Abstract
Data indicates that genetic factors alone do not account for ovarian tumorigenesis, suggesting that epigenetic status additionally affects this process. Therefore, we assessed the possible contribution of polymorphic variants of genes that may affect DNA methylation to the risk of ovarian cancer incidence in the Polish population. Using PCR-RFLP and HRM analyses, we studied the distribution of BHMT (rs3733890), MTHFD1 (rs2236225), MTHFR (rs1801133), MTR (rs1805087), MTRR (rs1801394) and TCN2 (rs1801198) genotypes and alleles in patients with ovarian cancer (n = 136) and controls (n = 160). Moreover, using DNA and methylation-specific PCR (MSP) we also determined the methylation of the Cadherin 13 (CDH13) promoter in cancerous tissue from these patients. We did not observe a significant association between all studied gene variants and the incidence of ovarian cancer. The lowest P trend = 0.1226 was observed for the MTHFR Ala222Val polymorphism. Moreover, the lowest P = 0.0772 was found in the comparison of MTHFR Ala/Ala versus Val/Val and Val/Ala genotypes in patients and control groups. The multifactor dimensionality reduction analysis also did not indicate a significant interactive genetic effect on ovarian cancer incidence for all analyzed SNPs. However, we observed frequent methylation of the CDH13 promoter in approximately 21% (29/136) patients with ovarian carcinomas. Our results might suggest that the selected polymorphic gene variants may not contribute to ovarian cancer incidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ovarian cancer is the one of the leading causes of malignant deaths in women in Europe and United States [1, 2]. Ovarian carcinogenesis remains unclear, though there is much evidence showing a decreased risk for ovarian cancer in women who use oral contraceptives, have greater parity, or breastfed long-term [3]. In contrast, an increased risk for ovarian cancer can be associated with environmental or inflammatory factors and a few significant-risk genetic components, such as high-penetrance genes (e.g., BRCA1) [3]. However, the genetic factors alone have been shown to be insufficient for ovarian carcinogenesis, suggesting the importance of changes in epigenetic status for both ovarian tumorigenesis and the development of other cancers [4–7].
Epigenetic changes include heritable alterations in gene expression that do not affect the DNA sequence. These changes encompass DNA methylation, covalent modification of histones, repositioning of nucleosomes, and micro-RNAs affecting posttranscriptional gene regulation [8, 9]. The transport of a methyl group to the carbon-5 position of cytosines within cytosine-guanine dinucleotides (CpG islands) leads to the formation of 5-methylcytosine. This methylation level of regulatory DNA sequences and the status of histone covalent modification correlate with the transcriptional activity of genes [10].
The methylation of genomic DNA is conducted by DNA methyltransferases (DNMTs) [10]. Their activity may contribute to aberrant DNA methylation and increased susceptibility to the development of various malignancies, including ovarian cancer [10]. DNMTs use S-adenosylmethionine (AdoMet) as their methyl group donor [10]. This common methyl group donor is biosynthesized from methionine and ATP by methionine adenosyltransferase [11] (Figure 1S, on-line supplementary data).
Intracellular levels of methionine can be maintained by the methylation of homocysteine by betaine-homocysteine methyltransferase (BHMT) (OMIM 602888) or 5-methyltetrahydrofolate-homocysteine methyltransferase (MTR) (OMIM 156570) (Figure 1S, on-line supplementary data). Either 5-methyltetrahydrofolate (5met-THF) or the choline oxidation product, betaine, may serve as a methyl group donor for the MTR and BHMT enzymes, respectively [12, 13]. 5met-THF is biosynthesized during the reduction of 5,10-methylenetetrahydrofolate by 5,10-methylenetetrahydrofolate reductase (MTHFR) (OMIM 607093) [14]. The cellular level of 5met-THF can also be controlled by methylenetetrahydrofolate dehydrogenase/methenyltetrahydrofolate cyclohydrolase/formyltetrahydrofolate synthetase (MTHFD1) (OMIM 172460) [15]. Transcobalamin II (TCN II) (OMIM 613441) is a blood plasma protein that functions as the primary transport protein for vitamin B12, which is necessary for MTR functionality [16]. MTR activity also requires reductive activation, which is conducted by methionine synthase reductase (MTRR) (OMIM 602568) [17].
