Abstract
Neurotensin receptors are overexpressed in several human tumors and can be targets for tumors diagnosis and therapy. In this study, a new neurotensin analogue was labeled with 99mTc via HYNIC and tricine/EDDA as coligands and investigated further. [HYNIC0, Gly7, Lys9, d-Tyr11]-Neurotensin (7–13) was synthesized using a standard Fmoc strategy. Labeling with 99mTc was performed at 100 °C for 10 min and radiochemical analysis involved ITLC and HPLC methods. The stability of radiopeptide was checked in the presence of humane serum at 37 °C up to 24 h. The receptor bound internalization and externalization rates were studied in neurotensin receptor expressing HT-29 cells. Biodistribution of radiopeptide was studied in nude mice bearing HT-29 tumor. Labeling yield of 98.6 ± 0.54 % (n = 3) was obtained corresponding to a specific activity of 81 MBq/nmol. Peptide conjugate showed good stability in the presence of human serum. The radioligand showed specific internalization into HT-29 cells (12.43 ± 0.52 % at 4 h). In biodistribution studies, a receptor-specific uptake was observed in neurotensin receptor positive organs so that after 1 h the uptakes in mouse intestine and tumor were 0.87 ± 0.16 and 0.63 ± 0.12 % ID/g respectively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Peptides are potential vectors for tumor targeting as their receptors can be overexpressed in different human tumors [1]. These receptors have become important and useful as targets for molecular imaging and therapy of tumors [2, 3]. Several receptors such as somatostatin, neurotensin and bombesin receptors have attracted considerable interest in recent years [4]. Neurotensin (NT) is a tridecapeptide localized in central nervous system and in peripheral tissues. Three different receptor subtypes for neurotensin (NTR1, NTR2 and NTR3) have been described [5, 6]. NT receptors, in particular the first one with high affinity binding for NT, are expressed in several human tumors such as small cell lung cancer and colon, pancreatic and prostate carcinomas [7]. Due to the high incidence and density of NT receptors in exocrine pancreatic carcinomas, NT is considered the best possible candidate for peptide based diagnosis or therapy of these tumors [8]. Over 75 % of all ductal pancreatic carcinomas were reported to overexpress NT receptors, whereas normal pancreas tissue, pancreatitis and endocrine pancreas devoid of NT receptors [9]. Since pancreas carcinoma is among the most frequent causes of cancer deaths, the need to use new radiopharmaceuticals which are able to diagnose cancer in the early steps is evident.
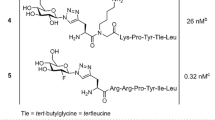
In the use of NT, the main drawback is its extremely short half life due to very rapid cleavage by different peptidases. The C-terminal hexapeptide fragment NT (8–13) is slightly more stable while contains the amino acids essential for binding NT receptors. However, this peptide can be easily broken down and metabolized in plasma by endogenous peptidases, thus reducing their biological activity on physiologic surrounding [10]. To change this situation, various NT analogues have been synthesized, including linear peptides [10–12], cyclic peptides [13], and nonpeptide molecules [14]. It is known that two main cleavage bonds (Arg8–Arg9 and Tyr11–Ile12) play an important role in the stability of NT (8–13) [15, 16]. Garcia-Garayoa et al. [17] designed a series of analogues to enhance the biological properties of NT by offering a double stabilization of the cleavage sites. Heyl et al. [18] modified NT (8–13) through N-methylation of Arg8 and replacement of Arg9 by Lys and Ile12 by Tle.
NT analogs have been radiolabeled with different radionuclides including 111In [19], 18F [20], 105Rh [21], 188Re [22] and 99mTc [23]. 99mTc based conjugates of NT and other peptide derivatives continue to be attractive due to the availability of low cost 99Mo/99mTc generator, favorable physical characteristics of 99mTc (t 1/2 of 6 h, γ 140 keV 89 % abundance) and high specific activity of radionuclide. Recently, several new NT conjugates radiolabeled with 99mTc have been reported [23]. Radiolabeling has been performed indirectly via a ligand including N3S [24], N4 [25], hydrazino nicotinic acid (HYNIC) [24] and carbonyl [17]. We should consider various limitations are associated with some of the above labeling procedure, such as low radiochemical yield, extended reaction time, high temperature, high pH values, and high lipophilicity of the radiometal chelate. For example in 99mTc-carbonyl approach, although 99mTc-carbonyl commercial kits currently are readily available, consideration of the two steps preparation and the further purification of the final product seem to be unsuitable for its routine uses in the nuclear medicine centers.
