Abstract
Chronic kidney disease (CKD) has been typically implicated in cardiovascular risk, considering the function the kidney has related to blood pressure, vitamin D, red blood cell metabolism, and electrolyte and acid-base regulation. However, neurological consequences are also attributed to this disease. Among these, recent large epidemiological studies have demonstrated an increased risk for Parkinson’s disease (PD) in patients with CKD. Multiple studies have evaluated individually the association of blood pressure, vitamin D, and red blood cell dysmetabolism with PD, however, no study has reviewed the potential mechanisms related to these components in context of CKD and PD. In this review, we explored the association of CKD and PD and linked the components of the former to propose potential pathways explaining a future increased risk for PD, where renin-angiotensin system, oxidative stress, and inflammation have a main role. Potential preventive and therapeutic interventions based on these associations are also explored. More preclinical studies are needed to confirm the potential link of CKD conditions and future PD risk, whereas more interventional studies targeting this association are warranted to confirm their potential benefit in PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As the life expectancy increases, and the prevalence of the elderly population increases, more focus is attributed to chronic degenerative diseases. Parkinson’s disease (PD) is the second most common neurodegenerative disease, after Alzheimer’s (de Lau and Breteler 2006; Lee and Gilbert 2016; Nussbaum and Ellis 2003). Its prevalence increases with age, affecting 1 to 2% of the population over 60 years (Tysnes and Storstein 2017; Wirdefeldt et al. 2011). The cardinal signs characteristic of PD include resting tremor, rigidity, bradykinesia, which can be exhibited as hypomimia, hypophonia and micrographia, and postural and gait impairment, characterized by decreased arm swing, and multiple small steps. These present with a unilateral onset, respond to levodopa therapy, and patients can develop dyskinesia (Williams and Litvan 2013). Besides these motor symptoms, PD patients experience a range of non-motor symptoms, including constipation, sleep disorders, orthostatic hypotension, depression, among others (Tolosa et al. 2006; Massano and Bhatia 2012). These cardinal signs have been typically attributed to the loss of dopaminergic neurons in the substantia nigra (Shulman et al. 2011). Although great efforts have been made to fully understand the pathophysiology and cause of this dopaminergic cell loss, no mechanism that explains the exact cause of this disease has been described. Several factors have been associated with an increased risk of developing PD such as diabetes, vitamin D deficiency, anemia, and hypertension, among others (Yue et al. 2016; Knekt et al. 2010; Rozani et al. 2019; Hou et al. 2018).
Chronic kidney disease (CKD) results from chronic kidney damage, which can be confirmed via renal markers and reduction of estimated glomerular filtration rate (eGFR) to less than 60 ml/ min/ 1.73m2. The elderly population has an increased prevalence of CKD, owed primarily to an increase in risk factors such as diabetes, hypertension, and other cardiovascular risk factors (Mallappallil et al. 2014). Moreover, patients with CKD have an increased cardiovascular risk (Roderick et al. 2009). However, not only are CKD patients at risk for cardiovascular diseases, but evidence has shown that neurological complications such as cognitive dysfunction, peripheral and autonomic neuropathies, and encephalopathy are common in these patients (Arnold et al. 2016). Furthermore, dementia is more prevalent in this population (Etgen et al. 2012), and albuminuria, a marker of renal damage, is associated with cognitive impairment (Deckers et al. 2017), which might suggest a contribution of CKD conditions to neurodegenerative processes.
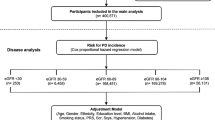
In addition to these complications, case reports have shown reversible parkinsonism, a clinical disorder characterized primarily by bradykinesia, resting tremor, rigidity and postural instability, in uremic patients, attributing the basal ganglia affection to uremic toxins, vascular changes, and metabolic acidosis (Wang et al. 1998; Lee et al. 2006; Sheu et al. 2007; Wang and Cheng 2003). This was supported by a retrospective cohort study that demonstrated increased risk for parkinsonism in uremic patients (Lin et al. 2012). However, these studies did not evaluate the presence of parkinsonism in the context of PD, as these two terms are not equally meaning, and shall not be used interchangeably. On the other side, few large epidemiological studies have assessed PD risk in patients with CKD (Nam et al. 2019; Wang et al. 2014; Wang et al. 2017), demonstrating an increased risk for PD in this population (characteristics of these studies are shown in Table 1). Nonetheless, the mechanisms behind this potential relation are not yet elucidated. In this review, we explore the association of CKD and PD based on the elements that compose CKD, such as oxidative stress and uremia, hypertension, vitamin D insufficiency, and anemia, and propose different pathways that may explain this increased future risk.
Oxidative stress in uremia and in PD: Common pathological pathways?
Accumulating evidence indicates a main role of oxidative stress in CKD pathophysiology (Duni et al. 2019; Vaziri 2004; Gyurászová et al. 2020; Sung et al. 2013; Liakopoulos et al. 2017; Kao et al. 2009; Ling and Kuo 2018). Studies have shown oxidative stress markers are present even in early stages of the disease (Kuchta et al. 2011; Annuk et al. 2001). The mechanism underlying oxidative stress in CKD involves greater presence of pro-oxidant substances producing reactive oxygen species (ROS), and a reduction in antioxidant processes. This greater presence of ROS is attributed to an impairment in mitochondria function, responsible for over-production of ROS, which is seen in CKD patients (Galvan et al. 2017; Granata et al. 2009). Moreover, a study evaluating rats with CKD demonstrated an up-regulation of NADPH oxidase, an enzyme responsible for the formation of ROS (Vaziri et al. 2003). Apart from mitochondrial dysfunction, another mechanism for elevation of ROS levels in CKD patients are uremic toxins. These promote inflammation via priming of polymorphonuclear leukocytes (Gyurászová et al. 2020; Tumur et al. 2010), which exacerbate oxidative stress as generation of myeloperoxidase by these cells promotes nitric oxide (NO) inactivation and ROS generation, the first necessary for its antioxidant function at kidney level (Modlinger et al. 2004; Kisic et al. 2016). Moreover, accumulation of homocysteine in CKD patients increases oxidative stress levels related to an inhibition of antioxidant activity of superoxide dismutase (SOD) (Massy et al. 2001). Regarding antioxidant processes, hemodialysis contributes greatly to this manner, as studies have observed that even a single session of hemodialysis increases lipid peroxides and decreases antioxidants (Peuchant et al. 1994; Jackson et al. 1995), which perpetuates damage and oxidative stress. In fact, this process increases as CKD progresses (Dounousi et al. 2006), which may derive from hemodialysis and its effect on ROS and antioxidants levels. Hemodialysis increase in oxidative stress levels are attributed to an activation of polymorphonuclear leukocytes which promote inflammation and ROS production (Cristol et al. 1994; Borazan et al. 2004). In this manner, over activation of immune response due to uremic toxins and hemodialysis promotes an inflammatory state, which added to the oxidative stress environment, contributes to CKD.
Similar to CKD, oxidative stress plays a major role in the pathophysiology of PD. Moreover, mitochondria dysfunction contributes primarily to ROS formation in PD (Schapira 2008), considering that the brain tissue is considerably vulnerable to oxidative stress, as most energy derives from oxidative phosphorylation and has high unsaturated lipid concentration, apart from the low density of antioxidant enzymes in this tissue (Floyd 1999; Hall et al. 2012). Complex I deficiencies in the respiratory chain origin most of the ROS in PD (Blesa et al. 2015). Furthermore, toxins used in animal models are based among other mechanisms on inhibition of this complex (Blesa and Przedborski 2014; Greenamyre et al. 2010), explaining the main role mitochondria has in PD genesis. On the other side, inflammation contributes to PD, as observed and discussed in CKD. Microglia activation and increase pro-inflammatory cytokines’ levels have been observed in animal models of PD (Członkowska et al. 1996), and this activation enhances NADPH oxidase activity in microglia, which in turn form ROS and contribute to the neurotoxicity of this process (Surace and Block 2012). Interestingly, as angiotensin II has shown to have inflammatory properties, inducing ROS via NADPH oxidase when binding to AT1 receptors (Seshiah et al. 2002; Benigni et al. 2010), studies have analyzed its role in animal models of PD, demonstrating that inflammatory response to these PD inducing toxins could be mediated via angiotensin II (Joglar et al. 2009; Rodriguez-Pallares et al. 2008). In fact, several reviews have discussed the presence of a renin-angiotensin system (RAS) in brain (Wright and Harding 2011; Wright and Harding 2013), and AT1 receptors have been shown to be present in high density in human striatum and substantia nigra (Rey et al. 2007), suggesting a role in the disease.
