Abstract
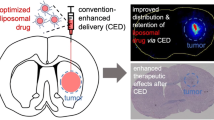
Convection-enhanced delivery (CED) of highly stable PEGylated liposomes encapsulating chemotherapeutic drugs has previously been effective against malignant glioma xenografts. We have developed a novel, convectable non-PEGylated liposomal formulation that can be used to encapsulate both the topoisomerase I inhibitor topotecan (topoCED™) and paramagnetic gadodiamide (gadoCED™), providing an ideal basis for real-time monitoring of drug distribution. Tissue retention of topoCED following single CED administration was significantly improved relative to free topotecan. At a dose of 10 μg (0.5 mg/ml), topoCED had a half-life in brain of approximately 1 day and increased the area under the concentration–time curve (AUC) by 28-fold over free topotecan (153.8 vs. 5.5 μg day/g). The combination of topoCED and gadoCED was found to co-convect well in both naïve rat brain and malignant glioma xenografts (correlation coefficients 0.97–0.99). In a U87MG cell assay, the 50% inhibitory concentration (IC50) of topoCED was approximately 0.8 μM at 48 and 72 h; its concentration–time curves were similar to free topotecan and unaffected by gadoCED. In a U87MG intracranial rat xenograft model, a two-dose CED regimen of topoCED co-infused with gadoCED greatly increased median overall survival at dose levels of 0.5 mg/ml (29.5 days) and 1.0 mg/ml (33.0 days) vs. control (20.0 days; P < 0.0001 for both comparisons). TopoCED at higher concentrations (1.6 mg/ml) co-infused with gadoCED showed no evidence of histopathological changes attributable to either agent. The positive results of tissue pharmacokinetics, co-convection, cytotoxicity, efficacy, and lack of toxicity of topoCED in a clinically meaningful dose range, combined with an ideal matched-liposome paramagnetic agent, gadoCED, implicates further clinical applications of this therapy in the treatment of malignant glioma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma multiforme (GBM) remains one of the most difficult CNS neoplasms to treat despite intensive multimodal therapy. Patients with GBM have a median survival of 12–15 months with surgical resection, radiation and the addition of systemic chemotherapy and only few patients survive for more than 2 years [1]. The median survival for patients with recurrent GBM is approximately 6 months [2].
Topotecan (TPT) is a topoisomerase I inhibitor that is well established for the treatment of several systemic cancers including ovarian and small-cell lung cancer. Significant activity of TPT in treating malignant gliomas has been reported [3]. TPT induced a marked growth inhibition in several human glioma cell lines in vitro [4, 5], and an apparent supra-additive effect of TPT on ionizing radiation-induced cytotoxicity was observed in human GBM cells [4]. Furthermore, TPT showed synergistic activity with temozolomide in vitro through upregulation of topoisomerase I in glioma cell lines [6]. Based on these findings, TPT was tested in a number of clinical studies as a systemic agent combined with radiotherapy [7–11]; or paclitaxel [12]. Overall, the results of these studies suggest that delivering a large enough concentration of systemic TPT to kill the tumor cells results in unacceptable toxicity.
The observed lack of efficacy is commonly believed to be primarily due to poor penetration of TPT across the blood–brain barrier. The blood–brain barrier is disrupted at the core of the tumor allowing most systemically delivered chemotherapy agents access to the mostly inactive center of the tumor, but the barrier remains intact at the growing tumor margin. It has been clinically observed that 90% of malignant gliomas recur within 2 cm of an original resection site [13].
A strategy to overcome the blood–brain barrier is a direct intracerebral infusion approach called convection-enhanced delivery (CED). CED employs a positive pressure generating a local pressure gradient to distribute agents, including therapeutic macromolecules, in the extra-cellular space. Unlike diffusion, CED is not significantly influenced by the concentration, molecular weight or particle size of the agent. In addition, CED leads to reproducible distribution within a given target tissue and results in high and homogeneous drug concentrations throughout the volume of distribution (Vd) [14–16].
Bypassing the blood–brain barrier, CED allows tumors and other target tissues to be exposed to concentrations of TPT that could not be achieved following systemic application, while providing a much wider distribution of the therapeutic agent across the target site than with simple diffusion [17, 18]. At the same time, it minimizes systemic exposure and can therefore be expected to be associated with fewer systemic side effects [14]. Since its introduction, CED has shown considerable promise for the treatment of brain tumors with active agents in phase II and III clinical trials [19].
Liposomal carriers have been shown to provide stable encapsulation for various anticancer drugs and offer distinct advantages over unencapsulated agents [18, 20]. Liposomes are microscopic phospholipid nanoparticles with a bilayered membrane structure surrounding an aqueous core that can be used to encapsulate small molecules. Preclinical studies of liposome-encapsulated camptothecin drugs given via CED have shown improvement in the sustained release of the drug, with prolongation of the drug’s half-life leading to increased exposure of tumor cells to the agent, while increasing the therapeutic index compared to free drug [20–22]. Saito and colleagues showed athymic nude rats implanted with U87MG human glioma cells survived significantly longer when they were treated by CED with PEGylated nanoparticle liposome-encapsulated TPT (nLs-TPT) as compared to free TPT or empty control liposomes [21]. Similar observations of a significant survival benefit as compared to free drug or empty control liposomes delivered by CED were made in the same tumor model with PEGylated liposome-encapsulated CPT-11 (irinotecan), another topoisomerase I inhibitor [22]. Hence, there is good consistency within the class of topoisomerase I inhibitors for both anti-glioma activity and the positive impact on efficacy of PEGylated liposomal encapsulation when delivered by CED.
Surface PEGylation of liposomes leads to steric stabilization and is generally thought to reduce the immunogenicity of the vesicles and prolong their circulation in blood [23]. However, it has recently been demonstrated that PEGylated liposomes may induce complement activation which cannot only lead to accelerated blood clearance of the vesicles upon repeated injection [24], but can also cause complement activation-related pseudoallergy (CARPA), an acute and potentially life-threatening Type I hypersensitivity reaction [25, 26]. Therefore, there is a strong rationale for the development of a non-PEGylated liposomal formulation that is suitable for use in a targeted delivery setting such as CED, which effectively bypasses the bloodstream but requires minimized tissue affinity [27].
