Abstract
CancerGene Connect (CGC) is a web-based program that combines the collection of family and medical history, cancer risk assessment, psychosocial assessment, report templates, a result tracking system, and a patient follow up system. The performance of CGC was assessed in several ways: pre-appointment completion data analyzed for demographic and health variables; a time study to assess overall time per case and to compare the data entry by the genetic counselor compared to the patient, and a measured quality assessment of the program via observation and interview of patients. Prior to their appointment, 52.3 % of 2,414 patients completed the online patient questionnaire section of CGC. There were significant differences in completion rates among racial and ethnic groups. County hospital patients were less likely to complete the questionnaire than insured patients (p < 0.0001); and likewise uninsured patients and patients with Medicare/Medicaid were less likely to complete the questionnaire than private patients (p < 0.0001). The average genetic counseling time per case was 82 min, with no significant differences whether the counselor or the patient completed CGC. CGC reduces genetic counselor time by approximately 14–46 % compared to average time per case using traditional risk assessment and documentation methods previously reported. All surveyed users felt the questionnaire was easy to understand. CGC is an effective tool that streamlines workflow, and provides a standardized data collection tool that can be used to evaluate and improve the genetic counseling process.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Due to recent government initiatives and the increasing demands on healthcare practitioners, the field of healthcare information technology (IT) is rapidly expanding. The Health IT for Economic and Clinical Health (HITECH) Act was enacted in 2009 to promote the adoption and meaningful use of health IT and to incentivize the use of IT in medical practice. While health IT is rapidly expanding as an industry, its application to cancer genetics risk assessment is more limited. In 1998, we developed one of the first electronic cancer risk assessment programs; CancerGene.
Across health care professions, electronic programs have been used to improve efficiency (Chaudhry et al. 2006; Euhus 2001; Lepanto et al. 2006) and have been shown to decrease face-to-face time spent with patients in a genetic counseling setting (S. A. Cohen and McIlvried 2011). The incorporation of a computer program to assist with the genetic counseling process would likely allow more time for patient focused care during the genetic counseling process (Euhus 2001).
One of the most time-consuming components of the genetic counseling process is family history collection. It is also one of the most crucial components of a genetic counseling session, with specific guidelines published by the American Society of Clinical Oncology (Lu et al. 2014), the Commission on Cancer (COC 2012), and the National Accreditation Program for Breast Cancers (NAPBC 2012). Additionally, even though eliciting a family history is crucial, its accuracy cannot be assured. Multiple studies have shown that patient recall of their family history is often inadequate (Dominguez et al. 2007; Gaff et al. 2004; Glanz et al. 1999; King et al. 2002; Mai et al. 2011; Murff et al. 2004; Ozanne et al. 2012; Pinsky et al. 2003; Quillin et al. 2006; Weinrich et al. 2002; Wideroff et al. 2010; Ziogas and Anton-Culver 2003) and can vary by education level (Wideroff et al. 2010), income (Weinrich et al. 2002), race (Dominguez et al. 2007; Pinsky et al. 2003; Wideroff et al. 2010), gender (Glanz et al. 1999; Pinsky et al. 2003; Wideroff et al. 2010) and cancer site of origin (King et al. 2002; Mai et al. 2011; Murff et al. 2004; Ziogas and Anton-Culver 2003). Asking patients to report their family history before the genetic counseling session provides an opportunity for the patient to confer with relatives and gather information, allowing for more comprehensive and accurate family history collection.
In addition to potentially improving the accuracy of the family history and decreasing the time it takes to collect it during the genetic counseling appointment, integration of an electronic family history data collection tool into genetic counseling clinics has the potential to decrease errors due to illegibility and incomplete data collection. There is a paucity of studies that explore this potential benefit within the genetic counseling setting. However, this benefit is documented in other areas of health care, with significant reductions in prescription errors (Shamliyan et al. 2008), legibility issues (Ali et al. 2010; Jani et al. 2008; Smith et al. 2009), and incomplete prescriptions (Ali et al. 2010; Jani et al. 2008). Similar benefits would be expected when electronic systems are applied to family history collection.
The majority of the electronic tools created to assist in the genetic counseling process center around the collection of family history. Electronic family history collection, versus handwritten notes or lists, is beneficial because an electronic tool can automatically organize this data for patients and clinicians, often before the appointment. Patient acceptance of electronic family history collection has been previously reported (Westman et al. 2000). Researchers have also compared family histories collected by electronic tool versus those collected by a genetic counselor and found the majority of affected family members were reported on both pedigrees (Acheson et al. 2006). And when there were discrepancies, it was more common for cancer to be recorded by their electronic tool only, versus reported by the genetic counselor only (Acheson et al. 2006). Several family history collection tools that can be used to assist the genetic counseling process are displayed in Table I.
Despite the number of family history tools available, there are barriers to their use. Widmer et al. (2013) found that only 16 % of the genetic counselors they surveyed had ever had access to an electronic version of their patients’ family histories, and a smaller percentage had patient populations who consistently had access. Barriers to use include concern over ease of use and the inability to modify family history with additional information collected during the session (Widmer et al. 2013). Also, many family history collection tools do not allow both patient and provider to input and modify family history information within the electronic system, or collect medical history, which is an important component of the cancer risk assessment.
