Abstract
Temporal lobe epilepsy (TLE) is a common form of drug-resistant epilepsy that sometimes responds to dietary manipulation such as the ‘ketogenic diet’. Here we have investigated the effects of metformin in the rat pilocaroin model of TLE. Male rats were treated with intra peritoneal injection of pilocarpine hydrochloride, in dose of 360 mg/kg to induce status epilepticus (SE). At 45 day after induction of SE, metformin was injected intraperitoneally in dose of 250 mg/kg/day for 5 days. We show that metformin potently reduces the progression of seizures and blocks seizure-induced over-expression of brain-derived neurotropic factor (BDNF) and its receptor, Tropomyosin receptor kinase B (TrkB). We have shown that this reduced expression pattern is mediated by the transcriptional co-repressor CtBP (C-terminal binding protein). Moreover, metformin decreased mechanistic target of rapamycin (mTOR) activation through activation of AMP-activated protein kinase (AMPK) signaling pathway. Our findings have been shown that metformin has anticonvulsant and antiepileptic properties, and suggesting that antiglycolytic compounds such as metformin may represent a new class of drugs for treating epilepsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epilepsy is a disorder of the nervous system that, despite decades of research, yet clinically uninhibited and effective treatment has not been found. Temporal lobe epilepsy (TLE) is characterized usually by a complex partial seizure and sclerosis in the hippocampus, and usually does not respond to common treatment (Schipper et al. 2016). Recent reports show that this condition sometimes responds to diet like the ketogenic diet (Garriga-Canut et al. 2006). New studies show that glycolytic metabolism increases epileptic seizures and inhibition of glycolysis has antiepileptic effects. There are several reports showing that the ketogenic diets (including high-fat and low-carbohydrate diets) that reduce glycolysis, are effective in the treatment of epilepsy (Ding et al. 2010).
AMP-activated protein kinase (AMPK) is heterotrimeric serine/threonine protein kinase, which functions as a cellular energy sensor and regulator that is normally activated in response to diminishing energy supply, e.g. ATP depletion or glucose starvation (Guan et al. 2016; Hang et al. 2016). Activated AMPK coordinates an energy-conserving program by increasing cellular ATP production and reducing ATP consumption by shutting down energy intensive processes such as the mammalian target of rapamycin (mTOR) signaling pathway (Potter et al. 2010). Indeed AMPK activation has previously been shown to lead to inhibition of the mTOR signaling pathway. AMPK inhibits mTOR via phosphorylation and activation of the Tuberous Sclerosis Complex (TSC) as well as directly phosphorylating the RAPTOR subunit of mTORC1 (Potter et al. 2010).
Metformin, a classic anti-diabetic drug, is a potent activator of AMPK and able to crosses the blood brain barrier (BBB) and has different metabolic effects, including increased sensitivity to insulin, increasing glucose uptake and decreased hepatic glucose synthesis. Ma et al. have been shown that metformin is effective in the treatment of Huntington’s disease by increasing AMPK signaling (Ma et al. 2007). Otherwise, Li et al. have reported that metformin improves cognitive changes and synaptic proteins in Alzheimer’s disease (Li et al. 2012). Moreover, Labuzek et al. have been proven beneficial effects of metformin in the different models of neuroinflammatory and neurodegenerative diseases (Labuzek et al. 2010). It has been reported that metformin has protective effects against apoptosis of neuronal cell (El-Mir et al. 2008). In one study, Grzybowska et al. showed that metformin can be used to cancer, Alzheimer’s disease and type 1 diabetes and AMPK is an important mediator in these trends (Grzybowska et al. 2011). Potter et al. reported that AMPK inhibitors such as compound-C and ara-A rescues the suppression of late-phase long-term potentiation (L-LTP) by energy stress (Potter et al. 2010).
