Abstract
Several genes have been implicated as influencing the outcome following traumatic brain injury (TBI). Currently the most extensively studied gene has been APOE. APOE can influence overall and rehabilitation outcome, coma recovery, risk of posttraumatic seizures, as well as cognitive and behavioral functions following TBI. Pathologically, APOE is associated with increased amyloid deposition, amyloid angiopathy, larger intracranial hematomas and more severe contusional injury. The proposed mechanism by which APOE affects the clinciopathological consequences of TBI is multifactorial and includes amyloid deposition, disruption of cytoskeletal stability, cholinergic dysfunction, oxidative stress, neuroprotection and central nervous system plasticity in response to injury. Other putative genes have been less extensively studied and require replication of the clinical findings. The COMT and DRD2 genes may influence dopamine dependent cognitive processes such as executive/frontal lobe functions. Inflammation which is a prominent component in the pathophysiological cascade initiated by TBI, is in part is mediated by the interleukin genes, while apoptosis that occurs as a consequence of TBI may be modulated by polymorphisms of the p53 gene. The ACE gene may affect TBI outcome via mechanisms of cerebral blood flow and/or autoregulation and the CACNA1A gene may exert an influence via the calcium channel and its effect on delayed cerebral edema. Although several potential genes that may influence outcome following TBI have been identified, future investigations are needed to validate these genetic studies and identify new genes that might influence outcome following TBI.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Several genes have been implicated as influencing the outcome following traumatic brain injury (TBI). Currently the most extensively studied gene is apolipoprotein E (APOE). However, several other genes have been investigated and/or speculated. These include APOE promoter, catechol-o-methyltransferase (COMT), dopamine D2 receptor (DRD2), interleukin, p53, and CACNA1A genes. The following paper will review the current state of knowledge regarding genetic influences on outcome following TBI and discuss possible mechanisms and methodological considerations.
Apolipoprotein E
The APOE gene, which encodes for a cholesterol carrier lipoprotein is polymorphic and exists in three common isoforms ε2, ε3, and ε4. APOE ε4 allele has been identified as susceptibility gene for late onset familial and sporadic Alzheimer’s disease [1–3]. In the clinical literature, many studies support the hypothesis that APOE genotype influences the outcome from TBI [4–22] Teasedale et al. [4] in a prospective evaluation of 89 patients sustaining TBI, observed that 17 (57%) of 30 patients with APOE ε4 had an unfavorable outcome at 6 months compared with 16 (27%) of 59 patients without APOE ε4. Unfavorable outcome was defined as dead, vegetative state, or severe disability using the Glasgow Outcome Scale (GOS). Also using the GOS, Chiang et al. [5] observed similar findings regarding overall outcome at 6 months following TBI. In this prospective investigation of 100 patients with TBI admitted to a neurosurgical unit, 52% of patients with the ε4 allele exhibited an unfavorable outcome compared with 21% of patients without the ε4 allele. Individuals with the ε4 allele also tended to experience longer hospital stays (39.2 days for +ε4 allele group and 27.9 days for the −ε4 allele group).
In addition to influencing overall outcome, APOE may also influence various clinical aspects of TBI. Friedman et al. [6] noted that individuals with the APOE ε4 allele were five times more likely to experience more than 7 days of unconsciousness following TBI. Furthermore, patients with posttraumatic unawareness who did not recover had a higher frequency of the ε4 allele compared with those who did recover [7]. It has also been observed that patients possessing the ε4 allele tend to experience larger intracranial hematomas following TBI [8] and are at increased risk of posttraumatic seizures [9].
APOE may also influence rehabilitation outcome following TBI. Friedman et al. [6] reported a strong association between the APOE ε4 allele and a poor clinical outcome. In this investigation, 1 of 27 (3%) of individuals with the APOE ε4 allele had a favorable outcome compared to 13 of 42 (31%) of those without the ε4 allele. A favorable outcome was defined by the absence of dysarthria or dysphasia, lack of behavioral abnormalities, no evidence of severe cognitive impairment, and the ability to live independently. Lichtman et al. [10] also noted that patients with the APOE ε4 allele experienced a poorer outcome than those without the e4 allele following rehabilitation. This differential in recovery was noted in the total and motor Functional Independence Measures (FIM) scores but not in the cognitive FIM score. The lack of a difference noted in cognitive function may reflect the relative insensitivity of the cognitive portion of the FIM. In a 1 year follow up of 39 patients with TBI who completed a neuropsychological rehabilitation program, the presence of the APOE ε4 allele was associated with poorer outcome [11]. Patients with the APOE ε4 allele showed deterioration in functioning compared to those without the APOE ε4 allele.
Several studies suggest that APOE may influence cognitive and/or behavioral function following TBI. Liberman et al. [12] noted that patients possessing the ε4 allele exhibited lower mean scores on 12 of 13 neuropsychological test measures compared to those without the ε4 allele following predominantly mild TBI. Two tests, the grooved pegboard and the paced auditory serial addition task, were statistically significant. Similarly, Sundstrom et al. [13] using within person comparisons also assessed cognitive function in a small cohort of individuals before and after mild TBI. In this study, patients with the ε4 allele exhibited significantly decreased performance on tests of divided attention, facial recognition and recall of actions. Crawford et al. [14] has presented evidence that APOE gene may influence memory function following TBI and observed that ε4 positive subjects had more impairments on memory testing than those patients that were ε4 negative. The ε4 allele had no effect on executive function. In contrast, in an analysis of 77 patients suffering from moderate to severe TBI, those with the ε4 allele in addition to demonstrating impaired learning and verbal memory, also exhibited impairments in frontal lobe functioning such as motor speed, fine motor coordination, visual scanning, attention, executive function and mental flexibility [16]. Koponen et al. [15] reported that the ε4 allele was more commonly associated with dementia and not psychiatric disorders following TBI. Individuals with the ε4 allele experienced a statistically significantly higher frequency of definite and subclinical dementia when assessed on an average 31 years following moderate and severe TBI. Carriers of the ε4 allele have also been observed to exhibit more behavioral disturbances than those without the ε4 allele [16].
