Abstract
Mutations at the codon 132 in the isocitrate dehydrogenase 1 (IDH1) gene occur early, with a high frequency, in World Health Organization (WHO) grade II gliomas. We investigated the impact of IDH1 mutations on spontaneous glioma growth rate, known to be an early prognostic factor.The mean tumor diameter was assessed on the first MRI performed at diagnosis and on a second MRI, performed immediately before surgery, in a series of 64 WHO grade II gliomas. The patients did not undergo treatment before surgery. Because of a frequent association, we jointly analyzed the 1p19q co-deletion and IDH1 mutations effects on tumor velocity of diameter expansion (mm/year) during preoperative spontaneous growth period. 1p19q co-deletion had a significant slowing effect (p = 0.0133) on tumor growth estimated at −1.7760 ± 0.711 mm/year (95% CI −3.154, −0.366), whereas IDH1 mutations estimated effect of +0.036 ± 0.833 mm/year (95% CI −1.668; +1.596) was not significant (p = 0.9654). Our results provide first evidence that IDH1 mutations are not significantly involved in tumor growth rate. By contrast, we confirm that 1p19q co-deletion decreases growth velocity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent sequencing of the genome of glioblastomas identified novel mutations in the isocitrate dehydrogenase 1 gene (IDH1) in the highly conserved residue R132 [1]. The highest rates of IDH1 mutations, comprised between 73 and 100% depending on the series, have been reported in World Health Organization (WHO) grade II gliomas [2–4]. Watanabe et al. [3] showed that IDH1 mutations occur very early in low-grade gliomas.
WHO grade II gliomas (GIIG) are diffuse infiltrating tumors which inexorably progress to high grade. The timing of their evolution is quite unpredictable, making early prognostic markers essential to improve the therapeutic management. Until now, the prognosis value of IDH1 mutations was only investigated with survival as an end point [5–8]. In GIIG, IDH1 mutations were proved to have significant impact on overall survival only (OS). OS does not take into account the heterogeneity of therapeutic schemes experienced by the patients. This is all the more important as no consensus therapeutic management has been validated to date in GIIG. Finally, OS in GIIG can be as long as 15 and even 20 years. Therefore, OS is an inappropriate way to evaluate the impact of a molecular event on the first steps of a spontaneous tumor course. In contrast, the tumor growth kinetics directly evaluates the tumor behavior. The tumor growth is a continuous process [9], and a prognosis value has been assigned to growth rate [10]. When assessed before any treatment, including surgery, any influence of treatment is ruled out.
1p19q co-deletion is an independent favorable prognostic factor on OS as reported by many studies [11–17]. Moreover, a preliminary study on a short series showed an effect of 1p19q loss on GIIG spontaneous growth [18]. In addition, Labussiere et al. [19] reported that 1p19q complete deletion and IDH1/IDH2 mutations are closely associated. Thus, ignoring the effect of 1p19q on tumor growth rate while estimating the effect of IDH1, or vice versa, could lead to serious bias. Instead, we assessed the combined effects of IDH1 mutations and 1p19q loss on spontaneous tumor growth kinetics with a linear model.
Materials and methods
Patients
Patients were selected according to the following criteria: histological diagnosis of WHO grade II glioma, no treatment before surgery, and measurable tumor disease on at least two serial magnetic resonance imaging (MRI) examinations. The first MRI was performed at diagnosis and the second immediately before surgery in order to assess the tumor kinetics during the whole spontaneous growth period. The two MRIs were spaced by at least 3 months. Frozen tumor and blood DNA were available. Patients gave written informed consent. Sixty-four patients were eligible for this study.
Mean tumor diameter (MTD) estimation and evaluation of the MTD slope
The tumor volume was calculated on the basis of the three largest diameters (D1, D2, D3) on FLAIR or T2-weighted signal abnormalities according to the three orthogonal planes (axial, sagittal, and coronal). An estimation of the tumor volume was calculated by the ellipsoid approximation [V = (D1 × D2 × D3)/2] as described by Mandonnet et al. [9]. Volumes were converted into Mean Tumor Diameter [MTD = (2 × V)1/3]. The Velocity of Diameter Expansion (VDE) was evaluated by the mean annual growth rate (mm/year) between the two MRI measurements.