Brain-derived neurotropic factor (BDNF) is an upstream component of the mTOR cascade and is sufficient to enhance potentiation at CA1 synapses in a rapamycin sensitive manner (Tang et al. 2002). BDNF as an important landmark in progress of epilepsy, increase the release of stimulatory neurotransmitters. BDNF significantly increases in the hippocampus after epilepsy (Ding et al. 2010). It has been reported that BDNF injection to cause epilepsy (Scharfman et al. 2002) and reducing its level will prevent it (Binder et al. 1999). Kokaia et al. showed that in heterozygous mice for BDNF, there was more than two-fold decrease in epileptic seizures (Kokaia et al. 1995). On the other hand, it has been shown that BDNF receptor, Tropomyosin receptor kinase B (TrkB) has an important role in the development of epilepsy (Garriga-Canut et al. 2006).
It has been shown that 2-Deoxy-D-glucose (2DG), a glycolytic inhibitor, is a potent activator of AMPK and prevents stimulation-induced mTOR activation eventually slowing the progression of epilepsy (Garriga-Canut et al. 2006). Garriga-Canut et al. showed that 2DG reduced epileptic seizures by reducing the expression of BDNF and its receptor TrkB through activation of Neuron-Restrictive Silencer Factor (NRSF) (Garriga-Canut et al. 2006). Activation of NRSF increases the activity of BDNF gene promoter repressor protein C-terminal binding protein (CtBP), therby preventing the overexpression of BDNF gene (Garriga-Canut et al. 2006). CtBP family includes four proteins (CtBP1 [CtBP1-L], CtBP3/BARS [CtBP1-S], CtBP2, and RIBEYE) (Verger et al. 2006) are transcriptional regulators that involve in the energy homeostasis (Chinnadurai 2002). In this investigation we are examining whether AMPK-mediated metformin effects are equivalent to CtBP- mediated 2DG effects in the prevention of epileptogenesis using animal model.
Material and methods
Animals
Adult male Wistar rats weighing 250–270 g were housed in a controlled environment with light/dark cycle at 22 ± 1 °C for 2 weeks before beginning of experiment. Rats had free access to food and water. All animal experiments were performed in accordance with the Helsinki declaration and the study was approved by the Ethics in Research Committee of Iran University of Medical Sciences. All efforts were made to minimize the number of animals and their pain or suffering. Trained personnel handled animals.
Induction of Pilocarpine induced epilepsy (PIE) model
Rats were treated with pilocarpine hydrochloride, a muscarinic cholinergic agonist (Sigma; 360 mg/kg dissolved in saline, i.p; intra peritoneal) to induce status epilepticus (SE), as previously described (Eftekhari et al. 2014). Animals were pretreated with cholinergic antagonist, scopolamine methyl nitrate (Sigma; 1 mg/kg IP) 30 min before pilocarpine injection to reduce the peripheral cholinergic effects (Ferhat et al. 2003). The behavior of the rats was observed for several hours after injection and was scored using Racine’s classification (Racine 1972). The rats, which had shown visible SE behavioural changes (stages 3–5) for 3–4 h were selected in this study. Diazepam (7 mg/kg IP) was injected to terminate the period of seizures. SE induced animals were hand fed until they could eat and drink on their own and parallel control received saline was maintained under similar conditions. Two weeks after pilocarpine hydrochloride injection, all rats were video monitored for 6 weeks (8 h/day, 5 days/week) to record spontaneous seizures.
Drug administration
At 45 d after induction of SE, animals were randomly divided into three groups with six in each group. The control group received vehicle. The epileptic group received 360 mg/kg ip pilocarpin as was explained. Treatment group received i.p injections of metformin (250 mg/kg/day), for 5 days.
Behavioral evaluation
One week after SE, 6 rats from each group were evaluated in different hyperexcitability tests. All tests were performed twice weekly for 6 weeks.
Approach-response test
A pen held vertically is moved slowly toward the face of the animal. Responses were recorded as 1 – no reaction; 2 – the rat sniffs at the object; 3 – the rat moves away from the object; 4 – the rat freezes; 5 –the rat jumps away from the object; and 6 – the rat jumps at or attacks the object.
