Abstract
Family history questionnaires (FHQ) are useful tools for cancer genetic counseling, providing an informational basis for pedigree construction and individualized cancer risk assessment. Reported return rates of mailed FHQs amongst familial cancer clinics that utilize them are lower than desired however, and it is unknown whether patients perceive required completion of a FHQ as a barrier to access of cancer genetics services. This study critically evaluated the use of a mailed FHQ for all routine new patient referrals to a single hereditary cancer clinic in Quebec, Canada. Reasons for response/non-response to a FHQ and the effect of administration of a questionnaire on patients’ self-reported level of motivation to pursue genetic counseling, were examined. Of 112 eligible individuals referred during the study period, 86 completed a semi-structured telephone survey; of these, 45% had returned the mailed FHQ prior to the telephone survey (Responders) and 55% had not (Non-responders). Overall, the majority of participants indicated a FHQ is an acceptable and understandable method of collecting family history information. Most prevalent reasons for not returning the FHQ were (bad) timing (56%), and difficulty accessing family history information (46%). Non-response was significantly associated with difficulty in asking relatives for the requested information (p = 0.011), and Non-responders cited fewer overall perceived benefits of cancer genetic counseling as compared with Responders (p < 0.0001). One quarter of Non-responders returned the mailed FHQ following administration of the telephone survey, suggesting implementation of a follow-up prompt is a cost-effective way to increase response.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of individuals seeking cancer genetic counseling services across North America has risen steadily over the past ten years, owing in part to greater public awareness of the availability of genetic testing for a variety of hereditary cancers. In an effort to streamline the referral process to hereditary cancer services and reduce patient waiting lists, genetic counselors have developed clinical tools such as the family history questionnaire (FHQ) to collect pertinent medical, cancer, and family history information in advance of the first genetic counseling session. By doing so, patients can be provided with a more accurate cancer genetic risk assessment without the need for multiple clinic visits. One major limitation of this approach, however, is that reported return rates of mailed FHQs amongst clinics that utilize them is lower than desired (Armel et al. 2009; Mancuso et al. 2004; Rahm et al. 2007). Also, it is not known whether the use of a mailed FHQ represents a barrier to patients wishing to access hereditary cancer services.
Central to nearly every cancer risk assessment is the careful collection and interpretation of a patient’s personal and family history of cancer. A comprehensive cancer history provides the genetic counselor with a basis for estimating the likelihood of a hereditary cancer syndrome in a family and determining eligibility for genetic testing. While many familial cancer clinics utilize a questionnaire or its equivalent to collect family history information, some centers may choose to obtain medical and cancer histories by telephone or at the first clinic visit. These differences may simply reflect individual preferences of a clinical service, the extent of patient waiting lists, existing hospital policies, and/or available resources. Despite these differences, no research to date has systematically examined whether patients themselves perceive the use of mailed FHQs to be an obstacle or even deterrent to access of hereditary cancer services, although several studies have investigated related questions. In the context of using a cancer FHQ as a screening tool in general practice, Leggatt et al. (2004) determined that administering the questionnaire did not increase a patient’s anxiety or cancer-related worry. Similarly, in an Ontario-based study, Armel et al. (2009) found use of a self-administered, mailed FHQ in a hereditary breast and ovarian cancer (HBOC) clinic was an effective means of both obtaining cancer family history information and assessing eligibility for genetic testing. Specifically, only 5% of families in their study acquired changes during genetic counseling that altered their eligibility for genetic testing. One limitation of their study, however, is that cancer risk level and eligibility for testing amongst the nearly half of all referred patients who did not respond to the FHQ were not assessed, nor was the reason(s) for non-response. In a recent follow-up study, Armel et al. (2011) found non-responders to a mailed FHQ who subsequently provided their family history by phone (28%), were less likely to be eligible for genetic testing. Among these non-responders, 114 (53%) provided reasons for not completing the mailed FHQ. Reasons included lack of familiarity with their family history (25%), being busy, procrastinating or having forgotten (26%), never having received the mailed FHQ (19%), and feeling overwhelmed or confused (19%).
In a study conducted by the Ontario Familial Cancer Registry, Mancuso et al. (2004) found that low return rates for a self-administered questionnaire can be improved with additional prompting. Amongst the group of patients who initially did not return a mailed FHQ, 42% were later willing to provide the information when questioned over the phone. Those who still declined to complete the questionnaire by phone cited reasons such as lack of knowledge regarding their family history, death/illness in the family, the subject matter being too distressing, and not remembering the information. These researchers also found that the group of self-identified visible ethnic minorities was less likely to respond to the mailed questionnaire than the telephone interview, with 12.3% citing language as a barrier for not completing the mailed questionnaire (Mancuso et al. 2004).
One possible explanation for low FHQ return rates is that non-completion of the questionnaire may reflect an implicit decision by the patient not to pursue cancer genetic counseling at a particular point in time. In this respect, studies investigating why patients do not pursue genetic counseling have found that for some, this is a considered decision, while for others, genetic counseling is an option they are still considering but are not actively pursuing for a variety of reasons (Culver et al. 2001; Ford et al. 2007; O’Neill et al. 2006; Thompson et al. 2002). O’Neill et al. (2006) found that of 43 women offered genetic counseling for HBOC, 36% declined immediately while a further 27% still intended to pursue genetic counseling even 6 months after the initial referral. Among those who declined, there were no differences noted in their knowledge or awareness of cancer, but they were more likely to cite reasons for declining such as not wanting more tests, already having enough information about their risk, and not having enough time. Notably, nearly 50% of their participants who did accept genetic counseling, did so only after a follow-up call, citing forgetfulness, lost paper work, or waiting to be called as reasons for not pursuing genetic counseling at the initial time of offer. Similar studies have reported a variety of patient-specific reasons for declining cancer genetic counseling such as a belief that genetic counseling is not useful if it cannot prevent cancer, and a belief that a patient’s own behavior ultimately moderates risk (Ford et al. 2007). A Dutch study also found that immediate decliners of cancer genetic counseling tended to be older, reported a lower perceived risk, saw fewer benefits for testing, and expressed a general disbelief in the process as a reason for declining (Schlich-Bakker et al. 2007).