APOE genotype may also influence neurocognitive outcome following sports related TBI. In an APOE genotype analysis of 30 active and retired boxers, high exposure boxers (i.e. those with greater than 12 professional bouts) who possessed the ε4 allele exhibited more neurological impairment than those high exposure boxers without the ε4 [17]. In addition, all of the boxers with severe CTBI possessed an APOE ε4 allele. The ε4 allele had no effect on neurological function in low exposure boxers. In agreement with the boxing study, older active professional football players possessing the APOE ε4 allele scored lower on cognitive tests than did older active players without the allele or younger active players of any genotype [18]. Football players with the ε4 allele performed poorer in the areas of memory, attention, and reaction time. Both studies, although based on relatively small sample sizes, suggest that there may be an interaction between exposure to TBI and APOE genotype on neurological outcome in contact/collision sports.
Autopsy studies have provided information regarding the neuropathological features associated with the inheritance of the ε4 allele. Individuals possessing the ε4 allele exhibit more amyloid deposition in the brain following fatal TBI [19], are 8.75 times more likely to develop cerebral amyloid angiopathy [20], and experience more severe contusional injury [21]. There was also a trend towards more severe hypoxic injury among carriers of the ε4 allele following TBI but this did not reach statistical significance [21].
Although most studies indicate that the APOE genotype may influence outcome following TBI, there have been some negative studies failing to confirm this association. In a large prospective study involving 1094 subjects, ranging in age from 0 to 93 years, no association between APOE genotype and overall outcome was identified at 6 months following TBI [22]. In this investigation outcome was dichotomized as favorable and unfavorable using the GOS. Thirty-six percent of patients with the APOE ε4 allele had an unfavorable outcome compared with 33% of those individuals without the APOE ε4 allele. However, despite the negative findings among all ages, an interaction between age and APOE genotype on outcome was observed [22]. Younger TBI patients (15 years of age or less) possessing the APOE ε4 allele had an increased risk of an unfavorable outcome compared to younger individuals without the ε4 allele. Seventeen percent of younger patients with the allele had an unfavorable outcome compared to 6% of younger patients without the ε4 allele (odds ratio 3.06, 95% confidence ratio 1.22–7.65). No interaction between APOE genotype and injury severity on outcome was observed. Although the exact mechanism as to how APOE genotype might influence outcome in the young is unknown, a lack of an association between APOE genotype and posttraumatic brain diffuse brain swelling in young patients aged 2–19 years of age has been noted [23].
Other studies have also failed to demonstrate an association between overall outcome and APOE genotype. In a cohort of 110 African patients with traumatic cerebral contusions, 24% of 45 patients with the ε4 allele experienced an unfavorable outcome compared with 15.4% of 65 patients without the allele (P = 0.34) [24]. Of interest, the prevalence of the ε2 and ε4 alleles in this study cohort was higher than that encountered in other populations [24]. Failure to document an association between APOE genotype and TBI outcome among black Africans may reflect a differential effect of the APOE gene according to race. The majority of studies documenting an effect of APOE genotype on TBI outcome have been performed in predominantly Caucasian and Caucasian derived populations [24]. It has been postulated that variable expression APOE ε4 and its effect on TBI outcome among black Africans and Caucasians may be related to either interpopulation differences in the sequence variation underlying the APOE isoforms; the presence of other modifier genes; and/or a gene-environment interaction [24].
In agreement with the abovementioned negative findings, a long term follow-up study of 396 patients assessed on average 18 years after a TBI, revealed a lack of an association between APOE genotype and neuropsychological function [25]. Similarly, Chamelian et al. [26] found no association between APOE genotype and cognitive and behavioral outcome 6 months following mild to moderate TBI. More recently, Isonemi et al. [27] observed that the ε4 allele was not associated with the development of hippocampal or ventricular atrophy following TBI and concluded that if APOE ε4 is associated with a poorer outcome following TBI, then it is not associated with the development of brain atrophy. In support of this hypothesis, APOE ε4 did result in cell loss following TBI in a mouse model but instead was associated with amyloid deposition [28].
Evidence of an interaction between APOE genotype and TBI influencing the risk of subsequent AD has also been conflicting. Early case control studies have observed a synergistic [29] and additive [30] interaction between possession of the ε4 allele and history of prior TBI on the risk of developing AD. Mayeaux et al. [29] noted the risk of AD in individuals with both the ε4 allele and history of TBI to be 10 times that of individuals lacking the ε4 allele without a history of TBI. Katzman et al. [30] reported the risk of AD was 13.5 times higher in those cases who possessed the ε4 allele and experienced previous TBI compared to those without those risk factors. In another case control study, history of TBI and possession of the APOE ε4 allele were independent risk factors for AD without any evidence of interaction or confounding [31]. A large prospective investigation of 6645 participants aged 55 years and older were free of dementia at baseline failed to demonstrate mild head trauma as a risk factor for AD and did not observe an interaction between TBI and APOE genotype [32]. In another prospective study of World War II veterans, Plassman et al. [33] noted that moderate and severe but not mild TBI was associated with increased risk of AD and also observed a nonsignificant trend towards a stronger association between AD and TBI in men with more ε4 alleles. Although Guo et al. [34] noted a higher risk of AD among those with both TBI and the APOE ε4 allele, TBI increased the risk of AD more among those without the ε4 allele. Similarly, a retrospective autopsy study of 55 consecutive patients with residual closed TBI lesions, noted that severe TBI was associated with a higher risk of AD in those lacking the ε4 allele [35].
The variable results of the abovementioned studies assessing the influence of APOE genotype on outcome following TBI may be related to variations in study design and methodological limitations of genetic association studies. Potential selection biases can influence the homogeneity of the cases and relatively small sample sizes can lack the statistical power to identify true associations. In retrospective case control studies, the recall of a previous TBI (especially mild) may, either, be inaccurate or selective. In addition, retrospective documentation of the severity of the TBI can be difficult and is potentially influenced by the operational definition of TBI. Another confounding variable is the potential for selective mortality among ε4 patients that experience TBI compared to those without the ε4 allele. Accordingly, individuals who possess the ε4 allele and survive a TBI may not be a representative sample and their outcome may be influenced by other genetic and/or environmental factors. Since subjects may not representative of well defined homogenous populations and are often referred heterogeneous cohorts to a particular health care facility, potentially there is considerable variation in the population substructure between studies which can influence the replication of results. Another important methodological consideration is the outcome measures employed by various studies. Some studies may assess neuropsychological function while others may utilize radiological measures (e.g. cerebral atrophy, size of intracranial hematoms), clinical features (e.g. posttraumatic seizures, duration of coma), or pathological findings (e.g. amyloid deposition).
