Abstract
Recurrent diffuse intrinsic pontine gliomas (DIPG) are traditionally treated with palliative care since no effective treatments have been described for these tumors. Recently, clinical studies have been emerging, and individualized treatment is attempted more frequently. However, an informative way to compare the treatment outcomes has not been established, and historical control data are missing for recurrent disease. We conducted a retrospective chart review of patients with recurrent DIPG treated between 1998 and 2010. Response progression-free survival and possible influencing factors were evaluated. Thirty-one patients were identified who were treated in 61 treatment attempts using 26 treatment elements in 31 different regimens. The most frequently used drugs were etoposide (14), bevacizumab (13), irinotecan (13), nimotuzumab (13), and valproic acid (13). Seven patients had repeat radiation therapy to the primary tumor. Response was recorded after 58 treatment attempts and was comprised of 0 treatment attempts with complete responses, 7 with partial responses, 20 with stable diseases, and 31 with progressive diseases The median progression-free survival after treatment start was 0.16 years (2 months) and was found to be correlated to the prior time to progression but not to the number of previous treatment attempts. Repeat radiation resulted in the highest response rates (4/7), and the longest progression-free survival. These data provide a basis to plan future clinical trials for recurrent DIPG. Repeat radiation therapy should be tested in a prospective clinical study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
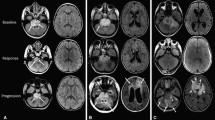
Pediatric diffuse intrinsic pontine gliomas (DIPGs) are frequent and devastating tumors typically occurring at school age. The diagnosis is typically defined based on clinical symptoms and radiographic appearance [1–4]. The typical MRI morphology of a DIPG is a non-enhancing enlarged pons with homogeneous low signal intensity on T1-weighted images, high signal intensity on T2-weighted images [5], and distinct patterns in DTI fiber tracking [6], which also provides prognostic information [7]. Surgical interventions have not been recommended because complete resection is impossible and any manipulation of the pons is associated with a high risk of severe neurological deficits [1, 4, 8]. In addition, the histological results from pathologic specimens have not been found to be of prognostic relevance [9]: Grade II (WHO) astrocytic tumors have a relatively favorable prognosis in other locations in the brain, yet the same histological finding in the pons is linked to a very poor prognosis. DIPGs often shrink in response to conformal radiation therapy of 54–60 Gy with improvement of patients’ symptoms [10], but the median time to progression is only 5–6 months after radiation therapy with a median overall survival rate of less than 1 year [10–15]. Numerous prospective clinical trials have reported the use of chemotherapy prior to [16], instead of [17, 18] during [9] or after [10, 19, 20] radiation. Despite some possible minor benefit from chemotherapy for small subsets of patients [9], the dismal median overall survival times remains unchanged.
Recently, an increasing number of pediatric clinical studies have included patients with recurrent DIPGs. The first phase II studies specifically addressing this population have been conducted, but it is hard to judge the results because control groups are typically missing. Here, we summarize the experience of The University of Texas MD Anderson Cancer Center with treatments of recurrent DIPG. In a retrospective chart review we evaluated response and event-free survival (EFS) in patients with recurrent pontine glioma, and we considered possible influencing factors to build a basis for further studies.
Methods
After obtaining institutional review board (IRB) approval, a retrospective chart review was conducted for all patients treated at MD Anderson Cancer Center with tumor locations in the brain stem. This study was performed independently of previous analyses by the same group [21, 22]; it had different objectives, separate IRB applications, independent data accumulations and novel statistical methods, although the patient data and source of information were overlapping. Eligibility criteria for this analysis included a tumor centered in the pons, with radiographic appearance as described above, that had been previously treated, and was recurrent or progressive. Exclusion criteria were surgical treatment of the recurrence and unclear documentation of treatment. We did not exclude patients treated partially in collaborating institutions as long as the patient was also a formal patient at the MD Anderson Cancer Center. The medical records, treatment history, and all available MRI scans were reviewed.