The MTHFR Ala222Val (rs1801133), MTR Asp919Gly (rs1805087), and TCN2 Arg259Pro (rs1801198) polymorphisms have been linked to hypomethylation of genomic DNA in cancer cells [18–20]. Moreover, the BHMT Arg239Gln (rs3733890), MTHFD1 Arg653Gln (rs2236225), and MTRR Ile22Met (rs1801394) polymorphic variants have been shown to contribute to the incidence of various cancers [21–25].
Therefore, these functional variants of the BHMT, MTHFD1, MTHFR, MTR, MTRR and TCN2 (Figure 1S, on-line supplementary data) encoding enzymes associated with the biosynthesis of methionine may regulate the cellular AdoMet levels, DNMTs activity, and DNA methylation in cancer cells. We studied the frequency of the genotypes and alleles of these polymorphisms in women with ovarian cancer and controls in a sample from a Polish cohort. The promoter of Cadherin 13 (CDH13) has demonstrated an increased frequency of methylation in ovarian cancer patients [26, 27]. Therefore to determine the effect of investigated polymorphic variants on DNA methylation we also evaluated the methylation of the Cadherin 13 (CDH13) promoter in cancerous tissues from these tested patients.
Materials and methods
Patients and controls
The patient group was composed of one hundred thirty-six women with histologically recognized ovarian carcinoma according to the International Federation of Gynecology and Obstetrics (FIGO). All patient data including formalin-fixed, paraffin-embedded ovarian cancer samples were collected in the Clinic of Gynecological Surgery, Poznań University of Medical Sciences, Poland. Histopathological classification, including the stage, grade and tumor type, was performed by an experienced pathologist (Table 1). Written informed consent was obtained from all participating individuals. The procedures of the study were approved by the Local Ethical Committee of Poznań University of Medical Sciences. The control group comprised of one hundred sixty unrelated healthy female volunteers who were matched by age to the cancer patients (Table 1). All patients and controls were Caucasian from the Wielkopolska area of Poland.
Genotyping
DNA was isolated from peripheral blood leucocytes by salt extraction technique.. The chosen genes encode enzymes contributing directly or indirectly to the methylation of homocysteine to methionine. The six selected single nucleotide polymorphisms (SNPs) were chosen according to their functionality, location in the coding sequence, and minor allele frequency >0.1 in Caucasian population (Table 2). Genotyping of MTHFD1 (rs2236225), MTHFR (rs1801133), MTR (rs1805087), and TCN2 (rs1801198) was carried out by PCR, followed by restriction fragment length polymorphism (PCR-RFLP) analysis conducted according to the manufacturer’s instructions (Fermentas, Vilnius, Lithuania). DNA fragments were separated in 2% agarose gels and visualized by ethidium bromide staining. Starter sequences and conditions for PCR-RFLP analyses are provided in Table 1S on-line supplementary data. The BHMT SNP (rs3733890) and MTRR SNP (rs1801394) were genotyped by high-resolution melting curve analysis (HRM) on the LightCycler 480 system (Roche Diagnostics, Mannheim, Germany) (Table 1S on-line supplementary data). The genotyping quality of all polymorphisms was examined by repeat analysis of approximately 10% of the samples using the initial genotyping method or direct commercial sequencing.
Bisulphite modification of DNA and methylation-specific polymerase chain reaction (MSP)
Genomic DNA was isolated from formalin-fixed, paraffin-embedded tissue sections using QIAamp DNA FFPE Tissue Kit™ Qiagen GmbH, (Hilden, Germany). One μg of genomic DNA was subjected to bisulfite conversion of cytosine to uracil according to EZ DNA Methylation Kit™ procedure from Zymo Research Corp. (Orange, CA). In order to determine CDH13 gene promoter methylation we used the MSP technique.
PCR amplification was performed by FastStart Taq DNA Polymerase Roche Diagnostic GmbH, (Penzberg, Germany). Since bisulfite conversion of cytosine to uracil results to sequence differences, we used two pairs of primers: one for the unmethylated template and another for the methylated template (Table 1S online supplementary data) [26]. All MSP reactions were repeated and an additional third round of MSP was performed when the results were not consistent. Methylated and non-methylated bisulfite treated DNA from human methylated/non-methylated DNA Set Zymo Research Corp. (Orange, CA) was used as MSP positive control of methylated and unmethylated CDH13 gene (Fig. 1). In both reactions water was employed as a negative PCR control. For quality control, 20% of the samples were used for direct bisulphite sequencing.