Furthermore, the majority of these tools are unable to automatically generate mutation risk estimates. In addition to entering the patient information into an electronic system to document the encounter, the provider would need to re-enter the patient’s medical and family history information into a computer risk program, such as CancerGene to generate a risk estimate.
The impetus for developing CGC was to expand the use of technology within the genetic counseling process beyond the collection of family history to include streamlining cancer risk assessment and clinic documentation. The limitations and barriers to the use of other electronic tools for genetic counseling were addressed by the model for CGC. The goal was to create an all-encompassing program where the patient’s targeted medical and family history could be entered one time and then used to generate risk assessment reports, track results, and manage patient follow-up. As a result, patient care would be improved by obtaining more complete and more accurate intake information, as well as facilitating clinical research. Genetic counseling throughput could be maximized by allowing the patient to enter their own medical and family history prior to the appointment, improving the accuracy and completeness of information collected from the patient and enhancing efficacy and efficiency of genetic counseling sessions. As a result, patient care would be improved by allowing more time for addressing, rather than assessing, patient’s risk, and future research would be improved by standardized data collection.
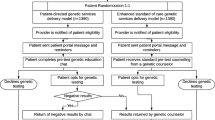
The purpose of this research was to determine whether CGC helps achieve these goals and streamline the cancer genetic counseling session. Here, three aspects of CGC were evaluated (Fig. 1). First, completion rates were assessed to determine whether demographic and health status variables were associated with completion of the patient-accessible portion of CGC. Second, we asked whether CGC was able to improve genetic counseling workflow by comparing time spent per patient when CGC was used versus traditional genetic counseling processes without CGC. Finally, we discuss measures taken to determine whether the questions within the patient-accessible portion of CGC were easy to understand, and whether patient responses to the questions in CGC were valid.
Methods
CGC Completion Rates and Demographics
Participants
The analyses included all patients entered in the CGC database between January 1, 2010 and June 30, 2013, (N = 5,157) seen at our four primary sites: Simmons Cancer Center (SCC); Moncrief Cancer Institute (MCI); John Peter Smith Hospital (JPS); and Parkland Memorial Hospital (PMH). Data regarding patient completion were collected beginning May 1, 2011. However, the Spanish version of the online patient questionnaire portion of CGC was not available until March 2013, and patients seen at our county safety net clinics (JPS and PMH) (30 % of our patients) were not asked to enter their own data until that time. Therefore, patient completion of the online CGC questionnaire was evaluated from May 2011 to June 2013 at our two primary clinics (SCC and MCI). This included a total of 2,414 patients. For comparison between clinic populations and testing funding source, completion rates were separately analyzed from April 2013 to June 2013 for all four clinics, after the Spanish version of the online questionnaire became available, and when the online questionnaire was routinely offered in all clinics. This analysis included 499 patients. Of these patients, 153 patients did not have genetic testing, and were not included in the analysis of completion by testing funding source. IRB approval was obtained (IRB #STU 072013-051- Evaluation of Utilization of CancerGene Connect and Genetics Navigation in a Clinical Cancer Risk Assessment Program), and an informed consent waiver for this retrospective data review was granted.
Data Analysis
The pre-appointment patient completion rates for CGC were analyzed by several demographic and health status categories (gender, age, race, ethnicity, cancer status, and genetic test status) to assess if these categories affect the likelihood that the patient would complete CGC. The association between patient completion and demographic and health status variables were analyzed using the Fisher’s Exact Test or 2-tailed Chi-square tests for independence using GraphPad InStat software. In this study, we did not adjust for multiple comparisons.
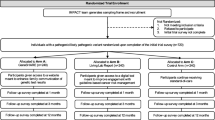
Effects of CGC use on Genetic Counseling Workflow
Procedures
A time study was conducted from May 2011 to August 2011 to analyze the genetic counselor’s time in two scenarios: when the patient completed the CancerGene Connect program prior to their appointment, and when the genetic counselor had to do the data entry themselves. A time tracking form was developed to capture time spent on various genetic counseling tasks, including pre-appointment chart review, time in clinic, documentation of clinic visit, follow up activities, calling results, and documenting and sending results. The genetic counselor used this form to self-report the time they spent on each of these tasks as they worked through each case. The genetic counselor also documented the reasons why patients did not complete the online patient questionnaire portion of CGC on this tracking form.
Participants
Five genetic counselors were each asked to prospectively record the time spent on each task for the first 10 patients that completed the online CGC questionnaire prior to their appointment and for the first 10 patients that did not from the study initiation. Data were collected on a total of 89 patients; 39 patients in this cohort completed the online CGC questionnaire prior to their appointment, and 50 did not.
Data Analysis
Time spent on various counseling tasks was compared based on patient completion of the online questionnaire portion of CGC (Fig. 2). The data were analyzed using the 2-tailed unpaired t-test with Welsch correction.
