Abstract
Background The incidence of severe maternal morbidity (SMM) during childbirth is increasing in the United States. A better characterization of risk factors for SMM may identify targets for improving maternal outcomes. This study aims to characterize patient-, hospital-, and neighborhood-level factors associated with SMM during childbirth. Methods SMM during childbirth was identified in the 2013–2014 State Inpatients Database for New York. Hospital and neighborhood characteristics were abstracted from the American Hospital Association and the Area Health Resources files. Multilevel modeling was used to identify factors associated with SMM, with and without blood transfusion, and its between-hospital variation. Results 403,116 delivery-related discharges from 139 hospitals were analyzed; 1557 (0.39%) recorded SMM without blood transfusion. In the final multilevel model, 7 patient-level factors were associated with a greater than fourfold increase in the risk of SMM: pulmonary hypertension, postpartum hemorrhage, placenta accreta, chronic kidney disease, cardiac conduction disorders, emergent cesarean delivery, and preeclampsia. Three hospital-level factors were associated with SMM: proportion of non-White patients, proportion of Medicaid beneficiaries, and coding intensity. No neighborhood-level factors were predictive of SMM. The proportion of variation in SMM explained by the model was 23.5 with 23.2% related to patient-level factors. The model explained 55% of the between-hospital variation, primarily related to patient-level factors. Similar results were observed for SMM with blood transfusion. Conclusions This study confirms the association between patient-level factors and SMM. It identifies patient-level factors as the major driver of between-hospital variation in SMM. Efforts to improve maternal outcomes should target patient-level factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Significance
Patient- but not hospital- and neighborhood-level factors significantly contribute to severe maternal morbidity during childbirth. Improvement in maternal outcomes should target patient-level factors.
Introduction
The number of reported pregnancy-related deaths in the United States has markedly increased during the las two decaded, from 11.1 to 17.3 deaths per 100,000 live births between 1993 and 2013, with very marked racial and ethnic disparities (Creanga et al. 2017). This increase prompted collaborative state- and nationwide initiatives to improve maternal outcomes, such as the California Maternal Quality Care Collaborative and the National Partnership for Maternal Safety (D’Alton et al. 2014). Severe maternal morbidity (SMM) during chilbirth is 100 times more frequent than mortality, with a continuum between morbidity and mortality. In addition, SMM is likely more amendable to successful interventions than events that result in death (Creanga et al. 2014). Similar to maternal mortality, the estimated incidence of severe maternal morbidity during childbirth is increasing; it has tripled between 1993 and 1994 and 2013–2014, from 0.48 to 1.42% (Centers for Disease Control and Prevention). Factors contributing to this disturbing trend include the increase in average maternal age, chronic maternal comorbidities, cesarean deliveries, and complications of pregnancy (Creanga et al. 2014).
Characterizating patient-, hospital-, and neighborhood-level factors associated with the development of SMM has the potential to lead to targeted interventions to improve maternal outcomes. To date, studies on factors associated with SMM have primarily examined patient-level factors. Socioeconomic and racial disparities, advanced maternal age, presence of chronic comorbidities, high-risk pregnancy, induction of labor, and cesarean delivery are well established risk factors for SMM (Creanga et al. 2014). Previous research suggests that some hospital-level factors are associated with SMM such as non-teaching status, low neonatal level-of-care designation, low volume of delivery, and high proportion of minority patients (Creanga et al. 2014; Kyser et al. 2012). In addition, the rate of SMM and other obstetrical outcomes vary considerably across hospitals (Creanga et al. 2014; Glance et al. 2014; Grobman et al. 2014). Factors associated with the between-hospital variation in SMM have been little examined (Glance et al. 2014; Grobman et al. 2014). Finally, data also suggest an association between SMM and some patient residency characteristics. For example, longer driving time from home to hospital or lower maternal-fetal medicine specialist density in the state of residence have been associated with increased neonatal and maternal mortality (Frolich et al. 2014; Ravelli et al. 2011; Sullivan et al. 2005). Analysis of adverse outcomes in women clustered within hospitals requires advanced statistical techniques taking into consideration correlation of women within hospitals, such as multilevel modeling. Multilevel modeling is also required to identify factors associated with the between hospital variation in SMM through analysis of the between hospital variance (Birkmeyer et al. 2006; Glance et al. 2014). This study aimed to characterize patient-, hospital- and neighborhood-level factors associated with SMM during childbirth and SMM variation among hospitals in New York State in 2013–2014.