Touch-response test
The animal is gently prodded in the rump with the blunt end of a pen. Responses were recorded as 1 – no reaction; 2 – the rat turns toward the object; 3 – the rat moves away from the object; 4 – the rat freezes; 5 – the rat moves close to the touch; 6-the rat turns away from the touch; and 7 – the rat jumps with or without vocalizations.
Finger-snap test
A finger snap several inches above the head of the animal is performed. Responses were recorded as 1 – no reaction; 2 – the rat jumps slightly (normal reaction); and 3 – the rat jumps dramatically.
Pick-up test
The animal is picked up by grasping it around the body. Responses were recorded as 1 – very easy; 2 – easy with vocalizations; 3 – some difficulty, the rat rears and faces the hand; 4 – the rat freezes; 5 – difficult, the rat avoids the hand by moving away; and 6 – very difficult, the rat behaves defensively, and may attack the hand.
These tests were done by three independent observers; the means of their scores were calculated for each animal for each test. The tests were performed in the home cage with 30 min interval between each test.
Real-time RT-PCR
One week after drug administration rats were anesthetized by ketamine and the hippocampal tissue was removed and washed by cold PBS. Total RNA was extracted from the tissue using RNA extraction kit (Bioneer, Korea). The quantity and quality of the isolated RNA was determined by measurement of the optical density at 260 and 280 nm using a UV/VIS spectrophotometer (Ultrospec 2000; Pharmacia) and agarose gel electrophoresis, respectively. The cDNA was generated from 1 μg of total RNA by reverse transcription using the CycleScript Reverse Transcription system (Bioneer, Korea). The mRNA expression levels of BDNF, Trk and Ctbp were determined by quantitative RT-PCR using a real-time thermal cycler (Rotor-Gene 6000: Qiagen: Germany). B-actin mRNA was used as the internal control.
The PCR reactions were set up in a volume of 10 μl containing 1 μg of cDNA, 5 μl AccuPower 2X GreenStarq PCR Master Mix (Bioneer, Korea) and 10 pM of each forward and reverse specific primer (Qiagen). The sequences of the primers is as follows: bactin forward: CGGTCAGGTCATCACTATCGG, bactin reverse: ATGCCACAGGATTCCATACCCA, TrkB forward: GGCCGTGAAGACGCTGAAG, TrkB reverse: TCGTGCTGGAGGTTGGTCA, BDNF forward: GGCTCTCATACCCACTAAGATACATC, BDNF reverse: CGGAAACAGAACGAACAGAAACAG, Ctbp forward: CCTGCCGCTGGTAAGACTTTG, Ctbp reverse: GTTCTGTCACGGAGCCTCATC. The reaction conditions were 95 °C for 10 min, followed by 40 cycles at 95 °C for 15 s and 60 °C for 1 min. Amplification specificity was checked by verifying a single peak on the melting curves. All samples and controls were normalized against reference gene. No template controls and reverse transcriptase control were included in each PCR run. All assays were carried out three times as independent PCR runs for each cDNA sample. The ΔΔCT method (Livak and Schmittgen 2001) was used to quantify the amplification-fold difference between groups; each gene expression was normalized with respect to b-actin mRNA content.
To validate the use of the ΔΔCT method, 5-fold serial dilutions were performed on a cDNA sample over a 125-fold range. For each dilution sample, amplifications were performed in triplicate using reference and target genes primers. The average CT of all tests was calculated and the ΔCT of target (BDNF, Trk and Ctbp) and reference (b-actin) genes was determined. A plot of the log cDNA dilution versus ΔCT (ΔCT target – ΔCT reference) was made for each target and reference genes (Fig. 1) and the slope of fitted line was determined (Livak and Schmittgen 2001).
Histopathological studies
Tissue preparation and staining
After performing behavioral assessment tests in each experimental group, rats were i.p. euthanized using ketamine (50 mg/kg) and xylezine (4 mg/kg), followed by cervical dislocation and opening the diaphragm. Thereafter, mice were transcardially perfused first with PBS and then with 4% paraformaldehyde (PFA) in PBS (pH 7.4). Brains were dissected from the skull and post-fixed overnight in 4% PFA in BPS at 4 °C. Fixed brains were coronal sectioned (10 μm thickness) using the floor standing fully automatic cryostat, MNT-SLEE (Mainz GmbH, Germany), and hippocampus were identified. Hematoxylin and eosin (H&E) staining was performed to study.