Representative results of methylation-specific polymerase chain reaction (MSP) analysis of the CDH13 promoter methylation in ovarian cancer tissues. PCR products in lane U represent unmethylated alleles, whereas PCR products in lane M correspond to the presence of methylated alleles. PU and PM represent positive control for unmethylated and methylated templates, respectively, obtained from MSP reaction of bisulfite treated DNA of Human Methylated/Non-methylated DNA Set Zymo Research Corp. (Orange, CA). N represents negative PCR control with the addition of water. Numbers 1, 2, and 3 correspond to patients
Statistical analysis
The distribution of genotypes in patients and controls was tested for deviation from Hardy–Weinberg equilibrium. The χ2 square or Fisher exact tests were used to evaluate differences in genotypic and allelic prevalence between patients and controls. All polymorphisms were tested for association with ovarian cancer incidence using the χ2 test for trend (P trend). Moreover, the odds ratio (OR) and 95% confidence intervals (95% CI) were calculated. Statistical power was evaluated by power and sample size calculation program version 2.1.30 (http://medipe.psu.ac.th/episoft/pssamplesize/). Associations between the studied polymorphisms and the risk of ovarian cancer were tested using the nonparametric and genetic model-free Multifactor dimensionality reduction (MDR) approach (MDR version 2.0 beta 5). Statistical significance was evaluated using a 1,000-fold permutation test (MDR permutation testing module 0.4.9 alpha). A p value of <0.05 was considered statistically significant.
Results
Distribution of BHMT Arg239Gln, MTHFD1 Arg653Gln, MTHFR Ala222Val, MTR Asp919Gly, MTRR Ile22Met and TCN2 Arg259Pro polymorphic variants with regards to the incidence of ovarian cancer
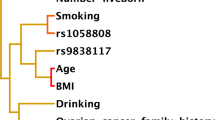
Genotype analysis of all studied polymorphisms did not display a significant deviation from Hardy–Weinberg equilibrium in the patient and control groups. We did not find a significant association between all studied SNPs and the incidence of ovarian cancer (Table 3). The lowest P trend = 0.1226 was observed for the MTHFR Ala222Val polymorphism. Moreover, the lowest P = 0.0772 was found in the comparison of MTHFR Ala/Ala versus Val/Val and Val/Ala genotypes in patients and control groups. The MDR evaluation also did not display a significant interactive genetic effect on ovarian cancer incidence for all analyzed SNPs (Table 4). All possible two-, three- and four-way SNP interactions were tested using tenfold cross validation in an exhaustive search (considering all possible SNP combinations). All of the “best models” (presenting the highest testing balanced accuracy and cross validation consistency >5 out of ten) did not demonstrate statistical significance, as evaluated by 1,000-fold permutation test. We also did not observe a significant contribution of the studied SNPs to tumor characteristics (data not shown).
CDH13 promoter methylation
We observed methylation of the CDH13 promoter in approximately 21% (29/136) of our patients with ovarian carcinomas. There was no association between the promoter methylation frequency and histological grade, clinical stage and differentiation. Moreover, we did not find differences in the frequency distribution of the methylation of the CDH13 promoter in groups of BHMT, MTHFD1, MTHFR, MTR, MTRR, and TCN2 genotypes and alleles (data not shown).
Discussion
Ovarian cancers are extremely heterogeneous at the clinical, histopathological, and molecular level [28]. The development of ovarian cancer is associated with an accumulation of genetic alterations and the presence of some polymorphisms in numerous cancer related genes [29]. These cancer related genes encode compounds of the steroid hormone pathway and its metabolic enzymes, components involved in cell cycle control, DNA repair and mismatch repair, and proteins linked to cellular signaling and chromosome segregation [29, 30]. These genetic factors may modulate cellular signaling pathways, the accumulation of genetic mistakes, and may increase cell proliferation, all of which are some of the features of ovarian carcinogenesis [29].
Recent findings have suggested that the initiation of ovarian carcinogenesis requires both genetic and epigenetic aberrations [31, 32]. To date it has been reported that multiple tumor suppressor genes and several cancer-associated genes are silenced via the hypermethylation of DNA regulatory sequences in ovarian cancer [32]. Moreover, ovarian tumorigenesis is also accompanied by global DNA hypomethylation, which increases the expression of many oncogenes, proto-oncogenes, cancer-promoting genes and cancer-associated genes [33].