When analyzing the link between PD and CKD regarding oxidative stress and inflammation, two suggestions for this appear: RAS and peripheral inflammation via a damaged blood brain barrier. A recent review analyzed Alzheimer’s disease and CKD association, and postulated an overactivated RAS in CKD pathology, mediated by an overactivation of renin owed among other causes, to sympathetic activation (Zhang et al. 2020). This then may activate angiotensin II and, in conditions where blood brain barrier is disrupted as CKD (Mazumder et al. 2016), may reach brain tissue binding to AT1 receptors, causing ROS formation and oxidative stress, damaging neuronal tissue. This has been proposed in hypertension mechanisms, where the increased permeability of the blood brain barrier may allow access of angiotensin II to brain regulating pressure centers (Biancardi et al. 2014; Biancardi and Stern 2016). However, as AT1 receptors are also find in striatum and substantia nigra, this might be a pathway in which angiotensin II links CKD and PD. A study in an animal model of CKD showed disruption of SOD and catalase activities, as well as astrocytosis, in substantia nigra (Mazumder et al. 2019), indicating how oxidative stress conditions in CKD might reflect in neuronal damage. Moreover, as inflammation is present in CKD, and as blood brain barrier disruptions due to the disease may be found, systemic inflammation might contribute to neuroinflammation, a component essential in PD. A study evaluated the risk of PD in patients with serum elevated IL-6, a pro-inflammatory cytokine, and found a significantly increased risk compared to controls (Chen et al. 2008). In this manner, disruption of blood brain barrier and increase in RAS might contribute to link the inflammatory and oxidant conditions in CKD with PD brain damage.
Apart from the mechanism involving a disrupted brain blood barrier, a study in an animal model of CKD described a reno-cerebral reflex involving RAS when exposed to high-salt intake (Cao et al. 2015), where renal afferent sympathetic nerves activate brain RAS and this enhances renal RAS activity via efferent sympathetic activation, perpetuating kidney damage and fibrosis. As angiotensin II has inflammatory and ROS inducing properties, this brain RAS activation mediated by kidney damage might contribute to greater concentrations of angiotensin II in brain tissue, and activate AT1 receptors, inducing oxidative stress and inflammation in brain regions where these receptors are present, such as striatum and substantia nigra (Rey et al. 2007), thus eliciting a possible link between PD and CKD (shown in Fig. 1). However, more studies evaluating oxidative stress in brain regions in CKD conditions are needed, particularly to elicit if renal and brain RAS systems’ activation originated due to CKD mediate any oxidative stress damage in substantia nigra.
Hypothesis of the link between CKD and PD based on the overactivation of circulating and brain RAS. CKD conditions involve an altered RAS due to increased renin which lead to increase circulating angiotensin II levels. This in conditions of altered BBB barrier reach brain regions and bind to AT1 receptors, inducing oxidative stress and microglia activation. Moreover, SNS activation in CKD leads to increased activity of brain RAS, and increased angiotensin II levels, which may bind AT1 receptors, inducing neuronal damage. CKD = chronic kidney disease, PD = Parkinson’s disease, RAS = renin-angiotensin system, AT1R = angiotensin II receptor type 1, BBB = blood-brain-barrier, SNS = sympathetic nervous system, ROS= reactive oxygen species, Ang II= angiotensin II
Hypertension in CKD and PD risk
Patients with CKD experience a high prevalence of hypertension, especially as the disease progresses (Agarwal et al. 2003; United States Renal Data System 2019), considering that the kidney has a main role in regulating solute excretion and RAS activation. The pathophysiology involved in the high blood pressure is multifactorial, and several reviews have studied these mechanisms (Tedla et al. 2011; Huan et al. 2015). As the kidney’s function deteriorates due to tissue damage, sodium excretion decreases (Hall 2003), leading to a higher extracellular volume prompting a volume-dependent pressure increase. Moreover, as mentioned earlier, an overactivated RAS system is present in patients with CKD (Zhang et al. 2020; Weidmann et al. 1971; Sim et al. 2011), which together with an overactivated sympathetic nerve activity (Klein et al. 2003) contribute to the pathophysiology of hypertension in CKD. The interrelated mechanisms of these systems are well explained by the reno-cerebral reflex described due to high salt intake in an animal model (Cao et al. 2015). Furthermore, oxidative stress present in CKD conditions contributes to this increase in blood pressure related to inactivation of NO, which lead to endothelial dysfunction (Vaziri et al. 1998). Other mechanisms related to endothelins and renal prostaglandins are described in other studies, as elevated levels of endothelins are present in CKD patients with high levels of blood pressure (Dhaun et al. 2006; Kohan 2010).
Patients with PD experience blood pressure disorders related to an autonomic dysfunction (Asahina et al. 2013), thus having an impaired regulation of blood pressure, showing fluctuations in this value (Tsukamoto et al. 2013). Considering hypertension as risk factor for PD, various meta-analysis have studied their association and have found an increased risk of presenting PD in hypertensive population (Hou et al. 2018; Chen et al. 2019). The pathophysiological mechanisms for this relation are however speculative. One idea relies on the ischemic damage generated by chronic hypertensive states on basal ganglia, thalamus, and brain stem (Qiu et al. 2011; Greenberg et al. 2009), which could affect dopaminergic neurons. On the other side, oxidative stress and RAS system are common mechanism shared between these diseases (Manrique et al. 2009). The latter combined with a disrupted blood brain barrier due to hypertensive state (Biancardi et al. 2014; Zhang et al. 2010) could lead to an increase in circulating angiotensin II in brain regions with AT1 receptors, and circulating inflammatory cells, causing oxidative stress and inflammation, affecting neuronal tissue. Moreover, blockade of AT1 receptors in animal hypertensive models have shown to protect and improve blood brain barrier permeability (Kucuk et al. 2002; Pelisch et al. 2011), showing how RAS system contributes to this barrier disruption. Another mechanism that may link hypertension and PD is endothelin-mediated, as CKD patients with high endothelin levels experience endothelial dysfunction and high blood pressure levels which may be reduced with its antagonism (Dhaun et al. 2006; Kohan 2010; Goddard et al. 2004). Endothelin’s role in PD has been related to induction of oxidative stress and inflammation (Jain et al. 2014), and the high levels of this peptide in hypertensive conditions may promote neuronal damage via these mechanisms. In this manner, hypertensive states seen in CKD could contribute to the future PD risk mainly by RAS system, disruption of blood brain barrier, and endothelin and ischemia-induced neuronal damage.
