Abstract
It has been accepted that kidney function is connected with brain activity. In clinical studies, chronic kidney disease (CKD) patients have been found to be prone to suffering cognitive decline and Alzheimer’s disease (AD). The cognitive function of CKD patients may improve after kidney transplantation. All these indicators show a possible link between kidney function and dementia. However, little is known about the mechanism behind the relation of CKD and AD. This review discusses the associations between CKD and AD from the perspective of the pathophysiology of the kidney and complications and/or concomitants of CKD that may lead to cognitive decline in the progression of CKD and AD. Potential preventive and therapeutic strategies for AD are also presented. Further studies are warranted in order to confirm whether the setting of CKD is a possible new determinant for cognitive impairment in AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The kidneys and the brain are both exposed to a high volume of blood flow. As life expectancy extends, the incidence of chronic kidney disease (CKD) and Alzheimer’s disease (AD) increases with age.
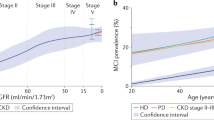
CKD is characterized by a reduced glomerular filtration rate (GFR) and by various complications including renal hypertension, renal anemia, and renal osteopathy. In China, the overall prevalence of CKD is 10.8%; the absolute number of patients with CKD is estimated to be about 119.5 million (Zhang et al. 2012). Most of the CKD cases are caused by lifestyle problems including hypertension, a high-salt diet, obesity, smoking, diabetes, binge drinking, and so forth. CKD is found to be associated with mental disorders (Zhang et al. 2017) and impaired cognitive performance (Van Sandwijk et al. 2015). The risk of cognitive damage is obviously higher in CKD patients than in non-CKD patients, as found in a systematic meta-analysis of 54,779 patients (Etgen et al. 2012). Another study showed that executive dysfunction is present in 5% of patients with moderate CKD, in 23% of patients with advanced CKD, and in up to 37% patients with ESRD (Kurella et al. 2014). Cognitive deficits in dialysis patients can be significantly improved or even reversed after successful kidney transplantation (Van Sandwijk et al. 2015). The improvement of cognitive performance is closely linked to graft function as well as to CKD stage. Additionally, abnormal amyloid β 42 expression and increased oxidative stress in plasma are found in CKD patients with cognitive dysfunction (Vinothkumar et al. 2017).
Alzheimer’s disease (AD)—a neurodegenerative disorder characterized by cognitive deterioration and memory loss—is the most common form of dementia. The morbidity of AD is so high that 24 million people worldwide suffered dementia in 2006, and the amount was expected to be 42 million by 2020 (Ferri et al. 2005). Similar to CKD, multiple risk factors—including hypertension, hypercholesterolemia, atherosclerosis, and diabetes mellitus—are related to AD. Lifestyle problems are participating in the disease process. A long-term high-glycemic diet has been linked to cerebral amyloid accumulation and cognitive deficits which may manifest before the onset of overt obesity or metabolic dysfunction (Hawkins et al. 2018; Taylor et al. 2017). Dysregulation in metabolic, inflammatory, and vascular factors that impact hippocampal function and prefrontal-mesolimbic reward pathways are potential mechanisms of the carbohydrate-cognition relationship. 24S-hydroxycholesterol—an oxidized product of cholesterol mainly synthesized in the brain—is higher in AD patients than in healthy control subjects (Lütjohann et al. 2000). Chronic consumption of a high-fat diet may result in beta-amyloid deposition (Lethem and Orrell 1997). Microbiota-gut-brain axis unbalance is part of a mechanistic link between the long-term consumption of a high-fat diet and the cognitive impairment of an individual (Proctor et al. 2017). Recently, Faraco et al. (2019) reported that excessive salt intake leads to cognitive impairment via a nitric oxide-tau phosphorylation pathway in mice. The nitric oxide deficiency in cerebral endothelial cells contributes to the hyperphosphorylation of tau by activating cyclin-dependent kinase. Salt-induced cognitive dysfunction can be retrieved after being treated with anti-tau antibodies. In addition, a dietary pattern that benefits for normal kidney function was inversely associated with cognitive deterioration in the elderly (Yin et al. 2019). These findings identify a causal link between dietary habits and cognition decline in CKD and AD. The avoidance of unbalanced dietary habits, and the maintenance of vascular health, may help to protect against some neurodegenerative pathologies in CKD and AD.
Alternatively, researchers have put forward a novel mechanism of renin-angiotensin system (RAS) disorders that may play roles in AD. Collectively, these factors contribute to the extracellular deposition of amyloid β (Aβ) with plaque development and intracellular aggregation of hyper-phosphorylated protein tau with tangle formation, which are the hallmarks of AD.
The pathogenesis of AD and the role of CKD in the progression of AD are not clear to date. As effective treatment of AD remains limited, studies aiming at prevention against significant, modifiable risk factors will matter a lot.
This review explained the fact that CKD promotes the development of cognitive decline and AD from the aspects of accumulation of uremic toxin; elevation of blood pressure; over-activation of RAS; lack of erythropoietin; disturbance of 1,25-dihydroxyvitamin D (1,25(OH)2D) production; and disordered expression of klotho gene. Last but not least, small vessel disease is discussed, as micro-vasculature dysfunction is a precipitating factor for both CKD and AD.
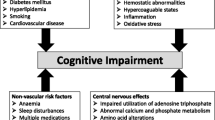
Mechanisms of cognitive impairment and AD related to CKD
Uremic toxins and AD
CKD leads to the accumulation of uremic toxins
Uremic toxins accumulate in CKD patients as a result of decreased GFR. In 2012, the European Uremic Toxin Work Group listed at least 88 uremic toxins (Duranton et al. 2012). Low renal perfusion and severely decreased GFR are the most common reasons for the accumulation of uremic toxins in CKD patients. Even in conventional hemodialysis patients, some uremic toxins are still insufficient to be removed due to their high protein-binding property, making them unable to pass across the dialysis membranes. The fierce competition among numerous toxins for the shared excretion pathway makes some of them unable to be secreted. Additionally, some uremic toxins are secondary to the impaired excretion and secretion function of the diseased kidney; e.g., parathyroid hormone (PTH).
Uremic toxins act as risk factors of cognition impairment
Among the uremic compounds, uric acid, PTH, and indoxyl sulfate (IS) are most likely to be involved in the cognitive decline of CKD patients.
Recently, several studies have suggested that hyperuricemia may act as an independent risk factor for brain atrophy and memory decline in CKD. High serum uric acid level was associated with impaired cognition and memory loss in the elderly population. Shao et al. (2016) demonstrated that high uric acid increased gliosis in the hippocampus of rats via triggering the expression of pro-inflammatory cytokines as well as the activation of the Toll-like receptor 4 (TLR4)/nuclear factor (NF)-κB pathway. Inhibition of the TLR4/NF-κB signaling pathway significantly ameliorated the uric acid-induced hippocampal inflammation and cognitive decline.
Given the ability of PTH to cross the blood brain barrier (BBB), and given that PTH receptors are widely distributed in the human brain, excess PTH is found to be associated with cognitive deterioration and dementia. Parathyroidectomy in CKD patients with secondary hyperparathyroidism can improve cognition function (Lourida et al. 2015). Several mechanisms are proposed to explain the possible links among PTH, cognitive decline, and dementia. First of all, PTH has a role in regulating intra- and extracellular calcium levels. It may induce cell apoptosis via calcium overloading. Vascular calcifications due to calcium deposition in the brain is related to dementia (Bonelli and Cummings 2008). PTH and serum vitamin D levels are linked through a feedback loop. A long-term vitamin D deficiency in CKD patients may induce secondary hyperparathyroidism, which is also connected with an increased risk of cognitive impairment and AD (Balion et al. 2012). Lastly, increased PTH concentration decreases local cerebral blood flow (Cermik et al. 2007), which may accelerate the process of AD.
