Abstract
Extracranial metastasis is a unique but rare manifestation of glioblastoma multiforme. It is thought to arise from glioblastoma cells disseminated into the blood stream. We undertook a comprehensive analysis of 88 cases of extracranial glioblastoma (5 were gliosarcomas) published between 1928 and 2009. Cases included in the analysis were primary or secondary glioblastomas that subsequently invaded organs outside the brain or spinal cord. The median age was 38 years and the median overall survival time was 10.5 months (range 0.0–60.0 months). The median time from symptom onset to diagnosis of primary glioblastoma was 2.5 months, from diagnosis to detection of extracranial metastasis was 8.5 months, and from metastasis to death was 1.5 months. From 1940 to 2009, there has been progressive lengthening of the interval from detection of extracranial metastasis to death, at a rate of 0.7 months per decade (95% confidence interval 0.5–1.0 month). Use of magnetic resonance imaging correlates with an increase in overall survival but not age, gender, or site of primary glioblastoma. Patients treated with surgery + radiation + chemotherapy + cerebrospinal fluid shunting had the longest average survival interval from metastasis to death when compared to those treated with surgery alone, radiation alone, surgery + radiation, and surgery + radiation + chemotherapy. Lung metastasis is a prognostic factor of extremely poor outcomes. We conclude that patients with glioblastoma extracranial metastasis have poor prognosis, but there has been a progressive lengthening of survival in each successive decade from 1940 to 2000.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extracranial metastases are reported to occur in 0.4–0.5% of all glioblastomas [1, 2]. The rarity of this phenomenon has been attributed to the extremely shortened survival of patients, and consequently there is not sufficient time for glioblastoma cells to establish metastasis in extracranial organs. Additionally, there are intrinsic biological obstacles that prevent tumor cells from infiltrating and surviving beyond the neural environment, such as (i) absence of a lymphatic system within the brain and spinal cord to allow systemic dissemination, (ii) dense dura around intracranial veins that prevents tumor cell penetration, and (iii) lack of a nurturing stroma in other organs to facilitate the survival and proliferation of glioblastoma cells. However, despite these obstacles, extracranial glioblastomas have been consistently seen and reported in the literature.
Davis [3] first reported in 1928 a patient with glioblastoma that had disseminated to lung, soft tissue of an arm, and chest wall. Since then, there have been more documented cases of glioblastoma depositing in organs outside the brain. With the advent of aggressive surgical resection, biopsy, and ventriculopleural shunting, extracranial metastases have been attributed commonly to tumor cells depositing into the blood stream or to surgical defects in the dura and skull. However, a review by Anzil [4] found that more than 10% of all cases occurred in the absence of prior surgical intervention. He also concluded that surgery, radiation, or long survival durations are not prerequisites for extraneural dissemination of glioblastomas, suggesting early hematogenous spread may be a mechanism.
The natural history of extracranial metastasis from glioblastoma is unknown. Identifying the clinical factors that promote extracranial metastasis may help to elucidate the mechanisms of tumor cell invasion within the brain. Furthermore, glioblastoma cells shed into the blood stream may, in the future, provide a means of non-invasive detection and monitoring of the biological status of intracranial glioblastomas. Therefore, we undertook this meta-analysis of published literature to define patient survival, characteristics of metastases, prognostic factors, and predictive factors from treatments.
Materials and methods
Comprehensive electronic searches for extracranial glioblastoma case studies published in English were performed using Boston University Medical Center MEDLINE Plus/OVID. Publications in other languages were included, provided that an abstract written in English was available. Cases chosen included primary and secondary glioblastomas, as well as gliosarcomas, that subsequently invaded organs outside the brain or spinal cord. Cases with metastasis to meninges, skull, and spine were included, provided that distant metastasis outside the central nervous system (CNS) was also present. All non-glioblastoma and non-gliosarcoma histologies were excluded.
From the published reports, the following data were collected: (1) survival time, divided into four epochs: (i) symptom onset to diagnosis of primary glioblastoma, (ii) diagnosis to detection of extracranial metastasis, (iii) detection of extracranial metastasis to death, and (iv) overall survival (from diagnosis of primary glioblastoma to death), (2) year of publication, categorized into decades from 1940 to 2000; reports published prior to 1940 were included within the 1940 category; (3) age of patient, divided into 3 groups: <40, 40–60, and >60 years; (4) gender; (5) modern neuroimaging modality used, categorized as computed tomography (CT), magnetic resonance imaging (MRI), or none of the above; (6) site of glioblastoma, categorized into frontal, parietal, temporal, occipital, cerebellum, brainstem and spinal cord locations; (7) site of metastasis, compiled into systemic vasculature, bone, liver, lung, lymph node, neck; and (8) treatment received, categorized as no therapy or a combination of tumor resection, radiation, chemotherapy, and/or cerebrospinal fluid (CSF) shunting.