Immunohistochemistry (IHC) analysis
We serially sectioned rat brains (10 μm) in the coronal planes using cryostat, and collected onto poly-L-lysine coated coverslips and rostral part of the CC used for tissue analysis. The sections were air dried at room temperature for 30 min. The sections were then rehydrated in 0.1 M PBS twice (10 min each), incubated in blocking solution (0.1 M PBS containing 2% bovina serum albumin (BSA), 1% normal goat serum and 0.2% Triton X-100), and afterwards incubated for 1 h in permeabilization buffer (10% goat serum, 0.1% Triton X-100 in PBS). Then sections incubated with appropriately primary antibody at 4 °C overnight followed by washing and further incubation with secondary antibodies for 2 h in antibody solution (5% goat serum, 0.05% Triton X-100 in PBS). Primary antibody for IHC was chicken polyclonal antibodies to P-AMPK and P-mTor (1:200; neuromics). The secondary antibodies (Santa Cruz Biotechnology) used included: to detect immunostaining we used FITC conjugated goat anti-mouse IgG (1:200); for P-AMPK and we used FITC conjugated goat anti-rat (1:200); for m-Tor. All sections were counterstained with DAPI (2 μg/ml) to visualize the nuclei. Negative controls were obtained by omitting either the primary or secondary antibody and gave no signal (data not shown). All analysis was examined using a fluorescence microscope (Olympus BX51), and images were captured using a digital camera (Olympus DP72).
Statistical analysis
All statistical analyses on PCR data were performed using SSPS 19.0 (SPSS; USA) and p < 0.05 was considered statistically significant. Kruskal–Wallis two-way analysis of variance was used to examine significant differences between groups. Mann-Whitney U tests was used for post-hoc comparisons with Bonferroni correction. All results were presented as mean values ± standard error of mean.
Results
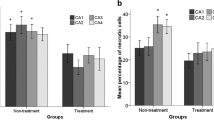
Behavioral alterations in epileptic rats
The PSBB was done at several time points after SE to determine the behavioral changes in epileptic rats and the effect of metformin treatment in this regard (n = 6 for each group). When we compared pilocarpine-injected animals with the control group on the 7th day post-treatment, a significant difference (P < 0.05) was observed in the touch-response, pick-up, finger snap and approach response test indicating that epileptic rats are more sensitive to environmental stimuli. Metformin treatment counteracted these behaviors (Fig. 1).
Effects of metformin on BDNF, Trk and CtBP expression
Metformine (250 mg/kg/day) were administered during the latent phase of pilocarpine-induced TLE. The animals were sacrificed one week post drug administration and the BDNF, Trk and CtBP expression was quantified by RT-PCR. Compared to the epileptic animals, BDNF and Trk expression were decreased significantly in the metformin group. Also expression of CtBP showed significant increase after drug administration (Fig. 2).
Validation of ΔΔCT method. Four serial dilutions (5-fold) on a cDNA sample over a 125-fold range. Serial dilutions were amplified by real-time PCR using reference and target gene primers in triplicates. The average CTs and ΔCT (ΔCT target – ΔCT reference) was calculated for each cDNA dilution. The line was fitted using linear regression analysis. The slope of the line was less than 0.1; therefore, the ΔΔCT method can be used to analyze the data. Trk, BDNF and ctbp expression was quantified by real-time PCR. Trk and BDNF expression were significantly decreased in metformin treatment group compared to untreated epileptic animals. Ctbp expression was significantly increased in metformin treatment group compared to untreated epileptic animals. * p < 0.05 compared to control group. # p < 0.05 compared to epileptic group. Results were shown using the mean ± standard error (SE)
Effects of metformin on p-AMPK and p -mTOR protein expression
p-AMPK and p-mTOR expression throughout pilocarpin and metformin treatment. Immunohistochemistry of coronal sections through the hippocampus showing labelling with a monoclonal antibody that is specific to p-AMPK and p-mTOR. p-AMPK double-staining shows decreased immunoreactivity after pilocarpin treatment in comparison with control. Treatment by metformin increased the protein expression of p-AMPK. p-mTOR double-staining shows increased immunoreactivity after pilocarpin treatment in comparison with control. Treatment by metformin decreased the protein expression of p-mTOR (Fig. 3).
