Abstract
There is a paucity of data regarding patterns of progression in children with high-grade glioma (HGG) or diffuse intrinsic pontine glioma (DIPG) treated with bevacizumab (BVZ) at diagnosis. We performed a retrospective study of 20 children with HGG or DIPG who received BVZ-based therapy at diagnosis on, or according to, a bi-institutional study. Magnetic resonance imaging (MRI) characteristics of first and most recent progressions were reviewed. Comparison was made to a control group of 19 patients who never received BVZ. Imaging definitions of progressive disease (PD) were local: at primary site or within 2 cm, contiguous; diffuse: >2 cm away but contiguous with primary site, ill-defined and infiltrative; distant: new, non-contiguous disease. In the BVZ-treated group, 14 patients had DIPG, six patients had HGG. Median age was 7 years (range: 3–21). Median time to PD and follow-up were 8.8 months (range 4–21) and 11 months (range: 6–25), respectively. Among 14 patients with PD, 8 (57.1 %) had local PD, 6 (42.9 %) had local and diffuse/distant PD, at initial progression. At most recent progression, a median of 10.8 months (range 6-25) from diagnosis, 10 of 14 (71.4 %) had at least diffuse (n = 8), or distant (n = 6) PD. In the comparable control group, 15 patients had PD: 11(73.3 %) local, 4 (26.7 %) local and diffuse/distant PD at first and most recent progressions. Based on these data, we postulate that BVZ may lead to a higher incidence of distant and diffuse disease in newly-diagnosed children with HGG or DIPG who received BVZ-based therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The outcomes for children with high-grade gliomas (HGG) or diffuse intrinsic pontine gliomas (DIPG) remain uniformly poor [1, 2] despite multi-modal therapy with surgery when possible, radiation therapy (RT) and chemotherapy. Although RT has been successful in prolonging time to progression in children with DIPG [3], chemotherapy has had little impact on survival in children with HGG or DIPG [4–6].
Bevacizumab (Avastin; Genentech, San Francisco, CA) is a vascular endothelial growth factor (VEGF)-specific recombinant, humanized monoclonal antibody. It binds with high affinity and specificity to all four VEGF isoforms inhibiting it from binding to its receptors. HGG are highly vascularized tumors and VEGF plays a critical role in tumor angiogenesis in HGG [7] making it a rational therapeutic target in these tumors. Bevacizumab (BVZ) has gained interest in many HGG studies. In trials in adults with glioblastoma multiforme (GBM) [8, 9] single agent BVZ demonstrated durable objective responses earning accelerated FDA approval for second-line treatment of GBM in 2009. Unfortunately, patients with GBM and DIPG invariably progress. Patterns of progression for these patients can be classified as local, distant or diffuse invasive based on neuroimaging characteristics.
The pattern of failure of adult patients with GBM is predominantly local with a historical rate of diffuse progression of approximately 10 % [10] with conventional chemo-radiotherapy. Recently, a shift in the patterns of progression in patients with GBM treated with angiogenic blockade was reported. In newly-diagnosed or recurrent adult patients, Narayana et al. [11, 12] reported diffuse invasive recurrence in up to 75 % of patients who received BVZ-based regimens. Another trial, in which adults with recurrent HGG were treated with BVZ plus irinotecan, reported similar results with 60.5 % of patients having diffuse or distant progression [13]. More recent frontline Phase III trials (AVAglio [14] and Radiation Therapy Oncology Group study 0825 [15] ) have failed to demonstrate an increase in diffuse recurrence, making this phenomenon still controversial.
Pediatric studies have retrospectively reviewed patterns of DIPG and HGG progression and show conflicting results. Before the era of anti-angiogenic agents, Gururangan et al. [16] found that 17 % of patients with DIPG progressed with neuraxis metastases. On the other hand, Heideman et al. [17] and Vaidya et al. [18] reviewed patterns of progression in children with HGG and found that 31 and 46 % of patients progressed with neuraxis dissemination, respectively. A Pediatric Brain Tumor Consortium trial that administered BVZ-based therapy to children with recurrent HGG or DIPG [19] briefly described patterns of radiologic progression as being predominantly local. In contrast, a diffuse invasive recurrence pattern was noted in 45.5 % of 12 children with progressive HGG or DIPG treated with BVZ plus irinotecan [20] in another single institution study. In addition, in a series of 8 pediatric patients with recurrent HGG treated with different BVZ-containing regimens, five patients had progression with non-enhancing lesions and three patients progressed with distant disease [21].