Despite the methodological limitations of genetic association studies, there is a general consensus that APOE genotype can influence TBI outcome. Although the mechanism by which APOE influences the outcome following TBI is unknown there are several established and putative neurobiological functions of APOE that may affect neurological homeostasis (Table 1). These functions are also directly or indirectly, related to the pathophysiology of AD. These include amyloid deposition, neurofibrillary tangle (NFT) formation, cholinergic transmission disruption, oxidative stress, and CNS regeneration and repair injury.
One mechanism of action is that APOE ε4 may be associated with increased amyloid deposition following TBI. APOE acts to promote and/or modulate Aβ fibril formation [36] and the absence of APOE dramatically reduces Aβ deposition [37] and limits neuritic degeneration associated with Aβ deposition [38]. In postmortem late-onset AD brains, a strong association between the presence of the ε4 allele and increased Aβ deposits compared to patients homozygous for APOE ε3 has been noted [39]. Furthermore, isoform specific differences in APOE binding or oxidation of Aβ peptide have also been observed [40]. It appears that APOE ε3 is much more effective in complexing with Aβ peptide than APOE ε4. Clinically, the presence of APOE ε4 allele promotes amyloid deposition in individuals experiencing TBI [19].
APOE genotype may play a role in neuronal cytoskeletal stability and metabolism and influence NFT formation. Transgenic mice that over-express human APOE ε4 exhibited increased hyperphosphorylation of microtubule-associated protein tau in the brain that correlated with the expression of APOE ε4 [41]. In vitro studies indicate that there are isoform-specific interactions of APOE with microtubule-associated protein tau that may regulate intraneuronal tau metabolism and the formation of paired helical filaments and NFT. APOE ε3 binds more avidly to tau forming a biomolecular complex than does APOE ε4 [42], therefore suggesting that APOE ε4 is more likely to be associated with NFT formation.
APOE may also exert an influence on cholinergic integrity and function. Gordon et al. [43] noted that APOE deficient mice exhibited markedly lower brain choline acetyltransferase activity in the hippocampus and frontal cortex. It has also been suggested that APOE ε4 allele has a direct impact on cholinergic function in AD [44]. Alzheimer patients who possess the ε4 allele exhibited a more severe cholinergic deficit than AD patients without the ε4 allele [45].
Anti-oxidant activity of APOE may play a role in mediating the neuronal maintenance and repair following TBI [46]. APOE ε4 gene increases the susceptibility of CA1 neurons to trauma and oxidative stress through excitotoxic mechanisms [47]. Postmortem examination of AD brains assessing differing antioxidant activity of APOE isoforms indicates that ε4 has the lowest antioxidant activity and ε2 has the highest antioxidant activity [48]. In AD, it has been suggested that mitochondrial/oxidative damage may be more important for cognitive function in patients that carry the ε4 allele [49]. A more recent theory hypothesizes that APOE exerts an influence on mitochondrial metabolic activity [50]. It has been noted that there is a differential effect of APOE on mitochondrial metabolic dysfunction [49].
Chen et al. [51] reported that APOE deficient mice exhibited an impaired ability to recover from TBI and postulated that APOE may play an important role in neuronal repair. Although the mechanism has not been elucidated, one may speculate that lipid transport may play a role. In the hippocampus of AD patients, APOE mRNA levels are elevated and localize to astrocytes presumed to be involved with lipid uptake where neurons are degenerating or where synaptic modeling is taking place [52]. A differential effect of APOE ε3 and ε4 on neuronal growth has been observed in dorsal root ganglion neuron cultures. APOE ε3 increased neurite outgrowth, whereas APOE ε4 decreased neuronal outgrowth [53]. In response to CNS injury, dysfunctional regulation of phospholipid and cholesterol transport by APOE ε4 during compensatory sprouting and synaptic remodeling may occur [44]. In addition, APOE has also been reported to affect hippocampal plasticity isoform specifically and influence environmental stimulation of synaptogenesis and memory [54].
Another possible mechanism on how APOE genotype may influence outcome following TBI is via neuroprotection. In transgenic mice expressing human APOE, APOE ε3 may be more neuroprotective than ε4 following TBI [55]. In response to TBI, apoE is upregulated [56] and partially protects primary neuronal-glial cultures against glutamate excititoxicity [57]. A novel 17 amino acid apoE-mimetic peptide derived from apoE residues 133–149 (the receptor binding region) may protect against CNS injury following perinatal hypoxic-ischemic injury [58] and TBI [59] in the rodent. Furthermore, this novel peptide has enhanced bioactivity compared to the intact holoprotein and protects against glutamate excititoxicity [60].
APOE promoter gene
APOE is also polymorphic in the transcriptional regulatory region, which can influence the expression of APOE [61]. There is a G/T allelic polymorphism at site −219 and an A/T allelic polymorphism at site −491 of the APOE promoter gene. A single T to G base substitution at nucleotide −219 resulted in a 169% increase in APOE promoter activity, whereas an A to T substitution at −491 site resulted in a 63% decrease in promoter activity [61]. These allelic variations in the promoter region have been postulated to influence the susceptibility to AD independent of the risk associated with APOE ε4, by influencing the expression of apoE levels [62]. The TT genotype of G-219T and the AA genotype of A-491T have been found to increase the risk of AD [62] and appear to affect the amount of Aβ deposition in the brains of patients with AD [63, 64]. Lendon et al. [65] assessed the genetic variation of the APOE promoter and 6 month outcome following TBI and noted that poorer recovery was more common among carriers of the TT polymorphism of G-219T compared to the GG and GT genotypes. No association was found with A-491T promoter polymorphisms and outcome [65].
COMT Gene
The catechol-o-methyltransferase (COMT) gene, which encodes for the enzyme that inactivates dopamine (DA) and norepinephrine (NE) exists in three isoforms: (COMT Val/Val, COMT Val/Met, and COMT Met/Met). These three functional polymorphisms differentially affect DA levels [66], which have an effect on DA associated cognitive functions [67–69]. Lipsky et al. [70] reported an association between COMT Val158Met genotype and executive functioning following TBI. Patients exhibiting the high enzyme activity polymorphism (Val/Val), and presumably lower cortical DA levels, performed worse on the Wisconsin Card Sorting Test (WCST) compared to patients with the low activity polymorphism (Met/Met) and presumably higher cortical DA levels. Similarly, Flashman et al. [71] in a study of 39 TBI patients and 27 healthy controls reported a significant effect of the Val allele being associated with poorer performance on a Continuous Performance Test (CPT) of frontal lobe function.