Kaplan–Mier analysis was used to compare overall survival over time (specifically in decades) using the log-rank test. Wilcoxon rank sum test was used to compare the mean survival among the decades. Both Kaplan–Mier analysis and Wilcoxon rank sum test were also used to estimate the survival intervals from symptom onset to diagnosis of glioblastoma, from diagnosis to detection of extracranial metastasis, and from detection of extracranial metastasis to death. Because there were only a few censored observations, the inputs of survival time and survival intervals were used without identifying the censorship status. Linear regression was used to assess survival trends from predictive variables, such as treatment, and from prognostic variables, such as year of publication, age, gender, site of primary glioblastoma, and site of metastasis. Significance level was defined at P ≤ 0.05.
Results
Eighty-eight cases of extracranial metastasis from glioblastoma multiforme (n = 83) and gliosarcoma (n = 5), published between 1928 and 2009, were compiled, and patient characteristics were listed in Table 1. There were 65 men and 23 women. They had a median age of 38 years (range 6–64 years). The overall survival (from diagnosis to death) had a median of 10.5 months, ranging from 0 months, when glioblastoma multiforme diagnosis was made at autopsy, to 60.0 months. Excluding reports when duration of survival intervals was undisclosed, the median time from symptom onset to diagnosis of primary glioblastoma was 2.5 months (range 0.3–60.0 months), from diagnosis to detection of extracranial metastasis was 8.5 months (range 0.0–50.0 months), and from detection of extracranial metastasis to death was 1.5 months (range 0.0–14.0 months). The overall survival of 10.5 months (range 0.0–64.0 months) in this population is significantly shorter than those with typical intracranial glioblastomas [5, 6].
We analyzed whether or not advances in diagnosis and treatment would prolong the survival of patients with extracranial glioblastomas. Patients were grouped into decades from 1940 to 2000, and the median survival times were computed in each successive decade. The 1920 and 1930 decades were included in the 1940 decade due to only one patient reported in 1928 and another in 1935. There was a progressive lengthening of the duration from detection of extracranial metastasis to death at a rate of 0.7 months per decade from 1940 to 2000 (95% confidence interval [CI] 0.5–1.0 months, R 2 = 0.5893, P = 0.0019, Fig. 1c and Table 2). However, this lengthening was primarily due to a trend of decreasing time interval between symptom onset to diagnosis of primary glioblastoma (R 2 = 0.6125, P = 0.1687, Fig. 1a). There was neither a change in the time from diagnosis of primary glioblastoma to detection of extracranial metastasis (R 2 = 0.0212, P = 0.7531, Fig. 1b) nor time of overall survival (R 2 = 0.1911, P = 0.5707, Fig. 1d). These findings suggest that prolonged survival may be a result of lead time bias from early detection of the primary glioblastoma.
Decade of publication versus survival. Decade of glioblastoma incidence appears to be a predictive factor for detection of extracranial metastasis to death. Over the decades, trends of increasing duration were observed from symptom onset to diagnosis of primary glioblastoma and from detection of metastasis to death. No changes in duration were observed in the intervals from diagnosis of glioblastoma to detection of metastasis or from diagnosis of glioblastoma to death. a From symptom onset to diagnosis of primary glioblastoma, R 2 = 0.6125, P = 0.1687. b From diagnosis of primary glioblastoma to detection of extracranial metastasis, R 2 = 0.0212, P = 0.7531. c From detection of extracranial metastasis to death, R 2 = 0.5893, P = 0.0019. d From diagnosis of primary glioblastoma to death, R 2 = 0.1911, P = 0.5707
We next examined potential prognostic factors that may influence the survival of these patients. Because age is consistently a strong prognostic factor for glioblastoma [6, 7], we therefore analyzed the survival of our patients by categorizing them into three groups: Age less than 40 (n = 55), between 40 and 60 (n = 28), and 60 years (n = 5). There was no significant difference in overall survival (P = 0.5834) among these age groups, including the intervals from symptom onset to diagnosis of primary glioblastoma (P = 0.8352), from diagnosis to detection of extracranial metastasis (P = 0.2483), and from detection of metastasis to death (P = 0.8585). Unfortunately, the case reports provided insufficient information on neurological performance and extent of surgical resection for their analysis as prognostic factors.