Methods
The study protocol was reviewed by the Institutional Review Board of Columbia University Medical Center and was granted exemption under 45 Code of Federal Regulation 46 (not human subjects research). The Strengthening The Reporting of OBservational studies in Epidemiology (STROBE) and the Reporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statements were followed.
Study Sample
The study sample consisted of all discharges indicating vaginal or cesarean delivery in New York State between January 1, 2013 and December 31, 2014. Hospital discharge records of the State Inpatient Databases (SID) for New York were analyzed. SID are part of the Healthcare Cost and Utilization Project sponsored by the Agency for Healthcare Research and Quality. They capture all inpatient discharges from non-federal acute care community hospitals. For each discharge, the SID include patient characteristics, Zone Improvement Plan (ZIP) and Federal Information Processing Standard (FIPS) state/county codes of patient residence, one hospital identifier, and up to 15 procedural and 25 diagnostic codes defined in the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). New York State ranks third for the annual number of births and is the largest HCUP state available. Hospital characteristics were obtained from the American Hospital Association (AHA) file 2013 and 2014, and patient county of residence characteristics from the Area Health Resources (AHRF) file 2015–2016 release, respectively. AHA and AHRF data were linked with SID patient-level data. We did not use the 2013–2014 HCUP National Inpatient Sample, a 20% representative sample of inpatient discharges records, because it does not allow linkage with other data sytems such as the AHA and AHRF files.
Delivery-related discharges were identified with a combination of ICD-9-CM diagnosis and procedure codes as previously described (Supplemental Digital Content Table S1) (Kuklina et al. 2008). Discharges were excluded if the hospital identifier was missing, if the ZIP or FIPS state/county codes of patient residence were missing or not located in New York State, or if the patient was transferred from another hospital.
Outcome Measures
The definition of SMM was adapted from the United States Centers for Disease Control and Prevention, which categorizes SMM as SMM with- or SMM without blood transfusion (Supplemental Digital Content Table S2). In this study, SMM included 22 conditions or procedures for which the hospital length-of-stay was greater than the 90th percentile (3 days for vaginal delivery and 5 days for cesarean delivery). The conditions and procedures were: (1) acute myocardial infarction or ischemia, (2) acute renal failure, (3) acute respiratory failure, (4) amniotic fluid embolism, (5) aortic aneurysm and dissection, (6) cardiac arrest, (7) disseminated intravascular coagulation, (8) eclampsia, (9) stroke, (10) heart failure, (11) anesthesia-related complications, (12) severe sepsis and septic shock, (13) sickle cell disease crisis, (14) pulmonary embolism, (15) air embolism, (16) pyemic and septic embolism, (19) hysterectomy, (20) tracheostomy, (21) mechanical ventilation, and (22) blood product transfusion.
Patient-Level Factors
The following patient-level factors were recorded directly from the SID: age, race or ethnicity, insurance type, median household income for patient residence ZIP code, admission for delivery during weekend, and admission type (elective or non-elective).
The following preexisting maternal conditions were identified with specific ICD-9-CM codes (Supplemental Digital Content Table S3): depression, bipolar disorders, drug use, smoking, diabetes mellitus, hypertension, pulmonary hypertension, heart valve disease, cardiac conduction disorders, obesity, asthma, chronic kidney disease, and chronic hepatitis (including viral hepatitis). The following pregnancy and delivery characteristics were also identified with specific ICD-9-CM codes (Supplemental Digital Content Table S4): gestational hypertension, preeclampsia, previous cesarean delivery, pregnancy resulting from assisted-reproductive technology, multiple gestation, abnormal presentation, fetal macrosomia, polyhydramnios, chorioamnionitis, placenta previa, placenta accreta, and postpartum hemorrhage. Preexisting maternal conditions or pregnancy characteristics with < 10 cases in discharges recording SMM were not included in the analysis.
Delivery was categorized as vaginal delivery after spontaneous labor, vaginal delivery after induced labor, non-emergent cesarean delivery, or emergent cesarean delivery. Labor, induction of labor and cesarean deliveries were identified with ICD-9-CM codes (Supplemental Digital Content Table S5). Emergent cesarean delivery was defined as a cesarean delivery with ICD-9-CM code indicating maternal and fetal conditions requiring urgent delivery (abnormal fetal heart rhythm, abruptio placenta, uterine rupture, umbilical cord prolapse, and placenta previa with hemorrhage).