p-AMPK and p-mTOR expression throughout pilocarpin and metformin treatment. Immunohistochemistry of coronal sections through the hippocampus showing labelling with a monoclonal antibody that is specific to p-AMPK and p-mTOR. p-AMPK double-staining shows decreased immunoreactivity after pilocarpin treatment in comparison with control. Treatment by metformin increased the protein expression of p-AMPK. p-mTOR double-staining shows increased immunoreactivity after pilocarpin treatment in comparison with control. Treatment by metformin decreased the protein expression of p-mTOR. Data are expressed as means ± SEM. ٭compared to control group, #compared to epileptic group (#,٭ P < 0.05, ## P < 0.05, and ٭٭٭P < 0.001).
Discussion
Recent studies demonstrated that metformin has neuroprotective properties (Martin-Montalvo et al. 2013). It has been reported that Metformin has beneficial effects in animal models of multiple sclerosis, stroke and Alzheimer’s disease (Zhao et al. 2014). It is well documented that metformin could activate AMPK signaling, an important sensor of energy balance (Zhou et al. 2001). Moreover, it has been shown that metformin activate AMPK-atypical PKC-CBP pathway to promote neurogenesis and enhance spatial memory function (Wang et al. 2012). Therefore, the beneficial effect of metformin could be due to the metformin action through AMPK signaling. In the present study, we confirmed that administration of metformin (250 mg/ kg) significantly reduced the mean seizure score as compared to epileptic group, showing anticonvulsant activity.
Neuroprotective effects of metformin have been confirmed in several models of neurologic disorders, through promotion of autophagy, inhibition of inflammation and control of oxidative stress (Ashabi et al. 2015; Sarkaki et al. 2015; Zhu et al. 2015). It has been reported that metformin reduced myocardial infarct size and decreased apoptosis in neurons (Lexis et al. 2014; Chen et al. 2016). Metformin as an AMPK agonist, improves anxiety-like behavior in rats with forebrain ischemia by regulating autophagy (Sarkaki et al. 2015). This evidence suggests that metformin may have a neuroprotective effect by increasing autophagy. Consistently, our results showed that metformin increased the expression of AMPK with concomitant decrease in mTOR expression levels.
Several studies have demonstrated a potential role of mTOR signaling in epilepsy and in particular, epileptogenesis (both convulsive and non-convulsive); however, the exact mechanism(s) involved in these processes have not yet been clarified (Russo et al. 2014a, b). Vliet et al. found that mTOR inhibition by the specific inhibitor Rapamycin (RAP) exerted antiepileptogenic effects in a post-status epilepticus rat model of temporal lobe epilepsy (van Vliet et al. 2012). Subsequently, Russo et al. demonstrated that RAP treatment inhibited the increase in absence seizures induced in WAG/Rij rats by intracerebral administration of LPS endotoxin (Russo et al. 2013). More recently, Wang et al. reported that RAP reduced the activation of inducible nitric oxide synthase (iNOS), cyclooxygenase-2 (COX-2) and IL-1β at mRNA level after pilocarpine- induced status epilepticus in rats (Wang et al. 2013).
mTOR signaling is known to be activated during the epileptogenic phase of several animal epilepsy models contributing to the development of seizures (Russo et al. 2014a, b). Moreover, its pharmacological inhibition by rapamycin resulted in a decrease in the development of spontaneous seizures. Russo et al. showed antiepileptogenic effect of rapamycin in a well-established animal model of absence epilepsy (Russo et al. 2013).
