Abstract
Introduction
The optimal management of high risk WHO grade II gliomas after surgery is debated including the role of initial temozolomide to delay radiotherapy and risk of cognitive defects.
Methods
A post-hoc analysis of a phase II multicenter study on high risk WHO grade II gliomas, receiving initial temozolomide alone, has re-evaluated the long-term results within the molecular subgroups of WHO 2016. The primary endpoint of the study was response according to RANO, being seizure response, PFS and OS secondary endpoints.
Results
Response rate among oligodendrogliomas IDH-mutant and 1p/19q codeleted (76%) was significantly higher than that among diffuse astrocytomas either mutant (55%) or wild-type (36%). A reduction of seizure frequency > 50% was observed in 87% of patients and a seizure freedom in 72%. The probability of seizure reduction > 50% was significantly associated with the presence of an IDH mutation. Median PFS, PFS at 5 and 10 years, median OS and OS at 5 and 10 years were significantly longer in oligodendrogliomas IDH-mutant and 1p/19q codeleted. Sixty-seven percent of patients with oligodendroglioma IDH mutant and 1p/19q codeleted did not recur with a median follow up of 9.3 years, while 59% did not receive radiotherapy at recurrence with a median follow up of 8.2 years.
Conclusions
The beneficial effects of initial temozolomide prevail in oligodendrogliomas IDH-mutant and 1p/19q codeleted: thus, these tumors, when incompletely resected or progressive after surgery alone, or with intractable seizures, should receive temozolomide as initial treatment with salvage radiotherapy and/o reoperation and/or second-line chemotherapy at recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diffuse low-grade gliomas (LGG) represent a heterogeneous group of tumors, and high-risk patients, i.e. those with age > 40 years or incomplete resection or intractable seizures or clinical and radiological progression following initial observation, need adjuvant treatments. Radiotherapy improves progression-free survival (PFS) but not overall survival (OS) compared with observation and delayed intervention at tumor progression [1]. Phase III RTOG 9802 trial [2] has reported a significant prolongation of PFS and OS by adding PCV chemotherapy to radiotherapy. However, a risk of cognitive decline in long-term survivors following radiotherapy exists [3], and this has led many clinicians to delay radiotherapy at salvage in favor of initial chemotherapy. Few studies have reported an efficacy of temozolomide (TMZ) in patients with LGG, who were radiotherapy-naïve [4, 5].
Dose-dense TMZ has been suggested to increase the chemosensitivity of LGGs by overcoming MGMT resistance [6, 7]. Phase III EORTC 22,033 trial in high-risk LGG has shown that PFS does not differ between dose dense TMZ and radiotherapy [8].
Between 2007 and 2010 the Italian Association for Neuro-Oncology (AINO) conducted a single arm phase II study to evaluate the efficacy and toxicity of dose-dense TMZ in high-risk oligodendroglial tumors based on the hypothesis that an intensification of chemotherapy would have been successful in such a chemosensitive subgroup. The inclusion of patients was based on the WHO classification of 2007 and preliminary results were reported in an abstract form [9]. In this post-hoc analysis we have re-evaluated the long-term results according to new WHO classification of 2016 [10].
Methods
Eligibility criteria
Inclusion criteria were as follows: age ≥ 18 years; KPS ≥ 70; high-risk patients, as defined by either incomplete resection or biopsy, or progression following initial observation with MRI in case of total/near total resection; measurable tumor on FLAIR MRI before the chemotherapy (>10 × 10 mm); absent or mild or patchy contrast enhancement on MRI; no previous radiotherapy or chemotherapy; no evidence of compromised hematologic, hepatic or renal function on laboratory testing, and HBV/HBC/HIV negative test. Exclusion criteria included: any previous antineoplastic treatment other than surgery; intense contrast enhancement; history of malignancy in remission for less than 5 years, and women who were pregnant, breastfeeding, or of child-bearing potential not willing to use contraception.
All patients had to sign an informed consent. The protocol was approved by the local EC and registered in EUDRACT (n.2007/000386-38).
Trial design and treatment
All patients underwent physical and neurological examination plus laboratory testing at baseline and before every cycle of chemotherapy. Brain MRI with gadolinium was performed at baseline and every three cycles. Seizure characteristics (frequency, type, duration) and antiepileptic medication were collected by means of a diary at each neurological examination. TMZ was administered orally once per day at a dose of 150 mg/m2 7 days-on/7 days-off every 28 days up to a maximum of 18 cycles. Prophylaxis against Pneumocystis Carinii pneumonia with oral trimethoprim/sulfamethoxazole was used in case of severe lymphopenia, and delays or dose reductions of TMZ were permitted. TMZ was stopped for any type of irreversible grade 3 or 4 toxicity.
