Abstract
The current study evaluated the effects of an intervention package designed to teach independent toileting skills to two boys with autism spectrum disorder (ASD). A non-concurrent multiple baseline across participants design was employed to investigate the effects of video modeling that utilized animation to depict in-toilet voiding combined with prompting and reinforcement procedures. Results indicated that the intervention package was effective in teaching a sequence of behaviors necessary for successful and independent toileting (e.g., walking to the toilet, undressing, sitting on the toilet, dressing, and flushing) as well as in-toilet urination for both boys. Skills generalized to the school and were maintained over 3 to 4 months. The intervention may have also been responsible for teaching in-toilet defecation for one participant. Results are interpreted in relation to the differential contributions of video modeling and behavioral instructional strategies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The acquisition of independent toileting skills is often delayed in children with developmental and intellectual disability and may not emerge without training that is more intensive than is required by typical developing children (e.g., Azrin and Foxx 1971; Radstaake et al. 2014; Szyndler 1996). For example, in a sample of 33 parents of children with ASD, up to 82 % reported difficulties toilet training their child (Szyndler 1996; Whiteley 2004). Toileting difficulties can result in reduced access to inclusive community settings, social stigma and inadequate hygiene (Cicero and Pfadt 2002; Kroeger and Sorensen-Burnworth 2009). Inadequate hygiene related to toileting may lead to physical ailments such as skin irritation and infection (e.g., Vermandel, Van Kampen, Van Gorp, and Wyndaele 2007). Finally, child incontinence can increase parental stress (Vermandel et al. 2007). Clearly, independent toilet use is a crucial life skill that has profound implications for independence, social relationships, vocational opportunities, and overall quality of life.
According to Lott and Kroeger (2004), there are two fundamental goals in toilet training; specifically, to recognize the need to go to the toilet and then to be able to independently complete the sequence of behaviors necessary for successful healthy toileting. Kroeger and Sorensen-Burnworth’s (2009) review of the literature identified 28 studies that focused on teaching toileting skills to individuals with developmental disabilities (including ASD) and reported that the most frequently recommended approaches are based upon the Rapid Toilet Training procedure (RTT) developed by Azrin and Foxx (1971). RTT involves several key components. These include: (a) scheduling specific opportunities for toileting, (b) increasing fluid intake, (c) providing reinforcement for voiding on the toilet, (d) graduated guidance prompting, and (e) delivering punishment (e.g., overcorrection, verbal reprimands) contingent on urination or defecation outside of the toilet (Rinald and Mirenda 2012).
RTT is a well-established evidenced-based practice (Kroeger and Sorensen-Burnworth 2009). However, RTT does not necessarily address collateral behaviors associated with completing a sequence of toileting behaviors (e.g., flushing the toilet, washing hands, etc.) and parents may oppose the use of punishment techniques. Further, Kroeger and Sorensen-Burnworth’s (2009) review highlighted the paucity of research examining parent training and social validity measures during toilet training interventions, as well as the lack of research investigating behaviors necessary for successful ongoing development, generalization and maintenance of independent toilet use.
Video modeling has been used successfully to teach children with a variety of diagnoses a diverse set of skills, including language, play, classroom behavior expectations, self-care, and social skills (e.g., Baker et al. 2009; Lang et al., 2009; Tereshko, MacDonald, and Ahearn 2010). Video modeling involves watching a video of a model engaging in target behaviors, with the goal that the observer will later imitate those behaviors. There are several types of video models including: (a) adult modeling, in which a familiar or unfamiliar adult models the targeted behavior; (b) peer modeling in which a same aged, familiar or unfamiliar peer models the target behavior; (c) video self-modeling which refers to the behavior being modeled by the children themselves (often requires video editing); and (d) point-of-view modeling that involves the video displaying the behavior as if through the eyes of the person engaging in the behavior. Each of these model types have been used effectively to teach target behaviors to children with ASD (McCoy and Hermansen 2007).
