Abstract
Synaptically released l-glutamate, the most important excitatory neurotransmitter in the CNS, is removed from extracellular space by fast and efficient transport mediated by several transporters; the most abundant ones are EAAT1/GLAST and EAAT2/GLT1. The review first summarizes their location, functions and basic characteristics. We then look at genetics and epigenetics of EAAT1/GLAST and EAAT2/GLT1 and perform in silico analyses of their promoter regions. There is one CpG island in SLC1A2 (EAAT2/GLT1) gene and none in SLC1A3 (EAAT1/GLAST) suggesting that DNA methylation is not the most important epigenetic mechanism regulating EAAT1/GLAST levels in brain. There are targets for specific miRNA in SLC1A2 (EAAT2/GLT1) gene. We also note that while defects in EAAT2/GLT1 have been associated with various pathological states including chronic neurodegenerative diseases, very little is known on possible contributions of defective or dysfunctional EAAT1/GLAST to any specific brain disease. Finally, we review evidence of EAAT1/GLAST involvement in mechanisms of brain response to alcoholism and present some preliminary data showing that ethanol, at concentrations which may be reached following heavy drinking, can have an effect on the distribution of EAAT1/GLAST in cultured astrocytes; the effect is blocked by baclofen, a GABA-B receptor agonist and a drug potentially useful in the treatment of alcoholism. We argue that more research effort should be focused on EAAT1/GLAST, particularly in relation to alcoholism and drug addiction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The most important neurotransmitter at excitatory synapses in the central nervous system is an acidic (dicarboxylic) amino acid l-glutamate (l-Glu, review: [1]; historical overview: [2]; recent review: [3]). According to a classical view, most of the synaptic l-Glu is synthesised in glutamatergic nerve terminals by conversion of l-glutamine via phosphate-activated glutaminase (PAG) and then actively transported into and stored in, synaptic vesicles. Several vesicular glutamate transporters (VGLUT’s) driven by H+-dependent ATPase assist the accumulation of l-Glu by the vesicles [4]. l-Glu is released from the synaptic nerve endings when the glutamate-containing vesicles discharge their content by a stimulus- (depolarization-) coupled Ca2+-dependent mechanisms into the synaptic cleft. l-Glu interacts with l-Glu receptors [3] on the surface of the postsynaptic neuron (or on other cells in the vicinity) and diffuses away or is taken up by a very efficient “high affinity” Na+-dependent l-glutamate transport (GluT) into surrounding cellular structures; these are mostly, but not exclusively, adjacent astrocytes.
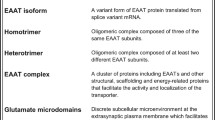
GluT is mediated by distinct protein molecules derived from five genes (reviews: [5, 6]). In some species such as humans and guinea pigs they are referred to as excitatory amino acid transporters (EAATs) and marked EAAT1-5, while in rats and mice they are called GLAST (GLutamate and ASpartate Transporter; homologous to EAAT1), GLT-1 (or GLT1; GLutamate Transporter One; homologous to EAAT2), EAAC1 (excitatory amino acid carrier one; homologous to EAAT3). There are no alternative designations for the rodent EAAT4 and EAAT5. As all EAATs are members of the solute carrier family SLC1A, the complete designations should be given as EAAT1/GLAST/SLC1A3, EAAT2/GLT1/SLC1A2, EAAT3/EAAC1/SLC1A1, EAAT4/SLC1A6, EAAT5/SLC1A7. Here we shall use EAAT1/GLAST and EAAT2/GLT1 designations when referring to the actual transporters (proteins) with the corresponding SLC1A3 and SLC1A2 terms reserved for the respective genes (see the following section for full details).
EAATs transport glutamate against very high concentration gradients [5] thus constantly “sweeping” any residual l-Glu from the extracellular space; this is held to be very important in preventing build-up of excess l-Glu in and around glutamatergic synapses which could act in an “excitotoxic” manner and trigger off, in extreme situations, death of the surrounding neurons [7].
l-Glu is co-transported with Na+ and it should be understood that the efficiency (or even the direction) of GluT by EAATs is conditional on existing transmembrane Na+ gradients. GluT should really be recognized as Na+- and K+-dependent because the gradients of both ions are required for a full GluT cycle to function: Na+ is co-transported with l-Glu into the cell while K+ is counter-transported (i.e. leaving the cell) by the l-Glu-free EAAT molecule. Additionally, pH and electrical gradients also contribute to the free energy driving the transport (for a review see [6]). Furthermore, EAAT1/GLAST, EAAT3-5 but not EAAT2/GLT1 act as activity dependent Cl− channels (reviews: [5, 6, 8]). The precise stoichiometries of the transport for EAAT1/GLAST and EAAT2/GLT1 have been well established: 3Na+, 1H+, 1 l-Glu and 1 K+ [9, 10, 11; review: 6]. While the Na+ and K+ gradients provide the bulk of the driving force for the system and the ions interact directly with the transporter protein molecule, Cl− passage is not thermodynamically coupled to GluT and follows slope of the Cl− gradient (review: [6, 8]).
Location of EAATs and Their Possible Roles in Brain Functions
As mentioned above, the role of GluT most often mentioned in the literature is to limit the spread of synaptically released l-Glu and prevent uncontrolled excitation and neurotoxicity. EAATs may, however, be involved in other physiological processes as indicated by their cellular location.
The majority of the EAAT molecules expressed in brain tissue have been located to astrocytes. This is particularly the case for EAAT1 (GLAST) and EAAT2 (GLT1) which both account for most of the EAAT protein expressed in brain [5, 6, 8]. EAAT2/GLT1 protein seems to be distributed in two pools, one enriched in the plasma membrane of astrocytic endfeet apposed to glutamatergic synapses and the other distributed over the whole surface of the cells [12, 13]. GLAST appears in some studies to be preferentially localised to the astrocytic regions close to excitatory synapses [14] but in other studies has been shown to be expressed by the cell bodies of astrocytes [15]. Again, like in the case of GLT1 this may indicate two pools of GLAST. EAAT2/GLT1 accounts, for at least 1 % of all protein in the CNS [8]. EAAT1/GLAST is about 4-times less abundant, based on assays of whole brains. EAAT2/GLT1 appears to be the principal EAAT in the forebrain, particularly in the cerebral cortex and to a lesser extent in the rest of the CNS. GLAST is the main EAAT in the cerebellar cortex where it is located in Bergman glia, which are a type of radial glial cells (reviews: [5, 8, 16]). In addition, GLAST is strongly expressed in other radial-like glial cells including the Müller cells of the retina and in tanycytes in the circumventricular organs [8]. Elsewhere there is evidence for expression in populations of astrocytes and oligodendrocytes. There are intriguing exceptions in the literature, though. For example, Roberts et al. [17] reported that EAAT1 labelling in human brain was located on the plasma membrane of astrocytes but also in the soma and nucleus. Furthermore, they detected EAAT1 protein in neurons, where it was present in the soma, all parts of the axon, dendritic spines and in the postsynaptic density (PSD). This is at variance with most of the other studies which have located EAAT1 in astrocytes; the presence of an apparent EAAT1 antigen in neurons might have been caused by changes taking place in the tissue during the post-mortem delay [17, 18] but there are other ways to explain the observed discrepancies, including the occurrence of splice variants. EAAT1 is now known to be subject to alternate splicing and to give rise to multiple variant proteins. At least one of these is known to be strongly expressed by neurons, especially when they have been subject to stressors such as ischaemia [18].
While EAAT1/GLAST, at least in the healthy CNS, is regularly expressed by glial cells, the location of EAAT2/GLT1, even in healthy brain, is less clear. In developing nervous tissue, particularly in developing cultured brain cells, EAAT2/GLT1 is present, at least transiently, in neurons [19, 20] where l-Glu may be involved in the process of differentiation [21]. Moreover, in the adult brain there is evidence of significant glutamate transport in axonal nerve endings, possibly mediated by a form of EAAT2/GLT1 [22–24] that is expressed by neurons. A neuronal localisation for some form of EAAT2 is supported at least in part by in situ hybridisation studies [25] but the precise role and importance of neuronal EAAT2 (or a related protein) remains contentious [26–28]. Recent data suggest that the contribution of neuronal GLT1 to glutamate transport may have been underestimated, particularly when using synaptosomal preparations [29].
