Abstract
Objective
Convection-enhanced delivery using carboplatin in brainstem glioma models was reported to prolong survival. Functional impairment is of additional importance to evaluate the value of local chemotherapy. We established a neurological scoring system for the rat brainstem glioma model.
Material and methods
In 46 male Fisher rats stereotactically 105 F-98 cells were implanted at 1.4-mm lateral to midline and at the lambdoid suture using guided screws. Following 4 days local delivery was performed using AlzetTM pumps (1 μl/h over 7 days) with either vehicle (5% dextrose) or carboplatin via one or two cannulas, respectively. All rats were subsequently tested neurologically using a specified neurological score. In 38 animals survival time was recorded. Representative MR imaging were acquired in eight rats, respectively, at day 12 after implantation. HE staining was used to evaluate tumor extension.
Results
Neurological scoring showed significantly higher impairment in the high dose carboplatin group during the treatment period. Survival was significantly prolonged compared to control animals in the high dose carboplatin-one cannula group as well as in both low dose carboplatin groups (18.6 ± 3 versus 26.3 ± 9, 22.8 ± 2, 23.6 ± 2 days; p < 0.05). Overall neurological grading correlated with survival time. MR imaging showed a focal contrast enhancing mass in the pontine brainstem, which was less exaggerated after local chemotherapy. Histological slices visualized decreased cellular density in treatment animals versus controls.
Conclusion
Local chemotherapy in the brainstem glioma model showed significant efficacy for histological changes and survival. Our neurological grading enables quantification of drug and tumor-related morbidity as an important factor for functional performance during therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The overall rate of brainstem gliomas is at about 10% to 15% of CNS tumors in childhood and adolescence. Sixty to seventy-five percent of those account for the malignant type, the so called diffuse pontine gliomas [9, 18, 31]. The prognosis in these cases is dismal and despite chemotherapy and radiation, mean survival is about 10 months after diagnosis and prolonged survival of more than 2 years is reported in less than 10% of the cases. Treatment benefits are rather limited [4, 30]. The standard treatment is radiation alone, which may result in transient improvements of neurological dysfunctions and progression-free survival benefit without influencing overall survival [12, 13, 30]. There have been many studies discussing adjuvant chemotherapy, however, there have been only a few reports of its benefits. In a retrospective evaluation of 153 cases with diffuse pontine gliomas systemic chemotherapy after irradiation resulted in a significant prolonged survival of at least 0.16 years with a 1-year survival rate of 45.8 ± 5.4% versus 34.4 ± 13.5% of patients with irradiation alone. This study is the largest showing only a marginal benefit of systemic chemotherapy in malignant brainstem gliomas [30]. Thus, new strategies of therapy in diffuse pontine gliomas based on enhanced delivery of antitumoral agents towards the site of the lesion might attenuate efficacy of treatment. Local delivery techniques such as injection of drugs in the carotid arteries, the opening of the blood brain barrier by a second compound or intranasal chemotherapy, as well as convection-enhanced delivery (CED) of antitumoral agents via implanted catheters have been described in experimental settings [6, 8, 11, 14, 15]. Among all, the latter technique has been proven for its safety and efficacy in experimental settings [6, 7, 16, 21, 24–28]. One case with a diffuse pontine glioma has been published “that received a stereotactic implanted catheter into the brainstem with local IL-13-PE infusion at 0.5 to 10 μl/min up to a total volume of 1.4 ml. However, due to the rather late stage of tumor progression no effect of therapy could be observed [21].