In recent years one of the bifunctional chelating ligand that has received considerable interest is HYNIC. The use of the 99mTc–HYNIC core was first reported for the labeling of IgG and since then, has been conjugated to various biomolecules including antibodies and peptides [26]. Since HYNIC could only occupy one or two coordination position on the radionuclide, coligands are necessary to complete the coordination sphere of the technetium core [27]. Usually a co-ligand, such as tricine or ethylenediamine diacetic acid (EDDA), is included in the 99mTc labeling of HYNIC conjugates. The co-ligand can sometimes play an important role in the stability, lipophilicity, clearance property and protein binding potency of the radiolabels. For example, while providing higher labeling efficiency, the tricine coligand also provides higher non-specific protein binding potential over the EDDA complexes. In labeling process coligands tricine and EDDA can be used separately or together via exchange labeling method. Teodoro et al. [24] recently evaluated the radiochemical and biological behavior of NT (8–13) analogue radiolabeled with 99mTc, using HYNIC and NHS–S–acetyl–MAG3 as chelator agents. They demonstrated that HYNIC seems to be a good choice since a very high stability as well as a predominantly renal excretion was observed.
We also recently reported the evaluation of a new somatostatin and bombesin analogues labeled via bifunctional chelating agents HYNIC and EDDA/tricine as coligands [28–30]. In continuation of our efforts to create a new 99mTc-labelled peptide for tumor targeting we chosed a NT (8–13) and a Gly7 as a spacer was between HYNIC and N-terminus of the peptide. We also modified Lys9 and d-Tyr11 instead of Arg9 and Tyr11 respectively to decrease enzymatic metabolism.
Here we present data on the synthesis of [HYNIC0, Gly7, Lys9, d-Tyr11]-Neurotensin (7–13) and describe optimum condition for radiolabeling of conjugate with 99mTc using tricine/EDDA as coligands. In addition we studied stability in human serum, receptor bound internalization and in vivo tumor uptake and tissue biodistribution of radiolabeled compound.
Experimental
Materials and methods
2-Chlorotrityl chloride resin and all of the Fmoc-protected amino acids were commercially available from NovaBiochem (Laufelfingen, Switzerland). The prochelator HYNIC–Boc was synthesized according to Abrams et al. [26]. Other reagents were purchased from Fluka, and used without further purification.
The reactive side chains of the amino acids were masked with one of the following groups: Lys, tert-butoxycarbonyl (Boc); Tyr, tert-butyl (tBu); Arg, 2,2,4,6,7-pentamethyl-dihydrobenzofurane-5-sulfonyl (pbf). The cell culture medium was Roswell Park Memorial Institute (RPMI-1640) supplemented with 10 % fetal bovine serum (FBS), amino acids, vitamins and penicillin/streptomycin from Gibco. Sodium pertechnetate (Na99mTcO4) obtained from commercial 99Mo/99mTc generator (Radioisotope Division, Atomic Energy Organization of Iran). Analytical reverse phase high performance liquid chromatography (RP-HPLC) was performed on a JASCO 880-PU intelligent pump HPLC system equipped with a multiwavelength detector and a flow-through Raytest-Gabi γ-detector. CC 250/4.6 Nucleosil 120-5 C18 column from Teknokroma was used for analytical HPLC. The gradient systems consisted of 0.1 % trifluoroacetic acid/water (Solvent A) and acetonitrile (Solvent B). For analytical HPLC, Gradient I was used: 0 min 95 % A (5 % B), 5 min 95 % A (5 % B), 25 min 0 % A (100 % B), 27 min 0 % A (100 % B), 30 min 95 % A (5 % B), flow = 1 ml/min, λ = 280 nm. Mass spectrum was recorded on an Agilent 1100/Bruker Daltonic (Ion trap) VL instrument (LC/MS). Quantitative gamma counting was performed on an EG&G/ORTEC (Ametek; Advanced Measurement Technology Division) Model 4001M Mini Bin & Power Supply counter.