Tumor response was classified as complete response (CR, disappearance of all measurable tumor on diagnostic imaging), partial response (PR, relevant shrinkage of at least 50%), stable disease (SD, no relevant change in tumor size), progressive disease (PD, tumor growth of at least 25%), and no data (ND). We used one-dimensional (largest measurable tumor diameter) measures if available. If quantitative measures were not available, we used radiology reports to come as close as possible to classifying the tumor response adequately. We evaluated responses using MRI scans taken 6 weeks after initiation of treatment, or the MRI scans taken closest to 6 weeks with limits of 2 weeks to 4 months after the beginning of the treatment. EFS times were defined as the time from date of start treatment to one of the following events: (1) tumor progression on MRI, (2) unquestionable deterioration of clinical symptoms, or (3) death. If two different treatments were given sequentially in one treatment plan without evaluation in between, the responses to both were classified as ND, and the next reported event was used to terminate the EFS times for both.
Originally, we attempted to include clinical data in this retrospective analysis. Treatment changes based on unquestionable clinical deterioration were to be considered tumor progression (PD), and treatment success was to be measured in clinical improvement. However, this plan was not feasible because there was no case of clinical deterioration that resulted in treatment change without an MRI scan. Gathering quality-of-live data from the medical records was attempted in the pilot phase of the project but then had to be dropped because data had been reported inconsistently and a consensus on how to quantify them was not found. For instance, the dose of dexamethasone could not be used as surrogate for quality of life since there was a change in medical practice during the last 5 years of the observation period, during which dexamethasone was used less frequently.
Several patients were treated with multiple different regimens for multiple recurrences or progression after therapy. To capture these data, the database included one line per documented treatment attempt (as opposed to the traditional structure of one line per patient). Calculations were done using the Statistical Package for Social Studies (SPSS, v.16.0). The analysis was aimed as an observational and hypothesis generating study, not as conformal testing. Potential prognostic factors were analyzed in Kaplan–Meier curves [23], log-rank tests[24], and COX regression [25], ANOVA and Kruskal–Wallis analyses. As described in the “Results”, only the prior time to progression was found to be a useful factor for predicting future progression-free survival time. This factor was then used in a regression analysis to calculate the predicted progression-free survival for each treatment attempt assuming average outcome independent of treatment. The individually observed progression-free survival was compared with the predicted, and “EFS-gain” was defined as the difference between the two numbers. This difference was used to assess the efficacy of treatments.
Various treatment concepts and combinations were used in this study population. To allow the analysis of the effects of individual agents, patient groups were defined as having or not having a specific drug (independent of other elements of treatment). This analysis was repeated for each drug. Cross-tables and χ 2 tests were used to evaluate responses, and non-parametric Wilcoxon rank sum tests to evaluate EFS-gain. Because the patients had been treated with various combinations, the different drug comparisons had overlapping patient groups, and every result was re-evaluated for drug combinations as subgroups.
Results
The database documented 184 treatment regimens in 64 patients with DIPG excluding first-line treatments, surgical procedures, and treatments that were started without progressive disease after radiation therapy; 61 treatment attempts in 31 patients met the eligibility requirements for further analysis. Thirteen patients were male, 18 female. The mean age at diagnosis was 7.0 years (SD ± 3.2, median 6.1) and the mean age at the start of the first treatment reported here was 7.8 years (±3.2, median 6.5).
The tumors had progressed during 58 out of the 61 cases. The relapse therapy was the third-, fourth-, fifth-, sixth- and seventh-line strategy in 31, 15, 9, 2, and 4 patients, respectively. The following drugs were used: etoposide (n = 14), bevacizumab (n = 13), irinotecan (n = 13), valproic acid (n = 13), nimotuzumab (n = 13), temozolomide (n = 8), cetuximab (n = 5), rapamycin (n = 3), cis-retinoic acid (n = 2), labradimil (RPM-7, n = 2), cisplatin (n = 2), carboplatin (n = 2) vincristine (n = 2), lomustine (CCNU, n = 2), temsirolimus (n = 2), the notch inhibitor MK0752 (n = 1), cyclophosphamide (n = 1), Ruta6 (n = 1), procarbazine (n = 1), sorafenib (n = 1), topotecan (n = 1), vinorelbine (n = 1), celecoxib (n = 1), vitamin D (n = 1), and fenofibrate (n = 1). Repeat radiation therapy was used in 9 cases; in 7 of these, the primary irradiated tumor was re-treated, while in 2 cases metastatic or infiltrative sites not included in the previous radiation field were treated. The radiation to the primary field was given as photon beam radiation with single fractions of 2 Gy up to a total of 20 Gy (n = 4) or 18 Gy (n = 2), and 2 Gy (n = 1: withdrawn before completing the plan). The treatment protocols included 31 different drug combinations. For instance, bevacizumab was mostly given in combination with irinotecan (n = 6), but it was also combined with temsirolimus (n = 2), rapamycin (n = 1), radiation therapy (n = 1), and with multiple other drugs (n = 3). The most frequently used protocols were: nimotuzumab [26] monotherapy (n = 12), combinations of valproic acid/etoposide (n = 9), bevacizumab/irinotecan and cetuximab/irinotecan (n = 3). All other combinations were used only twice (4 combinations) or once (24 combinations).
