Abstract
Purpose of Review
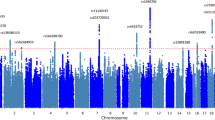
Traumatic brain injury (TBI) has a significant burden of disease worldwide and outcomes vary widely. Current prognostic tools fail to fully account for this variability despite incorporating clinical, radiographic, and biochemical data. This variance could possibly be explained by genotypic differences in the patient population. In this review, we explore single nucleotide polymorphism (SNP) TBI outcome association studies.
Recent Findings
In recent years, SNP association studies in TBI have focused on global, neurocognitive/neuropsychiatric, and physiologic outcomes. While the APOE gene has been the most extensively studied, other genes associated with neural repair, cell death, the blood-brain barrier, cerebral edema, neurotransmitters, mitochondria, and inflammatory cytokines have all been examined for their association with various outcomes following TBI. The results have been mixed across studies and even within genes.
Summary
SNP association studies provide insight into mechanisms by which outcomes may vary following TBI. Their individual clinical utility, however, is often limited by small sample sizes and poor reproducibility. In the future, they may serve as hypothesis generating for future therapeutic targets
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic brain injury (TBI) is a condition with a major global burden of disease with significant variance in outcomes [1]. The International Mission for Prognosis and Analysis of Clinical Trials in TBI (IMPACT) and Corticoid Randomization After Significant Head injury (CRASH) prognostic models have been developed to prognosticate utilizing known variables such as age, presenting Glasgow Coma Scale (GCS), pupil reactivity, and various CT and laboratory findings. Even with all of these initial parameters as inputs, the predictive ability of these models is incomplete with areas under the receiver operator curve as low as between 0.65 and 0.71 in some datasets [2].
These predictive models all focus mainly on characteristics of the initial insult and fail to account for the burden of ongoing secondary insult. The modification of secondary insult to improve outcomes is the goal of neurocritical and neurosurgical care; however, a growing body of evidence supports that certain genetic factors may impact outcomes following TBI. In this paper, we take an outcomes-based approach to reviewing recent literature on the implications of genetics on TBI. We will explore recent developments on global, neuropsychiatric, and physiologic outcomes and their association with single nucleotide genetic polymorphisms (SNPs) in TBI populations.
Global Outcomes
In this section, we explore the relationship between various SNPs and global patient outcomes following TBI. Often, these are measured utilizing the Glasgow Outcome Scale (GOS) or extended GOS (GOSE). These findings are summarized in Table 1.
Apolipoprotein E
The most extensively studied polymorphism in relation to outcomes following TBI is the APOE gene which codes for apolipoprotein E, a protein that plays a central role in central nervous system lipid transport and neural repair. Three common alleles of the APOE gene have been identified, ε2, 3, and 4, which code for protein isoforms E2, E3, and E4 respectively. Outside of TBI literature, the ε4 allele has been associated with a variety of negative neuropsychiatric outcomes including an increased risk of late-onset Alzheimer’s disease.[30]
The connection between the ε4 allele of APOE and global outcomes was first identified by Teasdale et al. in the 1997 study of 93 head injury patients admitted to a neurosurgical unit. The endpoint of an unfavorable outcome at 6 months post-injury, as defined as a GOS of 1–3 (i.e., dead, vegetative state, or severe disability), was found to be significantly more common in those with an APOE ε4 allele (57% vs 27%, p = 0.006). This significant difference persisted even when age, GCS, and CT finding at presentation were accounted for (p = 0.024) [3].
Since this original landmark paper, numerous studies have looked to evaluate the association between the APOE ε4 allele and poor outcomes following TBI. There have been four independent meta-analyses that have looked to summarize this body of literature, two of which were in the last 5 years [4,5,6,7]. In 2008, Zhou et al. published a meta-analysis of 14 cohort studies including 2527 patients and found that while possession of an APOE ε4 allele was not associated with initial injury severity it was significantly associated with poor outcomes (GOS of 1–3 or GOSE of 1–4) at 6 months after injury (RR = 1.36; 95% CI, 1.04–1.78) [4]. This work was expanded on in 2014 by Zeng et al. in a meta-analysis of 13 cohort studies with 2276 TBI patients which found that APOE ε4 allele was associated with a poor prognosis (OR = 0.68: 95%CI 0.48–0.96; p = 0.027). Furthermore, subgroup analysis found that this association was present in those with severe TBI (OR= 0.43; 95%CI 0.21–0.87; p = 0.020) but not those with mild or moderate TBI (p > 0.05) [5].
Most recently, McFadyen et al. published in 2019 a meta-analysis of 14 studies and 2 cohorts of unpublished data totaling 2593 subjects and found a higher likelihood of a favorable outcome following TBI in those not possessing an APOE ε4 allele as compared with homozygotes and carriers (OR = 1.39; 95%CI 1.05–1.84; p = 0.02). In this study, no subgroup analysis was done to examine the effect on severe, moderate, and mild TBI separately [6•].
In 2016, Kassam et al. published a meta-analysis of 6 studies encompassing 358 cases of pediatric (3 to 18 years of age) TBI examining the relationship of possessing an APOE ε4 allele and poor outcome (GOS score 1–3 or GOSE score 1–4). They found a significantly higher probability of a poor outcome at 6 months post-injury for those with an APOE ε4 allele (OR = 2.36; 95%CI 1.26–4.42; p = 0.007) [7].
These publications seem to point to a strong association between poor outcomes following TBI and the APOE ε4 allele. The prevailing belief is that the neurochemical mechanism for the toxic effect of the APOE ε4 allele is a result of the change in tertiary structure of the apolipoprotein E secondary to an amino acid substitution found in the E4 variant. This altered tertiary structure results in abnormal lysing of the protein in the endoplasmic reticulum with subsequent release of neurotoxic by-products that impair mitochondrial and cytoskeletal function [6•]. There is however data indicating that this may not be true over all ethnicities. Zeng et al. reported in a subgroup analysis of their meta-analysis that the association was significant in Asian populations (OR = 0.46; 95%CI 0.21–0.99; p = 0.046), but not in Caucasian populations (OR = 0.75; 95%CI 0.53–1.08; p = 0.120) [5]. Furthermore, in a 2015 study of 150 Kashmiri TBI patients, Yousuf et al. reported no association between the presence of a APOE ε4 allele and unfavorable outcomes (p = 0.92) [8].