Functional progression of kindled seizures is undoubtedly under complex regulatory control. The BDNF and TrkB signaling pathway has been implicated in various cellular alterations induced in neural circuits by experimental seizures and kindling (Frey and Morris 1997). It has been shown that BDNF and TrkB signaling is an important determinant of kindling progression. Conditional knockouts of BDNF and TrkB in mice have implicated neurotrophin signaling in the progression of kindling (Potter et al. 2010). Mice heterozygous for BDNF show a two-fold decrease in the rate of kindling, as measured by the number of after discharges to class V seizures (Guzowski et al. 2000). Potter et al. showed that 2DG has anticonvulsant and antiepileptic properties; suggesting that targeting pathways of energy metabolism can control seizures. 2DG decreases BDNF and TrkB expression in normal rats and prevents or reduces seizure-induced over expression of BDNF and TrkB in rats during the early stages of kindling (Potter et al. 2010). CtBP is a co-repressor of neuronal genes and that the interaction of NRSF with CtBP a property may contributes to the metabolic regulation of neuronal gene expression involved in epilepsy (Potter et al. 2010). It has been shown that 2DG reduces expression of the NRSF target genes encoding BDNF and TrkB. This reduced expression is mediated by the transcription factor NRSF, which recruits the NADH-binding co-repressor CtBP to generate a repressive chromatin environment around the BDNF promoter. Glycolytic inhibition results in an increase in recruitment of the CtBP co-repressor to NRSF-binding sites. Our study show that metformin through increasing CtBP could decree BDNF and TrkB; so it could decrease progression of epilepsy.
Our results suggest that metformin may have considerable potential as a therapeutic agent for epilepsy. The therapeutic actions of metformin may be partly due to metabolic regulation. The study may be a novel treatment strategy for patients with epilepsy.
Funding
Iran University of medical science, Tehran, Iran.
References
Ashabi G, Khalaj L, Khodagholi F, Goudarzvand M, Sarkaki A (2015) Pre-treatment with metformin activates Nrf2 antioxidant pathways and inhibits inflammatory responses through induction of AMPK after transient global cerebral ischemia. Metab Brain Dis 30(3):747–754
Binder DK, Routbort MJ, Ryan TE, Yancopoulos GD, McNamara JO (1999) Selective inhibition of kindling development by intraventricular administration of TrkB receptor body. J Neurosci 19(4):1424–1436
Chen B, Teng Y, Zhang XG, Lv XF, Yin YL (2016) Metformin alleviated Aβ-induced apoptosis via the suppression of JNK MAPK signaling pathway in cultured hippocampal neurons. Biomed Res Int 2016:1–8. https://doi.org/10.1155/2016/1421430
Chinnadurai G (2002) CtBP, an unconventional transcriptional corepressor in development and oncogenesis. Mol Cell 9(2):213–224
Ding Y, Wang S, Zhang MM, Guo Y, Yang Y, Weng SQ, Wu JM, Qiu X, Ding MP (2010) Fructose-1,6-diphosphate inhibits seizure acquisition in fast hippocampal kindling. Neurosci Lett 477(1):33–36
Eftekhari S, Mehrabi S, Soleimani M, Hassanzadeh G, Shahrokhi A, Mostafavi H, Hayat P, Barati M, Mehdizadeh H, Rahmanzadeh R, Hadjighassem MR, Joghataei MT (2014) BDNF modifies hippocampal KCC2 and NKCC1 expression in a temporal lobe epilepsy model. Acta Neurobiol Exp (Wars) 74(3):276–287
El-Mir MY, Detaille D, R-Villanueva G, Delgado-Esteban M, Guigas B, Attia S, Fontaine E, Almeida A, Leverve X (2008) Neuroprotective role of antidiabetic drug metformin against apoptotic cell death in primary cortical neurons. J Mol Neurosci 34(1):77–87