Outcomes
The primary end-point of the study was response based on RANO criteria for low-grade gliomas [11] (Supplementary Table 1). The response on MRI was reviewed independently by 2 investigators, who were unaware of seizure response and outcome.
Secondary end-points were seizure response, median PFS, PFS at 5 years, median OS, OS at 5 years, and toxicity. Seizure response was defined by reduction > 50% of seizure frequency and seizure freedom as compared with baseline in the absence of any change of antiepileptic drugs (AEDs).
Molecular analysis
1p/19q codeletion, IDH1-2 mutations and MGMT methylation status were analyzed either at the time of treatment or through a post-hoc analysis performed at the end of the study. 1p/19q codeletion testing was performed by fluorescence in situ hybridization (FISH) analysis. The mutational status of IDH1 and IDH2 was established by immunohistochemistry for the most common mutant IDH1 R132H, complemented by DNA sequencing in negative cases. MGMT methylation status was assessed using the MGMT-STP27 model. Then, the tumors were reclassified according to the new WHO classification of 2016 [10], that recognizes 3 subtypes, i.e. oligodendrogliomas IDH mutant and 1p/19q codeleted, diffuse astrocytomas IDH mutant, and diffuse astrocytomas IDH wild-type.
Statistical analysis
The sample size for a Simon minimax two-stage design was calculated, where the expected probability of response was 70% and the null hypothesis probability was 50%, with a one-sided α-error of 5% and a power of 80%. Under these assumptions, at least 13/23 responders were required for the first stage to continue to stage 2 and at least 24/37 responders were required in the end of the study to consider the drug potentially active and worth of further investigation. Overall, at the end of the second stage we observed 27/37 responses (73%): thus, considering also the high impact of the drug on seizures, the enrollment was prolonged until the end of year 2010, and the final analysis was performed on a total of 60 patients.
Baseline patient characteristics were compared according to primary endpoint (PR/MR vs. SD/PD) by using the Mann–Whitney U test and χ2 test (or Fisher’s exact test, if appropriate) for continuous variables and categorical variables.
The prognostic or predictive role of sociodemographic, clinical and molecular characteristics at baseline were assessed by logistic regression models, where response (PR/MR vs. SD/PD) was the outcome variable. Crude and adjusted odds ratios (ORs) and their 95% confidence intervals (95% CI) were reported.
PFS was measured from the date of chemotherapy start to the date of first disease progression or death or last follow-up (whichever occurred first). OS was measured from the date of chemotherapy start to the date of death or last follow-up (whichever occurred first).
Survival curves were estimated using the Kaplan–Meier method and differences were evaluated by the log-rank test. A Cox proportional hazard model was employed to estimate the crude and the multivariable-adjusted hazard ratios (HRs) with 95% confidence intervals (CIs) for possible predictors of survival. The proportional hazard assumption was verified by graphical checks and formal tests based on Schoenfeld residuals.
Prevalence of seizure reduction (more than 50%) and seizure freedom after TMZ therapy were reported for 39 patients at the end of follow-up.
Statistical analyses were performed using Stata 13.1 software (StataCorp LP, College Station, TX).
Results
Patient characteristics and treatment
From 4/2007 to 12/2010, 60 patients were enrolled from 6 Italian Institutions, and are evaluable (Table 1). Median number of TMZ cycles was 11 (range 7–18) with a median follow-up of 8.9 years (range 5.3–10.2 + ). In 31 patients (51.7%) the daily dose of TMZ was decreased from 150 to 100–130 mg/m2 following a median number of 4 cycles (range 2–9) due to persistent myelotoxicity, thus reducing the dose intensity.
Efficacy
Best response to dose-dense TMZ according to RANO criteria was as follows: CR in 0/60 patients, PR in 23/60 (38.3%), MR in 12/60 (20%), SD in 21/60 (35%), and PD in 4/60 (6.7%). Oligodendrogliomas achieved a PR in 8/29 (27.6%), a MR in 14/29 (48.3%), and a SD in 7/29 (24.1%), while diffuse astrocytomas IDH-mutant achieved a PR in 1/9 (11%), a MR in 4/9 (44.5%) and a SD in 4/9 (44.5%). Progressive disease was not observed in both tumor groups. Diffuse astrocytomas IDH-wild type displayed a PR in 3/22 (13.6%), a MR in 5/22 (22.7%), a SD in 10/22 (45.5%), and a PD in 4/22 (18.2%).