Synthesis
The peptide was synthesized by standard Fmoc solid phase synthesis on 2-chlorotrityl chloride resin with substitution, 1.4 mmol/g [31]. Coupling of each amino acid was performed in the presence of 3 mol excess of Fmoc-amino acid, 3 mol excess of N-hydroxybenzotriazole (HOBt), 3 mol excess of diisopropylcarbodiimide (DIC) and 5 mol excess of diisopropylethylamine (DIPEA) in dimethylformamide (DMF). Completeness of coupling reactions was monitored by the Kaiser test and the Fmoc groups were removed by adding 20 % piperidine in DMF. The fully protected peptide was cleaved from the resin with solution contain 20 % trifluoroethanol (TFE), 0.5 % trifluoroacetic acid (TFA), 0.5 % H2O in dichloromethane (DCM) and incubated at room temperature for 30 min. 1.2 mol HYNIC–Boc coupled with 1.2 molar of O-(7-azabenzotriazol-1-yl)-1, 1,3,3,tetramethyluronium hexafluorophosphate (HATU) and 3 mol excess of DIPEA in DMF to the N-terminus of the peptide. The amino acid side chains of the peptide HYNIC conjugate were also deprotected by treatment with a cocktail of TFA, triisopropylsilane and water (95:2.5:2.5). After removing the organic solvents in vacuum, the crude product was precipitated with cold petroleum ether and diisopropyl ether (50:50).
Purification
The crude peptide HYNIC conjugate was dissolved in water/methanol and purified by semi-preparative RP-HPLC. A VP 250/10 Nucleosil 100-5 C18 column was used for purification and the gradient system consisted of 0.1 % TFA/water (Solvent A) and acetonitrile (Solvent B) with the following program: 0 min 80 % A (20 % B), 2 min 80 % A (20 % B), 17 min 50 % A (50 % B), 19 min 0 % A (100 % B), 21 min 0 % A (100 % B), 25 min 80 %A (20 % B), flow = 2 ml/min, λ = 280 nm (Gradient II). After injection of crude peptide to HPLC and running the program each peak was accumulated as a separate fraction and the fraction regarding to our peptide conjugate was characterized by LC/MS which was dried and lyophilized.
Labeling with 99mTc
Labeling was performed based on our previous experience in labeling of peptides with 99mTc using HYNIC chelator [28–30]. Briefly a stock solution of HYNIC-peptide (concentration 1 mg/ml) was prepared by dissolving the peptide in distilled water. Radiolabeling of peptide was performed by adding 20 μl of the stock solution (20 μg of peptide), 15 mg of tricine and 5 mg of EDDA co-ligands in 0.5 ml of water. To this solution was added 40 μg SnCl2 (20 μl of 2 mg/ml SnCl2, 2H2O in nitrogen-purged 0.1 M HCl). Finally, 370-1,110 MBq of 99mTcO4 − in 0.5 ml saline was added to the solution and incubated for 10 min at 95 °C. After cooling down to room temperature the preparation was checked for bound and free 99mTc.
Radiochemical analysis
99mTc-labeled HYNIC-peptide was characterized by analytical RP-HPLC (Gradient I) and ITLC on silica gel 60 (Merck) using different mobile phases: 2-butanone for free 99mTcO4 − (R f = 1), 0.1 M sodium citrate (pH 5) to determine the non-peptide bound 99mTc coligand and 99mTcO4 − (R f = 1) and methanol/1 M ammonium acetate 1/1 for 99mTc colloid (R f = 0). The radioactivity was quantified by cutting the strip (1.5 × 10 cm2) into 1 cm pieces and counting in a well type gamma counter.
Protein binding, serum stability, and log P values
In order to evaluate structural conformational changes and transchelation between coligands and proteins, which bound to serum proteins the precipitation method was used. To a 1 ml of freshly prepared human serum, we added 86 MBq 99mTc–HYNIC-peptide and mixture was incubated in 37 °C environment. At different time points, 100 μl aliquots was removed and treated with 100 μl of alcohol. Sample was centrifuged for 5 min at 3,000 rpm to precipitate serum proteins. Supernatant was removed and activity in the supernatant was compared with the activity in sediment to give the percentage of radiopeptide or radiometal which is bound or transferred to the serum proteins. Supernatant was analyzed with HPLC Gradient I to determine the stability of labeled compound.
For partition coefficient, 0.5 ml of the 99mTc labeled peptide in PBS was mixed with 0.5 ml of octanol in a 2 ml micro tube. The tube was vigorously vortexed over a period of 10 min and centrifuged at 4,000×g for 5 min. Three aliquots of 100 μl were sampled from each layer and counted in the γ counter. The averaged activities from the aqueous and the octanol layers were used to calculate the log P values. The octanol-to-water partition coefficient (P o/w) of the radiolabeled peptide was calculated by dividing the counts of the octanol phase by that of the aqueous phase.