Among 58 treatments available for response evaluation, there was no complete response in CR, 7 resulted in PR (12%), 20 resulted in SD 34 and 31 resulted in PD (53%). The response rate was independent of gender, patient age group, whether the previous recurrence had occurred on treatment or in a watch-and-wait period, or the number of previous treatments. Table 1 shows the responses in relation to the individual treatments. The response after repeat radiation therapy to the primary tumor appeared superior to that after other treatments. The radiation therapy to the metastatic sites resulted in stable disease at first, but both patients died of primary tumor progressions.
The median time to progression was 0.16 years (2 months): Four patients had no event recorded of their most recent treatment attempts; those data were censored at the last date of observation at 0.02 to 0.29 years (0 to 3.5 months). The EFS range for the other 57 treatments attempts was 0.01 to 0.92 years (mean 0.21 = 2.5 months). There was a detectable relation between response status and median EFS: Kaplan–Meier estimates were 0.33 years [standard error (SE) ±0.125], 0.21 years (SE ± 0.02), and 0.096 years (±0.005), for treatments resulting in PR, SD, or PD, respectively (P < 0.005 log-rank test).
There was a moderate but significant correlation between the progression-free survival time after the previous treatment and the progression-free survival after the current treatment (P = 0.026, ANOVA regression analysis). We did not detect any consistent influence on EFS of gender, age at diagnosis, age at treatment start, or time between diagnosis and recurrence, or of the number of previous treatments. As only the previous time to progression had a prognostic relevance, the individual predicted EFS was calculated based only upon that number. We used linear regression to calculate the predicted EFS, and the difference between the predicted and the observed EFS was defined as “EFS-gain”. This number was used to measure individual treatment effect (Table 1; Fig 1).
EFS time in recurrent DIPG in relation to previous time to progression in the same patients after the previous treatment attempt. The two numbers correlated. The lines indicate the deviation of the observed EFS from the predicted EFS based on the regression analysis. The length of these lines were defined as EFS-gain and used as measure for treatment success: points far above the regression line suggest effective treatments and points below less than average outcomes
Repeat radiation therapy to the primary tumor resulted in tumor shrinkage in 4 of 7 patients. When comparing this rate to the 5 of 52 patients who responded to protocols without radiation therapy to the primary tumor, the low P value suggests the observation to be relevant (P = 0.008, χ 2; Fig. 2). All these treatments were given as individualized treatment attempts as opposed to prospective formalized protocols, and radiation was never given as a single treatment. Additional treatments included: HIT-GBM-C protocol [25], temozolomide, sirolimus, valproic acid, cyclophosphamide combined with valproic acid, bevacizumab, and bevacizumab combined with irinotecan. Radiation therapy to the primary tumor gave the most consistent benefit regardless of which method was used for evaluation. Repeat irradiation was also linked to longer EFS, and comparing the EFS-gain to patients without repeat radiation gave a P value of 0.017, also suggesting relevant efficacy of repeat radiation therapy. These findings were different when radiation therapy was used for metastatic sites, which was without measurable effect but was done only twice.