We studied functional variants of genes that encode enzymes involved in either directly or indirectly providing a methyl group for DNA methylation. Our study did not reveal a significant association of BHMT Arg239Gln, MTHFD1 Arg653Gln, MTHFR Ala222Val, MTR Asp919Gly, MTRR Ile22Met and TCN2 Arg259Pro genotypes or alleles to ovarian cancer incidence. However, in these patients, we found frequent methylation of the CDH13 promoter in cancerous tissues, which was also observed at a similar level in other studies [26, 27].
To date little is known of the BHMT Arg239Gln and TCN2 Arg259Pro polymorphism contribution to ovarian cancer. The lack of an association to ovarian cancer of the BHMT Arg239Gln polymorphism in our study can be supported by the findings of Kotsopoulos et al., who did not find that dietary betaine and choline intake affected ovarian cancer incidence [34]. However, the BHMT 239Gln gene variant had previously been associated with the risk of cervical cancer incidence in a cohort from the Polish population [35]. The BHMT 239Gln gene variant has been also found to be a factor that reduces the risk of breast cancer mortality and the incidence of colorectal adenoma in patients with high dietary intake of folate and methionine and low alcohol consumption [22, 23, 36]. By contrast, the TCN2 Arg259Pro polymorphism has been found in linkage with the CpG island methylator phenotype in colorectal cancer [19].
Currently there has been no reported contribution of the MTHFD1 Arg653Gln, MTR Asp919Gly and MTRR Ile22Met polymorphisms to ovarian cancer [37]. Moreover, this observation was partially supported by Kotsopoulos et al., who did not indicate a clear relationship between supplemental intake of folate and methionine and the incidence of ovarian cancer [38]. However, the MTHFD1 Arg653Gln polymorphism has been associated with head and neck cancer (HNSCC) in patients that smoke and abuse alcohol [39]. Individuals with the MTHFD1 653Gln variant demonstrated a lower probability of event-free survival in childhood acute lymphoblastic leukemia (ALL) [40]. The MTR 919Gly gene variant was found to be a risk factor of HNSCC, breast cancer and colorectal cancer occurrence in alcoholics, and increase the susceptibility to retinoblastoma, multiple myeloma and non-Hodgkin’s lymphoma (NHL) [41–46]. The MTRR 22Met gene variant has been linked to HNSCC, lung cancer in smokers, esophageal squamous cell, meningioma, and colorectal carcinomas, and pancreatic cancer in patients with a drinking habit [24, 25, 47–50]. The MTRR Ile22Met polymorphism has also been associated with breast cancer and folate intake in postmenopausal women [51].
In contrast to the other studied polymorphisms, the MTHFR Ala222Val polymorphism was found as risk for ovarian cancer development [52, 53], while this finding was not observed by Terry et al. and Kelemen et al. [37, 54]. Gershoni-Baruch et al. showed an association between the MTHFR Ala222Val polymorphism and ovarian cancer risk in Jewish women [52]. Moreover, Jakubowska et al. demonstrated a statistically significant higher frequency of the MTHFR 222Val gene variant in patients with ovarian cancer in a Polish cohort from the Western Pomeranian area of Poland [53]. We found a higher MTHFR Val/Val and Val/Ala genotype frequency in patients with ovarian cancer than controls in a Polish population from the Wielkopolska region of Poland. However, the lack of statistical significance in our study can be due to the small sample size. The MTHFR 222Val gene variant has also been found to be a risk factor in the incidence of HNSCC, esophageal, lung, breast, stomach, and proximal colon cancers, NHL and ALL, meningioma and glioma [46, 48, 55–61].
Our study did not show an association between ovarian cancer and the six studied SNPs in folate and choline metabolism genes, namely BHMT, MTHFD1, MTHFR, MTR, MTRR, and TCN2. Moreover, we did not observe an interaction between these polymorphic variants in patients with ovarian cancer. Our genetic study was performed on a limited number of women with ovarian cancer and controls, therefore the role of these genetic variants should be further studied in other populations.
