Abstract
Glioblastoma multiforme (GBM) is the most common and most aggressive form of intrinsic brain tumour. Despite standard treatment involving surgical resection, chemotherapy and radiotherapy this disease remains incurable with the majority of tumours recurring adjacent to the resection cavity. Consequently there is a clear need to improve local tumour control. Convection-enhanced delivery (CED) is a practical technique for administering chemotherapeutics directly into peritumoural brain. In this study, we have tested the hypothesis that carboplatin would be an appropriate chemotherapeutic agent to administer by CED into peritumoural brain to treat GBM. Within this study we have evaluated the relationships between carboplatin concentration, duration of exposure and tumour cell kill in vitro using GBM cell lines and the relationship between carboplatin concentration and clinical and histological evidence of toxicity in vivo. In addition, we have used laser ablation inductively coupled plasma mass spectrometry (LA-ICP-MS) to evaluate the distribution properties of carboplatin following CED into rat brain and to determine the rate at which carboplatin is cleared from the brain. Finally, we have compared the distribution properties of carboplatin and the MRI contrast agent gadolinium-DTPA in pig brain. The results of these experiments confirm that carboplatin can be widely distributed by CED and that it remains in the brain for at least 24 h after infusion completion. Furthermore, carboplatin provokes a significant GBM cell kill at concentrations that are not toxic to normal brain. Finally, we provide evidence that gadolinium-DTPA coinfusion is a viable technique for visualising carboplatin distribution using T1-weighted MR imaging.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma multiforme (GBM) is the most common and most aggressive form of primary brain tumour with an incidence of 2.8 cases per 100,000 per year in the United States [1]. Despite extensive research the prognosis for patients with GBM remains bleak. Current treatment involves a combination of surgical resection, systemic chemotherapy and radiotherapy. However, due to the highly infiltrative nature of GBM and the intrinsic chemoresistance of GBM cells, 80% of tumours recur within 2 cm of the tumour resection cavity [2] or in the context of tumours treated by radiotherapy and chemotherapy alone, recurrence most commonly occurs adjacent to the original tumour mass [3, 4]. As systemic dissemination of GBM is extremely rare and the median survival for recurrent GBM is typically less than 1 year [5], there is a clear and rational need for effective strategies aimed at improving local tumour control.
Techniques attempted in clinical trials to improve the local control of GBM have included the direct infusion or implantation of conventional chemotherapeutic agents such as carmustine [6] paclitaxel [7] and topotecan [8], or novel cytotoxic agents, including oncolytic herpes simplex and adenoviral vectors [9–13], viral and non-viral mediated gene therapy [14–17] and immunotoxins such as IL13-PE38QQR [18], into the tumour mass, resection cavity or peritumoural tissue. To date, the only technique of localised drug delivery that has become clinically accepted is the implantation of carmustine wafers (Gliadel) into the tumour resection cavity. However, a recent Cochrane Collaboration Review of the use of Gliadel wafers concluded that in combination with radiotherapy, Gliadel has survival benefits in the management of primary disease in a “limited number” of patients, but has “no demonstrable survival benefits in patients with recurrent disease” [19].
The principal limitation of many of the techniques of direct chemotherapy delivery to the brain, including Gliadel wafers, is their dependence on diffusion to achieve adequate spatial distribution within the brain. Diffusion is a highly inefficient process for drug distribution as it depends heavily on the infused drug concentration and molecular size of the drug. As a consequence, it is necessary to instil a very high concentration into the brain to generate an adequate concentration gradient which will distribute the drug a significant distance into the tissue.
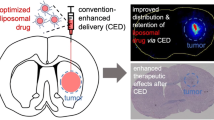
For many chemotherapeutic agents, this source concentration is likely to be toxic to normal brain tissue, leading to significant side-effects. Convection-enhanced delivery (CED) offers an alternative strategy for infusing drugs into the brain. CED utilises implanted intracranial catheters through which drugs are infused at precisely controlled, slow infusion rates. The use of an appropriate catheter, trajectory and infusion rate leads to bulk flow of drug directly into the brain extracellular space [20].
In contrast to techniques of drug delivery to the brain that depend on diffusion, such as Gliadel wafers, which lead to heterogeneous drug distribution over short distances, depending on the size of the drug, CED is capable of distributing drugs, homogeneously, over large volumes of brain, independently of the size of the drug [21].
Whilst preclinical studies confirm that CED is a viable and potentially highly effective approach for administering drugs directly into the brain, it is not appropriate for all drugs. CED bypasses the tight junctions of the blood–brain barrier to allow drug distribution within the brain extracellular space. However, whilst highly lipophilic drugs, such as carmustine [22], may diffuse freely across the blood–brain barrier, other drugs such as paclitaxel may act as substrates to efflux transporters located within the blood–brain barrier, causing these drugs to be rapidly eliminated from the brain [23]. It is therefore essential that in future trials utilising CED, therapeutic agents are carefully selected to ensure that they are retained in the brain for sufficient time for an anti-tumour effect to occur.
Carboplatin is a conventional chemotherapeutic agent that has been administered intravenously to patients with high-grade gliomas in isolation [24, 25] or in combination with erlotinib [26], tamoxifen [27], Gliadel [28], etoposide [29], human tumour-necrosis factor-α [30], thymidine [31], cyclophosphamide [32], RMP-7 [33], ifosfamide [34] and teniposide [35]. Although these trials failed to demonstrate significant evidence of efficacy, carboplatin represents an excellent chemotherapeutic agent for administration by CED. It is a hydrophilic agent, ensuring that it is unable to diffuse freely across the blood–brain barrier and as such it is a substrate for the principal efflux transporters in the blood–brain barrier. As a consequence, direct intracranial administration of carboplatin by CED should result in drug compartmentalisation within the brain. There is also in vivo evidence, from infusions into animal models, demonstrating that carboplatin is highly efficient at killing glioblastoma cells at concentrations that are not toxic to normal brain tissue [36–42]. Whilst some of these trials have had encouraging results, there is no convincing evidence that intravenous carboplatin administration confers significant benefit to patients with high-grade gliomas. However, there is compelling evidence that the concentration of carboplatin achieved within glioma tissue following intravenous administration is sub-therapeutic. Specifically, Whittle et al. demonstrated a peak glioma tissue concentration of just 0.013 mg/ml following high-dose intravenous delivery [43]. Indeed this represents just 40% of the concentration that has been demonstrated, in a meta-analysis of published chemosensitivity assays, to kill 50% of tumour cells (IC50) of carboplatin [37].