The hypothetical presynaptic EAAT2/GLT1 could directly help to replenish the presynaptic neurotransmitter stores. In contrast, l-Glu taken up by astrocytes is, at least in part, metabolized into l-glutamine, which may be passed via specific transport back to neurons including the excitatory glutamatergic nerve terminals, where it is converted to the neurotransmitter l-Glu (see e.g. [30]). Which process—active re-uptake by presynaptic EAAT or the conversion of l-glutamine to l-Glu by phosphate activated glutaminase—is more important to maintain presynaptic l-Glu stores may be a subject of debate [26–28, 31]. Experiments with brain cortical tissue in vitro have indicated that inhibition of GluT (this would include GluT in glia, neurons as well as the “presynaptic” GluT) depended somewhat on the type of inhibitor used but, those compounds which are not transported themselves but clearly inhibit at least one of the main EAATs [32], appeared to potentiate glutamatergic activity [33, 34]. This would seem to suggest that GluT has a primarily moderating effect on glutamatergic neurotransmission and would be consistent with the predominant role of GluT being that of limiting the spread of synaptically released l-Glu and preventing “runaway” excitation; if it was important mainly for replenishing presynaptic stores thus maintaining the potency of glutamatergic synapses, the effect of GluT inhibitors would not be expected to cause an increase in the overall intensity of glutamatergic excitation over a period of many minutes [33, 34].
Other experiments studying glutamate and energy metabolism in brain tissue pointed to a strong metabolic relationship between astrocytes and glutamatergic neurons; possibly favouring l-glutamine transport as being important for maintaining the normal glutamatergic neurotransmission in brain tissue [26, 30] but not necessarily ruling out a significant role of “re-used” l-Glu, i.e. l-Glu released and taken up back to the nerve terminals. Identification and characterization of the hypothetical presynaptic EAAT would help to resolve these questions.
Another potential role of the hypothetical presynaptic transporter is a feedback inhibition of l-Glu release. The neurotransmitter l-Glu has no known inhibitory ionotropic receptor which could play the role of the negative feedback at glutamatergic synapses. In general, it seems difficult to imagine that a powerful and ubiquitous process such as glutamatergic synaptic excitation would function in a system of the size and complexity of the mammalian brain without such a feedback control. More specifically, some models actually suggest that GluT, as it is thought to exert its influence in and around synapses (mainly the EAATs in astrocytes), can adequately protect the postsynaptic neurons from excess l-Glu but will not prevent access of l-Glu to the presynaptic terminal [35]. EAATs can act as Cl−-permeable channels, opening in the presence and during the transport of l-Glu ([36]; review: [37]). Therefore, if placed presynaptically, they could reduce the depolarization of the presynaptic terminals thus effectively exerting presynaptic feedback inhibition. Whilst this presynaptic inhibition model has been demonstrated in retinal bipolar neurons that express EAAT5 [38, 39] this chloride conductance is virtually absent in EAAT2/GLT1 which is currently the most prominent candidate for the brain presynaptic EAAT. However, the Cl− permeability is not a trait rigidly imposed by the type of EAATs; it could be altered by small structural changes in the particular EAAT molecule [40, 41]; for a review see [37]. Thus it remains a possibility that an as yet unidentified EAAT2/GLT1 variant with structural characteristics capable of assuming suitable conformation and displaying Cl− permeability may act as the hypothetical putative “inhibitory” glutamate receptor. As to the other EAATs, it is unlikely that GLAST, EAAT3 or EAAT4 can be involved in such process as there is little evidence for presynaptic GLAST (see [17] above, though) but it cannot be ruled out that the highly Cl−-permeable EAAT5 might contribute to the negative feedback control at glutamatergic synapses in some brain regions where it is present in significant amounts [38, 39, 42]. EAAT3 (EAAC1) is located in neurons but, overall, it is expressed at levels about two orders of magnitude lower then EAAT2/GLT1 [8] and is frequently expressed in postsynaptic locations rather than presynaptic elements. EAAT4 is a minor transporter in the cerebellar cortex, located on dendritic spines of Purkinje neurons [5]. Currently, the role of the presynaptic GluT remains hypothetical and will continue to be such at least until the nature of the transport system i.e. which form(s) or variant(s) of EAAT2/GLT1 or any other EAATs, is/are adequately described.
EAATs have also been widely reported outside the CNS. For example, GluT with properties similar to those observed in the CNS was found to be present in cultured 3T3 fibroblasts [43]. Analogous GluT systems were subsequently characterized in fibroblasts derived from several types of human tissue; although various EAATs were identified there by EAAT-selective antibodies, GLAST, or, possibly, GLT would seem to be the two most active EAATs in such preparations [44].
GLAST was found to be present and probably functional at the mammalian neuromuscular junction [45], in the choroid plexus [46] and in other tissues, for example in pancreas [47] and in the heart muscle cells where it may have an important function [48]. GLT and possibly other EAATs exist in testes [49, 50] and EAAT5 is present in many peripheral tissues [42, 51]. In general, GluT outside the CNS is likely to be involved in a variety of specific physiological processes that may or may not be directly related to the activity of peripheral nerves or any other excitable tissue [52].
At this point, it should be emphasized that the reliability of all data concerning the presence or absence of EAATs, whether in the CNS or in the rest of the body, is only as good as the quality and reliability (i.e. specificity) of antibodies (review: [5]), or, if mRNA is detected, on the selection of hybridizing oligonucleotides. EAATs tend to be present in many splice variants [53, 54] and are susceptible to post-translational modification such as phosphorylation and glycosylation so some forms of EAAT may easily escape attention. It is, therefore, not advisable to draw final conclusions as to the presence/absence and/or changes in the expression of any EAAT on the basis of data from a single antibody that may not recognise the rich diversity of EAAT splice variants and their post-translationally modified forms.
EAAT1, EAAT2, EAAT3, EAAT4, and EAAT5 transporters in humans and their mouse and rat homologues GLAST, GLT1, EAAC1, EAAT4 and EAAT5 are encoded by SLC1A3, SLC1A2, SLC1A1, SLC1A6, and SLC1A7 genes, respectively. In the remainder of this article, we shall look at and compare what is known of the genetics and epigenetics of the two most abundant EAATs: EAAT1/GLAST (SLC1A3) and EAAT2/GLT1 (SLC1A2) in human brain. We shall also briefly review short-term (non-genetic, non-epigenetic) regulation of EAAT1/GLAST and, when relevant, we shall include involvement of EAATs malfunction in disease, particularly in alcoholism.
Genetics of Human EAATs; Possible Involvement in Disease
Human SLC1A3 (encoding EAAT1) gene is located on chromosome 5 (5p13.2). The entire gene comprises 81980 bp and has 10 exons. To date, at least 16 splice variants of SLC1A3 gene have been described (e.g. [53–55]) but additional splice variants are likely to be discovered.
There are 1701 polymorphic sites that have so far been discovered in SLC1A3 gene. Two different mutations of SLC1A3 gene have been reported in patients with episodic ataxia (EA). The mutation rs137852619 in the SLC1A3 gene, resulting in Pro290Arg amino acid change was described by Jen et al. [56] in a juvenile patient displaying EA type 2 (EA2) with seizures, migraine, and alternating hemiplegia. MRI showed cerebellar atrophy, and neurologic examination showed mild interictal truncal ataxia. Functional expression studies showed decreased expression of the mutant EAAT1 protein with a markedly reduced capacity for GluT. This partial “human knockout” exhibits a phenotype which suggests that any potential compensatory up-regulation of EAAT2 is not sufficient to prevent damage or developmental perturbation of the brain. De Vries et al. [57] identified mutation rs137852620 in three members of a Dutch family with EA resulting in a Cys186Ser substitution in EAAT1. In these patients no mutations were found in the CACNA1A gene even though they showed symptoms of EA usually characteristic of EA2 and including interictal nystagmus (but no myokymia), attacks of mild ataxia with a duration of several hours and a positive response to acetazolamide. Additional associated symptoms such as vertigo, nausea/vomiting and photophobia were also present. The syndrome was designated as EA, type 6; in studies in vitro, this mutation produced an 18 % decrease in GluT compared to the normal (wild type) transporter [57].