References
Ferlay J, Autier P, Boniol M, Heanue M, Colombet M, Boyle P (2007) Estimates of the cancer incidence and mortality in Europe in 2006. Ann Oncol 18:581–592
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ (2008) Cancer statistics, 2008. CA Cancer J Clin 58:71–96
Sueblinvong T, Carney ME (2009) Current understanding of risk factors for ovarian cancer. Curr Treat Options Oncol 10:67–81
Jones PA, Baylin SB (2007) The epigenomics of cancer. Cell 128:683–692
Balch C, Huang TH, Brown R, Nephew KP (2004) The epigenetics of ovarian cancer drug resistance and resensitization. Am J Obstet Gynecol 191:1552–1572
Barton CA, Hacker NF, Clark SJ, O’Brien PM (2008) DNA methylation changes in ovarian cancer: implications for early diagnosis, prognosis and treatment. Gynecol Oncol 109:129–139
Balch C, Fang F, Matei DE, Huang TH, Nephew KP (2009) Epigenetic changes in ovarian. Cancer Endocrinol 150:4003–4011
Esteller M (2008) Epigenetics in cancer. N Engl J Med 358:1148–1159
Schickel R, Boyerinas B, Park SM, Peter ME (2008) MicroRNAs: key players in the immune system, differentiation, tumorigenesis and cell death. Oncogene 27:5959–5974
Turek-Plewa J, Jagodziński PP (2005) The role of mammalian DNA methyltransferases in the regulation of gene expression. Cell Mol Biol Lett 10:631–647
Cantoni GL (1953) S-adenosylmethionine; a new intermediate fordem enzymatically from l-methionine and adenosinetriphosphate. J Biol Chem 204:403–416
Li YN, Gulati S, Baker PJ, Brody LC, Banerjee R, Kruger WD (1996) Cloning, mapping and RNA analysis of the human methionine synthase gene. Hum Mol Genet 5:851–858
Garrow TA (1996) Purification, kinetic properties, and cDNA cloning of mammalian betaine-homocysteine methyltransferase. J Biol Chem 271:22831–22838
Frosst P, Blom HJ, Milos R, Goyette P, Sheppard CA, Matthews RG, Boers GJ, den Heijer M, Kluijtmans LA, van den Heuvel LP, Rozen R (1995) A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nature Genet 10:111–113
Hum DW, Bell AW, Rozen R, MacKenzie RE (1988) Primary structure of a human trifunctional enzyme: isolation of a cDNA encoding methylenetetrahydrofolate-dehydrogenase, methenyltetrahydrofolate-cyclohydrolase, formyltetrahydrofolate synthetase. J Biol Chem 263:15946–15950
Hakami N, Neiman PE, Canellos GP, Lazerson J (1971) Neonatal megaloblastic anemia due to inherited transcobalamin II deficiency in two siblings. New Eng J Med 285:1163–1170
Leclerc D, Wilson A, Dumas R, Gafuik C, Song D, Watkins D, Heng HH, Rommens JM, Scherer SW, Rosenblatt DS, Gravel RA (1998) Cloning and mapping of a cDNA for methionine synthase reductase, a flavoprotein defective in patients with homocystinuria. Proc Natl Acad Sci USA 95:3059–3064
Paz MF, Avila S, Fraga MF, Pollan M, Capella G, Peinado MA, Sanchez-Cespedes M, Herman JG, Esteller M (2002) Germ-line variants in methyl-group metabolism genes and susceptibility to DNA methylation in normal tissues and human primary tumors. Cancer Res 62:4519–4524
Hazra A, Fuchs CS, Kawasaki T, Kirkner GJ, Hunter DJ, Ogino S (2010) Germline polymorphisms in the one-carbon metabolism pathway and DNA methylation in colorectal cancer. Cancer Causes Control 21:331–345
Kang S, Kim JW, Kang GH, Park NH, Song YS, Kang SB, Lee HP (2005) Polymorphism in folate- and methionine-metabolizing enzyme and aberrant CpG island hypermethylation in uterine cervical cancer. Gynecol Oncol 96:173–180
