Abstract
Mitochondrial autophagy (Mitophagy), the specific autophagic elimination of mitochondria, has been related with several forms of degenerative disease and mitochondrial dysfunction. It is involved in multiple cellular processes. In addition to one of its established key roles in the maintenance of normal cellular phenotype and function, there is growing interest in the concept that targeted modulation of mitophagy may reduce cerebral ischaemia/reperfusion injury. Induction of mitophagy results in selective clearance of damaged mitochondria in cells. In response to stress such as ischaemia/reperfusion, prosurvival and prodeath pathways are concomitantly activated in neuronal cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
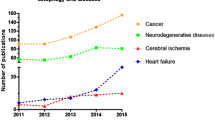
Autophagy, widely existing in eukaryotic cells, is a lysosomal degradation pathway with an astonishing number of connections to human disease and physiology. For example, autophagic dysfunction is associated with cancer, neurodegeneration, microbial infection and ageing [1, 2]. The ubiquitin–proteasome system (UPS) and autophagy-lysosome pathway (ALP) are the two most important mechanisms that normally repair or remove abnormal proteins. In contrast to the UPS, the major inducible pathway autophagy is likely to be the primary mechanism involved in the degradation of long-lived, stable proteins and is the only mechanism by which entire organelles such as mitochondria are recycled. Large membrane proteins and protein complexes that fail to pass through the narrow proteasome barrel can be degraded by autophagy [3]. Autophagy regulation is very complex. The mammalian target of rapamycin (mTOR), such as phosphatidylinositol 3-kinase/protein kinase B (PI3K/PKB), adenosine triphosphate/adenosine monophosphate-activated protein kinase (ATP/AMPK), is involved in the occurrence and form of autophagy [4–6] (Fig. 1). mTOR, a negative regulator of autophagy, is a serine/threonine protein kinase which controls cells reaction when the nutrition conditions change and regulates many pathways of energy metabolism. mTOR is considered to be the regulatory mechanism of autophagy [7, 8]. 3-Methyladenine (3-MA), a special inhibitor of autophagy, can activate target of rapamycin (TOR) to reduce the occurrence of autophagy by inhibiting the PI3K pathway [9]. TOR kinase mainly inhibits autophagy through two mechanisms. One is that TOR can be the signaling cascade to control transcription and translation by the downstream factor, such as ribosomal p70S6 kinase (S6K1) and eukaryotic initiation factor 4E-binding protein 1(eIF-4E). The other is that TOR, in the role of autophagy-related proteins, can directly or indirectly influence the formation of autophagosome [10]. Regulation of autophagy in recent reports mainly focuses on mTOR dependence or independence pathways [11–13] (Fig. 1). Rapamycin activate macroautophagy by inhibiting mTOR, the contra lateral site of autophagy [14]. Our latest research also confirmed that rapamycin is able to prevent the apoptosis of dopaminergic neurons following 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) induced treatment, likely via activation of autophagy pathways. The rapamycin pretreatment may therefore be a promising protection effect [15, 16].
Concurrent mitochondrial elimination and autophagy in many systems has led to the proposal that autophagy is the main mechanism of mitochondrial turnover during development and under pathological conditions. The term mitophagy was coined to describe the selective removal of mitochondria by autophagy but the process itself is still contentious [17]. There is a delicate balance between life and death in the neuronal cells during stress such as ischaemia/reperfusion (I/R), and the final outcome depends on the complex cross-talk between these pathways [18]. In this review, we provide a brief review of the roles of mitophagy in cerebral I/R injury, and discuss the controversies and challenges in exploiting mitophagy as a therapeutic strategy.
The Concept of Mitophagy
Mitochondria have double membranes and are essential organelles involved with oxidative phosphorylation, calcium homeostasis, reactive oxygen species (ROS) management, and programmed cell death [19–21]. In normal mammalian brains, it has been shown that mitochondria have an average half-life of 10–25 days [22]. Mitophagy was first observed in mammalian cells by Lemaster [17, 23]. During starvation, mitochondrial turnover can be accelerated by an autophagic process specifically called mitophagy [23–25]. Mitophagy and macroautophagy can be separated not only based on their different triggers, molecular mechanisms, consequences, but also based on the mitochondrial morphologies that characterize them: mitophagy is preceded by organelle fragmentation, while autophagy is accompanied conversely by their elongation [26].