Several other DNA polymorphisms of SLC1A3 gene have been studied in association studies of ADHD, schizophrenia, Gilles de la Tourette syndrome, glaucoma; mostly with negative results [58–61]. Murphy et al. [62] noted a weak association between suicidal behaviour and rs2269272 polymorphism. Turic et al. [63] described association between ADHD and rs2269272 polymorphism. Walsh et al. [64] published results of copy number variation (CNV) analysis of whole genome in patients with schizophrenia (150 cases) and controls (268 cases). He described microdeletion or microduplication in SLC1A3 gene in four cases of schizophrenic patients but none in controls. This could suggest a possible relationship between SLC1A3 gene mutation and schizophrenia. In this context, it may be of interest to mention that Shan et al. [65] reported decreased expression of EAAT1 protein in the superior temporal gyrus of patients with schizophrenia.
Human SLC1A2 (encoding EAAT2) gene is located to chromosome 11 (11p13-p12). The entire gene comprises 168859 bp and 17 exons. So far, 8 splicing variants of SLC1A2 have been described. To date, 3767 DNA polymorphisms have been discovered in this gene.
We have performed a guided computer analysis [66] of SLC1A2 mRNA and we have found several binding sites for miRNAs. We have found hsa-miR-19b-3p that has been reported to be upregulated in serum of children with autism [67]; in fact, hsa-miR-19b-3p has been suggested as a possible candidate for circulating miRNA-based prediction-marker of autism. Among other miRNA’s of interest here, hsa-miR-5585-5p was found to be associated with glioblastoma [68], hsa-miR-5095 and hsa-miR-1273a were detected in microvesicles released from glioma cells [69] and hsa-miR-136-5p was reported as associated with Alzheimer’s disease [70].
Association studies bewteen SLC1A2 gene and essential tremor yielded ambiguous results as they seemed to be reliant on the studied populations, diagnostic criteria, sample sizes etc. [71]. Fiorentino et al. [72] suggested that rare variants in the SLC1A2 gene may confer susceptibility to schizophrenia and bipolar disorder.
Mechanisms of EAATs involvement in neurological disease given the high abundance of EAATs in brain tissue coupled with the ubiquity of glutamatergic excitatory synapses, where EAATs appear to be indispensable, it would seem almost obvious that any changes in the expression, location or functional characteristics would have far-reaching consequences and could underlie pathologies of many neurological disorders. Indeed, it follows from what has been discussed so far that any deficiency in GluT could lead to chronically increased concentrations of l-Glu at the synapse and in its immediate environment. Such “hyperglutamatergic” state could profoundly influence the brain function and even result in l-Glu “excitotoxicity” producing neuronal death. The hyperglutamatergic excitotoxicity associated with the dysfunction of GluT may not be at work only in the “obvious” neurodegenerative diseases such as amyotrophic lateral sclerosis, Alzheimer disease or Huntington’s chorea [73, 74; reviews: 6, 7, 75]. For example, Ye et al. [76] analysed glioma cell lines from human brain tumours and this revealed up to 100-fold lower glutamate reuptake in comparison with normal astrocytes. There was both lower expression and change in subcellular distribution of EAAT1 in glioma cells compared to healthy astrocytes. Ye et al. [76] hypothesized that the brain necrosis and seizures typical for patients with glioblastoma could be influenced by unusual glutamate release from glioma cells; the effect could be directly linked to a deficient GluT by the pathologically transformed glia. The lack of reuptake (perhaps in addition to “leaky” plasma membranes in such glia or regulated release of glutamate by the glia, i.e. “gliotransmission”) would lead to higher extracellular concentrations of l-Glu and result in overexcitation and neurotoxicity associated with glioblastomas.
Interestingly, it has been suggested that a hyperactive GluT could contribute to the etiology of schizophrenia (characterised at least in part as exhibiting features of reduced glutamatergic neurotransmission) and this has been supported by several studies. Neuroleptics such as clozapine and haloperidol have been shown to downregulate GluT, GLT1 in particular [77, 78]. In addition, there is evidence from human studies that EAAT2/GLT1 may be significantly upregulated in parts of brain which display deficiencies in schizophrenia ([79]; review [80]). It is plausible that increased EAAT expression could lead to the hypoglutamatergic transmission state in such patients.
Complete knockout of GLT1 has initially no apparent serious consequences but the (-/-) GLT1 animals eventually develop severe seizures and tend to die prematurely with only about 50 % surviving at 6 weeks of age [81]. More recent studies, however, using a conditional knockout [82], show that there is only modest impact on adult animals when 80 % or more of the GLT1 is knocked out, suggesting that the lethality of GLT1 knockout in younger animals might be a consequence of a developmental event such as the known transient over-expression of NMDA receptors that is observed in the developing rodent brain. Accordingly, GLT1 may not be as essential for the adult brain as previously thought. Complete knockout of GLAST produced less serious defects than the complete knockout of GLT1 [83]. Obviously, there was a degree of compensation with the missing EAAT being, to some extent, substituted by the other most abundant one. Double knockout (both GLT and GLAST), however, resulted invariably in a sudden death in utero at about E17/E18 [84], illustrating the absolute necessity of GluT, at the very least, in brain development. The timelines for death appear to coincide approximately with the timeline for expression of GLT1 in the brain, but somewhat later than the initial timeline for expression of GLAST [85]. Interestingly, the pathology of the double knockout is complex and includes, for example, deficits in callosal formation, which argue for glutamate acting on multiple targets and against death being due solely to an excitotoxicity event.
Realization that deficient GluT could be, if not a cause, than at least a contributory factor, in the neuronal death as it occurs in neurodegenerative diseases resulted in several studies aimed at finding how to increase and restore the normal expression of EAAT (for reviews see [86, 87]). Several mechanisms capable of (up)regulating EAATs have been identified but neither of them helped to satisfactorily explain aetiology of any neurological disorder nor have they been shown to lead to a development of any truly useful therapies which would prevent or at least significantly slow down the neuronal death [88, 89]. One remarkable aspect of these studies is that they have been targeting, in almost all cases, EAAT2/GLT1 rather than EAAT1/GLAST. Given the already highly abundant expression of GLT1 by astrocytes, there is potentially only a limited capacity for the cells to further increase GLT1 expression, whereas there may be lesser impediments to the up-regulation of GLAST.
Epigenetics and Transcription Regulation of EAATs
Expression of EAATs is regulated by several mechanisms; this topic has been researched and reviewed extensively in recent years. In short, there are mechanisms capable to upregulate or downregulate glutamate transporters and they can operate at the level of transcription, or translation, via epigenetic mechanisms or in response to changes in the immediate environment (reviews: [6, 90, 91]).
Unger et al. [90] performed software analysis of the human EAAT1 promoter and identified 13 potential target sites for transcription factors. Furthermore, in her experimental studies in vitro, Unger et al. [90] described stimulatory effects of dbcAMP, PACAP, EGF, and TGFα on EAAT1 gene expression. Additional transcription regulators potentially active at the promoter (CART, CEBP, GATA, HAML, MZF1, NFjB, NKXH, Oct1, SP1, and YY1F) are yet to be evaluated.
Interestingly, in an earlier study, brain derived neurotrophic factor (BDNF) was found to have no effect on EAAT1/GLAST expression by cultured astrocytes [92]. This is in contrast with more recent investigation showing that BDNF can up-regulate GLAST, at least in the retina [93]. The GLAST upregulation would result in a more rapid clearance of l-Glu and this mechanism in concert with the concommitant increase in glutamine synthase which catabolises any accumulated glutamate, could contribute to the neuroprotective effects of BDNF [93]. Furthermore, the BDNF effect on EAAT1/GLAST expression might explain results of an association study which uncovered a relationship between 66Met allele of BDNF (that is associated with an increased BDNF expression) and protection of patients with alcoholism from colour vision deficiency induced by long-term excessive alcohol intake and thought to be linked to an increased NMDA receptor density [94].
Most of the other studies have been focusing on EAAT2/GLT1; this should not surprise as this transporter is not only responsible for much of GluT in brain tissue (perhaps 90 %, [8]; recent review: [95]) but also because it is, as discussed above, the EAAT most often related to neurological and mental diseases [reviews: 5, 7, 8, 75]. For example, the mechanisms of action of the antibiotic ceftriaxone that has been used to upregulate EAAT2/GLT1 in animal experiments and tested in human trials as a potential therapeutic agent for amyotrophic lateral sclerosis [87–89], have been investigated in great detail; ceftriaxone seems to upregulate EAAT2/GLT1 via the transcription factor NFκB signalling pathway [96]. Another case of a EAAT2/GLT1-focused study is a recent identification of a neuronal miRNA which can regulate EAAT2/GLT1 expression in astrocytes [97].