Dopamine D2 receptor gene
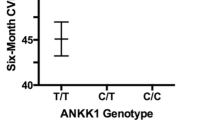
Another functionally polymorphic gene that may modulate DA function and therefore influence cognitive function is the dopamine D2 receptor gene (DRD2). One polymorphism of the DRD2 gene is a C/T single nucleotide polymorphism (SNP) at the Taq1 site. This particular polymorphism results in three isoforms (C/C, C/T, and T/T). The T allele (also known as the Taq1 A allele) is in linkage disequilibrium with a functional allelic variant that is associated with a 40% reduction in the expression of D2 receptors in the caudate of humans [72]. Although it has been speculated that the T allele is a risk factor for AD, this association has not been substantiated [73].
McAllister et al. [74] assessed the memory and attention function of 39 patients with mild TBI and 27 controls according to the presence of the T allele. Both subjects and controls who possessed the T allele performed worse on the California Verbal Learning Test (CVLT) compared to those without the T allele. Although there were no differences between the T allele positive and T allele negative groups on the CPT, individuals with the T allele and TBI exhibited slower response latencies on the CPT measures of reaction time, vigilance and distractibility compared to controls with the T allele. There were no significant differences between controls with the T allele and TBI patients without the T allele and controls without the T allele. Although these investigators noted an interaction between patients with TBI and the T allele, more compelling evidence of the T allele influencing outcome following TBI would be a significant performance difference in TBI patients compared to TBI patients without the T allele. Further study is necessary to determine the effects of the T allele on cognitive function following TBI.
Interleukin genes
At the onset of TBI, an inflammatory cascade is initiated that is in part mediated by the interleukin-1 (IL-1) system. The IL-1 family consists of three peptides (IL-1α, IL-1β, and the IL-1 receptor antagonist). Cytokines IL-1α and IL-1β are proinflammatory and are encoded, respectively, by the IL-1A and IL-1B genes [75]. The IL-1 receptor antagonist (IL-1RA), which represents a naturally occurring inhibitor of IL-1α and IL-1β, is encoded by the IL1RN gene [75]. A common polymorphism in the 5′ regulatory region of the IL-1A gene, is a C to T transition at position −889 relative to the start site of transcription, which results in 2 alleles, the IL-1A (−889) allele 1 (IL-1A*1) and the IL-1A (−889) allele 2 (IL-1A*2) [76]. Several studies have reported an association between the IL-1A* 2 polymorphisms and risk of AD [77–80]. The IL-1B gene is also polymorphic. One polymorphism of the IL-1B gene is in exon 5 at position +3953 (IL-1B + 3935). This polymorphism is bi-allelic, (IL-1B allele 1 and IL-1B allele 2) and results from an introduction on a Taq1 restriction site [72] Homozygosity for the allele 2 is associated with a fourfold increase in IL-1β production compared to the allele 1 homozygosity [81] Another polymorphism of the IL-1B gene is in the promoter region at position −511 (IL-1B-511) also resulting in IL-1B-511 allele 1 and IL-1B-511 allele 2 [82]. The IL-1RA gene has a penta-allelic polymorphic site in intron 2 containing variable number tandem repeats (VNTR) with the IL-1RA allele 2 being strongly associated with increased IL-1β secretion in vivo [83]. Associations between the IL-1B + 3935, IL-1B-511 and IL-1RA polymorphisms and the risk of Alzheimer’s disease have also been reported [78, 84].
A few studies have investigated the role of IL-1 polymorphisms and TBI outcome. Uzan et al. [85] observed an association between Il-1B gene polymorphism and outcome following TBI. In this investigation it was noted that 14 of 25 (56%) of patients with the IL-1B + 3953 allele 2 had an unfavorable outcome compared with eight of 44 (18.1%) without the IL-1B + 3953 allele 2. In addition, 20 out of 28 (71.4%) patients with the IL-1B-511 allele 2 had an unfavorable outcome compared with only 2% (2 of 41) patients without the IL-1B-511 allele 2 (P = 0.005). No association between the IL-1A gene (−889) and outcome following TBI has been observed [86]. Hadjigeorgiou et al. [87] assessed IL-1RN and IL-1B gene polymorphisms and cerebral hemorrhage following TBI. Carriers of the IL-1RN*2 were more likely to have hemorrhagic events after TBI (adjusted OR = 4.59) There was also a trend towards a lower GCS on admission among the carriers of IL-1RN*2. There were no associations between IL-1B polymorphisms and posttraumatic cerebral hemorrhagic events.
Interleukin-6 (IL-6) represents another cytokine that has been implicated in the pathophysiology of TBI. Winter et al. [88] have noted that raised levels of parenchymal IL-6 correlated with improve outcome following TBI and postulated that IL-6 is an endogenous neuroprotective cytokine that is produced in response to severe TBI. Although IL-6 concentrations are elevated in patients with brain injury, no association between IL-6 polymorphism and outcome has been observed in a mixed cohort of 62 patients with acute brain injury that included TBI and various intracranial hemorrhages [89]. However, failure to find an association could be related to the heterogenous population that was utilized.
p 53 Gene
Apoptosis has become well recognized to occur during the pathophysiological cascade following TBI [90]. The p53 gene which has been implicated as a regulator of apoptosis [91] exhibits a common polymorphism that results in either proline or arginine at amino acid 72 [92]. This functional polymorphism causes a variable induction of apoptosis with the Arg/Arg genotype more effectively performing this task [93]. Martinez et al. [94] assessed the outcome of patients with severe TBI according to the Arg72Pro polymorphism. It was noted that among patients with a poor outcome following TBI, the frequency of Arg/Arg genotype was higher (69%) compared to only 31% of patients exhibiting the Arg/Pro and Pro/Pro genotypes and that the Arg/Arg was associated with a 2.9 fold risk of experiencing a bad outcome at the time of discharge from the intensive care unit. Therefore, it has been concluded that p53 polymorphism may influence the outcome following TBI.