There also have been many laboratory studies investigating local delivery into an animal brainstem without tumors. Therefore, a rat model of brainstem glioma was developed [17]. A beneficial effect of experimental local chemotherapy infusion in the brainstem glioma model was described by Carson and coworkers [6]. A prolongation of survival could be achieved by continuous local carboplatin infusion. Moreover, feasibility studies were performed with continuous drug infusion into the brainstem using carboplatin, BCNU, IL-13-PE, and gemicitamine [7, 22, 25, 27]. Toxic side effects of local drug infusions within the brainstem were evaluated mainly in primates [22, 27]. Functional impairment is of significant importance to clarify the value and limitations of local chemotherapy. For the rat model of brainstem gliomas, no clinical evaluation has been described using local chemotherapy by convection-enhanced delivery to date. In this study we established the neurological grading scale for rats after implantation of glioma cells in the brainstem and additional CED chemotherapy using carboplatin. In addition, survival was documented and magnetic resonance (MR) imaging and histology was performed to analyze the tumor extension with and without therapy.
Materials and methods
Animals
Male Fischer 344 rats (Charles River Laboratories, Wilmington, MA, USA) weighing 250 to 350 g (mean 290 g) were used in this experiment. The rats were housed in standard facilities and given free access to Baltimore City water and rat chow. The experimental protocol was approved by the Animal Care and Use Committee of the Johns Hopkins University and met all federal guidelines (Table 1).
Tumor cell line
The F98 cell lines were maintained in the Johns Hopkins University Genetics CORE Cell Center facilities. This glioma cell line is widely used in neuro-oncology for intracranial implantation in syngeneic rats. It was developed by Wechsler and colleagues in BD IX rats using a single intravenous injection of N-ethyl-N-nitrosourea administered to a pregnant animal on the 20th day of gestation [32]. F98 cells develop as an infiltrative tumor with low immunogenic potential and moderate angiogenic activity. F98 cells are considered a good model of anaplastic glioma [2]. The tumor cells were prepared for injection via standard cell preparation protocol, centrifuged, and resuspended in Dulbecco’s modified eagle medium. The viable cells, determined by trypan blue exclusion, were counted with a hemocytometer. The cells were diluted to a concentration of 1 × 105 cells/3 μl.
Surgery
The animals were anesthetized with an intraperitoneal injection of a solution of ketamine 50 mg/kg (100 mg/ml; Abbott Laboratories, Chicago, IL, USA) and xylazine 10 mg/kg (100 mg/ml; Phoenix Pharmaceutical, St. Joseph, MO, USA). The posterior cranial region was shaved and prepared in a sterile fashion. An incision over the midline approximately 2 cm in length was cut in the skin over the skull and small burr holes were made using a steel drill bit (Plastics One, Roanoke, VA, USA) at coordinates 1.4-mm right of the sagittal and 2.5-mm anterior, onto the lambdoid suture and 2.5-mm posterior to it, respectively. Both of the posterior burr holes must be placed cautiously not to injure the transverse sinus. The cannulated guide screws (Plastics One) were inserted into the burr holes. Infusion cannulas were placed to a depth of 7 mm in the screw hole and fixed in place with surgical glue.
For tumor cell implantation in all rats the head was positioned +5° from the horizontal plane. A 22-gauge 10-μl Hamilton needle (Hamilton Company, Reno, NV, USA) was inserted to a depth of 7 mm from the dura mater and 3-μl brainstem injection of 1.0 × 105 F98 glioma cells were administered. To avoid cell leakage or backflow of the media, a stylet plug was inserted into the screw guide and the incision was closed with surgical clips in a standard fashion. After recovery, the animals were returned to their cages. Each animal was subsequently evaluated for neurological deficits.
On day 5 after the injection of tumor cells in the treatment groups, the animals were anesthetized and the clips removed. The bodies of the pump were implanted subcutaneously on the back of the anesthetized rats slightly posterior to the scapulas in a pocket created by inserting and opening a hemostat into a midscapular incision and thereby spreading the subcutaneous tissue on both sides. The pumps were inserted with sufficient catheter tubing to pass through a tunnel created under the skin of the back and neck to the site of the cannulas. The tubing and cannulas were empty on implantation to allow the tissue to seal before fluid flow. The skin was closed with surgical clips and the animals were returned to their cages.