Mitophagy is controlled either in conjunction with general macroautophagy or selectively through specific mitophagy genes. As in yeast and in mammalian cells, mitophagy can be selective and specific. Youth protein 1 (Uth1p), ancient ubiquitous protein 1 (Aup1p) and autophagy-related 32 (Atg32) are necessary for mitophagy in yeast. Uth1p is a member of the so-called SUN family [27], which is required for the removal of excessive mitochondria during starvation [28]. In addition, Aup1p, one of a family of protein phosphatase homologs, is also required for efficient mitophagy in stationary-phase cells. Atg32 is a 59-kDa protein which is critical for its interaction with Atg8 and Atg11. Recent studies found that Atg11 is also required for mitophagy [29, 30]. It was found that Atg32 is phosphorylated after nitrogen starvation, and the phosphorylation of Atg32 is required for mitophagy [31]. High osmolarity glycerol response protein 1 (Hog1) is a mitogen-activated protein kinase in yeast. Deletion of either Hog1 leads to inhibition of Atg32 phosphorylation as well as mitophagy [32].
Mammalian homologues of Atg32, Uth1p, and Aup1p have not been found. NIP3-like protein X (NIX), unc-51-like kinase 1 (ULK1) and Parkin are three proteins that can signal specific mitophagy in mammalian cells. AMPK is activated in response to decreased intracellular ATP and then phosphorylates ULK1 and ULK2 (two Atg1 homologues) to activate both general macroautophagy and mitophagy [25, 33]. ULK1, a serine threonine kinase, is a critical regulator of mitochondrial and ribosomal clearance during the final stages of erythroid maturation. Thus, many more reticulocytes with normal/numerous mitochondria that retained normal membrane potential accumulated in ULK1 knockout mice. As with all the other studies that show specificity, expression of ULK1p was not essential for induction of macroautophagy in response to nutrient deprivation or for survival of newborn mice. It should be noted that eventually, ULK1−/− cells cleared their organelles. The authors implicate NIX in this process [34, 35]. Together, these data suggest that the Atg1 homologue ULK1 is a component of the selective autophagy machinery that leads to the elimination of organelles in erythroid cells. Unlike Atg1, it is not an essential mechanistic component of mitophagy in erythrocyte maturation [16, 31].
Some studies found NIX, which is a homologue of BCL2/adenovirus E1B interacting protein 3 (BNIP3), and a member of inducible BCL2 homology domain 3 families, is regulated by hypoxia. The induction of mitophagy by NIX is thought to be mediated by direct binding to microtubule-associated protein 1 light chain 3 (LC3) and gamma-aminobutyric acid receptor associated protein (GABARAP) [36, 37]. NIX could be involved in the maturation of immature red blood cells by mitophagy and potentially induce mitophagy through apoptotic signaling [17, 37]. NIX mitochondria were robustly filled with a loss of mitochondrial membrane potential (ΔΨm)-dependent mitochondrial dye [17]. In mammalian cells, NIX is involved in mitochondrial clearance during erythrocyte maturation [25, 32].
Parkin is an E3 ubiquitin ligase, dysregulation of which is linked to Parkinson’s disease and loss of neurons of the substantia nigra [37]. Upon mitochondrial damage, mitochondria-localized phosphatase and tensin homolog-induced putative kinase 1 (PINK1) recruits E3-ligase Parkin to mitochondria. Ubiquitinated mitofusins are then degraded by proteasome that is recruited to mitochondria together with p97. Mitofusin degradation blocks fusion events and mitophagy can be activated. At the same time, Parkin can polyubiquitinate voltage-dependent anion channel 1 (VDAC1) creating K27-linked Ub-chains that recruit p62. Binding of p62 to VDAC1 on the mitochondria and Atg8/LC3/GABARAP on the developing autophagosome, results in mitochondrial sequestration and removal by autophagic machinery [17, 32, 36, 37].
Regulators of calcineurin 1 (RCAN1s) are identified as regulators of mitophagy. Recent research demonstrates that induction of RCAN1-1L can cause dramatic degradation of mitochondria. The mechanisms of such degradation involve the adenine nucleotide translocator and mitochondrial permeability transition pore opening [38].
Attention to date has focused largely on the mitophagy programmed cell death in cerebral I/R. In the past few years, the evidence of mitophagy for cell function is critically examined [39]. The modulation of mitophagy mechanisms of neural cells has recently been implicated as well [17, 25, 26, 37, 40]. Mitophagy functions as an eneuronal protective response, favoring adaptation to stress by removing damaged mitochondria. In contrast, increased oxidative stress and apoptotic proteases can inactivate mitophagy, allowing for the execution of cell death [18] (Fig. 2).