There may be a slightly higher incidence of primary brain tumors in men than women, particularly among younger patients at age 40 or below [8]. However, in our cohort, gender did not affect overall survival (P = 0.9354), as well as the intervals from symptom onset to diagnosis of primary glioblastoma (P = 0.9007), from diagnosis to detection of metastasis (P = 0.5032), and from detection of metastasis to death (P = 0.1953).
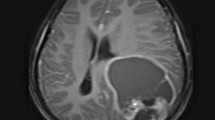
Because CT and MRI have enabled physicians earlier detection of intracranial diseases, we asked whether or not the use of CT or MRI would alter the natural history of extracranial glioblastomas. Compared to the group that did not have either CT or MRI for the detection of intracranial glioblastomas, the group that received MRI had a significant increase in overall survival (12.7 vs. 27.3 months, P = 0.0068, Fig. 2d), interval from diagnosis to detection of metastasis (8.9 vs. 19.5 months, P = 0.0268, Fig. 2b), and interval from detection of metastasis to death (1.6 vs. 7.8 months, P = 0.0045, Fig. 2c). In addition, there was also a trend toward a shortened interval from symptom onset to diagnosis (10.5 vs. 1.5 months, P = 0.2608, Fig. 2a). However, the group that received CT did not have as much benefit with respect to overall survival (12.7 vs. 17.3 months, P = 0.1725, Fig. 2d), interval from symptom onset to diagnosis (10.5 vs. 5.4 months, P = 0.7784, Fig. 2a), interval from diagnosis to detection of metastasis (8.9 vs. 13.9 months, P = 0.1803, Fig. 2b), and interval from detection of metastasis to death (1.6 vs. 3.5 months, P = 0.1274, Fig. 2c). Our data show that use of MRI correlates with prolonged patient survival and this finding may be a result of lead-time bias in the early detection of intracranial glioblastomas during the MRI era.
Modern neuroimaging modality (none, CT, or MRI) versus survival intervals. a From symptom onset to diagnosis: none versus CT, P = 0.7784; none versus MRI, P = 0.2608; and CT versus MRI, P = 0.2821. b From diagnosis to extracranial metastasis: none versus CT, P = 0.1803; none versus MRI, P = 0.0268; and CT versus MRI, P = 0.4856. c From extracranial metastasis to death: none versus CT, P = 0.1274; none versus MRI, P = 0.0045; and CT versus MRI, P = 0.0605. d From diagnosis to death: none versus CT, P = 0.1725; none versus MRI, P = 0.0068; and CT versus MRI, P = 0.1118
Neural stem cells have been shown to arise from the subventricular zone [9] and glioblastomas involving the subventricular zone are thought to have a more aggressiveness phenotype [10]. This stem-cell-like property may help glioblastomas to survive and proliferate in extracranial organs. Because the frontal lobe of the brain occupies a major part of the telencephalon, and the telencephalon undergoes the most robust cellular expansion during human brain development [11], we hypothesized that these stem-cell-like glioblastomas may arise predominantly in the frontal and parietal lobes. Of the 88 cases, tumor growth was most frequently diagnosed in the temporal lobe (n = 40) and least frequently in the cerebellum (n = 2). Primary glioblastomas found in the cerebellum were excluded from the analysis due to nondisclosure of survival durations. We found no correlation between the site of primary glioblastoma and overall survival (P = 0.5760), the interval from symptom onset to diagnosis of primary glioblastoma (P = 0.4860), from diagnosis to detection of metastasis (P = 0.7976), or from detection of metastasis to death (P = 0.6765).
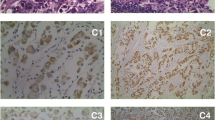
We also analyzed the prognostic significance of the extracranial organs where the glioblastoma had metastasized. Metastases were limited to tumor tissue displaying the same histological characteristics as the primary glioblastoma, and metastatic sites were recorded as locations where tumor growth was found at time of biopsy or autopsy. From the cases compiled, site of metastasis was found to be a prognostic factor for survival. There was statistical significance among the sites of extracranial metastases with respect to overall survival (P = 0.0045, Fig. 3d). Similar statistical significance was noted for the duration from diagnosis of primary glioblastoma to detection of extracranial metastasis (P = 0.0047, Fig. 3b) and from detection of metastasis to death (P = 0.0009, Fig. 3c). As expected, the site of metastasis did not correlate with the interval from symptom onset to diagnosis of primary glioblastoma (P = 0.6938, Fig. 3a).