Vitamin D serum levels in CKD and association with PD
A great proportion of patients with CKD experience vitamin D deficiency (González et al. 2004; Bhan et al. 2010), and this proportion increases as the disease progresses (Pitts et al. 1998). Besides the classical idea that a reduced renal mass decreases 1-alpha-hydroxylase and thus decreases 1,25-dihydroxivitamin D, different mechanisms have been proposed for this deficiency. These involve a decrease in 25-hydroxivitamin D, substrate necessary for production of 1,25-dihydroxivitamin D in kidneys. This decrease in substrate has been associated to a reduction in its diet uptake (Krassilnikova et al. 2014), an impaired synthesis related to uremic toxins (Michaud et al. 2010), and loss of its serum binding protein due to proteinuria (Caravaca-Fontan et al. 2016). Moreover, a reduction in glomerular filtration and renal megalin expression in CKD impedes 25-hydroxivitamin to reach renal tubular cells and be converted to its active form (Takemoto et al. 2003; Dusso 2011). However, apart from the classical actions related to calcium and phosphorus metabolism attributed to vitamin D, increase evidence points for a non-classical pathway, where extra-renal 1-alpha hydroxylase is found to be involved and regulates inflammation, cellular differentiation and proliferation (Jones 2007; Townsend et al. 2005). The importance of this non-classical pathway relies on its effect on CKD progression. Among these pathways, vitamin D deficiency has been related to an overactivation of RAS system (Li 2010; Zhang et al. 2008), which as discussed previously, interacts, and contributes to progression of CKD via inflammation and oxidative stress. Furthermore, the supplementation of this vitamin is then related to a suppression of this system (Li 2010; Zhang et al. 2008; Li et al. 2002), supporting the inverse relation of these mechanism. Another important mechanism relies on vitamin D role in the immune system, as studies have shown that 1,25-dihydroxivitamin D3 suppresses activation of NF-kappa B protein (Zhang et al. 2007; Yu et al. 1995), which play a role in modulating immune response, demonstrating an anti-inflammatory mechanism, where its deficit as in CKD conditions could exacerbate and lead to its progression.
In PD patients, similar to CKD conditions, low vitamin D levels have been proven to prevail (Soliman et al. 2019; Sleeman et al. 2017) compared to controls. Moreover, systematic reviews have assessed the association between low vitamin D levels and PD and have found an increased future risk for PD and an inverse association with disease severity via Hoehn and Yahr (HY) and Unified Parkinson Disease Rating Scale (UPDRS) Part III measurements (Rimmelzwaan et al. 2016; Luo et al. 2018). Among possible explanations in these studies, the limited outdoor activity has been proposed, however, patients in early PD, where ambulation is not severely affected, also present with low vitamin D levels (Soliman et al. 2019; Evatt et al. 2011). The possible explanation for the increased risk for PD in these patients may lie on the neuroprotective effects that have been attributed to vitamin D, as animal models of PD have shown attenuation of inflammation and dopamine degeneration when treated with vitamin D (Calvello et al. 2017), and increase production of neurotrophic factors in glial cells (Sanchez et al. 2009). Moreover, high levels of vitamin D receptor and 1-alpha hydroxylase have been found in the substantia nigra (Eyles et al. 2005), supporting the idea of a neuroprotective effect in this brain region. In fact, considering that vitamin D is a liposoluble substance, this can travel through the blood brain barrier and bind to receptors in substantia nigra, exerting its neuroprotective effects. Taken these mechanisms into consideration, low levels of vitamin D commonly seen in CKD conditions could exacerbate inflammatory conditions and promote neuronal damage due to decrease neurotrophic factors. Moreover, an important link between low vitamin D levels in CKD and PD may rely on RAS system. As discussed previously, vitamin D deficiency contributes to an increase in renin and angiotensin II (Li 2010; Zhang et al. 2008), which promote oxidant and inflammatory conditions, and together with the presence of disrupted blood brain barrier like CKD could reach brain regions and bind AT1 receptors, leading to neuronal damage.
Anemia in CKD and PD risk
A high proportion of patients with CKD experience anemia and this proportion increases as CKD progresses (Stauffer and Fan 2014; Voormolen et al. 2010). The main mechanism involved in its presence relies on a relative deficiency of erythropoietin (EPO) due to impaired kidney function (McGonigle et al. 1984; Babitt and Lin 2012), as EPO is produced via a hypoxia inducible manner mainly by renal cells (Suzuki and Yamamoto 2016). Moreover, other mechanisms play a role in anemia in CKD, one important being iron deficiency. In fact, a high percentage of patients with CKD have been found to be iron deficient (Ashby et al. 2009). Explanations to this deficiency have been attributed to an absolute and a functional deficiency (Babitt and Lin 2012). The latter is explained by increased levels of hepcidin in CKD patients (Zaritsky et al. 2009; Nemeth et al. 2004), which is in charge of regulating iron metabolism and in high levels inducing a reduction in its absorption and mobilization (Fishbane et al. 2009). Reduction of eGFR and inflammatory conditions in CKD contribute to this increase in hepcidin levels (Babitt and Lin 2012), leading to decreased iron levels, which are necessary for erythropoiesis.
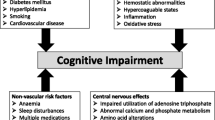
In PD, discrepancy exists whether hemoglobin levels are low or normal in patients compared to controls (Kasten et al. 2010; Deng et al. 2017). Moreover, this discrepancy also persists when assessing iron serum levels in these patients, as some studies have found low serum iron, while other have found no differences compared to controls (Medeiros et al. 2016; Mariani et al. 2013). A retrospective cohort study assessing PD risk in iron deficiency anemic patients found an increased risk compared to controls (Hong et al. 2016). Considering that iron deposition in substantia nigra has been found in PD patients (Martin et al. 2008), and iron is responsible for oxidative stress processes (Núñez et al. 2012), the question arises as why low iron serum levels may predispose to an increased PD risk. The answer may rely on an iron maldistribution process (Cabantchik et al. 2013), as iron overload in brain tissue and abnormal low serum levels may coexist. This maldistribution may be linked to hepcidin, as this has been shown to be widely distributed in the murine brain (Zechel et al. 2006). Furthermore, studies assessing hepcidin in cell culture and animal models of PD have shown contradictory results (Liang et al. 2020; Xu et al. 2016). A review proposed a dual role model of hepcidin, as pre-treatment with hepcidin can ameliorate iron accumulation, but its increased due to inflammatory conditions may contribute to oxidative stress and neuronal damage (Vela 2018). Considering that CKD involves an inflammatory state, this may lead to hepcidin detrimental role in neuronal damage, inducing iron overload and oxidative stress conditions. On the other side, EPO has been shown to exert neuroprotective effects in animal models of PD (Erbaş et al. 2015), resulting from its effect as antioxidant, anti-apoptotic, and anti-inflammatory agent (Ehrenreich et al. 2004). Thus, iron dysmetabolism and hepcidin, and EPO levels in CKD may be a possible link between PD and this disease. The association of CKD components and its pathophysiology and PD are displayed in Fig. 2.
Association of elements that compose CKD and PD. The main pathways in which most components of CKD may be indirectly linked to PD involve increased oxidative stress, inflammation, and RAS. However, anemic conditions due to EPO deficiency and iron dysmetabolism whereas vascular damage and high endothelin levels in hypertensive state may be directly linked to PD. CKD = chronic kidney disease, PD = Parkinson’s disease, RAS = renin-angiotensin system, EPO = erythropoietin
Therapeutic considerations of these associations
Considering the components that were discussed in the present review, different therapeutic modalities can be used for PD patients targeting the pathways previously mentioned, such as antioxidants for oxidative stress, anti-hypertensive medications, vitamin D supplementation, and iron chelators and erythropoietin. We reviewed any observational or interventional studies assessing these potential therapeutics. Considering antioxidant therapies and future PD risk, a meta-analysis showed patients with a dietary intake of vitamin E had a reduced risk for PD compared to controls (Etminan et al. 2005), but no association was found with other antioxidants such as vitamin C or beta-carotenes. However, more recent studies have shown inconsistent results (Hughes et al. 2016; Yang et al. 2017; Takeda et al. 2014). Two meta-analysis evaluating randomized clinical trials on the effect of antioxidant agents in PD showed no effect on disease progression (Negida et al. 2016; Attia et al. 2017).