Neurological evaluation
Neurological evaluation was performed in modification of other scoring systems used for cerebral ischemia [3, 34]. A novel brainstem scoring system specified as the Berlin–Baltimore brainstem (BBB) score motor function of the extremities was evaluated. For each extremity a value between zero to four can be graded. For all extremities a total of up to 16 points for cases of complete tetraplegia. Additional points were added for abnormal movement behaviors like, lateral body tilt, or axial body rotation. This evaluation possibly adds up to 2 points. The scoring system is shown in more detail in Table 2.
MR imaging
Magnetic resonance imaging was performed using a nuclear spectrometer equipped with actively shielded gradients (internal diameter 15 cm). Rats were anesthetized and placed in a Bruker Biospec (9.4 T; 400 MHz, 12 cm gradient, Karlsruhe, Germany). All rats received 0.5 ml of gadolinium-diethylenetriamine penta-acetic acid (MagnevistTM, Berlex Imaging, Wayne, NJ, USA) intraperitoneally 20 to 30 min prior to scanning. Spin-echo images were obtained using the following parameters; 800-ms repeat time, 17-ms echo time, 1.2-mm slice thickness, and a 64-mm field of view.
Histology
A small subset of animals were euthanized after 12 days. After administration of an intraperitoneal injection of ketamine hydrochloride 75 mg/kg and xylazine 15 mg/kg, perfusions were performed, in which the thorax was opened, the right atrium was incised, and a cannula was inserted into the left ventricle. Normal saline followed by 10% paraformaldehyde was pumped through the rat’s circulation. An intraperitoneal injection of Euthanasia-6 solution (Veterinary Laboratories, Lenexa, KS, USA) was then used to put the animal to sleep. After death, the entire brain was dissected and sliced into 1-mm coronal sections. These were placed into 10% paraformaldehyde. After fixation paraffin incorporation of the brain-sections, 7-µm slices were cut from each section using a microtome and then stained with hematoxylin and eosin. Presence of tumor and the pattern of infiltration were assessed and intrinsic tumor characteristics and effect of tumor presence on brainstem structure were recorded.
Experimental design
Male Fischer 344 rats (n = 46) were randomized into experimental groups. Animals in group 1 to 5 received a 3-μl injection of 1 × 105 cells/ml (100,000 cells) of F98 glioma cells at the coordinates 1.4-mm parasagittal, 1-mm posterior to lambdoid suture, and 7-mm deep. Five days after incorporation of cells in the brainstem, local chemotherapy treatment was started. While in group 1 animals received placebo (dextrose 5%, 1 µl/h for 7 days [n = 10]) via the same burr hole, in group 2 to 5 carboplatin treatment (low dose: 0.1 mg/ml; high dose: 0.5 mg/ml; 1 µl/h for 7 days; Table 1) was performed either thru one cannula (groups 2 [n = 10] and 3 [n = 9]) or two cannulas (groups 4 [n = 10] and 5 [n = 9]), at the respective burr hole positions either where the glioma cells were implanted (at lambda) or at the anterior and posterior burr holes (2.5 mm anterior and posterior of lambda). The animals were followed neurologically as described above and onset of deficit was documented. In the groups, in which survival was documented as an outcome parameter, either spontaneous death was recorded as endpoint or animals were sacrificed if severe disability hindered independent eating or drinking behavior. At day 7 after treatment (day 12 after tumor implantation), in two animals per group, a cranial MRI was performed and the animals were sacrificed for brain removal for histological staining as described above. In all other animals survival times were recorded.
Statistical analysis
Statistical analysis included comparison of neuroscore and body weight changes between the groups using the t test with nonparametric comparisons (Whitney–Mann test) followed by a Bonferroni correction by factor 3. Comparison of survival time between the groups was accomplished using the log-rank test and Kaplan–Meier survival curves were generated. All calculations were performed using the statistical software Graph Prism 4.0 (GraphPad, San Diego, CA, USA), and p values less than 0.05 were considered to be statistically significant.