Hospital-Level Factors
The following hospital characteristics were obtained from the SID: intensity of coding, annual volume of delivery, cesarean section rate, percent non-White patients, percent Medicaid/Medicare beneficiaries, and percent high-risk pregnancy. For each hospital, the intensity of coding was the mean number of diagnosis and procedure codes reported per discharge record. High-risk pregnancies were defined as a comorbidity index for obstetrics patients ≥ 2 (Bateman et al. 2013).
The following hospital characteristics were obtained from the AHA file: hospital location (rural or urban), teaching status, neonatal level-of-care designation (1, 2 or 3), resident- and nurse-to-bed ratio, and nurse mix. The following definitions were used. The resident (nurse)-to-bed ratio was the ratio of full-time equivalents (FTE) residents (nurses) to the number of hospital beds. The nurse mix was the proportion of FTE registered nurses among the total number of FTE registered nurses and licensed practical nurses.
Neighborhood-Level Factors
Patient residence type based on Urban Influence Codes (UIC) codes was obtained from the SID and categorized as large metropolitan areas (at least 1 million residents), small metropolitan areas (less than 1 million residents), micropolitan areas, and not metropolitan or micropolitan. The distance between the patient residence and hospital was calculated as the distance between the centroids of the hospital and patient ZIP codes.
The following patient county of residence characteristics were obtained from the AHRF file: number of gynecologists/obstetricians and anesthesiologists (per 10,000 deliveries); percent births of teenagers and unmarried women; percent female divorced, family with female head, and female without health insurance; percent population foreign born, with less than high school diploma, and non-White; median household income; percent unemployed, food stamp beneficiaries, and family below poverty level; percent house without phone and with more than 1 person per room; percent days with good quality air; death by homicide, AIDS, motor vehicle accident, and suicide (per 100,000 residents).
Statistical Analysis
Results are expressed as number (% or per 10,000), mean (1 standard deviation), or median (interquartile range). The statistical analysis was performed with R version 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria) and specifice packages (mice for multiple imputations).
Uni- and Multi-variable Analyses of Risk Factors for SMM
Univariable comparisons between discharges with and without SMM used Student’s t test for continuous variables and the Chi square test for categorical variables. Unadjusted odds ratios were calculated with univariable logistic regression.
To assess for clustering of patients within hospitals and within county of residence, the intraclass correlation coefficient (ICC) was calculated. An ICC greater than 5% is substantive evidence of a clustering effect. In the current study, the ICC for SMM without blood transfusion was 25.7% for hospital and < 1% for county of residence, and for SMM with blood transfusion, 26.3 and < 1%, respectively.
Multivariable analysis of risk factors for SMM used multilevel models. One model was developed for SMM without blood transfusion and one for SMM with blood transfusion. In these model, the fixed-effects included patient-, hospital-, and neighborhood-level factors with a P-value < 0.2 in the univariable analysis. The number of cesarean deliveries was not included because it was highly correlated with the number of deliveries (Pearson correlation coefficient > 0.9). The relationship between continuous candidate predictors and the risk of SMM was examined using the relationship between the predictor and the logarithm of the odds of SMM \(\left( {\log \frac{P}{{1 - P}}} \right)\). Continuous predictors with a nonlinear relationship were reduced to category data and predictors with a linear relationship remained continuous in the analysis. The random effect was the hospital identifier with the assumption of a normally distributed intercept and a constant slope. Multiple imputations were used to estimate missing data. The selection of variables used a backward procedure with a P-threshold of 0.05 for exclusion of variables. Performance of the model was assessed with the c-index, and a calibration plot.
The proportion of variation in SMM explained by the model was assessed with R2. To estimate the amount of variation in SMM attributed to patient-, hospital-, and neighborhood-level factors, successive multilevel models were built by successively adding patient-, hospital-, and neighborhood-level factors. The difference in R2 between successive models estimates the amount of variation explained by patient-, hospital-, and neighborhood-level factors.
Between-Hospital Variation in SMM
For each hospital, the indirectly standardized rate of SMM rate was calculated as the ratio of the observed to the expected (O/E) rates multiplied by the observed rate in the study sample. The expected rate was the mean of the individual probabilities of SMM for each hospital calculated with the final multilevel model.
