Abstract
Astrocytes have a pivotal role in brain as partners of neurons in homeostatic and metabolic processes. Astrocytes also protect other types of brain cells against the toxicity of reactive oxygen species and are considered as first line of defence against the toxic potential of xenobiotics. A key component in many of the astrocytic detoxification processes is the tripeptide glutathione (GSH) which serves as electron donor in the GSH peroxidase-catalyzed reduction of peroxides. In addition, GSH is substrate in the detoxification of xenobiotics and endogenous compounds by GSH-S-transferases which generate GSH conjugates that are efficiently exported from the cells by multidrug resistance proteins. Moreover, GSH reacts with the reactive endogenous carbonyls methylglyoxal and formaldehyde to intermediates which are substrates of detoxifying enzymes. In this article we will review the current knowledge on the GSH metabolism of astrocytes with a special emphasis on GSH-dependent detoxification processes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glutathione (GSH, γ-l-glutamyl-l-cysteinylglycine) is a tripeptide which is present in millimolar concentrations in most cell types including astrocytes [1]. GSH has essential cellular functions in many detoxification processes. In addition, to its chemical reaction with radicals and electrophiles, GSH serves as substrate or cofactor of a large number of detoxifying cellular enzymes [2]. Due to the dependence of many cellular processes on GSH it is not surprising that an impaired GSH metabolism has been connected with human diseases [3–6]. This appears to be especially the case for neurological disorders as ample evidence connects disturbances in the GSH metabolism of the brain with the progression of neurological disorders [7, 8], including Parkinson’s disease [9], Alzheimer’s disease [10], multiple sclerosis [11] as well as schizophrenia and bipolar disorder [12]. Also alterations of cognitive functions with ageing have been correlated with a decline in GSH content in brain and with impaired GSH-dependent functions [13].
Astrocytes have been reviewed to have important functions in synapse formation and modulation [14, 15], in brain metabolism [16–21] in the defence against oxidative stress [22–24], as well as in the homeostasis of essential metals [24–27]. Astrocytes are also considered to play an important role in the GSH metabolism of the brain [7, 16, 23, 28]. The high cellular GSH content and the strong capacity of astrocytes for GSH-dependent detoxification processes helps to protect these cells but also their neighbours against the toxic potential of oxidants and toxins [28–30]. In addition, astrocytes supply essential precursors for GSH synthesis to neighbouring neurons. In co-cultures, the presence of astrocytes maintains [31] or increases GSH levels in neurons [32, 33]. Especially the availability of cysteine determines the level of neuronal GSH. The supply by astrocytes of the cysteine required for neuronal GSH synthesis includes the export of GSH from astrocytes, extracellular processing of the exported GSH by ectoenzymes, and uptake of the GSH precursor amino acids into neurons [8, 23, 28].
As astrocytes cover with their end feet almost completely the brain capillaries, astrocytes are the first parenchymal brain cells which come into contact with energy substrates and amino acids that are delivered via the blood to the brain [34]. However, astrocytes will also encounter as first parenchymal brain cells potentially toxic compounds which have crossed the blood brain barrier. Thus, the strategically important localization of astrocytes as well as their strong detoxification potential defines astrocytes as first line of defence against toxins and xenobiotics that enter the brain. The metabolism of GSH in brain and the pivotal role of astrocytes in the GSH homeostasis of the brain have previously been extensively reviewed [23, 28, 35–37]. Here we summarize the current knowledge on the synthesis and metabolism of GSH in astrocytes with a focus on the GSH-dependent detoxification processes in these cells.
GSH Metabolism of Astrocytes
GSH Synthesis and Consumption
GSH is synthesized in astrocytes by two ATP-consuming cytosolic enzymes (Fig. 1), as in other cell types. In the first reaction, glutamate cysteine ligase (GCL) catalyzes the formation of the dipeptide γ-glutamylcysteine (γGluCys) from the amino acids glutamate and cysteine. This reaction is the rate limiting and regulated step in cellular GSH synthesis. The current knowledge on structure, function and regulation of GCL in GSH synthesis has recently been summarized [38]. The second reaction involved in GSH synthesis is catalyzed by GSH synthetase (GSH-Syn) which adds glycine in an ATP-driven reaction to γGluCys to generate the tripeptide GSH (Fig. 1). The activity of both GCL and GSH-Syn has been determined in cultured astrocytes [39–41]. Continuous synthesis of GSH is required in astrocytes to compensate for a continuous consumption of GSH in these cells. This has been demonstrated by exposure of cultured astrocytes to the GCL inhibitor buthionine sulfoximine (BSO), which lowers the astrocytic GSH content with a half-time of around 5 h [42].
Synthesis of GSH in astrocytes. GSH is synthesized by the consecutive reactions of glutamate cysteine ligase (GCL) and GSH synthetase (GSH-Syn) from the amino acid substrates glutamate (Glu), cysteine (Cys) and glycine (Gly). Preferred extracellular amino acid precursors for astrocytic GSH synthesis are the GSH substrates glutamate and glycine which are taken up into astrocytes by the excitatory amino acid transporters (EAATs) 1 or 2 and by the glycine transporter GlyT1, respectively. The cysteine required as substrate for GSH synthesis is predominately derived from extracellular cystine which is taken up into astrocytes by the cystine-glutamate antiporter X −C
The cellular content of GSH is determined by the rates of its synthesis and consumption. Concerning the synthesis of GSH, the activity of the enzymes involved in GSH synthesis, the intracellular availability of the substrates glutamate, cysteine and glycine as well as a feedback inhibition of GCL by high cellular GSH concentrations determine the rate of GSH synthesis. Accordingly, various compounds and treatments which foster GSH synthesis increase cellular GSH contents in cultured astrocytes (Table 1). In addition, also the inhibition of GSH consumption, for example the inhibition of GSH export, can contribute to an elevated cellular GSH content. At least cultured astrocytes from mice that are deficient of the multidrug resistance protein (Mrp) 1, the transporter predominantly responsible for astrocytic GSH export, contain higher specific GSH contents compared to cultures from wildtype mice [43].
The transcription of the GCL and GSH-Syn genes is regulated by the cis-acting antioxidant response element (ARE) which itself is controlled by the nuclear transcription factor erythroid-2-related factor 2 (Nrf2) [44, 45]. Under unstressed conditions Nrf2 is present in the cytosol in its inactive form, bound and targeted for degradation by the Kelch-like ECH-associated protein 1 (KEAP1). During oxidative stress or in presence of Nrf2 activators, Nrf2 is released from KEAP1 and translocates into the nucleus where it induces the transcription of genes of various detoxifying and antioxidant enzymes [44, 45]. In astrocytes, synthesis of both GCL and GSH-Syn, as well as of other proteins involved in GSH-dependent detoxification processes, are stimulated via the Nrf2 pathway during oxidative stress and by the presence of Nrf2-activators [44, 46]. Accordingly, a number of different compounds which activate the Nrf2-ARE pathway increase the GSH content of cultured astrocytes [41, 44, 46–51].
In addition to the activity of GSH synthesis enzymes, the availability of the amino acid precursors determines and limits astrocytic GSH synthesis [1, 35]. The substrate amino acids for GSH synthesis can either be directly taken up from the extracellular space or they can be generated from cellular or extracellular precursor molecules. Astrocytes express the sodium-dependent excitatory amino acid transporter (EAAT) 1 and 2 [52] and the glycine transporter GlyT1 [53] which allow efficient accumulation of the GSH substrates glutamate and glycine (Fig. 1). The best extracellular source of the cysteine required for astrocytic GSH synthesis is cystine which is reduced after uptake in astrocytes to cysteine [54, 55]. Astrocytes take up cystine predominately by the cystine-glutamate antiporter X −C , but also other transporters have been discussed to contribute to this import [56, 57]. In addition to these amino acids, astrocytes can use a large number of other amino acids, metabolites or peptides as precursors of the GSH synthesis substrates glutamate, cysteine or glycine [1, 58].
Astrocytes need GSH as substrate for various pathways (Fig. 2). GSH is essential for the detoxification of radicals and peroxides (Fig. 3) as well as the reactive carbonyls formaldehyde and methylglyoxal (Fig. 4). In these pathways GSH is not consumed as it is regenerated by the final enzymatic steps of the respective pathways (Figs. 3, 4). In contrast, the conjugation of GSH by GSH-S-transferases (GSTs) to electrophilic compounds and the export of GSH from the cells (Fig. 2) lower cellular GSH contents and require GSH synthesis to replenish a high cytosolic GSH concentration.