One of the challenging aspects of CED in clinical trials is the real-time assessment of drug distribution to visualize tumor coverage and maximize therapeutic effect. Liposomal carriers loaded with gadodiamide (GD) have shown the feasibility and accuracy of monitoring CED over time both in tumor and in normal brain using magnetic resonance imaging (MRI) in a rat glioma model [28, 29]. Liposomal encapsulation extends the half-life of GD to allow visualization up to 72 h [29]. Real-time MRI provides for accurate calculation of Vd within anatomical structures and the future ability to correlate the concentration of co-convected liposomal encapsulated therapeutic agents [30]. Moreover, image-guided CED with liposome-encapsulated GD allows for real-time alterations in delivery of liposome-encapsulated therapeutic agents, targeting the procedure to the pathologically altered brain anatomy caused by CNS tumors [31].
Critical to the accuracy of tracking a drug during CED with an imaging tracer is the expression of similar properties of drug and tracer, including molecular weight, metabolic degradation in the interstitial space, diffusivity and receptor binding [32]. We evaluated several non-PEGylated liposomal formulations of TPT, determining an optimal formulation designated topoCED™. The same unique liposomal formulation has been used to encapsulate GD, designated gadoCED™, providing a topoCED-compatible imaging tracer.
In this study, we report the statistically highly significant efficacy of topoCED co-infused by CED with the matching MRI imaging tracer gadoCED in a U87MG xenograft rat glioma model. The efficacy results are supported by a substantial pharmacokinetic advantage of topoCED over free TPT as well as the excellent cytotoxic potency of topoCED with or without adjunct gadoCED. In addition, we report the combined agents co-convect well in naïve rat brain and tumor-bearing rat brain with no evidence of toxicity induced by either agent.
Materials and methods
Test articles
Free TPT formulations were obtained from GlaxoSmithKline (Research Triangle Park, NC, USA) and Hisun Pharmaceuticals (Taizhou City, Zhejiang, China). Empty control liposomes and drug loaded liposomes were prepared by Northern Lipids Inc (NLI), Burnaby, BC, Canada. Control liposomes, not loaded with drug, were composed of distearoylphosphatidylcholine (DSPC), distearoylphosphatidylglycerol (DSPG) and cholesterol (chol) in the molar ratio of 7:2:1 and a target size of 75–120 nm. Liposomes were prepared by dissolution of all lipids in t-butanol/ethanol/water (45:45:10, vol/vol) heated to 70°C then added to a 250 mM solution of ammonium sulphate to generate multilamellar vesicles (MLVs). The MLVs were maintained at 70°C and extruded through a thermobarrel extruder with 4-stacked polycarbonate filters (Lipex Biomembranes Inc, Vancouver, CAN) with 80 nm pores to yield large unilamellar vesicles (LUVs) with a mean diameter of 75–120 nm as determined by quasi-elastic light scattering using a Nicomp 380 ZLS (Nicomp, Santa Barbara, CA, USA) particle sizer following each pass through the extruder. The LUVs were then diluted with histidine saline pH 6.0 buffer to a concentration of 5% solvent as the LUVs were unstable below their phase transition temperature of 55°C in 10% solvent. The LUVs were then concentrated to approximately 50 mg/ml total lipid by ultrafiltration and subsequently diafiltered against 10 wash volumes of 10 mM histidine, 145 mM NaCl buffer to remove the solvent and exchange the external buffer from ammonium sulphate to pH 6.0 histidine buffer. This buffer exchange resulted in the generation of a transmembrane pH gradient that was used to allow drug loading.
Research or good laboratory practice (GLP) grade TPT, Hisun Pharmaceuticals (Taizhou City, Zhejiang, China), was loaded into the liposomes by addition of a 10 mg/ml solution of TPT in water via a peristaltic pump (Masterflex, Cole-Palmer, Vernon Hills, IL, USA) to a heated (60°C) suspension of LUV (16.6 mg/ml) in 10 mM histidine, 145 mM sodium chloride (NaCl) buffer and water. TPT concentrations of 0.67 and 2.0 mg/ml in 5 mM histidine, 145 mM NaCl, pH 6.0, with a 0.1 and 0.3 (w/w) drug:lipid (D:L) ratio were respectively targeted assuming a 90–95% drug encapsulation efficiency. The TPT formulation of 0.3 D:L ratio was designated topoCED. A constant total lipid concentration target of 6.7 mg/ml was to be maintained in both formulations. Following drug loading, the un-encapsulated TPT was removed by diafiltration employing 5-wash volumes of a 5 mM histidine, 300 mM sucrose pH 6.0 buffer, which also exchanged the external buffer from NaCl solution to sucrose which acted as a cryo-protectant to allow freezing the formulation without changing its physical characteristics. After diafiltration the TPT concentration was determined by high-performance liquid chromatography (HPLC) analysis and the product was diluted to approximately 2.1 mg/ml. The diluted product was warmed to 50°C and passed through a clarifying cellulose acetate filter and then sterile filtered through two 0.2 μm sterilizing grade filters (Sartobran P, Sartorius AG, Goettingen, GER) at 35 psi nitrogen pressure connected in series and collected in a sterile vessel in an aseptic environment. The product was aseptically sampled and the TPT content determined by HPLC analysis. If required, the product was aseptically diluted with sterile histidine sucrose buffer to a TPT concentration of 2.0 mg/ml. The product was then vialed and frozen.
GD for liposomal loading was obtained from Beijing SHLHT Science & Trade (Beijing, China) for research grade material or Estech Pharma, Ansan-Si, Gyeonggi-Do, Korea for GLP grade material. Liposomal GD (gadoCED) was prepared similarly to topoCED, except that the GD was passively encapsulated in the liposomes. Following removal of un-encapsulated GD and solvents by diafiltration, the final GD encapsulation was ≥90%. The target GD content was 5.0 mg/ml ± 10% and a particle size range of 75–120 nm.
Test articles of Ls-TPT were to be stored frozen (−20 to −30°C), and Ls-GD was to be stored refrigerated (2–8°C). Both formulations were stored protected from light. Research grade material was used only for the tissue pharmacokinetic experiment, all others utilized GLP material. Dosing solutions were to be prepared fresh on the day of dosing and kept at room temperature. Appropriate dilutions with 5 mM histidine, 145 mM NaCl pH 6.0, 300 mM sucrose (for tissue pharmacokinetics), or 0.9% saline (all other tests), of stock solution were to be performed to yield the desired concentrations. Fresh vials of the stock test article solution were to be used on each dosing day.