To our knowledge, no studies have analyzed patterns of progression in children with newly-diagnosed HGG or DIPG receiving BVZ-based therapy. This study compares patterns of progression in children with HGG or DIPG who received front-line BVZ-based therapy to a control group of patients who never received BVZ.
Materials and methods
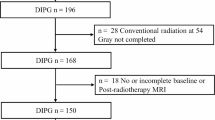
Institutional review board approval was obtained to perform this retrospective chart review analysis. The treatment group included patients ≥3 and <22 years of age diagnosed with HGG or DIPG between March 2009 and January 2013 who received BVZ-based therapy at initial diagnosis and were treated on, or according to, a study at Cincinnati Children’s Hospital Medical Center (CCHMC) or Anne and Robert Lurie Children’s Hospital. The control cohort included all patients ≥3 and <22 years of age diagnosed with DIPG or HGG from January 2000 until January 2014 at CCHMC. The cut-off point of January 2000 was used in order to have consistency in magnetic resonance imaging (MRI) techniques across both groups. To be included in the control group, patients must not have received BVZ at any time during their treatment and had to have adequate follow-up (defined as a minimum time of 9 months, since the median reported time-to-progression for DIPG patients ranges between 5 months and 8.8 months [2] ). Informed consent/assent was obtained upon enrollment on treatment protocol.
Briefly, patients with DIPG in the treatment group received local radiotherapy (54 Gy) with BVZ (10 mg/kg) every 2 weeks for 6 weeks, followed by a 4-week break, before maintenance therapy with BVZ (10 mg/kg) and irinotecan (125 mg/m2) every 2 weeks for 12 cycles. Radiation was delivered in 1.8 Gy daily fractions to the planned target volume (PTV) that included a 2 cm margin around the gross tumor volume (GTV). GTV was defined as the operative tumor bed in addition to any residual enhancing tumor and adjacent FLAIR signal abnormality. Therapy for children with HGG included resection/biopsy and localized radiotherapy (59.4 Gy). The regimen was otherwise identical to that described for the DIPG group, except that HGG patients also received temozolomide (90 mg/m2/dose) daily during radiation and temozolomide at a dose of 150 mg/m2/dose on days 1–5 of each cycle during maintenance.
Treatment for patients in the control cohort consisted of surgical resection when possible, localized RT (54–59.4 Gy) and a variety of adjuvant chemotherapeutic regimens (combination of cisplatin, vincristine, cyclophosphamide and etoposide, single agent capecitabine, temozolomide, vorinostat and oral cyclophosphamide).
Descriptive statistics summarizing the two cohorts are reported as medians, interquartile ranges (IQR), and frequencies. Differences in categorical and continuous variables were assessed with the Fisher exact and Wilcoxon rank sum tests, respectively. Differences in overall survival between patients with different disease progression patterns were assessed using the Log-Rank test.
Progressive disease (PD) was defined as a 25 % or more increase in the product of perpendicular diameters of any target lesion (taking as reference the smallest product observed since the start of treatment) or the appearance of one or more new lesions on MRI. Because RT may be associated with transient, reversible swelling during the first 3 months after therapy [22], an increase in the product of perpendicular diameters by 50 % was tolerated during that period.
MRI characteristics of first and last progressions were reviewed by the study neuroradiologist (J.L.). First progression was defined as the first time PD was radiologically detected and last progression corresponded to the pattern of progression at the time of the last available MRI. Definitions of patterns of PD (Fig. 1) were adapted from Zuniga et al. [13] and were as follows: local (at primary site or within 2 cm, contiguous), diffuse (>2 cm away but contiguous with primary site, ill -defined and infiltrative) and distant (new, non-contiguous enhancing or non-enhancing disease).