GSH-dependent metabolism in astrocytes. A GSH reacts with carbonyls (formaldehyde or methylglyoxal) to GSH-thiohemiacetals (GSH-THA) which serve as substrates for detoxifying reactions catalyzed by the enzymes (E) alcohol dehydrogenase (ADH) 3 or glyoxalase 1. B The GSH-dependent reduction of peroxide by glutathione peroxidases (GPx) produces GSSG which is rapidly reduced by glutathione reductase (GR) to regenerate GSH. C If substantial amounts of GSSG accumulate in astrocytes, these cells export GSSG via multidrug resistance protein (Mrp) 1. D Conjugation of GSH to electrophilic compounds (X) in reactions that are catalyzed by GSH-S-transferases (GSTs). GSH-conjugates (GS-X) are exported from astrocytes via Mrp1 or other transporters. E Mrp1-mediated export of GSH from astrocytes
GSH-GSSG redox cycling in astrocytes. GSH reacts with radicals (R·) in an enzyme-independent reaction (a) or with organic hydroperoxides (b) or hydrogen peroxide (c) in GPx-catalyzed reactions to GSSG and the reduced derivative of the respective reactive oxygen species (ROS). The GSSG generated during the GSH-dependent reduction of ROS (a–c) is reduced by GR in an NADPH-dependent reaction (d)
GSH-dependent detoxification of formaldehyde and methylglyoxal in astrocytes. GSH reacts with formaldehyde (a) or methylglyoxal (b) in enzyme-independent reactions to the respective thiohemiacetals (THA). S-Hydroxymethyl-GSH is substrate of alcoholdehydrogenase (ADH) 3 and becomes oxidized to S-formyl-GSH which is subsequently hydrolyzed to formate and GSH (a). The methylglyoxal-GSH-THA is converted by glyoxalase (Glo) 1 to S-D-lactoyl-GSH which is the substrate of Glo2 to become hydrolyzed to D-lactate and GSH (b)
GSH Redox Cycling
Radicals and peroxides are continuously generated in oxygen-consuming cells and a network of cellular antioxidative mechanisms prevent an accumulation of such reactive oxygen species (ROS) and ROS-induced oxidative damage of cellular macromolecules. GSH is involved in two important types of antioxidative reactions (Fig. 3a–c). GSH can react directly with radicals such as superoxide or hydroxyl radicals in non-enzymatic reactions, thereby reducing these radicals (Fig. 3a). In addition, GSH serves as electron donor for the reduction of organic hydroperoxides (Fig. 3b) or hydrogen peroxide (Fig. 3c) in reactions catalyzed by glutathione peroxidases (GPx). In both types of reactions, GSH is oxidized to glutathione disulfide (GSSG) (Fig. 3a–c).
For vertebrates, 8 isoforms of GPx have been described which differ in their catalytic center, their substrate preference and in their subcellular localization [59]. Of those isoforms, GPx1 is expressed in cultured astrocytes and contributes substantially to the detoxification of hydrogen peroxide and organic hydroperoxides [60, 61]. In addition, cultured astrocytes express GPx3 and enhance the secretion of this isoform after exposure to angiogenin [62]. In vivo, astrocytes strongly upregulate the expression of GPx4 after brain injury [63].
The GSSG generated by GSH-dependent reduction of ROS is reduced by the flavoenzyme glutathione reductase (GR) (Fig. 3d). This enzyme is expressed and active in cultured astrocytes [64, 65]. GR needs NADPH as electron donor [66], which is generated in the cytosol of astrocytes mainly by the pentose phosphate pathway [67–70]. Due to the low micromolar KM-values of GR for NADPH and GSSG [66], the small amounts of GSSG generated during normal metabolism are rapidly reduced to GSH. Thus, for unstressed conditions GSSG is hardly detectable in astrocytes and the ratio of GSH to GSSG is very high. However, if GR in astrocytes is inhibited by exposure to carmustin or zinc ions, GSSG accumulates in the cells and the normally high ratio of GSH to GSSG decreases [71]. During oxidative stress GR can become rate limiting for GSH-GSSG redox cycling which causes a transient increase in cellular GSSG levels and a corresponding decline in the GSH to GSSG ratio [68, 72, 73]. Under such conditions, GSSG can be exported from astrocytes (Fig. 2) by Mrp1 [43, 74, 75].
GSH Export and Extracellular GSH Metabolism
Cultured astrocytes have been shown to export up to 10 % of their GSH per hour [76]. The astrocytic GSH export is predominately mediated by Mrp1 [43, 77] which belongs to the Mrp family of ATP-driven export pumps [78–80]. In addition to Mrp1, astrocytes express a number of other Mrps and other potential GSH exporters in culture and in vivo [43, 81–86], but the contribution of these transporters in astrocytic export processes remains to be elucidated. GSH has also been shown to be released from astrocytes via gap junction hemichannels under certain conditions [87, 88].
The KM-value for GSH export from astrocytes is around 25 mM [89] and the cytosolic GSH concentration of untreated astrocytes is around 8 mM [1]. Consequently, treatments which increase the GSH concentration in astrocytes should lead to an increase in the rate of cellular GSH export. This has been confirmed for astrocytes that contained higher GSH contents due to a pre-incubation with ammonium [90], arsenate [89], arsenite [91], cadmium chloride [89, 91], copper chloride [89, 92], copper oxide nanoparticles [93], nitric oxide [94] or with fibroblast growth factor 1 and tertiary butyl hydroquinone [95].
Recently a number of compounds have been reported to strongly stimulate rapid GSH export from viable astrocytes, including formaldehyde [96], arsenate and arsenite [97, 98] and antiretroviral protease inhibitors [99, 100]. Although all of these stimulated GSH export processes were almost completely prevented by inhibition of Mrp1, the molecular mechanism how such structurally very diverse compounds accelerate Mrp1-mediated GSH export remains unclear. At least for the formaldehyde-stimulated GSH export from astrocytes it was shown that the Vmax-value for the export was strongly increased while the KM-values remained unchanged [89], suggesting that formaldehyde treatment of astrocytes may lead to a recruitment of Mrp1 from intracellular vesicles into the plasma membrane. Such a translocation of Mrp1 between intracellular and membrane location has previously been shown for bilirubin-treated astrocytes [101]. Also the upregulation of Mrp1 in astrocytes appears to increase GSH export. At least the upregulation of Mrp1 expression by a treatment of cultured astrocytes with the HIV1 envelope glycoprotein gp120 was accompanied by an elevated export of GSH and GSSG [102].
GSH which has been exported from astrocytes is a substrate of the ectoenzyme γ-glutamyl transpeptidase (γ-GT) [76]. γ-GT transfers the γ-glutamyl moiety of GSH to an acceptor which can be an amino acid, a peptide but also water [103]. Extracellular processing by γ-GT of the GSH released from astrocytes is a crucial step in the supply of GSH precursors from astrocytes to neurons [33]. A product of the reaction catalyzed by astrocytic γ-GT is the dipeptide CysGly which is either taken up into astrocytes by the dipeptide transporter PepT2 [104] or can be cleaved by the neuronal aminopeptidase N [105] to provide cysteine and glycine to neurons. These amino acids are efficiently taken up by neurons [106, 107] and can be used as substrates for neuronal GSH synthesis [33, 55].
GSH in Astrocytic Detoxification Processes
GSH and Peroxide Detoxification
Among the peroxides that are continuously produced by the cellular metabolism, hydrogen peroxide is quantitatively the most important one. This peroxide is formed predominantly by disproportionation of superoxide which can occur enzyme-independently or is catalyzed by superoxide dismutases [22]. Superoxide itself is generated in mitochondria as byproduct of respiratory chain complexes and enzymes [108] and as product of the NADPH oxidase reaction [109]. Hydrogen peroxide is also formed in the reactions of some oxidases, for example monoamine oxidases [110]. A second class of cellular peroxides are organic hydroperoxides which include stereospecifically-defined prostaglandin and leukotrine hydroperoxides that are products of cyclooxygenases and lipooxygenases, respectively, as well as various hydroperoxides that are generated by unspecific oxidation of polyunsaturated fatty acids in membranes by radical-mediated lipid peroxidation [111].