Molecular biology
Areas with tumor cell content superior to 60% were selected by pathologist examination. Tumour DNA was isolated according to a salting-out procedure [20]. Blood DNA was extracted from the patient’s EDTA peripheral blood using the MagNA Pure Compact robot (Roche Diagnostics, Mannheim, Germany).
1p19q Loss of heterozygosity
Blood and tumour DNA were genotyped for a panel of highly polymorphic microsatellite markers: on 1p (D1S2660, D41S450, D1S507, D1S234, D1S2890, D1S230, D1S207, D1S206) and 19q (D19S414, D19S420, D19S903, D19S571) provided by the ABI Prism Linkage Mapping Set 2.5 (Applied Biosystems, Foster City, USA).
IDH1 mutation screening
A fragment of 254 base pairs (bp) length spanning the catalytic domain of IDH1 including the codon 132 was amplified using the sense primer IDH1f 5′-ACCAAATGGCACCATACGA-3′ and antisense primer IDH1r 5′-TTCATACCTTGCTTAATGGGTGT-3′ in PCR conditions described by Balss et al. [21]. For confirmation, a 129-bp fragment was amplified by using the sense primer IDH1f’ 5′-CGGTCTTCAGAGAAGCCATT-3′ and the antisense primer IDH1r’ 5′-GCAAAATCACATTATTGCCAAC-3′ at the same conditions as for the first primers set. After purification (multiscreen PCR plates; Millipore, Corrigtwohill, Co.Cork, Ireland), the 254-bp fragments were submitted to the sequencing reaction using the Big Dye Terminator v 1.1.sequencing kit (Applied Biosystems, Foster City, USA) with the sense primer IDH1f. A second round of sequencing using the antisense primer IDH1r′ was performed on the 129-bp fragment in each case of unclear sequences for codon 132.
Immunohistochemistry for p53 and Ki67 expression detection on paraffin-embedded tissue
Since overexpression of p53 protein reflects to some extent the TP53 gene mutations status, we used protein immunostaining as a handing practice to evaluate the mutation rate of the TP53 gene [22–25]. Antigen retrieval for p53 and Ki67 staining was done using EDTA, pH 7–8. Monoclonal antibodies for p53 (Ménarini Diagnostics, Florence, Italy) and Ki67 (Dako, Glostrup, Denmark) were used at dilutions 1:40 and 1:100, respectively. Labeled streptavidin biotin kit was used as detection system (Benchmark Ultra; Ventana Medical Systems, Tucson, AZ, USA). For p53, cases where more than 10% of nuclei showed positivity were considered as positive. Immunopositive cases were graded from 1+ to 3+ as follows: 1+ positivity: 11–33% cells stained; 2+ positivity: 33–66% cells stained; 3+ positivity: 66–100% cells stained. For Ki67 staining, areas of highest cellularity were used for quantization. The percentage of labeled cells was determined from a count of 100 cells. The retained Ki67% labeling was assessed in the area with the highest level of proliferation.
Statistical analysis
Pearson’s Chi-square and Fisher’s exact tests were used to relate IDH1 mutations status with other molecular characteristics, histological type, localization and volume at diagnosis of the tumors and age of the patients, considering two groups in each case. Chi-square was performed when all the expected cell counts under null hypothesis were at least 5. Otherwise, Fisher’s exact test was performed instead. We then studied the simultaneous influence of IDH1 mutation and 1p19q deletion on the glioma growth rate. Separating between the effects of two or more factors influencing a common factor has been elucidated by Fisher [26] with the analysis of variance of factorial experiments, and its scope could be extended by Yates [27, 28] to unbalanced data. This is the case here as 1p19q deletion and IDH1 mutation are not independent.