Neural Repair and Cell Death–Associated Polymorphisms
Following TBI neural repair and apoptotic pathways are thought to play a pivotal role in recovery. One neurotropic factor that has been linked to neurogenesis and neuronal survival is brain-derived neurotropic factor (BDNF) [31]. Three studies have examined the association of various polymorphisms of BDNF gene and global outcomes following TBI [9,10,11].
Failla et al. reported in 2015 a study of 315 patients receiving care for closed head injuries. SNPs of the BDNF gene rs6265 (Val66Met) and rs7124442 (T>C) were evaluated for their association with mortality in the acute period (0–7 days) vs the post-acute period (8–365 days) post-injury. Individuals that were less than 45 years old being homozygous for rs6265 Val and rs71244 T had the highest probability of survival in the post-acute period [9]. This may point to an age-related interaction with the ability of BDNF gene polymorphism’s ability to predict mortality following TBI. In 2016, Failla et al. expanded on this work and found that these BDNF gene polymorphisms interact with serum BDNF levels to predict mortality through multi-variate modeling (HR = 0.987; p = 0.047) [10]. Munoz et al. built on this work by examining the interaction CSF cortisol levels have with these polymorphisms in predicting mortality following TBI. They found that models that incorporated CSF cortisol and these BDNF gene SNPs were able to predict mortality in those less than 48 years of age (p = 0.0004). While the pathway is far from clear, these studies point to prognostic value in BDNF gene polymorphisms rs6265 and rs71244 when combined with CSF cortisol and serum BDNF levels in younger patients.
Neural repair and apoptotic pathways often produce by-products that have been examined as biomarkers in TBI [32]. Polymorphisms in genes encoding for TBI biomarkers have been examined for their utility at predicating global outcomes following TBI. In a study of 305 severe TBI patients, Osier et al. examined 18 SNPs in biomarker-encoding genes. The primary endpoint was GOS at 3, 6, 12, and 24 months. One SNP of the gene encoding for S100 calcium-binding protein B (S100B), rs1051169 (G>C), was associated with higher scores on the GOS at 3 months (OR = 0.39; p = 0.04), 6 months (OR = 0.34; p = 0.02), 12 months (OR = 0.32; p = 0.02), and 24 months (OR = 0.30; p = 0.02). Multiple SNPs in genes encoding for glial fibrillary acid protein (GFAP) and ubiquitin C-terminal hydrolase L1 (UCHL1) were not found to be associated with global outcomes following TBI [12].
Neuronal apoptosis following TBI is a well-known phenomenon and is mediated by TP53 gene located on chromosome 17q13.1 that codes for p53 protein [13]. The Arg/Arg homozygous form of the rs1042522 (Arg72Pro) SNP of the TP53 gene is at least 5 times more efficient at inducing apoptosis than the other variants [33]. This prompted Mellett et al. to study its association with global outcomes in 429 patients with severe TBI. Patients with the homozygous arginine genotype had worse outcomes at 24 months by GOS (p = 0.048) and Disability Rating Scale (DRS, p = 0.022) [13].
Blood-Brain Barrier– and Cerebral Edema–Associated Polymorphisms
The blood-brain barrier (BBB) integrity has been speculated to contribute to various CNS pathologies and recently its role in recovery following TBI has been explored. ATP-binding cassette (ABC) transporters are the main proteins responsible for regulating transport across the BBB. Genetic polymorphisms in genes that code for this family of transport proteins have been examined recently to see if they are associated with global outcomes following TBI [14,15,16]. The ABCB1 gene SNPs were examined by Wang et al. in 2015. In their cohort of 182 TBI patients, the 6-month GOS was found to be associated with the ABCB1 gene polymorphism rs1045642 (C3435T) with the T homozygous genotype associated with a worse outcome as compared to other variants (OR = 2.71; 95% CI = 1.12–6.86) [14].
The ABCG2 transporter is one of the primary CNS efflux transporters and was the subject of a study by Adam et al. in 2018. GOS scores were obtained at 3, 6, 12, and 24 months following severe TBI for 436 patients. The rs2231142 (C421A) polymorphism, a common missense polymorphism that results in decreased protein expression, was identified for all patients. They found that patients that had at least one variant (A) allele had significantly improved odds of having a higher GOS score at all time points so long as age was less than 34. This did not hold true for patients over the age of 34 [15]. This points to a possible age-dependent association with prognosis following severe TBI.
In a study conducted by Jha et al. in 2018, 410 severe TBI patients were examined for an association with GOS at 3 months post-injury and 15 SNPs in the gene coding for the ABCC8 transporter protein. Three SNPs were found to be associated with GOS at 3 months. The homozygous T genotype of the rs2237982(C>T) SNP decreased odds of a favorable outcome (OR = 0.43; p = 0.010) and concordantly presence of a C allele increased odds of a favorable outcome (OR = 2.45; p = 0.006). Rs11024286 (G>A) heterozygotes had increased odds of favorable outcome (OR = 2.57; p = 0.000) versus those homozygous for the G allele. Additionally, the A allele was an independent predictor of a favorable outcome (OR = 2.40; p = 0.000). Finally in the rs4148622 (G>A) SNP, possessing a G allele decreased odds of a favorable outcome (OR = 0.40; p = 0.01) [16••].
Mitochondrial-Associated Polymorphisms
Mitochondrial dysfunction following TBI has been observed in animal studies and associated alterations in energy metabolism following injury have also been observed [34, 35]. It has been hypothesized that variations in mitochondrial function following injury may be genetically based. The role of mitochondrial-associated polymorphisms in TBI outcomes has been examined in three studies [17,18,19]. The B cell lymphoma 2 (BCL2) protein is a proto-oncogene that prevents apoptosis and is reassessed during mitochondrial damage and plays a role as a cell survival promoter [36]. Hoh et al. examined polymorphisms of the BCL2 gene in 205 patients with severe TBI. Global outcomes were measured for all patients at 3, 6, 12, and 24 months. While multiple SNPs were examined, the only polymorphism association that remained significant with Bonferroni correction was rs17759659 (A>G) where the presence of the variant allele was associated with poorer outcomes by GOS (p = 0.001) and higher mortality (OR = 4.23; 95%CI 1.31–13.61; p = 0.02) [17].