Factors associated with a decision to pursue cancer genetic counseling have also been investigated. Commonly cited reasons include a belief that genetic test results will help to make treatment decisions, wanting to know whether children are at increased risk (Cappelli et al. 1999; Patenaude et al. 1996), having a higher perceived risk of breast cancer (Culver et al. 2001), and being self-referred (Hagoel et al. 2000). Patient-specific variables such as a high degree of worry or cancer-related distress have also been shown to increase uptake of genetic counseling services (Keller et al. 2004; Thompson et al. 2002).
Although not directly addressed in the literature, there may be several benefits to genetic counselors having patients’ cancer and family history information prior to the first clinic visit. These may include more efficient triage of patients based on risk level, the ability to provide a more complete risk assessment and determine eligibility for genetic testing, and the opportunity to collect medical records on affected relatives, all while allocating less time during genetic counseling sessions for family history-taking. In their study of the informational needs of patients attending genetic counseling for familial breast and ovarian cancer, Hallowell et al. (1997) found that patients also recognize the importance of completeness of cancer family history information for the genetic counseling process. Among those patients surveyed, only 35% reported feeling adequately prepared for their appointment despite having been mailed a cancer family history form prior to their first clinic visit. Nearly one third reported a preference for more information beforehand on the precise details required from their cancer family histories; and gaps in their ability to provide these details resulted in a worry for these patients that the risk assessments provided were not accurate. These findings suggest there may be a greater incentive for patients to complete and return the FHQ if the purpose, nature, and anticipated benefits of having complete cancer family history information are clearly stated up-front.
Purpose of the Present Study
A few studies have examined the effectiveness of a FHQ as a clinical tool in genetic counseling. However, no study to date has assessed whether use of a self-administered mailed questionnaire within a familial cancer clinic is perceived by patients to be a barrier to access of cancer genetic counseling services. Furthermore, it remains unclear as to whether patients’ level of motivation to pursue genetic counseling can be reasonably inferred from their decision to complete/not complete a FHQ.
The Hereditary Cancer Clinic at the Montreal General Hospital, Quebec, Canada, utilizes a mailed FHQ to collect pertinent medical, cancer, and family history information for all routine new patient referrals. Within this patient population, an appointment is given once the completed questionnaire is returned, thereby prioritizing clinic appointments for those patients who return the FHQ. The aim of this study was to critically evaluate the use of a self-administered mailed questionnaire within a busy, university hospital-based hereditary cancer clinic and to elucidate patients’ opinions of the questionnaire and reasons for response/non-response. A secondary aim was to assess the effect of administration of a mailed FHQ on patients’ self-reported level of motivation to pursue cancer genetic counseling.
Methods
Background: Family History Questionnaire (FHQ)
The Hereditary Cancer Clinic at the Montreal General Hospital (McGill University Health Centre) in Quebec, Canada, utilizes a mailed FHQ, available in both English and French versions, to collect relevant medical, cancer and family history information for all routine new patient referrals. The FHQ is comprised of a series of tables and questions designed to elicit a three-generation pedigree for both maternal and paternal sides of the family, with a focus on first and second-degree relatives. For ease of completion, the questionnaire is organized by section, from most closely related relatives (children, siblings, parents) to more distantly related relatives (aunts/uncles, cousins). Information requested includes total number of relatives both living and deceased, cancer type (e.g., breast, colon) and age at diagnosis (if known) for all affected individuals, the treating hospital and year hospitalized, current age or age at death for all relatives, and cause of death, if known. Since completion of the FHQ may require the patient to consult with his/her family members, release of medical information forms (2) as well as a Patient Information Sheet are provided outlining the reasons why this information is being requested as well as what to expect from the overall genetic counseling process.
Recruitment of Sample
Of 373 individuals referred to the Hereditary Cancer Clinic during the study period from May to December 2008, the most common indications for genetic counseling included a personal or family history of breast/ovarian cancer, colon cancer, and a variety of polyposis conditions. Of note, at the time of study recruitment and to date, there exist no formal referral guidelines or “criteria” for cancer genetic counseling within the institution under study or within the province of Quebec, Canada.
Amongst all new patient referrals received during the study period, 112 were identified as being eligible for this study. Eligibility was based on the following criteria: referral triaged as routine based on information provided by referring physician, having been sent a FHQ by mail upon receipt of referral, ≥18 years of age, able to respond to a telephone interview in English or French, no known hereditary syndrome in the patient or family, and not identifiable on the initial referral as being terminally ill. Over half of the group of ineligible patients included young female breast cancer patients of Ashkenazi Jewish or French Canadian background, for whom eligibility for testing of recurrent founder mutations in the BRCA1/2 genes could be determined based on the referral information provided. At the time of recruitment for this study, this group of patients were offered an appointment date for genetic counseling in advance of being mailed a FHQ. In this way, FHQ return rates as a measure of motivation to pursue genetic counseling could not be reliably measured in this population. Similarly, referrals for assessment of rare syndromes which may or may not be accompanied by a positive family history (e.g., Gorlin syndrome, Cowden syndrome, Familial Adenomatous Polyposis) were deemed ineligible as these patients are typically offered a genetic counseling appointment irrespective of their family histories.
