Abstract
The C677T and A1298C polymorphisms of methylenetetrahydrofolate reductase (MTHFR) have been reported to alter the risk of ovarian cancer. However, the results are still inconclusive. For better understanding of the effect of these two polymorphisms on ovarian cancer risk, a meta-analysis was performed. An extensive search was performed to identify all case–control studies investigating such association. The strength of association between these two polymorphisms and ovarian cancer risk was assessed by odds ratio (OR) with the corresponding 95 % confidence interval (95 % CI). 3,496 cases and 3,631 controls for C677T polymorphism and 3,280 cases and 3,346 controls for A1298C polymorphism were included in this meta-analysis. The results suggested that there were no significant associations between C677T and A1298C polymorphisms and ovarian cancer risk in overall comparisons in all genetic models (For C677T: TT vs. CC: OR = 0.94, 95 % CI = 0.71–1.24, P = 0.65; CT vs. CC: OR = 1.03, 95 % CI = 0.93–1.14, P = 0.57; TT/CT vs. CC: OR = 1.01, 95 % CI = 0.88–1.16, P = 0.87; TT vs. CC/CT: OR = 0.93, 95 % CI = 0.72–1.20, P = 0.58. For A1298C: CC vs. AA: OR = 1.05, 95 % CI = 0.88–1.25, P = 0.65; CA vs. AA: OR = 0.98, 95 % CI = 0.88–1.08, P = 0.66; CC/CA vs. AA: OR = 0.99, 95 % CI = 0.90–1.09, P = 0.85; CC vs. AA/CA: OR = 1.06, 95 % CI = 0.90–1.26, P = 0.46). Subgroup analysis based on ethnicities and influence analysis did not perturb the results. In conclusion, the results of this meta-analysis indicate that the MTHFR C677T and A1298C polymorphisms are not associated with ovarian cancer risk, especially in Caucasians.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One-carbon metabolism, also referred as folate-mediated one-carbon metabolism, which plays a critical role in DNA synthesis and methylation, has an impact on both genetic and epigenetic pro-carcinogenic processes [1]. Folate plays an important role as a donor of one-carbon unit for nucleotide synthesis and DNA methylation [2]. Low folate levels were reported to be associated with uracil disincorporation, chromosomal DNA damage, DNA strand breaks, impaired DNA repair and DNA hypomethylation [3]. Thus may increase the risk of several cancers [4–7].
Methylenetetrahydrofolate reductase (MTHFR), which located on short arm of chromosome 1 (1p36.3), plays a key role in the folate metabolism [8]. MTHFR mediates the irreversible conversion of 5,10-methylenetetrahydrofolate (5,10-MTHF) to 5-methyltetrahydrofolate (5-MTHF) [2]. Several single nucleotide polymorphisms (SNPs) in the MTHFR gene have been identified. Among which the most commonly studied are C677T in exon 4 and A1298C in exon7 [9–11]. These two polymorphisms were shown to be associated with reduced enzyme activity, leading to an increase amount of 5,10-MTHF for thymidylate and purine synthesis and a decrease amount of 5-MTHF for DNA methylation [10–12]. Several studies have reported that MTHFR polymorphisms were associated with susceptibility to several cancer types including colorectal, prostate, bladder, endometrial, and breast [13–18].
Ovarian cancer is the one of the leading causes of malignant deaths in women in the world [19]. Considering the important role of MTHFR gene in the folate metabolism, it is reasonable that MTHFR genotype may also have an impact on ovarian cancer risk. In recent years, several studies have been conducted to evaluate the association between MTHFR C677T and A1298C polymorphisms and ovarian cancer risk, with inconclusive results [20–23]. Therefore, to derive a more precise estimation of the association between MTHFR C677T and A1298C polymorphisms and ovarian cancer risk, a meta-analysis was performed.
Materials and methods
Publication search
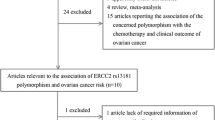
We performed an extensive search of studies that examined the association of the MTHFR polymorphisms with ovarian cancer. All eligible studies were identified by searching the PubMed and Embase database. The following terms were used: “MTHFR” or ‘‘methylenetetrahydrofolate reductase’’, ‘‘polymorphism(s)’’, “ovarian cancer” or ‘‘ovarian carcinoma’’. There was no language restriction in the search. All studies that evaluated the associations between polymorphisms of MTHFR gene and ovarian cancer risk were retrieved. The retrieved literatures were then read in their entirety to assess their appropriateness for the inclusion in this meta-analysis by the two authors (Liu and Liao) independently. References of cited articles were reviewed to identify additional studies.