Tissue pharmacokinetics
Adult male Sprague-Dawley rats (Harlan, Indianapolis, IN) weighing 250–350 g were housed under aseptic conditions (Explora BioLabs, LaJolla, CA, USA). The protocol was approved by the Institutional Animal Care and Use Committee at Explora BioLabs. Each animal was given a single 20 μl infusion by CED bilaterally into the striatal region of the brain of TPT as 0.5 mg/ml in three liposomal formulations or free TPT (Hisun Pharmaceuticals). The three TPT liposomal formulations prepared by NLI were: DSPC/Chol 0.1 (w/w) D:L ratio; DSPC/DSPG/Chol 0.3 (w/w) D:L ratio (topoCED); DSPC/DSPG/Chol 0.1 (w/w) D:L ratio. The three liposomal formulations were co-infused with gadodiamide at 1.15 mg/ml in a liposome formulation. The animals (n = 3 per group) were sacrificed at 1 and 6 h, 2, 4 and 7 days. The brains were removed, placed on ice, the striata dissected using a dorsal approach and the tissue frozen in liquid nitrogen. Equal volume of ice cold water (1:1 w/w) was added and the thawed tissue was homogenized (Biospec Products Inc., Bartleville, OK, USA) mechanically for 2 min and frozen. The frozen homogenate was shipped to NLI for analysis.
Two hundred microliters of the thawed homogenate samples were transferred to an Eppendorf tube containing 800 μl of cold methanol (1:4) and centrifuged at 12,000 rpm for 2–5 min. The supernatant solution, 200 μl was placed in an autosampler vial for immediate analysis (or stored at −70°C until analysis up to 3 months later). Analysis was done by NLI using a validated reversed phase HPLC method. Standards were freshly prepared by extraction of spiked blank tissue for the lactone form utilizing methanol:water:trifluoroacetic acid (40:60:0.02) and for the carboxylate form, 20 mM borate buffer: Methanol (60:40) as the diluents. Analysis was conducted on a Waters 2690/5 Separation Module and Empower software HPLC system with a C18 reverse-phase silica column [Phenomenex Inc. Luna C-18(2) column, 250 mm × 4.6 mm inner diameter, 5 μm particle size, ambient temperature] preceded by a C18 security guard cartridge (Phenomenex Inc., 4 × 3.0 mm). Samples were placed in an autosampler tray at 5 ± 3°C, a sample injection volume of 30–50 μl was used, and the column was eluted at a flow rate of 1.0 ml/min with a mobile phase consisting of mobile phase A: 3% triethylamine acetic acid buffer, pH 5.5, (TEAA) and mobile phase B: acetonitrile:3% TEAA (50:50). Gradient elution initial 78:22 A:B to 50:50 A:B in 5 min, held 3 min, back to initial in 0.5 min, total run time 15 min. TPT detected by a Waters 2475 Multi λ fluorescence detector (excitation 380 nm, emission 520 nm). Typical retention time for TPT carboxylate and lactone forms were 5.5 and 7.5 min, respectively. Total TPT was determined by addition of the concentrations of the carboxylate and lactone forms.
Pharmacokinetic parameters that included tissue half-lives (t1/2) of the drug, and area under the concentration–time curve (AUC) were all determined by noncompartmental pharmacokinetics data analysis utilizing WinNonlin 5.0 (Pharsight Corporation, Mountain View, CA, USA).
Tumor cell lines
Human glioblastoma multiforme cell line U87MG was used for in vivo and xenograft implant experiments and obtained from the Brain Tumor Research Center Tissue Bank at University of California, San Francisco. The cells were established in T175 Falcon flasks (BD Bioscience, San Jose, CA, USA). Cells were maintained as monolayers in Eagle’s minimal essential medium supplemented with 10% fetal calf serum, antibiotics (streptomycin 100 ug/ml, penicillin 100 U/ml), and nonessential amino acids. Cells were cultured at 37°C in a humidified atmosphere of 95% air and 5% carbon dioxide. Cells were to be harvested on the day of tumor inoculation surgery and adjusted to a concentration of 50,000–100,000 cells/μl.
Cell cytotoxicity assay
Cells from the U87MG cell line above were seeded at 10,000 cells/well in 96-well plates (Corning Inc., NY, USA), allowed to attach for 24 h, and then exposed to the following test articles at concentrations of 0.01, 0.1, 1.0 and 10 μM: free TPT (Hisun Pharmaceuticals), free TPT (GlaxoSmithKline), Ls-TPT (topoCED; NLI), Ls-GD (gadoCED; NLI) at 200 μM, and topoCED plus gadoCED at 200 μM, as well as culture medium only as background control. After exposure to test article, luminescence-based cell viability assays (CellTiter-Glo™, Promega, Madison, WI, USA) were conducted at 24, 48 and 72 h. All treatments and control were run in triplicate. The background absorbance was determined by incubating media with substrate alone, and subtracting the values from wells containing cells only.
Animals and intracranial xenograft technique
Congenitally athymic, male, homozygotic, nude rats (rnu/rnu; 200–275 g) 6–8 weeks of age, were acquired from Taconic (Germantown, NY, USA) and were housed under aseptic conditions (Perry Scientific, San Diego, CA, USA). The protocol was approved by the Institutional Animal Care and Use Committee at Perry Scientific. For the intracranial xenograft tumor model, U87MG cells as described earlier were harvested on the day of tumor inoculation and resuspended in Hank’s balanced salt solution without Ca2+ and Mg2+ (HBSS) for implantation. A target cell suspension of 5 × 105 cells/10 μl HBSS was implanted unilaterally into the right striatal region of the athymic rat brains. Under isoflurane anesthesia, rats were mounted in a stereotaxic frame (David Kopf Instruments, Tujunga, CA, USA) with the head positioned by ear bars and the incisor bar. A longitudinal incision was made in the skin on top of the skull and blunt dissection was used to remove connective tissue overlying the skull. A burr-hole was drilled 0.5 mm anterior and 3.0 mm lateral from the bregma. U87MG cell suspension was stereotaxically injected into the right striatum using the appropriate dorso-ventral coordinates from pial surface (−4.5 to −5 mm with the incisor bar at −3.3 mm). The volume of injection was adjusted between 5 and 10 μl to ensure that a total of 5 × 105 cells ± 2.5 × 104 cells were delivered over a period of 10 min. Following inoculation, the skin was stapled. The survival time following implantation was expected to be approximately 0–60 days, wherein the animal was to be euthanized and the brain harvested.
