Abstract
Objectives Severe maternal morbidity (SMM) is an important indicator for identifying and monitoring efforts to improve maternal health. Studies have identified independent risk factors, including race/ethnicity; however, there has been limited investigation of the modifying effect of socioeconomic factors. Study aims were to quantify SMM risk factors and to determine if socioeconomic status modifies the effect of race/ethnicity on SMM risk. Methods We used 2008–2012 NYC birth certificates matched with hospital discharge records for maternal deliveries. SMM was defined using an algorithm developed by the Centers for Disease Control and Prevention. Mixed-effects logistic regression models estimated SMM risk by demographic, socioeconomic, and health characteristics. The final model was stratified by Medicaid status (as a proxy for income), education, and neighborhood poverty. Results Of 588,232 matched hospital deliveries, 13,505 (229.6 per 10,000) had SMM. SMM rates varied by maternal age, birthplace, education, income, pre-existing chronic conditions, pre-pregnancy weight status, trimester of prenatal care entry, plurality, and parity. Race/ethnicity was consistently and significantly associated with SMM. While racial differences in SMM risk persisted across all socioeconomic groupings, the risk was exacerbated among Latinas and Asian-Pacific Islanders with lower income when compared to white non-Latinas. Similarly, living in the poorest neighborhoods exacerbated SMM risk among both black non-Latinas and Latinas. Conclusions for Practice SMM determinants in NYC mirror national trends, including racial/ethnic disparities. However, these disparities persisted even in the highest income and educational groups suggesting other pathways are needed to explain racial/ethnic differences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
What is already known on this subject? Studies have identified independent risk factors for severe maternal morbidity (SMM), including race/ethnicity. However, there has been limited investigation of the potential modifying effect of socioeconomic factors on racial differences in SMM risk.
What does this study add? This study examines the determinants of SMM in New York City from 2008 to 2012. Findings demonstrate independent individual-level SMM risk factors and the persistent effect of race/ethnicity even within the highest socioeconomic groups.
Introduction
As nationwide rates of maternal mortality increase, severe maternal morbidity (SMM) has emerged as a marker to identify and monitor the effectiveness of interventions to improve maternal health (Lu et al. 2015). In 2012, the US Centers for Disease Control and Prevention (CDC) standardized the measurement of this construct by focusing on 25 indicators of life-threatening complications at childbirth (Callaghan et al. 2012). This algorithm uses diagnosis and procedure codes from the International Classification of Diseases, 9th Edition, Clinical Manual (ICD-9-CM), making population-based surveillance of SMM possible using hospital discharge data (Centers for Disease Control and Prevention 2017).
Using this algorithm, national estimates suggest SMM affects 129 per 10,000 deliveries, or approximately 52,000 women a year (Callaghan et al. 2012). Women with advanced maternal age, multiple births, previous cesarean delivery, or pre-existing chronic disease are at elevated risk for SMM (Gray et al. 2012; Centers for Disease Control and Prevention 2017). Racial/ethnic disparities in SMM have also been found, with particularly high rates among black non-Latina women (Creanga et al. 2014). Variation in hospital site and performance has emerged as an important contributor to these racial/ethnic differences (Howell et al. 2016a).
Socioeconomic factors, such as education, income, and neighborhood poverty, have also been acknowledged as important drivers of SMM and racial/ethnic disparities (Louis et al. 2015). In a national study, Medicaid status and area-based poverty were both associated with higher SMM rates, but did not fully explain racial/ethnic disparities (Creanga et al. 2014). Given the well-known importance of socioeconomic status on population health and inequities among racial groups (Anderson et al. 2014; Williams et al. 2010), this paper sought to examine whether higher education attainment, income level, or neighborhood wealth reduced racial/ethnic differences in SMM.