Angiotensin converting enzyme (ACE)
Angiotensin converting enzyme (ACE) is a component of the rennin angiotensin system, which regulates vascular homeostasis. ACE converts angiotensin I to angiotensin II, a potent vasopressor [95]. The ACE gene, which resides on chromosome 17q23 exhibits an insertion/deletion (I/D) polymorphism in intron 16 resulting in three genotypes (II, ID and DD) that influence the levels of ACE [96] with circulating levels of plasma ACE being higher among DD individuals [97]. It has been suggested that I allele may be associated with an increased risk of AD [98, 99], whereas the D allele has been associated with cognitive decline in the population [100–102] and dementia in the elderly above the age of 74 years [103].
Ariza et al. [104] assessed the influence of ACE I/D polymorphism on cognitive performance following moderate and severe TBI. These investigators observed differences in the Grooved Pegboard and part A of the Trail Making tests. Individuals that possessed the D allele performed worse on these tests of attention and processing speed than those harboring the I allele. The exact mechanism as to how ACE can influence TBI outcome is unknown. It has been postulated that it might involve cerebrovascular factors such as disturbances in cerebral blood flow and/or autoregulation of blood pressure influencing vasospasm and ischemic brain injury [104]. Another potential influence of ACE on TBI outcome may related to its ability to inhibit Aβ aggregation and the associated cytotoxicity [105].
CACNA1A gene
Indirect evidence has linked missense mutations in the CACNA1A calcium channel subunit gene to delayed cerebral edema and fatal coma following mild TBI [106]. Three patients that experienced delayed cerebral edema and coma following mild TBI exhibited a mutation in the CACNA1A gene characterized by a C to T substitution resulting in the substitution of serine for lysine at codon 218 (S218L). The possible influence of mutations of the CACNA1A gene is only speculative and to this date, larger clinical studies assessing outcome associated with genetic variations of the CACNA1A gene have not been conducted.
Concluding remarks
Several genes may influence outcome following TBI by a variety of potential mechanisms. The APOE and APOE promoter genes may influence outcome by influencing the brain’s ability to repair and/or protect against injury and may involve mechanisms similar to those involved in the pathophysiology of AD. The COMT and DRD2 genes may modulate dopamine dependent cognitive processes such as executive/frontal lobe functions that are invariable affected by TBI. The interleukin genes in part mediate inflammation, which is a prominent component in the pathophysiological cascade initiated by TBI. Apoptosis that occurs as a consequence of TBI may be modulated by polymorphisms of the p53 gene. The ACE gene may affect TBI outcome via mechanisms of cerebral blood flow and/or autoregulation and the CACNA1A gene may exert an influence via the calcium channel and its effect on delayed cerebral edema.
Of interest, several genes that may influence outcome following TBI also have been implicated as possible susceptibility genes for risk of AD. These include APOE [1–3], APOE promoter [62], DRD2 [73], IL-1 [77–80, 84] and ACE [98, 99] genes. Whether this overlap reflects common pathophysiological mechanisms that underlie both TBI and AD remains to be determined. Both TBI and AD share many common pathophysiological features [107, 108]. Although a full discussion of these similarities is beyond the scope of this review, an understanding the common mechanisms will advance our knowledge of the neuropatholophysiology of TBI and AD in hopes of achieving more effective treatment and protection.
There are several inherent complexities in the investigation of genetic influences on outcome following TBI. Firstly, TBI is a heterogeneous disorder characterized by variable clinical (e.g. mild vs. severe) and pathological (e.g. contusions vs. diffuse axonal injury) presentations. Secondly, TBI represents an extremely complex pathophysiological cascade of events that includes inflammation, oxidative stress, amyloid deposition, cholinergic dysfunction, NFT formation, apoptosis, calcium dysregulation, and excitotoxicity. In addition there are host of diverse clinical (e.g. cognitive, behavioral, neurological, and social) outcomes following TBI that can be influenced by other genetic and/or environmental factors. Furthermore, there are several methodological considerations associated genetic association studies [109] that limit the ability to replicate findings among investigations [110]. These include confounding from population substructure, small sample sizes, misclassification of outcome, selection biases and allelic heterogeneity. Accordingly, any attempt to link a gene with a specific pathophysiological occurrence that exerts influence on a specific disease or clinical outcome can be problematic.
In conclusion, many genes are associated with the pathophysiology and outcome following TBI. Microarray analysis may identify genes that are upregulated and downregulated during the neurobiological cascade induced by TBI [111]. Future studies identifying potential genes that may modulate recovery or provide neuroprotection from TBI will need to assess outcome variables specific to clinicopathological domains representative of neurobiological properties and functions of the speculated genes.
References
Corder EH, Saunders AM, Strittmatter WJ et al (1993) Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science 261:921–923
Saunders AM, Strittmatter WJ, Schmechel D et al (1993) Association of apolipoprotein E allele ε4 with late-onset familial and sporadic Alzheimer’s disease. Neurology 43:1467–1472
Strittmatter WJ, Saunders AM, Schmechel D et al (1993) Apolipoprotein E: high-avidity binding to β-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. PNAS 90:1977–1981