Cellular hydrogen peroxide is detoxified in astrocytes predominantly by the enzymes GPx and catalase [22]. Cultured astrocytes efficiently dispose of exogenous hydrogen peroxide with half-times in the minute range [72, 112–114]. The specific clearance rates of astrocytes for hydrogen peroxide are similar to values reported for cultured neurons and microglial cells but higher than those found for cultured oligodendrocytes [22, 113, 115, 116]. In hydrogen peroxide clearance both the GSH system and catalase are involved and the capacity of each of the two contributing enzyme systems is sufficiently high to compensate at least in part for an impairment of the other system [72, 112]. Cultured astrocytes also efficiently dispose of exogenous organic hydroperoxides such as tertiary butyl hydroperoxide (tBHP) and cumene hydroperoxide (CHP) with half-times similar to that for hydrogen peroxide [61, 68, 73, 114, 117]. As inhibition of catalase does not affect the clearance of organic hydroperoxides by astrocytes, only the GSH system appears to be involved in the disposal of these peroxides [61, 68, 73, 117]. This view is supported by the strong increase in the half-time of the peroxides in astrocytes that had been pre-incubated with BSO to lower cellular GSH contents, with mercaptosuccinate to inhibit GPx or in the absence of glucose which slows NADPH regeneration by pentose phosphate pathway [68, 73].
Another class of enzymes which can contribute to the cellular peroxide disposal are peroxiredoxins [2, 118]. Concerning GSH dependent processes, especially peroxiredoxin 6 is of interest as this peroxiredoxin requires for peroxide reduction GSH and involves GSTs [2]. Peroxiredoxin 6 is expressed in cultured astrocytes and its expression is upregulated by the Nrf2 activator tertiary butyl hydroquinone which accelerates the clearance of tBHP and increases the resistance of astrocytes towards hydrogen peroxide and tBHP [114].
The ability of cultured astrocytes to detoxify hydrogen peroxide is affected by ageing. At least cultured astrocytes derived from old mice have a slower hydrogen peroxide clearance rate than astrocytes cultured from young mice [119]. This may be caused by a lowered GR activity and an increased GSH export rate observed for astrocytes cultured from old mice [119].
GSH-GSSG redox cycling is the base of the GSH-dependent peroxide detoxification in astrocytes. During the GPx-catalyzed reduction of peroxides, GSH becomes oxidized to GSSG (Fig. 3b, c) which is subsequently reduced to GSH by GR (Fig. 3d). For cultured astrocytes this is demonstrated by the transient occurrence of GSSG in cultures that had been exposed to hydrogen peroxide [60, 72, 117, 120], tBHP [73] or CHP [61, 68]. Among the different isoforms of GPx, especially the cytosolic isoform GPx1 appears to be important for astrocytic peroxide detoxification as astrocytes cultured from GPx1-deficient mice dispose hydrogen peroxide and CHP much slower than wild type cells, did not show a transient increase in cellular GSSG contents and were more vulnerable towards peroxide mediated toxicity [60, 61].
Severe oxidative stress or conditions that make GR rate limiting for GSH-GSSG redox cycling lead to a strong accumulation of cellular GSSG. Under such conditions, astrocytes export efficiently GSSG via Mrp1. This has been demonstrated for astrocytes which have been exposed to chronic hydrogen peroxide stress [43, 74], to high concentrations of dopamine [75] or to zinc chlorid [71].
GSH as Cofactor in the Detoxification of Reactive Carbonyls
GSH is the essential substrate for the cellular pathways that detoxify the reactive carbonyls formaldehyde and methylglyoxal. These carbonyls are endogenously generated during normal metabolism and react non-enzymatically with GSH to thiohemiacetals which serve as substrates for an enzymatic conversion of the respective carbonyl to a less reactive compound which can be released from cells (Fig. 4). Efficient detoxification of formaldehyde and methylglyoxal appears to be especially important for the brain as disturbances of the respective metabolic pathways have been connected with neurological disorders and ageing [121–123]. Recent studies suggest that astrocytes have a prominent role in the detoxification of formaldehyde and methylglyoxal in brain.
Formaldehyde
Formaldehyde is generated in substantial amounts in the human body during normal metabolism. The formaldehyde concentration in blood is around 0.1 mM [124], while formaldehyde concentrations in brain have been reported to be even higher [125]. The steady state formaldehyde concentrations in brain are maintained low due to the effective action of enzymes which oxidize formaldehyde to formate [122]. Cellular formaldehyde oxidation involves either the mitochondrial aldehyde dehydrogenase (ADH) 2 and/or the cytosolic GSH-dependent formaldehyde dehydrogenase (ADH3) [122]. The ADH3 reaction requires the presence of S-hydroxymethyl-GSH which is generated by the enzyme-independent reaction of formaldehyde with GSH (Fig. 4a). Oxidation of S-hydroxymethyl-GSH by ADH3 generates S-formyl-GSH which is hydrolyzed by a thiolase to regenerate GSH and to generate formate [122].
Cultured astrocytes contain the mRNAs of enzymes which generate and oxidize formaldehyde including ADH3 [126], suggesting that astrocytes are able to produce and to detoxify formaldehyde. Indeed, cultured astrocytes remove exogenously applied formaldehyde very efficiently with a rate of around 0.2 µmol/(h × mg) [126]. The KM-value for formaldehyde clearance by cultured astrocytes is around 0.19 mM, suggesting that the cytosolic ADH3 which has a low micromolar KM-value for its substrate S-hydroxymethyl-GSH contributes substantially to astrocytic formaldehyde oxidation [126].
Astrocytes convert the majority (>90 %) of exogenously applied formaldehyde to formate that is subsequently exported from the cells [126], indicating that the S-formyl-GSH generated by the ADH3 reaction is rapidly hydrolyzed in these cells to GSH and formate. The observed rate of formaldehyde oxidation to formate by astrocytes is with 0.23 µmol/(h × mg) in a range similar to that of glucose consumption (0.73 µmol/(h × mg) [126], underlining the high capacity of astrocytes to detoxify formaldehyde. A similar formaldehyde clearance rate was recently reported for cultured neurons, although these cells release less formate than astrocytes [127]. The formate generated via formaldehyde oxidation may also be harmful for brain cells, as formate-induced inhibition of mitochondrial respiration is the likely reason for the observed accelerated glycolytic flux in formaldehyde-treated astrocytes and neurons [126, 127].
Methylglyoxal
Methylglyoxal is a ubiquitous product of cellular glucose metabolism and is predominately formed by non-enzymatic decomposition of the glycolysis intermediates glyceraldehyde-3-phosphate and dihydroxyacetone phosphate [128]. In order to avoid unspecific glycation reactions of proteins, the reactive methylglyoxal is efficiently detoxified in cells by the GSH-dependent glyoxalase system which consists of the two enzymes glyoxalase 1 and glyoxalase 2. The enzyme-independent reaction of methylglyoxal with GSH generates a thiohemiacetal that is the substrate of glyoxalase 1 (Fig. 4b). This enzyme converts the thiohemiacetal to the thioester S-D-lactoyl-GSH which is subsequently hydrolyzed by glyoxalase 2 to GSH and d-lactate [128].
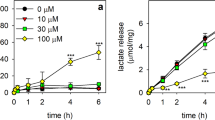
In brain, especially astrocytes appear to have a highly efficient glyoxalase system to detoxify methylglyoxal. Both glyoxalase 1 and glyoxalase 2 are strongly expressed in cultured astrocytes and the specific activity determined for this enzyme is higher in astrocytes than in cultured neurons [129]. Strong immunoreactivity for glyoxalase 1 was also found for astrocytes in mouse and rat brain [129, 130]. Cultured astrocytes convert exogenously applied methylglyoxal more efficiently to d-lactate than neurons [129]. Also the higher toxic potential of methylglyoxal to cultured neurons compared with cultured astrocytes as well as the protection by astrocytes of co-cultured neurons against methylglyoxal induced toxicity demonstrates the high capacity of astrocytes to detoxify this carbonyl [129].
Conjugation of GSH with Endogenous Compounds and Xenobiotics
GSH is an essential substrate for the cellular detoxification of endogenous and exogenous compounds by GSTs which covalently conjugate GSH via its thiol group to the respective electrophilic substrate (Fig. 2). Although this type of detoxification lowers the cellular GSH concentration, it is of advantage as GSH-conjugates are in most cases less toxic than their precursors and will be actively exported from cells by Mrps [79, 85]. Endogenous substrates of GSTs are for example intermediates of the eicosanoid metabolisms but also lipid peroxides and reactive aldehydes such as 4-hydroxynonenal [131]. In addition, various electrophilic compounds of exogenous origin (xenobiotics) are substrates of GSTs [132]. For cultured astrocytes a large number of reactive compounds have been reported to rapidly lower the cellular GSH content (Table 2). However, it is currently not known to which extent astrocytic GSTs contribute to the rapid reactions of such compounds with GSH.