Approval for this study was obtained from the Montreal General Hospital, McGill University Health Centre, Research Ethics Board. Prospective participants were contacted via a study invitation letter which briefly outlined the goals and requirements of the study and informed them that further contact from the Study Coordinator (JAT) would be made by telephone in two to three weeks time to assess their interest in the study. A second copy of the FHQ was also included with the study invitation letter.
Eligible individuals referred to the Hereditary Cancer Clinic between May to December 2008 were contacted in four successive groups, after an average of 3 months (range 2 to 4.5 months) had elapsed from the time the initial FHQ was mailed (Appendix A). Group sizes were limited by the number of referrals received during each time frame. Those in groups 1 through 3 who were not successfully contacted within their group were included in the next group’s contact time frame. For those individuals who expressed interest in participating in the telephone survey, a convenient date and time to complete the survey was agreed upon with the Study Coordinator. All individuals who agreed to participate in the study were provided with further information regarding the purpose of the study, confidential participation with anonymized responses, intent to publish results, and freedom to withdraw at any time without penalty. Verbal consent was then obtained.
At the point of study entry, eligible individuals were classified as Responders or Non-responders based on whether or not their FHQ had been received by the Hereditary Cancer Clinic prior to the mailing of the study invitation letter (average of 3 months from date of referral). At the time of the telephone survey, participants who either indicated their FHQ was in the mail or that all required information had been compiled and return of their FHQ was imminent, were also included in the Responder group. Eventual return of the FHQ at any point during the duration of the study was tracked for these participants as well as for Non-responders. Following the study close date, those Non-responders who had since returned the FHQ (n = 21), and those Responders who had indicated imminent return but whose FHQ was not received within 3 weeks of the study close date (n = 1) were reclassified as “Intenders” (Appendix A). The “Intender” group was designated to minimize potential bias introduced by the study intervention (i.e., telephone survey). The data were then re-analyzed to determine whether the inclusion of this third group changed the findings of the original analysis of Responders versus Non-responders. As the inclusion of the Intender subgroup did not significantly change the study findings, presentation of these data is limited to the results section “Intention to Complete the FHQ.”
Survey Instrument
A 43 question semi-structured telephone survey was developed by the authors (Appendix B). The survey was divided into five sections based on a review of the relevant literature concerning identification of factors influencing return rates of mailed FHQs and uptake of cancer genetic counseling services. Section one included closed-ended ordinal-response questions about the referral itself such as whether it was self- or doctor-initiated and the adequacy of information provided by the referring doctor regarding the reason(s) for consultation. Participants were then asked to recall their level of motivation to pursue cancer genetic counseling at the time of initial referral and to assign a value between 1 and 10 on a continuous rating scale (i.e. Likert-type scale), with 1 indicating very low level of motivation and 10 representing very high motivation. Section two focused on the content of the FHQ, including the clarity of instructions, understandable purpose, length, degree of difficulty in obtaining requested information, and appropriateness of language. These variables were measured using closed-ended questions with three possible ordinal responses: yes, no or somewhat. To assess whether receipt of the FHQ changed a participant’s initial self-reported level of motivation at time of referral, three possible ordinal responses were used: increased, decreased or unchanged. Section three was applicable only to those who had not returned the FHQ (labeled “Non-Responders”) and focused on commonly cited reasons for non-response: lack of familiarity with their family history, the timing of the referral, level of cancer distress, and intent to complete the FHQ in the future (Culver et al. 2001; Geer et al. 2001; O’Neill et al. 2006). These variables were also measured using closed-ended questions with three possible ordinal responses: yes, no or somewhat. Additional reasons for non-response were elicited through an open-ended question. Section four assessed opinions regarding the perceived utility of cancer genetic counseling through closed-ended ordinal-response, and open-ended questions. Section five elicited demographic data including age, gender, ethnicity, cancer status, type of cancer, time since diagnosis, children, employment status and difficulty in attending medical appointments. Additional comments and suggestions regarding the FHQ and the referral process were collected through a final open-ended question.
Data Analysis
Quantitative data were coded and analyzed using SPSS software (Windows), version 11.5.1 or GraphPad InStat version 3.1a for Macintosh, GraphPad Software, San Diego California USA, https://doi.org/www.graphpad.com. Closed-ended questions with ordinal responses (e.g., yes, no, or somewhat) were analyzed using Pearson’s chi-square test where possible; however, when the distribution of ordinal responses was insufficient to meet the minimum number of expected observations per cell required for a valid chi-square calculation, the ordinal responses were re-coded into binary responses (e.g., yes = yes and not-yes = no and somewhat) and analyzed using a two-sided Fisher’s Exact test. Continuous data, such as motivation level, age, and time since cancer diagnosis were analyzed using one-way ANOVA. Motivation level was then re-coded into ordinal responses (e.g., < 7 and ≥ 7) based on the mean level of motivation between Responders (6.85) and Non-responders (8.16) and analyzed using a two-sided Fisher’s Exact test. Age was re-coded into ordinal responses of equivalent n and analyzed using Pearson’s chi-square test. Demographic data, such as ethnicity and cancer type was divided into sub-categories, such as French-Canadian, Ashkenazi Jewish, Caucasian-other and non-Caucasian; and breast cancer, colon cancer and cancer-other, and analyzed using Pearson’s chi-square test.
All participants were presented with five reasons cited in the literature as to why cancer genetic counseling may be useful (Pros) and nine reasons why this service may not be useful (Cons). Summed scores of Pros and Cons were calculated for each participant by awarding points for agreement or partial agreement with each reason why cancer genetic counseling may be useful and by likewise subtracting points for each reason why it may not be useful. The summed score could range from -9 to +5, depending on the combined total of Pros / Cons measured.