Apart from uric acid and PTH, indoxyl sulfate (IS) may play a role in cognitive dysfunction. IS is protein-bound and not easily dialyzable. The plasma concentration of IS in hemodialysis patients is 20 to 80 times higher than in health controls. Due to a dysfunctional transport mechanism in CKD patients, IS is easily accumulated in the brain. IS conducts neurotoxic effects, mainly doing so via endothelial injury. IS stimulates vascular calcification and aging in hypertensive rats, which is an effect that is potential detrimental to patients with dementia (Toshimitsu 2012). IS induces inflammation by enhancing the interaction between leukocyte and endothelial cells (Ito et al. 2010), which is notable in the development of AD.
Hypertension and AD
Hypertension and CKD are serious global public health issues. They are closely associated with interrelated causes and relationships. Blood pressure typically elevates in patients with kidney function failure. In turn, a continuous rise in blood pressure accelerates the progression of kidney disease. Approximately 30% and 15% of adults have hypertension and CKD, respectively, in the US (Horowitz et al. 2015). In hemodialysis patients, the prevalence is much larger—over 70% patients have hypertension. Two types of renal hypertension—renoprival (excretory failure) and renovascular hypertension— are two of the most common complications of CKD.
Generally, the progress of renal hypertension of the two-kidney type is associated with three stages: (i) Vasoconstrictor effect from the over-activation of RAS;(ii)Excess volume load, attributable to impairment of the kidney’s ability to handle sodium; and (iii) Irreversible renal vascular stenosis and glomerular degeneration, resulting from structural deterioration of the kidney. In addition, excessive activation of the renal sympathetic nerve; hyperparathyroidism secondary to end-stage renal disease (ESRD); decreased inactivation of endothelium-derived contracting factors by injured kidney; and correction of renal anemia with EPO in dialysis patients have also been proven to induce the rise of blood pressure in patients with CKD.
Hypertension acts as a risk factor of AD
Blood pressure may elevate in AD decades before the onset of symptoms. Several long-term, population-based studies (Skoog et al. 1996; Kivipelto et al. 2001; Debette et al. 2011; Launer et al. 2000) have proven that hypertension increases the risk of AD (Table 1).
The mechanisms behind these associations are not explicit. Hypertension leads to hypo-perfusion, hypoxia, and ischemia—initiating vascular injuries via inflammation, endothelial dysfunction, vascular stiffness and calcifications, which may connect to the pathological process of AD. Vascular stiffness is engaged in CKD progression, and is closely associated with disturbances in cognitive functioning (Oh et al. 2016).
Additionally, hypertension-clustering vascular risk factors of obesity, diabetes mellitus, and hypercholesterolemia may induce cerebrovascular diseases leading to the development of AD. Recently, Carnevale et al. (2016) have identified that hypertension leads to Aβ accumulation and learning impairment by increasing the expression of the receptor of advanced glycated end products (RAGE). In addition, hypertension induces impairment in networks, or disequilibrium in AD brain connectivity (Son et al. 2015), thus suggesting a novel contribution of hypertension to the progression of AD.
Association between anti-hypertensive therapy and AD
As hypertension is a risk factor of AD, the practice of anti-hypertensive therapy is more than just cardiovascular protection. Experiments have shown that L-type voltage-sensitive Ca2+ channel blocker of S-312-d has positive effects on Aβ-induced cell death in the primary cultures of rat cortical neurons (Yagami et al. 2004). Isradipine is a potent calcium channel blocker targeting APP C-terminal fragment neurotoxicity in MC65 cells (Anekonda et al. 2011). Ca2+ channel blockers can also preserve synaptic deficits in the entorhinal-hippocampal network; this works against Aβ toxicity (Gholami Pourbadie et al. 2016). Additionally, some of the RAS inhibitors may also play a role in neuroprotection via its anti-hypertensive effects (which will be discussed latter in the part of the paper addressing RAS and AD).
Apart from cell and animal experiments, some of the randomized, placebo-controlled trials showed a reduced prevalence of dementia in patients treated with antihypertensive medications (Forette et al. 1998; Levi Marpillat et al. 2013); while others draw negative conclusions (Levi Marpillat et al. 2013). It is noteworthy that the sample size and the duration of observation may have significant impact on the results. Furthermore, some of the studies did not distinguish between vascular dementia and AD, which might also influence the final results. In a word, proper anti-hypertensive therapy may be beneficial to relieving cognition damage and AD progression in CKD.
RAS and AD
CKD acts as a key stimulator of the over-activation of RAS
RAS executes fundamental control over the water and sodium balance in the kidney. Renin, as a key rate-limiting enzyme for catalyzing angiotensinogen to angiotensin I, is secreted and released within the juxtaglomerular (JG) cells of the renal afferent arteriole at the entrance of the glomerular capillary network.
Renin secretion is modulated via multiple mechanisms, of which at least four regulatory pathways are undisputed: the macula densa, the renal baroreceptor, the renal nerves, and the effects of certain hormones and messengers. These factors eventually lead to an increase of the second messenger cyclic adenosine monophosphate(cAMP)in JG cells. In normal physiological conditions, high sodium chloride (NaCl) in the tubular fluid in the distal tubule induces afferent arteriolar vasoconstriction; and low tubular NaCl results in renin release, modulated by the JG apparatus. While in CKD, progressive tubular atrophy and interstitial fibrosis both lead to ischemia and low-perfusion pressure of the afferent arteriole, which contribute to a decreased concentration of NaCl in the tubular fluid, sensed by the macula densa via a Na:2Cl:K cotransporter mechanism, followed by the excessively release of renin. Sensed by the renal baroreceptor, decreased renal perfusion pressure and shear stress contribute to vasodilation and upregulation of cAMP followed by increased renin secretion.
Another typical manifestation of CKD is the chronic over-activation of the sympathetic nervous system (SNS), which derives from decreased NO bioavailability. Increased systemic catecholamines act on ß1-adrenergic receptors of the JG cells via the G protein-coupled transmembrane receptors—activating the adenylyl cyclase and phospholipases, and altering ion channels to reduce intracellular calcium with a cAMP-dependent signaling stimulating the exocytosis of renin. Additionally, GPR91—a recently classified succinate receptor, and one which is highly expressed in diabetic nephropathy—is associated with the activation of extracellular signal-regulated kinases 1/2 (ERK1/2), cyclooxygenase-2 (COX-2), and the synthesis of prostaglandin E2 (PGE2) to modulate the function of JG cells leading to renin release. Recently, calcium-calmodulin-mediated signals and synaptosome-associated protein (SNAP) have been proven to be involved in renin release.
In summary, multiple factors under the setting of CKD contribute to the excessive release of renin, leading to the over-activation of RAS (Fig. 1).