In 2014, Bulstrode et al. analyzed the mitochondrial DNA (mtDNA) of 1094 TBI patients and identified that those with haplogroup K had an association with favorable outcomes by 6-month GOS (OR = 1.64; 95%CI 1.08–2.51; p = 0.02). In the same year, Conley et al. examined the roles of mtDNA polymorphisms 1 year after severe TBI in 136 patients and found that the A10398G SNP was associated with DRS at 6 and 12 months (p = 0.02) with the A allele associated with slower recovery.
Neurotransmitter-Associated Polymorphisms
Gene polymorphisms in those that code for proteins in neurotransmitter pathways have been examined for their association with global outcomes following TBI. One such protein is catechol-O-methyltransferase (COMT) which is an enzyme that is intricately involved in the degradation of dopamine. In 2014, a report by Willmott et al. of 223 patients with moderate to severe TBI found that the SNP rs4680 (Val158Met) on the COMT gene was not associated with outcomes at 12 and 24 months post injury as defined by the GOSE [20]. Contrary to this, Winkler et al. reported an association with the rs4680 Met allele and higher GOSE scores following moderate TBI in 93 patients 6 months post-injury (OR = 2.87; 95%CI 1.20–6.86; p < 0.05). However, this association failed to reach significance when accounting for comorbid post-traumatic stress disorder (PTSD) by multivariable analysis [21].
Failla et al. studied SNPs in the neurotransmitter-associated genes dopamine D2 receptor (DRD2) and ankyrin repeat and kinase domain (ANKK1). In 108 severe TBI patients, when adjusting for age, GCS, and education, the DRD2 rs6279 (C>G) (p = 0.0430) and ANKK1 rs1800497 (C>T) (p = 0.0468) SNPs had an association with improved outcomes at 6 months when the variant allele was present. This association failed to meet significance under multiple comparisons correction [22].
Inflammatory Cytokine–Associated Polymorphisms
Following TBI, a series of inflammatory cascades are initiated with many of these associated with secondary injury. Neuroinflammatory cytokines in cerebral spinal fluid following acute brain injury have been found to be associated with global outcomes and their use as biomarkers following TBI has been facilitated by cerebral microdialysis [37, 38]. This spurred work in the early 2000s to examine the associations with SNPs in genes coding for inflammatory cytokines and global outcomes following brain injury. Early work mostly found SNPs in interleukin (IL) 1α and IL-6 genes not to be associated with outcomes following brain injury [23, 24, 26]. There were, however, studies that produced positive results with Uzan et al. finding an association with two IL-1β SNPs and GOS 6 months following TBI in 69 patients [25].
The past decade has seen similarly mixed results. A 2011 study by Dalla Libera et al. reexamined the IL-6 gene SNP rs1800795 (G>C), which is associated with levels of IL-6. Here, 77 male patients were monitored following severe TBI. The G homozygous genotype was found more frequently in patients who survived than those who did not (67% vs 41%; p < 0.05) and those G allele carriers were also found more frequently in the survivor group than in the non-survivor group (81% vs 65%; OR = 2.39; 95%CI 1.07–5.36; p = 0.031) [27]. Counter to this, a much larger study of 1096 TBI patients failed to associate the IL-6 gene SNP rs1800795 with GOS at 6 months. In fact, of the 11 SNPs screened for in IL-1α, IL-1β, IL-6, tumor necrosis factor-α (TNF-α), and transforming growth factor-β (TGF-β) genes, only the TNF-α SNP rs1800629 (G>A) was found to have an association with the variant allele being associated with unfavorable global outcomes (39% vs 31%; OR = 1.67; 95%CI 1.19–2.35; p = 0.003) [28•].
The lectin pathway is a less commonly known pro-inflammatory pathway. Most recently, a study of 44 patients with severe TBI failed to find an association with eight SNPs in genes coding for lectin pathway proteins and mortality or consciousness at 14 days. A favorable GOS at 90 days was also not found to be associated with any of the eight SNPs [29].
Neuropsychiatric and Neurocognitive Outcomes
In recent years, SNP association studies in TBI have turned their attention to neuropsychiatric and neurocognitive outcomes. These studies are often plagued with heterogeneity as, unlike with global outcomes, numerous tests are available to analyze various neuropsychiatric and neurocognitive domains. These findings are summarized in Table 2.
Apolipoprotein E
As discussed previously, APOE has become the quintessential gene for association studies of global outcomes following TBI. More recently, its association with neuropsychiatric and neurocognitive outcomes following TBI has been explored. This can be traced back to a study done in 2007 by Han et al. wherein 78 mild to moderate TBI patients the APOE ε4 allele was actually found to be associated with marginal but statistically significant improved outcomes in certain neuropsychologic outcomes. A trend that was independent of TBI severity [39].
While the study by Han et al. seemed to infer a protective neuropsychiatric affect following TBI, subsequent research has not demonstrated this positive association with the ε4 allele. In a study of 42 college athletes that sustained mild TBI, Merritt et al. reported that those with a ε4 allele had significantly worse self-reported symptomatology at 3 months post injury as determined by the Post-Concussion Symptom Scale (PCSS, p < 0.05). When broken down into the domains of physical, cognitive, affective, and sleep symptoms, significantly worse outcomes were found in the physical (p < 0.01) and cognitive (p < 0.05) domains [40]. Further to this, 6-month verbal memory outcomes were found to be worse in ε4 carriers by Yue et al. in a cohort of 114 mild TBI patients from the Transforming Research and Clinical Knowledge in TBI Pilot (TRACK-TBI Pilot) study [41]. The APOE ε4 allele was also found to be associated with worse neuropsychiatric outcomes following mild to moderate TBI in a military population with worse score in the Beck Depression Inventory-II (BDI-II; p = 0.008) and Beck Anxiety Inventory (BAI; p = 0.020) [42]. A similar study of 53 military veterans with mild TBI showed that the ε4 allele was associated with worse memory and processing speed as well as overall cognitive impairment (p < 0.05) [43].