Liu H, Jin G, Wang H, Wu W, Liu Y, Qian J, Fan W, Ma H, Miao R, Hu Z, Sun W, Wang Y, Jin L, Wei Q, Shen H, Huang W, Lu D (2008) Association of polymorphisms in one-carbon metabolizing genes and lung cancer risk: a case-control study in Chinese population. Lung Cancer 61:21–29
Hazra A, Wu K, Kraft P, Fuchs CS, Giovannucci EL, Hunter DJ (2007) Twenty-four non-synonymous polymorphisms in the one-carbon metabolic pathway and risk of colorectal adenoma in the Nurses’ Health Study. Carcinogenesis 28:1510–1519
Xu X, Gammon MD, Wetmur JG, Bradshaw PT, Teitelbaum SL, Neugut AI, Santella RM, Chen J (2008) B-vitamin intake, one-carbon metabolism, and survival in a population-based study of women with breast cancer. Cancer Epidemiol Biomark Prev 17:2109–2116
Suzuki T, Matsuo K, Hasegawa Y, Hiraki A, Wakai K, Hirose K, Saito T, Sato S, Ueda R, Tajima K (2007) One-carbon metabolism-related gene polymorphisms and risk of head and neck squamous cell carcinoma: case-control study. Cancer Sci 98:1439–1446
Suzuki T, Matsuo K, Hiraki A, Saito T, Sato S, Yatabe Y, Mitsudomi T, Hida T, Ueda R, Tajima K (2007) Impact of one-carbon metabolism-related gene polymorphisms on risk of lung cancer in Japan: a case control study. Carcinogenesis 28:1718–1725
Wu Q, Lothe RA, Ahlquist T, Silins I, Tropé CG, Micci F, Nesland JM, Suo Z, Lind GE (2007) DNA methylation profiling of ovarian carcinomas and their in vitro models identifies HOXA9, HOXB5, SCGB3A1, and CRABP1 as novel targets. Mol Cancer 6:45
Bol GM, Suijkerbuijk KP, Bart J, Vooijs M, van der Wall E, van Diest PJ (2010) Methylation profiles of hereditary and sporadic ovarian cancer. Histopathology 57:363–370
Cho KR, Shih IM (2009) Ovarian cancer. Annu Rev Pathol 4:287–313
Bast RC Jr, Hennessy B, Mills GB (2009) The biology of ovarian cancer: new opportunities for translation. Nat Rev Cancer 9:415–428
Fasching PA, Gayther S, Pearce L, Schildkraut JM, Goode E, Thiel F, Chenevix-Trench G, Chang-Claude J, Wang-Gohrke S, Ramus S, Pharoah P, Berchuck A; OCAC (Ovarian Cancer Association Consortium) (2009) Role of genetic polymorphisms and ovarian cancer susceptibility Mol Oncol 3:171–181
Feinberg AP, Ohlsson R, Henikoff S (2006) The epigenetic progenitor origin of human cancer. Nat Rev Genet 7:21–33
Sharma S, Kelly TK, Jones PA (2010) Epigenetics in cancer. Carcinogenesis 31:27–36
Kwon MJ, Shin YK (2011) Epigenetic regulation of cancer-associated genes in ovarian cancer. Int J Mol Sci 12:983–1008
Kotsopoulos J, Hankinson SE, Tworoger SS (2010) Dietary betaine and choline intake are not associated with risk of epithelial ovarian cancer. Eur J Clin Nutr 64:111–114
Mostowska A, Myka M, Lianeri M, Roszak A, Jagodziński PP (2011) Folate and choline metabolism gene variants and development of uterine cervical carcinoma. Clin Biochem 44:596–600
Xu X, Gammon MD, Zeisel SH, Bradshaw PT, Wetmur JG, Teitelbaum SL, Neugut AI, Santella RM, Chen J (2009) High intakes of choline and betaine reduce breast cancer mortality in a population-based study. FASEB J 23:4022–4028
Kelemen LE, Sellers TA, Schildkraut JM, Cunningham JM, Vierkant RA, Pankratz VS, Fredericksen ZS, Gadre MK, Rider DN, Liebow M, Goode EL (2008) Genetic variation in the one-carbon transfer pathway and ovarian cancer risk. Cancer Res 68:2498–2506
Kotsopoulos J, Hecht JL, Marotti JD, Kelemen LE, Tworoger SS (2010) Relationship between dietary and supplemental intake of folate, methionine, vitamin B6 and folate receptor alpha expression in ovarian tumors. Int J Cancer 126:2191–2198