On the other side, a meta-analysis evaluating anti-hypertensive medications and future PD risk observed an insignificant risk ratio for PD in overall anti-hypertensive agents use (Mullapudi et al. 2016), showing in subgroup analysis a significant risk reduction only in calcium channel blockers. Despite this reduction, a recent phase III randomized clinical trial assessing isradipine, a dihydropyridine calcium channel blocker, in PD patients showed isradipine failed to affect clinical progression of the disease (Parkinson Study Group STEADY-PD III Investigators 2020). Nonetheless, a pilot study evaluating an angiotensin converting enzyme (ACE) inhibitor in PD patients showed this may serve in management of motor fluctuations (Reardon et al. 2000), but a great limitation was its small sample size (n = 7 patients). Another study demonstrated ACE inhibitor use and a reduced number of falls in PD patients (Laudisio et al. 2017). These results exhibit the need of more clinical studies to elucidate the role of RAS modulating agents and other anti-hypertensive agents in PD.
A study evaluating EPO treatment in PD patients demonstrated its safety and tolerability in this population, showing in addition an improvement in motor function (Pedroso et al. 2012). However, its small sample size and the lack of a placebo control group limit the interpretation of these results regarding motor function. The same group of authors assessed EPO treatment in cognitive function in another sample of PD patients compared to placebo and observed a discrete improvement in this parameter, not different however, to the placebo group (Pedroso et al. 2018). Another study showed EPO treatment significantly improved non-motor, but not motor, symptoms compared to control (Jang et al. 2014). Considering iron depositions in substantia nigra, a study evaluated deferiprone, an iron chelator agent, in PD patients and observed a reduction in iron accumulation in substantia nigra and in UPDRS motor scores, relating this reduction to ceruloplasmin, an iron modulator, activity (Grolez et al. 2015). Another study assessing this agent showed a decrease in iron accumulation in dentate and caudate nucleus, but only few patients had a reduction in substantia nigra. Moreover, no significant improvement was observed in UPDRS motor scores compared to control (Martin-Bastida et al. 2017).
Lastly, vitamin D supplementation in PD patients has been evaluated in two studies. One showed that patients with Vitamin D supplementation had less worsening of HY and UPDRS part II compared to control (Suzuki et al. 2013), while the other showed no differences in PD severity, quality of life, balance or cognition compared to control, demonstrating however a difference in balance only when grouping patients based on age, having younger patients a greater benefit of vitamin D (Hiller et al. 2018).
Remarks on these associations: Correlations do not imply causation
It is important to consider that some mechanisms discussed in this review do not imply a direct causal effect on PD incidence. As described above, patients with CKD have high markers of oxidative stress, and reduction of antioxidant capacity, however, this mechanism is not unique for CKD, as these patients may have multiple comorbidities that may predispose to an oxidant environment, and the relation between these two conditions is to be viewed with caution. Nonetheless, in this review, we presented speculative pathways related to kidney function that may contribute to PD based on oxidant properties, as RAS and sympathetic mechanisms. Another mechanism that must be considered with caution is hypertension. On the one side, as hypertensive patients have been observed to have an increased risk for PD, the link between CKD related hypertension and PD might not be direct and specific. This is supported by hypertension contributing itself to future incidence of CKD. On the other side, the altered kidney’s contribution in function of RAS and overactivation of sympathetic system to hypertensive state is not to be neglected and might indirectly contribute to this association.
Anemia and vitamin D deficiency seen in CKD might be directly related to PD, considering the role the kidney has in vitamin D and red blood metabolism. This is supported by the increased prevalence of these conditions as CKD progresses. As vitamin D and EPO have a neuroprotective function, and iron dysmetabolism is observed in PD patients, the abnormalities present in CKD related to these elements might have a direct association to the later onset of PD. Nonetheless, this review considers that, although the mechanisms of hypertension and oxidative stress might not be specific for CKD and directly relate to PD, the pathways proposed in this study are interconnected and based primarily on RAS and its oxidant and inflammatory properties, thus, vitamin D deficiency and anemia, which are more specific for CKD, and hypertension, which is common but unspecific for CKD, might synergistically contribute to PD. It is important to mention, however, that the pathways proposed, linking CKD elements reviewed, are speculative and might lead to further research to confirm these potential associations.
Other mechanisms linking CKD and PD
In this review, we focused on analyzing the association of CKD and PD based on oxidative stress caused by CKD conditions, hypertension, vitamin D deficiency, and anemia. Furthermore, we integrated sympathetic nervous system role in RAS activity, oxidative stress, and inflammation in CKD (as shown in Fig. 1). However, there are other elements present in CKD that could be associated with PD, and these are shown in Table 2.
Conclusion
CKD and PD share common mechanisms regarding their pathophysiology. When breaking down CKD components and analyzing their association with PD, this review links evidence showing different potential pathways that may lead to an increased future risk for PD in patients with CKD, as retrospective cohort studies have shown. One potential pathway discussed is RAS system, as this is increased in CKD conditions, and this has been involved in preclinical studies of PD. Furthermore, studies evaluating therapies that target CKD components in PD have shown variable results. Further studies are needed to confirm the therapeutic potential of these interventions.
References
Agarwal R, Nissenson AR, Batlle D, Coyne DW, Trout JR, Warnock DG (2003) Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med 115:291–297
Annuk M, Fellström B, Akerblom O et al (2001) Oxidative stress markers in pre-uremic patients. Clin Nephrol 56(4):308–314
Arnold R, Issar T, Krishnan AV, Pussell BA (2016) Neurological complications in chronic kidney disease. JRSM Cardiovasc Dis 5:2048004016677687
Asahina M, Vichayanrat E, Low DA et al (2013) Autonomic dysfunction in parkinsonian disorders: assessment and pathophysiology. J Neurol Neurosurg Psychiatry 84(6):674–680
Ashby DR, Gale DP, Busbridge M, Murphy KG, Duncan ND, Cairns TD, Taube DH, Bloom SR, Tam FWK, Chapman RS, Maxwell PH, Choi P (2009) Plasma hepcidin levels are elevated but responsive to erythropoietin therapy in renal disease. Kidney Int 75(9):976–981