Results
Body weight and BBB-neuroscore
The body weight changes over time of all animals are given in Table 3. The weight loss in placebo animals was continuously increasing from day 10 to 18. In group 2, significant weight changes (p < 0.05) with intermittent weight gain was observed from day 6 to 13. In the high dose carboplatin groups, the weight loss was significantly higher from day 6 to 14 (group 4) and day 7 to 12 (group 5), respectively (p < 0.05).
Using the BBB-neuroscore in the placebo animals a continuous increase of neuroscore over time could be observed. Until day 18 after tumor cell implantation placebo animals reached highest scoring for neurological deficit. A similar neurological course could be shown in animals using low-dose carboplatin treatment. Both groups (2 and 3) using either one or two cannulas showed significant less neurological impairment from day 14 to day 17 compared to placebo (Fig. 1; p < 0.05). Using high dose carboplatin (group 4 and 5) a significant higher neurological impairment during the early treatment period was observed (p < 0.05), which was more exaggerated in group 4 were only one cannula was used (Fig. 2). Over time this impairment remained stable with significant lower neurological deficit in the one cannula group (4) at day 17 after tumor implantation (p < 0.05).
Neuroscore evaluation started at day 1 and continued from day 4 continuously until day 18 after implantation of F98 cells into the brainstem. Placebo animals showed constantly increasing neurological deficit from day 8 until day 18. Neurological deficit after CED of low dose carboplatin remained significant lower in both groups compared to placebo using either one or two cannula from day 9 to day 17 (*p < 0.05)
Neuroscore was evaluated after implantation of F98 cells into the brainstem at day 1 and from day 4 to 18 on a daily basis. Placebo animals showed constantly increasing neurological deficit from day 8 until day 18. In the one cannula group after CED of carboplatin the neurological deficit increases significantly compared to placebo and remained stable over the remaining time of observation. The two cannula group had less initial deficit, however, the neuroscore increased to the same level as in the one cannula group at day 13 and remained stable thereafter (*p < 0.05)
Survival
Convection-enhanced delivery after F98 brainstem glioma implantation in the brainstem did significantly prolong the survival compared to control animals (18.5 ± 3 days) in the high dose carboplatin, one cannula group (group 4, 28.4 ± 14 days, p < 0.05; Fig. 3) as well as in both low-dose carboplatin groups (group 2, 23 ± 6 days, group 3, 24.4 ± 7 days, p < 0.05; Fig. 4). Overall neurological grading correlated significantly with survival time (p < 0.001; Fig. 5).
Kaplan–Meier curves of animal survival comparing high dose carboplatin to placebo. In both, one and two cannula groups, mean survival was longer compared to placebo (18.5 ± 3 days), while one cannula group reached statistical significance (28.4 ± 14 days, p < 0.05; two cannula group, 22.7 ± 6 days; p = 0.08)
MR imaging
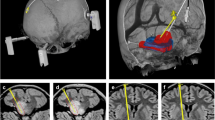
At 12 days after tumor implantation the glioma was visualized using MR imaging. A solid contrast enhancing mass in the pontine brainstem could be depicted in sagittal and coronal sections. Contrast enhancement and tumor size appeared to be less exaggerated after local chemotherapy using carboplatin (Fig. 6a–c).
MR imaging (Bruker Biospec, 9.4 T) of the rat brain 12 days after implantation of F98 cells into the brainstem (sagittal orientation, a) following CED with placebo (b) and carboplatin (c). A solid contrast-enhancing tumor is visualized in the brainstem with mass effect and midline deviation. After CED with carboplatin the tumor appears to be smaller in size with lower intensity of contrast enhancement
Histology
In H&E stained brain sections the lesion was characterized by a tumor mass within the pontine brainstem with infiltrative character at the tumor margins. After CED the slices showed decreased cellular density in treatment animals compared to controls at day 12 after cell implantation (Fig. 7a,b).