Mechanisms of the over-activation of RAS in CKD. Progressive tubular atrophy and interstitial fibrosis lead to ischemia and low perfusion pressure of the afferent arteriole, which together contribute to a decreased concentration of NaCl in the tubular fluid, as sensed by the JG cells, eventually leading to an increase of the second messenger cAMP and inducing the release of renin. The chronic over-activation of SNS in CKD—which acts on the ß1-adrenergic receptors of the JG cells with a cAMP dependent-signaling—stimulates the exocytosis of renin. Decreased renal perfusion pressure, via the renal baroreceptor mechanism, contributes to decreased shear stress followed by vasodilation and increased cAMP. Next, it increases renin secretion. GPR91 is associated with the activation of ERK1/2, COX-2, and PGE2—modulating the function of JG cells that induce the release of renin. CCMS and SNAP are also involved in renin production. Renin acts on Ang to release Ang I, and stimulates the activation of RAS. Abbreviations: ACE = Angiotensin converting enzyme; Ang = Angiotensin; cAMP=Cyclic adenosine monophosphate; CCMS=Calcium-calmodulin-mediated signals; CKD = Chronic kidney disease; COX = Cyclooxygenase-2; ERK1/2 = Extracellular signal–regulated kinases 1/2 (ERK1/2); JG = Juxtaglomerular; PGE2 = Prostaglandin E2; SNS=Sympathetic nervous system
The role of RAS and RAS inhibitors in AD
RAS is a crucial regulator of blood pressure; however, RAS plays a role in the progression of AD more than contributing to the formation of hypertension. Abundant studies have shown the relation between RAS activation and Aβ deposition (Fig. 2). In 2001, Bayer et al. (2001) reported that angiotensin-converting enzyme (ACE) had the effect of retarding Aβ aggregation and deposition in vitro by cleaving the Aβ sequence at the Asp7-Ser8 site. The effect was counteracted after the ACE inhibitor lisinopril was added. Similar results were obtained by Hemming and Selkoe (2005) via using cloned ACE from human neuroblastoma cells—proving that ACE was able to degrade Aβ plaques and that captopril suppressed it.
Potential interactions between RAS and Aß metabolism. ACE has retarding effects on Aβ aggregation and deposition and Ang II has inhibitory effects on Ach release (see the dotted line). Ang II/Ang receptor signal is able to induce APP cleavage and leads to NAPA processing (see the dotted line). Therefore, ACEI—by reducing the level of ACE and Ang II—generates both beneficial and negative effects for AD. ARB—by increasing Ang II and reducing Ang II/Ang receptor signals and HTN—also generates both beneficial and negative effects for AD. Abbreviations: Aβ = Amyloid β; ACE = Angiotensin-converting enzyme; ACEI = Angiotensin converting enzyme inhibitor; Ach = Acetylcholine; Ang = Angiotensin; APP = Amyloid precursor protein; ARB = Angiotensin II receptor blocker; HTN=Hypertension; NAPA = non-amyloidogenic pathway of APP
Additionally, angiotensin II might inhibit the release of acetylcholine (Ach). Ach is an important neurotransmitter participating in memory processing. Decreased Ach is found in the brain of AD patients. Angiotensin II/angiotensin receptor signal is able to induce amyloid precursor protein (APP) cleavage via G protein activation. Angiotensin II receptor blockers (ARBs) telmisartan can diminish this non-amyloidogenic pathway of APP processing (Kanarek et al. 2017). These studies have given new insight into the roles of RAS and RAS inhibitors in the treatment of AD.
However, in other studies (Hemming et al. 2007; Wang et al. 2007; Ferrington et al. 2011; Kurata et al. 2014), the role of RAS inhibitors in AD was found to be diverse and controversial in animal models (Table 2). Valsartan and telmisartan were associated with reduced Aβ accumulation and improved cognitive function in rodents (Wang et al. 2007; Kurata et al. 2014). Based on previous studies, Yang et al. (2014) reported that valsartan prevented aluminum trichloride- and d-galactose-induced cognitive decline, partly through an upregulation of Ach and an attenuation of oxidative stress. However, in ACE knockout mice (Eckman et al. 2006) and in APP transgenic mice (Hemming et al. 2007) treated with perindopril and captopril, respectively, the Aβ level altered little. Similar results were obtained in a triple transgenic mouse model of AD with ACE inhibitor (captopril) and ARBs (eprosartan and valsartan) (Ferrington et al. 2011).
These findings provide new evidence for the prevention and treatment of AD. ACE inhibitors lead to both beneficial and negative effects for the progression of AD by reducing both ACE and angiotensin II. Such an explanation also provides clues as to why the effects of ARBs can be varied (Fig. 2). It is especially noteworthy that some of these data were derived from animal experiments that might be inapplicable to their human-equivalent diseases. In a word, different ACE inhibitors and ARBs may have different effects on AD progression. It is requisite to conduct further studies focusing on these issues.
Erythropoietin and AD
Kidney injury acts as a major contributor to impaired erythropoietin (EPO) secretion
EPO is a glycoprotein hormone primarily secreted by the kidney in adults, acting to stimulate the proliferation and differentiation of erythroid stem cells and to maintain normal hemoglobin concentrations. EPO secretion depends on kidney oxygen tension (Dimke et al. 2015). Tubular-interstitial fibrosis in CKD leads to the loss of EPO secretion. Activation of transforming growth factor β-Smad signaling—a major pathway leading to renal fibrosis—is found to impair EPO synthesis (Lan 2011). Unbalanced microenvironments in injured kidneys, such as uremic toxins, suppress EPO secretion via a hypoxia-inducible, transcription-factor-α-dependent channel (Chiang et al. 2011) and NG-monomethyl-L-arginine (L-NMMA)-GATA2 signaling (Tarumoto et al. 2000). In addition, lipid deposition and deranged fatty acid metabolism may be involved in EPO gene regulation in kidneys (Kang et al. 2015).
Collectively, these results elaborate the mechanisms of the downregulated synthesis and release of EPO in an injured kidney.
The role of EPO/EPO receptor in the progression of AD
EPO is widely used in ESRD patients targeting renal anemia. EPO and EPO receptors (EPORs) have been proven to present in the human brain and to play significant roles in the nervous system. EPO/EPOR signaling is essential to normal brain development; as well as being essential to rescuing neurons from apoptosis, oxidative stress, glutamate excitotoxicity, and inflammation (Kawakami et al. 2001; Wu et al. 2007). EPO binding to EPORs leads to the activation of Janus kinase 2-phosphatidylinositol 3-phosphate signaling (Ruscher et al. 2002), and phosphoinositide 3-kinase-protein kinase B (PI3K-PKB)-dependent mechanism in the hippocampal neurons (Sirén et al. 2001), both of which mediate neuroprotection against neuronal death. EPO decreased the mRNA level of tumor necrosis factor ɑ, Fas and Fas ligand, as well as the activities of caspase-3, 8, and 9 (Lee et al. 2006). EPO had a protective effect of reducing oxidative stress and Tau phosphorylation induced by Aβ and improving memory function by diminishing endothelial dysfunction on cellular level (Lee et al. 2012). EPO prevented Aβ accumulation-induced learning deficits by alleviating lipid peroxidation in the hippocampus in animal experiments (Maurice et al. 2013). EPO has also been proven to decrease the cerebral excitatory neurotransmitter release and to protect synaptic plasticity from toxic levels of glutamate in the hippocampus (Maurice et al. 2013). EPO exerted anti-inflammatory effects via mechanisms associating with microglial activation, phosphatidylserine exposure, and PKB activity or by suppressing several pro-inflammatory cytokines including interleukin-6, tumor necrosis factor and monocyte chemoattractant protein-1 (Chong et al. 2004). In addition, EPO can reduce levels of RAGE which participates in Aβ production and deposition in the brain and in synaptic dysfunction; it helps to decrease the accumulation of Aβ (Lee et al. 2012). All these evidence suggest that EPO may be neuroprotective in AD.