Tumor growth was supposed to follow the standard linear model for a two-way analysis of variance without interaction; that is to say, the effects of IDH1 mutation and 1p19q mutation are supposed to add up:
where Y i is the glioma growth rate of patient i, a is the effect of IDH1 mutation, b is the effect of 1p19q deletion, 1 IDH1 (i) is the indicator of an IDH1 mutation on patient i, 11p19q (i) is the indicator of a 1p19q deletion on patient i, and E i is a random variation.
Because of the presence of several outliers in the growth rates, we replaced the analysis of variance for this model with a robust method, the M-estimation [29] that is not sensitive to a reasonable number of outliers. This M-estimation was carried out using the Robustreg procedure of the version 9.2 of SAS software (SAS Institute, Cary, NC, USA).
Results
Patient demographics and clinical characteristics
All the 64 patients included in this study underwent surgery for a WHO grade II glioma. No chemotherapy or radiotherapy was performed before surgery in this series. The sex ratio was 1.78 (41 men and 23 women). The median age at diagnosis was 36.5 years and the median follow-up duration of spontaneous growth was 10 months. The median tumor volume evaluated on the MRIs performed at diagnosis was 39.5 cm3, while it was 53.5 cm3 on immediate preoperative MRI. No contrast enhancement was seen in any of the tumors. The median tumor growth kinetics (VDE) was 3.5 mm/year in accordance with other reports [9, 10, 30]. A summary of patient clinical data is given in Table 1.
Histological and molecular characteristics of the tumors
The distribution of histological subtypes was balanced in our series: 33% of oligodendrogliomas (21/64), 33% of oligoastrocytomas (21/64), and 34% of astrocytomas (22/64). IDH1 mutations were present in 52 (81%) of the 64 patients. The most frequently found mutation of IDH1 gene was G395A (Arg132His) retrieved in 85% (44/52) of the cases. In other cases, mutations occurred at C394 nucleotide with a C > G (4/52, 8%), a C > T (2/52, 4 %) or a C > A (2/52, 4%) changes. IDH1 mutations were mainly associated with oligodendrogliomas (95% of mutation rate). The IDH1 mutations were less frequent in oligoastrocytomas and astrocytomas (80 and 68%, respectively); however, this difference did not reach significance (Fisher’s exact test, p = 0,067). Thirty percent (19/64) of the tumors displayed a complete 1p19q co-deletion. As expected, 1p19q complete co-deletion was more frequent in oligodendroglioma than in oligoastrocytoma and astrocytoma (χ 2 test, p < 0,001). In the same way, p53 overexpression was more frequent in both oligoastrocytomas and astrocytomas than in oligodendrogliomas (χ 2 test, p < 0,001), being found in 54% (32/60) of all tumors and with a higher frequency of 70% in both oligoastrocytomas and astrocytomas.
The data are summarized in Table 2.
Correlation of IDH1 mutation status with clinical and molecular characteristics of tumors
Comparison of IDH1 mutations rate in tumors with or without 1p19q complete co-deletion or in tumors with or without p53 overexpression did not show statistically significant differences. The insula was the most frequent brain location of our series nevertheless the IDH1 mutation rate was not significantly dependent on location (χ 2 test p = 0.15). IDH1 mutations had no influence on tumor volume or age of the patients at diagnosis. All the data and statistical analyses relative to correlation of IDH1 mutation status and tumors characteristics are compiled in Table 3.
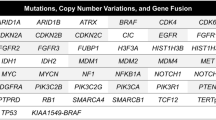
Combined effect of IDH1 mutations and 1p19q complete deletion on VDE
The 1p19q co-deletion effect on growth rate was estimated at −1.7760 ± 0.711 mm/year (95 % CI −3.154, −0.366), thus significantly decreasing the effect (p = 0.0133). By contrast, the effect of IDH1 mutations on growth rate was not significant (p = 0.9654): it was estimated at +0.036 ± 0.833 mm/year (95% CI −1.668; +1.596). A scatter plot of VDE (mm/year) versus genotype is shown in Fig. 1 together with the means and SEM of VDE in each of the four groups.