Autophagy in Cerebral Ischaemia/Reperfusion
Hypoxia is involved in the ischemic stroke [41]. Autophagy is markedly activated after neonatal ischaemia. The amount of LC3-II increases and highly correlates with the number of autophagosome [42]. Beclin 1, a component of the PI3K complex that is required for autophagy and LC3, a microtubule-associated protein that is lipidated upon activation of autophagy, rapidly increase in cells of the injured side [43–45]. Furthermore, during reperfusion period in stroke and brain trauma, inflammation response occurs and causes injury. Because this reperfusion induced injury is involved in the brain’s ischemic cascade and reintroduction of oxygen within cells may cause damage to cellular proteins, DNA, and the plasma membrane [46, 47]. Recent study found that rapamycin administration increases autophagy, decreases apoptosis and significantly reduces brain damage. After hypoxia–ischaemia, when autophagy is blocked neuronal cells rapidly progress toward necrotic cell death [48]. Rapamycin can reduce infarct volume, brain edema and motor deficits induced by permanent focal ischaemia and increase the protein levels of LC3-II and beclin [49]. In contrast, this increased cell death was inhibited by the specific autophagy inhibitor, 3-MA [47, 50]. 3-MA reduced the increased Beclin 1 expression, the neuroprotective effect of rapamycin without affecting Akt phosphorylation. However, both compounds significantly increased necrotic cell death. Taken together, these data indicate that in neonatal hypoxia–ischaemia autophagy can be part of an integrated prosurvival signaling which includes the PI3K/Akt-mTOR axis. When the autophagic or the PI3K/Akt-mTOR pathways are interrupted cells undergo necrotic cell death [48].
Mitophagy in Cerebral Ischaemia/Reperfusion
Ischaemia and reperfusion are two fundamental events that cause cerebral damage. Different mechanisms may take a lead in the evolution of brain injury: initiated by mitochondrial dysfunction, cellular injury, followed by the neuroinflammation [51]. Mitochondrial dysfunction is the key mechanism of cell damage in cerebral hypoxia–ischaemia and reperfusion. Neurons rely heavily upon mitophagy for normal development and function [52]. Neurons are particularly dependent on mitochondria, the power generators, for ATP production. These cells are more sensitive to mitochondrial dysfunction. Dynamic mitochondrial changes in their shape and populations are critical for normal cellular energy homeostasis. Many recent studies suggest that neuronal cell death is related to mitochondrial dysfunction in stroke [19, 53].
Mitochondria are the major sites of generation and action of ROS in brain cells [25]. Mitophagy is up-regulated in a neuroprotective effort to protect the nerve cells from excessive damage due to an accumulation of dysfunctional mitochondria [54]. ΔΨm appears to be a common feature of mitophagy. A damaged mitochondrion signals the autophagic machinery to remove it—perhaps via ROS production [17].
The different steps of mitophagy are regulated by Atg proteins. Mitophagy describes the engulfment of mitochondria into vesicles that are coated with the autophagosome marker mannosidase processing 1 (MAP1) LC3 [37]. Mitochondrial respiratory chain is increasingly recognized as a source for ROS in the postischemic tissue [51]. ROS activates the protease Atg4B, the enzyme that cleaves the c-terminus of LC3-I, an essential precursor to conversion of LC3I to LC3II. Via ROS production, the autophagic machinery is signaled to remove a damaged mitochondrion [55]. ROS, such as superoxide, hydrogen peroxide, and hydroxyl radical, attack proteins, lipids and nucleic acids and initiate peroxidation chain reactions, contribute to the reperfusion-driven oxidative stress and promote mitochondrial membrane permeabilization. The loss of mitochondrial membranes integrity during reperfusion is considered as the major mechanism of secondary energy failure [23, 51]. Mitophagy regulates mitochondrial number to match metabolic demand and might also be a form of quality control to remove damaged mitochondria [37]. Excessive or damaged mitochondria may generate ROS and release proapoptotic proteins to promote cell death [56]. Tracking multiple proteins in different steps of the mitophagy could be employed to evaluate relative contributions of I/R injury.