Teasdale GM, Nicoll JAR, Murray G et al (1997) Association of apolipoprotein E polymorphism with outcome after head injury. Lancet 350:1069–1071
Chiang MF, Chang JG, Hu CJ (2003) Association between apolipoprotein E genotype and outcome of traumatic brain injury. Acta Neurochir 145:649–654
Friedman G, Froom P, Sazbon L et al (1999) Apolipoprotein E e4 genotype predicts a poor outcome in survivors of traumatic brain injury. Neurology 52:244–248
Sorbi S, Benedetta N, Piacentini S et al (1995) ApoE as a prognostic factor for post-traumatic coma. Nature Med 1:852
Liaquat I, Dunn LT, Nicoll JAR et al (2002) Effect of apolipoprotein E genotype on hematoma volume after trauma. J Neurosurg 96:90–96
Diaz-Arrastia R, Gong Y, Fair S et al (2003) Increased risk of late posttraumatic seizures associated with the inheritance of APOE ε4 allele. Arch Neurol 60:818–822
Lichtman SW, Seliger G, Tycko B et al (2000) Apolipoprotein E and functional recovery from brain injury following postacute rehabilitation. Neurology 55:1536–1539
Teasedale TW, Jorgensen OS, Ripa C et al (2000) Apolipoprotein E and subjective symptomatology following brain injury rehabilitation. Neuropsych Rehab 10:151–166
Liberman JN, Stewart WF, Wesnes K et al (2002) Apolipoprotein E ε4 and short-term recovery from predominantly mild brain injury. Neurology 58:1038–1044
Sundstrom A, Markland P, Nilsson LG et al (2004) APOE influences on neuropsychological function after mild head injury: within-person comparisons. Neurology 62:1963–1966
Crawford FC, Vanderploeg RD, Freeman MJ et al (2002) APOE genotype influences acquisition and recall following traumatic brain injury. Neurology 58:1115–1118
Koponen S, Taiminen T, Karisto V et al (2004) APOE-ε4 predicts dementia but not other psychiatric disorders after traumatic brain injury. Neurology 63:749–750
Ariza M, Pueyo R, Matarin MD et al (2006) Influence of APOE polymorphism on cognitive and behavioural outcome in moderate and severe traumatic brain injury. J Neurol Neurosurg Psychiatry 77:1191–1193
Jordan BD, Relkin NR, Ravdin LD et al (1997) Apolipoprotein Ee4 associated with chronic traumatic brain injury in boxing. JAMA 278:136–140
Kutner KC, Ehrlanger DM, Tsai J et al (2000) Lower cognitive performance of older football players possessing apolipoprotein E ε4. Neurosurgery 47:651–658
Nicoll JAR, Roberts GW, Graham DI (1995) Apolipoprotein Ee4 allele is associated with deposition of amyloid beta protein following head injury. Nat Med 1:135–137
Leclercq PD, Graham DI, Nicoll JA et al (2002) Influence of ApoE genotype on cerebral amyloid angiopathy after closed head injury. Neuropathol Appl Neurobiol 28:161
Smith C, Graham DI, Murray L et al (2006) Association of APOE e4 and cerebrovascular pathology in traumatic brain injury. J Neurol Neurosurg Psychiatry 77:363–366
Teasdale GM, Murray GD, Nicoll JAR (2005) The association between APOE ε4, age and outcome after head injury: a prospective cohort study. Brain 128:2556–2561
Quinn TJ, Smith C, Murray L et al (2004) There is no evidence of an association in children and teenagers between the apolipoprotein E ε4 allele and post-traumatic brain swelling. Neuropath Appl Neurobiol 30:569–575
Nathoo N, Chetty R, Van Dellen JR et al (2003) apolipoprotein E polymorphism and outcome after closed traumatic brain injury: influence of ethnic and regional differences. J Neurosurg 98:302–306
Millar K, Nicoll JAR, Thornhill S et al (2003) Long term neuropsychological outcome after head injury: relation to APOE genotype. J Neurol Neurosurg Psychiatry 74:1047–1052
Chamelian L, Reis M, Feinstein A (2004) Six-month recovery from mild to moderate traumatic brain injury: the role of APOE-ε4 allele. Brain 127:2621–2628
Isoniemi H, Kurki T, Tenovuo et al (2006) Hippocampal volume, brain atrophy, and APOE genotype after traumatic brain injury. Neurology 67:756–760
Hartman KA, Laurer H, Longhi L et al (2002) Apolipoprotein E4 influences amyloid deposition but not cell loss after traumatic brain injury in a mouse model of Alzheimer’s disease. J Neurosci 22:10083–10087
Mayeux R, Ottman R, Maestre G et al (1995) Synergistic effects of traumatic head injury and apolipoprotein −ε4 in patients with Alzheimer’s disease. Neurology 45:555–557
Katzman R, Galosko DR, Saitoh T et al (1996) Apolipoprotein e4 and head trauma: synergistic or additive risks? Neurology 46:889–892
O’Meara ES, Kukull WA, Sheppard L et al (1997) Head injury and risk of Alzheimer’s disease by apolipoprotein E genotype. Am J Epidemiol 146:373–384
Mehta KM, Ott A, Kalmijn S et al (1999) Head trauma and risk of dementia and Alzheimer’s disease: the rotterdam study. Neurology 53:1959–1962
Plassman BL, Havlik RJ, Steffens DC et al (2000) Documented head injury in early adulthood and risk of Alzheimer’s disease and other dementias. Neurology 55:1158–1166
Guo Z, Cupples LA, Kurz A et al (2000) Head injury and the risk of AD in the MIRAGE study. Neurology 54:1316–1323
Jellinger KA, Paulus W, Wrocklage C et al (2001) Effects of closed traumatic brain injury and genetic factors on the development of Alzheimer’s disease. Eur J Neurology 8:707–710
Wisniewski T, Castano EM, Golabek et al (1994) Acceleration of Alzheimer’s fibril formation by apolipoprotein E in vitro. Am J Pathol 145:1030–1035
Bales KR, Verina T, Dodel RC et al (1997) Lack of apolipoprotein E dramatically reduces amyloid β-peptide deposition. Nat Genet 17:254–256
Holzman DM, Fagan AM, Mackey B et al (2000) Apolipoprotein E facilitates neuritic and cerebrovascular plaque formation in an Alzheimer’s disease model. Ann Neurol 47:739–747
Schmechel DE, Saunders AM, Strittmatter WJ et al (1993) Increased amyloid β-peptide deposition in cerebral cortex as consequence of apolipoprotein E genotype in late-onset Alzheimer disease. PNAS 90:9649–9653
Strittmatter WJ, Weisgraber KH, Huang DY et al (1993) Binding of human apolipoprotein E to synthetic amyloid β peptide: isoform-specific effects and implications for late-onset Alzheimer disease. PNAS 90:8098–8102