Quality Assurance Testing of Patient Comprehension of CGC
Procedures
In 2012, the online questionnaire section of CGC was translated to Spanish. UT Southwestern’s Clinical Sciences team then performed cognitive interviews on over 50 patients (both English and Spanish speaking) to ensure that questions were understandable and responses are valid in both languages. Cognitive interviewing is a type of semi-structured interview intended to refine survey instruments and behavioral interventions (Weidmar et al. 1999; Hurtado et al. 2005; Willis 2004). The cognitive interviews consisted of various questions about items included in the computer program as well as the formatting and usability of the program. We assessed whether participants understood what the questions in the computer program were asking and what the various response options meant. Prior to this evaluation, we determined the completion rate for each question to determine questions that were not being answered by the participants. Though some sections of the interface had 100 % completion rates for those accessing the system, other sections, such as the physical activity section, had completion rates of only 35 %. Qualitative data from the cognitive interviews were analyzed through techniques outlined by Willis 2004, Weidmar et al. 1999, and Hurtado et al. 2005. Interviews were transcribed and a code book was developed. For each survey item, a list of codes relevant to the cognitive processing of the question was developed. Codes included: respondent has difficulty understanding the question (comprehension), respondent has difficulty remembering the question (recall), and respondent has difficulty understanding the meaning of particular words or concepts. Coders applied the codebook to each survey question using study notes, audiotapes and transcripts. Coding discrepancies were identified and brought back to the language validation team for resolution. After all discrepancies were worked out, appropriate changes were incorporated to the final versions which were then used for pilot testing. These participants were also administered a separate questionnaire with Likert-style and open ended questions to assess their reaction to the program (IRB #STU 102011–028 CancerGene Connect Study funded by CPRIT, Cancer Prevention Research Institute of Texas).
Participants
Altogether, 50 users underwent cognitive interviews; 32 users underwent interviews to assess the initial format, and 18 users (11 English, 7 Spanish) were interviewed to assess the revised format. These participants were recruited from our PMH general cancer genetics clinic. All English and Spanish speaking patients being scheduled in this clinic between the ages of 18 and 64 were invited to participate in this study, and were enrolled until the target enrollment was reached. Informed consent was obtained from study participants after the nature of the procedure was fully explained to them.
Description of CGC
CGC was developed by the UT Southwestern Cancer Genetics team under the direction of Dr. David Euhus and Linda Robinson, MS, CGC. It was first piloted in late 2009 at Moncrief Cancer Institute (UT Southwestern-affiliated) and UT Southwestern Simmons Cancer Center.
CGC was designed as a secure, password-protected web-based application. When patients are scheduled for a genetics appointment, they are provided with a secure ID and password and a link to the CGC website that allows them to complete the online questionnaire from their home prior to appointment. The online, patient-accessible questionnaire consists of over 130 targeted questions that cover the topics of: patient demographics; referring physician information; obstetric/gynecologic (Ob/Gyn) history; hormonal and birth control history; surgical history (targeted for breast and gynecological surgery); colon history (including surveillance, surgery, and risk factors); general health; social history (including alcohol, tobacco use and exercise habits); psychological screens (discussed below); and family history.
The online questionnaire is designed with branching logic, such that patients are only prompted to complete applicable information. For example, males are not asked about gynecological, hormonal, or birth control use history; patients who have not had a breast biopsy are not asked for biopsy results, etc. By patient report and observation, it typically takes the patient 20 min to complete this online questionnaire, but length of time may vary. The website is hosted by UT Southwestern server using HTTPS secure encryption. Data are encrypted and transferred to a secure UT Southwestern SQL server where it is stored.
All data input by the patient is immediately accessible by the genetic counselor, and does not need to be printed by the patient. A pedigree is automatically generated. This, and the patient’s targeted medical history, can be viewed by patient and provider. At this time, the program is not integrated directly into the medical record. The data within the program can be printed and scanned into the patient’s electronic medical record or copied and pasted.
CGC incorporates a number of previously validated cancer risk assessment models, including the Gail, Claus, BRCAPRO, MMRpro, PancPro, and MelaPro models (Chen et al. 2006). Links to the PENN II, LAMBDA, Tyrer-Cuzick, BODICEA, and PTEN models, as well as the Myriad tables, MMR predict and NCI colon cancer risk model are also included on the provider interface of CGC. Once the patient has completed the online questionnaire, the provider can review patient responses, run the risk assessment models, print the pedigree and patient summary, and document patient encounters. The provider has the ability to update and edit any of the information that the patient has entered. The provider also can complete additional fields that are only accessible to the provider, such as head circumference, maternal and paternal ancestry, consanguinity, and genetic testing status (e.g. pending, negative, variant of uncertain significance, etc.). All fields can be updated by the provider (e.g. when test result status changes from “pending” to “negative”).