Studies of epigenetic regulation of EAATs expression have barely begun [review: 6]. In our current investigations we have performed CpG island analysis of 5′ end of SLC1A3 human gene (RefSeq: JQ085380, GenBank). Using the software of Takai and Jones [98] we have found no CpG islands; this would seem to suggest that the methylation of that part of the gene is not an important regulatory mechanism of the human EAAT1 expression.
In the case of human EAAT2, CpG island analysis of 5′ end of SLC1A3 gene (RefSeq: EF078920, GenBank) by the same method [98] identified a CpG island spanning 1515 bp upstream of the first exon. Interestingly, Zschocke et al. [99] found that the lack of EAAT2 expression in human glioma cell lines was associated with a densely methylated SLC1A2 promoter. This contrasts with a hypomethylation of the same promoter region of SLC1A2 gene in normal human brain. It is therefore, probable that EAAT2 expression is, at least in part, regulated by the differential methylation of the SLC1A2 gene promoter. Perisic et al. [100] have recently extended the earlier studies and provided a more detailed analysis of the methylation site at the SLC1A2 (EAAT2/GLT1) promoter in the rat brain. They found higher methylation in the cerebellum compared to the cerebral cortex which is in agreement with the differential distribution of EAAT2/GLT1 in the mammalian CNS [reviews: 5, 15].
Rapid Regulation of GluT Activity by Other Than Genetic or Epigenetic Mechanisms
EAATs are not only subject to genetic or epigenetic regulation; there are important mechanisms which can activate GluT on the scale of seconds, minutes and hours and are independent of the mechanisms such as transcription, translation or DNA methylation. It was shown many years ago that GluT could be “activated” in the presence of its substrate [101]. It was later demonstrated that, in particular in the case of EAAT1/GLAST, there can be a shift from an “inactive” pool of the transporter in the cytoplasm to the “active” location in the plasma membrane in response to the presence of l-Glu (or indeed any other transportable EAAT substrate) in the extracellular environment (for a review and discussion see [102]).
The movements of GLAST in response to D-aspartate and other transportable substrates have been visualised in cultured astrocytes and it has been shown that they are sensitive to inhibitors of enzymes mediating phosphorylation (protein kinase C-delta [103, 104]) and dephosphorylation (okadaic acid; inhibitor of protein phosphatases [104, 105]). Use of rottlerin as an inhibitor of PKC-δ in these studies has, however, been questioned and alternative explanations for its actions have been advanced including an inhibitory effect of rottlerin on Na+,K+-dependent ATPase [105–107]. Indeed, there is evidence that glutamate transporters, including EAAT1/GLAST, are colocalized in the plasma membrane with Na+/K+-dependent ATPase [14, 108–110], which drives the GluT by generating the necessary ionic gradients directly into a local subcellular microdomain. Other enzymes and even mitochondria have been suggested to exist in a tight complex [110] driving and regulating GluT. In fact, combined effects of subtoxic doses of metabolic inhibitors and compounds which interfere with GluT will cause neuronal death both in mixed cultures of neurons and glia and in vivo [111, 112] thus further illustrating the tight functional relationship between energy supplying metabolic enzyme systems and GluT.
EAAT1/GLAST: Possible Role in Alcoholism?
Rimondini et al. [113] reported an increase in the expression of EAAT1/GLAST in the cingulate cortex of rats intermittently exposed to ethanol vapours. Furthermore, similar or higher overexpression of EAAT1/GLAST has been reported in post mortem brains of patients suffering from alcoholism [114]. In fact the increase in EAAT1/GLAST, studied by Western blotting using a custom-prepared antibody was among the quantitatively largest neurochemical changes reported in alcoholism [114]. At about the same time, it was noted [115] that mutant mice transfected with a mutant gene Per2 (Period2) that had been shown to associate with alcoholism in humans displayed a lower level of EAAT1/GLAST (but not that of EAAT2/GLT which might have even shown a modest compensatory increase [115]). Significantly, the affected mutant mice were more prone to drinking alcohol than the wild type mice, when given a choice. The overall lower activity of EAAT1/GLAST appeared to be a result of a disturbed diurnal cycle in EAAT1/GLAST expression which might have lead to “hyperglutamatergic” states i.e. increased concentration of l-Glu in the extracellular space, overexcitation of neurons which would then be compensated by the intake of alcohol and ensuing inhibition of the NMDA-type of glutamate receptors (review: [116]). This mechanism, however, does not directly explain the observed increase in EAAT1/GLAST apparently caused by long-term excessive drinking; one might surmise though that the increase in EAAT1/GLAST is a part of a compensatory mechanism responding to the excessive extracellular levels of l-Glu [117]. In order to further explore mechanisms by which alcohol may influence the activity of GluT we initiated experiments testing alcohol effects on the distribution of GLAST in astrocytes derived from neonatal rats.
Presence of D-aspartate and other substrates of GluT can produce a shift of EAAT1/GLAST from a cytoplasmic compartment (possibly in the form of small vesicles) to the plasma membrane which may be accompanied by an increase in GluT [103–106]. We have carried out a series of preliminary experiments testing a hypothesis that ethanol interferes with this mechanism thus perhaps increasing the need for expression of additional GLAST protein to keep GluT functioning. In fact, we found that ethanol itself, at concentrations which can occur during heavy drinking [118], caused a shift of GLAST from cytoplasm to the plasma membrane. Some of the results are shown in Fig. 1.
Effect of alcohol on the distribution of GLAST in the cultured rat astrocytes. Cultured astrocytes were prepared from foetal rat brains and cultured as described previously [104]. Distribution of GLAST antibody (same antibody as used before [104–106]) is expressed as relative fluorescence index defined as earlier [104]. Essentially, when RFI = 1, the fluorescence (GLAST) is distributed approximately equally between the plasma membrane and cytoplasm, while RFI >1 signifies shift of the fluorescence (GLAST) to the membrane. The results are means SEM from 5 to 11 randomly selected cells. The value of RFI in the presence of 100 mM ethanol is significantly different from control (P < 0.05) and RFI under 100 mM ethanol plus 300 µM baclofen is significantly lower (P < 0.05) than the RFI observed with after 100 mM ethanol only (both marked with an asterisk; not all statistically significant differences are marked). Statistics were computed by ANOVA multiple comparisons using Tukey’s test. Baclofen alone produced no significant effect. The cells were incubated in the presence of drugs for 45 min
We do not yet know whether the effect of alcohol is accompanied by an increased GluT, however, we noticed that baclofen, a GABA(B) agonist that has been proposed as a drug alleviating pathological alcohol-craving in alcohol-dependent humans [119, 120] reversed this process (Fig. 1). The mechanism of baclofen actions on craving is not clear but it may be related to a GABA(B) receptor mediated regulation of one of the fibre tracts from midbrain to ventral striatum which are involved in actions of psychoactive drugs such as alcohol [121].
The activation of EAAT1/GLAST by ethanol is consistent with the “hyperglutamatergic” hypothesis of alcoholism, particularly as it applies to the mechanism of “craving” and its relief by ethanol. Ethanol would not only antagonize the effect of the high extracellular l-Glu by inhibiting NMDA receptors but could further relieve the stressed/overexcited neurons by activating EAAT1/GLAST which would then move excess l-Glu away from the extracellular space into the surrounding astrocytes. This mechanism could reinforce the chronic upregulation of EAAT1/GLAST thus facilitating the rapid relief of hyperglutamatergic states by ingested ethanol.
As there are few or no data on the effect of baclofen during heavy alcohol intoxication, at least not at the cellular/molecular level, and we have not yet tested an effect of baclofen on EAAT1/GLAST in astrocytes previously chronically exposed to ethanol, we cannot unequivocally relate the current observations to the “anti-craving” effect of baclofen. The above finding, however, represents the first identification of a possible common molecular target of ethanol and baclofen in brain and further underscores the central position of GluT in regulating synaptic functions in brain. It also potentially expands the “glutamatergic” hypothesis of alcoholism perhaps providing an additional therapeutic target [122, 123].
Concluding Remarks
We have presented a brief summary of the most important information on the location and function of excitatory amino acid transporters (EAATs) in brain. Additionally, we have surveyed recent progress in genetics and epigenetics of EAAT1/GLAST and EAAT2/GLT and extracted (“in silico”) some new information on the corresponding genes, particularly with respect to the transcriptional and epigenetic regulation of their expression. We have also addressed the question of rapid regulation of EAAT1/GLAST in response to extracellular environment and presented preliminary data which, together with existing data in the literature, support the role of glutamate transport (GluT)—particularly that which is mediated by EAAT1/GLAST—in the brain cells exposed to alcohol.