Mitochondrial fission protein dynamin-related protein 1 (Drp1) and fusion protein optic atrophy 1 (Opa1) were both upregulated in the ischemic penumbra. In contrast, both Drp1 and Opa1 showed progressive decreases in the ischemic core because of necrotic brain damage. The present study suggests that there was a continuous mitochondrial fission and fusion during these periods in the ischemic penumbra after hypoxia–ischaemia, probably in an effort toward mitophagy and cellular survival. A mitochondrial fission and fusion in the dying neurons, probably in an effort toward mitophagy and cellular survival [19].
Rapamycin and Propofol Regulate Cerebral Ischaemia/Reperfusion
Rapamycin, a lipophilic macrolide antibiotic, has been found to reduce injury in different models of neurodegenerative disorders. The neuroprotective effect of rapamycin was associated with increased autophagy and decreased caspase-3 activation because after rapamycin treatment there was a marked reduction of Bax and Bad translocation to mitochondria, cytochrome c release, and caspase-3 activation. The TOR pathway, which senses nutrient availability and environmental stress, has recently emerged as a major regulator of lifespan. The TOR complex 1 (TORC1) and its downstream effectors influence lifespan by regulating cellular metabolism and mitochondrial functions. TORC1 can regulate mitochondrial biogenesis and turnover through the Atgs. TORC1 influences the levels of mitochondrial ROS. Defects in the clearance of damaged mitochondria by TORC1-regulated autophagy also contribute to ROS accumulation [57, 58]. Rapamycin administered before I/R injury prevents the apoptotic signaling taking place through the mitochondrial pathway [59].
In another research, propofol reduced the I/R-induced death of cells. The prevention of neuron death by the inhibition of autophagy after hypoxic-ischemic injury has been documented to be dependent on an autophagy induction-related gene, Atg7. The present results indicate that a group of factors including class III PI3K, Beclin 1 and Bcl2 are also engaged in the neuroprotection of propofol against oxygen-glucose deprivation-induced damage in neuronal PC12 cells [60].
Conclusion
Mitophagy is the specific degradation of the mitochondria in response to global signals, including starvation and oxidative stress, or specific signals including mitochondrial targeting of signaling proteins or modification of mitochondrial proteins. As it is an essential cellular pathway to eliminate damaged or depolarized mitochondria to maintain the homeostasis of cells, the dysfunction of mitophagy is closely related to cerebral diseases. Mitophagy pathway can be activated after focal cerebral I/R. It may be a therapeutic strategy to protect the nerve cells by regulating the mitophagy pathway after cerebral I/R injury.
In recent years, the research of mitophagic molecular mechanism has made great progress. However, the regulation of mitophagy, especially a variety of interaction between promotion and inhibition, has limited information. Therefore, while in the study of autophagy has achieved some successes; there are still many unknown issues to be researched. We believe that we will have a deeper understanding of mitophagy eventually, and regulate mitophagy as targets for treatment. This will help the treatment of ischemic stroke.
References
Levine B, Kroemer G (2008) Autophagy in the pathogenesis of disease. Cell 132(1):27–42
Mizushima N et al (2008) Autophagy fights disease through cellular self-digestion. Nature 451(7182):1069–1075
Pan T et al (2008) The role of autophagy-lysosome pathway in neurodegeneration associated with Parkinson’s disease. Brain 131(Pt 8):1969–1978
Pattingre S et al (2008) Regulation of macroautophagy by mTOR and Beclin 1 complexes. Biochimie 90(2):313–323
McCray BA, Taylor JP (2008) The role of autophagy in age-related neurodegeneration. Neurosignals 16(1):75–84
Yang YP et al (2005) Molecular mechanism and regulation of autophagy. Acta Pharmacol Sin 26(12):1421–1434