a Local Progression (Patient 2). Top: Initial tumor in the central pons (arrows). Middle: Decrease in size of signal and pons with treatment (arrows). Bottom: Increase in size of tumor signal and pons with no cerebellar or other distant disease identified (arrows). b Local, diffuse, and distant progression. (Patient 8) Top: Large tumor in the pons with some extension into the right middle cerebellar peduncle (arrows). Middle: Decrease in size of signal and pons with treatment. Bottom: Increase in size of signal of primary tumor site, new infiltrative ill-defined signal in cerebellar hemispheres (arrows, left), and new infiltrative, non-contiguous periventricular signal (arrows, right) consistent with distant progression. c Local, diffuse, and distant progression. (Patient 9) Top: Tumor occupying the pons with extension into the left middle cerebellar peduncle and left cerebellar hemisphere. Middle: Marked decrease in signal at the site of original tumor with return of pons to nearly normal size after treatment. Bottom Left Increased tumor signal at site of original tumor (arrowheads), ill-defined bilateral cerebellar signal changes (arrows) consistent with diffuse recurrence. Right: Ill-defined white matter and cortical signal changes in the frontal periventricular regions, corpus callosum, and basal ganglia (arrows)
Results
Patient and tumor characteristics-study group
Twenty patients met inclusion criteria in the BVZ treatment group and were included in the final analysis. Table 1 summarizes patient characteristics. Of 20 patients, 6 had HGG (stratum 1) and 14 had DIPG (stratum 2) (Table 2). One patient (patient 9 listed in Table 3) did not receive BVZ with radiation but received maintenance BVZ. Median age at enrollment was 10 years for stratum 1 (range: 3–17 years) and 6.5 years for stratum 2 (range: 3–21 years). Median follow-up was 11 months (range 6–25 months) for all patients who have progressed. Among 20 patients reviewed, 14 (70 %) had radiologic PD at the time of analysis. Median time to first progression was 8 months (range 4–21 months) for HGG and 9 months (range 5–14 months) for DIPG. Patients received a median number of 14 doses (range 2–26 doses) of BVZ (10 mg/kg/dose).
Patterns of progression-study group
Among 14 patients with PD (Table 3), eight patients (57.1 %; 7 DIPG and 1 HGG) had local PD, two patients (14.3 %; both HGG) had local and diffuse PD and four patients (28.6 %; 3 DIPG and 1 HGG) had local, diffuse and distant PD, at first progression. Patterns of distant PD at initial progression included hemispheric and periventricular (n = 2; DIPG) and non-contiguous hemispheric PD (n = 2; 1 DIPG and 1 HGG). Of the 13 patients with contrast MRI exams at first progression, seven had new or increasing contrast enhancement, three had decreased contrast enhancement and three had no enhancement within tumor regions. At the time of last PD, at a median time of 10.8 months (range 6–25 months) from diagnosis, 10 of 14 (71.4 %) had diffuse or distant PD. Among these 10 patients, four patients had local, diffuse and distant PD, four patients had local and diffuse PD and two patients had local and distant PD. None of the patients with distant PD had symptoms attributable to distant disease. There was no significant difference (p = 0.08) in the number of BVZ doses received between patients who had local PD (median number of doses = 10, IQR = 8.75–11.5) and patients who had diffuse or distant PD (median number of BVZ doses = 16, IQR = 12.75–18.5).
Two patients with DIPG (patients 8 and 9) had distant non-contiguous changes on brain MRI before the target lesion in the pons progressed. Patient 8 had white matter signal abnormalities that were hyperintense on T2/FLAIR sequences involving the frontal lobes bilaterally. These changes preceded the pontine tumor progression by approximately 3 months. Patient 9 had ill-defined regions of abnormal signal in the right frontal lobe and left frontal lobe and left periventricular white matter that appeared 8 months before the target lesion in the pons enlarged. MRI brain with spectroscopy was performed sequentially on one of these lesions (right frontal lobe of patient 9) and showed a progressive increase in choline/creatine ratio (1.41–1.82) as the lesion enlarged, suggesting tumor progression [23]. F-18 fluorodeoxyglucose (FDG)-PET scan of the brain was performed on both patients and did not show any significant increase in FDG uptake in the pontine tumors or distant lesions in either case. Patient 9 had a brain-only autopsy performed after consent was obtained. Extensive leptomeningeal involvement with tumor spreading to the right frontal lobe was confirmed, pathology was consistent with WHO Grade IV GBM.