GSTs represent a large superfamily of enzymes which are encoded by a polymorphic gene superfamily [133, 134]. GSTs differ in their cellular localization (cytosolic, microsomal or mitochondrial). However, already for the cytosolic GSTs seven subfamilies (alpha, mu, pi, sigma, theta, omega and zeta) have been classified [133, 134]. Little is known on the expression and functions of the various isoforms of GSTs in brain astrocytes. Rodent astrocytes were shown to express mu- and alpha-type GSTs as well as microsomal GSTs [135–138]. GST activity was also found in mitochondrial fractions of cultured astrocytes [139]. Chromatographic methods allowed to separate the cytosol of cultured astrocytes into several fractions which differed regarding their GST activity towards various GST substrates [140]. The expression of members of different GSTs in astrocytes is likely to be regulated separately. At least a treatment of astrocytes with conditioned media from activated microglial cells increased the expression of GST-pi1 and GST-mu3, while treatment with conditioned media from non-activated microglial cells only increased GST-pi1 but decreased GST-mu3 expression [141]. As another trigger ethyl pyruvate was identified to elevate GST levels in primary astrocytes via activation of Nrf2 [48].
Alterations in the expression of GST isoenzymes in brain have been connected to neurological disorders including Alzheimer´s disease [142], epilepsy [143] and Parkinson´s disease [144, 145]. However, it remains to be elucidated whether the expression or activity of astrocytic GSTs are altered in such diseases.
Conclusions and Perspectives
Astrocytes have a key function in the GSH-dependent detoxification processes in brain. These cells have a high capacity for GPx-catalyzed peroxide reduction, for the detoxification of methylglyoxal and formaldehyde, as well as for the GST-catalyzed conjugation reactions of xenobiotics and endogenous compounds. As all these processes require sufficiently high concentrations of intracellular GSH in astrocytes, the different detoxification processes may under certain conditions interfere with each other and even compete for the substrate GSH. For example, an acute decline of cellular GSH by an alkylating substance will lower GSH-dependent peroxide reduction. Furthermore, impairments of astrocytic GSH synthesis, recycling and export are likely to affect the GSH-dependent detoxification processes in astrocytes which may harm these cells directly but may also increase the toxic potential of oxidants and toxins for other brain cells. At least the protection by astrocytes of co-cultured neurons against various toxins is compromized, if astrocytes contain low levels of GSH [146–148].
Most of the data described in this review article were obtained in experiments performed on cultured primary astrocytes which are considered as a suitable model system to investigate properties and metabolic functions of astrocytes [149, 150]. Confirmation of a given cell culture result on GSH-dependent detoxification processes for the in vivo situation is in many cases difficult to obtain and remains a challenge. Nevertheless, results from future studies on the GSH-dependent pathways in astrocytes in vivo are highly warranted.
Although GSH synthesis takes place exclusively in the cytosol, the presence of GSH has been reported for many other cellular compartment, including nucleus [151], mitochondria [152] and lysosomes [153]. For astrocytes, at least the presence of GSH and GSH-dependent enzymes in mitochondria as well as the transport of GSH in astrocytic mitochondria have been investigated [139, 154, 155]. Future studies are now required to elucidate in more detail the subcellular distribution of GSH in astrocytes, the particular functions of GSH in the different compartments and the transport mechanisms which are responsible for intracellular trafficking of GSH in astrocytes.
Impairments in GSH-dependent detoxification processes in astrocytes as well as the supply of GSH precursors by astrocytes to neurons are likely to contribute to disturbances in brain GSH homeostasis as well as to neural damage and cognitive impairments reported for neurological disorders which have been connected with alteration in GSH metabolism in the brain. Accordingly, strategies which would help astrocytes to maintain a high cellular GSH concentration, including delivery of GSH as pro-drugs or with carriers [156], could prove beneficial for the defence of the brain against oxidative stress and toxins.
References
Dringen R, Hamprecht B (1998) Glutathione restoration as indicator for cellular metabolism of astroglial cells. Dev Neurosci 20:401–407
Deponte M (2013) Glutathione catalysis and the reaction mechanisms of glutathione-dependent enzymes. Biochim Biophys Acta 1830:3217–3266
Ballatori N, Krance SM, Notenboom S, Shi S, Tieu K, Hammond CL (2009) Glutathione dysregulation and the etiology and progression of human diseases. Biol Chem 390:191–214
Franco R, Schoneveld OJ, Pappa A, Panayiotidis MI (2007) The central role of glutathione in the pathophysiology of human diseases. Arch Physiol Biochem 113:234–258
Morris D, Khurasany M, Nguyen T, Kim J, Guilford F, Mehta R, Gray D, Saviola B, Venketaraman V (2013) Glutathione and infection. Biochim Biophys Acta 1830:3329–3349
Traverso N, Ricciarelli R, Nitti M, Marengo B, Furfaro AL, Pronzato MA, Marinari UM, Domenicotti C (2013) Role of glutathione in cancer progression and chemoresistance. Oxid Med Cell Longev 2013:972913
Aoyama K, Nakaki T (2013) Impaired glutathione synthesis in neurodegeneration. Int J Mol Sci 14:21021–21044
Johnson WM, Wilson-Delfosse AL, Mieyal JJ (2012) Dysregulation of glutathione homeostasis in neurodegenerative diseases. Nutrients 4:1399–1440
Smeyne M, Smeyne RJ (2013) Glutathione metabolism and Parkinson’s disease. Free Radic Biol Med 62:13–25
Saharan S, Mandal PK (2014) The emerging role of glutathione in Alzheimer’s disease. J Alzheimers Dis 40:519–529
Carvalho AN, Lim JL, Nijland PG, Witte ME, Van Horssen J (2014) Glutathione in multiple sclerosis: more than just an antioxidant? Mult Scler 20:1425–1431
Kulak A, Steullet P, Cabungcal JH, Werge T, Ingason A, Cuenod M, Do KQ (2013) Redox dysregulation in the pathophysiology of schizophrenia and bipolar disorder: insights from animal models. Antioxid Redox Signal 18:1428–1443
Currais A, Maher P (2013) Functional consequences of age-dependent changes in glutathione status in the brain. Antioxid Redox Signal 19:813–822
Clarke LE, Barres BA (2013) Emerging roles of astrocytes in neural circuit development. Nat Rev Neurosci 14:311–321
Bernardinelli Y, Muller D, Nikonenko I (2014) Astrocyte-synapse structural plasticity. Neural Plast 2014:232105
Hirrlinger J, Dringen R (2010) The cytosolic redox state of astrocytes: maintenance, regulation and functional implications for metabolite trafficking. Brain Res Rev 63:177–188
Verkhratsky A, Nedergaard M, Hertz L (2014) Why are astrocytes important? Neurochem Res. doi:10.1007/s11064-014-1403-2
Bouzier-Sore AK, Pellerin L (2013) Unraveling the complex metabolic nature of astrocytes. Front Cell Neurosci 7:179
Schousboe A, Bak LK, Waagepetersen HS (2013) Astrocytic Control of Biosynthesis and Turnover of the Neurotransmitters Glutamate and GABA. Front Endocrinol (Lausanne) 4:102
Dienel GA, Cruz NF (2014) Contributions of glycogen to astrocytic energetics during brain activation. Metab Brain Dis. doi:10.1007/s11011-014-9493-8