To confuse matters further, a number of studies have failed to find any association with APOE ε4 allele status and neuropsychiatric and neurocognitive outcomes post-TBI. Padgett et al. studied 170 TBI patients for an effect of APOE genotype on information processing, executive function, and working memory following injury but failed to find an association [44]. In 2017, Banks et al. did not find any association between cognitive outcomes and APOE ε4 status in a cohort of professional fighters [45]. Finally, in a study of 57 college athletes having sustained a concussion, no significant difference was found between those with and without an ε4 allele in neurocognitive standardized scores (p > 0.05) [56].
Neural Repair and Cell Death–Associated Polymorphisms
The significant role that BDNF has on neural plasticity, survival, and growth has made the BDNF gene a key target in the search for SNPs associated with neuropsychiatric and neurocognitive outcomes. The rs6265 (Val66Met) SNP has garnered particular attention due to its effect on the secretion and neuroplastic effect of BDNF [57]. An early study done by Krueger et al. in Vietnam combat veterans with frontal lobe lesions attributable to penetrating TBI revealed that the variant allele was associated with improved recovery of executive function [46]. A follow-up work done by the same group in the same cohort of patients found that while the Met allele carriers did not differ from the Val homozygotes in general cognitive ability before injury, following injury there was a significant difference in general intelligence, verbal comprehension, perceptual organization, working memory, and processing speed with the Val homozygotes having worse outcomes [47]. A work done by McAllister et al. in a population of 75 patients with mild TBI contradicted these results with the Val allele being associated with better processing speed following injury [48].
Bagnato et al. hypothesized that since emergence from a vegetative state (VS) after a TBI implies that the brain undergoes plastic changes and BDNF is involved in neuroplasticity, perhaps there is a connection between the rs6265 SNP and recovery from VS. They examined 53 patients in VS 1 month following TBI and scored cognitive function at 1, 3, 6, and 12 months post-TBI but found no association with the Met allele of rs6265 and recovery of consciousness and cognitive functions [49].
More recent studies seem to point to worse neurocognitive and neuropsychiatric outcomes following TBI in Met allele carriers. Narayanan et al. examined cognition in 48 mild TBI patients at admission and at 6-month follow-up and found that those with the Met allele had lower scores in cognitive testing in most domains at admission that remained impaired at 6 months post-injury [50]. In a study by Wang et al., the Beck Anxiety Inventory (BAI) and Beck Depression Inventory (BDI) scores for 192 minor TBI patients were determined in the first and sixth weeks following injury. They found that in male patients, the Met allele had higher scores of both BAI and BDI in the first and sixth weeks [51].
Neurotransmitter-Associated Polymorphisms
Dopamine systems, especially those involved in the prefrontal cortex, influence executive function, memory consolidation, verbal language skills, and attention. All of these significantly impact neurocognitive outcomes. It is no wonder then that SNPs in genes that code for proteins in the dopamine pathways have been examined for their influence on neurocognitive and neuropsychiatric outcomes following TBI. Catechol-o-methyltransferase (COMT) is an enzyme that mediates dopamine clearance and is coded for by the COMT gene. In the past 5 years, SNPs of this gene have been extensively examined for associations with neurocognitive outcomes [52].
In a 2016 study, Mygra et al. looked at 90 survivors of severe TBI and examined the interaction of depression, frontal lobe dysfunction, and the SNP rs4680 (Val158Met) in the COMT gene. They found that at 12 months post injury, in those with depression, Met homozygotes were found to have significantly worse behavior than Val carriers [52]. The association with verbal processing speed and the rs4680 SNP was examined by Winkler et al. in 100 subjects from the TRACK-TBI Pilot study with mild TBI. The Val homozygotes were found to have worse processing speed than Met carriers by the Wechsler Adult Intelligence Test Processing Speed Index Composite Score (WAIS-PSI; mean increase 7.9 points; 95%CI 1.4–14.3; p = 0.017) [53]. In a follow-up work done by the same group that looked at 93 subjects from the TRACK-TBI Pilot study with mild TBI, the Met allele was associated with lower incidences of PTSD following injury, even when controlling for race (multivariable OR = 0.29; 95%CI 0.10–0.83) and pre-existing psychiatric disorders or substance abuse (multivariable OR = 0.32; 95%CI 0.11–0.97) [21].
Nekrosius et al. looked at 89 patients with mild to moderate TBI during the first 4 days of their admission to hospital and assessed them for signs of delirium. They found that Val homozygotes had an increased risk of delirium in multivariable regression analyses adjusted for alcohol misuse, history of neurological disorder, age, and admission GCS (OR = 4.57; 95%CI 1.11–18.9; p = 0.036) and the Met allele was associated with better functional outcomes in univariate analysis (OR = 2.82; 95%CI 1.10–7.27; p = 0.031) [54].
The COMT gene is not the only dopamine-associated gene that has been studied for its association with neurocognitive and neuropsychiatric outcomes. DRD2 gene and ANKK1 gene SNPs have also been assessed. In a cohort of 108 severe TBI survivors, functional recovery at 6 and 12 months was examined using 8 neuropsychological tests targeting different cognitive domains. When adjusting for age, GCS, and education, DRD2 rs6279 C homozygotes and ANKK1 rs1800497 heterozygotes were found to have better cognitive composite scores at 6 months. At 12 months, only the influence of rs1800497 remained significant [22].
In the Mygra et al. study of 90 survivors of severe TBI, ANKK1 rs1800497 genotyping was also performed and frontal lobe dysfunction was found to be worse at 12 months post injury in C homozygotes compared to T carriers in the bivariant analysis (p = 0.028) [52]. Yue et al. looked at 6-month cognitive performance following TBI in 492 patients and the association with ANKK1 rs1800497 genotype. Using the CVLT-II Trial 1–5 Standard Score, a dose-dependent effect for the T allele was found, with T/T homozygotes scoring the lowest on language testing (T/T 45.1, C/T 51.1, C/C 52.1, ANOVA; p = 0.008) [55].
Much more work is needed before a consistent pattern of influence of neurotransmitter-associated SNPs can be identified. The heterogeneity in outcomes tested, populations examined, and ultimately results makes deriving any clear conclusion difficult at this time.