Patient and tumor characteristics-control group
Nineteen patients met inclusion criteria for the control group and were included in the final analysis. Table 2 summarizes patient characteristics. Of 19 patients, 11 had HGG and 8 had DIPG. Median age was 11 years for patients with HGG (range: 3–17 years) and 6 years for patients with DIPG (range: 3–15 years). Median follow-up for all patients who have progressed was 11 months (range 1–31 months). Among 19 patients, 15 (78.9 %) had radiologic PD at the time of analysis. Median time to first progression was 10 months (range 1–20 months) for HGG and 8 months (range 4–14 months) for DIPG.
Patterns of progression-control group
Among 15 patients with PD (Table 4), 11 patients (73.3 %; 6 DIPG and 5 HGG) had local PD, 2 patients (13.3 %; both DIPG) had local and diffuse PD and 2 patients (13.3 %; both HGG) had local and distant PD (periventricular, n = 1; leptomeningeal, n = 1) at first progression. All instances of diffuse PD occurred in the cerebellum. No changes in patterns of progression were noted at last progression, at a median time of 11 months after diagnosis.
Comparison of study and control groups
Using the statistical tests described under the “materials and methods” section, no statistically significant difference was detected in age (p = 0.45), number of patients with DIPG (p = 0.11) and number of patients who progressed (p = 0.72) between the two groups. Patients who progressed had a comparable median time of follow-up in both groups (p = 0.51).
When patterns of failure were compared at first progression, no significant difference was detected in the incidence of diffuse or distant disease (six patients in the BVZ-treated group and four patients in the control group, p = 0.24). At last progression, there was a trend towards a higher occurrence of diffuse or distant disease (10 patients in the BVZ-treated group and four patients in the control group, p = 0.1). Among patients with diffuse PD, while there was no significant difference between the two groups at first progression (four patients in the BVZ-treated group and two patients in the control group, p = 0.66), the difference increased at last progression (eight patients in the BVZ-treated group and 2 patients in the control group, p = 0.06).
Discussion
In this study, we compare patterns of progression in children with newly-diagnosed HGG or DIPG who received BVZ-based therapy with children who did not receive BVZ. We did not detect a significant difference in the incidence of diffuse or distant disease at the time of first progression between the BVZ-treated and control groups (p = 0.24). Our analysis however suggests a trend towards a higher incidence of diffuse or distant progression at last progression (p = 0.1). Interestingly, the incidence of diffuse disease reported at last progression in the BVZ-treated group was higher than the control group, almost reaching statistical significance (p = 0.06). Within the BVZ-treated group, the limited number of HGG patients who progressed prevented any meaningful comparison to DIPG patients with PD. An important limitation of this study is the small sample size in both cohorts which limits the power of the statistical analysis; however, these are all the available patients who met inclusion criteria.
Reviews of patterns of progression in children with HGG or DIPG receiving BVZ are limited to the recurrent setting and report conflicting patterns of progression. While some authors reported a predominantly local pattern of disease progression (78.2 %) [19], others noted an increase in diffuse invasive recurrence pattern (45.5 %) [20]. One explanation for the divergence of our results from those previously reported by Gururangan et al. [19] may be the timing of BVZ administration. Pre-clinical data [24, 25] support the use of BVZ to treat HGG in the frontline setting concomitantly with RT. Indeed, BVZ can “prune” the vasculature and normalize blood supply to tumors decreasing hypoxia and acting as a radio-sensitizer. Given the crucial role that angiogenesis plays in gliomagenesis [26], it is possible that administration of BVZ as part of the initial treatment of patients may have a more pronounced effect than after progression.
Mechanisms of BVZ resistance have been implicated in this “shift” to diffuse invasive disease progression and have been well-described in pre-clinical models. In a GBM intracranial xenograft [27] model, anti-VEGF treatment was associated with slowing the progression of tumors in athymic rats but also with an increase in infiltration and a 23-fold increase in the number of distant satellite tumor areas when compared to control. It is thought that, after reaching a threshold of hypoxia caused by prolonged anti-angiogenic treatment, tumor cells switch to an invasive phenotype [28] and express a variety of proteases [29] that allow them to infiltrate through the extracellular matrix. Tumor cells can also “co-opt” existing blood vessels to spread to more distant areas in the brain following pharmacologic inhibition of VEGF [27]. Initial observations on tissue obtained from five adult HGG patients before and after treatment with RT and BVZ [30] revealed a trend towards an increase in immunostaining for D2-40 and fascin, two markers that suggest a more invasive phenotype post-BVZ treatment. Finally, the activation of alternative pro-angiogenic signaling pathways was suggested in GBM patients treated with a VEGF receptor inhibitor [31]. In these patients, levels of another pro-angiogenic mediator, basic fibroblast growth factor [32] (bFGF) were elevated in the blood of patients at progression, explaining evasive resistance to VEGF receptor inhibition.