CGC also includes previously validated psychological scales that assess depression, social support and post-traumatic stress (CES-D, ISEL, IES-R, respectively) (S. Cohen and Hoberman 1983; Horowitz et al. 1979; Radloff 1977). These scales use Likert-style questions to provide a raw score for each of these categories. CGC reports both the raw score and a qualitative “yes/no” indicator that the patient’s responses suggest that they have one or more of these psychosocial conditions. Psychological scales allow for standardization of the psychosocial assessment process. Standardization of psychosocial assessment is consistent with the 2012 American College of Surgeons Commission on Cancer Program Standard 2.3, mandating psychosocial assessment as part of the hereditary cancer risk assessment process (Greene 2013). The provider can view a summary of the patient’s scores and can incorporate recommendations for psychological support and/or document referrals for psychological services into the risk assessment report using templates. CGC also includes a follow-up screen in which the provider can document prophylactic surgeries, surveillance, chemoprevention, and psychosocial support interventions for the patient. This feature allows the provider to create reminders for patient surveillance, or otherwise follow patients to ensure appropriate management.
Several report templates are built into the provider interface of CGC, including risk assessment reports, family letters, and positive, negative, and variant of uncertain significance result reports. The reports include drop-down menus with editable text. The positive results templates incorporate management recommendations based on literature review and/or National Comprehensive Cancer Network (NCCN) guidelines, which are cited within the templates’ text. The templates are revised as new versions of NCCN guidelines and/or new literature becomes available.
After piloting the program in late 2009, the online patient questionnaire portion of CGC was updated based on patient and genetic counselor feedback, and the UT Southwestern Cancer Genetics group began entering all patients into CGC in January 2010. The program has been regularly updated since its creation. Updates include the creation of additional fields to capture method of test payment and other clinical/administrative data, the incorporation of updates to national management guidelines, and the addition of test menus and patient fact sheets.
Beyond its clinical application, CGC is a powerful administrative, patient care, and research tool. Every data point collected within the patient and provider interface is stored within a secure database. This information can be used to analyze patient volumes, referral patterns, and result statistics. The information can also be used for patient care, to generate lists of patients with pending test results or lists of patients positive for a given gene mutation. Finally, the database can facilitate research, by providing a method to identify health disparities or identify patients that might meet criteria for a given protocol. At UT Southwestern, the CGC database has been linked with the Informatics for Integrating Biology and the Bedside program, a tool that allows database queries for researchers.
Results
CGC Completion Rates and Demographics
Data collection of completion rates began May 1, 2011 and ended June 30, 2013. During that time, completion rates based on demographic variables were assessed at our main clinic sites (Simmons Cancer Center and Moncrief Cancer Institute), where patients were routinely offered the online CGC questionnaire prior to their appointment. A total of 52.3 % of patients in this cohort completed the questionnaire. Thus 47.7 % either did not start the questionnaire or did not complete enough of it such that the genetic counselor needed to go back into CGC and complete it themselves. For this cohort, there were statistically significant differences in completion rates based on age (p = 0.026); 30.4 % of individuals younger than 18 years completed the questionnaire, versus 55.1 % of individuals aged 18–29 years, 54.2 % aged 30–49 years, 52.7 % aged 50–64 years, and 46.6 % aged 65 and older. Post-hoc comparison indicates that patients ages 18–64 had a higher completion rate compared to patients under 18 and above 65, although patients under 18 had a much lower completion rate (p = 0.0052). The differences in completion rates among racial groups were statistically significant (p < 0.0001), and are as follows; American Indian/Native Alaskans 53.3 %, Asians 52.6 %, African Americans 37.0 %, Native Hawaiian/Pacific Islanders 8.3 %, and White/Caucasians 55.2 %. Post-hoc comparison indicates that completion rates were significantly less among African Americans and Hawaiian/Pacific Islanders compared with the other racial groups (p < 0.0001). Individuals of reported Hispanic ethnicity (35.5 %) were less likely to complete the questionnaire than individuals who did not report Hispanic ethnicity (55.9 %) (p < 0.0001). The differences in completion rates by gender and cancer status were not statistically significant.
For comparison, completion rates for our main clinics and county hospital clinics were assessed from April 1, 2013 to June 30, 2013, when the online questionnaire was routinely offered at all sites. Patients seen at our county hospital clinics (21.5 %) were less likely to complete the questionnaire than patients seen in our main clinics (SCC 47.3 %; MCI 56.7 %) (p < 0.0001). Significant differences were observed in completion rates among patients without insurance, patients with Medicare/Medicaid, and patients with private insurance (p < 0.0001). Patients without insurance (27.0 %) were significantly less likely to complete CGC compared to patients with private insurance (50.0 %) (p < 0.0001); as were patients with Medicare/Medicaid (29.6 %) (p = 0.015). See Table II for more detail and information on non-statistically significant associations.
Reasons for non-completion were not collected during the entire time frame of the study. However, reasons for non-completion were documented by the genetic counselors from 43 patients seen between May 2011 and August 2011 (prior to the implementation of the Spanish version of the program). The reasons given for non-completion were either because the patient: was not offered the questionnaire at their clinic site (n = 11); was seen as a walk-in (n = 10); did not have internet access (n = 8); did not speak English (n = 7); had technical difficulties using the program (n = 2); forgot their password (n = 2); forgot to complete the questionnaire (n = 2); and declined to complete the questionnaire (n = 1). If patients had not done so before arriving to clinic, they no longer had the opportunity to complete the online questionnaire.