EPO supplement improves cognition in AD
As EPO is important in neuroprotection, EPO supplement in CKD may be beneficial for cognition improvement and for decreasing the incidence of AD. The systemic administration of EPO has proven to be capable of crossing the BBB; and it takes effect in the cerebrospinal fluid of rodents and humans (Statler et al. 2007). The experimental injection of EPO can improve the long-term memory of mice (Adamcio et al. 2008). Weekly EPO therapy improves cognitive functions and slows down the progressive atrophy of brain in schizophrenia for as little as 3 months (Wüstenberg et al. 2011). The systematic administration of EPO biweekly for 6 weeks resulted in a significant improvement of cognition as detected by the electro-neurophysiological method in 15 anemic predialysis and 15 anemic dialysis patients (Singh et al. 2006). Recombinant human EPO therapy has an effective neuroprotective impact on platelet GSK3β, p-Tau 181, amyloid precursor protein, and neuropsychological assessment scores in CKD patients with cognitive dysfunction (Vinothkumar et al. 2019; Vinothkumar et al. 2018).
EPO presents neuroprotection via multiple mechanisms in AD. EPO treatment can upregulate the level of dopamine receptors 1 and 2, which play roles in synaptic plasticity via modulating the calcium/calmodulin-dependent protein kinase II (CaMKII) in striatum (Armand-Ugón et al. 2014). EPO administration enhanced the Janus kinase 2-phosphorylated signal transducers and activators of transcription 5 (STAT5), followed by the increase of the downstream gene products Bcl-xL and the X-linked inhibitor of apoptosis protein, initiating a pro-survival signaling cascade (Zhang et al. 2007). In addition, it was reported that EPO was a local messenger which was against ischemia secreted by the astrocytes (Ruscher et al. 2002).
1,25(OH)2D and AD
1,25(OH)2D insufficiency is common in CKD
1,25(OH)2D is an active form of vitamin D. It is predominantly produced by the kidneys. Parenchymal damage and mass loss of the kidneys decrease the secretion of 1,25(OH)2D. CKD leads to down-regulation of 1ɑ-hydroxylase, which limits the ability of the kidneys to produce 1,25(OH)2D. Loss of vitamin D binding protein in urine contributes to an impairment in the accumulation of vitamin D in the body. Uremic toxins may interfere with the generation and activation of vitamin D through interfering with the vitamin D receptor (as indicated by in vitro study). Moreover, phosphate retention may inhibit the activation of 1ɑ-hydroxylase. Accumulation of fibroblast growth factor 23 (FGF23) in CKD has also been shown to be involved in decreasing the production of calcitriol. These observations indicate that CKD is a predominant risk factor for reduced 1,25(OH)2D production.
Lack of 1,25(OH)2D is a risk factor for AD
Low serum 1,25(OH)2D concentration is associated with cognitive impairment. A previous study reported impaired acquisition of the spatial navigation task in a water maze test in 1,25(OH)2D-insufficient rats (Mohamed et al. 2014). Decreased serum 25(OH)D concentrations were found in 20 mild dementia cases as compared with 40 normal controls (Kipen et al. 1995), and in 100 AD cases as compared with 100 controls (Sato et al. 2005), respectively. Studies indicated a positive association between serum 25(OH)D and cognitive levels in a population-based study with 1766 participants (Llewellyn et al. 2009). Similarly, it was found that higher levels of active vitamin D were associated with better cognitive performance in AD patients (Oudshoorn et al. 2008; Annweiler et al. 2012). Dietary intake of vitamin D could delay the onset of dementia in elderly women, as indicated by a 7-year follow-up study (Annweiler et al. 2012). Recently, the data have been explicit that 1,25(OH)2D receptors exist in the cortex and hippocampus (Mccann and Ames 2008). A significant reduction of nuclear vitamin D receptors was found during the development of AD. These findings suggest the importance of 1,25(OH)2D in cognition among people with AD.
Some relatively small studies reported no associations between 1,25(OH)2D level and cognition impairment or dementia (Jorde et al. 2006; Mcgrath et al. 2007). However, none of these studies had been population-based or had been adjusted for confounding factors; and standardized neurocognitive screening tests had not been applied.
Taking these results together, it seems that having a deficiency of 1,25(OH)2D somewhat contributes to the process of dementia.
1,25(OH)2D supplementation is neuroprotective in AD
As a lack of 1,25(OH)2D is detrimental for AD, 1,25(OH)2D supplementation may be neuroprotective. Mohamed et al. (2014) found that in rats with AD, the prophylactic use of 1,25(OH)2D was associated with better performance in the water maze test, decreased Aß deposition, and a significant increase of brain-derived neurotrophic factors (BDNF) and antioxidants in the hippocampus. Similarly, Yu et al. (2011) reported a correlation between vitamin D supplement and decreased Aß deposition and inflammation in AβPP transgenic mice. Additionally, long-term administration of active vitamin D in rats delayed the degenerative processes in the hippocampus during aging (Kalueff et al. 2004).
Serum 1,25(OH)2D may play important roles in anti-oxidation, anti-inflammation, neurotrophin production, and the elimination of Aß out of the brain. Vitamin D helps reduce reactive oxygen and nitrogen species in various models of brain oxidative stress. 1,25(OH)2D has the effect of up-regulating the activity and expression of brain γ-glutamyl transpeptidase in order to increase the level of brain glutathione, an important antioxidant (Garcion et al. 2002). Calcitriol, one of the active metabolites of 1,25(OH)2D, can increase the level of glutathione via inhibiting the production of nitric oxide synthase and reducing cellular calcium (Ibi et al. 2001). The imbalance of oxidation and the anti-oxidation system caused by the 1,25(OH)2D shortage is considered as being a trigger in mitochondrial dysfunction and apoptosis in neurodegeneration as well as in AD. In addition, vitamin D could control the pro-inflammatory state and increase the activity of the Aß degrading enzyme (in rats) with regard to age-related cognitive decline (Briones and Darwish 2012). Furthermore, vitamin D could modulate the function of the immune system by stimulating phagocytosis and clearance of Aß against cell apoptosis (Masoumi et al. 2009). In vitro, calcitriol is found to regulate the synthesis of neurotrophic factors including nerve growth factor, neurotrophin, and nerve growth factor as well as neurotrophin receptor in brain neurons, glial cells, and schwann cells (Kalueff et al. 2004). It was shown that 1,25(OH)2D could help enhance the clearance of intracephalic Aß out of the BBB in mice (Ito et al. 2011). Vitamin D was proven to down-regulate the expression of inducible nitric oxide synthase (iNOS), which played a role in Aß deposition in AD (Garcion et al. 1997).
Considering these results, the dietary supplementation of 1,25(OH)2D or its analogues for AD prevention and therapy is possible.