To estimate the amount of variation in SMM among hospitals attributed to patient-, hospital-, and neighborhood-level factors, successive multilevel models were built. First, a model including the hospital identifier as a random effect was fitted. Patient-, hospital-, and neighborhood-level were successively added. The percent reduction in the standard deviation of the between-hospital variance between successive models estimates the amount of variation between hospitals related to patient-, hospital-, and neighborhood-level factors.
Results
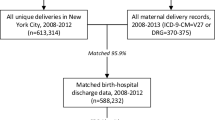
The final study sample included 403,116 delivery-related discharges from 139 hospitals (Fig. 1). Twenty-eight percent of women delivered in a hospital not located in their county of residence. Thirty-four percent of deliveries were cesarean deliveries and 8.6% were emergent cesarean deliveries. The most frequent indication for emergent cesarean delivery was abnormal fetal heart rhythm (92%).
SMM without blood transfusion was recorded in 1557 discharges (38.6 per 10,000; 95% CI 36.7–40.6) and SMM with blood transfusion in 2847 (70.6 per 10,000; 95% CI 68.1–73.3). The 3 most frequently recorded conditions and procedures were blood transfusion (46.8 per 10,000), heart failure (7.9 per 10,000), and disseminated intravascular coagulation (7.7 per 10,000) (Table 1).
Univariable and Multivariable Analysis of Risk Factors for SMM
In the univariable analyses comparing discharges with and without SMM, higher risk of SMM was observed in younger or older low-income minority women, women with preexisitng or pregnancy-related conditions, in women undergoing induction of labor or cesarean delivery, in women delivering in urban or teaching or level 3 hospitals, and in women living in deprived neighborhoods (Supplemental Digital Content Tables S6 and S7).
In the final multilevel model for SMM without blood transfusion (Table 2), 7 patient-level factors were associated with a greater than fourfold increase in the odds of SMM. They included pulmonary hypertension (adjusted odds ratio (aOR) 11.85), postpartum hemorrhage (aOR 11.37), placenta accreta (aOR 8.25), chronic kidney disease (aOR 7.46), cardiac conduction disorders (aOR 6.67), emergent cesarean delivery (aOR 4.86), and preeclampsia (aOR 4.56). Three hospital-level factors were associated with SMM: proportion of non-white patients (aOR 1.011 per 1% increase), proportion of Medicaid/Medicare beneficiaries (aOR 0.999 per 1% increase), and intensity of coding (aOR 1.19 per 1-point increase). No neighborhood-level factor was associated with SMM.
The total proportion of variation in SMM explained by the model (R2) was 23.5% (Table 3); 23.3% was related to patient-level factors. The c-index was 0.886 (95% CI 0.877–0.895), and calibration was good (Supplemental Digital Content Fig. 1).
Similar results were observed for SMM with blood transfusion (Tables 2, 3).
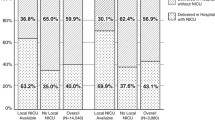
Between-Hospital Variation in SMM
Marked variation was observed across hospitals in SMM with a median indirectly standardized rate of SMM without blood transfusion of 37.5 per 10,000 (interquartile range: 24.2–43.4; extremes: 0–289.5). The model explained 55% of the between-hospital variation (Table 3) which was mostly accounted for by patient-level factors. Similar results were observed for SMM with blood transfusion. The model explained 50% of the between-hospital variation which was mostly explained by patient-level factors.
Discussion
In this study, we aimed to identify patient-, hospital- and neighborhood-level factors associated with in-hospital SMM and its variation across hospitals. These factors could be potential targets to develop interventions to improve maternal safety. We confirm the role of patient-level factors in the development of in-hospital SMM and report for the first time that patient-level factors are the major driver of the between-hospital variation in SMM. The 3 hospital-level factors accounted for a small proportion of the variation in SMM and we did not identify any neighborhood-level factors. Altogether, these findings indicate that improvement in maternal outcomes should focus on antepartum and intrapartum patient-level factors.