Cell culture
The HT-29 cells were cultured in RPMI-1640 supplemented with 10 % FBS, 2 mM glutamine and penicillin–streptomycin. Cells were maintained in a humidified 5 % CO2/air atmosphere at 37 °C. For all cell experiments, the cells were seeded at a density of 1 million cells per well in six-well plates and incubated over night with internalization medium (RPMI with 1 % FBS).
Competition binding assay
The binding affinity of HYNIC-peptide was tested in a competition assay against 125I–NT as a radioligand. HT-29 cell membranes were used as a source for NT receptor. Membrane preparation was performed according to a published method [32]. In a multiscreen well plate, 50 μl competitor solution of increasing concentration (0.001–1,000 nM), 50 μl of radioligand solution (50,000 cpm) and 100 μl of membrane solution (50 μg protein/tube) were incubated in triplicate for 2 h at room temperature. Incubation was interrupted by filtration of the medium and rapid rinsing with 200 μl ice-cold washing buffer, followed by 50 μl 15 mM Tris–HCl buffer, pH 7.4 and filters were counted in a gamma counter. IC50 values were calculated following non-linear regression with Origin software (Microcal Origin 6.0).
Internalization/efflux
Medium was removed from the six-well plates contain HT-29 cells with density of 1 million cells per well and cells were washed once with 2 ml of internalization medium (RPMI with 1 % FBS). Furthermore, 1.5 ml internalization medium was added to each well, and the plates were incubated at 37 °C for about 1 h. Afterwards, about 150 kBq (2.5 pmol total peptide mass per well) was added to the medium, and the cells were incubated at 37 °C for various time periods. To determine nonspecific membrane binding and internalization, we incubated cells with the radioligand in the presence of 150 μl, 1 μmol/L NT. The cellular uptake was stopped at appropriate time periods (30 min, 1, 2 and 4 h) by removing medium from the cells and washing twice with 1 ml of ice-cold phosphate-buffered saline (PBS). An acid wash for 10 min with a glycine buffer (pH 2.8) on ice was also performed twice. This step was taken to distinguish between membrane-bound (acid releasable) and internalized (acid resistant) radioligand. Finally, the cells were treated with 1 N NaOH. The culture medium and the receptor-bound and internalized fractions for both with and without cold peptide were measured radiometrically in a gamma counter.
In connection to the release of the activity after maximal internalization and determination of the radioactivity which has remained in tumour cells the externalization of the maximal internalized activity was also measured. The HT-29 cells (106/well) were incubated with radioligand. After 2 h internalization at 37 °C and 5 % CO2, the medium was removed and the cells were washed twice with 1 ml ice cold PBS. Acid wash for a period of 5 min twice with a glycine buffer of pH 2.8 was done to remove the receptor bound ligand. Cells were then incubated again at 37 °C with fresh internalization medium. After different time points (15, 30 min, 1, 2 and 4 h), the external mediums were removed for quantification of radioactivity in a gamma counter. The cells were solubilized in 1 N NaOH and removed, and the internalized radioactivity was quantified in a gamma counter. The externalized fraction was expressed as percentage of the total internalized amount per 1 million cells.
Biodistribution
Animal experiments were performed in compliance with the regulations of our institution and with generally accepted guidelines governing such work. A suspension of human HT-29 cells (107) in PBS buffer was subcutaneously injected in the right flank of each nude mouse. Seven to ten days after inoculation, the tumors were inducted and then, an activity of 20 MBq (0.35 nmol) of 99mTc–HYNIC-peptide was injected via the femoral vein. In order to determine the non-specific uptake of the radiopeptides, in receptor-positive organs, a group of three animals were injected with 100 μg NT in 50 μl saline as a co-injection with the radiopeptides (blocked animals). After 1, 4 and 24 h, the mice in groups of three animals were killed, organs of interest were collected, weighed and radioactivity was measured in a gamma-counter. The percentage of the injected dose per gram (% ID/g) was calculated for each tissue.
Statistical methods
The calculations of means and standard deviations for internalization and biodistribution were performed on Microsoft Excel. Student’s t test was used to determine statistical significance. Differences at the 95 % confidence level (P < 0.05) were considered significant.
Results
Synthesis and purification
[HYNIC0, Gly7, Lys9, d-Tyr11]-Neurotensin (7–13) was synthesized by Fmoc strategy supplying an overall yield of 40 % based on the removal of the first Fmoc group after cleavage, purification and lyophilization (Fig. 1). The composition and structural identity of purified HYNIC-peptide was verified by analytical HPLC and LC–MS (Fig. 2; Table 1). The purity was >98 % as confirmed by HPLC method.