Silva LM, Silva JN, Galbiatti AL, Succi M, Ruiz MT, Raposo LS, Maniglia JV, Pavarino-Bertelli EC, Goloni-Bertollo EM (2011) Head and neck carconogenesis: impact of MTHFD1 G1958A polymorphism. Rev Assoc Med Bras 57:194–199
Krajinovic M, Lemieux-Blanchard E, Chiasson S, Primeau M, Costea I, Moghrabi A (2004) Role of polymorphisms in MTHFR and MTHFD1 genes in the outcome of childhood acute lymphoblastic leukemia. Pharmacogenomics J 4:66–72
Zhang Z, Shi Q, Liu Z, Sturgis EM, Spitz MR, Wei Q (2005) Polymorphisms of methionine synthase and methionine synthase reductase and risk of squamous cell carcinoma of the head and neck: a case-control analysis. Cancer Epidemiol Biomark Prev 14:1188–1193
Ma E, Iwasaki M, Junko I, Hamada GS, Nishimoto IN, Carvalho SM, Motola J Jr, Laginha FM, Tsugane S (2009) Dietary intake of folate, vitamin B6, and vitamin B12, genetic polymorphism of related enzymes, and risk of breast cancer: a case-control study in Brazilian women. BMC Cancer 9:122
Matsuo K, Ito H, Wakai K, Hirose K, Saito T, Suzuki T, Kato T, Hirai T, Kanemitsu Y, Hamajima H, Tajima K (2005) One-carbon metabolism related gene polymorphisms interact with alcohol drinking to influence the risk of colorectal cancer in Japan. Carcinogenesis 26:2164–2171
de Lima EL, da Silva VC, da Silva HD, Bezerra AM, de Morais VL, de Morais AL, Cruz RV, Barros MH, Hassan R, de Freitas AC, Muniz MT (2010) MTR polymorphic variant A2756G and retinoblastoma risk in Brazilian children. Pediatr Blood Cancer 54:904–908
Lima CS, Ortega MM, Ozelo MC, Araujo RC, De Souza CA, Lorand-Metze I, Annichino-Bizzacchi JM, Costa FF (2008) Polymorphisms of methylenetetrahydrofolate reductase (MTHFR), methionine synthase (MTR), methionine synthase reductase (MTRR), and thymidylate synthase (TYMS) in multiple myeloma risk. Leuk Res 32:401–405
Skibola CF, Forrest MS, Coppedé F, Agana L, Hubbard A, Smith MT, Bracci PM, Holly EA (2004) Polymorphisms and haplotypes in folate-metabolizing genes and risk of non-Hodgkin lymphoma. Blood 104:2155–2162
Stolzenberg-Solomon RZ, Qiao YL, Abnet CC, Ratnasinghe DL, Dawsey SM, Dong ZW, Taylor PR, Mark SD (2003) Esophageal and gastric cardia cancer risk and folate-and vitamin B(12)-related polymorphisms in Linxian, China. Cancer Epidemiol Biomark Prev 12:1222–1226
Bethke L, Webb E, Murray A, Schoemaker M, Feychting M, Lönn S, Ahlbom A, Malmer B, Henriksson R, Auvinen A, Kiuru A, Salminen T, Johansen C, Christensen HC, Muir K, McKinney P, Hepworth S, Dimitropoulou P, Lophatananon A, Swerdlow A, Houlston R (2008) Functional polymorphisms in folate metabolism genes influence the risk of meningioma and glioma. Cancer Epidemiol Biomark Prev 17:1195–1202
Matsuo K, Hamajima N, Hirai T, Kato T, Inoue M, Takezaki T, Tajima K (2002) Methionine synthase reductase gene A66G polymorphism is associated with risk of colorectal cancer. Asian Pac J Cancer Prev 3:353–359
Suzuki T, Matsuo K, Sawaki A, Mizuno N, Hiraki A, Kawase T, Watanabe M, Nakamura T, Yamao K, Tajima K, Tanaka H (2008) Alcohol drinking and one-carbon metabolism-related gene polymorphisms on pancreatic cancer risk. Cancer Epidemiol Biomarkers Prev 17:2742–2747
Suzuki T, Matsuo K, Hirose K, Hiraki A, Kawase T, Watanabe M, Yamashita T, Iwata H, Tajima K (2008) One-carbon metabolism-related gene polymorphisms and risk of breast cancer. Carcinogenesis 29:356–362