To the best of our knowledge, this study is the first to simultaneously analyse the association betwwen patient-,hospital-, and neighborhood-level factors and SMM using a very large study sample and multilevel modeling to account for the clusterd nature of the data. For the purpose of this study, we adapted the validated definition developed by the U.S. Centers for Disease Control and Prevention for nationwide surveillance purposes, associating specific conditions or procedures and an excessive length of hospital stay (Centers for Disease Control and Prevention). Similar to nation- and state-based studies, we identified blood transfusion, heart failure, and disseminated intravascular coagulation as the three most frequent conditions/procedures (Callaghan et al. 2012; Centers for Disease Control and Prevention; Creanga et al. 2015; Wanderer et al. 2013).
Increased morbidity and mortality is reported in mothers living in disadvantaged neighborhoods and in mothers with reduced access to health care such as those with longer driving time to hospitals (de Graaf et al. 2012; Frolich et al. 2014; Sullivan et al. 2005). We did not observe an association between SMM and a comprehensive panel of neighborhood-level characteristics, encompassing neighborhood deprivation, access to care (medical density, distance to hospital), and racial or migrant composition. A possible explanation for this finding is the availability of comprehensive health care throughout New York State. For example, the number of active physicians in this state is 1.4 times the mean U.S. value (394 versus 273 per 100,000 residents, respectively). Similarly, the proportion of women of reproductive age residing within 30-min driving times to the nearest hospital offering perinatal services is 94% in New York State compared with 87% in the United States overall (Brown et al. 2014; Rayburn et al. 2012). Another possible explanation is that our analysis examined the narrow time-period of hospitalization for delivery. We cannot exclude that neighborhood deprivation or access to health care has an influence on morbid events occurring outside the secured hospital environment such as during pregnancy or after discharge (de Graaf et al. 2013; Posthumus et al. 2016).
A higher proportion of minority women, lower proportion of Medicaid beneficiaries, and higher intensity of coding were the three hospital-level factors associated with an increased risk of SMM. Neither structural characteristic (e.g. neonatal level-of-care designation or teaching status), nor staffing pattern (e.g. nurse-to-bed ratio) or volume of delivery were associated with SMM. This finding suggests, as recently outlined, that “once in the hospital, the level of care women receive is generally superb” (Clark and Belfort 2017). Our results seems to contradict the recent study by Howell et al. in New York City who reported a lower risk of SMM in teaching hospitals, hospitals with level 3 or 4 nurseries, private ownership and high delivery volume (Howell et al. 2016b). The study examined a small number of hospitals (40) and a small number of patient- and hospital-level factors, which may explain this discrepancy.
Worse maternal outcomes have been reported in women who deliver in hospitals serving primarily ethnic minority patients (Creanga et al. 2014). These hospitals have been arbitrarily defined as hospitals in which the proportion of deliveries of ethnic minority patients is greater than 50%. Our results indicate that this dichotomization is an oversimplification and that the actual proportion of minority patients should be considered when comparing maternal outcomes across hospitals. Mechanisms underlying worse outcomes in minority-serving hospitals are poorly understood. Recent research suggests that minority patients may seek care in lower quality hospitals (Howell et al. 2016a, b).
The influence of insurance type on patient outcomes within the same hospital has been recently examined in nonobstetric patients (Spencer et al. 2013, 2015). On average, lower mortality rates are observed in Medicaid beneficiaries for medical conditions such as congestive heart failure, stroke or pneumonia. We extend this finding to obstetric patients and SMM. The reasons for improved maternal outcome in hospitals with a high proportion of Medicaid beneficiaries is unclear but research suggests that Medicaid status may improve utilization of antenatal care (Anum et al. 2010; Howell et al. 1991).
Rates of complications based on administrative data depend on the intensity of ICD-9-CM coding in discharge records. Coding indensity displays between-hospital and geographical variations (Finkelstein et al. 2017). Our results indicate that comparison of performance across hospitals should be adjusted for the intensity of coding (Guglielminotti et al. 2016).