Evaluation of toxicity
Normal athymic rats, three per group, were evaluated for potential local toxicity after CED-mediated co-infusion of topoCED and gadoCED at two dose levels of topoCED. Rats were monitored daily for general appearance and behavior (activity, excreta, appearance, grooming, posture, behavior and weekly food consumption). Animal weights were reported prior to test article administration and on the day of necropsy. Two intermediate dose levels of topoCED between the safe (0.5 mg/ml) and toxic (5.0 mg/ml) concentrations established previously were selected [20]. After CED of a 20 μl solution containing topoCED (0.02 mg, 1.0 mg/ml or 0.032 mg, 1.6 mg/ml) and gadoCED (0.023 mg, 1.15 mg/ml) into the striatum on days 1 and 4, rats were euthanized on day 11, and their brains fixed in 4% paraformaldehyde. Fixed brain tissue was subjected to paraffin sectioning (30 μm), and every fourth section was stained with hematoxylin and eosin (H&E). The sections, 42 total, were microscopically evaluated for necrosis, edema, inflammation, hemorrhage, histocytes, pigmented histocytes, calcification and lipofuscin. Transcardiac blood samples were taken on day 11 (7 days after the last treatment) prior to necropsy for determination of TPT and GD plasma levels.
Topotecan and gadodiamide plasma levels
Blood samples for plasma TPT and GD extraction and measurement were centrifuged to separate plasma. Four-hundred microliters of the supernatant was added to 2.0 ml Eppendorf tubes containing 1.6 ml cold methanol kept on ice and vortexed. Plasma extracts were stored at −70°C until shipment for analysis using a validated reversed phase HPLC method by NLI as described above for determination of TPT levels in brain tissue. For GD levels, the plasma extracts were analyzed by inductively coupled plasma mass spectroscopy by a contract laboratory, Cantest (Burnaby, BC, Canada).
TopoCED therapy by CED in the U87MG intracranial xenograft model
Thirty adult male athymic rats were implanted with U87MG tumor cells as previously described under Animals and Intracranial Xenograft Technique. The protocol was approved by the Institutional Animal Care and Use Committee at Perry Scientific. Animals treated on days 5 and 8 after tumor implantation were randomly assigned into 3 groups: (1) CED of topoCED 0.5 mg/ml plus gadoCED 1.15 mg/ml (n = 10), (2) CED of topoCED 1.0 mg/ml plus gadoCED 1.15 mg/ml (n = 10), and (3) control (no treatment, n = 10). CED of 20 μl of the specified test article was performed for each group. Test articles were delivered by CED as described previously [21]. Infusions were performed at the same depth as that used for the tumor cell inoculation and were done on days 5 and 8 following inoculation. A complete gross necropsy of all animals found dead or sacrificed was performed as well as brain fixation and sectioning as previously described under Evaluation of Toxicity.
Distribution of topoCED and gadoCED in normal rodent brain and U87MG brain tumor xenografts
Normal athymic rats (n = 3) or athymic rats implanted with U87MG (n = 4) tumor cells as previously described under Animals and Intracranial Xenograft Technique were used. The protocol was approved by the Institutional Animal Care and Use Committee at Perry Scientific. Different fluorophores were used to label topoCED and gadoCED in order to allow differential microscopic fluorescence/luminescence, marina blue-DHPE (1,2-dehexadecanoyl-sn-glycero-3-phosphoethanolamine) (Invitrogen, Carlsbad, CA) for topoCED and rhodamine-PE (phosphoethanolamine) (Invitrogen, Carlsbad, CA) for gadoCED. Marina blue-DHPE and rhodamine-PE labeled liposomes were prepared similarly to topoCED and gadoCED, respectively, as previously described under Test Articles, with the fluorophores added to the lipid powder at the same time as the solvent solution in an amount based on a DSPC:DSPG:cholesterol:fluorophore molar ratio of 69.7:20:10:0.3. CED of 20 μl over 40 min was performed bilaterally into the striatum 10 days after implantation for the tumor group (right side tumor implanted only), and on day 1 for the naïve group. Animals were euthanized immediately after the infusion procedure. Brains were fixed in 4% paraformaldehyde and cut into 30–40 μm sections on a cryostat. Every fifth section was collected on a glass slide and cover slipped with Fluoromount-G for analysis. The convection profiles and tissue distribution of both topoCED and gadoCED were determined by means of fluorescence microscopy, and the Vd of both marina blue-DHPE and rhodamine-PE fluorophores in the sections were calculated using National Institute of Health image software. The CORR procedure in Statistical Analysis System (SAS) was used to produce Pearson correlation coefficients.
Statistical analysis
Results for the survival studies are expressed as a Kaplan–Meier (KM) survival analysis which was performed using a log rank statistic for comparative purposes. Median survival (MS) times were presented based on the KM curve. Separate analyses of survival were performed with euthanized animals considered as either uncensored (dead) and censored (alive).
Results
Tissue pharmacokinetics of liposomal topotecan co-administered with liposomal gadodiamide by CED in rat brain
Three formulations of liposomal TPT (NLI) containing 0.01 mg TPT, each combined with 0.023 mg GD in separate liposomes, as well as free TPT alone, were infused by a single CED treatment (20 μl over 40 min) into the brains of adult rats. Brain tissue levels of TPT were determined by a validated HPLC method at various times after infusion (Fig. 1). The highest brain tissue concentrations were achieved with the DSPC/DSPG/Chol 0.3 D:L ratio liposomal formulation of TPT, while the other two liposomal formulations performed similarly to free TPT. A brain tissue concentration range of 1.24–146.4 μM over the first 96 h was determined for the DSPC/DSPG/Chol 0.3 D:L ratio liposomal formulation. Due to the limited number of data points, as each data point required sacrificing 3 animals, meaningful PK variables could not be calculated with the exception of AUC. The AUC(0–last) was markedly larger for the DSPC/DSPG/Chol 0.3 D:L ratio formulation (153.8 μg day/g) compared to DSPC/Chol 0.1 and DSPC/DSPG/Chol 0.1 (38.3 and 68.2 μg day/g, respectively), and free TPT (5.5 μg day/g). All the liposomal formulations yielded half-lives in the range of 1 day while the half-life of free topotecan was much shorter. Based on these results, the DSPC/DSPG/Chol 0.3 D:L ratio formulation of TPT was selected for further study and designated topoCED.