Klotho gene and AD
The disordered expression of klotho caused by CKD
Klotho is a novel anti-aging gene predominantly expressed in the kidneys. The loss of renal mass in CKD decreases klotho expression. Studies have suggested that klotho expression was significantly inhibited in renal ischemia-reperfusion injury and angiotensin II-induced renal damage (Sugiura et al. 2012). In turn, the downregulation of klotho mRNA and protein, in a cultured cell line, may accelerate renal damage resulting from increased oxidative stress (Yamamoto et al. 2005), which may further aggravate the impaired expression of klotho in the kidneys. Additionally, the increased tumor necrosis factor and interferon-γ in CKD can reduce renal klotho expression. It is known that having low levels of calcitriol, due to the loss of 1ɑ-hydroxylase in CKD, increases renal renin production. Activation of the RAS, in turn, reduces the renal expression of klotho followed by high levels of FGF-23 or FGF-23 resistance. A high level of FGF-23 also leads to the reduced secretion of 1,25(OH)2-vitamin D, which creates a vicious circle (Fig. 3).
Cross-talk between vitamin D, RAS and FGF 23-klotho in CKD patients. The activity of 1ɑ-HOase is reduced due to nephron loss and high FGF 23 (see the dotted line), leading to reduced secretion of 1,25(OH)2 D—which, in turn, upregulates renal renin production (see the dotted line). The subsequently higher levels of Ang II cause renal klotho loss (see the dotted line) and impair phosphaturia, raising FGF 23 levels. RAS activation, vitamin D deficiency, high FGF 23 levels, and low renal klotho have all been associated with adverse renal outcomes in CKD. Abbreviations: ACE = Angiotensin converting enzyme; Ang = Angiotensin; 1ɑ-HOase = 1ɑ-hydroxylase; 1,25(OH)2D = 1,25-dihydroxyvitamin D; FGF 23 = Fibroblast growth factor 23
Klotho plays a significant role in AD
As aging is the greatest risk factor for AD, klotho—a putative aging-suppressor gene—may act as a neuroprotective factor by anti-senescence and modulating oxidative stress in the process of AD. The extracellular domain of klotho is secreted into the blood and cerebrospinal fluid and potentially acts as an age-defying factor. Klotho mutation causes impaired cognition, systemic aging, lessened longevity in mice (Shiozaki et al. 2008), and senile changes in the white matter of rhesus monkeys (Duce et al. 2008). The downregulation of klotho mRNA levels and protein expression was correlated with brain senility, AD-associated Aß production, neuron loss, and memory decline in elderly SAMP8 mice (Kuang et al. 2014). Recently, klotho has been reported to conduct neuroprotective effects via the induction of oxidative stress tolerance against cognitive damage in AD (Adeli et al. 2017). Prior to the onset of cognitive impairment, oxidative DNA damage and lipid peroxidation increased in the hippocampus in klotho mutant mice (Nagai et al. 2003). Other anti-aging effects of klotho includes suppression of growth factor signaling; the regulation of several ion channels and transporters.
Other factors
Small vessel disease in CKD and AD
The kidney and brain are similar anatomically and functionally in terms of the regulation of the micro-vasculatures. Both of the two organs share unique susceptibilities to small vessel injury, because both of them have short, small strain vessels directly arising from high-pressure arteries. Severe hypertension damage can occur in such vessels.
In adults with CKD, retinal microvascular abnormality is associated with poor performance in several cognitive domains, including executive function and attention (Yaffe et al. 2013). Pirici et al. (2017) utilized 80 hypertensive-stroke-prone rats at various ages (12 to 44 weeks); and they quantified tubulointerstitial renal damage, the prevalence of cerebral microhemorrhages, and Aβ accumulations. Finally, they found an association between vascular pathology and Aβ deposition in CKD. Chronic kidney disease affects cognitive damage and AD, partly through the high prevalence of small vessel diseases in the brain.
Concluding remarks
At present, the data available support the idea that there is a high possibility of cognitive impairment or AD-like dementia in CKD patients. The settings of CKD (which is mainly characterized by the accumulation of uremic toxins, renal hypertension, excessively activated RAS, renal anemia, renal osteopathy, and the impaired expression of klotho) caused by renal dysfunction are reasonable mechanisms of CKD promotion of the progression of AD. Additionally, small vessel injury may play a non-negligible role in contributing to cognition impairment in both CKD and AD. These discoveries highlight a novel point of view for the diagnosis and potential treatment of CKD and AD. If we focus on changes in the kidneys and the brain in further studies, we may find more significant results in the prevention and treatment for both CKD and AD.
References
Adamcio B, Sargin D, Stradomska A, Medrihan L, Gertler C, Theis F, Zhang M, Müller M, Hassouna I, Hannke K, Sperling S, Radyushkin K, El-Kordi A, Schulze L, Ronnenberg A, Wolf F, Brose N, Rhee JS, Zhang W, Ehrenreich H (2008) Erythropoietin enhances hippocampal long-term potentiation and memory. BMC Biol 6:37
Adeli S, Zahmatkesh M, Tavoosidana G, Karimian M, Hassanzadeh G (2017) Simvastatin enhances the hippocampal klotho in a rat model of streptozotocin-induced cognitive decline. Prog Neuro-Psychopharmacol Biol Psychiatry 72:87–94
Anekonda TS, Quinn JF, Harris C, Frahler K, Wadsworth TL, Woltjer RL (2011) L-type voltage-gated calcium channel blockade with isradipine as a therapeutic strategy for Alzheimer's disease. Neurobiol Dis 41(1):62–70
Annweiler C, Rolland Y, Schott AM, Blain H, Vellas B, Herrmann FR, Beauchet O (2012) Higher vitamin D dietary intake is associated with lower risk of Alzheimer's disease: a 7-year follow-up. J Gerontol A Biol Sci Med Sci 67(11):1205–1211
Armand-Ugón M, Aso E, Moreno J, Riera-Codina M, Sánchez A, Vegas E, Ferrer I (2014) Memory improvement in the AβPP/PS1 mouse model of familial Alzheimer's disease induced by carbamylated-erythropoietin is accompanied by modulation of synaptic genes. J Alzheimers Dis 45(2):407–421
Balion C, Griffith LE, Strifler L, Henderson M, Patterson C, Heckman G, Llewellyn DJ, Raina P (2012) Vitamin D, cognition, and dementia: a systematic review and meta-analysis. Neurology 79(13):1397–1405