We conclude that, in general, the role of EAAT1/GLAST has not been given sufficient attention; there is evidence that GLAST can be functionally upregulated to a significant extent and potentially targeted to functional compartments, such that it can reduce excitotoxicity. Obviously the desired pharmacological tool to evoke this type of upregulation to deal with disease states such as ALS or stroke is probably not alcohol, but the mechanisms underpinning this upregulation indicate tremendous scope for manipulating GLAST expression to minimise excitotoxicity. There is a scope for a great expansion of research into the regulation of EAAT1/GLAST at transcriptional, translational, epigenetic and cellular level in both health and disease.
References
Fonnum F (1984) Glutamate: a neurotransmiter in mammalian brain. J Neurochem 42:1–11
Bennett MR, Balcar VJ (1999) Forty years of amino acid transmission in the brain. Neurochem Int 35:269–280
Zhu Y, Danbolt NC (2014) Glutamate as a neurotransmitter in the healthy brain. J Neural Transm 121:799–817
Omote H, Miyaji T, Juge N, Moriyama Y (2011) Vesicular neurotransmitter transporter: bioenergetics and regulation of glutamate transport. Biochemistry 50:5558–5565
Danbolt NC (2001) Glutamate uptake. Prog Neurobiol 65:1–105
Grewer C, Gameiro A, Rauen T (2014) SLC1 glutamate transporters. Pflügers Arch 466:3–24. doi:10.1007/s00424-013-1397-7
Beart PM, O’Shea RD (2007) Transporters for l-glutamate: an update on their molecular pharmacology and pathological involvement. Br J Pharmacol 250:5–17. doi:10.1038/sj.bjp.0706949
Zhu Y, Danbolt NC (2013) GABA and glutamate transporters in brain. Front Neuroendocrinol 4(165):1–14. doi:10.3389/fendo.2013.00165
Zerangue N, Kavanaugh MP (1996) Flux coupling in a neuronal glutamate transporter. Nature 383:634–637. doi:10.1038/383634a0
Levy LM, Warr O, Attwell D (1998) Stoichiometry of the glial glutamate transporter GLT-1 expressed inducibly in a chinese hamster ovary cell line selected for low endogenous glutamate uptake. J Neurosci 18:9620–9628
Owe SG, Marcaggi P, Attwell D (2006) The ionic stoichiometry of the GLAST glutamate transporter in salamander retinal glia. J Physiol 577:591–599
Minelli A, Barbaresi P, Reimer RJ, Edwards RH, Conti F (2001) The glial glutamate transporter GLT1 is localized both in the vicinity of and at distance from axon terminals in the rat cerebral cortex. Neuroscience 108:51–59
Melone M, Bellesi M, Ducati A, Iacoangeli M, Conti F (2011) Cellular and synaptic localization of EAAT2a in human cerebral cortex. Front Neuroanat 4:151. doi:10.3389/fnana.2010.00151
Cholet N, Pellerin L, Magistretti PJ, Hamel E (2002) Similar perisynaptic glial localization for the Na+ , K+-ATPase α2 subunit and the glutamate transporters GLAST and GLT1 in the rat somatosensory cortex. Cereb Cortex 12:515–525
Sullivan SM, Lee A, Björkman ST, Miller SM, Sullivan RK, Poronnik P, Colditz PB, Pow DV (2007) Cytoskeletal anchoring of GLAST determines susceptibility to brain damage: an identified role for GFAP. J Biol Chem 282:29414–29423
Balcar VJ (2002) Molecular pharmacology of the Na+-dependent transport of acidic amino acids in the mammalian brain. Biol Pharmacol Bull Jpn Pharm Soc 25:291–301
Roberts RC, Roche JK, McCullumsmith RE (2014) Localization of excitatory amino acid transporters EAAT1 and EAAT2 in human postmortem cortex: a light and electron microscopic study. Neuroscience 277:522–540. doi:10.1016/j.neuroscience.2014.07.019
Sullivan SM, MacNab LT, Björkman ST, Colditz PB, Pow DV (2007) GLAST1b, the exon-9 skipping form of the glutamate-aspartate transporter EAAT1 is a sensitive marker of neuronal dysfunction in the hypoxic brain. Neuroscience 149:434–445
Meaney JA, Balcar VJ, Rothstein JD, Jeffrey PJ (1998) Glutamate transport in cultures from developing avian cerebellum: presence of GLT1 immunoreactivity in Purkinje neurons. J Neurosci Res 54:595–603
Plachez C, Danbolt NC, Récasens M (2000) Transient expression of the glial glutamate transporters GLAST and GLT in hippocampal neurons in primary culture. J Neurosci Res 59:587–593
Jeffrey PL, Balcar VJ, Tolhurst O, Weinberger RP, Meaney JA (2003) Avian Purkinje neuronal cultures: extrinsic control of morphology by cell type and glutamate. Methods Cell Biol 71:89–109
Gundersen V, Danbolt NC, Ottersen OP, Storm-Mathisen J (1993) Demonstration of glutamate/aspartate uptake activity in nerve endings by use of antibodies recognizing exogenous D-aspartate. Neuroscience 57:97–111
Furness DN, Dehnes Y, Akhtar AQ et al (2008) A quantitative assessment of glutamate uptake into hippocampal synaptic terminals and astrocytes: new insights into a neuronal role for excitatory amino acid transporter 2 (EAAT2). Neuroscience 157:80–94
Chen W, Mahadomrongkul V, Berger UV et al (2004) The glutamate transporter GLT1a is expressed in excitatory axon terminals of mature hippocampal neurons. J Neurosci 24:1136–1148
Berger UV, Hediger MA (1998) Comparative analysis of glutamate transporter expression in rat brain using differential double in situ hybridization. Anat Embryol (Berlin) 198:13–30
Sonnewald U (2014) Glutamate synthesis has to be matched by its degradation—Where do all the carbons go? J Neurochem 13:399–406. doi:10.1111/jnc.12812
Billups D, Marx MC, Mela I, Billups B (2013) Inducible presynaptic glutamine transport supports glutamatergic transmission at the calyx of Held synapse. J Neurosci 33:17429–17434. doi:10.1523/JNEUROSCI.1466-13.2013
Bjørnsen LP, Hadera MG, Zhou Y, Danbolt NC, Sonnewald U (2014) The GLT-1 (EAAT2; slc1a2) gluamate transporter is essential for glutamate homeostasis in the cortex of the mouse. J Neurochem 128:641–649
Petr GT, Sun Y, Frederick NM, Zhou Y, Dhamne SC, Hameed MQ, Miranda C, Bedoya EA, Fischer KD, Armsen W, Wang J, Danbolt NC, Rotenberg A, Aoki CJ, Rosenberg PA (2015) J Neurosci 35:5187–5201. doi:10.1523/JNEUROSCI.4255-14.2015
Rae C, Hare N, Bubb WA, McEwan SR, Bröer A, McQuillan JA, Balcar VJ, Conigrave AD, Bröer S (2003) Inhibition of glutamate transport depletes glutamate and GABA neurotranspitte pools: further evidence for metabolic compartmentation. J Neurochem 85:503–514
Marx M-C, Billups D, Billups B (2015) Maintaining the presynaptic glutamate supply for excitatory neurotransmission. J Neurosci Res. doi:10.1002/jnr.23561
Bridges RJ, Esslinger CS (2005) The excitatory amino acid transporters: pharmacological insights on substrate and inhibitor specificity of the EAAT subtypes. Pharmacol Ther 107:271–285
Moussa CEH, Mitrovic AD, Vandenberg RJ, Provis Rae C, Bubb WA, Balcar VJ (2002) Effects of l-glutamate transport inhibition by a conformationally restricted glutamate analogue (2S,1′S, 2′R)-2-(carboxycyclopropyl)glycine (L-CCG III) on metabolism in brain tissue in vitro analysed by NMR spectroscopy. Neurochem Res 27:27–35
Moussa CEH, Rae C, Bubb WA, Griffin JL, Deters NA, Balcar VJ (2007) Inhibitors of glutamate transport modulate distinct pattern in brain metabolism. J Neurosci Res 85:342–350