Radiolabeling
Radiochemical purity of 99mTc–HYNIC-peptide conjugate was evaluated by RP-HPLC using the gradient systems consisted of 0.1 % TFA/water (Solvent A) and acetonitrile (Solvent B). The labeling yield was 98.6 ± 0.54 % (n = 3), acquired via HPLC and also ITLC at a specific activity of 81 MBq/nmol. The HPLC elution times (Gradient I) were 4.28 min for free pertechnetate and 14.75 min for labeled peptide (Fig. 3).
Stability and lipophilicity
In serum protein binding studies, 22.2 ± 1.56 % of the activity was associated with the precipitate obtained after ethanol addition, indicating the low binding of complex with serum proteins due to transchelation. The complex was found to be stable in aqueous solution even after a 24 h period. The ethanol fraction was characterized by HPLC where a single peak was observed at the same time (>95 %) as that of the complex, indicating no decomposition of the complex was occurred. The partition coefficient for labeled compound was calculated (log P = −3.55 ± 0.23 %) which is good indicator of its high hydrophilicity.
Receptor binding and internalization
The in vitro competitive cell membrane binding assays demonstrated a high specificity and affinity for this analogue. The specific binding of 125I–NT was inhibited by increasing concentrations of HYNIC-peptide so that IC50 value of 1.86 ± 0.43 nmol/L was obtained. The result with respect to the time-dependent and specific internalization of the radioligand into HT-29 cells was shown in Fig. 4. The specific cell uptake after 1 h was 3.28 ± 0.45 %, which increased to 12.43 ± 0.52 % up to 4 h. In all experiments, the internalization was strongly reduced in the presence of excess cold. In fact, nonspecific internalization was 0.74 ± 0.18 % after 4 h, and the surface-bound peptide (acid removable) was 1.2 ± 0.33 % of the added activity after 4 h.
The externalization in HT-29 cells was evaluated after 2 h of the radioligand internalization (Fig. 5). After 15 min, 14.56 ± 1.21 % of radioactivity was externalized, and this amount increased to 45.52 ± 2.21 % up to 4 h which was the maximum and after that the percentage of externalization reaches a plateau. In other words approximately 55 % of the internalized activity remained inside the cells after 4 h. In comparison, a less stable compound shows a significant decrease of internalized activity at the very first hours. It can be due to a rapid degradation of the compound in the tumour cells. So, the more stable the compound, the higher the radioactivity retention.
Animal biodistribution
Results from biodistribution studies using the 99mTc-labeled peptide are presented in Table 2 as the percentage of injected dose per gram of tissue (% ID/g). 99mTc–HYNIC-peptide displayed rapid blood clearance with 0.42 ± 0.11 % ID/g at 1 h. Fast clearance from the NT receptor-negative tissues except the kidneys was found as well. Labeled peptide shows high uptake values in the HT-29 tumor and in the NT peptide receptor-positive organs. By blocking the receptor through prior injection of cold peptide, the uptake in intestine and tumor is diminished and this confirms the specificity of radioconjugate. Reduction uptake were 56 % (0.87 % ID/g vs. 0.38 % ID/g at 1 h) and 79 % (0.63 % ID/g vs. 0.13 % ID/g at 1 h) respectively (Fig. 6). On the other hand, the uptake reduction in non-targeted tissues due to blocking dose was not significant.
Discussion
Peptide receptors are overexpressed on various cancer cells and illustrate interesting targets for tumour imaging and therapy. NT receptors were overexpressed in a variety of human tumors such as breast, pancreatic, prostate, lung and colon. Based on this fact and the experience with other peptides like somatostatin [28, 33] and Bombesin [29, 30, 34, 35] we conclude that targeting the NT receptor with optimized analogue of NT is very important for imaging of pancreatic, lung and colon tumors. In the present study, we investigated a new HYNIC coupled analog with substitution of Lys8 instead of Arg8 and d-Tyr11 instead of Tyr11 in NT (8–13) sequences which lead to a substantial increase in metabolic stability. We attached HYNIC chelator via a Gly spacer to the N-terminus of NT (8–13) peptide which can be labeled with a more desirable radionuclide such as 99mTc.