In this study, patient-level factors were the main determinant of the variation in SMM explained and in the variation in SMM among hospitals. This suggests that efforts to reduce SMM and its between-hospital variation should address patient-level factors. A greater than fourfold increase in the risk of SMM was observed for seven factors, including three preexisting conditions (pulmonary hypertension, cardiac conduction disorders, and chronic kidney disease), two pregnancy-associated conditions (preeclampsia, placenta accreta), and two delivery characteristics (emergent cesarean delivery, postpartum hemorrhage). The contribution of preexisting maternal conditions, especially heart disease, to SMM reemphasizes the need for preconception counseling of these high-risk women and close monitoring during pregnancy and labor in hospitals that can adress their health needs. Cardiovascular conditions are now the leading cause of ICU admission and maternal death in the United States (Creanga et al. 2017; Kuklina and Callaghan 2011). The American College of Obstetricians and Gynecologists intoduced levels of maternal care in 2016 with the aim to provide uniform designations that are complementary but distinct from levels of neonatal care and that address maternal health needs, thereby reducing maternal morbidity and mortality (The American College of Obstetricians and Gynecologists & The Society for Maternal Fetal Medicine 2015).
Our study also confirms the maternal risks associated with hypertensive disorder of pregnancy and postpartum hemorrhage and confirms the choice of the National Partnership for Maternal Safety to target these two conditions (D’Alton et al. 2014). The increased risk of SMM associated with placenta accreta and emergent cesarean delivery, highlights the American College of Obstetricians and Gynecologists’ recommendations on the prevention of not-clinically indicated cesarean delivery, including decision-making based on fetal heart rhythm (American College of Obstetricians Gynecologists and Society for Maternal-Fetal Medicine 2014).
There are limitations to our study. First, our analysis was restricted to delivery hospitalizations and excluded postpartum hospitalizations. In addition to underestimating SMM rate by excluding postpartum hospitalizations, we could not determine whether risk factors for SMM during postpartum hospitalizations, especially neighborhood-level factors, differ from risk factors during delivery hospitalizations. Second, the analysis was limited to New York State and our findings may not be generalizable to the rest of the country. Socioeconomic characteristics of New York State are different from the rest of the United States and may influence maternal outcomes. For example, New York State has a higher proportion of non-White population compared with the US average (43 vs. 39%) and a lower proportion of uninsured (6 vs. 9%). Third, administrative data are for billing purpose and not as accurate as individual chart review to identify women comorbidites or outcomes. In addition, some factors that also contribute to maternal morbidity are not availbale in these data. It includes the education level, quality of antenatal care (e.g., start of antenatal care during pregnancy or number of antenatal visits), and process of care and delivery unit management practices in each hospital (Howell et al. 2014; Plough et al. 2017). It may explain why our model explained only 23% of the variation in SMM observed, suggesting that we did not identify the majority of factor that contribute to SMM. Finally, the assignment of certain characteristics as patient level is questionable. For example race and socioeconmomic status are individual indicators of macro social forces.
In conclusion, this study confirms the association between patient-level factors and SMM during childbirth. It identifies these factors as the major driver of between-hospital variation in SMM. Improvement of maternal outcomes should target the seven patient-level factors identified in this study.
References
American College of Obstetricians Gynecologists and Society for Maternal-Fetal Medicine. (2014). Obstetric care consensus no. 1: Safe prevention of the primary cesarean delivery. Obstetrics and Gynecology, 123(3), 693–711.
Anum, E. A., Retchin, S. M., Garland, S. L., & Strauss, J. F. 3rd (2010). Medicaid and preterm births in Virginia: An analysis of recent outcomes. Journal of Women’s Health (Larchmt), 19(11), 1969–1975.
Bateman, B. T., Mhyre, J. M., Hernandez-Diaz, S., Huybrechts, K. F., Fischer, M. A., Creanga, A. A., Callaghan, W. M., & Gagne, J. J. (2013). Development of a comorbidity index for use in obstetric patients. Obstetrics and Gynecology, 122(5), 957–965.
Birkmeyer, J. D., Dimick, J. B., & Staiger, D. O. (2006). Operative mortality and procedure volume as predictors of subsequent hospital performance. Annals of Surgery, 243(3), 411–417.
Brown, S. A., Richards, M. E., Elwell, E. C., & Rayburn, W. F. (2014). Geographical information systems for mapping maternal ground transport to level III care neonatal centers. American Journal of Perinatology, 31(4), 287–292.
Callaghan, W. M., Creanga, A. A., & Kuklina, E. V. (2012). Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstetrics and Gynecology, 120(5), 1029–1036.
Centers for Disease Control and Prevention. Severe maternal morbidity in the United States. Retrieved from http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/SevereMaternalMorbidity.html.
Clark, S. L., & Belfort, M. A. (2017). The case for a national maternal mortality review committee. Obstetrics and Gynecology, 130(1), 198–202.