The New York City Department of Health and Mental Hygiene (DOHMH) recently established the first-ever local SMM surveillance system in 2015, utilizing the CDC algorithm and linked hospital discharge records and birth certificates that were available from 2008 to 2012. These data provide a unique opportunity to explore a broad range of demographic, socioeconomic, and health-related risk factors for SMM within a large, diverse sample of women. Therefore, the objectives of this study were to describe the determinants of SMM in NYC from 2008 to 2012 including race/ethnicity, and to examine the role of socioeconomic status in reducing or eliminating racial disparities in SMM risk.
Methods
We used 2008–2012 NYC birth certificates matched with hospital discharge records for maternal deliveries. DOHMH collects information on all live births that take place in NYC facilities for legal registration and public health purposes (Howland et al. 2015). A total of 625,505 births were registered in NYC from 2008 to 2012, 99% of which took place in a hospital (Fig. 1). Hospital discharge records are collected by the New York Statewide Planning and Research Cooperative System (SPARCS) (New York State Department of Health). Maternal delivery records from SPARCS were matched with NYC birth certificates using a combination of unique identifiers, resulting in a 95.9% match rate and a final matched sample size of 588,232. The study protocol was approved by the NYC Department of Health and Mental Hygiene (DOHMH) Institutional Review Board (#14-052).
Measures
Severe maternal morbidity (SMM) was defined based on the CDC algorithm, described in detail elsewhere (Callaghan et al. 2012). Briefly, the algorithm includes 25 indicators of SMM that correspond with ICD-9-CM codes found in the hospital discharge record (Table S1). Delivery records with ≥ 1 indicator were categorized as having SMM. Compared to an expert review of abstracted medical records, the SMM algorithm has a 77% sensitivity, 99% specificity, and 44% positive predictive value (Main et al. 2016). To rule out less severe cases, deliveries categories as SMM based solely on diagnosis (rather than procedure codes) were only included if the length of stay was in the 90th percentile or higher by delivery method or if the woman was transferred or died during hospitalization (Callaghan et al. 2012).
Demographic variables of interest included maternal age (≤ 19, 20–24, 25–29, 30–34, 35–39, and ≥ 40 years), year of birth (2008–2012), birthplace (foreign- or US-born), race/ethnicity (White non-Latina, black non-Latina, Latina, Asian-Pacific Islander, and Other or multiple non-Latina ethnicities). Measures of socioeconomic status included educational attainment (less than high school, high school graduate, and college graduate or higher), Medicaid insurance status (yes, no), as a proxy for individual income, and neighborhood poverty, which was derived from the American Community Survey (2011–2013) and linked to the data based on the community district of residence reported on the birth certificate (New York City Department of City Planning). Neighborhood poverty was defined as percent of residents living below the federal poverty level, and empirically categorized as low (< 15%), medium (15–29%) and high (30–44%).
Health and clinical status variables included were smoking in the 3 months before or anytime during pregnancy, parity (0 or 1 + previous live births), plurality (singleton or multiple birth), entry into prenatal care (first, second, third trimester, or never), and pre-pregnancy weight (Underweight = BMI < 18.5, Normal weight = BMI 18.5–24.9, Overweight = BMI 25.0–29.9, Obese Class I = BMI 30.0–34.9, Obese Class II = BMI 35–39.9, and Obese Class III BMI ≥ 40.0). We also included pre-existing chronic conditions (heart disease, hypertension, and diabetes) if they were reported either on the birth certificate or hospital discharge record (Table S2).
Analysis
Mixed-effects logistic regression models estimated the effects of demographic, socioeconomic, and health characteristics on the binary outcome of SMM or not. Variables were included in the model as categorical fixed effects nested within facility identifiers, and normal distribution of the random effects was assumed. Crude odds ratios were initially estimated for the effect of each variable on the outcome, and odds ratios were subsequently adjusted for all variables simultaneously included in the final model. We separately tested for an interaction between race/ethnicity and key socioeconomic variables (education, income, and neighborhood poverty) in the final model. If evidence of an interaction was found, results were stratified accordingly to further explore the effect modification. Due to the low reported specificity of blood transfusion codes (i.e., they can indicate one or ten units of blood), a sensitivity analysis was also conducted to compare adjusted odds ratios across SMM outcomes with or without blood transfusion (Main et al. 2016). Women with multiple hospital deliveries from 2008 to 2012 were identified and one birth was randomly selected for inclusion in regression analyses. Missing values (5%) were omitted from the analysis, resulting in a final sample size of 486,982. Data management and analysis were conducted in SAS (Version 9.2; SAS Institute, Cary, NC) and Stata (Version 14.2; Stata Corp, College Station, TX).