Age, risk group and dose intensity of TMZ did not display any association with response. MGMT methylation was significantly associated with response in univariate (p = 0.002) and multivariable (p = 0.015) analysis: PR + MR occurred in 33/35 (94.3%) of MGMT methylated patients and in 2/35 (5.7%) of MGMT unmethylated patients. Oligodendrogliomas were associated with response in univariate analysis only (p = 0.006). All these correlations are reported in Table 2 and in Supplementary Table 2.
A seizure reduction ˃ 50% was observed in 34 out of 39 (87.2%) patients, while an increase of seizure frequency did not occur. The median time to maximal seizure reduction ˃ 50% and maximal response on MRI were 3 months and 6 months, respectively (Supplementary Table 3).
A seizure freedom at the end of TMZ was observed in 26/39 (66.7%) patients, with a reduction of AEDs in 11/28 (39%), and a withdrawal in 2/28 (7%).
The association of reduction of seizures > 50% and seizure freedom with clinical and molecular factors is reported in Table 3. Twenty-four out of 34 (70.6%) patients with a seizure reduction > 50% displayed either a PR or MR on FLAIR MRI, while 10/34 (29.4%) a SD/PD (p = 0.047). Twenty-five out of 34 (73.5%) patients with a seizure reduction > 50% had an IDH mutation, while 9/33 (27.3%) were IDH wild-type (p = 0.035). Seizure freedom was not associated with any clinical or molecular factor.
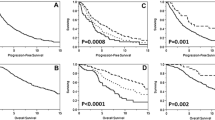
Median PFS was 3.4 years (CI95% 2.2–4.3). PFS was 54.6% (CI95% 41.1–66.2) at 3 years and 32.4% (CI95% 20.9–44.4) at 5 years. PFS curves according to histological/molecular type and MGMT methylation are shown in Fig. 1. Age, risk group and TMZ dose intensity did not display any association with PFS. Univariate analysis showed that PFS was associated with MGMT methylation (HR 0.49, 95% CI 0.25–0.96, p = 0.038) and oligodendroglioma subtype (HR 0.43, 95% CI 0.23–0.80, p = 0.008). After multivariable analysis oligodendroglioma subtype (HR 0.42, 95% CI 0.20–0.89, p = 0.024) retained an independent prognostic value. All these correlations are reported in Table 4.
Oligodendrogliomas showed a median PFS of 4.2 years (CI95% 3.3–7.2) and a 3- and 5-year PFS of 72.4% (CI95% 52.33–85.1) and 37.9% (CI95% 20.9–54.9), respectively. Diffuse astrocytomas IDH-mutant showed a median PFS of 3.6 years (CI95% 0.8–7.8) and a PFS of 55.5% at 3- and 5-years (CI95% 20.4–80.4). Diffuse astrocytomas IDH-wild type displayed a median PFS of 10.8 months (CI95% 8.4–31.2) and a 3- and 5-year PFS of 30% (CI95% 12.5–49.8) and 15.0% (CI95% 3.18–33.3), respectively. Ten-year PFS was 27.2% (CI95% 12.6–44.0) in oligodendrogliomas and 10% (CI95% 1.7–27.1) in diffuse astrocytomas IDH-wild type. None of the diffuse astrocytomas IDH-mutant survived 10 years (Fig. 1).
Thirty-five of 60 patients (58.3%) died during the follow-up period. Median OS and OS at 3 and 5 years were 9.2 years (8.2–11–9), 85.0% (CI95% 73.2–91.9) and 80.0% (CI95% 67.5–88.1), respectively.
Age and risk group did not display any association with OS, while oligodendroglioma was the sole factor with statistical significance in both univariate (p < 0.001) and multivariable (p < 0.001) analysis (Table 5). Median OS and OS at 3 and 5 years for oligodendrogliomas were 9.8 years (CI95% 7.6–9.9), 96.5% (CI95% 77.9–99.5) and 89.7% (CI95% 71.2–96.5), respectively. Median OS for diffuse astrocytoma IDH.mutant was 9.3 years (CI95% 9.0–9.8) with 85% (CI95% 67.3–93.1) of patients surviving at 3 and 5 years. Median OS and OS at 3 and 5 years for diffuse astrocytomas IDH wild type were 5.4 years (CI95% 3.8–7.0), 63.6% (CI95% 40.2–79.9) and 59.1% (CI95% 36.1–76.2), respectively.