A variety of chelators have been used as bifunctional chelating agent (BFCA) in labeling proteins, peptides and other biologically active molecule with 99mTc. These include N3S triamidethiols [36], N2S2 diamidedithiols [37], PnAo propyleneamine oxime [38], N4 tetramines [25], (N αHis)Ac Retro[N α-carboxymethyl-histidine] [17] and HYNIC [24, 33]. Among these, HYNIC is the best candidate because we can achieve labeling in high specific activity followed by using various coligands, which permit control of the hydrophilicity and pharmacokinetics of the labeled peptide [29, 30, 33–35, 39, 40]. In the group of different coligands, tricine gives the best radiolabeling efficiency. However, it have been reported that with tricine as a coligand 99mTc-complex was not stable, particularly in dilute solutions, due to different bonding modalities of the hydrazine moiety of the HYNIC and the tricine coligand [41]. The coligand EDDA is also of particular interest because it is a potentially tetradentate ligand and is expected to form a more symmetrical and stable complex with technetium when compared to tricine [41]. It has been shown that using both coligands together to produce 99mTc–HYNIC-peptide via a trans-metallation type of reaction, produces very good results [42]. In this study we used 20 μg of HYNIC-peptide with tricine and EDDA together as a coligand in amounts of 15 mg and 5 mg in final volume of labeled solution respectively. We obtained high radiochemical yield >98 % with very low amount of 99mTc-pertechnetate (<0.6) 99mTc-radiocolloid (<0.2) and 99mTc-coligands (<1.0). In RP-HPLC analysis we observed a single major peak without any impurities due to isomeric forms of the new 99mTc–HYNIC conjugate. In comparison to those report regarding 99mTc/tricine–HYNIC complex instability [43], our new labeled peptide conjugate was stable up to a 24 h post labeling period in the room temperature. These high labeling yield and stability may be due to optimization of formulation in amount of materials and also in our exchange labeling method.
Specific internalization was observed in this conjugate (12.43 ± 0.52 % up to 4 h) which was not unexpected since NT sequence offers agonistic property to the compound. Besides efflux curve of [99mTc/EDDA/Tricine/HYNIC0, Gly7, Lys8]-Neurotensin (7–13) in HT-29 cells after 2 h of internalization showed an acceptable intracellular trapping. Previous studies in a series of 99mTc-labeled NT derivatives (NT (8–13), NT-I, NT-II, NT-IV, NT-VI, NT-X, NT-VIII, NT-XI, NT-XII and NT-XIX) and also Demotensin 1–4 demonstrate internalization and receptor mediated trapping of labeled compounds [11, 17, 44]. These studies show that the highest rate of internalization corresponds to 99mTc-NT-II with 25.1 % specific cellular uptake at 4 h, followed by 99mTc-Demotensin 4 reaching a 90–95 % internalization plateau within 30 min [44]. Considering a fast and receptor specific internalization which was demonstrated with uptake results in NT receptor blocked cells experiments is an indication of not affecting the binding properties for the complex by this modification.
HYNIC–NT analog showed metabolic stability in human serum up to 24 h after labeling and incubation. Pervious Results show relatively low metabolic stability for NT. The two main cleavage bonds in the metabolic deactivation of NT (8–13) are Arg8–Arg9 and Tyr11–Ile12 [15]. The studies by Garcia-Garayoa et al. [11, 17] shows that changes in the NT amino acid sequence can have a marked effect on the peptides stability. They also found that stabilization of bond 11–12 is more important than stabilization of bound 8–9. The nonstabilized analog (NT-II) showed a half life of 5 min, which increased to only 7 min after stabilization of bond 8–9 (NT-VI). The stability of our compound could be attributed to the use of Lys9 and d-Tyr11 instead of Arg9 and Tyr11 respectively which have caused stabilization in both metabolic bonds.
In biodistribution studies, clearance from the blood circulation was fast with 0.11 % ID/g remaining in the blood at 4 h and the whole body clearance proceeded via the urinary system. Clearance from NT receptor negative tissues was also rapid except from the kidneys. Accumulation of radiopeptide in NT receptor positive tissues like the intestines and the xenografted tumor was observed. The uptake in tumor and intestine was specific and receptor mediated, as shown by the co-injection of cold peptide, indicating that these organs are also NT receptor positive. Tumor uptake was significantly reduced from 0.63 % ID/g in the control group (un block) to 0.13 % ID/g in the blocked group.