Tissue pharmacokinetics of nanoliposomal TPT in three unique formulations co-administered with GD in a liposomal formulation plus free TPT in the normal adult rat brain after single CED infusion. All values are mg TPT per gram of brain tissue versus time after CED of 20 μl infusate. Drug concentrations were determined by HPLC assay for total TPT. Values are means ± SD of three animals per time point
Distribution of topoCED co-infused with gadoCED in normal rat brain and U87MG brain tumor xenografts
Co-convection by CED of topoCED with gadoCED was tested in both normal brain tissue and tumor xenograft implanted brain tissue in athymic rats utilizing different fluorophores to label topoCED and gadoCED in order to allow differential microscopic fluorescence/luminescence. Representative slides of staining are shown in Fig. 2.
In naïve brain tissue of normal athymic rats (n = 3), the Vd values of topoCED-marina blue DHPE were in a tight range with a mean of 38.5 ± 5.6 mm3 and a corresponding Vd to volume of infusion (Vi) ratio of 1.9. In contrast, the Vd values were markedly smaller and generally more variable in the tumor-implanted animals (n = 4), with means of 31.2 ± 6.9 mm³ in right hemisphere tumor tissue and 21.4 ± 10.3 mm3 in left hemisphere naïve brain tissue. The corresponding Vd:Vi ratios were 1.6 in tumor tissue and 1.1 in naïve brain tissue in the tumor-implanted animals. The results for gadoCED-rhodamine-PE were remarkably consistent with those for topoCED-marina blue DHPE. Specifically, the mean Vd value was 39.3 ± 5.3 mm3 in naïve brain tissue of normal athymic rats, with a corresponding Vd:Vi ratio of 2.0. In the tumor-implanted animals, the mean Vd value was 32.2 ± 8.1 mm³ in right hemisphere tumor tissue and 22.3 ± 9.2 mm³ in left hemisphere naïve brain tissue. The corresponding Vd:Vi ratio was 1.6 in tumor tissue and 1.1 in naïve brain tissue. Consistent with the individual distribution results, the correlation between the mean Vd values of topoCED-marina blue DHPE and gadoCED-rhodamine-PE was excellent in all treatment groups (range: 0.97–0.99), and there were no appreciable differences in the correlation between tissue types (naïve brain tissue vs. tumor tissue). Graphic representation of the results is shown in Fig. 3.
Volume of distribution of topoCED-marina blue DPHE co-infused with gadoCED-rhodamine-PE by CED (20 μl infused in each hemisphere) in naive rodent brain (n = 3) and U87MG xenograft rodent brain (normal left hemisphere, tumor right hemisphere, n = 4). Pearson’s correlation coefficients (r) confirm good co-convection
Cell cytotoxicity assay
The cell survival fractions by concentration of TPT after 24, 48 and 72 h treatment of U87MG cells are presented in Fig. 4, panels A, B, and C, respectively. Cytotoxic activity and potency of free TPT from two different sources (GlaxoSmithKline and Hisun Pharmaceutical) and of topoCED appeared very similar at comparable concentrations (0.01, 0.1, 1.0 and 10 μM) and time points (24, 48 and 72 h). The in vitro IC50 of topoCED at 48 and 72 h was approximately 0.8 μM supporting the potential efficacy of this liposomal TPT formulation. GadoCED alone or co-infused with topoCED did not appear to result in cytotoxicity, or affect the cytotoxicity of topoCED, even at the very high concentration of 200 μM.
Cell survival fraction of U87MG cells versus TPT concentration at 24, 48 and 72 h exposure (a–c, respectively). U87MG cells were exposed to culture medium (control), Ls-GD (gadoCED; 200 μM), TPT concentrations of 0.01, 0.1, 1.0 and 10 μM as free TPT (Hisun Pharmaceuticals), free TPT (GlaxoSmithKline), topoCED, and combination topoCED and gadoCED (200 μM). Cells were analyzed by luminescence-based cell viability assays as described in Materials and Methods
Effect of topoCED co-infused with gadoCED in U87MG brain tumor xenografts
Survival in rats with intracranial U87MG brain tumor xenografts treated 5 and 8 days after cell implantation was studied. The main efficacy analysis considered euthanized animals as uncensored (dead). Survival curves by treatment group are presented in Fig. 5. Control rats (n = 10) that received no treatment or procedure died or were euthanized 19–21 days after tumor implantation due to neurological symptoms indicative of tumor progression. Median survival (MS) for this group was 20.0 days (95% CI, 19–21). Rats in each treatment group, 10 each, of low dose topoCED, 0.5 mg/ml plus gadoCED 1.15 mg/ml, or high dose topoCED, 1.0 mg/ml plus gadoCED 1.15 mg/ml, showed a significant improvement in survival versus control (P < 0.0001 for both groups) with a MS of 29.5 (95% CI, 27–33) and 33.0 days (95% CI, 31–40), respectively. MS was increased by 65% for the high dose group and 48% for the low dose group over the control group. MS for the active treatment groups combined was 31.5 (95% CI, 30–36) days, a 58% increase, and also statistically significant when compared to the control group (P < 0.0001). Although a dose/concentration response trend was observed with a hazard ratio of 0.567 (95% CI, 0.23–1.38), the difference between the two actively treated groups did not reach the level of statistical significance (0.5 vs. 1.0 mg/ml, P = 0.215).
A secondary efficacy analysis was performed considering euthanized animals as censored. This analysis was consistent with main analysis, revealing a longer survival for active-treated animals compared to control animals, with median survivals of 48.0 (95% CI, not determined) in the high dose topoCED group (9 of 10 animals euthanized), 33.0 (95% CI, 30.0–48.0) in the low dose topoCED group (5 of 10 animals euthanized), and 23.0 (95% CI, 20.0–23.0) days in the control group (6 of 10 animals euthanized). These differences were also statistically significant when compared to control (high dose topoCED vs. control, P = 0.0014; low dose topoCED vs. control, P = 0.0014). Median survival for the active-treated groups combined was 48.0 (95% CI, 36.0–48.0) days and also statistically significant when compared to controls (P < 0.0001).
Overall gross necropsy findings included abnormalities involving the brain in the majority of the animals. The brain abnormalities were consistent with the tumor xenograft in place including hemispheric enlargement ipsilateral to the tumor xenograft and tumor often protruding through the cannula track with mass effect. Representative histology showing control, low-dose treated and high-dose treated rats bearing U87MG xenograft 20, 27 and 42 days after implant, respectively, are shown in Fig. 6a–c.