Creanga, A. A., Bateman, B. T., Kuklina, E. V., & Callaghan, W. M. (2014). Racial and ethnic disparities in severe maternal morbidity: A multistate analysis, 2008–2010. American Journal of Obstetrics & Gynecology, 210(5), 435, e431–e438.
Creanga, A. A., Bateman, B. T., Mhyre, J. M., Kuklina, E., Shilkrut, A., & Callaghan, W. M. (2014). Performance of racial and ethnic minority-serving hospitals on delivery-related indicators. American Journal of Obstetrics & Gynecology, 211(6), 647, e641–e616.
Creanga, A. A., Berg, C. J., Ko, J. Y., Farr, S. L., Tong, V. T., Bruce, F. C., & Callaghan, W. M. (2014). Maternal mortality and morbidity in the United States: Where are we now? Journal of Women’s Health (Larchmt), 23(1), 3–9.
Creanga, A. A., Berg, C. J., Syverson, C., Seed, K., Bruce, F. C., & Callaghan, W. M. (2015). Pregnancy-related mortality in the United States, 2006–2010. Obstetrics and Gynecology, 125(1), 5–12.
Creanga, A. A., Syverson, C., Seed, K., & Callaghan, W. M. (2017). Pregnancy-related mortality in the United States, 2011–2013. Obstetrics and Gynecology, 130(2), 366–373.
D’Alton, M. E., Main, E. K., Menard, M. K., & Levy, B. S. (2014). The national partnership for maternal safety. Obstetrics and Gynecology, 123(5), 973–977.
de Graaf, J. P., Schutte, J. M., Poeran, J. J., van Roosmalen, J., Bonsel, G. J., & Steegers, E. A. (2012). Regional differences in Dutch maternal mortality. BJOG, 119(5), 582–588.
de Graaf, J. P., Steegers, E. A., & Bonsel, G. J. (2013). Inequalities in perinatal and maternal health. Current Opinion in Obstetrics and Gynecoly, 25(2), 98–108.
Finkelstein, A., Gentzkow, M., Hull, P., & Williams, H. (2017). Adjusting risk adjustment—accounting for variation in diagnostic intensity. The New England Journal of Medicine, 376(7), 608–610.
Frolich, M. A., Banks, C., Brooks, A., Sellers, A., Swain, R., & Cooper, L. (2014). Why do pregnant women die? A review of maternal deaths from 1990 to 2010 at the University of Alabama at Birmingham. Anesthesia and Analgesia, 119(5), 1135–1139.
Glance, L. G., Dick, A. W., Glantz, J. C., Wissler, R. N., Qian, F., Marroquin, B. M., Mukamel, D. B., & Kellermann, A. L. (2014). Rates of major obstetrical complications vary almost fivefold among US hospitals. Health Affairs, 33(8), 1330–1336.
Glance, L. G., Mukamel, D. B., Osler, T. M., & Dick, A. W. (2014). Ranking trauma center quality: Can past performance predict future performance? Annals of Surgery, 259(4), 682–686.
Grobman, W. A., Bailit, J. L., Rice, M. M., Wapner, R. J., Varner, M. W., Thorp, J. M. Jr.,. Leveno, K. J., Caritis, S. N., Iams, J. D., Tita, A. T., Saade, G., Sorokin, Y., Rouse, D. J., Tolosa, J. E., & Van Dorsten, J. P. & Eunice Kennedy Shriver National Institute of Child Health Human Development Maternal-Fetal Medicine Units Network. (2014). Can differences in obstetric outcomes be explained by differences in the care provided? The MFMU Network APEX study. American Journal of Obstetrics & Gynecology, 211(2), 147 e141–e116.
Guglielminotti, J., Deneux-Tharaux, C., Wong, C. A., & Li, G. (2016). Hospital-level factors associated with anesthesia-related adverse events in cesarean deliveries, New York State, 2009–2011. Anesthesia and Analgesia, 122(6), 1947–1956.
Howell, E. A., Egorova, N., Balbierz, A., Zeitlin, J., & Hebert, P. L. (2016a). Black-white differences in severe maternal morbidity and site of care. American Journal of Obstetrics & Gynecology, 214(1), 122, e121–e127.