The moderate activity of stomach and thyroid gland in comparison to other organs indicates a doubt whether some degrees of free 99mTcO4 − release has occurred in vivo or these organs are included in normal accumulation sites for radiolabeled NT analogue due to the expression of NT receptor on their mucosal parts. Since the neuromodulatory actions of the mentioned peptide at the periphery level are well established [45–47], maybe there was a relation between mucosal excretion potency of organs and their ability to absorb the radiopeptide. However in blocking study non significant decreased of activity was observed in them. In blocked tumor and intestines reduction was significant which indicate specific targeting in these organs.
The tumor and intestine accumulation of this radioconjugate and its good pharmacokinetic behavior such as low tendency to accumulate in liver followed by its high kidney excretion due to low lipophilicity and high stability are the major advantages of this compound.
Conclusion
In this study, we have shown synthesis and radiolabeling of [HYNIC0, Gly7, Lys9, d-Tyr11]-Neurotensin (7–13). The labeling was completed within a very short time in high specific activity. Furthermore, this conjugates prepared by labeling of peptide, HYNIC and tricine/EDDA as a coligands demonstrated an excellent radiochemical stability even up to 24 h post labeling. Our new labeled conjugate had a specific cell binding and internalization followed by a good stability in human serum at 37 °C for at least 24 h and no significant impurities were detected by HPLC. The prepared conjugate showed high accumulation in tumor and intestine as a positive NT receptors targeted tissues followed by excretion via the kidney. These promising characteristics make our new designed labeled peptide conjugate as a very suitable candidate for diagnostic of malignant tumors.
References
Reubi JC (1995) J Nucl Med 36:1825
Okarvi SM (2004) Med Res Rev 24(3):357
Hoffman TJ, Quinn TP, Volkert WA (2001) Nucl Med Biol 28(5):527
Reubi JC (2003) Endocr Rev 24:389
Morinville A, Martin S, Lavallee M, Vincent JP, Beaudet A, Mazella J (2004) Int J Biochem Cell Biol 36:2153
Kitabgi P (2002) Curr Opin Drug Discov Devel 5:764
Vincent JP, Mazella J, Kitabgi P (1999) Trends Pharmacol Sci 20:302
Reubi JC, Maecke HR, Krenning EP (2005) J Nucl Med 46:67
Reubi JC, Waser B, Friess H, Buchler M, Laissue J (1998) Gut 42:546
Achilefu S, Srinivasan A, Schmidt MA, Jimenez HN, Bugaj JE, Erion JL (2003) J Med Chem 46:3403
Garcia-Garayoa E, Allemann-Tannahill L, Blauenstein P, Willmann M, Carell-remy N, Tourwe D, Iterbeke K, Conrath P, Schubiger PA (2001) Nucl Med Biol 28:75
Kokko KP, Hadden MK, Orwig KS, Mazella J, Dix TA (2003) J Med Chem 46:4141
Lundquist JT, Dix TA (1999) Biorg Med Chem Lett 9:2579
Hong F, Zaidi J, Cusack B, Richelson E (2002) Bioorg Med Chem 10:3849
Kitabgi P, De Nadai F, Rovere C, Bidard JN (1992) Ann N Y Acad Sci 668:30
Davis TP, Konings PNM (1993) Crit Rev Neurobiol 7:163
Garcıa-Garayoa E, Maes V, Blauenstein P, Blanc A, Hohn A, Tourwe D, Schubiger PA (2006) Nucl Med Biol 33:495
Heyl D, Sefler NM, He JX, Sawyer TK, Wustrow DJ, Akunne HC, Davis MD, Pugsley TP, Heffner TG, Corbin AE, Cody WL (1994) Chem Biol Drug Des 44:233
Hoffman TJ, Gali H, Smith VJ, Siekman GL, Hayes DL, Owen NK, Volkert WA (2003) J Nucl Med 44:823
Bergmann R, Scheunemann M, Heichert C, Mding P, Wittrisch H, Kretzschmar M, Rodig H, Tourwe D, Iterbeke K, Chavatte K, Zips D, Reubi JC, Johannsen B (2002) Nucl Med Biol 29:61