Ten-year OS was 78.2% (CI95% 57.4–89.7) in oligodendrogliomas, 22.2% (CI95% 3.3–51.3) in diffuse astrocytomas IDH-mutant, and 17.1% (CI95% 4.8–35.7) in diffuse astrocytomas IDH-wild type.
Recurrence
A local tumor recurrence on MRI occurred in 48/60 patients (80%), who received salvage therapies, either alone or in combination. Twenty-six patients (54.2%) underwent reoperation, 31 (64.5%) radiotherapy, and 42 (87.5%) chemotherapy with nitrosoureas.
Twelve of 60 patients (20%) did not recur with a median follow-up of 9.7 years (range 4.8–11.9): 8/12 (66.7%) were oligodendrogliomas and 3/12 (25%) diffuse astrocytomas IDH-wild type, while 1/12 (8.3%) was a diffuse astrocytoma IDH-mutant.
Twenty-nine of 60 patients (48%) did not receive radiotherapy with a median follow-up of 8.2 years (range 0.7–11.9): 17/29 (58.6%) were oligodendrogliomas, 2/29 (6.9%) diffuse astrocytomas IDH-mutant, and 10/29 (34.5%) diffuse astrocytomas IDH-wild type.
Of 20 patients, who were MGMT methylated at first surgery, 7 (35%) retained their original status, while 13 (75%) became unmethylated. Among these patients, 9 were oligodendrogliomas, 1 a diffuse astrocytoma IDH mutant, and 3 diffuse astrocytomas IDH wild type. The 6 patients, who were unmethylated at first surgery, remained unmethylated.
Discussion
The optimal management of high-risk LGGs (WHO grade II) after surgery is still debated, as these tumors are rare and the WHO classification of 2016 [10] has recognized new molecular subgroups, that display a different outcome. Recent clinical trials, randomized [2, 8] or single arm [5], have added information on the role of radiotherapy and chemotherapy in high risk patients; however, there is paucity of information on the impact of treatments within the molecular subgroups of WHO 2016.
At the best of our knowledge, this is the first study that analyzed within the new molecular subgroups of WHO 2016 the response on MRI and seizure outcome following initial TMZ in a cohort of high risk LGGs. Dose-dense TMZ yielded a response rate (PR + MR) of 58%, which overlaps that of standard [4, 12] or protracted [6, 7] schedules. Oligodendrogliomas had the highest response rate (76% PR + MR) as compared to diffuse astrocytomas either IDH-mutant (55%) or wild-type (36% PR + MR). The response rate of oligodendrogliomas as defined by molecular characteristics was significantly higher than that reported with traditional histologic criteria (76% vs. 31% to 61%) [4, 12]: the likely explanation is that old studies were enriched for the less chemosensitive diffuse astrocytomas.
A strong seizure response following TMZ occurred, with a reduction of seizure frequency > 50% in 87% of patients and seizure freedom in 72%. This finding is of utmost clinical significance as commonly seizures represent the sole symptom of LGGs. Of note this trial pre-specified seizures as a secondary endpoint as suggested by the RANO criteria [13], and did not allow any increase of the AED medication that would have contributed to seizure response. Conversely, all previous retrospective studies did not consider the changes of AEDs concurrent with TMZ, and some included both radiotherapy-naïve and radiotherapy pretreated patients, with a wide range of seizure response after TMZ (18% to 90%) [4, 12, 14,15,16].
Seizure reduction following TMZ more often occurred earlier than response on MRI, and was not always associated with tumor shrinkage, similarly to what described following radiotherapy [17].
A novel finding of this study is that IDH mutation, which is associated with a higher risk for seizures at presentation [18, 19], is predictive of response of seizures to TMZ as well. This finding could be most likely explained by the association of IDH mutation with MGMT methylation, thus with a higher probability to respond to TMZ.
PFS of oligodendrogliomas was of the same order in our study (4.2 years) and in EORTC (4.6 years) and Wahl (4.9 years) studies, while PFS of diffuse astrocytomas IDH-mutant was slightly lower (3 and 3.6 years). OS of oligodendrogliomas is similar in our study (9.8 years) and Wahl study (9.7 years), while EORTC data on OS are still not mature.
Overall, PFS and OS following radiotherapy plus PCV in RTOG 9802 (10.4 and 13.3 years), respectively [2], are definitely longer than those observed following initial TMZ. However, the analysis of the impact of combined treatment within the molecular subgroups was performed only in a small number of patients due to unavailability of pathologic material.