Representative histology of animals used in this study. a Shows control rat (7640) bearing U87MG xenograft 20 days after implant, rat euthanized; b shows 2 × 0.5 mg/ml topoCED treated rat (7632) bearing U87MG xenograft 27 days after implant, rat euthanized; c shows 2 × 1.0 mg/ml topoCED treated rat (7609) bearing U87MG xenograft 42 days after implant, rat euthanized
Evaluation of toxicity
Toxicity of higher doses of topoCED (1.0 or 1.6 mg/ml) in combination with gadoCED 1.15 mg/ml were tested in naïve rat brains prior to the conduct of the efficacy study to ensure tolerability of the selected efficacy study doses. No significant toxicity due to the agents was detected 11 days after CED infusion of 20 μl into the striatum on days 1 and 4. Relevant findings revealed by microscopic examination included foci of recent hemorrhage, mainly mild and focally moderate in degree, extending from the cortex into the white matter as well as the basal ganglia, and situated in or around the sections containing the cannula tract. In no case were there more than two sections showing hemorrhage. In addition, areas of histiocytic infiltration were localized with a similar distribution. Some of the histiocytes contained golden pigment, possibly hemosiderin. Negative findings included no evidence of significant neuronal loss or changes in glial cells such as gliosis or frank necrosis. The meninges, blood vessels and ventricles all appeared within normal limits within all sections. There was no evidence of significant edema, acute or chronic inflammation, calcification, or coagulative necrosis. Further, there were no significant differences in histologic findings between the two dose groups within the study.
Plasma extract measurements at day 11 (7 days after the last infusion) revealed both topotecan and gadodiamide levels were either absent or below the lower limit of quantification of the assay.
Discussion
Since the introduction of CED, this technique has shown considerable promise for the treatment of brain tumors with active agents in phase II and III clinical trials [19], although the phase III results did not meet their primary endpoints of overall survival [33, 34]. The failed phase III CED studies did not employ an adjunct agent for the real-time monitoring of drug distribution in the general study population, which may be an important factor explaining these disappointing study outcomes. The future success of CED-based delivery technology for clinical application will require continued refinements and improvements. These include an effective formulation of an active therapeutic agent with desirable convection properties and the ability to monitor delivery to the target tissue thereby increasing efficacy and reducing toxicity in the clinic [35].
Several groups have reported improved convection and pharmacologic properties of camptothecins, which are known to be active against malignant glioma, by encapsulation into PEGylated liposomes [21, 22, 36]. TPT is a good therapeutic candidate for GBM based on its known cytotoxic activity against various glioma cell lines in vitro and its preferential antiangiogenic effects at low concentrations [37]. A stable PEGylated liposomal formulation of TPT delivered by CED was shown to be effective in the U87MG intracranial rat xenograft model [21]. However, while PEGylation was found to enhance the distribution of liposomes given via CED by reducing their tissue affinity [27], recent reports about PEG-induced complement activation raised concerns about the safety of PEGylated formulations [24–26]. The feasibility and accuracy of monitoring CED over time was shown with PEGylated liposomal carriers loaded with gadodiamide in a rat glioma model both in tumor and in normal brain [28, 29, 38]. An ideal imaging tracer should possess convection properties similar to the therapeutic agent to ensure tracking accuracy [32].
Building on this work, we have developed and optimized a non-PEGylated liposomal DSPC/DSPG/Chol formulation of TPT (topoCED) and matched liposomal MR imaging tracer GD (gadoCED). This novel, convectable formulation provides an ideal basis for real-time monitoring of TPT distribution. Our study results demonstrate positive tissue pharmacokinetics, co-convection, cytotoxicity, efficacy, and lack of toxicity of topoCED with gadoCED, in a clinically meaningful dose range.
Tissue retention of topoCED following single CED administration was significantly improved relative to free topotecan. At a dose of 10 μg (0.5 mg/ml), topoCED had a half-life in brain of approximately 1 day and increased the area under the concentration–time curve (AUC) by 28-fold over free topotecan (153.8 vs. 5.5 μg day/g; see Fig. 1). The substantial AUC advantage of topoCED over free TPT supports the efficacy results.
Co-convection of topoCED combined with gadoCED was tested in both naïve rat brain tissue and U87MG intracranial rodent xenograft tumor tissue utilizing different fluorophores to label topoCED (marina blue labeled liposomes) and gadoCED (rhodamine labeled liposomes) in order to allow differential microscopic fluorescence/luminescence (see Fig. 2). Reliable and consistent drug distribution of both agents was demonstrated with Vd:Vi ratios of 1.9 in normal brain. The distribution of topoCED in naïve rat brain tissue is similar to liposome infusion by CED in normal non-human primate brain (Vd:Vi ratio of 2) [38], and in normal canine brain (Vd:Vi ratio range of 1.2–3.4) [39]. In the tumor-implanted animals, the corresponding Vd:Vi ratios were 1.6 in tumor tissue and 1.1 in naïve brain tissue, right and left hemispheres respectively. CED fluid dynamics appear to be impacted by intracranial pressure, with high intracranial pressure due to excessive tumor growth leading to impaired drug distribution in both naïve brain tissue and tumor tissue in the tumor implanted animals. Excellent co-convection of topoCED and gadoCED was observed in both tissue types with correlation coefficients between 0.97 and 0.99 (see Fig. 3).
TopoCED demonstrated excellent potency in a U87MG cell assay; its concentration–time curves were similar to free topotecan (see Fig. 4). The IC50 of topoCED was approximately 0.8 μM at 48 and 72 h, which is well below the brain tissue concentration range of 1.24–146.4 μM over the first 96 h that was observed in the pharmacokinetic study. GadoCED alone or co-infused with topoCED did not appear to result in additive or synergistic cytotoxicity even at the very high concentration of 200 μM.
A clear and consistent survival advantage as compared to untreated controls was demonstrated with a two-dose CED regimen of topoCED at two dose levels (1.0 and 0.5 mg/ml) in conjunction with gadoCED (1.15 mg/ml) using the in vivo U87MG intracranial rat xenograft model. The findings showed both topoCED dose levels resulted in a highly statistically significant increase in overall survival (P < 0.0001) when compared to controls (see Fig. 5). Median survival was increased by 65% for the high dose group (33.0 vs. 20 days) and by 48% for the low dose group (29.5 vs. 20 days) over the control group. In the low dose group the effect size was slightly more moderate than in the high dose group, thus suggestive of a dose/concentration dependent effect. Similar findings were observed when the survival analysis was performed with euthanized animals considered as censored which is a more conservative assessment method preventing any potential overestimation of the true effect size of topoCED while possibly underestimating that effect. The results of the secondary efficacy analysis were still highly statistically significant and strongly support the primary efficacy analysis findings in which euthanized animals were considered as uncensored.