Hoffman TJ, Li N, Volkert WA, Sieckman GL, Higginbotham C, Ochrymowcycz LA (1997) J Label Compd Radiopharm 40:490
Garcıa-Garayoa E, Blauenstein P, Blanc A, Maes V, Tourwe D, Schubiger PA (2009) Eur J Nucl Med Mol Imaging 36(1):37
Schubiger PA, Allemann-Tannahill L, Egli A, Schibli R, Alberto R, Carel-Remy N, Willmann M, Blauenstein P, Tourwe D (1999) Q J Nucl Med Mol Imaging 43:155
Teodoro R, Faintuch BL, Nunez EGF, Queiroz RG (2011) Nucl Med Biol 38:113
Maina T, Nikolopoulou A, Stathopoulou E, Galanis AS, Cordopatis P, Nock BA (2007) Eur J Nucl Med Mol Imaging 34:1804
Abrams MJ, Juweid M, tenKate CI, Schwartz DA, Hauser MM, Gaul FE, Fuccello AJ, Rubin RH, Strauss W, Fischman AJ (1990) J Nucl Med 31:2022
Faintuch BL, Santos RLSR, Souza ALFM, Hoffman TJ, Greeley M, Smith CJ (2005) Chemistry 35:43
Gandomkar M, Najafi R, Shafiei M, Mazidi M, Ebrahimi SES (2007) Nucl Med Biol 34:651
Sadeghzadeh N, Gandomkar M, Najafi R, Shafiei M, Sadat Ebrahimi SE, Shafiee A, Larijani B (2010) J Radioanal Nucl Chem 283:181
Sadeghzadeh N, Gandomkar M, Shafiee M, Mazidi M, Goudarzi M, Mirfallah SM, Sadat Ebrahimi SE (2009) Iran J Nucl Med 17(1):18
Atherton E, Sheppard R (1989) Fluorenylmethoxycarbonyl-poly-amide solid phase peptide synthesis—general principles and development. In: Solid phase peptide synthesis. A practical approach, Oxford Information Press, Oxford, p 25–38
Maina T, Nock B, Nikolopoulou A (2002) Eur J Nucl Med Mol Imaging 29:742
Erfani M, Shafiei M, Mazidi M, Goudarzi M (2013) Cancer Biother Radiopharm 28(3):240
Shirmardi SP, Gandomkar M, Mazidi M, Shafiei M, Ghannadi Maragheh M (2011) J Radioanal Nucl Chem 288:327
Shirmardi SP, Gandomkar M, Ghannadi Maragheh M, Shamsaei M (2011) Cancer Biother Radiopharm 26(3):309
Liu S, Edwards DS, Looby RJ, Poirier MJ, Rajopadhye M, Bourque JP, Carroll TR (1996) Bioconjug Chem 7(2):196
Kasina S, Rao T, Srinivasan A, Sanderson JA, Fitzner JN, Reno JM, Beaumier PL, Fritzberg AR (1991) J Nucl Med 32:1445
Maina T, Stolz B, Albert R, Bruns C, Koch P, Maecke HR (1994) Eur J Nucl Med 21(5):437
Yurt Lambrecht F, Durkan K, Ozgur A, Gunduz C, Avci CB, Susluer SY (2013) J Drug Target 21(4):383
Yurt Lambrecht F, Durkan K, Bayrak E (2010) J Radioanal Nucl Chem 284:539
Liu S, Edwards DS, Looby RJ, Harris AR, Poirier MJ, Barrett JA, Heminway SJ, Carrol TR (1996) Bioconj Chem 7:63
Gabriel M, Froehlich F, Decristoforo C, Ensinger C, Donnemiller E, von Guggenberg E, Heute D, Moncayo R (2004) Eur J Nucl Med Mol Imaging 31:330
Babich JW, Fischman AJ (1995) Nucl Med Biol 22(1):25
Nock BA, Nikolopoulou A, Reubi JC, Maes V, Conrath P, Tourwe D, Maina T (2006) J Med Chem 49:4767
Tanaka K, Masu M, Nakanishi S (1996) Neuron 4:847
Mule F, Serio R, Postorino A, Vetri T, Bonvissuto F (1996) Br J Pharmacol 117:488
Bidard JN, Nadai F, Rovere C, Moinier D, Laur J, Martinez J, Cuber JC, Kitabgi P (1993) Biochem J 291:225
Acknowledgments
The authors wish to thank Mr. Mirfallah and Mr. Talebi of the Radioisotope Department (AEOI) for providing sodium pertechnetate and assistance in quality control tests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahrabi, N.Z., Erfani, M., Parivar, K. et al. Preparation and evaluation of a new neurotensin analog labeled with 99mTc for targeted imaging of neurotensin receptor positive tumors. J Radioanal Nucl Chem 299, 461–469 (2014). https://doi.org/10.1007/s10967-013-2795-1
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10967-013-2795-1