Tumors have been divided into four groups according to IDH1 mutation (mutated, wild-type) and 1p19q (complete co-deletion, no complete co-deletion) genotypes. No complete 1p19q co-deleted tumors are tumors with partial deletion or no deletion in 1p and 19q chromosomes. The mean annual growth rate for each group is reported with corresponding standard error of the mean (SEM)
Discussion
The prognosis impact of IDH1 mutations has been investigated in several studies with a reported favorable effect on glioma outcome [5, 7, 8]. Conversely, Kim et al. [6], on the largest series of WHO grade II gliomas studied to date, reported a conflicting result: IDH1/2 mutations were devoid of significant effects on prognosis in their study. All these studies were conducted with overall survival and progression-free survival as main assessment criteria.
Until now, no study has focused on the spontaneous tumor growth rate (TGR). TGR is a direct way to estimate tumor behavior by exempting evaluation from treatment influences. Previously, a prognosis value has been demonstrated for mean tumor diameter assessment over time [10]. We used the dynamic analysis of WHO grade II gliomas growth to evaluate the impact of genetic changes occurring during gliomagenesis. In the same experimental conditions, considering the respective influence of each factor by means of a robust two-way analysis of variance, 1p19q co-deletion slowed down the tumor growth while IDH1 mutations did not have a significant effect. The significant effect of 1p19q deletion did not appear in t test group mean comparisons (see Fig. 1 group means and SEM), as this method is less powerful than the proper two-way analysis of variance, and the power is further impaired by the outliers which conversely do not influence the M-estimation. Limitations of the study are the size of the series (n = 64 patients) and the time interval of follow-up between the two serial MRIs (median 10 months). A larger series could have allowed the detection of a possible slight effect of IDH1 mutations on tumor growth. Concerning spontaneous growth follow-up duration, it is difficult to increase its length because the present therapeutic management of low-grade gliomas has moved from a “wait and see” attitude towards an early treatment implementation.
Recently reported studies confirm our results concerning IDH1 mutations effects: in the work of Kim et al. [6], using overall survival as prognosis indicator, IDH mutations did not probe to improve survival. A recent work from Houllier et al. [7] reported a questionable effect of IDH1/2 mutations on tumor spontaneous re-growth after surgery in patients who did not have adjuvant chemotherapy or radiotherapy. Even though surgery is known to have an actual impact on natural history of gliomas [31], this finding relating to re-growth in the absence of treatment trends towards the same results as ours on spontaneous preoperative growth.
For 1p19q co-deletion, our data confirm, but in a three-fold larger homogeneous series, previous findings [18]. In that study, the reported mean tumor growth rate was 3.4 mm/year in 1p19q co-deleted tumors versus 5.9 mm/year in non-deleted 1p19q tumors (p = 0.0016). So, if 1p19q co-deletion and slower natural progression of disease are linked together, it could be anticipated that 1p19q status is a prognosis factor per se. Taking into account the 1p19q co-deletion effect on tumor growth might provide some help in deciphering the intricate effects of 1p19q co-deletion on favorable outcome: is it an intrinsic prognosis factor or a chemosensitivity marker?