Schousboe A, Scafidi S, Bak LK, Waagepetersen HS, McKenna MC (2014) Glutamate metabolism in the brain focusing on astrocytes. Adv Neurobiol 11:13–30
Dringen R, Pawlowski PG, Hirrlinger J (2005) Peroxide detoxification by brain cells. J Neurosci Res 79:157–165
Schmidt MM, Dringen R (2012) Glutathione (GSH) synthesis and metabolism. In: Gruetter R, Choi IY (eds) Advances in neurobiology. Springer, New York, pp 1029–1050
Dringen R, Bishop GM, Koeppe M, Dang TN, Robinson SR (2007) The pivotal role of astrocytes in the metabolism of iron in the brain. Neurochem Res 32:1884–1890
Scheiber IF, Dringen R (2013) Astrocyte functions in the copper homeostasis of the brain. Neurochem Int 62:556–565
Hohnholt MC, Dringen R (2013) Uptake and metabolism of iron and iron oxide nanoparticles in brain astrocytes. Biochem Soc Trans 41:1588–1592
Scheiber IF, Mercer JF, Dringen R (2014) Metabolism and functions of copper in brain. Prog Neurobiol 116:33–57
Fernandez-Fernandez S, Almeida A, Bolanos JP (2012) Antioxidant and bioenergetic coupling between neurons and astrocytes. Biochem J 442:3–12
Bolanos JP, Heales SJ, Land JM, Clark JB (1995) Effect of peroxynitrite on the mitochondrial respiratory chain: differential susceptibility of neurones and astrocytes in primary culture. J Neurochem 64:1965–1972
Barker JE, Bolanos JP, Land JM, Clark JB, Heales SJ (1996) Glutathione protects astrocytes from peroxynitrite-mediated mitochondrial damage: implications for neuronal/astrocytic trafficking and neurodegeneration. Dev Neurosci 18:391–396
Sagara J, Miura K, Bannai S (1993) Maintenance of neuronal glutathione by glial cells. J Neurochem 61:1672–1676
Bolanos JP, Heales SJR, Peuchen S, Barker JE, Land JM, Clark JB (1996) Nitric oxide-mediated mitochondrial damage: a potential neuroprotective role for glutathione. Free Radical Biol Med 21:995–1000
Dringen R, Pfeiffer B, Hamprecht B (1999) Synthesis of the antioxidant glutathione in neurons: supply by astrocytes of CysGly as precursor for neuronal glutathione. J Neurosci 19:562–569
Valdovinos-Flores C, Gonsebatt ME (2012) The role of amino acid transporters in GSH synthesis in the blood-brain barrier and central nervous system. Neurochem Int 61:405–414
Dringen R (2000) Metabolism and functions of glutathione in brain. Prog Neurobiol 62:649–671
Dringen R, Gutterer JM, Hirrlinger J (2000) Glutathione metabolism in brain. Eur J Biochem 267:4912–4916
Dringen R, Hirrlinger J (2003) Glutathione pathways in the brain. Biol Chem 384:505–516
Lu SC (2013) Glutathione synthesis. Biochim Biophys Acta 1830:3143–3153
Makar TK, Nedergaard M, Preuss A, Gelbard AS, Perumal AS, Cooper AJ (1994) Vitamin E, ascorbate, glutathione, glutathione disulfide, and enzymes of glutathione metabolism in cultures of chick astrocytes and neurons: evidence that astrocytes play an important role in antioxidative processes in the brain. J Neurochem 62:45–53
Gegg ME, Clark JB, Heales SJ (2002) Determination of glutamate-cysteine ligase (γ-glutamylcysteine synthetase) activity by high-performance liquid chromatography and electrochemical detection. Anal Biochem 304:26–32
Lavoie S, Chen Y, Dalton TP, Gysin R, Cuenod M, Steullet P, Do KQ (2009) Curcumin, quercetin, and tBHQ modulate glutathione levels in astrocytes and neurons: importance of the glutamate cysteine ligase modifier subunit. J Neurochem 108:1410–1422
Devesa A, O’Connor JE, Garcia C, Puertes IR, Vina JR (1993) Glutathione metabolism in primary astrocyte cultures: flow cytometric evidence of heterogeneous distribution of GSH content. Brain Res 618:181–189
Minich T, Riemer J, Schulz JB, Wielinga P, Wijnholds J, Dringen R (2006) The multidrug resistance protein 1 (Mrp1), but not Mrp5, mediates export of glutathione and glutathione disulfide from brain astrocytes. J Nurochem 97:373–384
Vargas MR, Johnson JA (2009) The Nrf2-ARE cytoprotective pathway in astrocytes. Expert Rev Mol Med 11:e17
Niture SK, Khatri R, Jaiswal AK (2014) Regulation of Nrf2-an update. Free Radic Biol Med 66:36–44
Gupta K, Patani R, Baxter P, Serio A, Story D, Tsujita T, Hayes JD, Pedersen RA, Hardingham GE, Chandran S (2012) Human embryonic stem cell derived astrocytes mediate non-cell-autonomous neuroprotection through endogenous and drug-induced mechanisms. Cell Death Differ 19:779–787
Scannevin RH, Chollate S, Jung MY, Shackett M, Patel H, Bista P, Zeng W, Ryan S, Yamamoto M, Lukashev M, Rhodes KJ (2012) Fumarates promote cytoprotection of central nervous system cells against oxidative stress via the nuclear factor (erythroid-derived 2)-like 2 pathway. J Pharmacol Exp Ther 341:274–284
Shin JH, Kim SW, Jin Y, Kim ID, Lee JK (2012) Ethyl pyruvate-mediated Nrf2 activation and hemeoxygenase 1 induction in astrocytes confer protective effects via autocrine and paracrine mechanisms. Neurochem Int 61:89–99
Sun X, Erb H, Murphy TH (2005) Coordinate regulation of glutathione metabolism in astrocytes by Nrf2. Biochem Biophys Res Commun 326:371–377
Malone PE, Hernandez MR (2007) 4-Hydroxynonenal, a product of oxidative stress, leads to an antioxidant response in optic nerve head astrocytes. Exp Eye Res 84:444–454
Lin SX, Lisi L, Dello Russo C, Polak PE, Sharp A, Weinberg G, Kalinin S, Feinstein DL (2011) The anti-inflammatory effects of dimethyl fumarate in astrocytes involve glutathione and haem oxygenase-1. ASN Neuro 3:e00055
Had-Aissouni L (2012) Toward a new role for plasma membrane sodium-dependent glutamate transporters of astrocytes: maintenance of antioxidant defenses beyond extracellular glutamate clearance. Amino Acids 42:181–197
Szoke K, Hartel K, Grass D, Hirrlinger PG, Hirrlinger J, Hulsmann S (2006) Glycine transporter 1 expression in the ventral respiratory group is restricted to protoplasmic astrocytes. Brain Res 1119:182–189
Kranich O, Dringen R, Sandberg M, Hamprecht B (1998) Utilization of cysteine and cysteine precursors for the synthesis of glutathione in astroglial cultures: preference for cystine. Glia 22:11–18
Kranich O, Hamprecht B, Dringen R (1996) Different preferences in the utilization of amino acids for glutathione synthesis in cultured neurons and astroglial cells derived from rat brain. Neurosci Lett 219:211–214
Bender AS, Reichelt W, Norenberg MD (2000) Characterization of cystine uptake in cultured astrocytes. Neurochem Int 37:269–276
Shanker G, Aschner M (2001) Identification and characterization of uptake systems for cystine and cysteine in cultured astrocytes and neurons: evidence for methylmercury-targeted disruption of astrocyte transport. J Neurosci Res 66:998–1002
McBean GJ (2012) The transsulfuration pathway: a source of cysteine for glutathione in astrocytes. Amino Acids 42:199–205
Brigelius-Flohe R, Maiorino M (2013) Glutathione peroxidases. Biochim Biophys Acta 1830:3289–3303
Liddell JR, Hoepken HH, Crack PJ, Robinson SR, Dringen R (2006) Glutathione peroxidase 1 and glutathione are required to protect mouse astrocytes from iron-mediated hydrogen peroxide toxicity. J Neurosci Res 84:578–586
Liddell JR, Dringen R, Crack PJ, Robinson SR (2006) Glutathione peroxidase 1 and a high cellular glutathione concentration are essential for effective organic hydroperoxide detoxification in astrocytes. Glia 54:873–879
Skorupa A, Urbach S, Vigy O, King MA, Chaumont-Dubel S, Prehn JH, Marin P (2013) Angiogenin induces modifications in the astrocyte secretome: relevance to amyotrophic lateral sclerosis. J Proteomics 91:274–285