In both our patient cohorts, patterns of progression did not correlate with overall survival (OS): patients with local only, diffuse or distant PD had comparable OS independently from the occurrence of diffuse/distant disease at first or last progression. This is consistent with adult data showing that diffuse invasive disease following anti-angiogenic therapy is not an independent prognostic factor in HGG [33].
Interestingly, two of the patients in this study had evidence of distant disease before progression of the target lesion. While these atypical distant changes on brain MRI were initially attributed to RT, it became evident, as these lesions continued to enlarge, that these findings represented PD. In fact, in one patient, PD with GBM was confirmed on autopsy. Thus, based on these data, clinicians should consider the possibility of early occurrence of distant disease in patients with HGG or DIPG receiving BVZ.
Conclusion
This retrospective review in a unique pediatric population with newly-diagnosed HGG or DIPG suggests a change in patterns of progression and a trend towards a higher incidence of distant and especially diffuse disease following BVZ treatment. It would be important to review the patterns of progression in a larger cohort of patients such as the Children’s Oncology Group HGG study (ACNS0822), which utilizes BVZ as part of maintenance in children with newly-diagnosed HGG, to confirm our findings.
References
Cage TA, Mueller S, Haas-Kogan D, Gupta N (2012) High-grade gliomas in children. Neurosurg Clin N Am 23(3):515–523. doi:10.1016/j.nec.2012.04.007
Hargrave D, Bartels U, Bouffet E (2006) Diffuse brainstem glioma in children: critical review of clinical trials. Lancet Oncol 7(3):241–248. doi:10.1016/S1470-2045(06)70615-5
Donaldson SS, Laningham F, Fisher PG (2006) Advances toward an understanding of brainstem gliomas. J Clin Oncol 24(8):1266–1272. doi:10.1200/JCO.2005.04.6599
MacDonald TJ, Arenson EB, Ater J, Sposto R, Bevan HE, Bruner J, Deutsch M, Kurczynski E, Luerssen T, Guire-Cullen P, O’Brien R, Shah N, Steinbok P, Strain J, Thomson J, Holmes E, Vezina G, Yates A, Phillips P, Packer R (2005) Phase II study of high-dose chemotherapy before radiation in children with newly diagnosed high-grade astrocytoma: final analysis of Children’s Cancer Group Study 9933. Cancer 104(12):2862–2871
Finlay JL, Boyett JM, Yates AJ, Wisoff JH, Milstein JM, Geyer JR, Bertolone SJ, McGuire P, Cherlow JM, Tefft M (1995) Randomized phase III trial in childhood high-grade astrocytoma comparing vincristine, lomustine, and prednisone with the eight-drugs- in-1-day regimen. Childrens Cancer Group. J Clin Oncol 13(1):112–123
Sposto R, Ertel IJ, Jenkin RD, Boesel CP, Venes JL, Ortega JA, Evans AE, Wara W, Hammond D (1989) The effectiveness of chemotherapy for treatment of high grade astrocytoma in children: results of a randomized trial. A report from the Childrens Cancer Study Group. J Neurooncol 7(2):165–177
Oka N, Soeda A, Inagaki A, Onodera M, Maruyama H, Hara A, Kunisada T, Mori H, Iwama T (2007) VEGF promotes tumorigenesis and angiogenesis of human glioblastoma stem cells. Biochemical and biophysical research communications 360(3):553–559. doi:10.1016/j.bbrc.2007.06.094
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, Paleologos N, Nicholas MK, Jensen R, Vredenburgh J, Huang J, Zheng M, Cloughesy T (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27(28):4733–4740. doi:10.1200/JCO.2008.19.8721