Effects of CGC use on Genetic Counseling Workflow
The average genetic counseling time per case using CGC was 82 min. Completion of the online questionnaire portion of CGC prior to the appointment did not result in statistically significant reductions (or increases) in time spent on any of the genetic counseling tasks that were measured. Anecdotally, genetic counselors reported that while the same amount of time was spent with completers vs. non-completers, they were able to spend more time in the session addressing risk vs. assessing risk with the completers, giving the genetic counselors a greater feeling of efficacy with these patients.
We also used the time study to compare the total time a genetic counselor spends on a cancer genetics case from start to finish using CGC with the historical time commitment for a case. Prior to CGC, the genetic counselor would enter the pedigree obtained in the session into CancerGene, draw the pedigree in Progeny and write the follow up documentation in another system. At our institution, the estimated average time spent per case was approximately 2.5–3 h prior to the implementation of CGC, which is similar to genetic counseling times previously reported in the literature (reports vary from 85 to 150 min/case) (McPherson et al. 2008; Uhlmann et al. 2011; Wham et al. 2010; Cohen and McIlvried 2011). Compared to genetic counseling times reported in the literature, use of CGC reduced the time spent per case by approximately 14 to 46 %. At our institution, the implementation of CGC reduced the overall time spent on cancer genetics cases by half compared with estimated time spent per case prior to implementation of the program.
Quality Assurance Testing of Patient Comprehension of CGC
Seventy two percent of users strongly agreed that the program was easy to use and 100 % agreed or strongly agreed that the questions were easy to understand. In response to open ended questions asked about their satisfaction with the program, users commented that they enjoyed creating their family history, they liked being asked about how they feel (referring to the psychological assessment), and that the program was easy/simple/fast to use. Patient assessment of the program is summarized in Table III. Based on this pilot study, an updated “2.0” version of CGC was implemented in March 2013 where over 1,500 patients have been entered.
Discussion
Major Findings and Practice Implications
CGC is a web-based application that saves time, provides patients and providers the ability to continually update family history information, performs hereditary risk and cancer risk calculations, and includes modifiable macro-generated reports. CGC is a tool that has the potential to provide benefit to all components of the genetic counseling session including medical and family history collection, psychosocial assessment, reporting of test results to patient and provider, and documentation of follow-up procedures.
The workflow analysis showed that this program reduces the time spent per case from 14 to 46 % compared to previously reported genetic counseling times. In short, CGC saves genetic counselors time regardless of whether or not the patient completes the online questionnaire section prior to the session. With implementation of CGC, there is greater opportunity to reduce redundancy in clinic workflows because medical and family history information only needs to be entered once in order to be documented and to generate risk estimates and pedigrees.
CGC also enhances the quality of the genetic counseling encounter when patients complete the questionnaire before the appointment. By having the information before the appointment, the provider is given a better idea of what needs to be addressed in the session before they see the patient. Thus, when the provider is aware of patients’ individualized mutation risks, cancer risks, and psychosocial profile before the session, they can spend less time collecting information during the session, and more time establishing rapport and addressing individualized concerns. This finding is consistent with a previously predicted benefit following integration of a computer program to assist the genetic counseling process (Euhus 2001).
CGC also includes a validated psychosocial assessment tool to accommodate NCCN guidelines (not evaluated here). This is used to standardize the psychosocial assessment of cancer genetics patients. This standardization should help eliminate counselor variability in identifying psychosocial issues. Incorporating a psychosocial assessment into a pre-visit questionnaire provides the genetic counselor with the opportunity to easily identify which patients may require additional resources, support, or referrals to psychological services prior to the session. Based on psychological assessment scores, UT Southwestern genetic counselors have identified and documented the need for additional support and resources for over 600 patients, and have identified psychosocial disparities within our clinic population. Patients are routinely referred to psychological services at our institution based upon this needs assessment.
In addition to the benefits listed above, CGC has transformed the administrative tasks of compiling clinic volumes and tracking test results. This information is regularly requested by hospital administration to evaluate productivity, as well as for department administrative purposes such as evaluating clinic workload, referral patterns and need for additional resources; utilization for clinical purposes includes following up with positive patients. Previously, these data were captured by an administrative assistant entering every patient encounter into a database, recording the clinic site, visit type, referring physician, patient demographic information, genetic counselor, and test results. CGC has eliminated this process at UT Southwestern, as all of this information is gathered in the CGC database, and this information can be quickly retrieved via database query.
The modifiable macros and templates make it possible to incorporate ever-evolving updates of the national management guidelines, thereby preventing outdated patient information from being a barrier to use. CGC capitalizes on its ability to use health IT to improve accuracy, efficiency, and standardization of the genetic counseling process, and provides a standardized data collection platform from which evidence based outcomes of genetic counseling can be measured.