Ferhat L, Esclapez M, Represa A, Fattoum A, Shirao T, Ben-Ari Y (2003) Increased levels of acidic calponin during dendritic spine plasticity after pilocarpine-induced seizures. Hippocampus 13(7):845–858
Frey U, Morris RG (1997) Synaptic tagging and long-term potentiation. Nature 385(6616):533–536
Garriga-Canut M, Schoenike B, Qazi R, Bergendahl K, Daley TJ, Pfender RM, Morrison JF, Ockuly J, Stafstrom C, Sutula T, Roopra A (2006) 2-Deoxy-D-glucose reduces epilepsy progression by NRSF-CtBP-dependent metabolic regulation of chromatin structure. Nat Neurosci 9(11):1382–1387
Grzybowska M, Bober J, Olszewska M (2011) Metformin - mechanisms of action and use for the treatment of type 2 diabetes mellitus. Postepy Hig Med Dosw (Online) 65:277–285
Guan Y, Cui ZJ, Sun B, Han LP, Li CJ, Chen LM (2016) Celastrol attenuates oxidative stress in the skeletal muscle of diabetic rats by regulating the AMPK-PGC1alpha-SIRT3 signaling pathway. Int J Mol Med 37(5):1229–1238
Guzowski JF, Lyford GL, Stevenson GD, Houston FP, McGaugh JL, Worley PF, Barnes CA (2000) Inhibition of activity-dependent arc protein expression in the rat hippocampus impairs the maintenance of long-term potentiation and the consolidation of long-term memory. J Neurosci 20(11):3993–4001
Hang L, Basil AH, Lim KL (2016) Nutraceuticals in Parkinson's disease. NeuroMolecular Med 18(3):306–321
Kokaia M, Ernfors P, Kokaia Z, Elmer E, Jaenisch R, Lindvall O (1995) Suppressed epileptogenesis in BDNF mutant mice. Exp Neurol 133(2):215–224
Labuzek K, Liber S, Gabryel B, Okopien B (2010) Metformin has adenosine-monophosphate activated protein kinase (AMPK)-independent effects on LPS-stimulated rat primary microglial cultures. Pharmacol Rep 62(5):827–848
Lexis CPH, Wieringa WG, Hiemstra B, van Deursen VM, Lipsic E, van der Harst P, van Veldhuisen DJ, van der Horst ICC (2014) Chronic metformin treatment is associated with reduced myocardial infarct size in diabetic patients with ST-segment elevation myocardial infarction. Cardiovasc Drugs Ther 28(2):163–171
Li J, Deng J, Sheng W, Zuo Z (2012) Metformin attenuates Alzheimer's disease-like neuropathology in obese, leptin-resistant mice. Pharmacol Biochem Behav 101(4):564–574
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) method. Methods 25(4):402–408
Ma TC, Buescher JL, Oatis B, Funk JA, Nash AJ, Carrier RL, Hoyt KR (2007) Metformin therapy in a transgenic mouse model of Huntington's disease. Neurosci Lett 411(2):98–103
Martin-Montalvo A, Mercken EM, Mitchell SJ, Palacios HH, Mote PL, Scheibye-Knudsen M, Gomes AP, Ward TM, Minor RK, Blouin MJ, Schwab M, Pollak M, Zhang Y, Yu Y, Becker KG, Bohr VA, Ingram DK, Sinclair DA, Wolf NS, Spindler SR, Bernier M, de Cabo R (2013) Metformin improves healthspan and lifespan in mice. Nat Commun 4:2192
Potter WB, O'Riordan KJ, Barnett D, Osting SM, Wagoner M, Burger C, Roopra A (2010) Metabolic regulation of neuronal plasticity by the energy sensor AMPK. PLoS One 5(2):e8996
Racine RJ (1972) Modification of seizure activity by electrical stimulation. II. Motor seizure. Electroencephalogr Clin Neurophysiol 32(3):281–294
Russo E, Andreozzi F, Iuliano R, Dattilo V, Procopio T, Fiume G, Mimmi S, Perrotti N, Citraro R, Sesti G, Constanti A, De Sarro G (2014a) Early molecular and behavioral response to lipopolysaccharide in the WAG/Rij rat model of absence epilepsy and depressive-like behavior, involves interplay between AMPK, AKT/mTOR pathways and neuroinflammatory cytokine release. Brain Behav Immun 42:157–168