Physiologic Outcomes
A number of association studies have been done looking at the correlation of different SNPs and various physiologic outcomes such as cerebral perfusion, cerebral edema, and seizures following TBI. While clinically important in and of themselves, these studies help elucidate that causal by which SNPs may influence more general outcomes.
Cerebral Perfusion–Associated Polymorphisms
In recent years, cerebral autoregulation (CA) dysfunction has been revealed as a key prognostic marker following severe TBI. This has prompted exploration into the possible mechanisms of dysfunctional CA and more recently the association between polymorphisms of genes that code for proteins speculated to be involved in CA and global outcomes following TBI has been explored [58].
One such gene is the ACE gene that codes for angiotensin-converting enzyme (ACE). ACE plays a pivotal role in the regulation of vascular tone and blood pressure by activation of the vasoconstrictor angiotensin II. There has also been work showing that ACE is directly involved in modulating regional cerebral blood flow autoregulation and the responsiveness of the cerebral vasculature as measured by transcranial Doppler [59]. In a 2015 study, Dardiotis et al. examined 363 prospectively enrolled TBI patients. They were able to identify and associate three SNPs of the ACE gene (rs4461142, rs7221780, rs8066276) and 6-month GOS scores. The authors noted that these SNPs were all located in the 3′ downstream ACE gene region and point to the potential pharmacogenomic implications of this region [60].
Cerebral Edema
In the previously discussed study performed by Jha et al. of 410 severe TBI patients, the associations between the ABCC8 polymorphisms and cerebral edema and ICP were also examined. This was done by examining radiographic edema on CT scan as well as ICP measurements following TBI [16••].
The rs7105832 (A>C) SNP was significantly associated with differences in average ICP (p = 0.003), peak ICP (p = 0.02), and acute CT edema (p = 0.012). Homozygote variants were found to have a higher frequency of acute CT edema (66%) versus heterozygotes (36.8%) and homozygous wild-type (45.3%). They were also found to have higher mean ICPs (13.0 ± 7.5 mmHg) and peak ICP (31.9 ± 19.0 mmHg) versus heterozygotes (mean ICP 10.0 ± 4; p = 0.004; peak ICP 24.2 ± 10.3, p = 0.045) and homozygous wild-type (mean ICP 10.0 ± 3, p = 0.004; peak ICP 28.8 ± 17, p = 0.099). Notably, this SNP was not found to be associated with 3-month GOS (p = 0.358) [16••].
The rs2237982 (C>T) allele which was found to be associated with 3-month outcomes (p = 0.015) was also found to be associated with higher mean ICP (p = 0.0107), peak ICP (p = 0.0190), and acute CT edema (p = 0.0204) with, once again, the homozygous variant having the worst outcomes (mean ICP 12.4 ± 7.8 mmHg; peak ICP 31.6 ± 18.3 mmHg; acute CT edema 56.7%). Notably, the rs11024286 and rs4148622 SNPs that were associated with global outcomes were not significantly associated with these physiologic parameters.
Seizures and Epilepsy
Post-traumatic seizures and epilepsy are known phenomena and recently attempts have been made to find an association with various SNPs and post-traumatic epilepsy (PTE)/post-traumatic seizures (PTS). In a study of 256 patients with moderate to severe TBI, Diamond et al. examined IL-β gene SNPs for an association with post-traumatic epilepsy. They found that, of the three SNPs tested, the rs1143634 (C>T) SNP was associated with PTE with the heterozygotes having an increased risk compared to homozygotes (HR = 2.845; 95%CI 1.372–5.900; p = 0.005). Notably, the heterozygote group also had lower serum IL-1β levels (p = 0.014) and higher IL-1β CSF/serum ratios (p = 0.093) [61].
Diamond et al. further investigated the association of SNPs and PTE in a cohort of 162 adults with moderate to severe TBI. In this group, SNPs in the gene involved in adenosine homeostasis were examined, including adenosine kinase (ADK), ecto-5'-nucleotidase (NT5E, CD73), and equilibrative nucleoside transporter type-1 (ENT-1) genes. Nine ADK, three CD73, and two ENT-1 tagging SNPs were genotyped in each individual in the cohort. After adjusting for injury severity score (ISS), isolated TBI status, and SDH in multivariate Cox models, two SNPs were associated with PTE. The rs11001109 (ADK; G>A) SNP had an increased risk of PTE when the homozygous variant allele was present (HR = 4.47; 95%CI 1.27–15.7; p = 0.020). The rs9444348 (NT5E; G>A) SNP was also associated with PTE with the highest risk found in the heterozygotes (HR = 2.95; 95%CI 1.19–7.31; p = 0.019) [62].
Ritter et al. hypothesized that excitotoxicity may influence epileptogenesis following severe TBI and so they examined 32 SNPs in the neuronal glutamate transporter genes SLC1A1 and SLC1A6 in a cohort of 253 severe TBI patients to find an association with seizure rates up to 3 years post-injury. After adjusting for covariates known to be associated with PTS (SDH and depressed skull fracture), the SNPs rs7858819 (SLC1A1; C>T; HR 3.4; 95%CI 1.1–10.5; p = 0.023) and rs10974620 (SLC1A1; C>G; HR 3.4; 95%CI 1.3–9.3; p= 0.017) were found to be associated with PTS when comparing the variant homozygotes to the wild-type homozygotes [63].
The hypothesis of excitotoxicity influencing epileptogenesis following severe TBI was further examined in a recent study by Kumar et al. which examined 267 severe TBI patients over a 3-year period following TBI. In this study, 39 SNPs in the SLC1A2 and SLC1A3 genes were analyzed. After adjusting for covariates, the SLC1A3 SNP rs4869682 (T>G) was found to be associated with PTS risk with the GG homozygote having an increased risk (HR = 2.08; 95%CI 1.20–3.62; p = 0.009) [64].