A high degree of association between IDH1/2 mutations and 1p19q complete co-deletion has been reported by several studies [7, 8, 19]. It was reported as a systematic association in one of these studies mixing gliomas from all WHO grades [19]. However, in our series, some of the 1p19q co-deleted tumors were not IDH1 mutated. It is noteworthy that we did not perform IDH2 gene mutations research. IDH2 mutations are almost never associated with IDH1 mutations and retrieved rarely in about 2–3% of gliomas [4]. In a series of 360 low-grade gliomas, Kim et al. [6] retrieved 10% of 1p19q co-deleted tumors without IDH1 or IDH2 mutations. So, IDH2 mutations screening would possibly have increased the number of 1p19q co-deleted tumors harboring mutated IDH genes, but very little. Because of the strong association between these two molecular hallmarks, the prognosis value of each of them could interfere with the other. We thus performed a two-way analysis of variance with IDH1 mutations and 1p19q co-deletion as co-factors to eliminate 1p19q loss influence. With regard to spontaneous tumor growth rate, 1p19q loss had an effect whereas IDH1 mutations did not. On overall survival, Sanson et al. [5] showed a favorable effect of IDH1 mutations and 1p19q co-deletion in a study with numerous factors. In order to eliminate the influence of 1p19q co-deletion in their study of IDH mutations impact on overall survival, Metellus et al. [8] confirmed the first results obtained on the whole series by performing a second statistical analysis only on 1p19q non-co-deleted tumors. But then the size of the series restricted to 1p19q non-co-deleted tumors was greatly reduced, decreasing the statistical power.
IDH1 enzyme is involved in a fundamental metabolic pathway converting isocitrate, from the tricarboxylic acid cycle, in α-ketoglutarate. The codon 132 IDH1 gene mutations impair the enzymatic activity with a decrease of α-ketoglutarate and an induced illicit increase of 2-hydroxyglutarate levels [32]. These metabolic disruptions have many presumed consequences. Very recently, a functional study of metabolic impairments resulting from IDH1 mutations showed that they affected the in vivo activity of α-ketoglutarate-dependent dioxygenases such as histone demethylases and TET 5-methylcytosine hydroxylases [33]. Xu et al. concluded that consequential alteration of histone and DNA methylation may contribute to tumorigenesis through altering epigenetic control and the fates of stem or progenitor cells. This is in accordance with a previous report of Noushmer et al. that described a CpG island methylator phenotype displaying a genome-wide hypermethylation pattern and defining a distinct subgroup of glioma tightly associated with IDH1 mutations. Patients harboring gliomas of this subgroup experienced a significantly improved outcome [34]. The epigenetic landscape of cancer cells is profoundly distorted. These epigenetic alterations have a crucial early role in cancer spread because they might determine subsequent genetic changes. Therefore, the hypothesis of IDH1 mutations creating metabolic disturbances with widespread repercussions on epigenetic and secondarily on genetic programs of the tumor cell would fit with favorable prognostic impact of these mutations in spite of a lack of effect on spontaneous tumor growth.
In a preliminary study, Push et al. [35] described a secondary glioblastoma resulting from the malignant transformation from an IDH1 R132H-mutated WHO grade II astrocytoma in which the mutated IDH1 R132H allele failed to be detected by immunochemistry. This suggests that IDH1 R132H mutation is not essential to maintain malignant phenotype at least in late stages. This observation reinforces the hypothesis that IDH1 mutations do not play an essential role in tumor growth. In spite of the loss of IDH1 R132H mutation, the tumor outburst occurred, leading to the ultimate transformation of low-grade glioma into WHO grade IV glioma.
A second hypothesis to explain the reported favorable impact of IDH mutations on overall survival could be that the metabolic changes they induce contribute to a more chemosensitive or radiosensitive cellular environment. In a first study, Dubbink et al. [36] showed that IDH1 mutations had no effect on response to temozolomide. More recently, Houillier et al. [7] reported the opposite result with an association between IDH mutations and response to temozolomide.
In summary, this study sheds a new light on IDH1 mutations and 1p19q co-deletion oncological consequences. Whereas we confirm that 1p19q loss displays a slowing effect on tumor spread in good accordance with a direct favorable impact of this chromosomal deletion on tumor natural history, we provide first evidence that IDH1 gene mutations do not have a sizable correlation with tumor growth. As a consequence, IDH1 mutations because of their precocity might be considered instead as a causative link between early cellular metabolism disturbances and the emergence of driving molecular events in gliomagenesis.