In view of the aforementioned data, we hypothesise that carboplatin administered at an appropriate concentration directly into the peritumoural region by CED has the potential to be an efficacious treatment for patients with GBM. This is in contrast to direct intratumoural infusions of carboplatin, which due to grossly abnormal tissue architecture, necrosis and neovascularisation within the tumour, is unlikely to be a practical approach. However, prior to testing this hypothesis in a clinical trial, a number of factors require further evaluation. Firstly, it is feasible that carboplatin is a substrate for efflux transporters within the blood–brain barrier and consequently may have a short half-life within the brain, rendering it inappropriate for direct intracranial delivery. The principal aim of this study was therefore to determine the tissue half-life of carboplatin administered by CED. Secondly, it is possible that due to the binding properties of carboplatin, it would not distribute efficiently by CED. As a consequence, we have evaluated the distribution properties of carboplatin in both rat and pig brain, and assessed coinfusion of the MRI-contrast agent gadolinium-DTPA as a practical means for imaging carboplatin distribution clinically. As CED offers the possibility of producing sustained infusions of carboplatin over hours or even days, we have evaluated the GBM tumour cell kill that can be achieved at a range of carboplatin concentrations and treatment durations in vitro. Finally, we have undertaken a study to assess the toxicity of carboplatin administered by CED over a range of concentrations. It is our intention to utilise the findings from these studies to undertake a phase I/II dose-escalation study of carboplatin administration by CED to treat patients with recurrent GBM.
Materials and methods
In vitro studies
Cell lines and cell culture
Cell lines were kindly provided by Geoffrey Pilkington from the Institute of Biomedical and Biomolecular Sciences at Portsmouth University, UK. The cell lines used in this study were SNB19 (P20-P45) and UPAB (P20-P45).
MTT cytotoxicity assay
Briefly, SNB19 and UPAB glioma cells were plated at 1 × 104/well in a 24-well plate. Cells were treated 72 h later with Carboplatin at the following concentrations: 0.03, 0.06, 0.12, 0.18, 0.24, 0.3, 0.36, and 0.6 mg (TEVA, UK) for 24, 48, 72, or 96 h. Each concentration was repeated four times. Carboplatin was diluted in phosphate buffered saline (PBS; Sigma Aldrich, UK) and added to 0.5 mL culture media. PBS was used as a negative control and puromycin dihydrochloride (10 μg/mL; Sigma Aldrich, UK), which inhibits cell growth by preventing protein synthesis, was used as a positive control. Following the incubation period, culture media was changed. Then 50 μL methylthiazolyl-tetrazolium bromide solution (MTT; Sigma Aldrich, UK; 5 mg/mL) was added to each well and further incubated for 3 h at 37°C in a humidified 5% CO2 atmosphere to allow MTT to form formazan crystals in metabolically active cells. Following this, the media was removed, and the formazan crystals in each well were solubilized with 190 μL of isopropanol (Fisher Scientific, Loughborough, UK) acidified with hydrochloric acid (VWR, Leicestershire, UK). The cell lysate was transferred to a 96-well plate and the absorbance of each well was measured at 570 nm using a Multiskan Ascent plate reader (Thermo Electron Corporation, UK). Results are expressed as a percentage (%) of treated versus untreated cells.
In vivo studies
Rat infusion apparatus and procedures
All acute infusions were undertaken using in-house cannulae [44] and all procedures were carried out in accordance with UK Home Office animal welfare regulations and with appropriate home office licences.
Male Wistar rats (Charles River, UK) were group-housed and allowed to acclimatise prior to experimental procedures. Rats weighing 225–275 g were anaesthetised with an intraperitoneal dose of medetomidine (Dormitor; 0.4 mg/kg; Pfizer Animal Health, Kent, UK) and ketamine (Ketaset; 100 mg/kg; Pfizer, UK) and placed in a stereotactic frame (Stoelting Co, Wood Dale, IL, USA). A linear incision was made between the glabella and the occiput and the skull exposed. Burr holes with a diameter of ~2 mm were drilled 1.0 mm anterior and 2.5 mm lateral to the bregma and cannulae were inserted to a depth of 2.5 mm below the dura. All cannulae were pre-primed with either saline or carboplatin and the desired dose prior to insertion into the brain. Every attempt was made to ensure that no air bubbles were present in the infusion cannula. Infusions of 2.5 μl of carboplatin at specific concentrations (outlined in Table 1) were conducted at a rate of 5 μl/min. Following infusion completion, the cannula was left in situ for 10 min before being withdrawn at a rate of 1 mm/min. The wound was then closed with 5.0 vicryl (Ethicon, Gargrave, UK) a dose of intramuscular buprenorphine was administered (Vetergesic; 0.03 mg/kg; Alstoe Animal Health, York, UK) and the anaesthetic was reversed with an intraperitoneal dose of atipamezole hydrochloride (Antisedan; 5 mg/kg; Pfizer, UK). At predetermined time-points (see Table 1), animals were perfusion fixed with 100 mL of PBS followed by 100 mL of 4% paraformaldehyde (PFA; Fisher Scientific, UK) in PBS (pH 7.4). The brain was then removed from the skull and placed in 4% PFA for 48 h and then cryoprotected in 30% sucrose (Melford Laboratories, Ipswich, UK) in PBS prior to sectioning.