Liu K et al (2011) Activation of growth hormone secretagogue type 1a receptor inhibits T-type Ca2+ channel currents through pertussis toxin-sensitive novel protein kinase C pathway in mouse spermatogenic cells. Cell Physiol Biochem 27(5):613–624
Liu K et al (2008) Autophagic degradation pathway and possible mechanisms of mutant-type α-synuclein. Chin J Neurol 41(1):51–56
Zeng M, Zhou JN (2008) Roles of autophagy and mTOR signaling in neuronal differentiation of mouse neuroblastoma cells. Cell Signal 20(4):659–665
Cardenas ME et al (1999) The TOR signaling cascade regulates gene expression in response to nutrients. Genes Dev 13(24):3271–3279
Sarkar S et al (2009) Rapamycin and mTOR-independent autophagy inducers ameliorate toxicity of polyglutamine-expanded huntingtin and related proteinopathies. Cell Death Differ 16(1):46–56
Sarkar S et al (2007) Small molecules enhance autophagy and reduce toxicity in Huntington’s disease models. Nat Chem Biol 3(6):331–338
He C, Klionsky DJ (2009) Regulation mechanisms and signaling pathways of autophagy. Annu Rev Genet 43:67–93
Rubinsztein DC (2006) The roles of intracellular protein-degradation pathways in neurodegeneration. Nature 443(7113):780–786
Liu K et al (2013) Therapeutic effects of rapamycin on MPTP-induced Parkinsonism in mice. Neurochem Res 38(1):201–207
Liu K et al (2012) Protection against neurotoxicity by an autophagic mechanism. Braz J Med Biol Res 45(5):401–407
Tolkovsky AM (2009) Mitophagy. Biochim Biophys Acta 1793(9):1508–1515
Kubli DA, Gustafsson AB (2012) Mitochondria and mitophagy: the yin and yang of cell death control. Circ Res 111(9):1208–1221
Liu W et al (2012) Dynamic changes of mitochondrial fusion and fission proteins after transient cerebral ischemia in mice. J Neurosci Res 90(6):1183–1189
Henze K, Martin W (2003) Evolutionary biology: essence of mitochondria. Nature 426(6963):127–128
Vosler PS et al (2009) Mitochondrial targets for stroke: focusing basic science research toward development of clinically translatable therapeutics. Stroke 40(9):3149–3155
Menzies RA, Gold PH (1971) The turnover of mitochondria in a variety of tissues of young adult and aged rats. J Biol Chem 246(8):2425–2429
Lemasters JJ (2005) Selective mitochondrial autophagy, or mitophagy, as a targeted defense against oxidative stress, mitochondrial dysfunction, and aging. Rejuvenation Res 8(1):3–5
Dengjel J, Kristensen AR, Andersen JS (2008) Ordered bulk degradation via autophagy. Autophagy 4(8):1057–1059
Lee J, Giordano S, Zhang J (2012) Autophagy, mitochondria and oxidative stress: cross-talk and redox signalling. Biochem J 441(2):523–540
Gomes LC, Scorrano L (2013) Mitochondrial morphology in mitophagy and macroautophagy. Biochim Biophys Acta 1833(1):205–212
Austriaco NR Jr (1996) Review: to bud until death: the genetics of ageing in the yeast, Saccharomyces. Yeast 12(7):623–630
Kissova I et al (2004) Uth1p is involved in the autophagic degradation of mitochondria. J Biol Chem 279(37):39068–39074
Kanki T et al (2009) Atg32 is a mitochondrial protein that confers selectivity during mitophagy. Dev Cell 17(1):98–109
Okamoto K, Kondo-Okamoto N, Ohsumi Y (2009) Mitochondria-anchored receptor Atg32 mediates degradation of mitochondria via selective autophagy. Dev Cell 17(1):87–97
Aoki Y et al (2011) Phosphorylation of Serine 114 on Atg32 mediates mitophagy. Mol Biol Cell 22(17):3206–3217
Ding WX, Yin XM (2012) Mitophagy: mechanisms, pathophysiological roles, and analysis. Biol Chem 393(7):547–564
Egan DF et al (2011) Phosphorylation of ULK1 (hATG1) by AMP-activated protein kinase connects energy sensing to mitophagy. Science 331(6016):456–461
Sandoval H et al (2008) Essential role for Nix in autophagic maturation of erythroid cells. Nature 454(7201):232–235
Schweers RL et al (2007) NIX is required for programmed mitochondrial clearance during reticulocyte maturation. Proc Natl Acad Sci USA 104(49):19500–19505
Novak I (2012) Mitophagy: a complex mechanism of mitochondrial removal. Antioxid Redox Signal 17(5):794–802
Youle RJ, Narendra DP (2011) Mechanisms of mitophagy. Nat Rev Mol Cell Biol 12(1):9–14