Inclusion criteria
For inclusion in the meta-analysis, the criteria was defined as follows: (a) articles evaluating the association between MTHFR C677T and/or A1298C polymorphisms and ovarian cancer risk; (b) study designed as case–control; (c) sufficient data available to estimate an odds ratio (OR) with its 95 % confidence interval (95 % CI).
Data extraction
All the data were extracted independently by two authors (Liu and Liao) according to the prespecified inclusion criteria, and the two authors reached a consensus on all the items. The following variables were extracted from each study if available: first author’s surname, publication year, country in which the study was performed, ethnicity of the study population, numbers of cases and controls, and genotype distributions in both cases and controls. Different ethnicities were categorized as Caucasian, Asian, and mixed.
Statistical analysis
We calculated summary odd ratios (ORs) corresponding to a 95 % confidence interval (CI) to assess the strength of association between MTHFR C677T and/or A1298C polymorphisms and ovarian cancer risk. And the pooled OR was calculated by a fixed-effects model (the Mantel–Haenszel method) when between-study heterogeneity was absent [24]. Otherwise, a random-effects model (the DerSimonian and Laird method) was selected [25]. Statistical between-study heterogeneity was checked by the Q test and it was considered statistically significant with P < 0.10 [26].
We examined the association between MTHFR C677T polymorphism and ovarian cancer risk, and made comparisons with homozygotes (TT vs. CC), heterozygotes (CT vs. CC), the dominant genetic model (CT/TT vs. CC), and the recessive genetic model (TT vs. CC/CT). The same contrasts were performed for A1298C polymorphism. In addition, subgroup analyses for ethnicity were conducted. Sensitivity analysis was performed by omitting each study to find potential outliers.
The potential publication bias was examined visually in a funnel plot of log [OR] against its standard error (SE), and the degree of asymmetry was tested by Egger’s test (P < 0.05 was considered a significant publication bias) [27]. In the control populations, Hardy–Weinberg equilibrium (HWE) was tested. This meta-analysis was performed using the software STATA version 11.2.
Results
Study characteristics
A total of five publications met the inclusion criteria. Of these studies, one [28] was excluded as cases involved were restricted to BRCA1 mutation carriers. As a result, four publications were used for this meta-analysis [20–23]. Tables 1 and 2 list the main characteristics of these studies. Concerning C677T polymorphism, six case–control studies from four publications were eligible (3,496 cases and 3,631 controls). There were four studies of Caucasians, one study of Asians, and one study of mixed populations of which 95 % were Caucasians. Concerning A1298C polymorphism, four case–control studies from two publications were eligible (3,280 cases and 3,346 controls). There were three studies of Caucasians and one study of mixed populations of which 95 % were Caucasians. Genotype distributions in the controls of all studies were in agreement with HWE.
Meta-analysis result
C677T polymorphism
Table 3 lists the main results of the meta-analysis about C677T polymorphism. When all the eligible studies were pooled into the meta-analysis, C677T polymorphism did not reveal any relationship with ovarian cancer risk in all genetic models (TT vs. CC: OR = 0.94, 95 % CI = 0.71–1.24, P = 0.65; CT vs. CC: OR = 1.03, 95 % CI = 0.93–1.14, P = 0.57; TT/CT vs. CC: OR = 1.01, 95 % CI = 0.88–1.16, P = 0.87; TT vs. CC/CT: OR = 0.93, 95 % CI = 0.72–1.20, P = 0.58). In the subgroup analysis on ethnicity, similarly, no significant association was found (Table 3; Fig. 1).
A1298C polymorphism
As shown in Table 4, no significant associations between A1298C polymorphism and ovarian cancer susceptibility were observed in all genetic models (CC vs. AA: OR = 1.05, 95 % CI = 0.88–1.25, P = 0.65; CA vs. AA: OR = 0.98, 95 % CI = 0.88–1.08, P = 0.66; CC/CA vs. AA: OR = 0.99, 95 % CI = 0.90–1.09, P = 0.85; CC vs. AA/CA: OR = 1.06, 95 % CI = 0.90–1.26, P = 0.46). In the subgroup analysis on ethnicity, the results were all negative (Table 4; Fig. 2).
Sensitivity analysis
In the sensitivity analysis, the influence of each study on the pooled OR was examined by repeating the meta-analysis while omitting each study one at a time. The results suggested that no individual study significantly affected the pooled ORs (data not shown).