Results
Sample Demographics
From 373 individuals referred to the Hereditary Cancer Clinic during the study period, 112 were deemed eligible for participation in the telephone survey. Of these 112 eligible individuals who were mailed a study invitation letter, 86 (77%) consented to participate in the telephone survey. Seven individuals declined participation; six for unknown reasons (i.e., not stated) and one citing personal distress due to parental illness. Four individuals were excluded from the study group due to an inability to complete the survey by phone (language barrier or hearing disability), and the remaining 15 individuals were not available to complete the telephone survey during the study period, despite a minimum of five contact attempts. The 13% (n = 15/112) of possible individuals who were not reachable during the study period were not significantly different than those who participated in the study, according to the basic demographic information provided with the referral (data not shown). Of the 86 participants, 39 (45%) were classified as Responders, and 47 (55%) were classified as Non-responders.
Table 1 summarizes the response rates and demographic characteristics of the study participants. No significant differences were noted between the Responder and Non-responder groups, with the exception that Non-responders (34%, n = 16/47) were more likely to have been referred for a personal risk assessment of colon cancer than Responders (10%, n = 4/39) (p = .017).
Referral Characteristics
Seventy-four percent (n = 64/86) of all participants reported that their referral was doctor-initiated whereas 26% (n = 22/86) reported being self-referred. There was a non-significant trend towards more self-initiated referrals amongst Responders (33%, n = 13/39) than Non-Responders (19% n = 9/47) (p = .15). The initial mean level of self-reported motivation was significantly higher for self-initiated referrals (8.7; SD = 1.8) than doctor-initiated referrals (7.0; SD = 3.0) (t-test = 2.393, DF = 82, p = .019). Among all participants, 42% (n = 36/86) indicated they received sufficient information from their doctor regarding the reason for referral for cancer genetic counseling, and no significant differences were noted between Responder and Non-responder groups.
Opinions Regarding the Family History Questionnaire
Overall, the majority of participants had a good understanding as to why the information detailed in the FHQ was being requested (90%, n = 74/86), found the instructions for completing the FHQ to be clear (93%, n = 75/86), and the length to be appropriate (84%, n = 68/86) (Table 2). Among all participants, 32% (n = 26/86) found the information requested hard to obtain, and 28% (n = 23/86) found it difficult to ask their relatives for information about their personal cancer history. Non-Responders (40%, n = 17/47) were significantly more likely than Responders (15%, n = 6/39) to find it difficult to ask their relatives for information (p = .011). There was a non-significant trend towards Non-responders (24%, n = 10/47) being more likely than Responders (8%, n = 3/39) to find the FHQ too long (p = .069) (Table 2).
Reasons for Non-response
The most commonly cited reason for non-response to the FHQ was (bad) timing (56%, n = 25/47), followed by lack of familiarity with family history (46%, n = 21/47), cancer-related distress (31%, n = 14/47), and forgetfulness (17%, n = 8/47) (Table 3). Additional reasons offered included wanting a FHQ in French instead of English (or vice versa), ongoing radiotherapy, recent surgery, feeling the requested information was too personal and private to provide, concern regarding the impact on one’s ability to acquire insurance, a belief that one’s cancer is clearly genetic and thus an appointment would not be necessary, and a belief that release of information forms (provided with the FHQ) must be completed and returned with the FHQ. Overall, 20% (n = 16/86) of all participants stated a preference for their referring physician to have collected the information. While participants were not specifically asked about a preference for an alternate mode of delivery (i.e. in person, by phone or by email), no participant expressed a preference for an alternate mode of delivery during the open ended question.
Although the vast majority of Non-responders (89%, n = 41/47) indicated they intended to return the FHQ in the future, 63% (n = 29/47) still stated their desire to have an appointment without the necessity of first having to complete the FHQ, and 20% (n = 9/47) stated they were unsure about wanting an appointment without the FHQ.
Motivation Levels
Participants were asked to recall and rate their level of motivation to pursue cancer genetic counseling at different time points, both before (continuous rating scale) and after receipt of the FHQ (increased, decreased or unchanged motivation). The mean self-reported level of motivation for all participants at the time of physician referral was 7.4 (SD = 2.8) (on a Likert scale of 1 to 10) (Table 4), and was significantly higher among Responders (8.2; SD = 2.5) than among Non-responders (6.8; SD = 2.9) (F-test = 4.8, DF = 83, p = .032). Regarding the effect of receipt of the FHQ on initial motivation levels, Non-responders (60%, n = 26/47) and Responders (63%, n = 24/39) were equally likely to report no change in motivation whereas Non-responders were significantly more likely to report a decrease in motivation (26%, n = 11/47 vs. 5%, n = 2/39) while Responders were more likely to report an increase (32%, n = 12/39 vs. 14%, n = 6/47) (p = .001). The mean summed score of perceived Pros / Cons of cancer genetic counseling was significantly lower among participants with an initial motivation rating of less than 7 (1.5; SD = 2.7) when compared to those with self-reported motivation level of 7 or above (3.5; SD = 1.2) (t-test = 4.5, DF = 77, p < .0001) (Table 4).
Motivation measures before and after receipt of the FHQ were correlated; those who reported no effect on motivation due to introduction of the FHQ had a higher initial mean level of motivation (8.2; SD = 2.3), while those who reported a change in motivation following receipt of the FHQ (increased or decreased) had, on average, lower initial mean levels of motivation (6.9; SD = 2.7 and 6.3; SD = 3.1, respectively) (F-test = 3.8, DF = 78, p = .027) (Table 4). A reported decrease in motivation due to the FHQ was significantly associated with finding the FHQ too long (42%, n = 5/12 vs. 10%, n = 6/67, p = .001) and a preference for the referring doctor to collect the information (55%, n = 6/11 vs. 15%, n = 10/68, p = .007).