Future Directions
There are several limitations to the clinical utility of SNP association studies following TBI. Small sample sizes often mean that reproduction of results is often rare as can be seen in this review. The different distributions of SNPs in various populations and geographic regions both limit generalizability and make these studies susceptible to unknown confounders. These may be mitigated by large, multi-center international collaboration studies. A new approach has been to incorporate various SNPs into a gene score. These utilize multiple SNPs to create a prognostic model. Those that currently exist are simple and only utilize a handful of SNPs and are able to provide reasonable predictive value. In the future, given advances in computational power and machine learning, it is likely that clustering algorithms may be used to identify genotypes, characterized by hundreds of SNPs that are predictive of certain phenotypic outcomes. Ultimately, SNP association studies, taken on their own, provide no therapeutic intervention. By their very nature, they relate to non-modifiable factors. Perhaps the more practical utility of SNP association studies is as hypothesis generators. These studies give insight into molecular pathways that play a key role in recovery following TBI. These pathways may then go on to become therapeutic targets that may meaningfully impact outcomes following TBI.
Conclusions
Numerous SNP association studies have been performed to try to explain the high degree of variance in outcomes following TBI. Many of these have been able to identify associations with numerous SNPs and specific outcome metrics. The clinically relevant inferences that can be drawn from these studies, however, are questionable. Even when large meta-analyses are performed, the strength of their conclusions is tempered by the nature of the individual studies. Large collaborative, multi-institution networks may provide data with sufficient power to identify true causal relationships. The individual association studies discussed in this paper, while often not suitable to determine clinically significant relationships, do serve to identify targets for further scientific exploration. Hypothesis generating in nature, they give clues to the mechanisms of secondary brain injury and eventually may even lead to therapeutic targets.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lingsma HF, Yue JK, Maas AIR, et al. Outcome prediction after mild and complicated mild traumatic brain injury: external validation of existing models and identification of new predictors using the TRACK-TBI pilot study. Journal of Neurotrauma. 2015;32:83–94.
Roozenbeek B, Lingsma HF, Lecky FE, et al. Prediction of outcome after moderate and severe traumatic brain injury: external validation of the International Mission on Prognosis and Analysis of Clinical Trials (IMPACT) and Corticoid Randomisation After Significant Head injury (CRASH) prognostic models*. Critical Care Medicine. 2012;40:1609–17.
Teasdale GM, Nicoll JA, Murray G, Fiddes M. Association of apolipoprotein E polymorphism with outcome after head injury. The Lancet. 1997;350:1069–71.
Zhou W, Xu D, Peng X, Zhang Q, Jia J, Crutcher KA. Meta-analysis of APOE 4 allele and outcome after traumatic brain injury. Journal of Neurotrauma. 2008;25:279–90.
Zeng S, Jiang J-X, Xu M-H, Xu L-S, Shen G-J, Zhang A-Q, et al. Prognostic value of apolipoprotein E epsilon4 allele in patients with traumatic brain injury: a meta-analysis and meta-regression. Genetic Testing and Molecular Biomarkers. 2014;18:202–10.
• McFadyen CA, Zeiler FA, Newcombe V, Synnot A, Steyerberg E, Gruen RL, et al. Apolipoprotein E4 polymorphism and outcomes from traumatic brain injury: a living systematic review and meta-analysis. J Neurotrauma. 2019. https://doi.org/10.1089/neu.2018.6052Recent systematic review of Apo-E4 polymorphism with the most comprehensive collection of data to date.
Kassam I, Gagnon F, Cusimano MD. Association of the APOE-epsilon4 allele with outcome of traumatic brain injury in children and youth: a meta-analysis and meta-regression. J Neurol Neurosurg Psychiatry. 2016;87:433–40.
Yousuf A, Khursheed N, Rasool I, Kundal V, Jeelani H, Afroze D. Genetic variation of ApoE gene in Ethnic Kashmiri population and its association with outcome after traumatic brain injury. J Mol Neurosci. 2015;56:597–601.
Failla MD, Kumar RG, Peitzman AB, Conley YP, Ferrell RE, Wagner AK. Variation in the BDNF gene interacts with age to predict mortality in a prospective, longitudinal cohort with severe TBI. Neurorehabil Neural Repair. 2015;29:234–46.
Failla MD, Conley YP, Wagner AK. Brain-derived neurotrophic factor (BDNF) in traumatic brain injury–related mortality: interrelationships between genetics and acute systemic and central nervous system BDNF profiles. Neurorehabil Neural Repair. 2016;30:83–93.
Munoz MJ, Kumar RG, Oh B-M, Conley YP, Wang Z, Failla MD, et al. Cerebrospinal fluid cortisol mediates brain-derived neurotrophic factor relationships to mortality after severe TBI: a prospective cohort study. Front Mol Neurosci. 2017. https://doi.org/10.3389/fnmol.2017.00044.
Osier ND, Conley YP, Okonkwo DO, Puccio AM. Variation in candidate traumatic brain injury biomarker genes are associated with gross neurological outcomes after severe traumatic brain injury. Journal of Neurotrauma. 2018;35:2684–90.
Mellett K, Ren D, Alexander S, Osier N, Beers SR, Okonkwo DO, et al. Genetic variation in the TP53 gene and patient outcomes following severe traumatic brain injury. Biological Research For Nursing. 2020;109980042091233.
Wang ZL, Xu DS, Wang YX, Qin H, Geng D. Effect of single nucleotide polymorphisms in the ATP-binding cassette B1 gene on the clinical outcome of traumatic brain injury. Genet Mol Res. 2015;14:10948–53.
Adams SM, Conley YP, Ren D, Okonkwo DO, Puccio AM, Dixon CE, et al. ABCG2 c.421C>A is associated with outcomes after severe traumatic brain injury. J Neurotrauma. 2018;35:48–53.
•• Jha RM, Koleck TA, Puccio AM, et al. Regionally clustered ABCC8 polymorphisms in a prospective cohort predict cerebral oedema and outcome in severe traumatic brain injury. J Neurol Neurosurg Psychiatry. 2018;89:1152–62 Important finding suggesting edema response post-TBI may be linked to blood-brain barrier–related single nucleotide polymorphisms.
Hoh NZ, Wagner AK, Alexander SA, Clark RB, Beers SR, Okonkwo DO, et al. BCL2 Genotypes: functional and neurobehavioral outcomes after severe traumatic brain injury. Journal of Neurotrauma. 2010;27:1413–27.