Results
From 2008 to 2012 in NYC, 588,232 hospital deliveries and 13,505 cases of SMM (229.6 per 10,000 deliveries) occurred (Fig. 1). Blood transfusion was the leading indicator of SMM at 176.5 per 10,000 deliveries (Table S1). Other leading indicators included complications during procedure or surgery (19.7), disseminated intravascular coagulation (17.1), and hysterectomy (12.5). The NYC SMM rate in 2008–2012 was nearly double the national average from 2008 to 2009 (229.6 vs. 129.1) (Callaghan et al. 2012) and included higher rates of cardio monitoring, sickle cell anemia with crisis, and severe anesthesia complications.
Risk Factors
SMM rates were high among women who were 40 years or older (358.9 per 10,000 deliveries) or black non-Latina (386.9). Rates were also high among women who received no prenatal care (574.8), had multiple births (761.3), were morbidly obese (Obese Class III) (416.1), or were diagnosed with diabetes (340.6), hypertension (633.2), or heart disease (636.3) (Table 1).
Race/ethnicity was consistently and significantly associated with SMM after controlling for other variables (Table 2). Compared to white non-Latina women, SMM risk was significantly higher among black non-Latina (Adjusted Odds Ratio (AOR) 1.84, 95% CI 1.72–1.97), Latina (AOR 1.52, 95% CI 1.42–1.62), Asian or Pacific Islander (AOR 1.35, 95% CI 1.24–1.46) or other ethnicities (AOR 1.62, 95% CI 1.40–1.88). Maternal education, age, birthplace, and income were also significantly associated with SMM in the adjusted analysis. While women residing in high poverty neighborhoods had higher rates than those women living in low poverty areas (271.6 vs. 184.8 per 10,000 deliveries), this difference was not significant in adjusted analyses. A number of health variables also remained significantly associated with SMM in the adjusted analysis, including the lack of prenatal care, morbid obesity, multiple births, and pre-existing conditions. Finally, smoking in the 3 months before or during pregnancy was not a significant risk factor after adjustment.
Stratification by Socioeconomic Variables
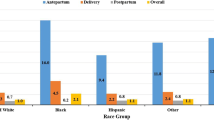
We found some evidence of an interaction between race/ethnicity and education (p-values ranged from 0.006 to 0.498), income (p-values ranged from 0.001 to 0.546), and neighborhood poverty (p-values ranged from < 0.001 to 0.893) and these results were further explored in stratified analyses. SMM rates, particularly for black non-Latina and Latina women, generally followed a socioeconomic gradient, with higher rates at lower education, income, and neighborhood wealth (Table 3).
Table 4 indicates that significant racial differences in SMM risk persisted across all socioeconomic groups for all race/ethnicities. Nevertheless, SMM risk was significantly higher among Latinas with lower income (AORmedicaid 1.69, 95% CI 1.53–1.87; AORother 1.27, 95% CI 1.15–1.41) and higher neighborhood poverty levels (AORhighest 1.96, 95% CI 1.62–2.37; AORlowest 1.31, 95% CI 1.13–1.53) than their higher income / lower poverty counterparts when compared to white non-Latinas in each of these groups. While not significant, results for education followed a similar trend, with higher SMM risk for Latina women with less than a high school education (AOR< HS 1.74, 95% CI 1.45–2.08; AORcollegegrad 1.31 95% CI 1.15–1.49). For Asian-Pacific Islanders, income also had a significant modifying effect on SMM, increasing risk from 1.27 (95% CI 1.15–1.41) to 1.69 (95% CI 1.53–1.87) for those women on Medicaid when compared to white non-Latinas in these groups; the modifying effect of education and neighborhood poverty on SMM risk was not found for Asian-Pacific Islanders. While income and education made a negligible difference in the black-white gap in SMM risk, residence in high poverty neighborhood significantly increased the SMM risk difference between black and white non-Latinas compared to this difference in wealthier neighborhoods (AORhigh poverty 2.36, 95% CI 1.94–2.86; AORlow poverty 1.67, 95% CI 1.42–1.96).