Howell, E. A., Egorova, N. N., Balbierz, A., Zeitlin, J., & Hebert, P. L. (2016b). Site of delivery contribution to black-white severe maternal morbidity disparity. American Journal of Obstetrics & Gynecology, 215(2), 143–152.
Howell, E. A., Zeitlin, J., Hebert, P. L., Balbierz, A., & Egorova, N. (2014). Association between hospital-level obstetric quality indicators and maternal and neonatal morbidity. JAMA, 312(15), 1531–1541.
Howell, E. M., Herz, E. J., Wang, R. H., & Hirsch, M. B. (1991). A comparison of medicaid and non-medicaid obstetrical care in California. Health Care Financing Review, 12(4), 1–15.
Kuklina, E., & Callaghan, W. (2011). Chronic heart disease and severe obstetric morbidity among hospitalisations for pregnancy in the USA: 1995–2006. BJOG, 118(3), 345–352.
Kuklina, E. V., Whiteman, M. K., Hillis, S. D., Jamieson, D. J., Meikle, S. F., Posner, S. F., & Marchbanks, P. A. (2008). An enhanced method for identifying obstetric deliveries: Implications for estimating maternal morbidity. Maternal and Child Health Journal, 12(4), 469–477.
Kyser, K. L., Lu, X., Santillan, D. A., Santillan, M. K., Hunter, S. K., Cahill, A. G., & Cram, P. (2012). The association between hospital obstetrical volume and maternal postpartum complications. American Journal of Obstetrics & Gynecology, 207(1), 42, e41-17.
Plough, A. C., Galvin, G., Li, Z., Lipsitz, S. R., Alidina, S., Henrich, N. J., Hirschhorn, L. R., Berry, W. R., Gawande, A. A., Peter, D., McDonald, R., Caldwell, D. L., Muri, J. H., Bingham, D., Caughey, A. B., Declercq, E. R., & Shah, N. T. (2017). Relationship between labor and delivery unit management practices and maternal outcomes. Obstetrics and Gynecology, 130(2), 358–365.
Posthumus, A. G., Borsboom, G. J., Poeran, J., Steegers, E. A., & Bonsel, G. J. (2016). Geographical, ethnic and socio-economic differences in utilization of obstetric care in the Netherlands. PLoS ONE, 11(6), e0156621.
Ravelli, A. C., Jager, K. J., de Groot, M. H., Erwich, J. J., Rijninks-van Driel, G. C., Tromp, M., Eskes, M., Abu-Hanna, A., & Mol, B. W. (2011). Travel time from home to hospital and adverse perinatal outcomes in women at term in the Netherlands. BJOG, 118(4), 457–465.
Rayburn, W. F., Richards, M. E., & Elwell, E. C. (2012). Drive times to hospitals with perinatal care in the United States. Obstetrics and Gynecology, 119(3), 611–616.
Spencer, C. S., Gaskin, D. J., & Roberts, E. T. (2013). The quality of care delivered to patients within the same hospital varies by insurance type. Health Affairs, 32(10), 1731–1739.
Spencer, C. S., Roberts, E. T., & Gaskin, D. J. (2015). Differences in the rates of patient safety events by payer: Implications for providers and policymakers. Medical Care, 53(6), 524–529.
Sullivan, S. A., Hill, E. G., Newman, R. B., & Menard, M. K. (2005). Maternal-fetal medicine specialist density is inversely associated with maternal mortality ratios. American Journal of Obstetrics & Gynecology, 193(3 Pt 2), 1083–1088.
The American College of Obstetricians and Gynecologists, & The Society for Maternal Fetal Medicine. (2015). Obstetric care consensus No. 2: Levels of maternal care. Obstetrics and Gynecology, 125(2), 502–515.
Wanderer, J. P., Leffert, L. R., Mhyre, J. M., Kuklina, E. V., Callaghan, W. M., & Bateman, B. T. (2013). Epidemiology of obstetric-related ICU admissions in Maryland: 1999–2008. Critical Care Medicine, 41(8), 1844–1852.
Funding
Support was provided solely from institutional and/or departmental sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Guglielminotti, J., Landau, R., Wong, C.A. et al. Patient-, Hospital-, and Neighborhood-Level Factors Associated with Severe Maternal Morbidity During Childbirth: A Cross-Sectional Study in New York State 2013–2014. Matern Child Health J 23, 82–91 (2019). https://doi.org/10.1007/s10995-018-2596-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-018-2596-9