Bulstrode H, Nicoll JAR, Hudson G, Chinnery PF, Di Pietro V, Belli A (2014) Mitochondrial DNA and traumatic brain injury: mitochondrial DNA and TBI. Ann Neurol 75:186–195
Conley YP, Okonkwo DO, Deslouches S, Alexander S, Puccio AM, Beers SR, et al. Mitochondrial polymorphisms impact outcomes after severe traumatic brain injury. Journal of Neurotrauma. 2014;31:34–41.
Willmott C, Withiel T, Ponsford J, Burke R. COMT Val 158 Met and cognitive and functional outcomes after traumatic brain injury. Journal of Neurotrauma. 2014;31:1507–14.
Winkler EA, Yue JK, Ferguson AR, et al. COMT ValMet polymorphism is associated with post-traumatic stress disorder and functional outcome following mild traumatic brain injury. Journal of Clinical Neuroscience. 2017;35:109–16.
Failla MD, Myrga JM, Ricker JH, Dixon CE, Conley YP, Wagner AK. Posttraumatic brain injury cognitive performance is moderated by variation within ANKK1 and DRD2 genes. Journal of Head Trauma Rehabilitation. 2015;30:E54–66.
Dardiotis E, Dardioti M, Hadjigeorgiou GM, Paterakis K. Re: Lack of association between the IL1A gene (-889) polymorphism and outcome after head injury. Tanriverdi T et al. Surg Neurol 2006;65:7-10; discussion 10. Surgical Neurology. 2006;66:334–5.
Tanriverdi T, Uzan M, Sanus GZ, Baykara O, Is M, Ozkara C, et al. Lack of association between the IL1A gene (-889) polymorphism and outcome after head injury. Surgical Neurology. 2006;65:7–10.
Uzan M, Tanriverdi T, Baykara O, Kafadar A, Sanus GZ, Tureci E, et al. Association between interleukin-1 beta (IL-1β) gene polymorphism and outcome after head injury: an early report. Acta Neurochir (Wien). 2005;147:715–20.
Miñambres E, Cemborain A, Sánchez-Velasco P, Gandarillas M, Díaz-Regañón G, Sánchez-González U, et al. Correlation between transcranial interleukin-6 gradient and outcome in patients with acute brain injury. Critical Care Medicine. 2003;31:933–8.
Dalla Libera AL, Regner A, de Paoli J, Centenaro L, Martins TT, Simon D (2011) IL-6 polymorphism associated with fatal outcome in patients with severe traumatic brain injury. Brain Injury 25:365–369
• Waters RJ, Murray GD, Teasdale GM, Stewart J, Day I, Lee RJ, et al. Cytokine gene polymorphisms and outcome after traumatic brain injury. Journal of Neurotrauma. 2013;30:1710–6 Highlights potential role of host neuroinflammatory response and individual cytokine polymorphism may play on global outcome after TBI.
Osthoff M, Walder B, Delhumeau C, Trendelenburg M, Turck N. Association of lectin pathway protein levels and genetic variants early after injury with outcomes after severe traumatic brain injury: a prospective cohort study. Journal of Neurotrauma. 2017;34:2560–6.
Verghese PB, Castellano JM, Holtzman DM. Apolipoprotein E in Alzheimer’s disease and other neurological disorders. The Lancet Neurology. 2011;10:241–52.
Chen Z-Y. Variant brain-derived neurotrophic factor (BDNF) (Met66) alters the intracellular trafficking and activity-dependent secretion of wild-type BDNF in neurosecretory cells and cortical neurons. Journal of Neuroscience. 2004;24:4401–11.
Gao J, Zheng Z. Development of prognostic models for patients with traumatic brain injury: a systematic review. Int J Clin Exp Med. 2015;8:19881–5.
Dumont P, Leu JI-J, Della Pietra AC, George DL, Murphy M. The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet. 2003;33:357–65.
Verweij BH, Muizelaar JP, Vinas FC, Peterson PL, Xiong Y, Lee CP. Impaired cerebral mitochondrial function after traumatic brain injury in humans. Journal of Neurosurgery. 2000;93:815–20.
Vink R, Golding EM, Headrick JP. Bioenergetic analysis of oxidative metabolism following traumatic brain injury in rats. Journal of Neurotrauma. 1994;11:265–74.
Bredesen DE. Apoptosis: overview and signal transduction pathways. Journal of Neurotrauma. 2000;17:801–10.
Thelin EP, Tajsic T, Zeiler FA, Menon DK, Hutchinson PJA, Carpenter KLH, et al. Monitoring the neuroinflammatory response following acute brain injury. Front Neurol. 2017;8:351.
Zeiler FA, Thelin EP, Czosnyka M, Hutchinson PJ, Menon DK, Helmy A. Cerebrospinal fluid and microdialysis cytokines in severe traumatic brain injury: a scoping systematic review. Front Neurol. 2017;8:331.
Han SD, Drake AI, Cessante LM, Jak AJ, Houston WS, Delis DC, et al. Apolipoprotein E and traumatic brain injury in a military population: evidence of a neuropsychological compensatory mechanism? Journal of Neurology, Neurosurgery & Psychiatry. 2007;78:1103–8.
Merritt VC, Arnett PA. Apolipoprotein E (APOE) ϵ4 allele is associated with increased symptom reporting following sports concussion. J Int Neuropsychol Soc. 2016;22:89–94.
Yue JK, Robinson CK, Burke JF, et al. Apolipoprotein E epsilon 4 (APOE- ε 4) genotype is associated with decreased 6-month verbal memory performance after mild traumatic brain injury. Brain Behav. 2017;7:e00791.
Merritt VC, Clark AL, Sorg SF, Evangelista ND, Werhane M, Bondi MW, et al. Apolipoprotein E ε4 genotype is associated with elevated psychiatric distress in veterans with a history of mild to moderate traumatic brain injury. Journal of Neurotrauma. 2018;35:2272–82.
Merritt VC, Clark AL, Sorg SF, Evangelista ND, Werhane ML, Bondi MW, et al. Apolipoprotein E (APOE) ε4 genotype is associated with reduced neuropsychological performance in military veterans with a history of mild traumatic brain injury. Journal of Clinical and Experimental Neuropsychology. 2018;40:1050–61.