SMM Without Blood Transfusion
A sensitivity analysis was conducted to compare adjusted effect estimates for each variable on SMM with or without blood transfusion (Table S3). While there was a significant increase in SMM occurrence for every year compared to 2008, there was a negligible difference across years for SMM without blood transfusion. In addition, we found significant effect differences across outcomes for maternal age and heart disease. Older women had significantly higher SMM risk with or without blood transfusion compared to 25–29 year olds. Yet the effect size among older age groups (30–34, 35–39 and 40 + years) was significantly greater for SMM without blood transfusion. Similarly, while heart disease significantly increased SMM risk with or without blood transfusion compared to no heart disease, the magnitude of the effect of heart disease was significantly greater for SMM without blood transfusion (AOR 5.21, 95% CI 4.17–6.51) compared to SMM with blood transfusion (AOR 3.25, 95% CI 2.70–3.92).
Conclusions for Practice
Overall, approximately 13,500 women experienced SMM during delivery in NYC from 2008 to 2012, at a rate almost two times higher than national estimates. SMM risk in NYC was associated with several demographic, socioeconomic, health variables. Similar to previous studies in both NYC and other settings, racial/ethnic disparities were persistent after adjusting for other factors (Creanga et al. 2014). All racial/ethnic groups had higher SMM risk than white non-Latina women and the greatest risk was found among black non-Latina women. A recent analysis found that between 38 and 48% of this racial/ethnic disparity in SMM rates in NYC could be attributed to differences in site of delivery, with clustering of deliveries among black non-Latina and Latina women in facilities with higher SMM rates (Howell et al. 2016b, 2017).
Building on this evidence, our analysis indicates that while socioeconomic status has some modifying effect on racial/ethnic differences in SMM, disparities persist even at higher education, individual-, and neighborhood-income levels. For Latina and Asian-Pacific Islanders, lower income significantly increased SMM risk compared to White non-Latinas, suggesting eligibility and by proxy, individual-level income, plays a role in reducing, but not eliminating, the SMM risk difference with white non-Latinas. Neighborhood-level poverty also significantly modified SMM risk for both Latina and black non-Latina women. This difference in risk between high and low poverty neighborhoods points to the role of broader physical, social, and environmental conditions. Research suggests that exposure to these environments can increase chronic stress and susceptibility to disease during pregnancy (Louis et al. 2015).
While education and income variables accounted for some of the elevated risk in SMM, disparities persisted across all socioeconomic variables, suggesting the need for other explanations or pathways. A focus on structural racism, including factors such as residential segregation or differential health care quality and access, is increasingly being used in public health as a way to advance health equity research (Bailey et al. 2017). Indeed, institutional disadvantage for black non-Latina and Latina women in health services has been shown to exacerbate racial disparities in maternal and infant health outcomes particularly for women living in the poorest neighborhoods (Bailey et al. 2017; Howell et al. 2016a, b, 2017; Louis et al. 2015). The complex inter-relationship of facility, neighborhood, and individual characteristics on SMM risk and its racial/ethnic differences merits further investigation, including an examination of where women deliver in combination with the full range of other social determinants of health. Studies that measure early life or chronic exposure to poverty may also capture the cumulative effect of socioeconomic status over the life course, considered an important driver of racial disparities in maternal health (Louis et al. 2015). Such evidence is critical to inform program and policy interventions aimed at eliminating preventable maternal mortality and SMM in NYC.