Pig infusion apparatus and procedures
Carboplatin infusions were undertaken into male large white landrace pigs weighing 45 kg using a cannula system developed in-house [44–47]. Pig anaesthesia, head immobilisation and brain imaging were achieved as we have previously described [48]. Infusions of 120 μl 0.03 mg/ml carboplatin mixed with 0.3% (6 μmol/l) Gadolinium-DTPA (Magnevist: Bayer Healthcare, Germany), were undertaken bilaterally into the corona radiata using a cannula composed of a length of fused silica (outer diameter 220 μm, inner diameter 150 μm) bonded to a glass Hamilton syringe. Except for the distal 3 mm, this fused silica tube was supported along its length by a series of zirconia tubes to ensure that it could be accurately inserted to target. Infusions were performed using the following regime: 0.5 μl/min for 5 min, 1 μl/min for 5 min, 2.5 μl/min for 5 min and then 5 μl/min for 20 min. This regime was employed in an attempt to minimise the occurrence of a sudden surge in pressure at the catheter tip due to elasticity in the infusion tubing. 120 μl was infused as this is the largest volume that we have previously infused into pig white matter without leakage into the ventricular system [44]. Following infusion completion, the cannula was left in place for 10 min prior to being withdrawn slowly by hand. CSF leakage from the burr hole and cannula track was sealed with Cerebond prior to wound closure. The animal was then transferred back to the MRI scanner and T1-weighted imaging performed to visualise infusate distribution. Upon the completion of imaging, the animal was transcardially perfused with 5 l of PBS and then 5 l of 10% neutral-buffered formalin at a rate of 500 ml/min using an infusion pump (Masterflex, UK).
Histology
Rat brains were cut into 35 μm thick coronal sections using a Leica CM1850 cryostat (Leica Microsystems, Wetzlar, Germany) at −20°C. For haematoxylin and eosin staining, fixed sections were mounted on gelatine-subbed slides. Sections were submerged in 4% PFA for 20 min, dehydrated and then stained with haematoxylin and eosin (Cell Path, Hemel Hempstead, UK) according to standard protocols. Following this, sections were coverslipped with Pertex mounting medium (Cell Path, UK) and allowed to dry in the fumehood overnight before imaging with a Leica CTR 5500 microscope (Leica Microsystems, Germany). Sections were assessed by light microscopy to ensure that the cannula track in each brain terminated in the corpus callosum. If the cannula track did not terminate in the corpus callosum, the infusion was repeated.
For fluorescent immunohistochemistry, free-floating sections were washed with PBS for 5 min × 3. Sections were then blocked in PBS plus 0.1% triton-x-100 (Sigma Aldrich, UK) containing 10% normal donkey serum (Sigma Aldrich, UK) for 1 h at RT. Sections were then washed with PBS for 5 min. Following washing, sections were incubated in polyclonal rabbit anti-glial fibrillary acidic protein primary antibody (GFAP; 1:300; Millipore, Watford, UK) at 4°C overnight. The next day, primary antibody was removed and sections were washed with PBS for 15 min × 3. Secondary antibody (donkey anti-rabbit Cy3 1:300; Jackson Laboratories, Sacramento, CA, USA) was added to the sections and incubated at RT for 1 h in the dark and then washed with PBS for 15 min × 3. Sections were mounted in Fluorsave mountant (Calbiochem, Germany) before viewing and image capture with a fluorescent microscope (Leica Microsystems, Germany) and digital camera (CX9000 Microbrightfield, VT, USA).
For DiI staining, free-floating sections were washed with PBS for 5 min. Sections were then submerged in a solution of 4′,6-diamidino-2-phenylindole (DAPI, 0.25 mg/ml, Sigma Aldrich, Gillingham, UK) in PBS for 5 min. After three PBS washes, sections were mounted onto gelatine-coated slides and stained with FAST-DiI oil (0.25 mg/ml; Invitrogen, Paisley, UK) diluted in 1:3 N,N,N′,N′-tetramethylethylenediamine (TEMED, Sigma Aldrich, UK) and ddH2O for 2 min. Slides were washed with ddH2O and coverslipped using Fluorsave mountant. Once dry, slides were imaged with a fluorescent microscope (Leica Microsystems, Germany) and digital camera (CX9000 Microbrightfield, VT, USA).
Laser ablation inductively coupled plasma (ICP) mass spectrometry
Samples were placed in a sealed ablation chamber under an argon gas flow. Laser interrogation caused sample vaporisation; ablated material was then transported from the sample cell to the ICP torch via an argon gas flow. Upon reaching the ICP the sample was completely atomised and ionised via high temperature plasma (7500–10000 K). Ions were then focused through a series of sampling cones and ion-lenses before isotopic mass discrimination (via quadrupole) for elements of interest and subsequent detection of ions (as electron multiplier (EM) detector counts).
Resultant data (csv files) was in the form of signal response for each monitored isotope (separate columns) against time; as such, ion-responses could be co-ordinated to form 2D elemental distribution maps, using the Graphis software package (Kylebank Software Ltd, Ayr, UK).
The laser ablation (LA) system was configured to perform multiple, parallel line-rastering of sections. Operating parameters ensured efficient removal of sample (i.e. total consumption of thin section incident to the laser) irrespective of section thickness. Additionally, a distance twice that of the laser beam diameter was used to separate raster lines, to prevent contamination of adjacent section areas with ejected material from previous raster runs.
Main operating parameters for ICP–MS (HP 4500, Agilent Technologies, Cheadle, UK), were: ICP forward power, 1340 W; plasma gas flow, 16 ml/min and auxiliary flow, 1.0 ml/min. Isotopes (13C, 57Fe, 66Zn, 157Gd and 195Pt) were monitored in a time-resolved mode and selected on the basis of high-percentage abundance and minimal isobaric and polyatomic interferences. Integration times for isotopes were 0.1 s (0.05 s for 13C).
Rat brain analysis
The LA system (New Wave UP MACRO, Nd:YAG, 266 nm) was configured to the following parameters: beam diameter, 240 μm; laser energy, 2.2 mJ; line raster rate, 50 μm/sec[1]; laser frequency, 10 Hz. A check standard (0.2 μg/g) was ablated at the beginning and end of each section interrogation in order to verify system stability. Total runtime for mapping individual sections (area 140–160 mm2) was approximately 2 h 30 min.
Matrix-matched standards were prepared as previously described [49], at corresponding thickness to brain sections and contained known amounts of Pt at 0.01, 0.1 and 0.2 μg/g (plus a blank). Standards were placed adjacent to the samples in the ablation chamber and triplicate line rasters (2 mm in length) performed prior to and after brain section analysis, on each standard. LA-ICP-MS conditions were identical to those used for tissue section analysis. Average 195Pt ion-responses of individual rasters were plotted against spiked concentration to yield linear calibration graphs of the form y = mx + c. This permitted distribution maps to be displayed in concentration units.