Perceived Utility of Cancer Genetic Counseling
The majority of participants (90%, n = 75/83) indicated cancer genetic counseling would be useful, according to the reasons presented in Table 5. Additional reasons cited included “helping the cause,” and aiding in cancer research. The mean summed score of Pros / Cons for cancer genetic counseling, representing the number of reasons why genetic counseling would/would not be useful, was significantly higher among Responders (3.5; SD = 1.5) than Non-responders (2.6; SD = 2.2) (t-test = 2.2, DF = 76, p = 0.03) (Table 5). Those who believed that cancer genetic counseling would be useful were significantly younger (mean = 46 years; SD = 13.1) than those who did not (mean = 60 years; SD = 14.2) (F-test = 8.3, DF = 82, p = .005).
Intention to Complete the FHQ
Eventual return of the FHQ by Non-responders after the study close date was tracked, and these individuals were reclassified into a third group labeled as “Intenders” (see Methods). Data were then re-analyzed in order to determine if the introduction of the Intender group changed the findings. Overall, Intenders (n = 22) appear more similar to Responders (n = 38) than Non-responders (n = 26), and were in general, intermediate to the two groups. The mean initial level of motivation was highest among Responders (8.1; SD = 2.6), intermediate among Intenders (7.5; SD = 2.5) and lowest among Non-responders (6.4; SD = 3.0) (F-test = 3.2, DF = 83, p = .047). Intenders were more likely than Non-responders to state an intention to return the FHQ in the future (95%, n = 20/21 vs. 72%, n = 18/25) (p = .043), and were less likely to cite bad timing as a factor in not returning the FHQ (27%, n = 4/15 vs. 60%, n = 18/30, p = .036). Overall, Intenders had a significantly more positive opinion towards the utility of cancer genetic counseling than Non-responders (3.5; SD = 1.0 vs. 1.8; SD = 2.8) (t-test = 2.7, DF = 27, p = .01, Fig. 1). Non-responders were more likely than Intenders to cite already having enough appointments or tests (22%, n = 5/23 vs. 0%, n = 0/21) (p = .043), not having enough time (35%, n = 8/23 vs. 5%, n = 1/21) (p = .016), and already having enough information regarding their cancer risk (30%, n = 7/23 vs. 0%, n = 0/21) (p = .006) as reasons for why cancer genetic counseling would not be useful.
Discussion
Response Rates: Who, When and Why
The response rate achieved for this study was very positive, with 77% of eligible individuals consenting to participation and only 6% (n = 7/112) declining participation (Table 1). This finding is consistent with the generally high response rates achieved by researcher-administered questionnaires and was likely influenced by the inclusion of study design elements such as preliminary and personalized notification, confidential participation with anonymized responses, and a stated study goal of improving patient care, which have been shown to increase response rates (Ornstein 1998). The majority of telephone surveys were conducted outside of regular work hours, which may have also influenced the perceived value of the study or the ability to make contact with potential participants.
Most of the participants in this study were white women in early middle age, without a personal history of cancer. Given that close to two-thirds of referrals were for personal or family history of breast cancer, these characteristics are perhaps not unexpected. The sample was, however, biased towards unaffected patients due to the nature of the intake process of the clinical service studied, whereby unaffected patients are more likely than affected patients to be triaged as routine referrals and therefore mailed a FHQ. Those individuals (n = 15) who were not reachable during the study period were not significantly different than those who participated in the study, according to the basic demographic information provided with the referral. However, those patients who were excluded from participation (n = 4) were either individuals whose comprehension of English or French was not sufficient to complete the telephone survey, or individuals with a hearing disability. As such, these two groups may be under-represented in the study findings. Overall, given the high response rate, the study population is likely to be a good representation of all routine patient referrals to the hereditary cancer clinic studied.
No Time/Bad Time: The Importance of Timing
Overall, a majority of participants regarded the FHQ as user-friendly and adequate for its intended task, that is, the collection of family history information. A few participants, however, would have benefitted if the FHQ were available in a language other than English or French. The most commonly identified factor contributing to non-response was (bad) timing. For some, a lack of free time to collect family history information was attributed to the competing demands of everyday life and work, while for others, (bad) timing was due to other significant life events such as an illness in the family. The decision to embark on the sometimes lengthy process of cancer genetic counseling must be balanced against other existing demands of work and family life, whereby the latter often assume priority over one’s time. Over the short-term, these competing demands may contribute to a delay in completing the FHQ. Over the longer term, there may be a critical period after which time non-response will reflect an implicit decision not to pursue cancer genetic counseling altogether. While this study did not assess the timing of this critical period (if any), it is possible the onus of completing the FHQ may compound the timing factor for a proportion of referred patients such that the questionnaire does present a barrier to access of services. On the other hand, perhaps independent of the questionnaire, (bad) timing alone would preclude some individuals from pursuing cancer genetic counseling at any particular point in time. It is also possible, as has been suggested (O’Neill et al 2006), that timing (good or bad) has more to do with a person’s readiness to embark on the process of genetic counseling and that this readiness is independent of any requirement to provide family history information in advance of the first counseling session.
The FHQ is a Barrier to Access: True or False?
To assess whether the FHQ is perceived by patients to be a barrier to access of hereditary cancer services, there are two main questions to be considered: Are individuals who are motivated to pursue cancer genetic counseling likely to return the questionnaire? and if so, Are reasons for non-response independent of the FHQ?