Of note in our study radiotherapy was delayed for 8.2 years in about half of the patients: the majority (59%) were oligodendrogliomas, while few (6.9%) only were diffuse astrocytomas IDH mutant. Thus, the question is whether a sequential approach, consisting of TMZ as initial treatment with reoperation and/or radiotherapy plus PCV at tumor relapse, is of the same value of early radiotherapy plus PCV in terms of balance between survival and cognitive preservation in patients with high risk oligodendrogliomas. PCV as initial treatment could be more effective than TMZ [20], but the level of evidence is low. In this regard, a phase III study from ANOCEF (France) is comparing in newly diagnosed IDH-mutant grade II gliomas PCV vs RT + PCV. The comparison between RT + PCV and RT + TMZ in IDH mutant 1p/19q codeleted grade II and III tumors is the objective of the phase III CODEL trial conducted by RTOG/Alliance and EORTC. Notably, in all ongoing trials a monitoring of cognitive functions over time is mandatory.
A retrospective analysis of a large registry in US has suggested that chemotherapy alone is not inferior in terms of OS to chemoradiation [21], but the median follow-up (4–6 years) was too short to capture a delayed efficacy of the combined treatment.
Conversely, our results do not support TMZ alone as initial treatment for diffuse astrocytomas either IDH mutant or wild-type.
This study confirms the well known predictive value of MGMT methylation for response to TMZ in low-grade gliomas. The subgroup of oligodendrogliomas was in this study the sole factor with a significant association with longer PFS and OS in multivariable analysis: this mainly reflects the predictive and prognostic importance of IDH1 mutation [22], whose presence is correlated with 1p/19q codeletion and MGMT methylation [23]. A recent subgroup analysis of NRG Oncology/RTOG 0424 single arm trial has suggested that MGMT methylation is an independent prognostic marker of high-risk low-grade gliomas treated with temozolomide and radiotherapy in addition to IDH mutation [24]. Our sample size was too small to investigate this issue.
An open question is whether an early alkylating chemotherapy, which induces a hypermutated status [25], accelerates malignant transformation, but thus far there is no evidence in the clinical setting. However, it is unknown whether an early use of TMZ could be detrimental in some subgroups of patients and whether a reoperation at first tumor progression is a safer option instead of chemotherapy. In this study the majority of patients, who were MGMT methylated at first surgery, became unmethylated at reoperation: this suggests a chemotherapy-induced shift toward a more chemoresistant phenotype.
This study has some limitations. The sample size is relatively small for a subgroup analysis and a central molecular testing was not performed.
In conclusion, among high-risk grade II gliomas the beneficial effects of initial TMZ significantly prevailed in oligodendrogliomas: thus, these tumors, when incompletely resected or progressive after surgery or with intractable seizures, should receive TMZ as initial treatment, with reoperation and/or radiotherapy plus PCV at recurrence, but controlled trials are needed to verify this hypothesis.
Change history
05 November 2019
The third and fourth authors' affiliation was incorrectly specified in the original publication. It is correctly shown here.
References
van den Bent MJ, Afra D, de Witte O et al (2005) Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: the EORTC 22845 randomised trial. Lancet 366(9490):985–990
Buckner JC, Shaw EG, Pugh SL et al (2016) Radiation plus procarbazine, CCNU, and vincristine in low-grade glioma. N Engl J Med 374(14):1344–1355
Douw L, Klein M, Fagel SS et al (2009) Cognitive and radiological effects of radiotherapy in patients with low-grade glioma: long-term follow-up. Lancet Neurol 8(9):810–818
Brada M, Viviers L, Abson C et al (2003) Phase II study of primary temozolomide chemotherapy in patients with WHO grade II gliomas. Ann Oncol 14(12):1715–1721
Wahl M, Phillips JJ, Molinaro AM et al (2017) Chemotherapy for adult low-grade gliomas: clinical outcomes by molecular subtype in a phase II study of adjuvant temozolomide. Neuro-Oncology 19(2):242–251
Pouratian N, Gasco J, Sherman JH et al (2007) Toxicity and efficacy of protracted low dose temozolomide for the treatment of low grade gliomas. J Neurooncol 82(3):281–288