Hematoxylin and eosin staining of rat brain sections (7 μm) 12 days after implantation of F98 cells in the brainstem following CED with placebo (left) and carboplatin (right). In the placebo animals a unilateral tumor mass is depicted in the brainstem. Following CED with carboplatin the same area shows tumor cells however with markedly decreased cell density
Discussion
In the present study, we showed that local infusion of carboplatin resulted in prolonged survival in the rat brainstem glioma model. Imaging studies and histology showed at day 12 after tumor implant, a diminished tumor extension in treated animals. During treatment neurological evaluation showed carboplatin-induced neurotoxicity in the high-dose carboplatin group. This was also revealed by changes in body weight over time. Low-dose carboplatin did not show this neurotoxic effect. However, the beneficial effect on survival time was lower in this group of animals. Neurological grading correlated significantly with survival time. No effect between two and one cannula application of local chemotherapy was observed.
Convection-enhanced delivery for local chemotherapy has become a matter of research for malignant CNS neoplasms which are surgically untreatable. Most recent patient data was published in patients with recurrent glioblastomas [5, 10, 19, 23, 29]. The basic idea of treatment in these patients is based on primary resection of the tumor with additional adjuvant radiation chemotherapy. In case of recurrence local chemotherapy is one treatment option, which was performed in different study designs [19, 20, 29]. In combination of surgery chemotherapy can be embedded in the resection cavity [1, 33]. Moreover, convection-enhanced delivery have been applied in these patients using different types of agents. Despite the progression of disease in these patients after recurrence results have been promising [19, 20, 23, 29]. We hypothesize that local chemotherapy can thus also be applied in patients with primarily surgically untreatable tumors. First of all diffuse intrinsic pontine gliomas are at highest need for more promising therapeutic options. In the past decades only limited progress was made to prolong survival in these patients and prognosis is rather dismal with a 2-year survival rate of about 10% [9, 18, 31]. In order to gain preclinical experience, experimental studies have been performed to investigate local chemotherapies in brainstem tumor models.
In our study we could verify that local chemotherapy has beneficial effects on survival in the rat F98 glioma model for the brainstem, which also is documented by others. Using F98 and 9L glioma cells implanted in the brainstem treated with local infusion of carboplatin over 7 days the survival time was prolonged from 13 to 27 days (F98) and 23 to 32 days (9L) [6]. CED using carboplatin of gemcitabine with dose escalation studies using the 9L brainstem glioma model documenting survival benefit for both regimens and long-term survival of 50% and 75%, respectively. However, the number of animals tested in this study for survival was limited [7]. Our presented data are in line with these published studies. Furthermore, to compare the application mode we used one and two cannulas in our study for carboplatin delivery. In the two cannulas group the tip were placed anterior and posterior to the side of tumor implantation, while in the one cannula group the tip of the cannula was applied at the same location of cell implant. There were no significant differences in survival time between these groups. Our group has reported previously that an amount of three unilateral cannulas is feasible for local carboplatin delivery in the brainstem [28]. However, further studies are warranted to clarify if multiple cannulas linked local chemotherapy has therapeutically benefits in the model of brainstem gliomas.
