nat Med 17(9):1060–1065
Mucke L, Selkoe DJ (2012) Neurotoxicity of amyloid β-protein: synaptic and network dysfunction. Cold Spring Harb Perspect Med 2(7):a006338
Acknowledgments
This study was supported by the following Brazilian agencies: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), and Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (FAPERGS). The authors thank PRONEX CNPq-FAPERGS (#10/0048-4). RL Frozza and JB Hoppe were recipients of Brazilian CNPq fellowships. A Bernardi was the recipient of a CAPES Post-doctoral fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frozza, R.L., Bernardi, A., Hoppe, J.B. et al. Neuroprotective Effects of Resveratrol Against Aβ Administration in Rats are Improved by Lipid-Core Nanocapsules. Mol Neurobiol 47, 1066–1080 (2013). https://doi.org/10.1007/s12035-013-8401-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-013-8401-2