Kesari S, Schiff D, Drappatz J et al (2009) Phase II study of protracted daily temozolomide for low-grade gliomas in adults. Clin Cancer Res 15(1):330–337
Baumert BG, Hegi ME, van den Bent MJ et al (2016) Temozolomide chemotherapy versus radiotherapy in high-risk low-grade glioma (EORTC 22033–26033): a randomised, open-label, phase 3 intergroup study. Lancet Oncol 17(11):1521–1532
Pellerino A, Franchino F, Pace A et al. (2017) Temozolomide (TMZ) 1 week on/1 week off as initial treatment for high risk low grade oligodendroglial tumors: a phase II AINO (Italian Association for Neuro-Oncology) study. Neuro Oncol 19(suppl_3):iii21
Louis DN, Perry A, Reifenberger G et al (2016) The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol 131(6):803–820
van den Bent MJ, Wefel JS, Schiff D et al (2011) Response assessment in neuro-oncology (a report of the RANO group): assessment of outcome in trials of diffuse low-grade gliomas. Lancet Oncol 12(6):583–593
Hoang-Xuan K, Capelle L, Kujas M et al (2004) Temozolomide as initial treatment for adults with low-grade oligodendrogliomas or oligoastrocytomas and correlation with chromosome 1p deletions. J Clin Oncol 22(15):3133–3138
Avila EK, Chamberlain M, Schiff D et al (2017) Seizure control as a new metric in assessing efficacy of tumor treatment in low-grade glioma trials. Neuro-Oncology 19(1):12–21
Kaloshi G, Benouaich-Amiel A, Diakite F et al (2007) Temozolomide for low-grade gliomas: predictive impact of 1p/19q loss on response and outcome. Neurology 68(21):1831–1836
Sherman JH, Moldovan K, Yeoh HK et al (2011) Impact of temozolomide chemotherapy on seizure frequency in patients with low-grade gliomas. J Neurosurg 114(6):1617–1621
Koekkoek JA, Dirven L, Heimans JJ et al (2015) Seizure reduction in a low-grade glioma: more than a beneficial side effect of temozolomide. J Neurol Neurosurg Psychiatry 86(4):366–373
Rudà R, Magliola U, Bertero L et al (2013) Seizure control following radiotherapy in patients with diffuse gliomas: a retrospective study. Neuro-Oncology 15(12):1739–1749
Stockhammer F, Misch M, Helms HJ et al (2012) IDH1/2 mutations in WHO grade II astrocytomas associated with localization and seizure as the initial symptom. Seizure 21(3):194–197
Liubinas SV, D'Abaco GM, Moffat BM et al (2014) IDH1 mutation is associated with seizures and protoplasmic subtype in patients with low-grade gliomas. Epilepsia 55(9):1438–1443
Donovan LE, Lassman AB (2019) Chemotherapy Treatment and Trials in Low-Grade Gliomas. Neurosurg Clin N Am 30(1):103–109
Jhaveri J, Liu Y, Chowdhary M et al (2018) Is less more? Comparing chemotherapy alone with chemotherapy and radiation for high-risk grade 2 glioma: an analysis of the National Cancer Data Base. Cancer 124(6):1169–1178
Houillier C, Wang X, Kaloshi G et al (2010) IDH 1 or IDH2 mutations predict longer survival and response to temozolomide in low-grade gliomas. Neurology 75(17):1560–1566
Leu S, von Felten S, Frank S et al (2013) IDH/MGMT-driven molecular classification of low-grade glioma is a strong predictor for long-term survival. Neuro-Oncology 15(4):469–479
Bell EH, Zhang P, Fisher BJ et al (2018) Association of MGMT promoter methylation status with survival Outcomes in Patients With High-Risk Glioma Treated With Radiotherapy and Temozolomide: An Analysis From the NRG Oncology/RTOG 0424 Trial. JAMA Oncol 4(10):1405–1409
Johnson BE, Mazor T, Hong C et al (2014) Mutational analysis reveals the origin and therapy-driven evolution of recurrent glioma. Science 343(6167):189–193
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and design: Roberta Rudà, Alessia Pellerino, Riccardo Soffietti. Provision of study materials or patients: All authors. Collection and assembly of data: Alessia Pellerino, Giulia Marchese. Statistical analysis: Enrica Migliore. Article writing: Roberta Rudà, Alessia Pellerino, Riccardo Soffietti. Final approval of article: All authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rudà, R., Pellerino, A., Pace, A. et al. Efficacy of initial temozolomide for high-risk low grade gliomas in a phase II AINO (Italian Association for Neuro-Oncology) study: a post-hoc analysis within molecular subgroups of WHO 2016. J Neurooncol 145, 115–123 (2019). https://doi.org/10.1007/s11060-019-03277-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03277-x