Savaskan NE, Borchert A, Brauer AU, Kuhn H (2007) Role for glutathione peroxidase-4 in brain development and neuronal apoptosis: specific induction of enzyme expression in reactive astrocytes following brain injury. Free Radic Biol Med 43:191–201
Gutterer JM, Dringen R, Hirrlinger J, Hamprecht B (1999) Purification of glutathione reductase from bovine brain, generation of an antiserum, and immunocytochemical localization of the enzyme in neural cells. J Neurochem 73:1422–1430
Petters C, Dringen R (2014) Comparison of primary and secondary rat astrocyte cultures regarding glucose and glutathione metabolism and the accumulation of iron oxide nanoparticles. Neurochem Res 39:46–58
Dringen R, Gutterer JM (2002) Glutathione reductase from bovine brain. Methods Enzymol 348:281–288
Garcia-Nogales P, Almeida A, Fernadez E, Medina JM, Bolanos JP (1999) Induction of glucose-6-phosphate dehydrogenase by lipopolysaccharide contributes to preventing nitric oxide-mediated glutathione depletion in cultrued rat astrocytes. J Neurochem 72:1750–1758
Kussmaul L, Hamprecht B, Dringen R (1999) The detoxification of cumene hydroperoxide by the glutathione system of cultured astroglial cells hinges on hexose availability for the regeneration of NADPH. J Neurochem 73:1246–1253
Dringen R, Hoepken HH, Minich T, Ruedig C (2007) Pentose phosphate pathway and NADPH metabolism. In: Gibson GE, Dienel GA (eds) Handbook of neurochemistry and molecular neurobiology, 3rd edn. Springer, New York, pp 41–62
Takahashi S, Izawa Y, Suzuki N (2012) Astroglial pentose phosphate pathway rates in response to high-glucose environments. ASN Neuro 4:e00078
Bishop GM, Dringen R, Robinson SR (2007) Zinc stimulates the production of toxic reactive oxygen species (ROS) and inhibits glutathione reductase in astrocytes. Free Radic Biol Med 42:1222–1230
Dringen R, Hamprecht B (1997) Involvement of glutathione peroxidase and catalase in the disposal of exogenous hydrogen peroxide by cultured astroglial cells. Brain Res 759:67–75
Dringen R, Kussmaul L, Hamprecht B (1998) Rapid clearance of tertiary butyl hydroperoxide by cultured astroglial cells via oxidation of glutathione. Glia 23:139–145
Hirrlinger J, Konig J, Keppler D, Lindenau J, Schulz JB, Dringen R (2001) The multidrug resistance protein MRP1 mediates the release of glutathione disulfide from rat astrocytes during oxidative stress. J Neurochem 76:627–636
Hirrlinger J, Schulz JB, Dringen R (2002) Effects of dopamine on the glutathione metabolism of cultured astroglial cells: implications for Parkinson’s disease. J Neurochem 82:458–467
Dringen R, Kranich O, Hamprecht B (1997) The γ-glutamyl transpeptidase inhibitor acivicin preserves glutathione released by astroglial cells in culture. Neurochem Res 22:727–733
Hirrlinger J, Schulz JB, Dringen R (2002) Glutathione release from cultured brain cells: multidrug resistance protein 1 mediates the release of GSH from rat astroglial cells. J Neurosci Res 69:318–326
Ballatori N, Krance SM, Marchan R, Hammond CL (2009) Plasma membrane glutathione transporters and their roles in cell physiology and pathophysiology. Mol Aspects Med 30:13–28
Keppler D (2011) Multidrug resistance proteins (MRPs, ABCCs): importance for pathophysiology and drug therapy. Handb Exp Pharmacol 201:299–323
Cole SP (2014) Targeting multidrug resistance protein 1 (MRP1, ABCC1): past, present, and future. Annu Rev Pharmacol Toxicol 54:95–117
Hirrlinger J, Konig J, Dringen R (2002) Expression of mRNAs of multidrug resistance proteins (Mrps) in cultured rat astrocytes, oligodendrocytes, microglial cells and neurones. J Neurochem 82:716–719
Hirrlinger J, Moeller H, Kirchhoff F, Dringen R (2005) Expression of multidrug resistance proteins (Mrps) in astrocytes of the mouse brain: a single cell RT-PCR study. Neurochem Res 30:1237–1244
Nies AT, Jedlitschky G, Konig J, Herold-Mende C, Steiner HH, Schmitt HP, Keppler D (2004) Expression and immunolocalization of the multidrug resistance proteins, MRP1-MRP6 (ABCC1-ABCC6), in human brain. Neuroscience 129:349–360
Mercier C, Masseguin C, Roux F, Gabrion J, Scherrmann JM (2004) Expression of P-glycoprotein (ABCB1) and Mrp1 (ABCC1) in adult rat brain: focus on astrocytes. Brain Res 1021:32–40
Dallas S, Miller DS, Bendayan R (2006) Multidrug resistance-associated proteins: expression and function in the central nervous system. Pharmacol Rev 58:140–161
Aronica E, Sisodiya SM, Gorter JA (2012) Cerebral expression of drug transporters in epilepsy. Adv Drug Deliv Rev 64:919–929
Stridh MH, Correa F, Nodin C, Weber SG, Blomstrand F, Nilsson M, Sandberg M (2010) Enhanced glutathione efflux from astrocytes in culture by low extracellular Ca2+ and curcumin. Neurochem Res 35:1231–1238
Rana S, Dringen R (2007) Gap junction hemichannel-mediated release of glutathione from cultured rat astrocytes. Neurosci Lett 415:45–48
Tulpule K, Schmidt MM, Boecker K, Goldbaum O, Richter-Landsberg C, Dringen R (2012) Formaldehyde induces rapid glutathione export from viable oligodendroglial OLN-93 cells. Neurochem Int 61:1302–1313
Murthy CR, Bender AS, Dombro RS, Bai G, Norenberg MD (2000) Elevation of glutathione levels by ammonium ions in primary cultures of rat astrocytes. Neurochem Int 37:255–268
Sagara J, Makino N, Bannai S (1996) Glutathione efflux from cultured astrocytes. J Neurochem 66:1876–1881
Scheiber IF, Dringen R (2011) Copper-treatment increases the cellular GSH content and accelerates GSH export from cultured rat astrocytes. Neurosci Lett 498:42–46
Bulcke F, Dringen R (2014) Copper oxide nanoparticles stimulate glycolytic flux and increase the cellular contents of glutathione and metallothioneins in cultured astrocytes. Neurochem Res. doi:10.1007/s11064-014-1458-0
Gegg ME, Beltran B, Salas-Pino S, Bolanos JP, Clark JB, Moncada S, Heales SJ (2003) Differential effect of nitric oxide on glutathione metabolism and mitochondrial function in astrocytes and neurones: implications for neuroprotection/neurodegeneration? J Neurochem 86:228–237
Vargas MR, Pehar M, Cassina P, Beckman JS, Barbeito L (2006) Increased glutathione biosynthesis by Nrf2 activation in astrocytes prevents p75NTR-dependent motor neuron apoptosis. J Neurochem 97:687–696
Tulpule K, Dringen R (2011) Formaldehyde stimulates Mrp1-mediated glutathione deprivation of cultured astrocytes. J Neurochem 116:626–635
Meyer N, Koehler Y, Tulpule K, Dringen R (2013) Arsenate accumulation and arsenate-induced glutathione export in astrocyte-rich primary cultures. Neurochem Int 62:1012–1019
Tadepalle N, Koehler Y, Brandmann M, Meyer N, Dringen R (2014) Arsenite stimulates glutathione export and glycolytic flux in viable primary rat brain astrocytes. Neurochem Int 76:1–11
Arend C, Brandmann M, Dringen R (2013) The antiretroviral protease inhibitor ritonavir accelerates glutathione export from cultured primary astrocytes. Neurochem Res 38:732–741
Brandmann M, Tulpule K, Schmidt MM, Dringen R (2012) The antiretroviral protease inhibitors indinavir and nelfinavir stimulate Mrp1-mediated GSH export from cultured brain astrocytes. J Neurochem 120:78–92
Gennuso F, Fernetti C, Tirolo C, Testa N, L’Episcopo F, Caniglia S, Morale MC, Ostrow JD, Pascolo L, Tiribelli C, Marchetti B (2004) Bilirubin protects astrocytes from its own toxicity by inducing up-regulation and translocation of multidrug resistance-associated protein 1 (Mrp1). Proc Natl Acad Sci USA 101:2470–2475