To address these two important questions, recalled motivation levels for cancer genetic counseling prior to receipt of the FHQ were measured on a continuous rating scale. Among all participants, the mean level of self-reported motivation was relatively high. Among Non-responders, the mean level of motivation reported was significantly lower than among Responders; however, the significant overlap between the two groups begs the question whether the Non-responder group were making an informed, conscious choice to decline this service. In fact, nearly all participants endorsed the utility of cancer genetic counseling, and the majority of Non-responders indicated that they would want an appointment were it not necessary to complete the FHQ first. A reasonable conclusion from these findings is that non-response is an imperfect indicator of interest/motivation to pursue cancer genetic counseling.
In order to determine whether use of a mailed FHQ, in and of itself, poses a barrier to access of hereditary cancer services, this study elicited reasons for non-response. As mentioned previously, the most common factor cited for non-response was timing, which may or may not compound the onus of completing the FHQ into a barrier. The next most commonly cited reason, and a recurrent theme when evaluating the content of the FHQ and reasons underlying the utility of cancer genetic counseling, was accessibility of information. Difficulty in accessing information was significantly correlated with both non-response and a more negative view of the utility of cancer genetic counseling. These findings are consistent with those of Hallowell et al. (1997), and suggest some Non-responders may be equating poor information accessibility with a lower perceived value of cancer genetic counseling. While this study was not designed to specifically assess the mode of delivery of the FHQ, participants were questioned on whether they would have preferred their referring physician to collect the family history information. A small minority of both Responders and Non-responders preferred this option, and no participant expressed a preference for an alternate mode of delivery (in person, by phone or by email) during the open ended question regarding their opinion of the FHQ. Thus, mode of delivery does not appear to be a significant determinant of patients’ decisions to return/not return the FHQ.
Although the merits of offering an appointment to those with insufficient information about their family history are debatable given the role of family history in the risk assessment process, it may not render the assessment categorically inaccurate. Furthermore, patients may still have much to benefit from the psychosocial support provided through genetic counseling as well as any recommendations regarding cancer screening. One obvious concern is that receipt of the FHQ represents the first point of contact with this particular patient population. Therefore, inability to provide the requested information may be interpreted by some individuals to mean that an appointment would not be useful or even given, thereby compounding the influence on non-response. Interestingly, despite inclusion of a Patient Information Sheet with the mailed FHQ which clearly states that return of the questionnaire is encouraged even with incomplete information, a proportion of patients may still have equated poor information accessibility with a low perceived utility of the genetic counseling process. What remains unclear, however, is whether this perception would exist irrespective of the collection method (e.g., in person, by telephone) and if so, whether elimination of a useful clinical tool such as the FHQ would actually translate into improved uptake of cancer genetic counseling services.
To Return or Not Return: Is the FHQ Part of a Time-Dependent Decision Making Process?
Uptake of cancer genetic counseling has been considered within the psychodynamic framework of applied behavioral models and the decision to pursue or not to pursue genetic testing has been viewed as the culmination of a time-dependent decision making process (O’Neill et al. 2006). In the present sample, the summed score of Pros and Cons towards the utility of cancer genetic counseling was calculated for Responders, Intenders and Non-responders. This summed score can be viewed as a numerical representation of the beliefs and attitudes pertaining to a particular health behavior (in this case, cancer genetic counseling), where the Pros of a specific course of action will begin to outweigh the Cons, with progression through successive stages of the decision making process (O’Neill et al. 2006). Non-responders had a significantly lower mean summed score than both Intenders and Responders, who had equivalent scores (Fig. 1). Given that the majority of Non-responders expressed their intention to return the FHQ, for many in this group, this lower score may reflect an early stage in the decision making process. With time, the balance of Pros and Cons can be expected to shift sufficiently to prompt a decision to either return the FHQ, and therefore embark on the genetic counseling process, or not. In the meantime, an opportunity exists for a targeted intervention (e.g., a telephone prompt) that could positively shift the Pro/Con balance such that “early-stage” Non-responders could be influenced towards returning the FHQ.
Intervention Effect
The value of a timely intervention in increasing uptake of genetic counseling has been demonstrated in a related study where the majority of referrals to a cancer genetics clinic were completed subsequent to a follow-up prompt (O’Neill et al. 2006). In the present study, the administration of the telephone survey and the inclusion of a second copy of the FHQ with the Study Invitation Letter can be considered as a follow-up prompt to the initial mailed FHQ. Following completion of the telephone survey, any outstanding participants questions were answered. Eleven percent of Non-responders stated that participation in the survey would prompt them to return the FHQ. As of July 1, 2009 (nearly 6 months after the final group of participants were initially contacted about the study), 61% of study participants had returned their FHQ (all but four of these patients subsequently attended genetic counseling appointments), representing a significant increase from the same time frame in the preceding year (37%). Notably, one fifth of FHQs (n = 22/112) from the study group were returned only after administration of the telephone survey. These findings suggest that incorporating a follow-up prompt to Non-responders, whether by a letter or a phone call, may be a simple and cost-efficient strategy to increase uptake.
Do Low FHQ Return Rates Matter?
An important question when evaluating the use of a self-administered questionnaire is whether response/non-response correlates with hereditary cancer risk level. For example, are Non-responders failing to respond to the FHQ because they evaluate their own family history of cancer to be insufficiently worrisome to pursue cancer genetic counseling (Culver et al. 2001; Schlich-Bakker et al. 2007)? Conversely, do high-risk patients with extensive family histories find it psychologically burdensome to complete the FHQ and therefore choose not to do so (Keller et al. 2004; Thompson et al. 2002)? A recent Ontario study (Armel et al. 2011) examined a sample of non-responders to a mailed FHQ referred to a hereditary breast and ovarian cancer clinic who subsequently provided their family history by phone. They found these initial non-responders were less likely to be eligible for genetic testing than the responders to the mailed FHQ. Armel et al. further found the majority of non-responders to the mailed FHQ were either unreachable by phone, declined a hereditary cancer risk assessment, or had received a hereditary cancer risk assessment from another clinic.