Lung metastasis stood out as having the worst prognosis (Table 3), with a relative decrease in time interval from extracranial metastasis to death of −2.7 months (95% CI −4.4 to −1.0 months, P = 0.0024). Neck metastasis had a relative increase of 13.9 months (95% CI 5.9–21.9 months, P = 0.0009) in time interval from diagnosis of primary glioblastoma to detection of extracranial metastasis, an increase of 2.8 months (95% CI 0.3–5.3 months, P = 0.0317) from detection of extracranial metastasis to death, and an increase of 15.3 months (95% CI 6.0–24.6 months, P = 0.0014) in overall survival (Table 3). For liver metastasis, there was an increase of 10.3 months (95% CI 2.6–18.0 months, P = 0.0104) in time from diagnosis of primary glioblastoma to detection of extracranial metastasis (Table 3).
We also analyzed treatment effect on the survival of patients with extracranial glioblastoma. Of the 88 cases, 86 (98%) underwent at least one type of treatment, such as surgery, radiation, chemotherapy, and/or CSF shunting, with 61 cases (69%) receiving two or more modalities. For two cases, information regarding treatment was not provided. The type of treatment used did not significantly influence overall survival (P = 0.8760, Fig. 4d), the interval from symptom onset to diagnosis of primary glioblastoma (P = 0.8692, Fig. 4a), from diagnosis to detection of metastasis (P = 0.8227, Fig. 4b), or from detection of metastasis to death (P = 0.2326, Fig. 4c). However, there was a trend of increasing interval of survival from detection of metastasis to death with successive additions of treatment modalities. Treatment with surgery alone provided a survival interval from detection of metastasis to death of 1.1 months (95% CI 0.0–4.5 months), 3.0 months (95% CI 0.0–11.5 months) with radiation alone, 2.8 months (95% CI 2.5–8.1 months) with surgery + radiation, 4.2 months (95% CI 0.0–15.3 months) with surgery + radiation + chemotherapy, and 6.1 months (95% CI 0.0–12.4 months) with surgery + radiation + chemotherapy + CSF shunting (P = 0.2326). The findings suggest a trend that aggressive treatment may have a favorable impact on survival.
Treatment combinations versus survival interval. Treatments include (1) surgery alone, (2) radiation alone, (3) surgery + radiation, (4) surgery + radiation + chemotherapy, and (5) surgery + radiation, chemotherapy + CSF shunting. a From symptom onset to diagnosis, P = 0.8692. b From diagnosis to extracranial metastasis, P = 0.8227. c From extracranial metastasis to death, P = 0.2326. d From diagnosis to death, P = 0.8760
Discussion
The rarity of extracranial metastasis of glioblastomas precludes prospective examination of its natural history, and meta-analysis of existing literature is the only means of a comprehensive analysis of this disorder. Although meta-analysis is often subjected to publication bias, this literature is unique because it is comprised primarily of clinicopathological descriptions of single cases or small case series. These case descriptions do not suffer from heterogeneity in data reported in treatment trials, in which inclusion and exclusion criteria may differ or drug pharmacodynamic and pharmacokinetic properties may influence patient selection. Therefore, we performed this meta-analysis to elucidate the survival and prognostic factors in patients with extracranial glioblastomas.
The overall survival of glioblastoma multiforme patients, in general, has improved marginally over the decades despite major advancements made in surgery, radiation, and chemotherapies. For example, temozolomide added to radiotherapy allowed nearly 10% of patients survive to 5 years after initial diagnosis, as compared to 1.9% of those treated with radiation alone [5]. Still, more than 70% of them die within 2 years of diagnosis [5]. It is increasing clear that patient survival is heavily influenced by the intrinsic molecular genetics of the glioblastoma. Patients with O6-methylguanine-DNA methyltransferase (MGMT) promoter methylation have a 2-year survival of 48.9% and 5-year survival of 13.8%, as compared to 14.8 and 8.3% respectively among those with unmethylated MGMT [12]. These data suggest that there is a small but incremental survival improvement, but the underlying molecular genetics of glioblastoma are the predominant determinants of outcome from treatment [12]. Similarly, our data showed that patients with extracranial glioblastoma metastases had a small but incremental survival improvement over time, at a rate of 0.7 months per decade since 1940. This improvement is probably a result of lead-time bias, as CT and MRI facilitate the early diagnosis of intracranial tumors. However, we cannot exclude a direct benefit from combined modality treatment that included surgery, radiation, chemotherapy, and CSF shunting. At present, the molecular determinants that predispose these patients to have extracranial metastasis are unknown.