Ronaldson PT, Bendayan R (2008) HIV-1 viral envelope glycoprotein gp120 produces oxidative stress and regulates the functional expression of multidrug resistance protein-1 (Mrp1) in glial cells. J Neurochem 106:1298–1313
Castellano I, Merlino A (2012) γ-Glutamyltranspeptidases: sequence, structure, biochemical properties, and biotechnological applications. Cell Mol Life Sci 69:3381–3394
Dringen R, Hamprecht B, Broer S (1998) The peptide transporter PepT2 mediates the uptake of the glutathione precursor CysGly in astroglia-rich primary cultures. J Neurochem 71:388–393
Dringen R, Gutterer JM, Gros C, Hirrlinger J (2001) Aminopeptidase N mediates the utilization of the GSH precursor CysGly by cultured neurons. J Neurosci Res 66:1003–1008
Aoyama K, Nakaki T (2013) Neuroprotective properties of the excitatory amino acid carrier 1 (EAAC1). Amino Acids 45:133–142
Zafra F, Gimenez C (2008) Glycine transporters and synaptic function. IUBMB Life 60:810–817
Cabezas R, El-Bacha RS, Gonzalez J, Barreto GE (2012) Mitochondrial functions in astrocytes: neuroprotective implications from oxidative damage by rotenone. Neurosci Res 74:80–90
Sorce S, Krause KH (2009) NOX enzymes in the central nervous system: from signaling to disease. Antioxid Redox Signal 11:2481–2504
Edmondson DE (2014) Hydrogen peroxide produced by mitochondrial monoamine oxidase catalysis: biological implications. Curr Pharm Des 20:155–160
Shichiri M (2014) The role of lipid peroxidation in neurological disorders. J Clin Biochem Nutr 54:151–160
Liddell JR, Robinson SR, Dringen R (2004) Endogenous glutathione and catalase protect cultured rat astrocytes from the iron-mediated toxicity of hydrogen peroxide. Neurosci Lett 364:164–167
Dringen R, Kussmaul L, Gutterer JM, Hirrlinger J, Hamprecht B (1999) The glutathione system of peroxide detoxification is less efficient in neurons than in astroglial cells. J Neurochem 72:2523–2530
Dowell JA, Johnson JA (2013) Mechanisms of Nrf2 protection in astrocytes as identified by quantitative proteomics and siRNA screening. PLoS ONE 8:e70163
Hirrlinger J, Gutterer JM, Kussmaul L, Hamprecht B, Dringen R (2000) Microglial cells in culture express a prominent glutathione system for the defense against reactive oxygen species. Dev Neurosci 22:384–392
Hirrlinger J, Resch A, Gutterer JM, Dringen R (2002) Oligodendroglial cells in culture effectively dispose of exogenous hydrogen peroxide: comparison with cultured neurones, astroglial and microglial cells. J Neurochem 82:635–644
Dringen R, Kussmaul L, Hamprecht B (1998) Detoxification of exogenous hydrogen peroxide and organic hydroperoxides by cultured astroglial cells assessed by microtiter plate assay. Brain Res Protoc 2:223–228
Poynton RA, Hampton MB (2014) Peroxiredoxins as biomarkers of oxidative stress. Biochim Biophys Acta 1840:906–912
Liddell JR, Robinson SR, Dringen R, Bishop GM (2010) Astrocytes retain their antioxidant capacity into advanced old age. Glia 58:1500–1509
Liddell JR, Zwingmann C, Schmidt MM, Thiessen A, Leibfritz D, Robinson SR, Dringen R (2009) Sustained hydrogen peroxide stress decreases lactate production by cultured astrocytes. J Neurosci Res 87:2696–2708
Xue M, Rabbani N, Thornalley PJ (2011) Glyoxalase in ageing. Semin Cell Dev Biol 22:293–301
Tulpule K, Dringen R (2013) Formaldehyde in brain: an overlooked player in neurodegeneration? J Neurochem 127:7–21
Hambsch B (2011) Altered glyoxalase 1 expression in psychiatric disorders: cause or consequence? Semin Cell Dev Biol 22:302–308
Heck H, Casanova M (2004) The implausibility of leukemia induction by formaldehyde: a critical review of the biological evidence on distant-site toxicity. Regul Toxicol Pharmacol 40:92–106
Tong Z, Han C, Luo W, Wang X, Li H, Luo H, Zhou J, Qi J, He R (2013) Accumulated hippocampal formaldehyde induces age-dependent memory decline. Age (Dordr) 35:583–596
Tulpule K, Dringen R (2012) Formate generated by cellular oxidation of formaldehyde accelerates the glycolytic flux in cultured astrocytes. Glia 60:582–593
Tulpule K, Hohnholt MC, Dringen R (2013) Formaldehyde metabolism and formaldehyde-induced stimulation of lactate production and glutathione export in cultured neurons. J Neurochem 125:260–272
Sousa Silva M, Gomes RA, Ferreira AE, Ponces Freire A, Cordeiro C (2013) The glyoxalase pathway: the first hundred years… and beyond. Biochem J 453:1–15
Belanger M, Yang J, Petit JM, Laroche T, Magistretti PJ, Allaman I (2011) Role of the glyoxalase system in astrocyte-mediated neuroprotection. J Neurosci 31:18338–18352
Pieroh P, Koch M, Wagner DC, Boltze J, Ehrlich A, Ghadban C, Hobusch C, Birkenmeier G, Dehghani F (2014) Temporal dynamics of glyoxalase 1 in secondary neuronal injury. PLoS ONE 9:e87364
Sharma R, Shakeel Ansari GA, Awasthi YC (2007) Physiological substrates of glutathione S-transferases. In: Awasthi YC (ed) Toxicology of glutathione transferases. CRC Taylor and Francis Group, Boca Raton, pp 179–205
Zimniak P (2007) Substrates and reaction mechanisms of glutathione transferases. In: Awasthi YC (ed) Toxicology of glutathione transferases. CRC Taylor and Francis Group, Boca Raton, pp 71–103
Board PG, Menon D (2013) Glutathione transferases, regulators of cellular metabolism and physiology. Biochim Biophys Acta 1830:3267–3288
Wu B, Dong D (2012) Human cytosolic glutathione transferases: structure, function, and drug discovery. Trends Pharmacol Sci 33:656–668
Cammer W, Tansey F, Abramovitz M, Ishigaki S, Listowsky I (1989) Differential localization of glutathione-S-transferase Yp and Yb subunits in oligodendrocytes and astrocytes of rat brain. J Neurochem 52:876–883
Abramovitz M, Homma H, Ishigaki S, Tansey F, Cammer W, Listowsky I (1988) Characterization and localization of glutathione-S-transferases in rat brain and binding of hormones, neurotransmitters, and drugs. J Neurochem 50:50–57
Ahmed I, John A, Vijayasarathy C, Robin MA, Raza H (2002) Differential modulation of growth and glutathione metabolism in cultured rat astrocytes by 4-hydroxynonenal and green tea polyphenol, epigallocatechin-3-gallate. Neurotoxicology 23:289–300
Johnson JA, el Barbary A, Kornguth SE, Brugge JF, Siegel FL (1993) Glutathione S-transferase isoenzymes in rat brain neurons and glia. J Neurosci 13:2013–2023
Huang J, Philbert MA (1995) Distribution of glutathione and glutathione-related enzyme systems in mitochondria and cytosol of cultured cerebellar astrocytes and granule cells. Brain Res 680:16–22
Sagara J, Sugita Y (2001) Characterization of cytosolic glutathione S-transferase in cultured astrocytes. Brain Res 902:190–197
Rohl C, Armbrust E, Kolbe K, Lucius R, Maser E, Venz S, Gulden M (2008) Activated microglia modulate astroglial enzymes involved in oxidative and inflammatory stress and increase the resistance of astrocytes to oxidative stress in vitro. Glia 56:1114–1126
Ghosh T, Mustafa M, Kumar V, Datta SK, Bhatia MS, Sircar S, Banerjee BD (2012) A preliminary study on the influence of glutathione S transferase T1 (GSTT1) as a risk factor for late onset Alzheimer’s disease in North Indian population. Asian J Psychiatr 5:160–163
Shang W, Liu WH, Zhao XH, Sun QJ, Bi JZ, Chi ZF (2008) Expressions of glutathione S-transferase alpha, mu, and pi in brains of medically intractable epileptic patients. BMC Neurosci 9:67
Shi M, Bradner J, Bammler TK, Eaton DL, Zhang J, Ye Z, Wilson AM, Montine TJ, Pan C, Zhang J (2009) Identification of glutathione S-transferase pi as a protein involved in Parkinson disease progression. Am J Pathol 175:54–65