We found that patients from our safety net clinics were less likely to complete the online questionnaire section of CGC than our private patients, and patients with private insurance were more likely to complete the online questionnaire than patients with Medicare, Medicaid, or no insurance. There may be several reasons for this, including differences in scheduling personnel for different clinics, patient access to the internet, computer literacy, and psychosocial factors. Computer illiteracy (Hilton et al. 2012; Simon et al. 2008) and the inability to access the internet at home (Simon et al. 2008) are associated with inability to engage in web-based health information. However, other research has shown that patients living in either suburban or urban areas were equally likely to access the internet, even though suburban residents were more likely to own a computer and urban residents had a higher odds of being uninsured (Bond et al. 2012). Household income cannot always predict internet use (Appleby-Tagoe et al. 2012; Bond et al. 2012; Simon et al. 2008). Research has shown that mental health issues and substance use have not been barriers to online health information either (Hilton et al. 2012).
Due to the limited, but undeniable, number of individuals who are unable to access the internet, a non-electronic option should always be available (Simon et al. 2008), even though, research has shown that race, age, education, personal history of cancer, or family history of cancer does not affect patients’ desire to use the internet (Simon et al. 2008). A paper version of the CGC questionnaire is available to our patients. Completion rates and demographic information of those who filled out the paper questionnaire, versus the online version, were not collected, however.
There are several topics that should be discussed with the patient when she/he is asked to complete the online family history data collection tool. It is important to explain to patients that they will have the opportunity to clarify any questions regarding their family history when they meet with the genetic counselor. The belief that patients will not have the opportunity to discuss their family history directly with health care providers is a reason some patients would not fill out an electronic family history tool (Simon et al. 2008). Privacy concerns should also be discussed, as the potential for additional loss of confidentiality has been established as a barrier to electronic family history intake (Simon et al. 2008). Furthermore, patients should be made aware of the importance of genetic counseling and that gathering a complete family history will allow them to maximize their benefit from the genetic counseling process (Appleby-Tagoe et al. 2012).
CGC does not obviate the need for review of family history during the genetic counseling session. For example, genetic counselors can clarify whether cancer represents a new primary versus a metastasis site (Acheson et al. 2006). Additional questions used to clarify family history can help to improve accuracy (Kadan-Lottick et al. 2003), including information about third degree relatives, which is not collected by CGC. Pathology should be used to verify cancer reports whenever possible, particularly when there is significant overrepresentation of malignancy within a family history (Parent et al. 1997).
Study Limitations
CGC is specific to the hereditary cancer genetic counseling process, and is not applicable for use in prenatal, pediatric, or other genetic counseling subspecialties. This study is limited by the fact that it was conducted within one cancer genetics program, and results may vary at other institutions. Assessment of patient completion rates is limited by the relatively short time that the Spanish translation of the questionnaire was available, and the relatively short time that the questionnaire was routinely offered to at all clinic sites. The statistical analysis is limited in that corrections for multiple comparisons were not performed. The qualitative assessment of the program is limited by the small number of participants that were included.
Research Recommendations
CGC can be further enhanced to increase the efficiency of the genetic counselor as well as provide patients with self-care tools. For example, we plan to target specific cancer risk factors, such as alcohol use, smoking and obesity, and offer the patient resources as they complete the online questionnaire portion of CGC based on their responses, such as links to alcohol and smoking cessation tools or weight management programs. We will continue to evaluate patient completion rates and analyze the outcomes of interventions to improve these, such as adding tablets in our waiting rooms for patients to complete the questionnaire prior to their appointment. We will continue to evaluate disparities in psychological assessment scores and develop interventions. We are currently developing a follow-up tool to generate automated reminders to our BRCA and Lynch positive patients for recommended screening tests. To measure the effect of cancer genetic testing and the role of genetic counseling in the reduction of cancer incidence, we are using the data obtained from our CGC program to model the uptake of prophylactic surgeries and compliance with NCCN management guidelines to determine the impact on the long term cancer incidence. A systematic data collection system is needed to measure genetic counseling outcomes. As the demand for services continues to increase, a technological tool will be needed to address inefficiencies. CancerGene Connect is a tool that can meet this need.
References
Acheson, L. S., Zyzanski, S. J., Stange, K. C., Deptowicz, A., & Wiesner, G. L. (2006). Validation of a self-administered, computerized tool for collecting and displaying the family history of cancer. Journal of Clinical Oncology, 24(34), 5395–5402. doi:10.1200/jco.2006.07.2462.
Ali, J., Barrow, L., & Vuylsteke, A. (2010). The impact of computerised physician order entry on prescribing practices in a cardiothoracic intensive care unit. Anaesthesia, 65(2), 119–123. doi:10.1111/j.1365-2044.2009.06134.x.
Appleby-Tagoe, J. H., Foulkes, W. D., & Palma, L. (2012). Reading between the lines: a comparison of responders and non-responders to a family history questionnaire and implications for cancer genetic counselling. Journal of Genetic Counseling, 21(2), 273–291. doi:10.1007/s10897-011-9399-0.
Bond, M. C., Klemt, R., Merlis, J., Kopinski, J. E., & Hirshon, J. M. (2012). Computer access and Internet use by urban and suburban emergency department customers. Journal of Emergency Medicine, 43(1), 159–165. doi:10.1016/j.jemermed.2011.03.034.
Chaudhry, B., Wang, J., Wu, S., Maglione, M., Mojica, W., Roth, E., et al. (2006). Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Annals of Internal Medicine, 144(10), 742–752.