Padgett CR, Summers MJ, Vickers JC, McCormack GH, Skilbeck CE. Exploring the effect of the apolipoprotein E (APOE) gene on executive function, working memory, and processing speed during the early recovery period following traumatic brain injury. Journal of Clinical and Experimental Neuropsychology. 2016;38:551–60.
Banks SJ, Miller JB, Rissman RA, Bernick CB. Lack of influence of apolipoprotein E status on cognition or brain structure in professional fighters. Journal of Neurotrauma. 2017;34:380–4.
Krueger F, Pardini M, Huey ED, Raymont V, Solomon J, Lipsky RH, et al. The role of the Met66 brain-derived neurotrophic factor allele in the recovery of executive functioning after combat-related traumatic brain injury. Journal of Neuroscience. 2011;31:598–606.
Barbey AK, Colom R, Paul E, Forbes C, Krueger F, Goldman D, et al. Preservation of general intelligence following traumatic brain injury: contributions of the Met66 brain-derived neurotrophic factor. PLoS ONE. 2014;9:e88733.
McAllister TW, Tyler AL, Flashman LA, Rhodes CH, McDonald BC, Saykin AJ, et al. Polymorphisms in the brain-derived neurotrophic factor gene influence memory and processing speed one month after brain injury. Journal of Neurotrauma. 2012;29:1111–8.
Bagnato S, Minafra L, Bravatà V, et al. Brain-derived neurotrophic factor (Val66Met) polymorphism does not influence recovery from a post-traumatic vegetative state: a blinded retrospective multi-centric study. Journal of Neurotrauma. 2012;29:2050–9.
Narayanan V, Veeramuthu V, Ahmad-Annuar A, Ramli N, Waran V, Chinna K, et al. Missense mutation of brain derived neurotrophic factor (BDNF) alters neurocognitive performance in patients with mild traumatic brain injury: a longitudinal study. PLoS ONE. 2016;11:e0158838.
Wang Y-J, Chen K-Y, Kuo L-N, et al. The association between BDNF Val66Met polymorphism and emotional symptoms after mild traumatic brain injury. BMC Med Genet. 2018;19:13.
Myrga JM, Juengst SB, Failla MD, Conley YP, Arenth PM, Grace AA, et al. COMT and ANKK1 Genetics interact with depression to influence behavior following severe TBI: an initial assessment. Neurorehabil Neural Repair. 2016;30:920–30.
Winkler EA, Yue JK, McAllister TW, et al. COMT Val 158 Met polymorphism is associated with nonverbal cognition following mild traumatic brain injury. Neurogenetics. 2016;17:31–41.
Nekrosius D, Kaminskaite M, Jokubka R, Pranckeviciene A, Lideikis K, Tamasauskas A, et al. Association of COMT Val 158 Met polymorphism with delirium risk and outcomes after traumatic brain injury. JNP. 2019;31:298–305.
Yue JK, Pronger AM, Ferguson AR, et al. Association of a common genetic variant within ANKK1 with six-month cognitive performance after traumatic brain injury. Neurogenetics. 2015;16:169–80.
Merritt VC, Rabinowitz AR, Arnett PA. The influence of the apolipoprotein E (APOE) gene on subacute post-concussion neurocognitive performance in college athletes. Archives of Clinical Neuropsychology. 2018;33:36–46.
Egan MF, Kojima M, Callicott JH, et al. The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell. 2003;112:257–69.
Zeiler FA, Thelin EP, Donnelly J, Stevens AR, Smielewski P, Czosnyka M, et al. Genetic drivers of cerebral blood flow dysfunction in TBI: a speculative synthesis. Nat Rev Neurol. 2019;15:25–39.
Hajjar I, Sorond F, Hsu Y-H, Galica A, Cupples LA, Lipsitz LA. Renin angiotensin system gene polymorphisms and cerebral blood flow regulation: the MOBILIZE Boston study. Stroke. 2010;41:635–40.
Dardiotis E, Paterakis K, Siokas V, et al. Effect of angiotensin-converting enzyme tag single nucleotide polymorphisms on the outcome of patients with traumatic brain injury. Pharmacogenetics and Genomics. 2015;25:485–90.
Diamond ML, Ritter AC, Failla MD, Boles JA, Conley YP, Kochanek PM, et al. IL-1β associations with posttraumatic epilepsy development: a genetics and biomarker cohort study. Epilepsia. 2015;56:991–1001.
Diamond ML, Ritter AC, Jackson EK, Conley YP, Kochanek PM, Boison D, et al. Genetic variation in the adenosine regulatory cycle is associated with posttraumatic epilepsy development. Epilepsia. 2015;56:1198–206.
Ritter AC, Kammerer CM, Brooks MM, Conley YP, Wagner AK. Genetic variation in neuronal glutamate transport genes and associations with posttraumatic seizure. Epilepsia. 2016;57:984–93.
Kumar RG, Breslin KB, Ritter AC, Conley YP, Wagner AK. Variability with astroglial glutamate transport genetics is associated with increased risk for post-traumatic seizures. Journal of Neurotrauma. 2019;36:230–8.
Funding
AG is supported through the University of Manitoba Clinician Investigator Program. CB is supported through the Centre on Aging Fellowship at the University of Manitoba. LF is supported through a University of Manitoba Department of Surgery GFT Grant, and through the URGP grant program. FAZ receives research support from the Manitoba Public Insurance (MPI) Neuroscience/TBI Research Endowment, the Health Sciences Centre Foundation Winnipeg, the United States National Institutes of Health (NIH) through the National Institute of Neurological Disorders and Stroke (NINDS)(Grant #: R03NS114335-01), the Canadian Institutes of Health Research (CIHR)(Grant #: 432061), the Canada Foundation for Innovation (CFI)(Project #: 38583), Research Manitoba (Grant #: 3906), the University of Manitoba VPRI Research Investment Fund (RIF), the University of Manitoba Centre on Aging, and the University of Manitoba Rudy Falk Clinician-Scientist Professorship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurotrauma
Rights and permissions
About this article
Cite this article
Gomez, A., Batson, C., Froese, L. et al. Genetic Variation and Impact on Outcome in Traumatic Brain Injury: an Overview of Recent Discoveries. Curr Neurol Neurosci Rep 21, 19 (2021). https://doi.org/10.1007/s11910-021-01106-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s11910-021-01106-1