Our cohort is younger (median age 38 years) than the typical adult glioblastoma patients. Because younger patients tend to have secondary glioblastomas [13], there is a possibility that metastases to extracranial organ may arise from untreated lower grade gliomas before their malignant transformation into glioblastomas. Nevertheless, age was not a prognostic factor in our patients with extracranial metastases. This is probably due to the extremely shortened overall survival of 10.5 months in this population.
There is heterogeneity in patient survival depending on the site of metastasis, and a number of observations were made. First, patients with metastases to neck and liver have a better prognosis than those with lung metastasis. When compared to the average, patients with metastases to the liver and neck experienced an increase in the time from diagnosis of primary glioblastoma to detection of metastasis by 10.3 and 13.9 months, respectively. This increase may be due to difficulty and delay in detecting tumor growth in the liver and neck. In contrast, metastasis to the lung resulted in a decrease of 2.7 months in the time interval from detection of extracranial metastasis to death. Lastly, neck metastasis had an increment of 15.3 months in overall survival, or interval from diagnosis of primary glioblastoma to death, as compared to the average. Taken together, our data suggest that it may be difficult to detect neck and liver metastases in a timely fashion. But once metastases are detected, patients with lung metastasis have the worst prognosis. Alternatively, it is possible that cellular and molecular heterogeneity may play a role here, and glioblastoma clones that migrated to the liver and neck may be less aggressive than the average, while clones that metastasized to the lung are more aggressive. This phenomenon of clonal heterogeneity within a primary tumor has been clearly demonstrated by Fidler and Kripke [14] using B16 melanoma cells, in which certain clones have a predilection for specific organs like lung or liver. Therefore, it would be worthwhile to analyze the molecular genetics of glioblastoma cells that give rise to specific metastases in various extracranial organs.
Extracranial metastasis may indicate the existence of circulating glioblastoma cells in the blood stream. Unlike systemic organs, the CNS does not have a lymphatic system to facilitate spread of primary glioma cells. Distant metastasis of glioblastomas can only occur spontaneously by hematogeneous dissemination. However, the rarity of these metastases may be due to a number of factors. First, glioblastoma cells may preferentially adhere to the neural stroma. But as the glioblastoma progresses, tumor cells may coopt existing cerebral vasculature [15], making them more likely to spread within the CNS and into the blood circulation. Second, circulating glioblastoma cells are probably present in low numbers as compared to the number of circulating monocytes. But the prolonged survival of young patients with glioblastoma may increase the probability of glioblastoma cells shedding into the blood stream, and therefore potentiate the development of distant metastases. Third, a metastatic niche must be established in distant organs in order for glioblastoma metastasis to occur. There is a high likelihood that significant stromal differences exist between the CNS and distant organs, such that extracranial glioblastoma metastases are difficult to develop. Lastly, there are reports of extracranial glioblastomas developed in recipients of kidney or liver transplanted from donors with glioblastomas [16–19]. The immunosuppressants used to prevent rejection of donor organs may further potentiate the development of these tumors in the recipient. More importantly, the development of extracranial glioblastomas indicates that systemic dissemination of the primary intracranial glioblastoma probably occurs early in the disease. Therefore, the fraction of glioblastoma cells in the circulation may provide an opportunity for early detection and genetic analysis of the intracranial glioblastoma.
Conclusions
Patients with glioblastoma extracranial metastasis have poor prognosis and those with lung metastasis have the worst survival. But there has been a progressive lengthening of survival in each successive decade from 1940 to 2000, at a rate of 0.7 months per decade.