EFS of patient treated with repeat radiation therapy to the primary tumor compared with patients treated with a variety of other protocols. This was not a hypothesis-driven protocol. If we had we formulated this comparison as a hypothesis before we did the analysis, than the data would have resulted in a P value of 0.019
None of the individual drugs therapies resulted in superior response rates that were significantly superior to those of other therapies.. Moderately higher median EFS was reported for intravenous cisplatin, intravenous etoposide, temozolomide, cetuximab temsirolimus, vincristine and nimotuzumab. Among those, temozolomide, cisplatin, intravenous etoposide and vincristine reached P values below 0.05. However, these drugs were often combined with other agents. Temozolomide, for example, was given to eight patients but was rarely given as a single agent. The drug had been combined with re-irradiation to the primary tumor, vincristine, cisplatin and etoposide, irinotecan, rapamycin, and lomustine.
Response to protocols containing bevacizumab was evaluable in 12 patients, 2 of whom responded to treatment, which was not different from the response rate to other treatments. In addition, both these patients had radiation therapy at the same time. The EFS was not different from that of the patients regardless which type of analysis was used.
Discussion
This retrospective chart review showed that 12% of recurrent DIPGs responded to treatment. The EFS varied between 1 month and 1 year, and the median time to progression was 0.16 years (2 months). This is the largest dataset so far published for recurrent pontine glioma and the result may serve a baseline for future studies. The most effective treatment was repeat radiation therapy, yet there is no long-term survivor documented in this retrospective chart review, indicating that outcomes are still far from acceptable.
There are obvious limitations to retrospective chart reviews. Several patients were not formally enrolled in prospective clinical trials, and therefore received heterogeneous treatment regimens. The most desirable endpoint for this patient population, quality of life, was not feasible in this setting. It was difficult to separate the effects of individual agents because patient groups using different drugs overlapped. However, prospective trials in which all patients are treated with the same protocol also do not provide data to separate the effects of single drugs. One strength of this analysis was that all patients were treated in the same institution. This minimized center effects, which may occur when at least two major institution follow different standards in undefined aspects of care. Also, there were no eligibility criteria which could specifically exclude certain patients with a poor prognosis, a problem increasingly common in both prospective cooperative trials and pharmaceutical drug development studies. Therefore, the data of an inclusive retrospective chart review realistically reflects this patient population. Well aware of these strengths and limitations, we aimed this project as a hypothesis-generating method, as opposed to a conformal hypothesis-driven clinical trial.
The choice of a study endpoint for comparing treatments should be disease specific. For instance, pseudoprogression which occurs more frequently after radiation could result in a bias favoring non-radiation treatments. In our analysis, response and EFS resulted in equivalent drug rankings, yet the quantification of EFS allowed more sensitive statistical tests. The most important observation—the effectiveness of repeat radiation therapy—was independent of the endpoint, and therefore not affected by the phenomenon of pseudoprogression.
It was surprising to us that neither the number of previous treatment attempts nor any of the traditional predictive factors such as age and gender had a relevant influence on the response or the EFS time in recurrent DIPG. We judge this as a result of selection: only tumors growing relatively slowly can be treated with eight different treatment concepts. These findings suggest that, even within the radiographically homogeneous population of DIPG, there are still considerable variations between individual tumors. The only factor found to be related to EFS in our data was the prior time to progression. Taking this into account allowed for a more precise comparison of treatment protocols.
The most relevant clinical finding was the tumor responsiveness to radiation therapy, the technical details of which are described separately [22] The repeat radiotherapy dose (20 Gy in 10 fractions) was much lower than the initial radiation (54 Gy in 30 fractions), which would predict a limited response in recurrent disease. We observed tumor response on MRI. Quantifying clinical improvement was impossible in this retrospective study and will remain to be shown in a future prospective trial. However, tumor shrinkage in the pons typically also results in an improvement of clinical signs [10], enabling patients to be able to walk and talk again. This radiation regimen only took 2 weeks of outpatient treatment making it worthwhile in the eyes of the patients and their parents. All our patients had other treatment in addition to the radiation therapy. We judge it unlikely that the additional chemotherapy was the primary reason for the response, as the drugs without radiation therapy did not show such results. However, it is possible that the response in some patients was also caused by radiosensitization.The effect of repeat radiation therapy remains insufficient and requires further study. This leads to the conclusion that repeat radiation therapy appears to be safe and should be explored as a component of a combination treatment possibly with novel radiosensitizers.