Bayer TA, Wirths O, Majtényi K, Hartmann T, Multhaup G, Beyreuther K, Czech C (2001) Key factors in Alzheimer's disease: beta-amyloid precursor protein processing, metabolism and intraneuronal transport. Brain Pathol 11(1):1–11
Bonelli RM, Cummings JL (2008) Frontal-subcortical dementias. Neurologist 14(2):100–107
Briones TL, Darwish H (2012) Vitamin D mitigates age-related cognitive decline through the modulation of pro-inflammatory state and decrease in amyloid burden. J Neuroinflammation 9:244
Carnevale D, Perrotta M, Lembo G, Trimarco B (2016) Pathophysiological links among hypertension and Alzheimer’s disease. High Blood Press Cardiovasc Prev 23(1):3–7
Cermik TF, Kaya M, Uğur-Altun B, Bedel D, Berkarda S, Yiğitbaşi ON (2007) Regional cerebral blood flow abnormalities in patients with primary hyperparathyroidism. Neuroradiology 49(4):379–385
Chiang CK, Tanaka T, Inagi R, Fujita T, Nangaku M (2011) Indoxyl sulfate, a representative uremic toxin, suppresses erythropoietin production in a HIF-dependent manner. Lab Investig 91(11):1564–1571
Chong ZZ, Kang JQ, Maiese K (2004) AKT1 drives endothelial cell membrane asymmetry and microglial activation through Bcl-xL and caspase 1, 3, and 9. Exp Cell Res 296(2):196–207
Debette S, Seshadri S, Beiser A, Au R, Himali JJ, Palumbo C, Wolf PA, DeCarli C (2011) Midlife vascular risk factor exposure accelerates structural brain aging and cognitive decline. Neurology 77(5):461–468
Dimke H, Sparks MA, Thomson BR, Frische S, Coffman TM, Quaggin SE (2015) Tubulovascular cross-talk by vascular endothelial growth factor a maintains peritubular microvasculature in kidney. J Am Soc Nephrol 26(5):1027–1038
Duce JA, Podvin S, Hollander W, Kipling D, Rosene DL, Abraham CR (2008) Gene profile analysis implicates klotho as an important contributor to aging changes in brain white matter of the rhesus monkey. Glia 56(1):106–117
Duranton F, Cohen G, De Smet R, Rodriguez M, Jankowski J, Vanholder R, Argiles A, European Uremic Toxin Work Group (2012) Normal and pathologic concentrations of uremic toxins. J Am Soc Nephrol 23(7):1258–1270
Eckman EA, Adams SK, Troendle FJ, Stodola BA, Kahn MA, Fauq AH, Xiao HD, Bernstein KE, Eckman CB (2006) Regulation of steady-state beta-amyloid levels in the brain by neprilysin and endothelin-converting enzyme but not angiotensin-converting enzyme. J Biol Chem 281(41):30471–30478
Etgen T, Chonchol M, Forstl H, Sander D (2012) Chronic kidney disease and cognitive impairment: a systematic review and meta-analysis. Am J Nephrol 35(5):474–482
Faraco G, Hochrainer K, Segarra SG, Schaeffer S, Santisteban MM, Menon A, Jiang H, Holtzman DM, Anrather J, Iadecola C (2019) Dietary salt promotes cognitive impairment through tau phosphorylation. Nature 574(7780):686–690
Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, Hall K, Hasegawa K, Hendrie H, Huang Y, Jorm A, Mathers C, Menezes PR, Rimmer E, Scazufca M, Alzheimer's Disease International (2005) Global prevalence of dementia: a Delphi consensus study. Lancet 366(9503):2112–2117
Ferrington L, Miners JS, Palmer LE, Bond SM, Povey JE, Kelly PA, Love S, Horsburgh KJ, Kehoe PG (2011) Angiotensin II-inhibiting drugs have no effect on intraneuronal Aβ or oligomeric Aβ levels in a triple transgenic mouse model of Alzheimer's disease. Am J Transl Res 3(2):197–208
Forette FO, Seux ML, Staessen JA, Thijs L, Birkenhäger WH, Babarskiene MR, Babeanu S, Bossini A, Gil-Extremera B, Girerd X, Laks T, Lilov E, Moisseyev V, Tuomilehto J, Vanhanen H, Webster J, Yodfat Y, Fagard R (1998) Prevention of dementia in randomised double-blind placebo-controlled systolic hypertension in Europe (Syst-Eur) trial. Lancet 352(9137):1347–1351
Garcion E, Nataf S, Berod A, Darcy F, Brachet P (1997) 1,25-Dihydroxyvitamin D-3 inhibits the expression of inducible nitric oxide synthase in rat central nervous system during experimental allergic encephalomyelitis. Brain Res Mol Brain Res 45(2):255–267
Garcion E, Wion-Barbot N, Montero-Menei CN, Berger F, Wion D (2002) New clues about vitamin D functions in the nervous system. Trends Endocrinol Metab 13(3):100–105
Gholami Pourbadie H, Naderi N, Janahmadi M, Mehranfard N, Motamedi F (2016) Calcium channel blockade attenuates abnormal synaptic transmission in the dentate gyrus elicited by entorhinal amyloidopathy. Synapse 70(10):408–417
Hawkins MAW, Keirns NG, Helms Z (2018) Carbohydrates and cognitive function. Curr Opin Clin Nutr Metab Care 21(4):302–330
Hemming ML, Selkoe DJ (2005) Amyloid beta-protein is degraded by cellular angiotensin-converting enzyme (ACE) and elevated by an ACE inhibitor. J Biol Chem 280(45):37644–37650
Hemming ML, Selkoe DJ, Farris W (2007) Effects of prolonged angiotensin-converting enzyme inhibitor treatment on amyloid beta-protein metabolism in mouse models of Alzheimer disease. Neurobiol Dis 26(1):273–281
Horowitz B, Miskulin D, Zager P (2015) Epidemiology of hypertension in CKD. Adv Chronic Kidney Dis 22(2):88–95
Ibi M, Sawada H, Nakanishi M, Kume T, Katsuki H, Kaneko S, Shimohama S, Akaike A (2001) Protective effects of 1α,25-(OH)2D3 against the neurotoxicity of glutamate and reactive oxygen species in mesencephalic culture. Neuropharmacology 40(6):761–771
Ito S, Osaka M, Higuchi Y, Nishijima F, Ishii H, Yoshida M (2010) Indoxyl sulfate induces leukocyte-endothelial interactions through up-regulation of e-selectin. J Biol Chem 285(50):38869–38875
Ito S, Ohtsuki S, Nezu Y, Koitabashi Y, Murata S, Terasaki T (2011) 1α,25-Dihydroxyvitamin D3 enhances cerebral clearance of human amyloid-β peptide(1-40) from mouse brain across the blood-brain barrier. Fluids Barriers CNS 8:20
Jorde R, Waterloo K, Saleh F, Haug E, Svartberg J (2006) Neuropsychological function in relation to serum parathyroid hormone and serum 25-hydroxyvitamin D levels. J Neurol 253(4):464–470
Kalueff AV, Eremin KO, Tuohimaa P (2004) Mechanisms of neuroprotective action of vitamin D(3). Biochemistry 69(7):738–741
Kanarek AM, Wagner A, Küppers J, Gütschow M, Postina R, Kojro E (2017) Crosstalk between angiotensin and the non-amyloidogenic pathway of Alzheimer's amyloid precursor protein. FEBS J 284(5):742–753