In order to investigate limits of local chemotherapy in the brainstem toxicity studies have been performed using local delivery of anti-tumoral agents in the brainstem [16, 25, 26]. In dose escalation studies for rats mortality was evaluated showing the limits for local chemotherapy on survival [6, 7, 26]. In primate studies agent specific toxic effects were evaluated to define the maximal tolerable dose [16, 27]. However, there is no neurological grading system for the rat model of brainstem gliomas. In the literature, some grading systems have been described for cerebral ischemia and traumatic brain injury [3, 34]. Our scoring system was evaluated already in the study of local delivery using carboplatin without tumor implantation [28]. As discussed earlier it was found to be practical and useful to evaluate primarily extremity function in our scoring system and exclude the evaluation of cranial nerve function in rodents. According to our present data we observed higher neurological impairment if chemotherapy was applied after tumor cell implantation compared to carboplatin application alone. This dramatically shows the limited functional compliance of the eloquent brainstem anatomy. Furthermore, we observed in later stages of tumor progression abnormal behavior like lateral tilting of the body as a precursor for lateral axial rotation. These were interpreted as signs for rapid neurological deterioration. Thus, they were included in the neurological scoring system. Our scoring system did correlate significantly with survival, thereby showing its quality as prognostic evaluation factor. We could also show significant differences in carboplatin-induced neurotoxicity predominantly in the early phase of treatment. This was most obvious in the high-dose carboplatin one cannula group with highest local concentration of carboplatin in the tissue. Nevertheless, survival was influenced by low dose as well as high dose of carboplatin delivery. In the higher dose group, however with the result of early functional impairment. Thus, our investigation emphasizes the need of functional evaluation in the rat brainstem tumor model to investigate not only efficacy but also functional quality of survival in the animals. Agents for local delivery in the brainstem can thereby be quantified for low neurotoxic effect as quality of their treatment modality.
We evaluated the extent of tumor growth in our model using MR imaging as well as histological staining. Histological evaluation has been performed in earlier studies [7, 16, 26]. In our current study we found that local delivery of carboplatin did not result in solid tumor erradication but in diminished cell density of F98 cells within the brainstem. However, MR imaging showed demarcated regions of blood brain barrier leakage at the site of tumor with contrast enhancement, which was less exaggerated in treated animals. On higher magnification of histology of the stage of primarily solid tumor growth, a limited infiltrative pattern of the F98 cell type was seen. This emphasizes that other cell lines might be superior in modelling the human disease of diffuse pontine glioma. The factor of only limited survival time in this model might impair the possibility to show beneficial effects of potent antitumoral agents.
Conclusion
Local chemotherapy in the brainstem glioma model showed significant efficacy for survival and tumor extension. Our neurological grading enables quantification of drug and tumor-related morbidity as important factor for functional performance during therapy.
References
Attenello FJ, Mukherjee D, Datoo G, McGirt MJ, Bohan E, Weingart JD, Olivi A, Quinones-Hinojosa A, Brem H (2008) Use of Gliadel (BCNU) wafer in the surgical treatment of malignant glioma: a 10-year institutional experience. Ann Surg Oncol 15(10):2887–2893