Publication bias
Funnel plot and Egger’s test were performed to assess the publication bias. The shape of the funnel plot did not reveal any evidence of obvious asymmetry (figures not shown). Then, the Egger’s test was used to provide statistical evidence of funnel plot symmetry. Similarly, the results did not suggest any evidence of publication bias (data not shown).
Discussion
MTHFR is a key enzyme in the folate metabolism pathway. The most commonly found polymorphisms of the MTHFR gene are C677T and A1298C. The C677T polymorphism which positioned in exon 4 leads to an alanine to valine conversion at codon 222. The other polymorphism A1298C located in exon 7 causes an amino acid substitution from glutamic to alanine at codon 429. These polymorphisms, which result in lowered blood levels of folate, has been linked to a variety of cancers including ovarian cancer [28–31].
Regarding the association between C677T and A1298C polymorphisms and ovarian cancer susceptibility, a total of four case–control studies were found by searching PubMed and Embase database, with inconclusive results. Since single study may have been underpowered in clarifying these polymorphisms with ovarian cancer risk, we performed a meta-analysis for better understanding of the association between two polymorphisms (C677T and A1298C) in MTHFR and ovarian cancer risk. To our knowledge, this is the first meta-analysis on the association between MTHFR and ovarian cancer risk. Six studies from four publications on the C677T genotype and four studies from two publications on the A1298C genotype were critically reviewed. The results strongly suggested that the MTHFR C677T and A1298C polymorphisms were not associated with ovarian cancer risk in all genetic models. Considering the possible role of ethnic differences in genetic backgrounds, we conducted subgroup analysis based on ethnicities. Similarly, no significant association was found in both Caucasians and Asians. Considering the limited sample size of Asians included in the meta-analysis, our results should be interpreted with caution. Further investigation may be needed confirm the result. In addition, no study on Africans was included in this meta-analysis. Studies focused on Africans may be needed to explore the possible relationship between C677T and A1298C polymorphisms and ovarian cancer risk in Africans. Moreover, influence analysis did not perturb the results, indicating that our results were statistically robust.
Similar to other meta-analysis, some limitations of this meta-analysis should be addressed. First, because ovarian cancer is a multi-stage, multi-factorial, and long-term disease which is influenced by numerous genes, MTHFR polymorphisms may have little influence on ovarian risk on the individual. Second, of these studies, most subjects were Caucasians, the number of Asians were relatively small, not having enough statistical power to explore the real association. Therefore, the conclusion about this association in Asian populations should be further investigated. In addition, no study on Africans was included in this meta-analysis. Third, this study is based on unadjusted estimates, while a more precise analysis should be conducted if individual data were available, which would allow for the adjustment by other co-variants including age, ethnicity, environmental factors and other lifestyle. Furthermore, between-study heterogeneity, which may impact on the results of this analysis, was observed in some subanalyses.
In conclusion, this meta-analysis suggests that the MTHFR C677T and A1298C polymorphisms were not associated with ovarian cancer risk in both overall comparisons and subgroup analysis. The findings seem mainly to apply to Caucasian populations. Due to the different genotype frequencies in different ethnicities and most studies included were conducted in Caucasians, additional, well-designed case–control studies focused on Africans and Asians are needed to further substantiate and enrich the present findings.