References
Smith DR, Hardman JM, Earle KM (1969) Metastasizing neuroectodermal tumors of the central nervous system. J Neurosurg 31:50–58
Pasquier B, Pasquier D, N’Golet A, Panh MH, Couderc P (1980) Extraneural metastases of astrocytomas and glioblastomas: clinicopathological study of two cases and review of literature. Cancer 45:112–125
Davis L (1928) Spongioblastoma multiforme of the brain. Ann Surg 87:8–14
Anzil AP (1970) Glioblastoma multiforme with extracranial metastases in the absence of previous craniotomy, case report. J Neurosurg 33:88–94
Stupp R, Hegi ME, Mason WP et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10:459–466
Curran WJ, Scott CB, Horton J, Nelson JS, Weinstein AS, Fischbach J, Chang CH, Rotman M, Asbell SO, Krisch RE, Nelson DF (1993) Recursive partitioning analysis of prognostic factors in three Radiation Therapy Oncology Group malignant glioma trials. J Natl Cancer Inst 85:704–710
Laws ER, Parney IF, Huang W, Anderson F, Morris AM, Asher A, Lillehei KO, Bernstein M, Brem H, Sloan A, Berger MS, Chang S, the Glioma Outcomes Investigators (2003) Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the Glioma Outcomes Project. J Neurosurg 99:467–473
Velema JP, Walker AM (1987) The age curve of nervous system tumour incidence in adults: common shape but changing levels by sex, race, and geographical location. Int J Epidemiol 16:177–183
Doetsch F, Caillé I, Lim DA, García-Verdugo JM, Alvarez-Buylla A (1999) Subventricular zone astrocytes are neural stem cells in the adult mammalian brain. Cell 97:703–716
Lim DA, Cha S, Mayo MC, Chen MH, Keles E, VandenBerg S, Berger MS (2007) Relationship of glioblastoma multiforme to neural stem cell regions predicts invasive and multifocal tumor phenotype. Neuro-Oncology 9:424–429
Crelin ES (1974) Development of the nervous system, a logical approach to neuroanatomy. Clin Symp 26:1–32
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JEC, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359:492–507
Fidler IJ, Kripke ML (1977) Metastasis results from preexisting variant cells within a malignant tumor. Science 197:893–895
Rubenstein JL, Kim J, Ozawa T, Zhang M, Westphal M, Deen DF, Shuman MA (2000) Anti-VEGF antibody treatment of glioblastoma prolongs survival but results in increased vascular cooption. Neoplasia 2:306–314
Morse JH, Turcotte JG, Merion RM, Campbell DA, Burtch GD, Lucey MR (1990) Development of a malignant tumor in a liver transplant graft procured from a donor with a cerebral neoplasm. Transplantation 50:875–877
Val-Bernal F, Ruiz JC, Cotorruelo JG, Arias M (1993) Glioblastoma multiforme of donor origin after renal transplantation: report of a case. Human Pathol 24:1256–1259
Colquhoun SD, Robert ME, Shaked A, Rosenthal JT, Millis JM, Farmer DG, Jurim O, Busuttil RW (1994) Transmission of CNS malignancy by organ transplantation. Transplantation 57:970–978
Jonas S, Bechstein WO, Lemmens HP, Neuhaus R, Thalmann U, Neuhaus P (1996) Liver graft-transmitted glioblastoma multiforme. A case report and experience with 13 multiorgan donors suffering from primary cerebral neoplasia. Transpl Int 9:426–429
Brandt M (1950) Problem of brain tumor metastases. Arch Psychiatr Nervenkr Z Gesamte Neurol Psychiatr 185:594–602
Brodskaia IA (1960) A case of extracranial metastasis of glioblastoma. Arkh Patol 22(4):78–80
Cerame MA, Guthikonda M, Kohli CM (1985) Extraneural metastases in gliosarcoma: a case report and review of the literature. Neurosurgery 17:413–418
Dolman CL (1974) Lymph node metastasis as first manifestation of glioblastoma. Case report. J Neurosurg 41:607–609
Eade OE, Urich H (1971) Metastasising gliomas in young subjects. J Pathol 103:245–256
Ehrenreich T, Devlin JF (1958) A complex of glioblastoma and spindle-cell sarcoma with pulmonary metastasis. AMA Arch Pathol 66:536–549