For determination of average and maximum Pt concentrations, data was processed (using MS Excel) such that all on-tissue Pt signal responses above background levels were included; with the omission of Pt signals in areas co-localising with high-intensity Fe signals. These areas were consistent with small haemorrhages caused by cannula insertion and generally resulted in anomalously high Pt response, likely due to Pt capture in haemorrhagic components.
Pig brain analysis
The LA system (Cetac, LSX-200, Nd:YAG, 266 nm) was configured to the following parameters: beam diameter, 200 μm; laser energy, 0.99 mJ; line raster rate, 65 μm/s; laser frequency, 20 Hz. Total runtime for mapping individual sections (scanned section areas were in the region of 30 mm by 38 mm) was ~ 10 h.
Results
Tissue distribution and half-life of carboplatin following CED into rat brain
Low concentration infusions of carboplatin (0.03 mg/ml) into rat brain led to widespread distribution at 0 h post-infusion. Although all infusions were performed through cannulae implanted into identical coordinates in the corpus callosum as defined by the Paxinos and Watson sereotactic rat brain atlas (1998), variable distribution patterns were observed. Apart from a single infusion analysed at 6 h, platinum was detectable by LA-ICP-MS for up to 24 h. After 24 h, trace levels of platinum were detected in a number of tissue sections. In these sections platinum, colocalised with high levels of iron derived from small haemorrhages along the cannula tracks (Fig. 1). The decrease in carboplatin concentration over time was reflected in measures of average and maximum platinum counts for each section at each time-point (Fig. 2).
Laser ablation ICP mass spectrometry (LA-ICP-MS) following in vivo infusions. Rats were infused with 0.03 mg/ml carboplatin into the corpus callosum. This is represented in the relevant coronal image from the Paxinos and Watson rat brain atlas (top left). The cannula position is demonstrated by the location of the arrow. Rat brains were harvested at time-points of 0, 3, 6, 12, 24, 48, 72 and 168h (7days). Coronal sections at the level of the cannula track were analysed by LA-ICP-MS. Results at each time point (n = 3) are shown in images a–h. The top row of images for each time-point show tissue maps of Pt levels (195Pt) and the lower row of each image show tissue maps of iron levels in each section (57Fe)
Carboplatin toxicity in rat brain
Increasing concentrations of carboplatin were infused into the corpus callosum of rats. Histological examination of brains was undertaken 30 days post-infusion. Concentrations of up to 0.9 mg/ml were well tolerated with no clinical evidence of toxicity and no histological evidence of tissue disruption based on haematoxylin and eosin staining (Fig. 3). Furthermore, Dil staining demonstrated no loss of white matter tract integrity and GFAP immunostaining showed minimal evidence of gliosis in the white matter compared to control infusions of 0.9% saline.
Carboplatin toxicity in vivo. Rat brains were infused with 0.9 (a), 0.6 (b), 0.3 (c), and 0.03 mg/ml (d) of carboplatin. Tissue sections were evaluated at 24, 48 and 72 h and 30 days to assess for evidence of tissue toxicity. Control infusions of 0.9% saline were performed and tissue analysed at 24 h (e) and 30 days (f). Representative images of haematoxylin and eosin staining (left column), GFAP immunostaining (middle column) and the myelin staining (Dil-right column) are shown. No evidence of tissue toxicity was observed at any carboplatin dose compared to controls (scale bar = 500 μm)
In vitro dose response to carboplatin in glioblastoma cell lines
MTT assays in glioblastoma cell lines exposed to carboplatin at different concentrations for increasing durations demonstrated a clear relationship between carboplatin concentration and duration of carboplatin exposure on the percentage of surviving cells compared to controls (Fig. 4). With a 96 h exposure, there was a negligible increase in cell kill (greater than 90%) at concentrations exceeding 0.18 mg/ml. Similarly, with a 72 h exposure, there was a negligible increase in cell kill at concentrations exceeding 0.24 mg/ml. Based on these results the IC50 value of carboplatin, assuming a 96 hour exposure of carboplatin, was between 0.06 and 0.12 mg/ml.
Dose response of glioma cell lines to carboplatin in vitro. a UPAB; b SNB19 glioma cells were exposed to increasing carboplatin concentrations for 24, 48, 72 and 96 h. Cell viability was assessed by MTA (graphs show values for group mean (n = 3) and standard deviation). With a 96 h exposure, there was a negligible increase in cell kill (>90%) at concentrations exceeding 0.18 mg/ml. Similarly, with a 72 h exposure, there was a negligible increase in cell kill at concentrations exceeding 0.24 mg/ml
Gadolinium-DTPA coinfusion to visualise carboplatin distribution by MRI
Gadolinium-DTPA (0.3%; 6 μmol/l) was coinfused with 0.03 mg/ml of carboplatin into the corona radiata of pigs. T1-weighted MR imaging demonstrated a close correlation between contrast-enhancement and carboplatin distribution. LA-ICP-MS was more sensitive than T1-weighted MR scanning at visualising gadolinium distribution and demonstrated that gadolinium-DTPA distributed over a larger volume of brain than carboplatin although widespread carboplatin distribution was observed through the corona radiata (Fig. 5).