Pinhel MA, Sado CL, Longo Gdos S, Gregorio ML, Amorim GS, Florim GM, Mazeti CM, Martins DP, Oliveira Fde N, Nakazone MA, Tognola WA, Souza DR (2013) Nullity of GSTT1/GSTM1 related to pesticides is associated with Parkinson’s disease. Arq Neuropsiquiatr 71:527–532
Pizzurro DM, Dao K, Costa LG (2014) Astrocytes protect against diazinon- and diazoxon-induced inhibition of neurite outgrowth by regulating neuronal glutathione. Toxicology 318:59–68
Gegg ME, Clark JB, Heales SJ (2005) Co-culture of neurones with glutathione deficient astrocytes leads to increased neuronal susceptibility to nitric oxide and increased glutamate-cysteine ligase activity. Brain Res 1036:1–6
Giordano G, Kavanagh TJ, Costa LG (2009) Mouse cerebellar astrocytes protect cerebellar granule neurons against toxicity of the polybrominated diphenyl ether (PBDE) mixture DE-71. Neurotoxicology 30:326–329
Tulpule K, Hohnholt MC, Hirrlinger J, Dringen R (2014) Primary cultures of rat astrocytes and neurons as model systems to study metabolism and metabolite export from brain cells. In: Hirrlinger J, Waagepetersen H (eds) Neuromethods 90: Brain Energy Metabolism. Springer, Heidelberg, pp 45–72
Lange SC, Bak LK, Waagepetersen HS, Schousboe A, Norenberg MD (2012) Primary cultures of astrocytes: their value in understanding astrocytes in health and disease. Neurochem Res 37:2569–2588
Diaz Vivancos P, Wolff T, Markovic J, Pallardo FV, Foyer CH (2010) A nuclear glutathione cycle within the cell cycle. Biochem J 431:169178
Ribas V, Garcia-Ruiz C, Fernadez-Checa JC (2014) Glutathione and mitochondria. Front Pharmacol 5:article 5
Kurz T, Eaton JW, Brunk UT (2010) Redox activity within the lysosomal compartment: implications for aging and apoptosis. Antioxid Redox Signal 13:511–523
Huang J, Philbert MA (1996) Cellular responses of cultured cerebellar astrocytes to ethacrynic acid-induced perturbation of subcellular glutathione homeostasis. Brain Res 711:184–192
Wilkins HM, Kirchhof D, Manning E, Joseph JW, Linseman DA (2013) Mitochondrial glutathione transport is a key determinant of neuronal susceptibility to oxidative and nitrosative stress. J Biol Chem 288:5091–5101
Cacciatore I, Baldassarre L, Fornasari E, Mollica A, Pinnen F (2012) Recent advances in the treatment of neurodegenerative diseases based on GSH delivery systems. Oxid Med Cell Longev 2012:240146
Caito S, Yu Y, Aschner M (2013) Differential response to acrylonitrile toxicity in rat primary astrocytes and microglia. Neurotoxicology 37:93–99
Wegrzynowicz M, Hilgier W, Dybel A, Oja SS, Saransaari P, Albrecht J (2007) Upregulation of cerebral cortical glutathione synthesis by ammonia in vivo and in cultured glial cells: the role of cystine uptake. Neurochem Int 50:883–889
Dringen R, Hamprecht B, Drukarch B (1998) Anethole dithiolethione, a putative neuroprotectant, increases intracellular and extracellular glutathione levels during starvation of cultured astroglial cells. Naunyn Schmiedebergs Arch Pharmacol 358:616–622
Li Y, Bao Y, Jiang B, Wang Z, Liu Y, Zhang C, An L (2008) Catalpol protects primary cultured astrocytes from in vitro ischemia-induced damage. Int J Dev Neurosci 26:309–317
Garcion E, Sindji L, Leblondel G, Brachet P, Darcy F (1999) 1,25-dihydroxyvitamin D3 regulates the synthesis of γ-glutamyl transpeptidase and glutathione levels in rat primary astrocytes. J Neurochem 73:859–866
Schmidt MM, Dringen R (2010) Fumaric acid diesters deprive cultured primary astrocytes rapidly of glutathione. Neurochem Int 57:460–467
Frade J, Pope S, Schmidt M, Dringen R, Barbosa R, Pocock J, Laranjinha J, Heales S (2008) Glutamate induces release of glutathione from cultured rat astrocytes—a possible neuroprotective mechanism? J Neurochem 105:1144–1152
Im JY, Paik SG, Han PL (2006) Cadmium-induced astroglial death proceeds via glutathione depletion. J Neurosci Res 83:301–308
Jia Z, Zhu H, Li Y, Misra HP (2009) Cruciferous nutraceutical 3H-1,2-dithiole-3-thione protects human primary astrocytes against neurocytotoxicity elicited by MPTP, MPP+, 6-OHDA, HNE and acrolein. Neurochem Res 34:1924–1934
Wang L, Jiang H, Yin Z, Aschner M, Cai J (2009) Methylmercury toxicity and Nrf2-dependent detoxification in astrocytes. Toxicol Sci 107:135–143
Bellaver B, Souza DG, Souza DO, Quincozes-Santos A (2014) Resveratrol increases antioxidant defenses and decreases proinflammatory cytokines in hippocampal astrocyte cultures from newborn, adult and aged Wistar rats. Toxicol In Vitro 28:479–484
Correa F, Mallard C, Nilsson M, Sandberg M (2012) Dual TNFα-induced effects on NRF2 mediated antioxidant defence in astrocyte-rich cultures: role of protein kinase activation. Neurochem Res 37:2842–2855
Dasgupta A, Das S, Sarkar PK (2007) Thyroid hormone promotes glutathione synthesis in astrocytes by up regulation of glutamate cysteine ligase through differential stimulation of its catalytic and modulator subunit mRNAs. Free Radic Biol Med 42:617–626
Carrera MP, Antolin I, Martin V, Sainz RM, Mayo JC, Herrera F, Garcia-Santos G, Rodriguez C (2007) Antioxidants do not prevent acrylonitrile-induced toxicity. Toxicol Lett 169:236–244
Ehrke E, Arend C, Dringen R (2014) 3-Bromopyruvate inhibits glycolysis, depletes cellular glutathione, and compromises the viability of cultured primary rat astrocytes. J Neurosci Res. doi:10.1002/jnr.23474
Schmidt MM, Rohwedder A, Dringen R (2011) Effects of chlorinated acetates on the glutathione metabolism and on glycolysis of cultured astrocytes. Neurotox Res 19:628–637
Clemedson C, Romert L, Odland L, Varnbo I, Walum E (1994) Biotransformation of carbon tetrachloride in cultured neurons and astrocytes. Toxicol In Vitro 8:145–152
Kaur P, Aschner M, Syversen T (2007) Role of glutathione in determining the differential sensitivity between the cortical and cerebellar regions towards mercury-induced oxidative stress. Toxicology 230:164–177
Liao SL, Ou YC, Chang CY, Chen WY, Kuan YH, Wang WY, Pan HC, Chen CJ (2013) Diethylmaleate and iodoacetate in combination caused profound cell death in astrocytes. J Neurochem 127:271–282
O’Connor E, Devesa A, Garcia C, Puertes IR, Pellin A, Vina JR (1995) Biosynthesis and maintenance of GSH in primary astrocyte cultures: role of L-cystine and ascorbate. Brain Res 680:157–163
Schmidt MM, Greb H, Koliwer-Brandl H, Kelm S, Dringen R (2010) 2-Deoxyribose deprives cultured astrocytes of their glutathione. Neurochem Res 35:1848–1856
Schmidt MM, Dringen R (2009) Differential effects of iodoacetamide and iodoacetate on glycolysis and glutathione metabolism of cultured astrocytes. Front Neuroenerg 1:1–10
Waak J, Dringen R (2006) Formation and rapid export of the monochlorobimane-glutathione conjugate in cultured rat astrocytes. Neurochem Res 31:1409–1416
Ré DB, Boucraut J, Samuel D, Birman S, Kerkerian-Le Goff L, Had-Aissouni L (2003) Glutamate transport alteration triggers differentiation-state selective oxidative death of cultured astrocytes: a mechanism different from excitotoxicity depending on intracellular GSH contents. J Neurochem 85:1159–1170
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Special Issue: In honor of Gerald Dienel.
Rights and permissions
About this article
Cite this article
Dringen, R., Brandmann, M., Hohnholt, M.C. et al. Glutathione-Dependent Detoxification Processes in Astrocytes. Neurochem Res 40, 2570–2582 (2015). https://doi.org/10.1007/s11064-014-1481-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-014-1481-1