El-Gindi S, Salama M, el-Henawy M, Farag S (1973) Metastases of glioblastoma multiforme to cervical lymph nodes. Report of two cases. J Neurosurg 38:631–634
Frappaz D, Mornex F, Saint-Pierre G, Ranchere-Vince D, Jouvet A, Chassagne-Clement C, Thiesse P, Mere P, Deruty R (1999) Bone metastasis of glioblastoma multiforme confirmed by fine needle biopsy. Acta Neurochir (Wien) 141:551–552
Friedman JH, Liu HM, Spremulli E, Calabresi P (1987) Distant metastases from a malignant glioma: unusual complications associated with treatment of a glioblastoma: distant metastases and focal white matter degeneration. J Neurol Neurosurg Psychiatry 50:237–238
Gamis AS, Egelhoff J, Roloson G, Young J, Woods GM, Newman R, Freeman AI (1990) Diffuse bony metastases at presentation in a child with glioblastoma multiforme. A case report. Cancer 66:180–184
Garret R (1958) Glioblastoma and fibrosarcoma of the brain with extracranial metastases. Cancer 11:888–894
Grampa G, Baroldi G (1958) Glioma with extracranial metastases. Oncologia 11:1–15
Gyepes MT, D’Angio GJ (1966) Extracranial metastases from central nervous system tumors in children and adolescents. Radiology 87:55–63
Haddon M, Slavin JD, Spencer RP (1989) Multiple bone metastases in a patient with glioblastoma multiforme. Clin Nucl Med 14(1):13–14
Houston SC, Crocker IR, Brat DJ, Olson JJ (2000) Extraneural metastatic glioblastoma after interstitial brachytherapy. Int J Radiat Oncol Biol Phys 48:831–836
Hulbanni S, Goodman PA (1976) Glioblastoma multiforme with extraneural metastases in the absence of previous surgery. Cancer 37:1577–1583
Jahraus CD, Dishop MK, Bayliff SL, Lee C, St Clair WH (2003) Atypical presentation and progression of glioblastoma multiforme in a 6-year-old girl: multidisciplinary case report. J Pediatr Hematol Oncol 25:243–247
Johnson RP, Guillan RA (1974) Glioblastoma multiforme with remote extracranial metastases. J Kans Med Soc 75:169–172
Kleinschmidt-Demasters BK (1996) Diffuse bone marrow metastases from glioblastoma multiforme: the role of dural invasion. Hum Pathol 27:197–201
Kohlmeier W (1941) Zur Frage der Metastasierung der Gliome Virchows Archiv 308:51–59
Komatsu K, Hiratsuka H, Takahashi S, Kamisasa A, Inaba Y (1972) Widespread extracranial metastases of glioblastoma multiforme. Report of case and clinicopathological review of cases in literature. Bull Tokyo Med Dent Univ 19:29–49
Kraft M, Lang F, Braunschweig R, Janzer RC (2008) Parotid gland metastasis from glioblastoma multiforme: a case report and review of the literature. Eur Arch Otorhinolaryngol 265:709–711
Labitzke HG (1962) Glioblastoma multiforme with remote extracranial metastases. Arch Pathol 73:223–229
Lampl Y, Eshel Y, Gilad R, Sarova-Pinchas I (1990) Glioblastoma multiforme with bone metastase and cauda equina syndrome. J Neurooncol 8:167–172
Ley A, Campillo D, Oliveras C (1961) Extracranial metastasis of glioblastoma multiforme. J Neurosurg 18:313–330
Liwnicz BH, Rubinstein LJ (1979) The pathways of extraneural spread in metastasizing gliomas: a report of three cases and critical review of the literature. Human Pathol 10:453–467
Miliaras G, Tsitsopoulos PP, Markoula S, Kyritsis A, Polyzoidis KS, Malamou-Mitsi V (2009) Multifocal glioblastoma with remote cutaneous metastasis: a case report and review of the literature. Cen Eur Neurosurg 70:39–42
Mittelbach A (1935) Uber Gliome mit Metastasen. Beifr Pathol Anat 96:538–572
Mujic A, Hunn A, Taylor AB, Lowenthal RM (2006) Extracranial metastases of a glioblastoma multiforme to the pleura, small bowel and pancreas. J Clin Neurosci 13:677–681
Myers T, Egelhoff J, Myers M (1990) Glioblastoma multiforme presenting as osteoblastic metastatic disease: case report and review of the literature. AJNR Am J Neuroradiol 11:802–803