Attia AH, Gadelkarim M et al (2017) Meta-analysis of Creatine for Neuroprotection against Parkinson's disease. CNS Neurol Disord Drug Targets 16(2):169–175
Babitt JL, Lin HY (2012) Mechanisms of anemia in CKD. J Am Soc Nephrol 23(10):1631–1634
Benigni A, Cassis P, Remuzzi G (2010) Angiotensin II revisited: new roles in inflammation, immunology and aging. EMBO Mol Med 2(7):247–257
Bhan I, Burnett-Bowie SA, Ye J et al (2010) Clinical measures identify vitamin D deficiency in dialysis. Clin J Am Soc Nephrol 5:460–467
Biancardi VC, Son SJ, Ahmadi S, Filosa JA, Stern JE (2014) Circulating angiotensin II gains access to the hypothalamus and brain stem during hypertension via breakdown of the blood-brain barrier. Hypertension 63:572–579
Biancardi VC, Stern JE (2016) Compromised blood-brain barrier permeability: novel mechanism by which circulating angiotensin II signals to sympathoexcitatory centres during hypertension. J Physiol 594:1591–1600
Bitner A, Zalewski P, Klawe JJ, Newton JL (2015) Drug interactions in Parkinson's disease: safety of pharmacotherapy for arterial hypertension. Drugs Real World Outcomes 2(1):1–12
Blesa J, Przedborski S (2014) Parkinson's disease: animal models and dopaminergic cell vulnerability. Front Neuroanat 8:155
Blesa J, Trigo-Damas I, Quiroga-Varela A, Jackson-Lewis VR (2015) Oxidative stress and Parkinson's disease. Front Neuroanat 9:91
Borazan A, Ustün H, Ustundag Y, Aydemir S, Bayraktaroglu T, Sert M, Yilmaz A (2004) The effects of peritoneal dialysis and hemodialysis on serum tumor necrosis factoralpha, interleukin-6, interleukin-10 and C-reactive-protein levels. Mediat Inflamm 13:201–204
Cabantchik ZI, Munnich A, Youdim MB, Devos D (2013) Regional siderosis: a new challenge for iron chelation therapy. Front Pharmacol 4:167
Calvello R, Cianciulli A, Nicolardi G, de Nuccio F, Giannotti L, Salvatore R, Porro C, Trotta T, Panaro MA, Lofrumento DD (2017) Vitamin D treatment attenuates neuroinflammation and dopaminergic neurodegeneration in an animal model of Parkinson's disease, shifting M1 to M2 microglia responses. J NeuroImmune Pharmacol 12:327–339
Cao W, Li A, Wang L, Zhou Z, Su Z, Bin W, Wilcox CS, Hou FF (2015) A salt-induced Reno-cerebral reflex activates renin-angiotensin systems and promotes CKD progression. J Am Soc Nephrol 26(7):1619–1633
Caravaca-Fontan F, Gonzales-Candia B, Luna E, Caravaca F (2016) Relative importance of the determinants of serum levels of 25-hydroxy vitamin D in patients with chronic kidney disease. Nefrologia 36:510–516
Chen H, O'Reilly EJ, Schwarzschild MA, Ascherio A (2008) Peripheral inflammatory biomarkers and risk of Parkinson's disease. Am J Epidemiol 167(1):90–95
Chen J, Zhang C, Wu Y, Zhang D (2019) Association between hypertension and the risk of Parkinson’s disease: a meta-analysis of analytical studies. Neuroepidemiology 52:181–192
Cristol JP, Canaud B, Rabesandratana H et al (1994) Enhancement of reactive oxygen species production and cell surface markers expression due to haemodialysis. Nephrol Dial Transplant 9(4):389–394
Członkowska A, Kohutnicka M, Kurkowska-Jastrzebska I, Członkowski A (1996) Microglial reaction in MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine) induced Parkinson's disease mice model. Neurodegeneration 5(2):137–143
de Lau LM, Breteler MB (2006) Epidemiology of Parkinson’s disease. Lancet Neurol 5(6):525–535
Deckers K, Camerino I, van Boxtel MP et al (2017) Dementia risk in renal dysfunction: a systematic review and meta-analysis of prospective studies. Neurology 88(2):198–208
Deng Q, Zhou X, Chen J, Pan M, Gao H, Zhou J, Wang D, Chen Q, Zhang X, Wang Q, Xu Y (2017) Lower hemoglobin levels in patients with parkinson's disease are associated with disease severity and iron metabolism. Brain Res 1655:145–151
Dhaun N, Goddard J, Webb DJ (2006) The endothelin system and its antagonism in chronic kidney disease. J Am Soc Nephrol 17:943–955
Dhondup T, Qian Q (2017) Electrolyte and Acid-Base disorders in chronic kidney disease and end-stage kidney failure. Blood Purif 43(1–3):179–188
Dounousi E, Papavasiliou E, Makedou A, Ioannou K, Katopodis KP, Tselepis A, Siamopoulos KC, Tsakiris D (2006) Oxidative stress is progressively enhanced with advancing stages of CKD. Am J Kidney Dis 48(5):752–760
Duni A, Liakopoulos V, Roumeliotis S et al (2019) Oxidative stress in the pathogenesis and evolution of chronic kidney disease: untangling Ariadne's thread. Int J Mol Sci 20(15):3711
Dusso AS (2011) Kidney disease and vitamin D levels: 25-hydroxyvitamin D, 1,25-dihydroxyvitamin D, and VDR activation. Kidney Int Suppl 1(4):136–141
Ehrenreich H, Aust C, Krampe H, Jahn H, Jacob S, Herrmann M, Sirén AL (2004) Erythropoietin: novel approaches to neuroprotection in human brain disease. Metab Brain Dis 19(3–4):195–206
Erbaş O, Çınar BP, Solmaz V, Çavuşoğlu T, Ateş U (2015) The neuroprotective effect of erythropoietin on experimental Parkinson model in rats. Neuropeptides 49:1–5
Etgen T, Chonchol M, Förstl H, Sander D (2012) Chronic kidney disease and cognitive impairment: a systematic review and meta-analysis. Am J Nephrol 35:474–482
Etminan M, Gill SS, Samii A (2005) Intake of vitamin E, vitamin C, and carotenoids and the risk of Parkinson's disease: a meta-analysis. Lancet Neurol 4(6):362–365
Evatt M, DeLong M, Kumari M, Auinger P, McDermott M, Tangpricha V, Parkinson Study Group DATATOP Investigators (2011) High prevalence of hypovitaminosis D status in patients with early Parkinson disease. Arch Neurol 68:314–319
Eyles DW, Smith S, Kinobe R, Hewison M, McGrath JJ (2005) Distribution of the vitamin D receptor and 1 alpha-hydroxylase in human brain. J Chem Neuroanat 29(1):21–30
Fishbane S, Pollack S, Feldman HI, Joffe MM (2009) Iron indices in chronic kidney disease in the National Health and nutritional examination survey 1988-2004. Clin J Am Soc Nephrol 4(1):57–61
Floyd RA (1999) Antioxidants, oxidative stress, and degenerative neurological disorders. Proc Soc Exp Biol Med 222(3):236–245
Galvan DL, Green NH, Danesh FR (2017) The hallmarks of mitochondrial dysfunction in chronic kidney disease. Kidney Int 92(5):1051–1057
Goddard J, Johnston NR, Hand MF, Cumming AD, Rabelink TJ, Rankin AJ, Webb DJ (2004) Endothelin-a receptor antagonism reduces blood pressure and increases renal blood flow in hypertensive patients with chronic renal failure: a comparison of selective and combined endothelin receptor blockade. Circulation 109:1186–1193
González EA, Sachdeva A, Oliver DA, Martin KJ (2004) Vitamin D insufficiency and deficiency in chronic kidney disease: a single center observational study. Am J Nephrol 24:503–510
Granata S, Zaza G, Simone S, Villani G, Latorre D, Pontrelli P, Carella M, Schena F, Grandaliano G, Pertosa G (2009) Mitochondrial dysregulation and oxidative stress in patients with chronic kidney disease. BMC Genomics 10:388
Greenamyre JT, Cannon JR, Drolet R, Mastroberardino PG (2010) Lessons from the rotenone model of Parkinson's disease. Trends Pharmacol Sci 31(4):141–143