Ermak G et al (2012) Chronic expression of RCAN1-1L protein induces mitochondrial autophagy and metabolic shift from oxidative phosphorylation to glycolysis in neuronal cells. J Biol Chem 287(17):14088–14098
Scherz-Shouval R, Elazar Z (2011) Regulation of autophagy by ROS: physiology and pathology. Trends Biochem Sci 36(1):30–38
Rambold AS, Lippincott-Schwartz J (2011) Mechanisms of mitochondria and autophagy crosstalk. Cell Cycle 10(23):4032–4038
Hossmann KA (2006) Pathophysiology and therapy of experimental stroke. Cell Mol Neurobiol 26(7–8):1057–1083
Tian F et al (2010) In vivo imaging of autophagy in a mouse stroke model. Autophagy 6(8):1107–1114
Carloni S, Buonocore G, Balduini W (2008) Protective role of autophagy in neonatal hypoxia-ischemia induced brain injury. Neurobiol Dis 32(3):329–339
Balduini W, Carloni S, Buonocore G (2012) Autophagy in hypoxia-ischemia induced brain injury. J Matern Fetal Neonatal Med 25(Suppl 1):30–34
Rami A, Langhagen A, Steiger S (2008) Focal cerebral ischemia induces upregulation of Beclin 1 and autophagy-like cell death. Neurobiol Dis 29(1):132–141
Wieloch T, Siesjo BK (1982) Ischemic brain injury: the importance of calcium, lipolytic activities, and free fatty acids. Pathol Biol (Paris) 30(5):269–277
Shi R et al (2012) Excessive autophagy contributes to neuron death in cerebral ischemia. CNS Neurosci Ther 18(3):250–260
Carloni S et al (2010) Activation of autophagy and Akt/CREB signaling play an equivalent role in the neuroprotective effect of rapamycin in neonatal hypoxia-ischemia. Autophagy 6(3):366–377
Sheng R et al (2010) Autophagy activation is associated with neuroprotection in a rat model of focal cerebral ischemic preconditioning. Autophagy 6(4):482–494
Puyal J, Clarke PG (2009) Targeting autophagy to prevent neonatal stroke damage. Autophagy 5(7):1060–1061
Ten VS, Starkov A (2012) Hypoxic-ischemic injury in the developing brain: the role of reactive oxygen species originating in mitochondria. Neurol Res Int 2012:542976
Chen H, Chan DC (2009) Mitochondrial dynamics–fusion, fission, movement, and mitophagy—in neurodegenerative diseases. Hum Mol Genet 18(2):R169–R176
Besancon E et al (2008) Beyond NMDA and AMPA glutamate receptors: emerging mechanisms for ionic imbalance and cell death in stroke. Trends Pharmacol Sci 29(5):268–275
Goldman SJ et al (2010) Autophagy and the degradation of mitochondria. Mitochondrion 10(4):309–315
Scherz-Shouval R, Elazar Z (2007) ROS, mitochondria and the regulation of autophagy. Trends Cell Biol 17(9):422–427
Bueler H (2010) Mitochondrial dynamics, cell death and the pathogenesis of Parkinson’s disease. Apoptosis 15(11):1336–1353
Wu JJ et al (2009) Mitochondrial dysfunction and oxidative stress mediate the physiological impairment induced by the disruption of autophagy. Aging (Albany NY) 1(4):425–437
Pan Y et al (2012) Metabolic regulation, mitochondria and the life-prolonging effect of rapamycin: a mini-review. Gerontology 58(6):524–530
Carloni S et al (2012) Inhibition of rapamycin-induced autophagy causes necrotic cell death associated with Bax/Bad mitochondrial translocation. Neuroscience 203:160–169
Cui D et al (2012) Propofol prevents autophagic cell death following oxygen and glucose deprivation in PC12 cells and cerebral ischemia-reperfusion injury in rats. PLoS ONE 7(4):e35324
Acknowledgments
This work was supported by grants from the project of National Natural Science Foundation of China (No. 31171014 and No. 30970869), the project of Science and Technology Commission of Shanghai Municipality (No. 09DZ1950400) and Board of Health of Shanghai, China (No. 2008086), the youth projects of National Natural Science Foundation of China (No. 31100783) and Youth Key Project in Shanghai college of Medicine of Fudan University (No. 09-L37).
Author information
Authors and Affiliations
Corresponding author
Additional information
Kangyong Liu and Yinyi Sun contributed to this work equally.
Rights and permissions
About this article
Cite this article
Liu, K., Sun, Y., Gu, Z. et al. Mitophagy in Ischaemia/Reperfusion Induced Cerebral Injury. Neurochem Res 38, 1295–1300 (2013). https://doi.org/10.1007/s11064-013-1033-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-013-1033-0