Kang HM, Ahn SH, Choi P, Ko YA, Han SH, Chinga F, Park AS, Tao J, Sharma K, Pullman J, Bottinger EP, Goldberg IJ, Susztak K (2015) Defective fatty acid oxidation in renal tubular epithelial cells has a key role in kidney fibrosis development. Nat Med 21(1):37–46
Kawakami M, Sekiguchi M, Sato K, Kozaki S, Takahashi M (2001) Erythropoietin receptor-mediated inhibition of exocytotic glutamate release confers neuroprotection during chemical ischemia. J Biol Chem 276(42):39469–39475
Kipen E, Helme RD, Wark JD, Flicker L (1995) Bone density, vitamin D nutrition, and parathyroid hormone levels in women with dementia. J Am Geriatr Soc 43(10):1088–1091
Kivipelto M, Helkala EL, Laakso MP, Hänninen T, Hallikainen M, Alhainen K, Soininen H, Tuomilehto J, Nissinen A (2001) Midlife vascular risk factors and Alzheimer’s disease in later life: longitudinal, population based study. BMJ 322(7300):1447–1451
Kuang X, Chen YS, Wang LF, Li YJ, Liu K, Zhang MX, Li LJ, Chen C, He Q, Wang Y, Du JR (2014) Klotho upregulation contributes to the neuroprotection of ligustilide in an Alzheimer's disease mouse model. Neurobiol Aging 35(1):169–178
Kurata T, Lukic V, Kozuki M, Wada D, Miyazaki K, Morimoto N, Ohta Y, Deguchi K, Ikeda Y, Kamiya T, Abe K (2014) Telmisartan reduces progressive accumulation of cellular amyloid beta and phosphorylated tau with inflammatory responses in aged spontaneously hypertensive stroke resistant rat. J Stroke Cerebrovasc Dis 23(10):2580–2590
Kurella M, Chertow GM, Luan J, Yaffe K (2014) Cognitive impairment in chronic kidney disease. J Am Geriatr Soc 52(11):1863–1869
Lan HY (2011) Diverse roles of TGF-β/Smads in renal fibrosis and inflammation. Int J Biol Sci 7(7):1056–1067
Launer LJ, Ross GW, Petrovitch H, Masaki K, Foley D, White LR, Havlik RJ (2000) Midlife blood pressure and dementia: the Honolulu-Asia aging study. Neurobiol Aging 21(1):49–55
Lee ST, Chu K, Sinn DI, Jung KH, Kim EH, Kim SJ, Kim JM, Ko SY, Kim M, Roh JK (2006) Erythropoietin reduces perihematomal inflammation and cell death with eNOS and STAT3 activations in experimental intracerebral hemorrhage. J Neurochem 96(6):1728–1739
Lee ST, Chu K, Park JE, Jung KH, Jeon D, Lim JY, Lee SK, Kim M, Roh JK (2012) Erythropoietin improves memory function with reducing endothelial dysfunction and amyloid-beta burden in Alzheimer’s disease models. J Neurochem 120(1):115–124
Lethem R, Orrell M (1997) Antioxidants and dementia. Lancet 349(9060):1189–1190
Levi Marpillat N, Macquin-Mavier I, Tropeano AI, Bachoud-Levi AC, Maison P (2013) Antihypertensive classes, cognitive decline and incidence of dementia: a network meta-analysis. J Hypertens 31(6):1073–1082
Llewellyn DJ, Langa KM, Lang IA (2009) Serum 25-hydroxyvitamin D concentration and cognitive impairment. J Geriatr Psychiatry Neurol 22(3):188–195
Lourida I, Thompson-Coon J, Dickens CM, Soni M, Kuźma E, Kos K, Llewellyn DJ (2015) Parathyroid hormone, cognitive function and dementia: a systematic review. PLoS One 10(5):e0127574
Lütjohann D, Papassotiropoulos A, Björkhem I, Locatelli S, Bagli M, Oehring RD, Schlegel U, Jessen F, Rao ML, von Bergmann K, Heur R (2000) Plasma 24S-hydroxycholesterol (cerebrosterol) is increased in Alzheimer and vascular demented patients. J Lipid Res 41(2):195–198
Masoumi A, Goldenson B, Ghirmai S, Avagyan H, Zaghi J, Abel K, Zheng X, Espinosa-Jeffrey A, Mahanian M, Liu PT, Hewison M, Mizwickie M, Cashman J, Fiala M (2009) 1alpha,25-dihydroxyvitamin D3 interacts with curcuminoids to stimulate amyloid-beta clearance by macrophages of Alzheimer's disease patients. J Alzheimers Dis 17(3):703–717
Maurice T, Mustafa MH, Desrumaux C, Keller E, Naert G, de la C García-Barceló M, Rodríguez Cruz Y, Garcia Rodríguez JC (2013) Intranasal formulation of erythropoietin (EPO) showed potent protective activity against amyloid toxicity in the Aβ25-35 non-transgenic mouse model of Alzheimer’s disease. J Psychopharmacol 27(11):1044–1057
Mccann JC, Ames BN (2008) Is there convincing biological or behavioral evidence linking vitamin D deficiency to brain dysfunction? FASEB J 22(4):982–1001
Mcgrath J, Scragg R, Chant D, Eyles D, Burne T, Obradovic D (2007) No association between serum 25-hydroxyvitamin D3 level and performance on psychometric tests in NHANES III. Neuroepidemiology 29(1–2):49–54
Mohamed AR, Soliman GY, Ismail CA, Mannaa HF (2014) Neuroprotective role of vitamin D3 in colchicine-induced Alzheimer’s disease in rats. Alexandr J Med 51:127–136
Nagai T, Yamada K, Kim HC, Kim YS, Noda Y, Imura A, Nabeshima Y, Nabeshima T (2003) Cognition impairment in the genetic model of aging klotho gene mutant mice: a role of oxidative stress. FASEB J 17(1):50–52
Oh YS, Kim JS, Park JW, An JY, Park SK, Shim YS, Yang DW, Lee KS (2016) Arterial stiffness and impaired renal function in patients with Alzheimer’s disease. Neurol Sci 37(3):451–457
Oudshoorn C, Mattace-Raso FU, van der Velde N, Colin EM, van der Cammen TJ (2008) Higher serum vitamin D3 levels are associated with better cognitive test performance in patients with Alzheimer's disease. Dement Geriatr Cogn Disord 25(6):539–543
Pirici D, Stanaszek L, Garz C, Niklass S, Heinze HJ, Kalinski T, Attems J, Schreiber S (2017) Common impact of chronic kidney disease and brain microhemorrhages on cerebral Aβ pathology in SHRSP. Brain Pathol 27(2):169–180
Proctor C, Thiennimitr P, Chattipakorn N, Chattipakorn SC (2017) Diet, gut microbiota and cognition. Metab Brain Dis 32(1):1–17
Ruscher K, Freyer D, Karsch M, Isaev N, Megow D, Sawitzki B, Priller J, Dirnagl U, Meisel A (2002) Erythropoietin is a paracrine mediator of ischemic tolerance in the brain: evidence from an in vitro model. J Neurosci 22(23):10291–10301
Sato Y, Honda Y, Hayashida N, Iwamoto J, Kanoko T, Satoh K (2005) Vitamin K deficiency and osteopenia in elderly women with Alzheimer's disease. Arch Phys Med Rehabil 86(3):576–581
Shao X, Lu W, Gao F, Li D, Hu J, Li Y, Zuo Z, Jie H, Zhao Y, Cen X (2016) Uric acid induces cognitive dysfunction through hippocampal inflammation in rodents and humans. J Neurosci 36(43):10990–11005
Shiozaki M, Yoshimura K, Shibata M, Koike M, Matsuura N, Uchiyama Y, Gotow T (2008) Morphological and biochemical signs of age-related neurodegenerative changes in klotho mutant mice. Neuroscience 152(4):924–941
Singh NP, Sahni V, Wadhwa A, Garg S, Bajaj SK, Kohli R, Agarwal SK (2006) Effect of improvement in anemia on electroneurophysiological markers (P300) of cognitive dysfunction in chronic kidney disease. Hemodial Int 10(3):267–273