References
Parsons DW, Jones S, Zhang X, Lin JC, Leary RJ, Angenendt P, Mankoo P, Carter H, Siu IM, Gallia GL, Olivi A, McLendon R, Rasheed BA, Keir S, Nikolskaya T, Nikolsky Y, Busam DA, Tekleab H, Diaz LA, Hartigan J, Smith DR, Strausberg RL, Nagahashi Marie SK, Oba Shinjo SM, Yan H, Riggins GJ, Bigner DD, Karchin R, Papadopoulos N, Parmigiani G, Vogelstein B, Velculescu VE, Kinzler KW (2008) An integrated genomic analysis of human glioblastoma multiforme. Science 321:1807–1812
Yan H, Parsons DW, Jin G, McLendon R, Rasheed BA, Yuan W, Kos I, Batinic-Haberle I, Jones S, Riggins GJ, Friedman H, Friedman A, Reardon D, Herndon J, Kinzler KW, Velculescu VE, Vogelstein B, Bigner DD (2009) IDH1 and IDH2 mutations in gliomas. N Engl J Med 360:765–773
Watanabe T, Nobusawa S, Kleihues P, Ohgaki H (2009) IDH1 mutations are early events in the development of astrocytomas and oligodendrogliomas. Am J Pathol 174:1149–1153
Hartmann C, Meyer J, Balss J, Capper D, Mueller W, Christians A, Felsberg J, Wolter M, Mawrin C, Wick W, Weller M, Herold-Mende C, Unterberg A, Jeuken JW, Wesseling P, Reifenberger G, von Deimling A (2009) Type and frequency of IDH1 and IDH2 mutations are related to astrocytic and oligodendroglial differentiation and age: a study of 1,010 diffuse gliomas. Acta Neuropathol 118:469–474
Sanson M, Marie Y, Paris S, Idbaih A, Laffaire J, Ducray F, El Hallani S, Boisselier B, Mokhtari K, Hoang-Xuan K, Delattre JY (2009) Isocitrate dehydrogenase 1 codon 132 mutation is an important prognostic biomarker in gliomas. J Clin Oncol 27:4150–4154
Kim YH, Nobusawa S, Mittelbronn M, Paulus W, Brokinkel B, Keyvani K, Sure U, Wrede K, Nakazato Y, Tanaka Y, Vital A, Mariani L, Stawski R, Watanabe T, De Girolami U, Kleihues P, Ohgaki H (2009) Molecular classification of low-grade diffuse gliomas. Am J Pathol 177:2708–2714
Houillier C, Wang X, Kaloshi G, Mokhtari K, Guillevin R, Laffaire J, Paris S, Boisselier B, Idbaih A, Laigle-Donadey F, Hoang-Xuan K, Sanson M, Delattre JY (2010) IDH1 or IDH2 mutations predict longer survival and response to temozolomide in low-grade gliomas. Neurology 75:1560–1566
Metellus P, Coulibaly B, Colin C, de Paula AM, Vasiljevic A, Taieb D, Barlier A, Boisselier B, Mokhtari K, Wang XW, Loundou A, Chapon F, Pineau S, Ouafik L, Chinot O, Figarella-Branger D (2010) Absence of IDH mutation identifies a novel radiologic and molecular subtype of WHO grade II gliomas with dismal prognosis. Acta Neuropathol 120:719–729
Mandonnet E, Delattre JY, Tanguy ML, Swanson KR, Carpentier AF, Duffau H, Cornu P, Van Effenterre R, Alvord EC Jr, Capelle L (2003) Continuous growth of mean tumor diameter in a subset of grade II gliomas. Ann Neurol 53:524–528
Pallud J, Mandonnet E, Duffau H, Kujas M, Guillevin R, Galanaud D, Taillandier L, Capelle L (2006) Prognostic value of initial magnetic resonance imaging growth rates for World Health Organization grade II gliomas. Ann Neurol 60:380–383
Cairncross JG, Ueki K, Zlatescu MC, Lisle DK, Finkelstein DM, Hammond RR, Silver JS, Stark PC, Macdonald DR, Ino Y, Ramsay DA, Louis DN (1998) Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst 90:1473–1479