Barth RF (1998) Rat brain tumor models in experimental neurooncology: the 9L, C6, T9, F98, RG2 (D74), RT-2 and CNS-1 gliomas. J Neurooncol 36:91–102
Bederson JB, Pitts LH, Tsuji M, Nishimura MC, Davis RL, Bartkowski H (1986) Rat middle cerebral artery occlusion: evaluation of the model and development of a neurologic examination. Stroke 17(3):472–476
Bernier-Chastagner V, Grill J, Doz F, Bracard S, Gentet JC, Marie-Cardine A, Luporsi E, Margueritte G, Lejars O, Laithier V, Mechinaud F, Millot F, Kalifa C, Chastagner P (2005) Topotecan as a radiosensitizer in the treatment of children with malignant diffuse brainstem gliomas: results of a French Society of Paediatric Oncology Phase II Study. Cancer 104(12):2792–2797
Brem S, Tyler B, Li K, Pradilla G, Legnani F, Caplan J, Brem H (2007) Local delivery of temozolomide by biodegradable polymers is superior to oral administration in a rodent glioma model. Cancer Chemother Pharmacol 60(5):643–650
Carson BS Sr, Wu Q, Tyler B, Sukay L, Raychaudhuri R, DiMeco F, Clatterbuck RE, Olivi A, Guarnieri M (2002) New approach to tumor therapy for inoperable areas of the brain: chronic intraparenchymal drug delivery. J Neurooncol 60(2):151–158
Degen JW, Walbridge S, Vortmeyer AO, Oldfield EH, Lonser RR (2003) Safety and efficacy of convection-enhanced delivery of gemcitabine or carboplatin in a malignant glioma model in rats. J Neurosurg 99(5):893–898
Dunn IF, Black PM (2003) The neurosurgeon as local oncologist: cellular and molecular neurosurgery in malignant glioma therapy. Neurosurgery 52(6):1411–1422
Epstein F, Wisoff JH (1988) Intrinsic brainstem tumors in childhood, surgical indications. J Neurooncol 6:309–317
Ferguson SD, Foster K, Yamini B (2007) Convection-enhanced delivery for treatment of brain tumors. Expert Rev Anticancer Ther 7(12 Suppl):79–85
Fernández-Hidalgo OA, Vanaclocha V, Vieitez JM, Aristu JJ, Rebollo J, Gúrpide A, Aramendía JM, Moreno-Palanques R, Martín-Algarra S, Subirá ML, Brugarolas A (1996) High-dose BCNU and autologous progenitor cell transplantation given with intra-arterial cisplatinum and simultaneous radiotherapy in the treatment of high-grade gliomas: benefit for selected patients. Bone Marrow Transplant 18(1):143–149
Freeman CR, Krischer J, Sanford RA, Burger PC, Cohen M, Norris D (1988) Hyperfractionated radiotherapy in brain stem tumors: results of a Pediatric Oncology Group study. Int J Radiat Oncol Biol Phys 15:311–318
Freeman CR, Krischer JP, Sanford RA, Cohen ME, Burger PC, del Carpio R, Halperin EC, Munoz L, Friedman HS, Kun LE (1993) Final results of a study of escalating doses of hyperfractionated radiotherapy in brain stem tumors in children: a Pediatric Oncology Group study. Int J Radiat Oncol Biol Phys 30;27(2):197–206
Hall WA, Doolittle ND, Daman M, Bruns PK, Muldoon L, Fortin D, Neuwelt EA (2006) Osmotic blood-brain barrier disruption chemotherapy for diffuse pontine gliomas. J Neurooncol 77(3):279–284
Hashizume R, Ozawa T, Gryaznov SM, Bollen AW, Lamborn KR, Frey WH 2nd, Deen DF (2008) New therapeutic approach for brain tumors: intranasal delivery of telomerase inhibitor GRN163. Neuro Oncol 10(2):112–120
Jallo GI, Becker M, Liu YJ, Carson BS Sr, Guarnieri M (2006) Local infusion therapy in the monkey brainstem: technical considerations. Surg Technol Int 15:311–316
Jallo GI, Volkov A, Wong C, Carson BS Sr, Penno MB (2006) A novel brainstem tumor model: functional and histopathological characterization. Childs Nerv Syst 22(12):1519–1525
Jallo GI (2006) Brainstem gliomas. Childs Nerv Syst 22(1):1–2
Kunwar S (2003) Convection enhanced delivery of IL13-PE38QQR for treatment of recurrent malignant glioma: presentation of interim findings from ongoing phase 1 studies. Acta Neurochir Suppl 88:105–111