Comparison of T1-weighted MR imaging and LA-ICP-MS following coinfusion of carboplatin and gadolinium-DTPA into the corona radiata of a pig. Carboplatin (0.03 mg/ml) was coinfused with gadolinium-DTPA (0.3%; (6 μmol/l) into the corona radiata of a pig bilaterally (a–c: right hemisphere, d–f: left hemisphere). T1-weighted MR images (a and d) and LA-ICP-MS images of 157Gd (b and e) and 195Pt (c and f) distribution on corresponding tissue sections are shown. T1-weighted MR imaging demonstrated a close correlation between contrast-enhancement and carboplatin distribution. LA-ICP-MS was more sensitive than T1-weighted MR scanning at visualising gadolinium distribution and demonstrated that gadolinium-DTPA distributed over a larger volume of brain than carboplatin. (all scale bars = 5 mm)
Discussion
In view of the highly infiltrative properties of malignant gliomas and their subsequent propensity to recur adjacent to tumour resection margins, the rarity of extracranial disease dissemination and the grim prognosis associated with this disease, there is a clear and rationale need to improve local tumour control. This requirement is complicated by the presence of the blood–brain barrier, which limits the access of chemotherapeutic agents into the brain, tumour infiltration into eloquent structures and the intrinsic chemo- and radioresistance of glioblastoma cells. The principal aim of the experiments outlined in this study was to determine whether carboplatin, administered by CED into peritumoural brain, is a potentially feasible treatment to achieve local control of GBM. Specifically, these experiments demonstrate that it is possible to achieve widespread carboplatin distribution by CED and that carboplatin remains in the brain for at least 24 h. Furthermore, we provide evidence from in vitro studies that carboplatin is capable of killing a significant proportion of GBM cells at concentrations that appear to be well-tolerated in the brain in vivo. Finally we demonstrate that coinfusion of gadolinium-DTPA with carboplatin and peri-infusional T1-weighted MRI represents a viable technique for visualising carboplatin distribution in clinical practice. The results of this study have informed the development of a phase I/II clinical trial protocol that we intend to enact in the near-future.
Convection-enhanced delivery of carboplatin into the corpus callosum of rats led to surprisingly variable distribution patterns. Two main patterns were observed with many infusions preferentially distributing through the striatum rather than the corpus callosum. This is likely to have occurred as the corpus callosum is a very shallow structure in rats and subtle variations in cannula tip position, despite using identical stereotactic coordinates, would have led to variable distribution patterns. In particular, if the cannula tip had been implanted fractionally too deep, carboplatin may have distributed into the striatum rather than along the corpus callosum. Attempts to ensure consistent cannula tip targeting in this study included the use of identical stereotactic coordinates for cannula insertion, the use of rats with an identical weight and examining tissue sections prior to undertaking LA-ICP-MS, to ensure that the cannula track was visible and terminated in the corpus callosum. However, in view of the very narrow cannulae employed in these infusions to achieve CED and the fact that brains were not harvested for up to 1 week, it was challenging to identify the cannula trajectory in many cases and this may explain why one 6 h time-point demonstrated no detectable carboplatin. Furthermore there is intrinsic variability with tissue analysis by LA-ICP-MS although regular machine calibration ensured that this was less than 15% [50]. Despite these potential sources of variability, carboplatin was visible in tissue sections that demonstrated preferential distribution in the striatum and in the corpus callosum (Fig. 1e) for at least 24 h. The observation of low levels of carboplatin at time points beyond 48 h and the approximate colocalisation of Pt with areas of iron, most likely reflects binding of carboplatin to serum proteins or haemoglobin at the site of trivial haemorrhages along the cannula track.
The presence of significant concentrations of carboplatin at 24 h is an encouraging finding and supports our hypothesis that due to its hydrophilic nature and subsequent inability to diffuse freely across the blood–brain barrier, carboplatin is an ideal agent to be delivered directly into peritumoural brain. Indeed, these findings are supported by similar clearance times calculated for radiolabelled albumin following injection into the caudate nucleus and internal capsule of rats [51]. Consequently, this relatively prolonged tissue half-life ensures that carboplatin can be distributed over large volumes of brain, despite the low flow-rates that are demanded by CED. Furthermore, this relative compartmentalisation of carboplatin in the brain over many hours should ensure that a clinically significant tumour cell kill is achieved whilst negligible plasma levels of carboplatin are maintained. Indeed, through the use of an implanted catheter system, repeated bolus infusions of carboplatin should facilitate maintenance of a relatively constant carboplatin concentration within the peritumoural tissue for a predetermined period of time.
Having identified that carboplatin remains in the brain for at least 24 h, we examined the relationships between carboplatin concentration and duration of exposure on the tumour cell kill achieved. Unsurprisingly, as the carboplatin concentration and exposure duration were increased, the proportion of tumour cells that were killed increased. This effect appeared to plateau with carboplatin concentrations of 0.18 and 0.24 mg/ml at exposure durations of 96 and 72 h, respectively. Although it is difficult to accurately simulate the effects of cytotoxic agents in vitro, particularly due to the lack of tumour cell heterogeneity, which is a feature of GBM [52], these results imply that using appropriate carboplatin concentrations, a maximal tumour cell kill could be achieved by maintaining a therapeutic carboplatin concentration in peritumoural brain for 3–4 days. In view of the tissue half-life of carboplatin that we have demonstrated in the brain and with the use of an implanted catheter system it should be feasible to effectively administer carboplatin to peritumoural brain for these periods of time in clinical practice. From a practical perspective, this approach would be similar to the phase III clinical trial of the immunotoxin IL13-PE38QQR, which was administered through 2–4 catheters for 96 h, to patients with recurrent glioblastoma [18].
In an attempt to determine whether carboplatin administered by CED was associated with significant toxicity in rats, we undertook a dose-escalation study. This study demonstrated no clinical or histological evidence of toxicity at concentrations of up to 0.9 mg/ml. This result supports previous studies in rats [36] and primates [53] that would suggest that carboplatin can be safely administered into the brain at a potentially efficacious dose. Specifically, Degen et al. undertook single infusions of carboplatin into the brainstem of rats at concentrations as high as 1 mg/ml without histological evidence of tissue damage [36], and Strege et al. undertook one-month long infusions into the brainstem of primates at a dose of 0.075 mg/kg with minimal clinical evidence of toxicity, manifesting as slight slowing of the animal’s movements [53]. In view of our in vitro results demonstrating an optimal tumour cell kill following prolonged infusions over several days; our toxicity study is limited by the fact that single infusions were performed. Ideally, we would have liked to have replicated infusions of 0.24 mg/ml over 72 h and 0.18 mg/ml over 96 h. However, whereas a clinical trial could employ short CED-based bolus infusions at intervals to achieve a steady-state concentration in the brain, due to the small size of the rat brain, continuous, low-rate infusions would need to be performed. These infusions would most likely have led to a toxic build-up of carboplatin in the brain, particularly around the catheter tip, at potentially much higher concentrations than the infused concentration. Consequently, undertaking continuous infusions into rat brain could have led to misrepresentative toxicity data and therefore they were not performed.