Greenberg SM, Vernooij MW, Cordonnier C, Viswanathan A, al-Shahi Salman R, Warach S, Launer LJ, van Buchem M, Breteler MM, Microbleed Study Group (2009) Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol 8(2):165–174
Grolez G, Moreau C, Sablonnière B, Garçon G, Devedjian JC, Meguig S, Gelé P, Delmaire C, Bordet R, Defebvre L, Cabantchik IZ, Devos D (2015) Ceruloplasmin activity and iron chelation treatment of patients with Parkinson's disease. BMC Neurol 15:74
Gyurászová M, Gurecká R, Bábíčková J, Tóthová Ľ (2020) Oxidative stress in the pathophysiology of kidney disease: implications for noninvasive monitoring and identification of biomarkers. Oxidative Med Cell Longev 2020:1–11
Hall CN, Klein-Flügge MC, Howarth C, Attwell D (2012) Oxidative phosphorylation, not glycolysis, powers presynaptic and postsynaptic mechanisms underlying brain information processing. J Neurosci 32(26):8940–8951
Hall JE (2003) The kidney, hypertension, and obesity. Hypertension. 41:625–633
Hiller AL, Murchison CF, Lobb BM et al (2018) A randomized, controlled pilot study of the effects of vitamin D supplementation on balance in Parkinson's disease: does age matter? PLoS One 13(9):e0203637
Hong CT, Huang YH, Liu HY, Chiou HY, Chan L, Chien LN (2016) Newly diagnosed Anemia increases risk of Parkinson's disease: a population-based cohort study. Sci Rep 6:29651
Hou L, Li Q, Jiang L, Qiu H, Geng C, Hong JS, Li H, Wang Q (2018) Hypertension and diagnosis of Parkinson's disease: a meta-analysis of cohort studies. Front Neurol 9:162
Huan Y, Cohen D, Townsend R (2015) Pathophysiology of hypertension in chronic kidney disease. In: Kimmel PL, and Rosenberg ME chronic renal disease. Elsevier Inc, London, pp. 163–169
Hughes KC, Gao X, Kim IY, Rimm EB, Wang M, Weisskopf MG, Schwarzschild MA, Ascherio A (2016) Intake of antioxidant vitamins and risk of Parkinson's disease. Mov Disord 31(12):1909–1914
Jackson P, Loughrey CM, Lightbody JH et al (1995) Effect of hemodialysis on total antioxidant capacity and serum antioxidants in patients with chronic renal failure. Clin Chem 41:1135–1138
Jain A, Migdalska A, Jain A (2014) Endothelin-1-induced endoplasmic reticulum stress in Parkinson's disease. Pharmacologia 5(3):84–90
Jang W, Park J, Shin KJ, Kim JS, Kim JS, Youn J, Cho JW, Oh E, Ahn JY, Oh KW, Kim HT (2014) Safety and efficacy of recombinant human erythropoietin treatment of non-motor symptoms in Parkinson's disease. J Neurol Sci 337(1–2):47–54
Jin X, Liu MY, Zhang DF, Gao H, Wei MJ (2018) Elevated circulating magnesium levels in patients with Parkinson's disease: a meta-analysis. Neuropsychiatr Dis Treat 14:3159–3168
Joglar B, Rodriguez-Pallares J, Rodriguez-Perez AI, Rey P, Guerra MJ, Labandeira-Garcia JL (2009) The inflammatory response in the MPTP model of Parkinson's disease is mediated by brain angiotensin: relevance to progression of the disease. J Neurochem 109(2):656–669
Jones G (2007) Expanding role for vitamin D in chronic kidney disease: importance of blood 25-OH-D levels and extra-renal 1alpha-hydroxylase in the classical and nonclassical actions of 1alpha,25-dihydroxyvitamin D(3). Semin Dial 20(4):316–324
Kao M, Ang D, Pall A, Struthers A (2009) Oxidative stress in renal dysfunction: mechanisms, clinical sequelae and therapeutic options. J Hum Hypertens 24(1):1–8
Kasten M, Tadic V, Klein C, Rocca WA, Savica R, Eric Ahlskog J, Grossardt BR (2010) Anemia or low hemoglobin levels preceding Parkinson disease: a case-control study. Neurology 74(20):1655–1656
Kisic B, Miric D, Dragojevic I et al (2016) Role of myeloperoxidase in patients with chronic kidney disease. Oxidative Med Cell Longev 2016:1069743
Klein IH, Ligtenberg G, Neumann J, Oey PL, Koomans HA, Blankestijn PJ (2003) Sympathetic nerve activity is inappropriately increased in chronic renal disease. J Am Soc Nephrol 14:3239–3244
Knekt P, Kilkkinen A, Rissanen H et al (2010) Serum vitamin D and the risk of Parkinson disease. Arch Neurol 67(7):808–811
Kohan DE (2010) Endothelin, hypertension and chronic kidney disease: new insights. Curr Opin Nephrol Hypertens 19(2):134–139
Krassilnikova M, Ostrow K, Bader A et al (2014) Low dietary intake of vitamin D and vitamin D deficiency in hemodialysis patients. J Nephrol Ther 4(3):166
Kuchta A, Pacanis A, Kortas-Stempak B, Çwiklińska A, Ziętkiewicz M, Renke M, Rutkowski B (2011) Estimation of oxidative stress markers in chronic kidney disease. Kidney Blood Press Res 34(1):12–19
Kucuk M, Kaya M, Kalayci R, Cimen V, Kudat H, Arican N, Elmas I, Korkut F (2002) Effects of losartan on the blood-brain barrier permeability in long-term nitric oxide blockade-induced hypertensive rats. Life Sci 71(8):937–946
Laudisio A, Lo Monaco MR, Silveri MC, Bentivoglio AR, Vetrano DL, Pisciotta MS, Brandi V, Bernabei R, Zuccalà G (2017) Use of ACE-inhibitors and falls in patients with Parkinson's disease. Gait Posture 54:39–44
Lee A, Gilbert RM (2016) Epidemiology of Parkinson disease. Neurol Clin 34(8):955–965
Lee PH, Shin DH, Kim JW, Song YS, Kim HS (2006) Parkinsonism with basal ganglia lesions in a patient with uremia: evidence of vasogenic edema. Parkinsonism Relat Disord 12:93–96
Li YC (2010) Renoprotective effects of vitamin D analogs. Kidney Int 78(2):134–139
Li YC, Kong J, Wei M, Chen ZF, Liu SQ, Cao LP (2002) 1,25-Dihydroxyvitamin D(3) is a negative endocrine regulator of the renin-angiotensin system. J Clin Invest 110(2):229–238
Liakopoulos V, Roumeliotis S, Gorny X et al (2017) Oxidative stress in hemodialysis patients: a review of the literature. Oxidative Med Cell Longev 2017:1–22
Liang T, Qian Z, Mu M et al (2020) Brain hepcidin suppresses major pathologies in experimental parkinsonism. iScience 23(7):101284
Lin H, Lin H, Chen Y (2012) Increased risks of parkinsonism in the 3 years after chronic renal failure. Int J Clin Pract 66(5):499–503
Ling X, Kuo K (2018) Oxidative stress in chronic kidney disease. Ren Replace Ther 4(1)
Luo X, Ou R, Dutta R, Tian Y, Xiong H, Shang H (2018) Association between serum vitamin D levels and Parkinson's disease: a systematic review and meta-analysis. Front Neurol 9:909
Mallappallil M, Friedman EA, Delano BG, McFarlane SI, Salifu MO (2014) Chronic kidney disease in the elderly: evaluation and management. Clin Pract (Lond) 11(5):525–535
Manrique C, Lastra G, Gardner M, Sowers JR (2009) The renin angiotensin aldosterone system in hypertension: roles of insulin resistance and oxidative stress. Med Clin North Am 93(3):569–582
Mao CJ, Zhong CK, Yang Y, Yang YP, Wang F, Chen J, Zhang JR, Zhang HJ, Jin H, Xu LL, Huang JY, Liu CF (2017) Serum sodium and chloride are inversely associated with dyskinesia in Parkinson's disease patients. Brain Behav 7(12):e00867
Mariani S, Ventriglia M, Simonelli I, Donno S, Bucossi S, Vernieri F, Melgari JM, Pasqualetti P, Rossini PM, Squitti R (2013) Fe and cu do not differ in Parkinson's disease: a replication study plus meta-analysis. Neurobiol Aging 34(2):632–633
Martin WR, Wieler M, Gee M (2008) Midbrain iron content in early Parkinson disease: a potential biomarker of disease status. Neurology 70:1411–1417