Lidar Z, Mardor Y, Jonas T, Pfeffer R, Faibel M, Nass D, Hadani M, Ram Z (2004) Convection-enhanced delivery of paclitaxel for the treatment of recurrent malignant glioma: a phase I/II clinical study. J Neurosurg 100(3):472–479
Lonser RR, Warren KE, Butman JA, Quezado Z, Robison RA, Walbridge S, Schiffman R, Merrill M, Walker ML, Park DM, Croteau D, Brady RO, Oldfield EH (2007) Real-time image-guided direct convective perfusion of intrinsic brainstem lesions. Technical note. J Neurosurg 107(1):190–197
Murad GJ, Walbridge S, Morrison PF, Garmestani K, Degen JW, Brechbiel MW, Oldfield EH, Lonser RR (2006) Real-time, image-guided, convection-enhanced delivery of interleukin 13 bound to pseudomonas exotoxin. Clin Cancer Res 12(10):3145–3151
Pöpperl G, Goldbrunner R, Gildehaus FJ, Kreth FW, Tanner P, Holtmannspötter M, Tonn JC, Tatsch K (2005) O-(2-[18F]fluoroethyl)-L-tyrosine PET for monitoring the effects of convection-enhanced delivery of paclitaxel in patients with recurrent glioblastoma. Eur J Nucl Med Mol Imaging 32(9):1018–1025
Rousseau J, Boudou C, Barth RF, Balosso J, Estève F, Elleaume H (2007) Enhanced survival and cure of F98 glioma-bearing rats following intracerebral delivery of carboplatin in combination with photon irradiation. Clin Cancer Res 13(17):5195–5201
Sandberg DI, Edgar MA, Souweidane MM (2002) Convection-enhanced delivery into the rat brainstem. J Neurosurg 96(5):885–891
Souweidane MM, Occhiogrosso G, Mark EB, Edgar MA, Dunkel IJ (2004) Interstitial infusion of carmustine in the rat brain stem with systemic administration of O6-benzylguanine. J Neurooncol 67(3):319–326
Strege RJ, Liu YJ, Kiely A, Johnson RM, Gillis EM, Storm P, Carson BS, Jallo GI, Guarnieri M (2004) Toxicity and cerebrospinal fluid levels of carboplatin chronically infused into the brainstem of a primate. J Neurooncol 67(3):327–334
Thomale UW, Tyler B, Renard VM, Dorfman B, Guarnieri M, Haberl HE, Jallo GI (2008) Local chemotherapy in the rat brainstem with multiple catheters: a feasibility study. Childs Nerv Syst 9 (in press)
Vogelbaum MA, Sampson JH, Kunwar S, Chang SM, Shaffrey M, Asher AL, Lang FF, Croteau D, Parker K, Grahn AY, Sherman JW, Husain SR, Puri RK (2007) Convection-enhanced delivery of cintredekin besudotox (interleukin-13-PE38QQR) followed by radiation therapy with and without temozolomide in newly diagnosed malignant gliomas: phase 1 study of final safety results. Neurosurgery 61(5):1031–1037
Wagner S, Warmuth-Metz M, Emser A, Gnekow AK, Sträter R, Rutkowski S, Jorch N, Schmid HJ, Berthold F, Graf N, Kortmann RD, Pietsch T, Sörensen N, Peters O, Wolff JE (2006) Treatment options in childhood pontine gliomas. J Neurooncol 79(3):281–287
Walker DA, Punt JA, Sokal M (1999) Clinical management of brainstem glioma. Arch Dis Child 80:558–567
Wechsler H, Ramadan MA, Pfeiffer SE (1979) Morphologic and biochemical characteristics of transplantable neurogenic tumors induced by N-ethyl-N-nitrosourea in inbred BD IX rats. J Natl Cancer Inst 62:811–817
Westphal M, Ram Z, Riddle V, Hilt D, Bortey E (2006) Executive Committee of the Gliadel Study Group. Gliadel wafer in initial surgery for malignant glioma: long-term follow-up of a multicenter controlled trial. Acta Neurochir 148(3):269–275
Zausinger S, Hungerhuber E, Baethmann A, Reulen H, Schmid-Elsaesser R (2000) Neurological impairment in rats after transient middle cerebral artery occlusion: a comparative study under various treatment paradigms. Brain Res 863(1–2):94–105
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomale, U.W., Tyler, B., Renard, V. et al. Neurological grading, survival, MR imaging, and histological evaluation in the rat brainstem glioma model. Childs Nerv Syst 25, 433–441 (2009). https://doi.org/10.1007/s00381-008-0767-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-008-0767-5