Lehre KP, Rusakov DA (2002) Asymetry of glia near central synapses favors presynaptically directed glutamte escape. Biophys J 83:125–134
Fairman WA, Vandenberg RJ, Arriza JL, Kavanaugh MP, Amara SG (1995) An excitatory amino-acid transporter with properties of ligand-gated chloride channel. Nature 375:599–603
Vandenberg RJ, Ryan RM (2013) Mechanisms of glutamate transport. Phys Rev 93:1621–1657. doi:10.1152/physrev.00007.2013
Wersinger E, Schwab Y, Sahel JA, Rendon A, Pow DV, Picaud S, Roux MJ (2006) The glutamate transporter EAAT5 works as a presynaptic receptor in mouse rod bipolar cells. J Physiol 577(Pt 1):221–234
Veruki ML, Mørkve SH, Hartveit E (2006) Activation of a presynaptic glutamate transporter regulates synaptic transmission trough electrical signaling. Nat Neurosci 9:1388. doi:10.1038/nn1793
Machtens J-P, Kortzak D, Lansche C, Leinenweber A, Kilian P, Begemann B, Zachariae U, Ewers D, de Groot BL, Briones R, Fahlke C (2015) Mechanisms of anion conduction by coupled glutamate transporters. Cell 160:542–553. doi:10.1016/j.cell.2014.12.035
Sogaard R, Borre L, Braunstein T, Madsen KL, MacAulay N (2013) Functional modulation of the glutamate transporter variant GLT1b by the PDZ domain protein PICK1. J Biol Chem 288:20195–20207. doi:10.1074/jbcM113.471128
Ochiai H, Saito M, Maruo T, Kanemaki N (2010) Molecular cloning of excitatory amino acid transporter 5 and its detection in primary lens epithelial cells. Exp Anim 59:449–457
Balcar VJ (1992) Na(+)-dependent high-affinity uptake of l-glutamate in cultured fibroblasts. FEBS Lett 300:203–207
Cooper B, Chebib M, Shen J, King NJC, Darvey IG, Kuchel PW, Rothstein JD, Balcar VJ (1998) Structural selectivity and molecular nature of l-glutamate transport in cultured human fibroblasts. Arch Biochem Biophys 353:356–364
Rinholm JE, Slettaløkken G, Marcaggi P, Skare Ø, Storm-Mathisen J, Bergersen LH (2007) Subcellular localization of the glutamate transporters GLAST and GLT at the neuromuscular junction in rodents. Neuroscience 145:579–591
Lee A, Anderson AR, Rayfield AJ, Stevens MG, Poronnik P, Meabon JS, Cook DG, Pow DV (2012) Localisation of novel forms of glutamate transporters and the cystine-glutamate antiporter in the choroid plexus: implications for CSF glutamate homeostasis. J Chem Neuroanat 43:64–75. doi:10.1016/j.jchemneu.2011.09.006
Meabon JS, Lee A, Meeker KD, Bekris LM, Fujimura RK, Yu C-E, Watson GS, Pow DV, Sweet IR, Cook DG (2012) Differential expression of the glutamate transporter GLT1 in pancreas. J Histochem Cytochem 60:139–151
Magi S, Arcangeli S, Castaldo P, Assunta Nasti A, Berrino L, Piegari L, Bernardini R, Amoroso S, Lariccia V (2013) Glutamate-induced ATP synthesis: relationship between plasma membrane Na+/Ca2+ exchanger and excitatory amino acid transporters in brain and heart cell models. Mol Pharmacol 84:503–614
Takarada T, Hinoi E, Balcar VJ, Taniura H, Yoneda Y (2004) Possible expression of functional glutamate transporters in rat testes. J Endocrinol 181:233–244
Lee A, Anderson AR, Barnett AC, Chan A, Pow DV (2011) Expression of multiple glutamate transporter splice variants in the rodent testis. Asian J Androl 13:254–265. doi:10.1038/aja.2010.99
Lee A, Anderson AR, Stevens MG, Beasley S, Barnett Pow DV (2013) Excitatory amino acid transporter 5 is widely expressed in peripheral tissues. Eur J Histochem 57:e11
Berger UV, Hediger MA (2006) Distribution of the glutamate transporters GLT1 (SLC1A2) and GLAST (SLC1A3) in peripheral organs. Anat Embryol 211:595–606. doi:10.1007/s))429-006-0109-x
Lee A, Pow DV (2010) Astrocytes: glutamate transport and alternate splicing of transporters. Int J Biochem Cell Biol 42:1901–1906
Lee A, Anderson AR, Beasley SJ, Barnett NL, Poronnik P, Pow DV (2012) A new splice variant of the glutamate-aspartate transporter: cloning and immunolocalization of GLAST1c in rat, pig and human brains. J Chem Neuroanat 43:52–63. doi:10.1016/j.jchemneu.2011.09.005
Vallejo-llaramendi A, Domercq M, Matute V (2005) A novel alternative splicing form of excitatory amino acid transporter 1 is a negative regulator of glutamate uptake. J Neurochem 295:341–348
Jen JC, Wan J, Palos TP, Howard BD, Baloh RW (2005) Mutation in the glutamate transporter EAAT1 causes episodic ataxia, hemiplegia, and seizures. Neurology 65:529–534
de Vries B, Mamsa H, Stam AH, Wan J, Bakker SL, Vanmolkot KR, Haan J, Terwindt GM, Boon EM, Howard BD, Frants RR, Baloh RW, Ferrari MD, Jen JC, van den Maagdenberg AM (2009) Episodic ataxia associated with EAAT1 mutation C186S affecting glutamate reuptake. Arch Neurol 66:97–101. doi:10.1001/archneurol.2008.535
Elia J, Capasso M, Zaheer Z, Lantieri F, Ambrosini P, Berrettini W, Devoto M, Hakonarson H (2009) Candidate gene analysis in an on-going genome-wide association study of attention-deficit hyperactivity disorder: suggestive association signals in ADRA1A. Psychiatr Genet 19:134–141. doi:10.1097/YPG.0b013e32832a5043
Deng X, Shibata H, Takeuchi N, Rachi S, Sakai M, Ninomiya H, Iwata N, Ozaki N, Fukumaki Y (2007) Association study of polymorphisms in the glutamate transporter genes SLC1A1, SLC1A3, and SLC1A6 with schizophrenia. Am J Med Genet B Neuropsychiatr Genet 144B:271–278
Laurin N, Wigg KG, Feng Y, Sandor P, Barr CL (2009) Chromosome 5 and Gilles de la Tourette syndrome: linkage in a large pedigree and association study of six candidates in the region. Am J Med Genet B Neuropsychiatr Genet 150B:95–103. doi:10.1002/ajmg.b.30779
Yasumura R, Meguro A, Ota M, Nomura E, Uemoto R, Kashiwagi K, Mabuchi F, Iijima H, Kawase K, Yamamoto T, Nakamura M, Negi A, Sagara T, Nishida T, Inatani M, Tanihara H, Aihara M, Araie M, Fukuchi T, Abe H, Higashide T, Sugiyama K, Kanamoto T, Kiuchi Y, Iwase A, Ohno S, Inoko H, Mizuki N (2011) Investigation of the association between SLC1A3 gene polymorphisms and normal tension glaucoma. Mol Vis 17:792–796
Murphy TM, Ryan M, Foster T, Kelly C, McClelland R, O’Grady J, Corcoran E, Brady J, Reilly M, Jeffers A, Brown K, Maher A, Bannan N, Casement A, Lynch D, Bolger S, Tewari P, Buckley A, Quinlivan L, Daly L, Kelleher C, Malone KM (2011) Risk and protective genetic variants in suicidal behaviour: association with SLC1A2, SLC1A3, 5-HTR1B & NTRK2 polymorphisms. Behav Brain Funct 7:22. doi:10.1186/1744-9081-7-22
Turic D, Langley K, Williams H, Norton N, Williams NM, Moskvina V, Van den Bree MB, Owen MJ, Thapar A, O’Donovan MC (2005) A family based study implicates solute carrier family 1-member 3 (SLC1A3) gene in attention-deficit/hyperactivity disorder. Biol Psychiatry 57:1461–1466
Walsh T, McClellan JM, McCarthy SE, Addington AM, Pierce SB, Cooper GM, Nord AS, Kusenda M, Malhotra D, Bhandari A, Stray SM, Rippey CF, Roccanova P, Makarov V, Lakshmi B, Findling RL, Sikich L, Stromberg T, Merriman B, Gogtay N, Butler P, Eckstrand K, Noory L, Gochman P, Long R, Chen Z, Davis S, Baker C, Eichler EE, Meltzer PS, Nelson SF, Singleton AB, Lee MK, Rapoport JL, King MC, Sebat J (2008) Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science 320:539–543. doi:10.1126/science.1155174