Newton HB, Rosenblum MK, Walker RW (1992) Extraneural metastases of infratentorial glioblastoma multiforme to the peritoneal cavity. Cancer 69:2149–2153
Nigogosyan G, De La Pava S, Pickren JW (1962) Brain tumor with extracranial metastases. Report of two cases. Arch Neurol 6:300–306
Nowotny K, Kraus H, Zeitlhofer J (1951) Zur Frage der extrakraniellen Metastasierung von Gliomen. Wien Z Nervenkeilk 4:120–133
Pang D, Ashmead JW (1982) Extraneural metastasis of cerebellar glioblastoma multiforme. Neurosurgery 10:252–257
Rajagopalan V, El Kamar FG, Thayaparan R, Grossbard ML (2005) Bone marrow metastases from glioblastoma multiforme. A case report and review of the literature. J Neurooncol 72:157–161
Saad AG, Sachs J, Turner CD, Proctor M, Marcus KJ, Wang L, Lidov H, Ullrich NJ (2007) Extracranial metastases of glioblastoma in a child: case report and review of the literature. J Pediatr Hematol Oncol 29:190–194
Sadik AR, Port R, Garfinkel B, Bravo J (1984) Extracranial metastasis of cerebral glioblastoma multiforme: case report. Neurosurgery 15:549–551
Sikl H (1950) Glioma of the Brain with Metastasis into the Lung. Acta Un Int Cancer 6:986–988
Taha M, Ahmad A, Wharton S, Jellinek D (2005) Extra-cranial metastasis of glioblastoma multiforme presenting as acute parotitis. Br J Neurosurg 19:348–351
Terheggen HG, Muller W (1977) Extracerebrospinal metastases in glioblastoma. Case report and review of the literature. Eur J Pediatr 124:155–164
Thiry S, Betz EH, Dewart L (1959) A case of cerebral glioma with hepatic metastases. Neurochirurgie 5:321–326
Trattnig S, Schindler E, Ungersbock K, Schmidbauer M, Heimberger K, Hubsch P, Stiglbauer R (1990) Extra-CNS metastases of glioblastoma: CT and MR studies. J Comput Assist Tomogr 14:294–296
Utsuki S, Tanaka S, Oka H, Iwamoto K, Sagiuchi T, Fujii K (2005) Glioblastoma multiforme metastasis to the axis. Case report. J Neurosurg 102:540–542
Vural G, Hagmar B, Walaas L (1996) Extracranial metastasis of glioblastoma multiforme diagnosed by fine-needle aspiration: a report of two cases and a review of the literature. Diagn Cytopathol 15:60–65
Waite KJ, Wharton SB, Old SE, Burnet NG (1999) Systemic metastases of glioblastoma multiforme. Clin Oncol (R Coll Radiol) 11:205–207
Wakamatsu T, Matsuo T, Kawano S, Teramoto S, Matsumura H (1971) Glioblastoma with extracranial metastasis through ventriculopleural shunt. Case report. J Neurosurg 34:697–701
Wisiol ES, Handler S, French LA (1962) Extracranial metastases of a glioblastoma multiforme. J Neurosurg 19:186–194
Wolf A, Cowen D, Stewart WB (1954) Glioblastoma with extraneural metastasis by way of a ventriculopleural anastomosis. Trans Am Neurol Assoc 13:140–142
Yasuhara T, Tamiya T, Meguro T, Ichikawa T, Sato Y, Date I, Nakashima H, Ohmoto T (2003) Glioblastoma with metastasis to the spleen—case report. Neurol Med Chir (Tokyo) 43:452–456
Yokoyama H, Ono H, Mori K, Kishikawa M, Kihara M (1985) Extracranial metastasis of glioblastoma with sarcomatous component. Surg Neurol 24:641–645
Yung WK, Tepper SJ, Young DF (1983) Diffuse bone marrow metastasis by glioblastoma: premortem diagnosis by peroxidase-antiperoxidase staining for glial fibrillary acidic protein. Ann Neurol 14:581–585
Zeitlhofer J, Kranus H (1952) Extracranial metastases of glioma. Zentralbl Neurochir 12:347–356
Acknowledgments
This research was supported in part by the “A Reason To Ride” research fund. We thank Marion Stein, M.D. and Pascal Zinn, M.D. for help in translating some of the published papers in foreign languages.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lun, M., Lok, E., Gautam, S. et al. The natural history of extracranial metastasis from glioblastoma multiforme. J Neurooncol 105, 261–273 (2011). https://doi.org/10.1007/s11060-011-0575-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-011-0575-8