References
Stern LL, Mason JB, Selhub J et al (2000) Genomic DNA hypomethylation, a characteristic of most cancers, is present in peripheral leukocytes of individuals who are homozygous for the C677T polymorphism in the methylenetetrahydrofolate reductase gene. Cancer Epidemiol Biomarkers Prev 9:849–853
Choi SW, Mason JB (2000) Folate and carcinogenesis: an integrated scheme. J Nutr 130:129–132
Duthie SJ (1999) Folic acid deficiency and cancer: mechanisms of DNA instability. Br Med Bull 55:578–592
Kim YI (1999) Folate and carcinogenesis: evidence, mechanisms, and implications. J Nutr Biochem 10:66–88
Mason JB, Choi SW (2000) Folate and carcinogenesis: developing a unifying hypothesis. Adv Enzyme Regul 40:127–141
La Vecchia C, Negri E, Pelucchi C et al (2002) Dietary folate and colorectal cancer. Int J Cancer 102:545–547
McCann SE, Freudenheim JL, Marshall JR et al (2000) Diet in the epidemiology of endometrial cancer in western New York (United States). Cancer Causes Control 11:965–974
Goyette P, Pai A, Milos R et al (1998) Gene structure of human and mouse methylenetetrahydrofolate reductase (MTHFR). Mamm Genome 9:652–656
Angeline T, Jeyaraj N, Granito S et al (2004) Prevalence of MTHFR gene polymorphisms (C677T and A1298C) among Tamilians. Exp Mol Pathol 77:85–88
Weisberg IS, Jacques PF, Selhub J et al (2001) The 129XA-C polymorphism in methylenetetrahydrofolate reductase (MTHFR): in vitro expression and association with homocysteine. Atherosclerosis 156:409–415
Weisberg I, Tran P, Christensen B et al (1998) A second genetic polymorphism in methylenetetrahydrofolate reductase (MTHFR) associated with decreased enzyme activity. Mol Genet Metab 64:169–172
Frosst P, Blom HJ, Milos R et al (1995) A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 10:111–113
Levine AJ, Figueiredo JC, Lee W et al (2010) Genetic variability in the MTHFR gene and colorectal cancer risk using the colorectal cancer family registry. Cancer Epidemiol Biomarkers Prev 19:89–100
Kim J, Cho YA, Kim DH et al (2012) Dietary intake of folate and alcohol, MTHFR C677T polymorphism, and colorectal cancer risk in Korea. Am J Clin Nutr 95:405–412
Bai JL, Zheng MH, Xia X et al (2009) MTHFR C677T polymorphism contributes to prostate cancer risk among Caucasians: a meta-analysis of 3511 cases and 2762 controls. Eur J Cancer 45:1443–1449
Kouidhi S, Rouissi K, Khedhiri S et al (2011) MTHFR gene polymorphisms and bladder cancer susceptibility: a meta-analysis including race, smoking status and tumour stage. Asian Pac J Cancer Prev 12:2227–2232
Xu WH, Shrubsole MJ, Xiang YB et al (2007) Dietary folate intake, MTHFR genetic polymorphisms, and the risk of endometrial cancer among Chinese women. Cancer Epidemiol Biomarkers Prev 16:281–287
Hosseini M, Houshmand M, Ebrahimi A (2011) MTHFR polymorphisms and breast cancer risk. Arch Med Sci 7:134–137
Jemal A, Siegel R, Ward E et al (2008) Cancer statistics. CA Cancer J Clin 2008(58):71–96
Terry KL, Tworoger SS, Goode EL et al (2010) MTHFR polymorphisms in relation to ovarian cancer risk. Gynecol Oncol 119:319–324
Prasad VV, Wilkhoo H (2011) Association of the functional polymorphism C677T in the methylenetetrahydrofolate reductase gene with colorectal, thyroid, breast, ovarian, and cervical cancers. Onkologie 34:422–426
Webb PM, Ibiebele TI, Hughes MC et al (2011) Folate and related micronutrients, folate-metabolising genes and risk of ovarian cancer. Eur J Clin Nutr 65:1133–1140
Pawlik P, Mostowska A, Lianeri M et al (2012) Folate and choline metabolism gene variants in relation to ovarian cancer risk in the Polish population. Mol Biol Rep 39:5553–5560
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22:719–748
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Zintzaras E, Ioannidis JP (2005) Heterogeneity testing in meta-analysis of genome searches. Genet Epidemiol 28:123–137
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Jakubowska A, Gronwald J, Menkiszak J et al (2007) Methylenetetrahydrofolate reductase polymorphisms modify BRCA1-associated breast and ovarian cancer risks. Breast Cancer Res Treat 104:299–308
Galbiatti AL, Ruiz MT, Maniglia JV et al (2012) Head and neck cancer: genetic polymorphisms and folate metabolism. Braz J Otorhinolaryngol 78:132–139
Zhao P, Lin F, Li Z et al (2011) Folate intake, methylenetetrahydrofolate reductase polymorphisms, and risk of esophageal cancer. Asian Pac J Cancer Prev 12:2019–2023
Zhang Y, Chen GQ, Ji Y et al (2012) Quantitative assessment of the effect of MTHFR polymorphisms on the risk of lung carcinoma. Mol Biol Rep 39:6203–6211
Author information
Authors and Affiliations
Corresponding author
Additional information
Lu Liu and Shao-Guang Liao equally contributed to this study.
Rights and permissions
About this article
Cite this article
Liu, L., Liao, SG. & Wang, YJ. MTHFR polymorphisms and ovarian cancer risk: a meta-analysis. Mol Biol Rep 39, 9863–9868 (2012). https://doi.org/10.1007/s11033-012-1852-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-012-1852-0