Gershoni-Baruch R, Dagan E, Israeli D, Kasinetz L, Kadouri E, Friedman E (2000) Association of the C677T polymorphism in the MTHFR gene with breast and/or ovarian cancer risk in Jewish women. Eur J Cancer 36:2313–2316
Jakubowska A, Gronwald J, Menkiszak J, Górski B, Huzarski T, Byrski T, Edler L, Lubiński J, Scott RJ, Hamann U (2007) Methylenetetrahydrofolate reductase polymorphisms modify BRCA1-associated breast and ovarian cancer risks. Breast Cancer Res Treat 104:299–308
Terry KL, Tworoger SS, Goode EL, Gates MA, Titus-Ernstoff L, Kelemen LE, Sellers TA, Hankinson SE, Cramer DW (2010) MTHFR polymorphisms in relation to ovarian cancer risk. Gynecol Oncol 119:319–324
Neumann AS, Lyons HJ, Shen H, Liu Z, Shi Q, Sturgis EM, Shete S, Spitz MR, El-Naggar A, Hong WK, Wei Q (2005) Methylenetetrahydrofolate reductase polymorphisms and risk of squamous cell carcinoma of the head and neck: a case-control analysis. Int J Cancer 115:131–136
Liu YX, Wang B, Wan MH, Tang WF, Huang FK, Li C (2011) Meta-analysis of the relationship between the metholenetetrahydrofolate reductase C677T genetic polymorphism, folate intake and esophageal cancer. Asian Pac J Cancer Prev 12:247–252
Arslan S, Karadayi S, Yildirim ME, Ozdemir O, Akkurt I (2011) The association between methylene-tetrahydrofolate reductase gene polymorphism and lung cancer risk. Mol Biol Rep 38:991–996
Maruti SS, Ulrich CM, Jupe ER, White E (2009) MTHFR C677T and postmenopausal breast cancer risk by intakes of one-carbon metabolism nutrients: a nested case-control study. Breast Cancer Res 11:R91
Lacasaña-Navarro M, Galván-Portillo M, Chen J, López-Cervantes M, López-Carrillo L (2006) Methylenetetrahydrofolate reductase 677C>T polymorphism and gastric cancer susceptibility in Mexico. Eur J Cancer 42:528–533
Iacopetta B, Heyworth J, Girschik J, Grieu F, Clayforth C, Fritschi L (2009) The MTHFR C677T and DeltaDNMT3B C-149T polymorphisms confer different risks for right- and left-sided colorectal cancer. Int J Cancer 125:84–90
Sood S, Das R, Trehan A, Ahluwalia J, Sachdeva MU, Varma N, Bansal D, Marwaha RK (2010) Methylenetetrahydrofolate reductase gene polymorphisms: association with risk for pediatric acute lymphoblastic leukemia in north Indians. Leuk Lymphoma 51:928–932
Acknowledgments
Supported by grant No. 502-01-01124182-07474, Poznan University of Medical Sciences. The technical assistance of Ms. Joanna Grzelczak and Longina Nowak is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
11033_2011_1359_MOESM1_ESM.tif
Figure 1S. Contribution of six folate and choline metabolism enzymes to DNA methylation. Enzyme abbreviations: BHMT, betaine-homocysteine methyltransferase; DNMTs, MTHFD1, methylenetetrahydrofolate dehydrogenase 1; MTHFR, 5,10-methylenetetrahydrofolate reductase; MTR, 5-methyltetrahydrofolate-homocysteine methyltransferase; MTRR, methionine synthase reductase; TCN2, transcobalamin II. Substrate abbreviations: AdoHcy, S-adenosylhomocysteine; AdoMet, S-adenosylmethionine; 5,10-CH2-THF, 5,10-methylenetetrahydrofolate; 5-CH3-THF, 5-metylotetrahydrofolate; DMG, dimethylglycine; HCY, homocysteine; MET, methionine; THF, tetrahydrofolate. (TIFF 33985 kb)
Rights and permissions
About this article
Cite this article
Pawlik, P., Mostowska, A., Lianeri, M. et al. Folate and choline metabolism gene variants in relation to ovarian cancer risk in the Polish population. Mol Biol Rep 39, 5553–5560 (2012). https://doi.org/10.1007/s11033-011-1359-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-011-1359-0