Tesseur I, Van Dorpe J, Spittaels K et al (2000) Expression of human apolipoprotein E4 in neurons causes hyperphosphorylation of protein tau in the brains of transgenic mice. Am J Pathol 156:951–964
Strittmatter WJ, Saunders AM, Goedert M et al (1994) Isoform-specific interactions of apolipoprotein E with microtubule-associated protein tau: implications for Alzheimer disease. PNAS 91:11183–11186
Gordon I, Grauer E, Genis I et al (1995) Memory deficits and cholinergic impairments in apolipoprotein E-deficient mice. Neurosci Lett 199:1–4
Poirer J (1996) Apolipoprotein E in the brain and its role in Alzheimer’s disease. J Psychiat Neurosci 21:128–134
Soininen H, Kosunen O, Helisalmi et al (1995) A severe loss of choline acetyltransferase in the frontal cortex of Alzheimer patients carrying apolipoprotein ε4 allele. Neurosci Lett 187:79–82
Lomnitski L, Chapman S, Hochman A et al (1999) Antioxidant mechanisms in apolipoprotein E deficient mice prior to and following closed head injury. Biochim Biophys Acta 1453:359–368
Wallis RA, Panizzon KL, Teter B et al (1999) Protection with MK-801 against susceptibility of mice expressing human apolipoprotein E4 to CA1 neuronal injury from trauma and oxidative stress. J Neurotrauma 16:986
Tamaoka A, Miyatake F, Matsuno S et al (2000) Apolipoprotein E allele dependent antioxidant activity in brains with Alzheimer’s disease. Neurology 54:2319–2321
Gibson GE, Haroutunian V, Zhang H et al (2000) Mitochondrial damage in Alzheimer’s disease varies with apolipoprotein E genotype. Ann Neurol 48:297–303
Roses AD, Saunders AM (2006) Perspective on a pathogenesis and treatment of Alzheimer’s disease. Alzheimer’s Dementia 2:59–70
Chen Y, Lomnitski L, Michaelson DM et al (1997) Motor and cognitive deficits in apolipoprotein E deficient mice after closed head injury. Neuroscience 80:1255–1262
Zarow C, Victoroff J (1998) Increased apolipoprotein E mRNA in the hippocampus in Alzheimer disease and in rats after entorhinal cortex lesioning. Exp Neurol 149:79–86
Nathan BP, Bellosta S, Sanan DA et al (1994) Differential effects of apolipoprotein E3 and E4 on neuronal growth in vitro. Science 264:850–852
Levi O, Jongen-Relo AL, Feldon J et al (2003) ApoE4 impairs hippocampal plasticity isoform-specifically and blocks the environmental stimulation of synaptogenesis and memory. Neurobiol Dis 13:273–282
Sabo T, Lomnitski L, Nyska A et al (2000) Susceptibility of transgenic mice expressing human apolipoprotein E to closed head injury: the allele E3 is neuroprotective whereas E4 increases fatality. Neuroscience 101:879–884
Iwata A, Browne KD, Chen XH et al (2005) Traumatic brain injury induces biphasic upregulation of ApoE and ApoJ protein in rats. J Neurosci Res 82:103–114
Aono M, Lee Y, Grant ER et al (2002) Apolipoprotein E protects against NMDA excitotoxicity. Neurobiol Dis 11:214–220
McAdoo JD, Warner DS, Goldberg RN et al (2005) Intrathecal administration of a novel apoE-derived therapeutic peptide improves outcome following perinatal hypoxic-ischemic injury. Neurosci Lett 381:305–308
Lynch JR, Wang H, Mace B et al (2005) A novel therapeutic derived from apolipoprotein E reduces brain inflammation and improves outcome after closed head injury. Exp Neurology 192:109–116
Aono M, Bennett ER, Kim KS et al (2003) Protective effect of apolipoprotein E-mimetic peptides on N-methyl-D-aspartate excitotoxicity in primary rat neuronal-glial cell cultures. Neuroscience 116:437–445
Artiga MJ, Bullido MJ, Sastre I et al (1998) Allelic polymorphisms in the transcriptional regulatory region of apolipoprotein E gene. FEBS Lett 421:105–108
Lambert JC, Araria-Goumidi L, Myllykangas L et al (2002) Contribution of APOE promoter polymorphisms to Alzheimer’s disease risk. Neurology 59:59–66
Lambert JC, Mann D, Goumidi L et al (2001) Effect of the APOE promoter polymorphisms on cerebral amyloid deposition in Alzheimer’s disease. Lancet 357:608–609
Lambert JC, Mann D, Richard F et al (2005) Is there a relation between APOE expression and brain amyloid load in Alzheimer’s disease. J Neurol Neurosurg Psychiatry 76:928–933
Lendon CL, Harris JM, Pritchard AL et al (2003) Genetic variation of the APOE promoter and outcome after head injury. Neurology 61:683–685
Weinshilboum RM, Otterness DM, Szumlanski CL (1999) Methylation pharmacogenetics: catechol O-metyltransferase, thiopurine methyltransferase, and histamine N-methyltransferase. Annu Rev Pharmacol Tox 39:19–52
Akil M, Kolachana BS, Rothmond DA et al (2003) Catechol-O-methyltransferase genotype and dopamine regulation in the human brain. J Neurosci 23:2008–2013
Diaz-Asper CM, Weinberger DR, Goldberg TE (2006) Catechol-O-methyltransferase polymorphisms and some implications for cognitive therapeutics. NeuroRx 23:97–105
Malhorta AK, Kestler LJ, Mazzanti C et al (2002) A functional polymorphism in the COMT gene and performance on a test of prefrontal function. Am J Psychiatry 159:652–654
Lipsky RH, Sparling MB, Ryan LM et al (2005) Association of COMT Val158Met genotype with executive functioning following traumatic brain injury. J Neuropsychiatry Clin Neurosci 17:465–471
Flashman LA, Saykin AJ, Rhodes CH et al (2004) Effect of COMT Val/Met genotype on frontal lobe functioning in traumatic brain injury. J Neuorpschiatry Clin Neurosci 16:238–239
Ritchie T, Noble EP (2003) Association of seven polymorphisms of the D2 dopamine receptor gene with brain receptor-binding characteristics. Neurochem Res 28:73–82
Small GW, Noble EP, Matsuyama SS et al (1997) D2 dopamine receptor A1 allele in Alzheimer disease and aging. Arch Neurol 54:281–285
McAllister TW, Rhodes CH, Flashman LA et al (2005) Effect of dopamine D2 receptor T allele on response latency after mild traumatic brain injury. Am J Psychiatry 162:1749–1751
Nicklin MJ, Weith A, Duff GW (1994) A physical map of the region encompassing the human interleukin-1 alpha, interleukin-1 beta, and interleukin-1receptor agonist genes. Genomics 19:382–384
Murzin AG, Lesk AM (1992) Beta-Trefoil fold. Patterns of structure and sequence in the Kunitz inhibitors interleukins-1beta and 1 alpha and fibroblast growth factors. J Mol Biol 223:531–543