Kreisl TN, Kim L, Moore K, Duic P, Royce C, Stroud I, Garren N, Mackey M, Butman JA, Camphausen K, Park J, Albert PS, Fine HA (2009) Phase II trial of single-agent bevacizumab followed by bevacizumab plus irinotecan at tumor progression in recurrent glioblastoma. J Clin Oncol 27(5):740–745. doi:10.1200/JCO.2008.16.3055
Narayana ARL, Gutin PH (2010) Central nervous system tumors. Saunders, Philadelphia
Narayana A, Kunnakkat SD, Medabalmi P, Golfinos J, Parker E, Knopp E, Zagzag D, Eagan P, Gruber D, Gruber ML (2012) Change in pattern of relapse after antiangiogenic therapy in high-grade glioma. Int J Radiat Oncol Biol Phys 82(1):77–82. doi:10.1016/j.ijrobp.2010.10.038
Narayana A, Gruber D, Kunnakkat S, Golfinos JG, Parker E, Raza S, Zagzag D, Eagan P, Gruber ML (2012) A clinical trial of bevacizumab, temozolomide, and radiation for newly diagnosed glioblastoma. J Neurosurg 116(2):341–345. doi:10.3171/2011.9.JNS11656
Zuniga RM, Torcuator R, Jain R, Anderson J, Doyle T, Ellika S, Schultz L, Mikkelsen T (2009) Efficacy, safety and patterns of response and recurrence in patients with recurrent high-grade gliomas treated with bevacizumab plus irinotecan. J Neurooncol 91(3):329–336. doi:10.1007/s11060-008-9718-y
Wick W, Cloughesy T, Nishikawa R (2013) Tumor response based on adapted Macdonald criteria and assessment of pseudoprogression (PsPD) in the phase III AVAglio trial of bevacizumab (Bv) plus temozolomide (T) plus radiotherapy (RT) in newly diagnosed glioblastoma (GBM). J Clin Oncol 31 suppl (abstract 2002)
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, Colman H, Chakravarti A, Pugh S, Won M, Jeraj R, Brown PD, Jaeckle KA, Schiff D, Stieber VW, Brachman DG, Werner-Wasik M, Tremont-Lukats IW, Sulman EP, Aldape KD, Curran WJ Jr, Mehta MP (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N. Engl. J. Med. 370(8):699–708. doi:10.1056/NEJMoa1308573
Gururangan S, McLaughlin CA, Brashears J, Watral MA, Provenzale J, Coleman RE, Halperin EC, Quinn J, Reardon D, Vredenburgh J, Friedman A, Friedman HS (2006) Incidence and patterns of neuraxis metastases in children with diffuse pontine glioma. J Neurooncol 77(2):207–212. doi:10.1007/s11060-005-9029-5
Heideman RL, Kuttesch J Jr, Gajjar AJ, Walter AW, Jenkins JJ, Li Y, Sanford RA, Kun LE (1997) Supratentorial malignant gliomas in childhood: a single institution perspective. Cancer 80(3):497–504
Vaidya SJ, Hargrave D, Saran F, Britton J, Soomal R, Bouffet E (2007) Pattern of recurrence in paediatric malignant glioma: an institutional experience. J Neurooncol 83(3):279–284. doi:10.1007/s11060-006-9313-z
Gururangan S, Chi SN, Young Poussaint T, Onar-Thomas A, Gilbertson RJ, Vajapeyam S, Friedman HS, Packer RJ, Rood BN, Boyett JM, LE Kun (2010) Lack of efficacy of bevacizumab plus irinotecan in children with recurrent malignant glioma and diffuse brainstem glioma: a Pediatric Brain Tumor Consortium study. J Clin Oncol 28(18):3069–3075. doi:10.1200/JCO.2009.26.8789
Narayana A, Kunnakkat S, Chacko-Mathew J, Gardner S, Karajannis M, Raza S, Wisoff J, Weiner H, Harter D, Allen J (2010) Bevacizumab in recurrent high-grade pediatric gliomas. Neuro Oncol 12(9):985–990. doi:10.1093/neuonc/noq033
Parekh C, Jubran R, Erdreich-Epstein A, Panigrahy A, Bluml S, Finlay J, Dhall G (2011) Treatment of children with recurrent high grade gliomas with a bevacizumab containing regimen. J Neurooncol 103(3):673–680. doi:10.1007/s11060-010-0444-x