Shan D, Lucas EK, Drummond JB, Haroutunian V, Meador-Woodruff JH, McCullumsmith RE (2013) Abnormal expression of glutamate transporters in temporal lobe areas in elderly patients with schizophrenia. Schizophr Res 144:1–8. doi:10.1016/j.schres.2012.12.019
Kozomara A, Griffiths-Jones S (2014) miRBase: annotating high confidence microRNAs using deep sequencing data. Nucleic Acids Res 42(Database issue):D68–D73
Vasu MM, Anitha A, Thanseem I, Suzuki K, Yamada K, Takahashi T, Wakuda T, Iwata K, Tsujii M, Sugiyama T, Mori N (2014) Serum microRNA profiles in children with autism. Mol Autism 5:40. doi:10.1186/2040-2392-5-40
Henriksen M, Johnsen KB, Olesen P, Pilgaard L, Duroux M (2014) MicroRNA expression signatures and their correlation with clinicopathological features in glioblastoma multiforme. Neuromol Med 16:565–577. doi:10.1007/s12017-014-8309-7
Li Y, Xu J, Chen H, Bai J, Li S, Zhao Z, Shao T, Jiang T, Ren H, Kang C, Li X (2013) Comprehensive analysis of the functional microRNA-mRNA regulatory network identifies miRNA signatures associated with glioma malignant progression. Nucleic Acids Res 41:e203. doi:10.1093/nar/gkt1054
Lau P, Bossers K, Janky R, Salta E, Frigerio CS, Barbash S, Rothman R, Sierksma AS, Thathiah A, Greenberg D, Papadopoulou AS, Achsel T, Ayoubi T, Soreq H, Verhaagen J, Swaab DF, Aerts S, De Strooper B (2013) Alteration of the microRNA network during the progression of Alzheimer’s disease. EMBO Mol Med 5:1613–1634. doi:10.1002/emmm.201201974
Kuhlenbäumer G, Hopfner F, Deuschl G (2014) Genetics of essential tremor: meta-analysis and review. Neurology 82:1000–1007. doi:10.1212/WNL.0000000000000211
Fiorentino A, Sharp SI, McQuillin A (2014) Association of rare variation in the glutamate receptor gene SLC1A2 with susceptibility to bipolar disorder and schizophrenia. Eur J Hum Genet. doi:10.1038/ejhg.2014.261
Rothstein JD, Martin LJ, Kuncl RW (1992) Decreased glutamate transport by the brain and spinal cord in amyotrophic lateral sclerosis. N Engl J Med 326:1464–1468
Howland DS, Liu J, She Y, Goad B, Maragakis NJ, Kim B, Erickson J, Kulik J, DeVito L, Psaltis G, DeGennaro LJ, Cleveland DW, Rothstein JD (2002) Focal loss of the glutamate transporter EAAT2 in a transgenic mutant-mediated amyotrophic lateral sclerosis (ALS). Proc Nat Acad Sci USA 99:1604–1609. doi:10.1073/pnas.042539299
Sheldon AL, Robinson MB (2007) The role of glutamate transporters in neurodegenerative disease and potential opportunities for intervention. Neurochem Int 51:333–355
Ye ZC, Rothstein JD, Sontheimer H (1999) Compromised glutamate transport in human glioma cells: reduction-mislocalization of sodium-dependent glutamate transporters and enhanced activity of cystine-glutamate exchange. J Neurosci 19:10767–10777
De Souza IE, McBean GJ, Meredith GE (1999) Chronic haloperidol treatment impairs glutamate transport in the rat striatum. Eur J Pharmacol 382:139–142
Melone M, Vitellaro-Zuccarello L, Vallejo-llaramendi A, Perez-Samartin A, Matute C, Cozzi A, Pellegrini-Giampetro DE, Rothstein JD, Conti F (2001) The expression of glutamate transporter GLT-1 in the rat cerebral cortex is down-regulated by the antipsychotic drug clozapine. Mol Psychiatry 6:380–386
Matute C, Melone M, Vallejo-Illarramendi A, Conti F (2005) Increased expression of the astrocytic glutamate transporter GLT-1 in the prefrontal cortex of schizophrenics. Glia 49:451–455
Nanitsos EK, Nguyen KTD, Stastny F, Balcar VJ (2005) Glutamatergic hypothesis of schizophrenia: involvement of Na+/K+-dependent glutamate transport. J Biomed Sci 12:975–984. doi:10.1007/s11373-005-9015-0
Tanaka K, Eatase K, Manabe T, Yamada K, Watanabe M, Takahashu K, Iwama H, Nishikawa T, Ichihara N, Kikuchi T, Okuyama S, Kawashima N, Hori S, Takimoto M, Wada K (1997) Epilepsy and exacerbation of brain injury in mice lacking the glutamate transporter GLT-1. Science 276:1699–1702
Aida T, Yoshida J, Nomura M, Tanimura A, Lino Y, Soma M, Bai N, Ito Y, Cui W, Aizawa H, Yanagisawa M, Nagai T, Takata N, Tanaka KF, Takanayagi R, Kano M, Götz M, Hirase H, Tanaka K (2015) Astroglial glutamate transporter deficiency increases synaptic excitability and leads to pathological repetitive behaviors in mice. Neuropsychopharmacol. doi:10.1038/npp.2015.26
Watase K, Hashimoto K, Kano M, Yamada K, Watanabe M, Inoue Y, Okuyama S, Sakagawa T, Ogawa S, Kawashima N (1998) Motor discoordination and increased susceptibility to cerebellar injury in GLAST mutant mice. Eur J Neurosci 10:976–988
Matsugami TR, Tanemura K, Mieda M, Nakatomi R, Yamada K, Kondo T, Ogawa M, Obata K, Watanabe M, Hashikawa T, Tanaka K (2006) Indispensability of the glutamate transporters GLAST and GLT1 to brain development. PNAS 103:12161–12166
Williams SM, Macnab LT, Pow DV (2006) Cryptic expression of functional transporters in the developing rodent brain. Neuron Glia Biol 2:199–215
O’Shea RD (2002) Roles and regulation of glutamate transporters in the central nervous system. Clin Exp Pharmacol Physiol 29:1018–1023
Rothstein JD, Patel S, Regan MR, Haenggeli C, Huang YH, Bergles DE, Jin L, Dykes-Hoberg M, Vidensky S, Chung DS, Toan SV, Bruijn LI, Su ZZ, Gupta P, Fisher PB (2005) Beta-lactam antibiotics offer neuroprotection by increasing glutamate transporter expression. Nature 433:73–77
Allritz C, Bette S, Figiel M, Engele J (2010) Comparative structural and functional analysis of the GLT-1/EAAT-2 promoter from man and rat. J Neurosci Res 88:1234–1241. doi:10.1002/jnr.22303
Cudkovicz ME, Titus S, Kearney M, Yu H, Sherman A, Schoenfeld D, Hayden D, Shui A, Brooks B, Conwit R, Felsenstein D, Greenblatt DJ, Keroac M, Kissel JT, Miller R, Rosenfeld J, Rothstein J, Simpson E, Tolkoff-Rubin N, Zinman L, Shefner JM, Ceftriaxone Study Investigators (2014) Safety and efficacy of ceftriaxone for amyotrophic lateral sclerosis: a multistage, randomised, double-blind, placebo-controlled trial. Lancet Neurol 13:1083–1091. doi:10.1016/S1474-4422(14)70222-4
Unger T, Lakowa N, Bette S, Engele J (2012) Transcriptional regulation of the GLAST/EAAT-1 gene in rat and man. Cell Mol Neurobiol 32:539–547. doi:10.1007/s10571-011-9790-2
Šerý O, Povová J, Balcar VJ (2014) Perspectives in genetic prediction of Alzheimer’s disease. Neuro Endocrinol Lett 35:359–366
Figiel M, Maucher T, Rozyczka J, Bayatti N, Engele J (2003) Regulation of glial glutamate transporter expression by growth factors. Exp Neurol 183:124–135
Dai M, Xia XB, Xiong SQ (2012) BDNF regulates GLAST and glutamine synthetase in mouse retinal Müller cells. J Cell Physiol 227:596–603. doi:10.1002/jcp.22762
Šerý O, Šťastný F, Zvolský P, Hlinomazová Z, Balcar VJ (2011) Association between Val66Met polymorphism of Brain-Derived Neurotrophic Factor (BDNF) gene and a deficiency of colour vision in alcohol-dependent male patients. Neurosci Lett 499:154–157. doi:10.1016/j.neulet.2011.05.038