The overall efficacy study findings, although highly statistically significant, differ somewhat from efficacy findings reported for animals receiving a PEGylated nanoparticle liposome-TPT (nLs-TPT) formulation reported by Saito and colleagues [21]. Also, Yamashita and colleagues reported a MS of 27.5 days for animals receiving the same nLs-TPT formulation at a dose of 0.25 mg/ml [40]. While these seeming differences between the study results may be attributable to differences between the liposomal formulations, they may also be due to a number of other factors including differences in the viability of the cell lines and technical factors leading to variable tumor coverage. The relative roles of these factors can only be determined in a direct head to head comparison of the different formulations in the same model.
TopoCED at higher concentrations (1.6 mg/ml) co-infused with gadoCED (1.15 mg/ml) in naïve brain tissue appeared to be safe with no evidence of histopathological changes within targeted regions that were attributable to either agent in a pilot toxicology study in rats. Small areas of acute hemorrhage were mostly localized along the cannula tract and presumably related to the experimental procedure and drug delivery system. Gross and microscopic changes related to the delivery technique including cannula insertion and CED have been described previously and the changes observed in this study are consistent with the delivery technique employed [16]. A concentration of 5.0 mg/ml TPT in the nLs-TPT formulation was previously reported to be toxic while 0.5 mg/ml was well tolerated [21]. In addition, TPT and GD plasma levels 11 days after infusion were below the lower level of quantitation for the assay consistent with the delivery method and drug properties.
In conclusion, TPT has been previously shown to be an active agent against malignant glioma. Direct intracerebral administration by CED lowers the systemic exposure significantly as compared to intravenous applications resulting in fewer systemic adverse events and thereby improvement of the safety of the drug. We have developed topoCED and gadoCED, unique non-PEGylated nanoparticle liposomal formulations of TPT and GD, respectively, and demonstrated desirable TPT pharmacokinetic properties that resulted in significant efficacy using the in vivo U87MG intracranial rodent xenograft model when the two agents were co-infused by CED. Excellent co-convection of the two agents indicates gadoCED will provide a means to visualize topoCED infusion during CED reducing the risk of leakage into the CNS while improving efficacy. The effective dose range is well tolerated and cleared within 7 days. The overall results reported here warrant further investigation of topoCED co-administered with gadoCED by CED in non-human primate tumor models with the goal of treating patients with malignant glioma in the near future.
References
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996. doi:10.1056/NEJMoa043330
Wong ET, Hess KR, Gleason MJ et al (1999) Outcomes and prognostic factors in recurrent glioma patients enrolled onto phase II clinical trials. J Clin Oncol 17:2572–2578
Rapisarda A, Zalek J, Hollingshead M et al (2004) Schedule-dependent inhibition of hypoxia-inducible factor-1α protein accumulation, angiogenesis, and tumor growth by topotecan in U251-HRE glioblastoma xenografts. Cancer Res 64:6845–6848. doi:10.1158/0008-5472.CAN-04-2116
Marchesini R, Colombo A, Caserini C et al (1996) Interaction of ionizing radiation with topotecan in two human tumor cell lines. Int J Cancer 66:342–346. doi:10.1002/(SICI)1097-0215(19960503)66:3<342::AID-IJC13>3.0.CO;2-D
Schmidt F, Rieger J, Wischhusen J, Naumann U, Weller M (2001) Glioma cell sensitivity to topotecan: the role of p53 and topotecan-induced DNA damage. Eur J Pharmacol 412:21–25. doi:10.1016/S0014-2999(00)00923-7
Mainwaring MG, Gomez SP, Marsh RD, Chen S (2001) Sequential temozolomide followed by topotecan in the treatment of glioblastoma multiforme. Proc Am Soc Clin Oncol 20:245 (abstract)
Fisher BJ, Scott C, Macdonald DR, Coughlin C, Curran WJ (2001) Phase I study of topotecan plus cranial radiation for glioblastoma multiforme: results of Radiation Therapy Oncology Group Trial 9507. J Clin Oncol 19:1111–1117
Fisher B, Won M, MacDonald D, Johnson DW, Roa W (2002) Phase II study of topotecan plus cranial radiation for glioblastoma multiforme: results of Radiation Therapy Oncology Group 9513. Int J Radiat Oncol Biol Phys 53:980–986. doi:10.1016/S0360-3016(02)02817-1
Grabenbauer GG, Anders K, Fietkau RJ et al (2002) Prolonged infusional topotecan and accelerated hyperfractionated 3d-conformal radiation in patients with newly diagnosed glioblastoma-a phase I study. J Neurooncol 60:269–275. doi:10.1023/A:1021100413142
Lesimple T, Hassel MB, Gedouin D et al (2003) Phase I study of topotecan in combination with concurrent radiotherapy in adults with glioblastoma. J Neurooncol 65:141–148. doi:10.1023/B:NEON.0000003647.66788.3b
Gross MW, Altscher R, Brandtner M et al (2005) Open-label simultaneous radio-chemotherapy of glioblastoma multiforme with topotecan in adults. Clin Neurol Neurosurg 107:207–213. doi:10.1016/j.clineuro.2004.07.016
Pipas JM, Meyer LP, Rhodes CH, Cromwell LD, McDonnell CE, Kingman LS, Rigas JR, Fadul CE (2005) A phase II trial of paclitaxel and topotecan with filgrastim in patients with recurrent or refractory glioblastoma multiforme or anaplastic astrocytoma. J Neurooncol 71:301–305. doi:10.1007/s11060-004-2026-2
Walter KA, Tamargo RJ, Olivi A, Burger PC, Brem H (1995) Intratumoral chemotherapy. Neurosurgery 37:1129–1145. doi:10.1097/00006123-199512000-00013
Lieberman DM, Laske DW, Morrison PF et al (1995) Convection-enhanced distribution of large molecules in gray matter during interstitial drug infusion. J Neurosurg 82:1021–1029