Brandsma D, Stalpers L, Taal W, Sminia P, van den Bent MJ (2008) Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol 9(5):453–461. doi:10.1016/S1470-2045(08)70125-6
Weybright P, Sundgren PC, Maly P, Hassan DG, Nan B, Rohrer S, Junck L (2005) Differentiation between brain tumor recurrence and radiation injury using MR spectroscopy. AJR Am J Roentgenol 185(6):1471–1476. doi:10.2214/AJR.04.0933
Zagzag D, Amirnovin R, Greco MA, Yee H, Holash J, Wiegand SJ, Zabski S, Yancopoulos GD, Grumet M (2000) Vascular apoptosis and involution in gliomas precede neovascularization: a novel concept for glioma growth and angiogenesis. Lab Invest 80(6):837–849
Jain RK (2001) Normalizing tumor vasculature with anti-angiogenic therapy: a new paradigm for combination therapy. Nat Med 7(9):987–989. doi:10.1038/nm0901-987
Jain RK, di Tomaso E, Duda DG, Loeffler JS, Sorensen AG, Batchelor TT (2007) Angiogenesis in brain tumours. Nat Rev Neurosci 8(8):610–622. doi:10.1038/nrn2175
Rubenstein JL, Kim J, Ozawa T, Zhang M, Westphal M, Deen DF, Shuman MA (2000) Anti-VEGF antibody treatment of glioblastoma prolongs survival but results in increased vascular cooption. Neoplasia 2(4):306–314
Du R, Lu KV, Petritsch C, Liu P, Ganss R, Passegue E, Song H, Vandenberg S, Johnson RS, Werb Z, Bergers G (2008) HIF1alpha induces the recruitment of bone marrow-derived vascular modulatory cells to regulate tumor angiogenesis and invasion. Cancer Cell 13(3):206–220. doi:10.1016/j.ccr.2008.01.034
Graham CH, Forsdike J, Fitzgerald CJ, Macdonald-Goodfellow S (1999) Hypoxia-mediated stimulation of carcinoma cell invasiveness via upregulation of urokinase receptor expression. Int J Cancer J Int du Cancer 80(4):617–623
Fischer I, Cunliffe CH, Bollo RJ, Raza S, Monoky D, Chiriboga L, Parker EC, Golfinos JG, Kelly PJ, Knopp EA, Gruber ML, Zagzag D, Narayana A (2008) High-grade glioma before and after treatment with radiation and Avastin: initial observations. Neuro Oncol 10(5):700–708. doi:10.1215/15228517-2008-042
Batchelor TT, Sorensen AG, di Tomaso E, Zhang WT, Duda DG, Cohen KS, Kozak KR, Cahill DP, Chen PJ, Zhu M, Ancukiewicz M, Mrugala MM, Plotkin S, Drappatz J, Louis DN, Ivy P, Scadden DT, Benner T, Loeffler JS, Wen PY, Jain RK (2007) AZD2171, a pan-VEGF receptor tyrosine kinase inhibitor, normalizes tumor vasculature and alleviates edema in glioblastoma patients. Cancer Cell 11(1):83–95. doi:10.1016/j.ccr.2006.11.021
Yoshiji H, Harris SR, Thorgeirsson UP (1997) Vascular endothelial growth factor is essential for initial but not continued in vivo growth of human breast carcinoma cells. Cancer Res 57(18):3924–3928
Narayana A, Perretta D, Kunnakkat S, Gruber D, Golfinos J, Parker E, Medabalmi P, Zagzag D, Pat Eagan RN, Gruber M (2011) Invasion is not an independent prognostic factor in high-grade glioma. J Cancer Res Ther 7(3):331–335. doi:10.4103/0973-1482.87039
Conflicts of interest
Authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salloum, R., DeWire, M., Lane, A. et al. Patterns of progression in pediatric patients with high-grade glioma or diffuse intrinsic pontine glioma treated with Bevacizumab-based therapy at diagnosis. J Neurooncol 121, 591–598 (2015). https://doi.org/10.1007/s11060-014-1671-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-014-1671-3