Martin-Bastida A, Ward RJ, Newbould R, Piccini P, Sharp D, Kabba C, Patel MC, Spino M, Connelly J, Tricta F, Crichton RR, Dexter DT (2017) Brain iron chelation by deferiprone in a phase 2 randomised double-blinded placebo controlled clinical trial in Parkinson's disease. Sci Rep 7(1):1398
Massano J, Bhatia KP (2012) Clinical approach to Parkinson's disease: features, diagnosis, and principles of management. Cold Spring Harb Perspect Med 2(6):a008870
Massy ZA, Ceballos I, Chadefaux-Vekemens B, Nguyen-Khoa T, Descamps-Latscha B, Drüeke TB, Jungers P (2001) Homocyst(e)ine, oxidative stress, and endothelium function in uremic patients. Kidney Int Suppl 78:S243–S245
Mazumder MK, Giri A, Kumar S, Borah A (2016) A highly reproducible mice model of chronic kidney disease: evidences of behavioural abnormalities and blood-brain barrier disruption. Life Sci 161:27–36
Mazumder MK, Paul R, Bhattacharya P et al (2019) Neurological sequel of chronic kidney disease: from diminished Acetylcholinesterase activity to mitochondrial dysfunctions, oxidative stress and inflammation in mice brain. Sci Rep 9:3097
McGonigle RJ, Wallin JD, Shadduck RK, Fisher JW (1984) Erythropoietin deficiency and inhibition of erythropoiesis in renal insufficiency. Kidney Int 25(2):437–444
Medeiros MS, Schumacher-Schuh A, Cardoso AM, Bochi GV, Baldissarelli J, Kegler A, Santana D, Chaves CMMBS, Schetinger MRC, Moresco RN, Rieder CRM, Fighera MR (2016) Iron and oxidative stress in Parkinson's disease: an observational study of injury biomarkers. PLoS One 11(1):e0146129
Michaud J, Naud J, Ouimet D, Demers C, Petit JL, Leblond FA, Bonnardeaux A, Gascon-Barré M, Pichette V (2010) Reduced hepatic synthesis of calcidiol in uremia. J Am Soc Nephrol 21(9):1488–1497
Modlinger P, Wilcox C, Aslam S (2004) Nitric oxide, oxidative stress, and progression of chronic renal failure. Semin Nephrol 24(4):354–365
Mullapudi A, Gudala K, Boya CS, Bansal D (2016) Risk of Parkinson's disease in the users of antihypertensive agents: an evidence from the meta-analysis of observational studies. J Neurodegener Dis 2016:5780809
Nam G, Kim N, Han K et al (2019) Chronic renal dysfunction, proteinuria, and risk of Parkinson's disease in the elderly. Mov Disord 34(8):1184–1191
Negida A, Menshawy A, El Ashal G et al (2016) Coenzyme Q10 for patients with Parkinson's disease: a systematic review and meta-analysis. CNS Neurol Disord Drug Targets 15(1):45–53
Nemeth E, Tuttle MS, Powelson J, Vaughn MB, Donovan A, Ward DM, Ganz T, Kaplan J (2004) Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science 306(5704):2090–2093
Núñez MT, Urrutia P, Mena N, Aguirre P, Tapia V, Salazar J (2012) Iron toxicity in neurodegeneration. Biometals 25(4):761–776
Nussbaum RL, Ellis CE (2003) Alzheimer’s disease and Parkinson’s disease. N Engl J Med 348(14):356–1364
Ori Y, Bergman M, Bessler H, Zingerman B, Levy-Drummer RS, Gafter U, Salman H (2013)
Parkinson Study Group STEADY-PD III Investigators (2020) Isradipine versus placebo in early Parkinson disease: a randomized trial. Ann Intern Med 172(9):591–598
Pedroso I, Bringas ML, Aguiar A, Morales L, Alvarez M, Valdés PA, Alvarez L (2012) Use of Cuban recombinant human erythropoietin in Parkinson's disease treatment. MEDICC Rev 14(1):11–17
Pedroso I, Garcia M, Casabona E, Morales L, Bringas M, Pérez L, Rodríguez T, Sosa I, Ricardo Y, Padrón A, Amaro D (2018) Protective activity of Erythropoyetine in the cognition of patients with Parkinson's disease. Behav Sci (Basel) 8(5):51
Pelisch N, Hosomi N, Ueno M, Nakano D, Hitomi H, Mogi M, Shimada K, Kobori H, Horiuchi M, Sakamoto H, Matsumoto M, Kohno M, Nishiyama A (2011) Blockade of AT1 receptors protects the blood-brain barrier and improves cognition in Dahl salt-sensitive hypertensive rats. Am J Hypertens 24(3):362–368
Peuchant E, Carbonneau MA, Dubourg L, Thomas MJ, Perromat A, Vallot C, Clerc M (1994) Lipoperoxidation in plasma and red blood cells of patients undergoing haemodialysis: vitamins A, E, and iron status. Free Radic Biol Med 16(3):339–346
Pitts TO, Piraino BH, Mitro R et al (1998) Hyperparathyroidism and 1,25-dihydroxyvitamin D deficiency in mild, moderate, and severe renal failure. J Clin Endocrinol Metab 67(5):876–881
Qiu C, Hu G, Kivipelto M, Laatikainen T, Antikainen R, Fratiglioni L, Jousilahti P, Tuomilehto J (2011) Association of blood pressure and hypertension with the risk of Parkinson disease: the national FINRISK study. Hypertension 57(6):1094–1100
Rama Rao KV, Jayakumar AR, Norenberg DM (2003) Ammonia neurotoxicity: role of the mitochondrial permeability transition. Metab Brain Dis 18(2):113–127
Reardon KA, Mendelsohn FA, Chai SY, Horne MK (2000) The angiotensin converting enzyme (ACE) inhibitor, perindopril, modifies the clinical features of Parkinson's disease. Aust NZ J Med 30(1):48–53
Rey P, Lopez-Real A, Sanchez-Iglesias S, Muñoz A, Soto-Otero R, Labandeira-Garcia JL (2007) Angiotensin type-1-receptor antagonists reduce 6-hydroxydopamine toxicity for dopaminergic neurons. Neurobiol Aging 28:555–567
Rimmelzwaan LM, van Schoor NM, Lips P et al (2016) Systematic review of the relationship between vitamin D and Parkinson's disease. J Parkinsons Dis 6(1):29–37
Roderick PJ, Atkins RJ, Smeeth L, Mylne A, Nitsch DDM, Hubbard RB, Bulpitt CJ, Fletcher AE (2009) CKD and mortality risk in older people: a community-based population study in the United Kingdom. Am J Kidney Dis 53:950–960
Rodriguez-Pallares J, Rey P, Parga JA, Muñoz A, Guerra MJ, Labandeira-Garcia JL (2008) Brain angiotensin enhances dopaminergic cell death via microglial activation and NADPH-derived ROS. Neurobiol Dis 31(1):58–73
Rozani V, Giladi N, Gurevich T, el-Ad B, Tsamir J, Hemo B, Peretz C (2019) Anemia in men and increased Parkinson's disease risk: a population-based large scale cohort study. Parkinsonism Relat Disord 64:90–96
Sanchez B, Relova J, Gallego R et al (2009) 1,25-Dihydroxyvitamin D3administration to 6-hydroxydopamine-lesioned rats increases glial cell line-derived neurotrophic factor and partially restores tyrosine hydroxylase expression in substantia nigra and striatum. J Neurosci Res 87(3):723–732
Schapira AH (2008) Mitochondria in the aetiology and pathogenesis of Parkinson's disease. Lancet Neurol 7(1):97–109
Seshiah PN, Weber DS, Rocic P et al (2002) Angiotensin II stimulation of NAD(P)H oxidase activity: upstream mediators. Circ Res 91(5):406–413
Sheu YL, Cheng SJ, Chen YM et al (2007) The syndrome of bilateral basal ganglia lesions in diabetic uremic patients presenting with a relapsing and remitting course: a case report. Acta Neurol Taiwanica 16:226–230
Shulman JM, De Jager PL, Feany MB (2011) Parkinson’s disease: genetics and pathogenesis. Annu Rev Pathol 6:193–222
Sim JJ, Shi J, Calara F, Rasgon S, Jacobsen S, Kalantar-Zadeh K (2011) Association of plasma renin activity and aldosterone-renin ratio with prevalence of chronic kidney disease: the Kaiser Permanente Southern California cohort. J Hypertens 29(11):2226–2235
Sleeman I, Aspray T, Lawson R, Coleman S, Duncan G, Khoo TK, Schoenmakers I, Rochester L, Burn D, Yarnall A (2017) The role of vitamin D in disease progression in early Parkinson's disease. J Parkinsons Dis 7(4):669–675