Jensen AA, Fahlke C, Bjørn-Yoshimoto WE, Bunch L (2015) Excitatory amino acid transporters: recent insights into molecular mechanisms, novel modes of modulation and new therapeutic possibilities. Curr Opin Pharmacol 20C:116–123. doi:10.1016/j.coph.2014.10.008
Lee S-G, Su Z-Z, Emdad L, Gupta P, Sarkar D, Borjabad A, Volsky DJ, Fisher PB (2008) Mechanism of ceftriaxone induction of excitatory amino acid transporter-2 expression and glutamate uptake in primary human astrocytes. J Biol Chem 283:13116–13123. doi:10.1074/jbcM707697200
Morel L, Regan M, Higashimori H, Ng SK, Esau C, Vidensky S, Rothstein JD, Yang Y (2013) Neuronal exosomal miRNA-dependent translational regulation of astroglial glutamate transporter GLT1. J Biol Chem 288:7105–7116. doi:10.1074/jbcM112.410944
Takai D, Jones PA (2002) Comprehensive analysis of CpG islands in human chromosomes 21 and 22. Proc Natl Acad Sci U S A 99:3740–3745
Zschocke J, Allritz C, Engele J, Rein T (2007) DNA methylation dependent silencing of the human glutamate transporter EAAT2 gene in glial cells. Glia 55:663–674
Perisic T, Holsboer F, Rhein T, Zschocke J (2012) The CpG island shore of the GLT-1 gene acts as a methylation-sensitive enhancer. Glia 60:1345–1355
Duan S, Anderson CM, Stein BA, Swanson RA (1999) Glutamate induces rapid upregulation of astrocyte glutamate transport and cell-surface expression of GLAST. J Neurosci 19:10193–10200
Robinson MB (2002) Regulated trafficking of neurotransmitter transporters: common notes but different melodies. J Neurochem 80:1–11
Susarla BTS, Robinson MB (2003) Rottlerin, an inhibitor of protein kinase Cδ (PKCδ) inhibits astrocytic glutamate transport activity and reduces GLAST immunoreactivity by a mechanism that appears to be PKCδ-independent. J Neurochem 86:635–645
Shin JW, Nguyen KT, Pow DV, Knight T, Buljan V, Bennett MR, Balcar VJ (2009) Distribution of glutamate transporter GLAST in membranes of cultured astrocytes in the presence of glutamate transport substrates and ATP. Neurochem Res 34:1758–1766. doi:10.1007/s11064-009-9982-z
Nguyen KTD, Shin JW, Rae C, Nanitsos EK, Acosta GB, Pow DV, Buljan V, Bennett MR, Else PL, Balcar VJ (2009) Rottlerin inhibits (Na+, K+)-ATPase activity in brain tissue and alters D-aspartate dependent redistribution of glutamate transporter GLAST in cultured astrocytes. Neurochem Res 34:1767–1774. doi:10.1007/s11064-009-9996-6
Nguyen KTD, Buljan V, Else PL, Pow DV, Balcar VJ (2010) Cardiac glycosides ouabain and digoxin interfere with the regulation of glutamate transporter GLAST in astrocytes cultured from neonatal rat brain. Neurochem Res 35:2062–2069. doi:10.1007/s11064-010-0274-4
Sheean RK, Lau CL, Shin YS, O’Shea RD, Beart PM (2013) Links between l-glutamate trnsporters, Na+/K+-ATPase and cytoskeleton in astrocytes: evidence following inhibition with rottlerin. Neuroscience 254:335–346
Pellerin L, Magistretti PJ (1997) Glutamate uptake stimulates Na+ , K+-ATPase activity in astrocytes via activation of a distinct subunit highly sensistive to ouabain. J Neurochem 69:2132–3137
Nanitsos EK, Acosta GB, Saihara Y, Stanton D, Liao LP, Shin JW, Rae C, Balcar VJ (2004) Effects of glutamte transport substrates and glutamate receptor ligands on the activity of Na+/K+-ATPase in brain tissue in vitro. Clin Exp Pharmacol Physiol 31:762–769
Bauer DE, Jackson JG, Genda EN, Montoya MM, Yudkoff M, Robinson MB (2012) The glutamate transporter, GLAST, participates in a macromolecular complex that supports glutamate metabolism. Neurochem Int 61:566–574. doi:10.1016/j.neuint.2012.01.013
Sanchez-Carbente NR, Massieu L (1999) Transient inhibition of glutamate uptake in vivo induces neurodegeneration when energy metabolism is impaired. J Neurochem 72:129–138
Garcia O, Massieu L (2003) Glutamate uptake inhibitor L-trans-pyrrolidine-2,4-dicarboxylate becomes neurotoxic in the presence of subthreshold concentrations of mitochondrial toxin 3-nitropropionate: involvement of mitochondrial reducing activity and ATP production. J Neurosci Res 74:956–966
Rimondini R, Arlinde C, Sommer W, Heilig M (2002) Long-lasting increase in voluntary ethanol consumption and transcriptional regulation in the rat brain after intermittent exposure to alcohol. FASEB J 16:27–35
Flatscher-Bader T, Wilce PA (2008) Impact of alcohol abuse on protein expression of midkine and excitatory amino acid transporter 1 in the human prefrontal cortex. Alcohol Clin Exp Res 32:1849–1858. doi:10.1111/j.1530-0277.2008.00754.x
Spanagel R, Pendyala G, Abarca C, Zghoul T, Sanchis-Segura C, Magnone MC, Lascorz J, Depner M, Holzberg D, Soyka M, Schreiber S, Matsuda F, Lathrop M, Schumann G, Albrecht U (2005) The clock gene Per2 influences the glutamatergic system and modulates alcohol consumption. Nat Med 11:35–42
Spanagel R (2009) Alcoholism: a system approach from molecular physiology to addictive behaviour. Physiol Rev 89:649–705
Karlsson RM, Ademark L, Molander A, Perreau-Lenz S, Singley E, Solomon M, Holmes A, Tanaka K, Lovinger R, Spanagel MH (2012) reduced alcohol intake and reward associated with impaired endocannabinoid signalling in mice with a deletion of the glutamate transporter GLAST. Neuropharmacology 63:181–189. doi:10.1016/j.neuropharmacol.2012.01.027
Jones AW (1999) The drunkest drinking driver in Sweden: blood alcohol concentration 0.545 % w/v. J Stud Alcohol 60:400–406
Adolorato G, Leggio L, Agabio R, Colombo G, Gasbarrini G (2006) Baclofen: a new drug for the treatment of alcohol dependence. Int J Clin Pract 60:1003–1008
Leggio L, Garbutt JC, Addolorato G (2010) Effectivness and safety of baclofen in the treatment of alcohol dependent patients. CNS Neurol Disord Srug Targets 9:33–44
Chuhma N, Choi WY, Mingote S, Rayport S (2009) Dopamine neuron glutamate cotransmission: frequency-dependent modulation in the mesoventromedial projection. Neuroscience 164:1068–1083. doi:10.1016/j.neuroscience.2009.08.057
Tsai G, Coyle JT (1998) The role of glutamatergic neurotransmission in the pathophysiology of alcoholism. Ann Rev Med 49:173–184
Holmes A, Spanagel R, Krystal JH (2013) Glutamatergic targets for new alcohol medications. Psychopharmacology 229:539–554. doi:10.1007/s00213-013-3226-2
Acknowledgments
This work has been supported by the Internal grant agency of the Ministry of Health of the Czech Republic (IGA MZCR) No. NT/14504-3 to OS and by NHMRC (Australia) Project Grant APP1043000 to D.V.P. and V.J.B.
Author information
Authors and Affiliations
Corresponding author
Additional information
Special Issue: In Honor of Dr. Gerald Dienel.
Rights and permissions
About this article
Cite this article
Šerý, O., Sultana, N., Kashem, M.A. et al. GLAST But Not Least—Distribution, Function, Genetics and Epigenetics of l-Glutamate Transport in Brain—Focus on GLAST/EAAT1. Neurochem Res 40, 2461–2472 (2015). https://doi.org/10.1007/s11064-015-1605-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-015-1605-2