A key consideration in the application of CED in clinical trials is the need to visualise infusate distribution to ensure that adequate drug distribution is achieved through the intended target volume. A simple strategy that has previously been employed in clinical practice is the coinfusion of an MR contrast agent such as gadolinium-DTPA [54]. As gadolinium is detectable by LA-ICP-MS, it was possible to evaluate the differential distribution properties of gadolinium-DTPA and carboplatin in the brain of a large animal model in which in vivo T1-weighted MR imaging could be performed. It is perhaps unsurprising that more widespread distribution of gadolinium was demonstrated with LA-ICP-MS compared to T1-weighted MRI, in view of the greater sensitivity of the former technique. Nevertheless, from the perspective of undertaking a clinical trial, it was encouraging that the area of contrast-enhancement on T1-weighted MR imaging approximately matched carboplatin distribution determined by LA-ICP-MS. Although, CED should lead to homogenous infusate distribution this was not the case with gadolinium-DTPA distribution visualised by LA-ICP-MS, presumably due to the ability of gadolinium-DTPA to diffuse through the brain extracellular space. Consequently, for future trials involving the administration of gadolinium-DTPA, the effect of modulating the infused concentration on the visualisation of contrast-enhancement by MRI would be invaluable.
We have utilised the results of this study to develop a regulatory-approved clinical trial protocol [55]. This clinical trial will be a phase I/II dose-escalation study with infused carboplatin concentrations ranging from 0.03 to 0.18 mg/ml administered through four catheters. Patients will receive infusions for 8 h a day for three consecutive days. It is our view that with existing data, this dosing regime provides the optimum balance between achieving a maximal therapeutic effect and minimising the risks of encountering significant toxicity.
In conclusion, this study provides experimental evidence that carboplatin can be efficiently administered into the brain by CED. In addition, due to its slow clearance from the brain and toxicity to glioblastoma cells at concentrations that are not toxic to normal brain, carboplatin administration by CED into peritumoural brain represents a promising therapeutic approach to treating patients with recurrent glioblastoma multiforme.
References
Deorah S, Lynch CF, Sibenaller ZA, Ryken TC (2006) Trends in brain cancer incidence and survival in the United States: surveillance, epidemiology, and end results program, 1973 to 2001. Neurosurg Focus 20:E1
Wallner KE, Galicich JH, Krol G, Arbit E, Malkin MG (1989) Patterns of failure following treatment for glioblastoma multiforme and anaplastic astrocytoma. Int J Radiat Oncol Biol Phys 16:1405–1409
Dobelbower MC, Burnett III OL, Nordal RA, Nabors LB, Markert JM, Hyatt MD, Fiveash JB (2011) Patterns of failure for glioblastoma multiforme following concurrent radiation and temozolomide. J Med Imaging Radiat Oncol 55:77–81
Oh J, Sahgal A, Sanghera P, Tsao MN, Davey P, Lam K, Symons S, Aviv R, Perry JR (2011) Glioblastoma: patterns of recurrence and efficacy of salvage treatments. Can J Neurol Sci 38:621–625
Stewart L, Burdett S (2002) Glioma meta-analysis trialists group (GMT). Chemotherapy for high-grade glioma. The Cochrane Collaboration
Westphal M, Hilt DC, Bortey E, Delavault P, Olivares R, Warnke PC, Whittle IR, Jaaskelainen J, Ram Z (2003) A phase 3 trial of local chemotherapy with biodegradable carmustine (BCNU) wafers (Gliadel wafers) in patients with primary malignant glioma. Neuro Oncol 5:79–88
Lidar Z, Mardor Y, Jonas T, Pfeffer R, Faibel M, Nass D, Hadani M, Ram Z (2004) Convection-enhanced delivery of paclitaxel for the treatment of recurrent malignant glioma: a phase I/II clinical study. J Neurosurg 100:472–479
Grahn AY, Bankiewicz KS, Dugich-Djordjevic M, Bringas JR, Hadaczek P, Johnson GA, Eastman S, Luz M (2009) Non-PEGylated liposomes for convection-enhanced delivery of topotecan and gadodiamide in malignant glioma: initial experience. J Neurooncol 95:185–197
Chiocca EA, Abbed KM, Tatter S, Louis DN, Hochberg FH, Barker F, Kracher J, Grossman SA, Fisher JD, Carson K, Rosenblum M, Mikkelsen T, Olson J, Markert J, Rosenfeld S, Nabors LB, Brem S, Phuphanich S, Freeman S, Kaplan R, Zwiebel J (2004) A phase I open-label, dose-escalation, multi-institutional trial of injection with an E1B-attenuated adenovirus, ONYX-015, into the peri tumoral region of recurrent malignant gliomas, in the adjuvant setting. Mol Ther 10:958–966
Harrow S, Papanastassiou V, Harland J, Mabbs R, Petty R, Fraser M, Hadley D, Patterson J, Brown SM, Rampling R (2004) HSV1716 injection into the brain adjacent to tumour following surgical resection of high-grade glioma: safety data and long-term survival. Gene Ther 11:1648–1658
Markert JM, Medlock MD, Rabkin SD, Gillespie GY, Todo T, Hunter WD, Palmer CA, Feigenbaum F, Tornatore C, Tufaro F, Martuza RL (2000) Conditionally replicating herpes simplex virus mutant, G207 for the treatment of malignant glioma: results of a phase I trial. Gene Ther 7:867–874
Papanastassiou V, Rampling R, Fraser M, Petty R, Hadley D, Nicoll J, Harland J, Mabbs R, Brown M (2002) The potential for efficacy of the modified (ICP 34.5(-)) herpes simplex virus HSV1716 following intratumoural injection into human malignant glioma: a proof of principle study. Gene Ther 9:398–406