Among the present participants, a non-significant trend towards a higher degree of doctor-initiated referrals was observed among Non-responders as compared to Responders, suggesting Non-responders may be less likely to find their family history of cancer sufficiently worrisome to raise the subject with their doctor. One concern, however, is that a patient’s perception of their own risk may be an imperfect indicator of their actual risk; thus, it is possible a proportion of non-responders are under-estimating their risk based on an inaccurate interpretation of their family histories.
While this study was not specifically designed to assess the correlation between response/ non-response and hereditary cancer risk level, the time to appointment among the group of Responders and Intenders can provide an indirect measure of risk for these subgroups (assuming that higher risk / urgent referrals are prioritized and given appointments first). Eligibility for this study required that all participants had been triaged as routine referrals based on the referral information provided. Upon receipt, all returned FHQs were reviewed by the clinical team as part of the existing triage protocol, and individuals then assigned a target for time to appointment based on an estimate of hereditary risk level. At the study close date, the mean time to appointment for the 66 Responders and Intenders with available data was 195 days (~ 6 months), corresponding to the typical wait time for routine patient referrals during the study period. Only 3 patients were seen within 3 months of returning their questionnaire, likely indicating a higher level of risk for a hereditary cancer syndrome. Although complete family history information was not available for Non-responders, if one were to assume a similar risk stratification among Non-responders based on the same triage protocol used for both groups of patients, this would correspond to approximately 1–2 individuals from the Non-responder group expected to be seen on an urgent/semi-urgent basis, or <5% of all routine referrals received during the study period. This estimate suggests that overall, the current intake process utilized by our clinic has an acceptable degree of specificity for identifying high-risk patients, and use of a self-administered questionnaire among routine referrals to this clinic does not appear to result in the exclusion of a significant number of high-risk individuals. Future studies to more specifically assess whether risk level is a significant determinant of response/non-response to a FHQ would provide further insight into this important question.
Study Limitations
One major limitation of this study is the findings are drawn from the experience of a single hospital center and a single, mainly bi-lingual (French, English) patient population. The results may therefore not be generalizable to other centers in North America offering cancer genetic counseling services. By design, the intake process of the Hereditary Cancer Clinic prioritizes high risk referrals to be booked directly, thereby excluding these patients from this study population. Thus, these findings may be more representative of lower/moderate risk patients and may not be applicable to the uptake of cancer genetic services among high risk patients.
In order to assess reasons for response/non-response to a FHQ prior to an intervention (in this case, a study survey), a retrospective study design was utilized. One limitation of this design; however, is that participants’ reported motivation levels may have been subject to recall bias. Additionally, self-reported motivation levels were highly weighted as a measure of interest in and eventual uptake of cancer genetic counseling; however, the reliability and validity of rating scales cannot be determined.
The generally positive response about the utility of cancer genetic counseling may have been subject to acquiescence bias introduced by the manner in which the questions were presented (i.e., a tendency to agree with survey questions) (McBurney 1994). Similarly, the act of conducting the survey may have biased participants’ opinions by increasing the perceived value of this service and introducing social desirability, such that participants tended to reply in a manner viewed favorably by others (McBurney 1994). Lastly, bias may have been introduced through the study design by allowing a minimum of 2 months (range 2 - 4.5 months) for return of the FHQ. While this decision was made on a logistical basis, in retrospect, when a 2007 comparison group was assessed for response rate, it was noted that the mean time to FHQ return was approximately 4 months. Given that 90% of study participants were contacted before 4 months, and 17 classified Non-responders also returned their FHQ before this time period, the Responder / Non-responder classification system may be slightly skewed in the direction of non-response. The Intender group; however, was introduced as a means to address this bias, and its inclusion did not significantly affect the findings of this study.
As an exploratory study, multiple univariate tests were conducted using a liberal alpha level of p ≤ .05, which increases the family-wise error rate. Thus, it is possible that some of the statistically significant findings are due to chance.
Practice Implications and Research Recommendations
This study demonstrates that within a busy university hospital setting, the collection of family history information via a mailed questionnaire is a practice that is both acceptable and understandable by the majority of patients referred to a hereditary cancer clinic. Moreover, the FHQ is not regarded as an unnecessary barrier to access of this service. While the requirement of family history information in advance of the first genetic counseling session may compound the effects of (bad) timing and lack of familiarity with one’s family history on non-response to a FHQ, these factors will to some extent remain independent of the FHQ. Patients with limited information accessibility may perceive that they have less to gain from genetic counseling and this perception may deter some from pursuing genetic counseling, irrespective of the collection method used. Furthermore, a proportion of patients citing (bad) timing as a reason for non-response may be at an early stage of deciding whether or not to pursue genetic counseling. Therefore, providing patients with an option to dictate the timing of their response to a mailed FHQ may actually be desirable.
Finally, while elimination of the FHQ would undoubtedly increase uptake of cancer genetic services as indicated by the relatively high motivation levels of all participants and their generally positive regard towards this service, this may not translate into an increase in the number of high-risk patients seen. On the contrary, the increased demands on clinical resources associated with obtaining family history information by telephone or at the first clinic visit would prompt a greater number of follow-up appointments and ultimately increase waiting times for newly referred patients. A reasonable compromise between maximizing uptake and judicious use of resources would be the implementation of a 4–6 month follow-up letter or telephone call to Non-responders to assess interest in cancer genetic counseling and to encourage return of the FHQ even with incomplete family history information. Future research to examine the relationship between information accessibility, hereditary risk level (actual and perceived), and response/non-response to a FHQ, could provide important insight to help clinics improve existing tools for family history collection. Additionally, further study is needed to explore whether the apparent perception of Non-responders that poor information accessibility equates with low perceived utility of cancer genetic counseling is dependent or independent on the method of family history collection used (e.g. FHQ, by phone, in-person).