Croteau D, Walbridge S, Morrison PF et al (2005) Real-time in vivo imaging of the convective distribution of a low-molecular-weight tracer. J Neurosurg 102:90–97
Lonser RR, Walbridge S, Garmestani K et al (2002) Successful and safe perfusion of the primate brainstem: in vivo magnetic resonance imaging of macromolecular distribution during infusion. J Neurosurg 97:905–913
Bobo RH, Laske DW, Akbasak A et al (1994) Convection-enhanced delivery of macromolecules in the brain. Proc Natl Acad Sci USA 91:2076–2080. doi:10.1073/pnas.91.6.2076
Morrison PF, Laske DW, Bobo H et al (1994) High-flow microinfusion: tissue penetration and pharmacodynamics. Am J Physiol 266:R292–R305
Vogelbaum MA (2007) Convection enhanced delivery for treating brain tumors and selected neurological disorders: symposium review. J Neurooncol 83:97–109. doi:10.1007/s11060-006-9308-9
Moog R, Burger AM, Brandl M et al (2002) Change in pharmacokinetics and pharmacodynamic behavior of gemcitabine in human tumor xenografts upon entrapment in vesicular phospholipid gels. Cancer Chemother Pharmacol 49:356–366. doi:10.1007/s00280-002-0428-4
Saito R, Krauze MT, Noble CO et al (2006) Convection-enhanced delivery of Ls-TPT enables an effective, continuous, low-dose chemotherapy against malignant glioma xenograft model. Neuro-oncology 8:205–214. doi:10.1215/15228517-2006-001
Noble CO, Krauze MT, Drummond DC et al (2006) Novel nanoliposomal CPT-11 infused by convection-enhanced delivery in intracranial tumors: pharmacology and efficacy. Cancer Res 66:2801–2806. doi:10.1158/0008-5472.CAN-05-3535
Woodle MC, Lasic DD (1992) Sterically stabilized liposomes. Biochim Biophys Acta 1113:171–199
Ishida T, Kiwada H (2008) Accelerated blood clearance (ABC) phenomenon upon repeated injection of PEGylated liposomes. Int J Pharm 354:56–62. doi:10.1016/j.ijpharm.2007.11.005
Szebeni J, Baranyi L, Savay S et al (2002) Role of complement activation in hypersensitivity reactions to doxil and hynic PEG liposomes: experimental and clinical studies. J Liposome Res 12:165–172. doi:10.1081/LPR-120004790
Szebeni J (2005) Complement activation-related pseudoallergy: a new class of drug-induced acute immune toxicity. Toxicology 216:106–121. doi:10.1016/j.tox.2005.07.023
Saito R, Krauze MT, Noble CO et al (2006) Tissue affinity of the infusate affects the distribution volume during convection-enhanced delivery into rodent brains: implications for local drug delivery. J Neurosci Methods 154:225–232. doi:10.1016/j.jneumeth.2005.12.027
Mamot C, Nguyen JB, Pourdehnad M et al (2004) Extensive distribution of liposomes in rodent brains and brain tumors following convection-enhanced delivery. J Neurooncol 68:1–9. doi:10.1023/B:NEON.0000024743.56415.4b
Saito R, Bringas JR, McKnight TR et al (2004) Distribution of liposomes into brain and rat brain tumor models by convection-enhanced delivery monitored with magnetic resonance imaging. Cancer Res 64:2572–2579. doi:10.1158/0008-5472.CAN-03-3631
Krauze MT, Forsayeth J, Park JW, Bankiewicz KS (2006) Real-time imaging and quantification of brain delivery of liposomes. Pharm Res 23:2493–2504. doi:10.1007/s11095-006-9103-5
Krauze MT, Vandenberg SR, Yamashita Y et al (2008) Safety of real-time convection-enhanced delivery of liposomes to primate brain: a long-term retrospective. Exp Neurol 210:638–644. doi:10.1016/j.expneurol.2007.12.015
Murad GJ, Walbridge S, Morrison PF et al (2006) Real-time, image-guided, convection-enhanced delivery of interleukin 13 bound to pseudomonas exotoxin. Clin Cancer Res 12:3145–3151. doi:10.1158/1078-0432.CCR-05-2583
Broaddus WC (2007) Convection enhanced delivery 3rd international symposium, trial update: TransMID. Available at http://cms.clevelandclinic.org/neuroscience/documents/1340%20Broaddus%20Update%20on%20TransMID%20Trial.pdf. Accessed 11 Feb 2008
Kunwar S, Westphal M, Medhorn M et al (2007) Results from PRECISE: a randomized phase 3 study in patients with first recurrent glioblastoma multiforme (GBM) comparing cintredekin besudotox (CB) administered via convection-enhanced delivery (CED) with Gliadel Wafers (GW). Neuro-oncology 9:531 (abstract)
Sampson JH, Raghavan R, Brady ML et al (2007) Clinical utility of a patient-specific algorithm for simulating intracerebral drug infusions. Neuro-oncology 9:343–353. doi:10.1215/15228517-2007-007
Krauze MT, Noble CO, Kawaguchi T et al (2007) Convection-enhanced delivery of nanoliposomal CPT-11 (irinotecan) and PEGylated liposomal doxorubicin (Doxil) in rodent intracranial brain tumor xenografts. Neuro-oncology 9:393–403. doi:10.1215/15228517-2007-019
Nakashio A, Fujita N, Tsuruo T (2002) Topotecan inhibits VEGF- and bFGF-induced vascular endothelial cell migration via downregulation of the PI3K-Akt signaling pathway. Int J Cancer 98:36–41. doi:10.1002/ijc.10166
Saito R, Krauze MT, Bringas JR et al (2005) Gadolinium-loaded liposomes allow for real-time magnetic resonance imaging of convection-enhanced delivery in the primate brain. Exp Neurol 196:381–389. doi:10.1016/j.expneurol.2005.08.016
Dickensen PJ, LeCouteur RA, Higgins RJ et al (2008) Canine model of convection-enhanced delivery of liposomes containing CPT-11 monitored with real-time magnetic resonance imaging. J Neurosurg 108:989–998. doi:10.3171/JNS/2008/108/5/0989
Yamashita Y, Krauze MT, Kawaguchi T et al (2007) Convection-enhanced delivery of a topoisomerase I inhibitor (nanoliposomal topotecan) and topoisomerase II inhibitor (pegylated liposomal doxorubicin) in intracranial brain tumor xenografts. Neuro-oncology 9:20–28. doi:10.1215/15228517-2006-016
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grahn, A.Y., Bankiewicz, K.S., Dugich-Djordjevic, M. et al. Non-PEGylated liposomes for convection-enhanced delivery of topotecan and gadodiamide in malignant glioma: initial experience. J Neurooncol 95, 185–197 (2009). https://doi.org/10.1007/s11060-009-9917-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-009-9917-1