Dehais C, Laigle-Donadey F, Marie Y, Kujas M, Lejeune J, Benouaich-Amiel A, Pedretti M, Polivka M, Xuan KH, Thillet J, Delattre JY, Sanson M (2006) Prognostic stratification of patients with anaplastic gliomas according to genetic profile. Cancer 107:1891–1897
Jenkins RB, Blair H, Ballman KV, Giannini C, Arusell RM, Law M, Flynn H, Passe S, Felten S, Brown PD, Shaw EG, Buckner JC (2006) A t(1;19)(q10;p10) mediates the combined deletions of 1p and 19q and predicts a better prognosis of patients with oligodendroglioma. Cancer Res 66:9852–9861
Kujas M, Lejeune J, Benouaich-Amiel A, Criniere E, Laigle-Donadey F, Marie Y, Mokhtari K, Polivka M, Bernier M, Chretien F, Couvelard A, Capelle L, Duffau H, Cornu P, Broët P, Thillet J, Carpentier AF, Sanson M, Hoang-Xuan K, Delattre JY (2005) Chromosome 1p loss: a favorable prognostic factor in low-grade gliomas. Ann Neurol 58:322–326
Iwamoto FM, Nicolardi L, Demopoulos A, Barbashina V, Salazar P, Rosenblum M, Hormigo A (2008) Clinical relevance of 1p and 19q deletion for patients with WHO grade 2 and 3 gliomas. J Neurooncol 88:293–298
Mariani L, Deiana G, Vassella E, Fathi AR, Murtin C, Arnold M, Vajtai I, Weis J, Siegenthaler P, Schobesberger M, Reinert MM (2006) Loss of heterozygosity 1p36 and 19q13 is a prognostic factor for overall survival in patients with diffuse WHO grade 2 gliomas treated without chemotherapy. J Clin Oncol 24:4758–4763
van den Bent MJ, Looijenga LH, Langenberg K, Dinjens W, Graveland W, Uytdewilligen L, Sillevis Smitt PA, Jenkins RB, Kros JM (2003) Chromosomal anomalies in oligodendroglial tumors are correlated with clinical features. Cancer 97:1276–1284
Ricard D, Kaloshi G, Amiel-Benouaich A, Lejeune J, Marie Y, Mandonnet E, Kujas M, Mokhtari K, Taillibert S, Laigle-Donadey F, Carpentier AF, Omuro A, Capelle L, Duffau H, Cornu P, Guillevin R, Sanson M, Hoang-Xuan K, Delattre JY (2007) Dynamic history of low-grade gliomas before and after temozolomide treatment. Ann Neurol 61:484–490
Labussiere M, Idbaih A, Wang XW, Marie Y, Boisselier B, Falet C, Paris S, Laffaire J, Carpentier C, Criniere E, Ducray F, El Hallani S, Mokhtari K, Hoang-Xuan K, Delattre JY, Sanson M (2010) All the 1p19q codeleted gliomas are mutated on IDH1 or IDH2. Neurology 74:1886–1890
Miller SA, Dykes DD, Polesky HF (1988) A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res 16:1215
Balss J, Meyer J, Mueller W, Korshunov A, Hartmann C, von Deimling A (2008) Analysis of the IDH1 codon 132 mutation in brain tumors. Acta Neuropathol 116:597–602
Vet JA, Bringuier PP, Schaafsma HE, Witjes JA, Debruyne FM, Schalken JA (1995) Comparison of P53 protein overexpression with P53 mutation in bladder cancer: clinical and biologic aspects. Lab Invest 73:837–843
Anker L, Ohgaki H, Ludeke BI, Herrmann HD, Kleihues P, Westphal M (1993) p53 Protein accumulation and gene mutations in human glioma cell lines. Int J Cancer 55:982–987
Louis DN, von Deimling A, Chung RY, Rubio MP, Whaley JM, Eibl RH, Ohgaki H, Wiestler OD, Thor AD, Seizinger BR (1993) Comparative study of p53 gene and protein alterations in human astrocytic tumors. J Neuropathol Exp Neurol 52:31–38