Chen, S., Wang, W., Lee, S., et al. (2006). PRediction of germline mutations and cancer risk in the lynch syndrome. JAMA, 296(12), 1479–1487. doi:10.1001/jama.296.12.1479.
Cohen, S., & Hoberman, H. M. (1983). Positive events and social supports as buffers of life change Stress1. Journal of Applied Social Psychology, 13(2), 99–125.
Cohen, S. A., & McIlvried, D. E. (2011). Impact of computer-assisted data collection, evaluation and management on the cancer genetic counselor’s time providing patient care. Familial Cancer, 10(2), 381–389. doi:10.1007/s10689-011-9417-2.
Commission on Cancer (COC). (2012). Cancer Program Standards 2012: Ensuing Patient-Centered Care. (1), 140. http://www.facs.org/cancer/coc/programstandards2012.pdf.
Dominguez, F. J., Lawrence, C., Halpern, E. F., Drohan, B., Grinstein, G., Black, D. M., et al. (2007). Accuracy of self-reported personal history of cancer in an outpatient breast center. Journal of Genetic Counseling, 16(3), 341–345. doi:10.1007/s10897-006-9067-y.
Euhus, D. M. (2001). Understanding mathematical models for breast cancer risk assessment and counseling. Breast Journal, 7(4), 224–232.
Gaff, C. L., Aragona, C., MacInnis, R. J., Cowan, R., Payne, C., Giles, G. G., et al. (2004). Accuracy and completeness in reporting family history of prostate cancer by unaffected men. Urology, 63(6), 1111–1116. doi:10.1016/j.urology.2003.12.032.
Glanz, K., Grove, J., Le Marchand, L., & Gotay, C. (1999). Underreporting of family history of colon cancer: correlates and implications. Cancer Epidemiology, Biomarkers and Prevention, 8(7), 635–639.
Greene, F.L. (2013). Cancer Program Standards 2012: Ensuring Patient-Centered Care, Version 1/2. Commission on Cancer. Retrieved from Cancer Program Standards 2012: Ensuring Patient-Centered Care, Version 1.2 website: http://www.facs.org/cancer/coc/programstandards2012.pdf.
Hilton, J. F., Barkoff, L., Chang, O., Halperin, L., Ratanawongsa, N., Sarkar, U., et al. (2012). A cross-sectional study of barriers to personal health record use among patients attending a safety-net clinic. PLoS ONE, 7(2), e31888. doi:10.1371/journal.pone.0031888.
Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of event scale: a measure of subjective stress. Psychosomatic Medicine, 41(3), 209–218.
Hurtado, M. P., Angeles, J., Blahut, S. A., & Hays, R. D. (2005). Assessment of the equivalence of the Spanish and English versions of the CAHPS Hospital Survey on the quality of inpatient care. Health Services Research, 40, 2140–2161.
Jani, Y. H., Ghaleb, M. A., Marks, S. D., Cope, J., Barber, N., & Wong, I. C. (2008). Electronic prescribing reduced prescribing errors in a pediatric renal outpatient clinic. Journal of Pediatrics, 152(2), 214–218. doi:10.1016/j.jpeds.2007.09.046.
Kadan-Lottick, N. S., Friedman, D. L., Mertens, A. C., Whitton, J. A., Yasui, Y., Strong, L. C., et al. (2003). Self-reported family history of cancer: the utility of probing questions. Epidemiology, 14(6), 737–740. doi:10.1097/01.ede.0000091602.06231.aa.
King, T. M., Tong, L., Pack, R. J., Spencer, C., & Amos, C. I. (2002). Accuracy of family history of cancer as reported by men with prostate cancer. Urology, 59(4), 546–550.
Lepanto, L., Pare, G., & Gauvin, A. (2006). Impact of PACS deployment strategy on dictation turnaround time of chest radiographs. Academic Radiology, 13(4), 447–452. doi:10.1016/j.acra.2005.12.008.
Lu, K. H., Wood, M. E., Daniels, M., Burke, C., Ford, J., Kauff, N. D., et al. (2014). American society of clinical oncology expert statement: collection and use of a cancer family history for oncology providers). Journal of Clinical Oncology, 32(8), 833–840.
Mai, P. L., Garceau, A. O., Graubard, B. I., Dunn, M., McNeel, T. S., Gonsalves, L., et al. (2011). Confirmation of family cancer history reported in a population-based survey. Journal of the National Cancer Institute, 103(10), 788–797. doi:10.1093/jnci/djr114.
McPherson, E., Zaleski, C., Benishek, K., McCarty, C. A., Giampietro, P. F., Reynolds, K., et al. (2008). Clinical genetics provider real-time workflow study. Genetics in Medicine, 10(9), 699–706.
Murff, H. J., Spigel, D. R., & Syngal, S. (2004). Does this patient have a family history of cancer? An evidence-based analysis of the accuracy of family cancer history. JAMA, 292(12), 1480–1489. doi:10.1001/jama.292.12.1480.
National Accreditation Program for Breast Centers (NAPBC). (2012). 2012 Breast Cancer Standards Manual. (1), 72. http://napbc-breast.org/standards/2012standardsmanual.pdf.