Our data indicated possible beneficial effects for temozolomide, cisplatin, etoposide, nimotuzumab and temsirolimus. This list includes drugs that were not successful when tested as first-line treatments for pontine glioma [27]; however, DIPG are not the same tumors when they recur. The former are often classified as low grade astrocytic tumors, while necrosis and vascular proliferation may be abundant in the latter, defining them as high grade gliomas. Hallmarks of the typical radiographic appearance of the primary tumors are homogeneity and lack of contrast enhancement, while recurrent DIPGs appear heterogeneous sometimes with leptomeningeal metastases and often with pronounced focal contrast enhancement [28]. It is therefore conceivable that the pattern of responsiveness also changes as the tumors recur. Some of these effects might also reflect treatment of necrosis. The data for bevacizumab found here were inconclusive, which is different from results of the drug in first-line treatment, where it was clearly not effective. Bevacizumab was reported to be effective to improve symptoms of radiation necrosis in pontine glioma patients [29, 30]. Recently, stereotactic biopsies were reported to be safe and effective for diagnostics in brain glioma patients [31], and it might be important to do them more frequently to reassess tumor histology and to guide treatment of recurrent disease.
Conclusion
Recurrent DIPGs can respond to treatment. The comparison of treatment results should take into account individual patients’ previous times to recurrence. Since DIPG remains incurable, new ways to study it are warranted. Clinical trials for patients with recurrent pontine glioma have rarely been attempted because a benefit for the patients was unlikely [32]. Conducting clinical trials in conjunction with reirradiation will allow improvement of quality of life and therefore enable further study of the disease. Our review of a large variety of treatment combinations for DIPG found repeat irradiation of the primary tumor to be the most beneficial. This retrospective analysis did not conclusively find a single drug to be effective, but it provided data which can serve as historical control data for future studies and insights as to how such data may be analyzed [33].
References
Rubin G, Michowitz S, Horev G et al (1998) Pediatric brain stem gliomas: an update. Childs Nerv Syst 14:167–173
Broniscer A, Gajjar A, Bhargava R et al (1997) Brain stem involvement in children with neurofibromatosis type 1: role of magnetic resonance imaging and spectroscopy in the distinction from diffuse pontine glioma. Neurosurgery 40:331–337, discussion 37–38
Broniscer A, Laningham FH, Sanders RP, Kun LE, Ellison DW, Gajjar A (2008) Young age may predict a better outcome for children with diffuse pontine glioma. Cancer 113:566–572
Mauffrey C (2006) Paediatric brainstem gliomas: prognostic factors and management. J Clin Neurosci 13:431–437
Hargrave D, Chuang N, Bouffet E (2008) Conventional MRI cannot predict survival in childhood diffuse intrinsic pontine glioma. J Neurooncol 86:313–319
Giussani C, Poliakov A, Ferri RT et al (2010) DTI fiber tracking to differentiate demyelinating diseases from diffuse brain stem glioma. Neuroimage 52:217–223
Chen X, Weigel D, Ganslandt O, Buchfelder M, Nimsky C (2007) Diffusion tensor imaging and white matter tractography in patients with brainstem lesions. Acta Neurochir (Wien) 149:1117–1131, discussion 31
Leach PA, Estlin EJ, Coope DJ, Thorne JA, Kamaly-Asl ID (2008) Diffuse brainstem gliomas in children: should we or shouldn’t we biopsy? Br J Neurosurg 22:619–624
Wagner S, Warmuth-Metz M, Emser A et al (2006) Treatment options in childhood pontine gliomas. J Neurooncol 79:281–287
Massimino M, Spreafico F, Biassoni V et al (2008) Diffuse pontine gliomas in children: changing strategies, changing results? a mono-institutional 20-year experience. J Neurooncol 87:355–361
Freeman CR, Krischer JP, Sanford RA et al (1993) Final results of a study of escalating doses of hyperfractionated radiotherapy in brain stem tumors in children: a pediatric oncology group study. Int J Radiat Oncol Biol Phys 27:197–206