Sirén AL, Fratelli M, Brines M, Goemans C, Casagrande S, Lewczuk P, Keenan S, Gleiter C, Pasquali C, Capobianco A, Mennini T, Heumann R, Cerami A, Ehrenreich H, Ghezzi P (2001) Erythropoietin prevents neuronal apoptosis after cerebral ischemia and metabolic stress. Proc Natl Acad Sci U S A 98(7):4044–4049
Skoog I, Lernfelt B, Landahl S, Palmertz B, Andreasson LA, Nilsson L, Persson G, Odén A, Svanborg A (1996) 15-year longitudinal study of blood pressure and dementia. Lancet 347(9009):1141–1145
Son SJ, Kim J, Lee E, Park JY, Namkoong K, Hong CH, Ku J, Kim E, Oh BH (2015) Effect of hypertension on the resting-state functional connectivity in patients with Alzheimer's disease (AD). Arch Gerontol Geriatr 60(1):210–216
Statler PA, Mcpherson RJ, Bauer LA, Kellert BA, Juul SE (2007) Pharmacokinetics of high-dose recombinant erythropoietin in plasma and brain of neonatal rats. Pediatr Res 61(6):671–675
Sugiura H, Yoshida T, Shiohira S, Kohei J, Mitobe M, Kurosu H, Kuro-o M, Nitta K, Tsuchiya K (2012) Reduced klotho expression level in kidney aggravates renal interstitial fibrosis. Am J Physiol Ren Physiol 302(10):F1252–F1264
Tarumoto T, Imagawa S, Ohmine K, Nagai T, Higuchi M, Imai N, Suzuki N, Yamamoto M, Ozawa K (2000) N(G)-monomethyl-L-arginine inhibits erythropoietin gene expression by stimulating GATA-2. Blood 96(5):1716–1722
Taylor MK, Sullivan DK, Swerdlow RH, Vidoni ED, Morris JK, Mahnken JD, Burns JM (2017) A high-glycemic diet is associated with cerebral amyloid burden in cognitively normal older adults. Am J Clin Nutr 106(6):1463–1470
Toshimitsu N (2012) Lindoxyl sulfate, a tryptophan metabolite, induces nephro-vascular toxicity. Biotechnol Biotechnol Equip 26(sup1):129–133
Van Sandwijk MS, Ten Berge IJ, Majoie CB, Caan MW, De Sonneville LM, Van Gool WA, Bemelman FJ (2015) Cognitive changes in chronic kidney disease and after transplantation. Transplantation 100(4):734–742
Vinothkumar G, Kedharnath C, Krishnakumar S, Sreedhar S, Preethikrishnan K, Dinesh S, Sundaram A, Balakrishnan D, Shivashekar G, Sureshkumar VP (2017) Abnormal amyloid β42 expression and increased oxidative stress in plasma of CKD patients with cognitive dysfunction: a small scale case control study comparison with Alzheimer's disease. BBA Clin 8:20–27
Vinothkumar G, Krishnakumar S, Shivashekar G, Sreedhar S, Dinesh S, Sundaram A, Balakrishnan D, Riya VP (2018) Therapeutic impact of rHuEPO on abnormal platelet APP, BACE 1, presenilin 1, ADAM 10 and Aβ expressions in chronic kidney disease patients with cognitive dysfunction like Alzheimer's disease: a pilot study. Biomed Pharmacother 104:211–222
Vinothkumar G, Krishnakumar S, Riya VP (2019) Correlation between abnormal GSK3β, β amyloid, total tau, p-tau 181 levels and neuropsychological assessment total scores in CKD patients with cognitive dysfunction: impact of rHuEPO therapy. J Clin Neurosci 69:38–42
Wang J, Ho L, Chen L, Zhao Z, Zhao W, Qian X, Humala N, Seror I, Bartholomew S, Rosendorff C, Pasinetti GM (2007) Valsartan lowers brain beta-amyloid protein levels and improves spatial learning in a mouse model of Alzheimer disease. J Clin Invest 117(11):3393–3402
Wu Y, Shang Y, Sun SG, Liu RG, Yang WQ (2007) Protective effect of erythropoietin against 1-methyl-4-phenylpyridinium-induced neurodegenaration in PC12 cells. Neurosci Bull 23(3):156–164
Wüstenberg T, Begemann M, Bartels C, Gefeller O, Stawicki S, Hinze-Selch D, Mohr A, Falkai P, Aldenhoff JB, Knauth M, Nave KA, Ehrenreich H (2011) Recombinant human erythropoietin delays loss of gray matter in chronic schizophrenia. Mol Psychiatry 16(1):26–36
Yaffe K, Ackerson L, Hoang TD, Go AS, Maguire MG, Ying GS, Daniel E, Bazzano LA, Coleman M, Cohen DL, Kusek JW, Ojo A, Seliger S, Xie D, Grunwald JE, CRIC Study Investigators (2013) Retinopathy and cognitive impairment in adults with CKD. Am J Kidney Dis 61(2):219–227
Yagami T, Ueda K, Sakaeda T, Itoh N, Sakaguchi G, Okamura N, Hori Y, Fujimoto M (2004) Protective effects of a selective L-type voltage-sensitive calcium channel blocker, −312-, on neuronal cell death. Biochem Pharmacol 67(6):1153–1165
Yamamoto M, Clark JD, Pastor JV, Gurnani P, Nandi A, Kurosu H, Miyoshi M, Ogawa Y, Castrillon DH, Rosenblatt KP, Kuro-o M (2005) Regulation of oxidative stress by the anti-aging hormone klotho. J Biol Chem 280(45):38029–38034
Yang WN, Hu XD, Han H, Shi LL, Feng GF, Liu Y, Qian YH (2014) The effects of valsartan on cognitive deficits induced by aluminum trichloride and d-galactose in mice. Neurol Res 36(7):651–658
Yin ZX, Ren ZP, Jing G, Liu D, Zhang J, Wang ZQ, Zhang M, Zhai Y, Song PK, Zhao YF, Pang SJ, Mi SQ, Zhao WH (2019) A cohort study on the association between dietary patterns which benefit for normal kidney function and the cognitive performance in the Chinese elderly. Zhonghua Liu Xing Bing Xue Za Zhi 40(4):427–432
Yu J, Gattoni-Celli M, Zhu H, Bhat NR, Sambamurti K, Gattoni-Celli S, Kindy MS (2011) Vitamin D3-enriched diet correlates with a decrease of amyloid plaques in the brain of AβPP transgenic mice. J Alzheimers Dis 25(2):295–307
Zhang F, Wang S, Cao G, Gao Y, Chen J (2007) Signal transducers and activators of transcription 5 contributes to erythropoietin-mediated neuroprotection against hippocampal neuronal death after transient global cerebral ischemia. Neurobiol Dis 25(1):45–53
Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, Chen M, He Q, Liao Y, Yu X, Chen N, Zhang JE, Hu Z, Liu F, Hong D, Ma L, Liu H, Zhou X, Chen J, Pan L, Chen W, Wang W, Li X, Wang H (2012) Prevalence of chronic kidney disease in China: a cross-sectional survey. Lancet 379(9818):815–822
Zhang CY, Chen Y, Chen S, Kong XC, Liu Y, You CQ, Wan C, Bondzie PA, Su H, Zhang C, He FF (2017) Evaluation of mental disorders using proton magnetic resonance spectroscopy in Dialysis and Predialysis patients. Kidney Blood Press Res 42(4):686–696
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (No. 81974162, No. 81670166, and No. 81770711) and the National Key R&D Program of China (2018YFC1314000).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, CY., He, FF., Su, H. et al. Association between chronic kidney disease and Alzheimer’s disease: an update. Metab Brain Dis 35, 883–894 (2020). https://doi.org/10.1007/s11011-020-00561-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-020-00561-y