Soliman RH, Oraby MI, Hussein M, Abd el-Shafy S, Mostafa S (2019) Could vitamin D deficiency have an impact on motor and cognitive function in Parkinson’s disease? Egypt J Neurol Psychiatry Neurosurg 55:34
Stauffer ME, Fan T (2014) Prevalence of anemia in chronic kidney disease in the United States. PLoS One 9(1):e84943
Sung CC, Hsu YC, Chen CC et al (2013) Oxidative stress and nucleic acid oxidation in patients with chronic kidney disease. Oxidative Med Cell Longev 2013:301982
Surace MJ, Block ML (2012) Targeting microglia-mediated neurotoxicity: the potential of NOX2 inhibitors. Cell Mol Life Sci 69(14):2409–2427
Suzuki M, Yoshioka M, Hashimoto M, Murakami M, Noya M, Takahashi D, Urashima M (2013) Randomized, double-blind, placebo-controlled trial of vitamin D supplementation in Parkinson disease. Am J Clin Nutr 97(5):1004–1013
Suzuki N, Yamamoto M (2016) Roles of renal erythropoietin-producing (REP) cells in the maintenance of systemic oxygen homeostasis. Pflugers Arch 468(1):3–12
Takeda A, Nyssen OP, Syed A, Jansen E, Bueno-de-Mesquita B, Gallo V (2014) Vitamin a and carotenoids and the risk of Parkinson's disease: a systematic review and meta-analysis. Neuroepidemiology 42(1):25–38
Takemoto F, Shinki T, Yokoyama K, Inokami T, Hara S, Yamada A, Kurokawa K, Uchida S (2003) Gene expression of vitamin D hydroxylase and megalin in the remnant kidney of nephrectomized rats. Kidney Int 64(2):414–420
Tedla FM, Brar A, Browne R, Brown C (2011) Hypertension in chronic kidney disease: navigating the evidence. Int J Hypertens 2011:132405
Tolosa E, Wenning G, Poewe W (2006) The diagnosis of Parkinson’s disease. Lancet Neurol 5:75–86
Townsend K, Evans KN, Campbell MJ, Colston KW, Adams JS, Hewison M (2005) Biological actions of extra-renal 25-hydroxyvitamin D-1α-hydroxylase and implications for chemoprevention and treatment. J Steroid Biochem Mol Biol 97:103–109
Tsukamoto T, Kitano Y, Kuno S (2013) Blood pressure fluctuation and hypertension in patients with Parkinson’s disease. Brain Behav 3(6):710–714
Tumur Z, Shimizu H, Enomoto A, Miyazaki H, Niwa T (2010) Indoxyl sulfate upregulates expression of ICAM-1 and MCP-1 by oxidative stress-induced NF-κB activation. Am J Nephrol 31(5):435–441
Tysnes O, Storstein A (2017) Epidemiology of Parkinson's disease. J Neural Transm (Vienna) 124(8):901–905
United States Renal Data System. 2019 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Bethesda, MD, 2019
Vaziri ND, Dicus M, Ho N et al (2003) Oxidative stress and dysregulation of superoxide dismutase and NADPH oxidase in renal insufficiency. Kidney Int 63(1):179–185
Vaziri ND (2004) Oxidative stress in uremia: nature, mechanisms, and potential consequences. Semin Nephrol 24(5):469–473
Vaziri ND, Oveisi F, Ding Y (1998) Role of increased oxygen free radical activity in the pathogenesis of uremic hypertension. Kidney Int 53:1748–1754
Vela D (2018) The dual role of Hepcidin in brain Iron load and inflammation. Front Neurosci 12:740
Voormolen N, Grootendorst DC, Urlings TA et al (2010) Prevalence of Anemia and its impact on mortality and hospitalization rate in Predialysis patients. Nephron Clin Pract 115:133–141
Wang HC, Brown P, Lees AJ (1998) Acute movement disorders with bilateral basal ganglia lesions in uremia. Mov Disord 13:952–957
Wang HC, Cheng SJ (2003) The syndrome of acute bilateral basal ganglia lesions in diabetic uremic patients. J Neurol 250:948–955
Wang I, Lin C, Wu Y et al (2014) Increased risk of Parkinson's disease in patients with end-stage renal disease: a retrospective cohort study. Neuroepidemiology 42(4):204–210
Wang S, Yun J, Shin D et al (2017) Chronic kidney disease: a risk factor for Parkinson’s disease. Korean J Clin Geriatr 18(2):95–101
Weidmann P, Maxwell MH, Lupu AN, Lewin AJ, Massry SG (1971) Plasma renin activity and blood pressure in terminal renal failure. N Engl J Med 285(14):757–762
Wesson DE, Buysse JM, Bushinsky DA (2020) Mechanisms of metabolic acidosis-induced kidney injury in chronic kidney disease. J Am Soc Nephrol 31(3):469–482
Williams DR, Litvan I (2013) Parkinsonian syndromes. Continuum (Minneap Minn) 19(5 movement disorders):1189-1212
Wirdefeldt K, Adami HO, Cole P et al (2011) Epidemiology and etiology of Parkinson’s disease: a review of the evidence. Eur J Epidemiol 26(Suppl 1):S1–S58
Wright JW, Harding JW (2011) Brain renin-angiotensin--a new look at an old system. Prog Neurobiol 95(1):49–67
Wright JW, Harding JW (2013) The brain renin-angiotensin system: a diversity of functions and implications for CNS diseases. Pflugers Arch 465(1):133–151
Xu Q, Kanthasamy AG, Jin H, Reddy MB (2016) Hepcidin plays a key role in 6-OHDA induced Iron overload and apoptotic cell death in a cell culture model of Parkinson's disease. Parkinsons Dis 2016:8684130
Yang F, Wolk A, Håkansson N, Pedersen NL, Wirdefeldt K (2017) Dietary antioxidants and risk of Parkinson's disease in two population-based cohorts. Mov Disord 32(11):1631–1636
Yu XP, Bellido T, Manolagas SC (1995) Down-regulation of NF-kappa B protein levels in activated human lymphocytes by 1,25-dihydroxyvitamin D3. Proc Natl Acad Sci U S A 92(24):10990–10994
Yue X, Li H, Yan H, Zhang P, Chang L, Li T (2016) Risk of Parkinson disease in diabetes mellitus. Medicine 95(18):e3549
Zahed NS, Chehrazi S (2017) The evaluation of the relationship between serum levels of Interleukin-6 and Interleukin-10 and metabolic acidosis in hemodialysis patients. Saudi J Kidney Dis Transpl 28(1):23–29
Zaritsky J, Young B, Wang HJ, Westerman M, Olbina G, Nemeth E, Ganz T, Rivera S, Nissenson AR, Salusky IB (2009) Hepcidin--a potential novel biomarker for iron status in chronic kidney disease. Clin J Am Soc Nephrol 4(6):1051–1056
Zechel S, Huber-Wittmer K, von Bohlen und Halbach O (2006) Distribution of the iron-regulating protein hepcidin in the murine central nervous system. J Neurosci Res 84(4):790–800
Zhang CY, He FF, Su H, Zhang C, Meng XF (2020) Association between chronic kidney disease and Alzheimer's disease: an update [published online ahead of print, 2020 Apr 3]. Metab Brain Dis 35:883–894. https://doi.org/10.1007/s11011-020-00561-y
Zhang M, Mao Y, Ramirez SH et al (2010) Angiotensin II induced cerebral microvascular inflammation and increased blood-brain barrier permeability via oxidative stress. Neuroscience 171(3):852–858
Zhang Z, Sun L, Wang Y, Ning G, Minto AW, Kong J, Quigg RJ, Li YC (2008) Renoprotective role of the vitamin D receptor in diabetic nephropathy. Kidney Int 73(2):163–171
Zhang Z, Yuan W, Sun L, Szeto FL, Wong KE, Li X, Kong J, Li YC (2007) 1,25-Dihydroxyvitamin D3 targeting of NF-kappaB suppresses high glucose-induced MCP-1 expression in mesangial cells. Kidney Int 72(2):193–201
Author information
Authors and Affiliations
Contributions
All authors contributed to the elaboration of this manuscript. All authors have approved final article version.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to report.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Meléndez-Flores, J.D., Estrada-Bellmann, I. Linking chronic kidney disease and Parkinson’s disease: a literature review. Metab Brain Dis 36, 1–12 (2021). https://doi.org/10.1007/s11011-020-00623-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-020-00623-1