Russo E, Citraro R, Donato G, Camastra C, Iuliano R, Cuzzocrea S, Constanti A, De Sarro G (2013) mTOR inhibition modulates epileptogenesis, seizures and depressive behavior in a genetic rat model of absence epilepsy. Neuropharmacology 69:25–36
Russo E, Follesa P, Citraro R, Camastra C, Donato A, Isola D, Constanti A, De Sarro G, Donato G (2014b) The mTOR signaling pathway and neuronal stem/progenitor cell proliferation in the hippocampus are altered during the development of absence epilepsy in a genetic animal model. Neurol Sci 35(11):1793–1799
Sarkaki A, Farbood Y, Badavi M, Khalaj L, Khodagholi F, Ashabi G (2015) Metformin improves anxiety-like behaviors through AMPK-dependent regulation of autophagy following transient forebrain ischemia. Metab Brain Dis 30(5):1139–1150
Scharfman HE, Goodman JH, Sollas AL, Croll SD (2002) Spontaneous limbic seizures after intrahippocampal infusion of brain-derived neurotrophic factor. Exp Neurol 174(2):201–214
Schipper S, Aalbers MW, Rijkers K, Swijsen A, Rigo JM, Hoogland G, Vles JSH (2016) Tonic GABA(a) receptors as potential target for the treatment of temporal lobe epilepsy. Mol Neurobiol 53(8):5252–5265
Tang SJ, Reis G, Kang H, Gingras AC, Sonenberg N, Schuman EM (2002) A rapamycin-sensitive signaling pathway contributes to long-term synaptic plasticity in the hippocampus. Proc Natl Acad Sci U S A 99(1):467–472
van Vliet EA, Forte G, Holtman L, den Burger JC, Sinjewel A, de Vries HE, Aronica E, Gorter JA (2012) Inhibition of mammalian target of rapamycin reduces epileptogenesis and blood-brain barrier leakage but not microglia activation. Epilepsia 53(7):1254–1263
Verger A, Quinlan KG, Crofts LA, Spano S, Corda D, Kable EP, Braet F, Crossley M (2006) Mechanisms directing the nuclear localization of the CtBP family proteins. Mol Cell Biol 26(13):4882–4894
Wang J, Gallagher D, DeVito LM, Cancino GI, Tsui D, He L, Keller GM, Frankland PW, Kaplan DR, Miller FD (2012) Metformin activates an atypical PKC-CBP pathway to promote neurogenesis and enhance spatial memory formation. Cell Stem Cell 11(1):23–35
Wang SJ, Bo QY, Zhao XH, Yang X, Chi ZF, Liu XW (2013) Resveratrol pre-treatment reduces early inflammatory responses induced by status epilepticus via mTOR signaling. Brain Res 1492:122–129
Zhao RR, Xu XC, Xu F, Zhang WL, Zhang WL, Liu LM, Wang WP (2014) Metformin protects against seizures, learning and memory impairments and oxidative damage induced by pentylenetetrazole-induced kindling in mice. Biochem Biophys Res Commun 448(4):414–417
Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, Wu M, Ventre J, Doebber T, Fujii N, Musi N, Hirshman MF, Goodyear LJ, Moller DE (2001) Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest 108(8):1167–1174
Zhu XC, Jiang T, Zhang QQ, Cao L, Tan MS, Wang HF, Ding ZZ, Tan L, Yu JT (2015) Chronic metformin preconditioning provides Neuroprotection via suppression of NF-kappaB-mediated inflammatory pathway in rats with permanent cerebral ischemia. Mol Neurobiol 52(1):375–385
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There is no conflict of interest.
Rights and permissions
About this article
Cite this article
Mehrabi, S., Sanadgol, N., Barati, M. et al. Evaluation of metformin effects in the chronic phase of spontaneous seizures in pilocarpine model of temporal lobe epilepsy. Metab Brain Dis 33, 107–114 (2018). https://doi.org/10.1007/s11011-017-0132-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-017-0132-z