Results should be viewed in light of some limitations. First, the proportion of birth certificate and hospital discharge records that matched was as low as 91.3% in 2009, resulting in fewer multiple births and Asian and Pacific Islanders in that year. Second, the matched dataset did not include other types of pregnancy outcomes that were part of national studies (e.g., stillbirths), potentially underestimating the SMM rate in NYC. Third, individual income was not collected directly; instead, we used Medicaid eligibility as a proxy, which in New York is set at 223% of household income, or approximately $35,524 for a household of two (pregnant women count as two)(New York State Department of Health 2015). Fourth, studies suggest the CDC algorithm has low to moderate positive predictive value, largely due to non-specific blood transfusion codes (Main et al. 2016; Sigakis et al. 2016). Our sensitivity analysis of SMM without blood transfusions indicated stronger effects of age and heart disease compared to the standard SMM definition. SMM risk also increased from 2008 to 2012 using the standard SMM definition compared to SMM without blood transfusion, mirroring national trends (Centers for Disease Control and Prevention 2017). Fifth, correlation between neighborhood-level variables and facility random effects may have biased the findings; however, previous literature has demonstrated that women’s preference for delivery facility is not limited to geographic proximity (Hebert et al. 2011). Furthermore, a recent study demonstrated that the majority of the clustering of SMM occurs at the facility-level, not the neighborhood-level (Guglielminotti et al. 2018). Finally, neighborhood-level poverty defined at the community district may not capture heterogeneity over a relatively large geographic unit.
Conclusion
In conclusion, population-based surveillance of SMM based on administrative hospital discharge data is an important way to identify high risk populations and investigate modifiable risk factors for poor maternal health outcomes at a state or regional level. This study found important demographic and health determinants associated with an increased risk of SMM in NYC. Moreover, racial disparities in SMM were persistent even after controlling for other variables, and were only partially explained by differences in education and income levels. While higher socioeconomic status might be expected to reduce SMM risk differences among racial/ethnic groups, other pathways, particularly structural racism and its effect on neighborhoods and health care quality and access, should be explored.
References
Anderson, N. B., Bulatao, R. A., & Cohen, B. (Eds.). (2014). Race/ethnicity, socioeconomic status, and health. In Critical perspectives on racial and ethnic differences in health in late life. Washington, DC: National Academies Press (US).
Bailey, Z. D., Krieger, N., Agénor, M., Graves, J., Linos, N., & Bassett, M. T. (2017). Structural racism and health inequities in the USA: Evidence and interventions. The Lancet. 389(10077), 1453–1463.
Callaghan, W. M., Creanga, A. A., & Kuklina, E. V. (2012). Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstetrics & Gynecology, 120(5), 1029–1036.
Centers for Disease Control and Prevention. (2017). Severe Maternal Morbidity in the United States. Retrieved from https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html.
Creanga, A. A., Bateman, B. T., Kuklina, E. V., & Callaghan, W. M. (2014). Racial and ethnic disparities in severe maternal morbidity: A multistate analysis, 2008–2010. American Journal of Obstetrics and Gynecology, 210(5), 435.e431–435.e438. https://doi.org/10.1016/j.ajog.2013.11.039.
Gray, K. E., Wallace, E. R., Nelson, K. R., Reed, S. D., & Schiff, M. A. (2012). Population-based study of risk factors for severe maternal morbidity. Paediatric and Perinatal Epidemiology, 26(6), 506–514. https://doi.org/10.1111/ppe.12011.
Guglielminotti, J., Landau, R., Wong, C. A., & Li, G. (2018). Patient-, hospital-, and neighborhood-level factors associated with severe maternal morbidity during childbirth: A cross-sectional study in New York State 2013–2014. Maternal and Child Health Journal. https://doi.org/10.1007/s10995-018-2596-9.