Grimaldi LME, Casedei VM, Veglia F et al (2000) Association of early-onset Alzheimer’s disease with an interleukin-1α gene polymorphism. Ann Neurol 47:361–365
Nicoll JA, Mrak RE, Graham DI et al (2000) Association of interleukin-1gene polymorphisms with Alzheimer’s disease. Ann Neurol 47:365–368
Du Y, Dodel RC, Eastwood BJ et al (2000) Association of an interleukin 1α polymorphism with Alzheimer’s disease. Neurology 55:480–483
Rainero I, Bo M, Ferrero M et al (2004) Association between the interleukin gene and Alzheimer’s disease: a meta-analysis. Neurobiol Aging 25:1293–1298
Pociot F, Moivig J, Wogensen L et al (1992) A taq1 polymorphism in the human interleukin-1 beta (IL-1 beta) gene correlates with IL-1 beta secretion in vitro. Eur J Clin Invest 22:396–402
di Giovine FS, Takhsh E, Blakemore AI, Duff GW (1992) Single base polymorphism at −511 in the human interleukin-1 beta gene (IL-1 beta). Hum Mol Genet 1:450
Santilla S, Savinainen K, Hurme M (1998) Presence of the IL-1RA allele 2 (IL1rn*2) is associated with enhanced IL-1beta production in vitro. Scand J Immunol 47:195–198
Yucesoy B, Peila R, White LR et al (2006) Association of interleukin-1 gene polymorphisms with dementia in a community-based sample: the Honolulu-Asia aging study. Neurobiol Aging 27:211–217
Uzan M, Tanriverdi T, Baykara et al (2005) Association between interleukin-1beta (IL-1β) gene polymorphism and outcome after head injury: an early report. Acta Neurochir 147:715–720
Tanriverdi T, Uzan M, Sanus GZ et al (2006) Lack of an association between the IL1A gene (−889) polymorphism and outcome after head injury. Surg Neurol 65:7–10
Hadjigeorgiou GM, Paterakis K, Dardiotis E et al (2005) IL-1RN and IL-1B gene polymorphisms and cerebral hemorrhagic events after traumatic brain injury. Neurology 65:1077–1082
Winter CD, Pringle AK, Clough GF et al (2004) Raised parenchymal interleukin-6 levels correlate with improved outcome after traumatic brain injury. Brain 127:315–320
Minambres E, Cemborian A, Sanchez-Velasco P et al (2003) Correlation between transcranial interleukin-6 gradient and outcome inpatients with acute brain injury. Crit Care Med 31:933–938
Raghupathi R, Graham DI, McIntosh TK (2000) Apoptosis after traumatic brain injury. J neurotrauma 17:927–938
Fisher DE (2001) The p53 tumor suppressor: critical regulator of life & death in cancer. Apoptosis 6:7–15
Ara S, Lee PSY, Hansen MF, Saya H (1990) Codon 72 polymorphism of the TP53 gene. Nucleic Acids Res 18:4961
Dumont P, Leu JI, Della Pietra AC et al (2003) The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet 33:357–365
Martinez-Lucas P, Moreno-Cuesta J, Sanchez-Sanchez F et al (2005) Relationship between the Arg72Pro polymorphism of p53 and outcome for patients with traumatic brain injury. Intensive Care Med 31:1168–1173
Erdos EG, Skidgel RA (1987) The angiotensin I converting enzyme. Lab Invest 56:345–348
Rigat B, Hubert C, Alhenc-Geias F et al (1990) An insertion/deletion polymorphism in the angiotensin I-converting enzyme gen accounting for half the variance of serum enzyme levels. J Clin Invest 86:1343–1346
Tiret L, Rigat B, Visvikis S et al (1992) Evidence from combined segregation and linkage analysis, that a variant of the angiotensin I-converting enzyme (ACE) gene controls plasma ACE levels. Am J Hum Genet 51:197–205
Narain Y, Yip A, Murphy T et al (2000) The ACE gene and Alzheimer’s disease susceptibility. J Med Genet 37:695–697
Elkins JS, Douglas VC, Johnston SC (2004) Alzheimer disease risk and genetic variation in ACE. Neurology 62:363–368
Amouyel P, Richard F, Cottel D et al (1996) The deletion allele of the angiotensin I converting enzyme gene as a genetic susceptibility factor for cognitive impairment. Neurosci Lett 217:203–205
Richard F, Berr C, Amant C et al (2000) Effect of the angiotensin I-converting enzyme I/D polymorphism on cognitive decline. The EVA study group. Neurobiol Aging 21:75–80
Stewart R, Powell J, Prince M, Mann A (2004) ACE genotype and cognitive decline in an African-Caribbean population. Neurobiol Aging 25:1369–1375
Richard F, Fromentin-David I, Ricolfi F et al (2001) The angiotensin I converting enzyme gene as a susceptibility factor for dementia. Neurology 56:1593–1595
Ariza M, Matarin MD, Jungue C et al (2006) Influence of the angiotensin-converting enzyme polymorphism on neuropsychological subacute performance in moderate and severe traumatic brain injury. J Neuropschiatry Clin Neurosci 18:39–44
Hu J, Igarashi A, Kamata M et al (2001) Angiotensin-converting enzyme degrades Alzheimer amyloid β-peptide (Aβ); Retards Aβ aggregation, deposition, fibril formation: and inhibits cytotoxicity. J Biol Chem 278:47863–47868
Kors EE, Terwindt GM, Vermeulen FL et al (2001) Delayed cerebral edema and fatal coma after minor head trauma: role of the CACNA1A calcium channel subunit gene and relationship with familial hemiplegic migraine. Ann Neurol 49:753–760
Nicoll JAR, Roberts GW, Graham DI (1996) Amyloid β-protein, APOE genotype and head injury. Ann NY Acad Sci 777:271–275
Jordan BD (2000) Chronic traumatic brain injury associated with boxing. Sem Neurology 20:179–185
Colhoun HM, McKeigue PM, Smith GD (2003) Problems of reporting genetic associations with complex outcomes. Lancet 361:865–872
Ioannidis JPA, Ntzani EE, Trikalinos TA et al (2001) Replication validity of genetic association studies. Nat Genetics 29:306–309
Yoshiya K, Tanake H, Kasai K et al (2003) Profile of gene expression in the subventricular zone after traumatic brain injury. J Neurotrauma 20:1147–1162
Author information
Authors and Affiliations
Corresponding author
Additional information
Special issue dedicated to John P. Blass.
Rights and permissions
About this article
Cite this article
Jordan, B.D. Genetic Influences on Outcome Following Traumatic Brain Injury. Neurochem Res 32, 905–915 (2007). https://doi.org/10.1007/s11064-006-9251-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-006-9251-3