References
Armel, S. R., McCuaig, J., Finch, A., Demsky, R., Panzarella, T., Murphy, J., et al. (2009). The effectiveness of family history questionnaires in cancer genetic counselling. Journal of Genetic Counseling, 18, 366–378.
Armel, S. R., Hitchman, K., Millar, K., Zahavich, L., Demsky, R., Murphy, J., et al. (2011). The use of family history questionnaires: an examination of genetic risk estimates and genetic testing eligibility in the non-responder population. Journal of Genetic Counseling. doi:https://doi.org/10.1007/s10897-011-9359-8.
Cappelli, M., Surh, L., Humphreys, L., Verma, S., Loga, D., Hunter, A., et al. (1999). Psychological and social determinants of women’s decisions to undergo genetic counseling and testing for breast cancer. Clinical Genetics, 55, 419–430.
Culver, J., Burke, W., Yasui, Y., Durfy, S., & Press, N. (2001). Participation in breast cancer genetic counseling: the influence of educational level, ethnic background, and risk perception. Journal of Genetic Counseling, 10, 215–231.
Ford, M. E., Hensley Alford, S., Britton, D., McClary, B., & Gordon, H. S. (2007). Factors influencing perceptions of breast cancer genetic counseling among women in an urban health care system. Journal of Genetic Counseling, 16, 735–753.
Geer, K. P., Ropka, M. E., Cohn, W. F., Jones, S. M., & Miesfeldt, S. (2001). Factors influencing patients’ decisions to decline cancer genetic counseling services. Journal of Genetic Counseling, 10(1), 25–39.
Hagoel, L., Dishon, S., Almog, R., Silman, Z., Bisland-Becktell, S., & Rennert, G. (2000). Proband family uptake of familial-genetic counseling. Psycho-Oncology, 9, 522–527.
Hallowell, N., Murton, N., Statham, H., Green, J. M., & Richards, M. P. M. (1997). Women’s need for information before attending genetic counselling for familial breast or ovarian cancer: a questionnaire, interview, and observational study. British Medical Journal, 314, 281–283.
Keller, M., Jost, R., Kadmon, M., Wüllenweber, H. P., Mastromarino Haunsletter, C., Willeke, F., et al. (2004). Acceptance of and attitude toward genetic testing for hereditary nonpolyposis colorectal cancer: a comparison of participants and nonparticipants in genetic counseling. Diseases of the Colon and Rectum, 47, 153–162.
Leggatt, V., Mackay, J., Marteau, T. M., & Yates, R. W. (2004). The psychological impact of a cancer family history questionnaire completed in general practice. Journal of Medical Genetics, 37, 470–472.
Mancuso, C., Glendon, G., Anson-Cartwright, L., Juqing, E., Andrulis, I., & Knight, J. (2004). Ethnicity, but not cancer family history, is related to response to a population-based mailed questionnaire. Annals of Epidemiology, 14, 36–43.
McBurney, D. H. (1994). Research methods. Pacific Grove: Brooks/Cole.
O’Neill, S. M., Peters, J. A., Vogel, V. G., Feingold, E., & Rubinstein, W. S. (2006). Referral to cancer genetic counseling: are there stages of readiness? American Journal of Medical Genetics, Part C, 142C, 221–231.
Ornstein, M. D. (1998). Survey research. Current Sociology, 46, iii–136.
Patenaude, A. F., Schneider, K. A., Kieffer, S. A., Calzone, K. A., Stopfer, J. E., Basili, L. A., et al. (1996). Acceptance of invitations for p53 and BRCA1 predisposition testing: factors influencing potential utilization of cancer genetic testing. Psycho-Oncology, 5, 241–250.
Rahm, A. K., Sukhanova, A., Ellis, J., & Mouchawar, J. (2007). Increasing utilization of cancer genetic counseling services using a patient navigator model. Journal of Genetic Counseling, 16, 171–177.
Schlich-Bakker, K. J., ten Kroode, H. F., Wárlám-Rodenhuis, C. C., van den Bout, J., & Ausems, M. G. (2007). Barriers to participating in genetic counseling and BRCA testing during primary treatment for breast cancer. Genetics in Medicine, 9, 766–777.
Thompson, H. S., Valdimarsdottir, H. B., Duteau-Buck, C., Guevarra, J., Bovbjerg, D. H., Richmond-Avellaneda, D. A., et al. (2002). Psychosocial predictors of BRCA counseling and testing decisions among urban African-American women. Cancer Epidemiology, Biomarkers & Prevention, 11, 1579–1585.
Acknowledgements
This study was financially supported by the Department of Human Genetics, McGill University. French translation was provided by Danielle Veyre (Study Invitation Letter) and Guillaume Sillon (Telephone Survey), whose help is gratefully acknowledged. Assistance in the statistical analysis was provided by Jean-Sébastien Brunet.
Author information
Authors and Affiliations
Corresponding author
Appendices
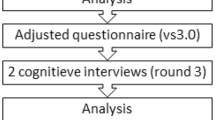
Appendix A: Study Design Flow-Chart

Appendix B




Rights and permissions
About this article
Cite this article
Appleby-Tagoe, J.H., Foulkes, W.D. & Palma, L. Reading Between the Lines: A Comparison of Responders and Non-responders to a Family History Questionnaire and Implications for Cancer Genetic Counselling. J Genet Counsel 21, 273–291 (2012). https://doi.org/10.1007/s10897-011-9399-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10897-011-9399-0