Herbert, P. L., Chassin, M. R., & Howell, E. A. (2011). The contributioni of geography to black/white differences in the use of low neonatal mortality hospitals in New York City. Medical Care, 49(2), 200–206. https://doi.org/10.1097/MLR.0b013e3182019144.
Howell, E. A., Egorova, N., Balbierz, A., Zeitlin, J., & Hebert, P. L. (2016a). Black-white differences in severe maternal morbidity and site of care. American Journal of Obstetrics and Gynecology, 214(1), 122.e121–122.e127. https://doi.org/10.1016/j.ajog.2015.08.019.
Howell, E. A., Egorova, N. N., Balbierz, A., Zeitlin, J., & Hebert, P. L. (2016b). Site of delivery contribution to black-white severe maternal morbidity disparity. American Journal of Obstetrics and Gynecology, 215(2), 143–152. https://doi.org/10.1016/j.ajog.2016.05.007.
Howell, E. A., Egorova, N. N., Janevic, T., Balbierz, A., Zeitlin, J., & Hebert, P. L. (2017). Severe maternal morbidity among Hispanic women in New York City: Investigation of health disparities. Obstetrics & Gynecology, 129(2), 285–294. https://doi.org/10.1097/aog.0000000000001864.
Howland, R. E., Madsen, A. M., Toprani, A., Gambatese, M., Mulready-Ward, C., & Begier, E. (2015). How well do birth records serve maternal and child health programs? Birth registration system evaluation, New York City, 2008–2011. Maternal and Child Health Journal, 19(7), 1559–1566. https://doi.org/10.1007/s10995-015-1664-7.
Louis, J. M., Menard, M. K., & Gee, R. E. (2015). Racial and ethnic disparities in maternal morbidity and mortality. Obstetrics & Gynecology, 125(3), 690–694. https://doi.org/10.1097/aog.0000000000000704.
Lu, M. C., Highsmith, K., de la Cruz, D., & Atrash, H. K. (2015). Putting the “M” back in the maternal and child health bureau: Reducing maternal mortality and morbidity. Maternal and Child Health Journal, 19(7), 1435–1439.
Main, E. K., Abreo, A., McNulty, J., Gilbert, W., McNally, C., Poeltler, D., et al. (2016). Measuring severe maternal morbidity: Validation of potential measures. American Journal of Obstetrics and Gynecology. 214(5), 643.e641–643.e610. https://doi.org/10.1016/j.ajog.2015.11.004.
New York City Department of City Planning. (n.d.). Community Portal. Retrived from https://www1.nyc.gov/site/planning/community/community-portal.page.
New York State Department of Health. (n.d.). Statewide Planning and Research Cooperative System (SPARCS). Retrieved from https://www.health.ny.gov/statistics/sparcs/.
New York State Department of Health. (2015). Medicaid (annual and monthly) income levels for pregnant women and children. Retrived from https://www.health.ny.gov/community/pregnancy/health_care/prenatal/income.htm.
Sigakis, M. J., Leffert, L. R., Mirzakhani, H., Sharawi, N., Rajala, B., Callaghan, W. M., et al. (2016). The Validity of discharge billing codes reflecting severe maternal morbidity. Anesthesia & Analgesia, 123(3), 731–738. https://doi.org/10.1213/ane.0000000000001436.
Williams, D. R., Mohammed, S. A., Leavell, J., & Collins, C. (2010). Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Annals of the New York Academy of Science, 1186, 69–101. https://doi.org/10.1111/j.1749-6632.2009.05339.x.
Acknowledgements
Data were prepared by New York State Bureau of Biometrics and Health Statistics and the New York City Department of Health and Mental Hygiene Office of Vital Statistics. This project was supported by a grant from the Merck for Mothers Program and managed by the Fund for Public Health in New York, Inc.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Howland, R.E., Angley, M., Won, S.H. et al. Determinants of Severe Maternal Morbidity and Its Racial/Ethnic Disparities in New York City, 2008–2012. Matern Child Health J 23, 346–355 (2019). https://doi.org/10.1007/s10995-018-2682-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-018-2682-z