Rampling R, Cruickshank G, Papanastassiou V, Nicoll J, Hadley D, Brennan D, Petty R, MacLean A, Harland J, McKie E, Mabbs R, Brown M (2000) Toxicity evaluation of replication-competent herpes simplex virus (ICP 34.5 null mutant 1716) in patients with recurrent malignant glioma. Gene Ther 7:859–866
Chiocca EA, Smith KM, McKinney B, Palmer CA, Rosenfeld S, Lillehei K, Hamilton A, DeMasters BK, Judy K, Kirn D (2008) A phase I trial of Ad.hIFN-beta gene therapy for glioma. Mol Ther 16:618–626
Lang FF, Bruner JM, Fuller GN, Aldape K, Prados MD, Chang S, Berger MS, McDermott MW, Kunwar SM, Junck LR, Chandler W, Zwiebel JA, Kaplan RS, Yung WK (2003) Phase I trial of adenovirus-mediated p53 gene therapy for recurrent glioma: biological and clinical results. J Clin Oncol 21:2508–2518
Rainov NG (2000) A phase III clinical evaluation of herpes simplex virus type 1 thymidine kinase and ganciclovir gene therapy as an adjuvant to surgical resection and radiation in adults with previously untreated glioblastoma multiforme. Hum Gene Ther 11:2389–2401
Yoshida J, Mizuno M, Fujii M, Kajita Y, Nakahara N, Hatano M, Saito R, Nobayashi M, Wakabayashi T (2004) Human gene therapy for malignant gliomas (glioblastoma multiforme and anaplastic astrocytoma) by in vivo transduction with human interferon beta gene using cationic liposomes. Hum Gene Ther 15:77–86
Kunwar S, Chang S, Westphal M, Vogelbaum M, Sampson J, Barnett G, Shaffrey M, Ram Z, Piepmeier J, Prados M, Croteau D, Pedain C, Leland P, Husain SR, Joshi BH, Puri RK (2010) Phase III randomized trial of CED of IL13-PE38QQR vs Gliadel wafers for recurrent glioblastoma. Neuro Oncol 12:871–881
Hart MG, Grant R, Garside R, Rogers G, Somerville M, Stein K (2008) Chemotherapeutic wafers for high grade glioma. Cochrane Database Syst Rev, CD007294
Chen MY, Lonser RR, Morrison PF, Governale LS, Oldfield EH (1999) Variables affecting convection-enhanced delivery to the striatum: a systematic examination of rate of infusion, cannula size, infusate concentration, and tissue-cannula sealing time. J Neurosurg 90:315–320
Bobo RH, Laske DW, Akbasak A, Morrison PF, Dedrick RL, Oldfield EH (1994) Convection-enhanced delivery of macromolecules in the brain. Proc Natl Acad Sci U S A 91:2076–2080
Fleming AB, Saltzman WM (2002) Pharmacokinetics of the carmustine implant. Clin Pharmacokinet 41:403–419
Begley DJ (2004) ABC transporters and the blood-brain barrier. Curr Pharm Des 10:1295–1312
Gruber ML, Glass J, Choudhri H, Nirenberg A (1998) Carboplatin chemotherapy before irradiation in newly diagnosed glioblastoma multiforme. Am J Clin Oncol 21:338–340
Prados MD, Warnick RE, Mack EE, Chandler KL, Rabbitt J, Page M, Malec M (1996) Intravenous carboplatin for recurrent gliomas. A dose-escalating phase II trial. Am J Clin Oncol 19:609–612
De Groot JF, Gilbert MR, Aldape K, Hess KR, Hanna TA, Ictech S, Groves MD, Conrad C, Colman H, Puduvalli VK, Levin V, Yung WK (2008) Phase II study of carboplatin and erlotinib (Tarceva, OSI-774) in patients with recurrent glioblastoma. J Neurooncol 90:89–97
Tang P, Roldan G, Brasher PM, Fulton D, Roa W, Murtha A, Cairncross JG, Forsyth PA (2006) A phase II study of carboplatin and chronic high-dose tamoxifen in patients with recurrent malignant glioma. J Neurooncol 78:311–316
Limentani SA, Asher A, Heafner M, Kim JW, Fraser R (2005) A phase I trial of surgery, Gliadel wafer implantation, and immediate postoperative carboplatin in combination with radiation therapy for primary anaplastic astrocytoma or glioblastoma multiforme. J Neurooncol 72:241–244
Franceschi E, Cavallo G, Scopece L, Paioli A, Pession A, Magrini E, Conforti R, Palmerini E, Bartolini S, Rimondini S, Esposti RD, Crino L (2004) Phase II trial of carboplatin and etoposide for patients with recurrent high-grade glioma. Br J Cancer 91:1038–1044
Yamamoto M, Oshiro S, Tsugu H, Hirakawa K, Ikeda K, Soma G, Fukushima T (2002) Treatment of recurrent malignant supratentorial astrocytomas with carboplatin and etoposide combined with recombinant mutant human tumor necrosis factor-alpha. Anticancer Res 22:2447–2453
Robins HI, Chang SM, Prados MD, Yung WK, Hess K, Schiff D, Greenberg H, Fink K, Nicolas K, Kuhn JG, Cloughesy T, Junck L, Mehta M (2002) A phase II trial of thymidine and carboplatin for recurrent malignant glioma: a North American Brain Tumor Consortium Study. Neuro Oncol 4:109–114
Vinolas N, Gil M, Verger E, Villa S, Pujol T, Ceral L, Garcia M, Graus F (2002) Pre-irradiation semi-intensive chemotherapy with carboplatin and cyclophosphamide in malignant glioma: a phase II study. Anticancer Drugs 13:163–167
Prados MD, Schold SJS, Fine HA, Jaeckle K, Hochberg F, Mechtler L, Fetell MR, Phuphanich S, Feun L, Janus TJ, Ford K, Graney W (2003) A randomized, double-blind, placebo-controlled, phase 2 study of RMP-7 in combination with carboplatin administered intravenously for the treatment of recurrent malignant glioma. Neuro Oncol 5:96–103
Lopez-Aguilar E, Sepulveda-Vildosola AC, Rivera-Marquez H, Cerecedo-Diaz F, Hernandez-Contreras I, Ramon-Garcia G, Diegoperez-Ramirez J, Santacruz-Castillo E (2000) Preirradiation ifosfamide, carboplatin, and etoposide for the treatment of anaplastic astrocytomas and glioblastoma multiforme: a phase II study. Arch Med Res 31:186–190