Packer RJ, Boyett JM, Zimmerman RA et al (1993) Hyperfractionated radiation therapy (72 Gy) for children with brain stem gliomas. A childrens cancer group phase I/II trial. Cancer 72:1414–1421
Farmer JP, Montes JL, Freeman CR, Meagher-Villemure K, Bond MC, O’Gorman AM (2001) Brainstem gliomas. A 10-year institutional review. Pediatr Neurosurg 34:206–214
Freeman CR, Farmer JP (1998) Pediatric brain stem gliomas: a review. Int J Radiat Oncol Biol Phys 40:265–271
Fangusaro J (2009) Pediatric high-grade gliomas and diffuse intrinsic pontine gliomas. J Child Neurol 24:1409–1417
Wagner S, Reinert C, Schmid HJ et al High-dose methotrexate prior to simultaneous radiochemotherapy in children with malignant high-grade gliomas. Anticancer Res 252583–7
Finlay JL, Zacharoulis S (2005) The treatment of high grade gliomas and diffuse intrinsic pontine tumors of childhood and adolescence: a historical-and futuristic-perspective. J Neurooncol 75:253–266
Bouffet E, Khelfaoui F, Philip I, Biron P, Brunat-Mentigny M, Philip T (1997) High-dose carmustine for high-grade gliomas in childhood. Cancer Chemother Pharmacol 39:376–379
Wolff JE, Westphal S, Molenkamp G et al (2002) Treatment of paediatric pontine glioma with oral trophosphamide and etoposide. Br J Cancer 87:945–949
Wolff JE, Molenkamp G, Westphal S et al (2000) Oral trofosfamide and etoposide in pediatric patients with glioblastoma multiforme. Cancer 89:2131–2137
Zhang M, Segerer F, Ketonen L, Mahajan A, Wolff J (2008) Prediction of tumour regrowth of pontine glioma using a two-term model. Anticancer Res 28:741–9
Fontanilla HP, Pinnix CC, Ketonen LM et al (2011) Palliative reirradiation for progressive diffuse intrinsic pontine glioma. Am J Clin Oncol (in press)
Kaplan EL, Meier P (1958) Nonparametric estimation from incomplete observations. J Am Stat Assoc 53:457–481
Mantel N (1966) Evaluation of survival data and two new rank order statistics arising in its consideration. Cancer Chemother Rep 50:163–170
Cox C (1988) Multinomial regression models based on continuation ratios. Stat Med 7:435–441
Massimino M, Bode U, Biassoni V, Fleischhack G (2011) Nimotuzumab for pediatric diffuse intrinsic pontine gliomas. Expert Opin Biol Ther 11:247–256
Wolff JE, Driever PH, Erdlenbruch B et al (2010) Intensive chemotherapy improves survival in pediatric high-grade glioma after gross total resection: results of the HIT-GBM-C protocol. Cancer 116:705–712
Wagner S, Benesch M, Berthold F et al (2006) Secondary dissemination in children with high-grade malignant gliomas and diffuse intrinsic pontine gliomas. Br J Cancer 95:991–997
Liu AK, Macy ME, Foreman NK (2009) Bevacizumab as therapy for radiation necrosis in four children with pontine gliomas. Int J Radiat Oncol Biol Phys 75:1148–1154
Roujeau T, Machado G, Garnett MR et al (2007) Stereotactic biopsy of diffuse pontine lesions in children. J Neurosurg 107(1 Suppl):1–4
Perez-Gomez JL, Rodriguez-Alvarez CA, Marhx-Bracho A, Rueda-Franco F (2010) Stereotactic biopsy for brainstem tumors in pediatric patients. Childs Nerv Syst 26:29–34
Donaldson SS, Laningham F, Fisher PG (2006) Advances toward an understanding of brainstem gliomas. J Clin Oncol 24:1266–1272
Wolff JE, Classen CF, Wagner S et al (2008) Subpopulations of malignant gliomas in pediatric patients: analysis of the HIT-GBM database. J Neurooncol 87:155–164
Acknowledgment
This research is supported in part by the National Institutes of Health through MD Anderson’s Cancer Center Support Grant, CA016672.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The patient population presented here overlaps with earlier reports from the same institution as well as several clinical trials in which the patients were enrolled.
Rights and permissions
About this article
Cite this article
Wolff, J.E., Rytting, M.E., Vats, T.S. et al. Treatment of recurrent diffuse intrinsic pontine glioma: the MD Anderson Cancer Center experience. J Neurooncol 106, 391–397 (2012). https://doi.org/10.1007/s11060-011-0677-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-011-0677-3