Ozanne, E. M., O’Connell, A., Bouzan, C., Bosinoff, P., Rourke, T., Dowd, D., et al. (2012). Bias in the reporting of family history: implications for clinical care. Journal of Genetic Counseling, 21(4), 547–556. doi:10.1007/s10897-011-9470-x.
Parent, M. E., Ghadirian, P., Lacroix, A., & Perret, C. (1997). The reliability of recollections of family history: implications for the medical provider. Journal of Cancer Education, 12(2), 114–120. doi:10.1080/08858199709528465.
Pinsky, P. F., Kramer, B. S., Reding, D., & Buys, S. (2003). Reported family history of cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. American Journal of Epidemiology, 157(9), 792–799.
Quillin, J. M., Ramakrishnan, V., Borzelleca, J., Bodurtha, J., Bowen, D., & Baer Wilson, D. (2006). Paternal relatives and family history of breast cancer. American Journal of Preventive Medicine, 31(3), 265–268. doi:10.1016/j.amepre.2006.05.002.
Radloff, L. S. (1977). The CES-D scale a self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Shamliyan, T. A., Duval, S., Du, J., & Kane, R. L. (2008). Just what the doctor ordered. Review of the evidence of the impact of computerized physician order entry system on medication errors. Health Services Research, 43(1 Pt 1), 32–53. doi:10.1111/j.1475-6773.2007.00751.x.
Simon, C., Acheson, L., Burant, C., Gerson, N., Schramm, S., Lewis, S., et al. (2008). Patient interest in recording family histories of cancer via the Internet. Genetics in Medicine, 10(12), 895–902. doi:10.1097/GIM.0b013e31818de708.
Smith, M., Dang, D., & Lee, J. (2009). E-prescribing: clinical implications for patients with diabetes. Journal of Diabetes Science and Technology, 3(5), 1215–1218.
Uhlmann, W. R., Schuette, J. L., & Yashar, B. (2011). A guide to genetic counseling: Wiley. com.
Weidmar, B., Brown, J., & Garcia, L. (1999). Translating the CAHPS 1.0 survey instrument into spanish. Medical Care, 37(3 Suppl), MS89–MS96.
Weinrich, S. P., Faison-Smith, L., Hudson-Priest, J., Royal, C., & Powell, I. (2002). Stability of self-reported family history of prostate cancer among African American men. Journal of Nursing Measurement, 10(1), 39–46.
Westman, J., Hampel, H., & Bradley, T. (2000). Efficacy of a touchscreen computer based family cancer history questionnaire and subsequent cancer risk assessment. Journal of Medical Genetics, 37(5), 354–360.
Wham, D., Vu, T., Chan-Smutko, G., Kobelka, C., Urbauer, D., & Heald, B. (2010). Assessment of clinical practices among cancer genetic counselors. Familial Cancer, 9(3), 459–468. doi:10.1007/s10689-010-9326-9.
Wideroff, L., Garceau, A. O., Greene, M. H., Dunn, M., McNeel, T., Mai, P., et al. (2010). Coherence and completeness of population-based family cancer reports. Cancer Epidemiology, Biomarkers and Prevention, 19(3), 799–810. doi:10.1158/1055-9965.epi-09-1138.
Widmer, C., Deshazo, J. P., Bodurtha, J., Quillin, J., & Creswick, H. (2013). Genetic counselors’ current use of personal health records-based family histories in genetic clinics and considerations for their future adoption. Journal of Genetic Counseling, 22(3), 384–392. doi:10.1007/s10897-012-9557-z.
Willis, G. B. (2004). Cognitive interviewing: A tool for improving questionnaire design. Thousand Oaks: Sage Publications.
Ziogas, A., & Anton-Culver, H. (2003). Validation of family history data in cancer family registries. American Journal of Preventive Medicine, 24(2), 190–198.
Acknowledgments
This work was supported by the Cancer Prevention and Research Institute of Texas (grant #PP110220). The authors thank the support of the entire staff of the UT Southwestern Cancer Genetics group, Parkland Hospital Oncology and John Peter Smith Hospital, as well as the UT Southwestern Clinical Sciences Department, including Dr. Celette Skinner, Saddyna Belmashkan, and Maria Funes.
Conflict of interest
Mary Pritzlaff, Arielle Yorczyk, Linda S Robinson, Sara Pirzadeh-Miller, Tirun Lin, David Euhus and Theodora Ross, declare that they have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. An informed consent waiver was obtained from the Institutional Review Board for all patients that were included in the study.
Human and Animal rights
No animal or human studies were carried out by the authors for this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Mary Pritzlaff and Arielle Yorczyk contributed equally to this work.
Rights and permissions
About this article
Cite this article
Pritzlaff, M., Yorczyk, A., Robinson, L.S. et al. An Internal Performance Assessment of CancerGene Connect: An Electronic Tool to Streamline, Measure and Improve the Genetic Counseling Process. J Genet Counsel 23, 1034–1044 (2014). https://doi.org/10.1007/s10897-014-9732-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-014-9732-5