Peraud A, Kreth FW, Wiestler OD, Kleihues P, Reulen HJ (2002) Prognostic impact of TP53 mutations and P53 protein overexpression in supratentorial WHO grade II astrocytomas and oligoastrocytomas. Clin Cancer Res 8:1117–1124
Fisher RA (1925) Statistical methods for research workers. Oliver and Boyd, Edinburgh
Yates F (1933) The principles of orthogonality and confounding in replicated experiments. J Agric Sci 23:108–145
Yates F (1934) The analysis of multiple classifications with unequal numbers in the different classes. J Am Stat Soc 29:51–66
Huber PJ (1973) Robust regression: asymptotis, conjecture and Monte Carlo. Ann Stat 1:799–821
Mandonnet E, Pallud J, Fontaine D, Taillandier L, Bauchet L, Peruzzi P, Guyotat J, Bernier V, Baron MH, Duffau H, Capelle L (2010) Inter- and intrapatients comparison of WHO grade II glioma kinetics before and after surgical resection. Neurosurg Rev 33:91–96
Smith JS, Chang EF, Lamborn KR, Chang SM, Prados MD, Cha S, Tihan T, Vandenberg S, McDermott MW, Berger MS (2008) Role of extent of resection in the long-term outcome of low-grade hemispheric gliomas. J Clin Oncol 26:1338–1345
Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM, Fantin VR, Jang HG, Jin S, Keenan MC, Marks KM, Prins RM, Ward PS, Yen KE, Liau LM, Rabinowitz LC, Thompson CB, Vander Heiden MG, Su SM (2009) Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature 462:739–744
Xu W, Yang H, Liu Y, Yang Y, Wang P, Kim SH, Ito S, Yang C, Wang P, Xiao MT, Liu LX, Jiang WQ, Liu J, Zhang JY, Wang B, Frye S, Zhang Y, Xu YH, Lei QY, Guan KL, Zhao SM, Xiong Y (2011) Oncometabolite 2-hydroxyglutarate is a competitive inhibitor of alpha-ketoglutarate-dependent dioxygenases. Cancer Cell 19:17–30
Noushmehr H, Weisenberger DJ, Diefes K, Phillips HS, Pujara K, Berman BP, Pan F, Pelloski CE, Sulman EP, Bhat KP, Verhaak RG, Hoadley KA, Hayes DN, Perou CM, Schmidt HK, Ding L, Wilson RK, Van Den Berg D, Shen H, Bengtsson H, Neuvial P, Cope LM, Buckley J, Herman JG, Baylin SB, Laird PW, Aldape K, Cancer Genome Atlas Research Network (2010) Identification of a CpG island methylator phenotype that defines a distinct subgroup of glioma. Cancer Cell 17:510–522
Pusch S, Sahm F, Meyer J, Mittelbronn M, Hartmann C, Von Deimling A (2011) Glioma IDH1 mutation patterns off the beaten track. Neuropathol Appl Neurobiol 37:428–430
Dubbink HJ, Taal W, van Marion R, Kros JM, van Heuvel I, Bromberg JE, Zonnenberg BA, Zonnenberg CB, Postma TJ, Gijtenbeek JM, Boogerd W, Groenendijk FH, Sillevis Smith PA, Dinjens WN, van den Bent MJ (2009) IDH1 mutations in low-grade astrocytomas predict survival but not response to temozolomide. Neurology 73:1792–1795
Acknowledgment
This work was supported by a grant of the Ligue Nationale contre le Cancer, Comité du Gard, France.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gozé, C., Bezzina, C., Gozé, E. et al. 1P19Q loss but not IDH1 mutations influences WHO grade II gliomas spontaneous growth. J Neurooncol 108, 69–75 (2012). https://doi.org/10.1007/s11060-012-0831-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-012-0831-6