Brandes AA, Rigon A, Zampieri P, Ermani M, Carollo C, Altavilla G, Turazzi S, Chierichetti F, Florentino MV (1998) Carboplatin and teniposide concurrent with radiotherapy in patients with glioblastoma multiforme: a phase II study. Cancer 82:355–361
Degen JW, Walbridge S, Vortmeyer AO, Oldfield EH, Lonser RR (2003) Safety and efficacy of convection-enhanced delivery of gemcitabine or carboplatin in a malignant glioma model in rats. J Neurosurg 99:893–898
Wolff JE, Trilling T, Molenkamp G, Egeler RM, Jurgens H (1999) Chemosensitivity of glioma cells in vitro: a meta analysis. J Cancer Res Clin Oncol 125:481–486
Yang W, Huo T, Barth RF, Gupta N, Weldon M, Grecula JC, Ross BD, Hoff BA, Chou TC, Rousseau J, Elleaume H (2011) Convection enhanced delivery of carboplatin in combination with radiotherapy for the treatment of brain tumors. J Neurooncol 101:379–390
Kondo A, Goldman S, Lulla RR, Mania-Farnell B, Vanin EF, Sredni ST, Rajaram V, Soares MB, Tomita T (2009) Longitudinal assessment of regional directed delivery in a rodent malignant glioma model. J Neurosurg Pediatr 4:592–598
Tange Y, Kondo A, Egorin MJ, Mania-Farnell B, Daneriallis GM, Nakazaki H, Sredni ST, Rajaram V, Goldman S, Soares MB, Tomita T (2009) Interstitial continuous infusion therapy in a malignant glioma model in rats. Childs Nerv Syst 25:655–662
Rousseau J, Boudou C, Barth RF, Balosso J, Esteve F, Elleaume H (2007) Enhanced survival and cure of F98 glioma-bearing rats following intracerebral delivery of carboplatin in combination with photon irradiation. Clin Cancer Res 13:5195–5201
Thomale UW, Tyler B, Renard V, Dorfman B, Chacko VP, Carson BS, Haberl EJ, Jallo GI (2009) Neurological grading, survival, MR imaging, and histological evaluation in the rat brainstem glioma model. Childs Nerv Syst 25:433–441
Whittle IR, Malcolm G, Jodrell DI, Reid M (1999) Platinum distribution in malignant glioma following intraoperative intravenous infusion of carboplatin. Br J Neurosurg 13:132–137
White E, Bienemann A, Malone J, Megraw L, Bunnun C, Wyatt M, Gill S (2011) An evaluation of the relationships between catheter design and tissue mechanics in achieving high-flow convection-enhanced delivery. J Neurosci Methods 199:87–97
White E, Bienemann A, Megraw L, Bunnun C, Gill S (2011) Evaluation and optimization of the administration of a selectively replicating herpes simplex viral vector to the brain by convection-enhanced delivery. Cancer Gene Ther 18:358–369
White E, Bienemann A, Sena-Esteves M, Taylor H, Bunnun C, Castrique E, Gill S (2011) Evaluation and optimization of the administration of recombinant adeno-associated viral vectors (serotypes 2/1, 2/2, 2/rh8, 2/9, and 2/rh10) by convection-enhanced delivery to the striatum. Hum Gene Ther 22:237–251
White E, Woolley M, Bienemann A, Johnson DE, Wyatt M, Murray G, Taylor H, Gill SS (2011) A robust MRI-compatible system to facilitate highly accurate stereotactic administration of therapeutic agents to targets within the brain of a large animal model. J Neurosci Methods 195:78–87
White E, Woolley M, Bienemann A, Johnson DE, Wyatt M, Murray G, Taylor H, Gill SS (2010) A robust MRI-compatible system to facilitate highly accurate stereotactic administration of therapeutic agents to targets within the brain of a large animal model. J Neurosci Methods
Pugh JAT, Cox AG, McLeod CW, Bunch J, Whitby B, Gordon B, Kalber T, White E (2011) A novel calibration strategy for analysis and imaging of biological thin sections by laser ablation inductively coupled plasma mass spectrometry. J Anal At Spectrom, 1667–1673
Becker JS, Zoriy M, Matusch A, Wu B, Salber D, Palm C (2010) Bioimaging of metals by laser ablation inductively coupled plasma mass spectrometry (LA-ICP-MS). Mass Spectrom Rev 29:156–175
Szentistvanyi I, Patlak CS, Ellis RA, Cserr HF (1984) Drainage of interstitial fluid from different regions of rat brain. Am J Physiol 246:F835–F844
Shapiro JR, Yung WK, Shapiro WR (1981) Isolation, karyotype, and clonal growth of heterogeneous subpopulations of human malignant gliomas. Cancer Res 41:2349–2359
Strege RJ, Liu YJ, Kiely A, Johnson RM, Gillis EM, Storm P, Carson BS, Jallo GI, Guarnieri M (2004) Toxicity and cerebrospinal fluid levels of carboplatin chronically infused into the brainstem of a primate. J Neurooncol 67:327–334
Lonser RR, Schiffman R, Robison RA, Butman JA, Quezado Z, Walker ML, Morrison PF, Walbridge S, Murray GJ, Park DM, Brady RO, Oldfield EH (2007) Image-guided, direct convective delivery of glucocerebrosidase for neuronopathic Gaucher disease. Neurology 68:254–261
White E, Bienemann A, Taylor H, Hopkins K, Cameron A, Gill S (2011) A phase I trial of carboplatin administered by convection-enhanced delivery to patients with recurrent/progressive glioblastoma multiforme. Contemp Clin Trials
Acknowledgments
The authors acknowledge the financial assistance of the Cure Parkinson’s Trust and the Friends of the Bristol Oncology and Haematology Centre. We also kindly acknowledge the support of Roy Harris for his engineering expertise.
Conflict of interest
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
White, E., Bienemann, A., Pugh, J. et al. An evaluation of the safety and feasibility of convection-enhanced delivery of carboplatin into the white matter as a potential treatment for high-grade glioma. J Neurooncol 108, 77–88 (2012). https://doi.org/10.1007/s11060-012-0833-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-012-0833-4