Despite the success of video modeling, only four previous studies have investigated the use of video modeling to support toilet training in children with ASD (Bainbridge and Myles 1999; Drysdale, Lee, Anderson, and Moore 2014; Keen, Brannigan, and Cuskelly 2007; Lee, Anderson, and Moore 2014). Bainbridge and Myles (1999) used a commercially-produced video in order to teach a 3-year old boy with autism to initiate toilet use. In this study, the video was followed by a verbal prompt “it’s time to go to the toilet”, and the child’s response to this priming was recorded. Keen, et al. (2007) also used a commercially-produced video as opposed to videos designed specifically for the target participant. In this study five children with autism, aged 4 years 5 months to 6 years 9 months, were taught to follow the steps in the toileting sequence, in addition to in-toilet elimination. The use of the video model was also paired with prompting and reinforcement. Although improvements in target skills were evident in both studies, independent movement through a sequence of behaviors related to toileting (e.g., undressing, redressing, flushing and washing hands) was not demonstrated in either of the studies.
Research comparing commercial- versus custom-made videos (Palechka and MacDonald 2010; Rosenberg, Schwartz, and Davis 2010) has indicated slower rates of skill acquisition with commercial videos. Lee and colleagues (2014) used a changing criterion design to assess the effects of an intervention package on toileting for a 4-year-old boy with ASD. The intervention was effective in teaching dressing, sitting on the toilet and flushing. However, the intervention did not result in the acquisition of reliable in-toilet voiding. The authors attributed this to the fact that in-toilet voiding was not shown in the training video due to privacy concerns. Due to concerns regarding privacy and the display of sensitive content (e.g., genitalia and excretion) in video models (Darden-Brunson, Green, and Goldstein 2008), Drysdale et al. (2014) developed a video that incorporated animation to depict in-toilet voiding. Use of animation allowed for content to be depicted that would otherwise be considered inappropriate to record using a live model. A multiple baseline across behaviors design was used to evaluate the effects of the intervention package on toileting skills for two boys diagnosed with autism. After introduction of the video demonstrating animated in-toilet urination, one participant acquired the skill. However, the other child already began using the toilet appropriately before introduction of the video. The effects of animation to support acquisition of in-toilet voiding therefore remain unknown (Drysdale et al. 2014).
The objective of the present study was to examine the effects of an intervention package that included video modeling, with animations that depicted both urination and defecation, combined with prompting and reinforcement on the toileting skills of two children with ASD. Generalization across settings and maintenance in the absence of ongoing intervention was also measured.
Method
Ethical Clearance and Informed Consent
Ethical clearance for the study was provided by the relevant University human ethics committee and a parent of each child provided written consent for their child to participate in the study.
Participants
Both participants met the following predetermined inclusion criteria: (a) a formal diagnosis of ASD, (b) between the ages of 3 and 10 years, (c) motor skill ability necessary to perform the steps of the toileting sequence (e.g. ability to mount and remain stably seated on the toilet), and (d) an absence of toileting skills (confirmed in baseline).
Harvey
Harvey was 8 years, 1 month old. He attended a special education school, and he was receiving approximately 10 h per week of home-based ABA therapy. Harvey had a score of 11 months on the receptive language, and 7 months and on the expressive language subdomains of the Vineland Adaptive Behavior Scales-II (VABS-II; Sparrow et al. 2005). He had a score of 2 years 1 month on the personal, 10 months on the domestic, and less than 1 month on the community daily living skills subdomains of the VABS-II. Harvey was still wearing diapers throughout the day and night as well as a one-piece suit in order to prevent fecal smearing. Harvey’s parents had previously attempted toilet training on several occasions but were unsuccessful. Harvey did not have any spoken language but was able to communicate basic one-word requests using a speech-generating device (SGD; Lang et al. 2014). For Harvey, the results of the two-stage stimulus preference assessment (Green et al. 2008) indicated that chocolate chips, Jellybeans, and pebbles candy were high level reinforcers. A talking puzzle was a moderate level reinforcer, and nuts and crackers low level reinforcers.
Joseph
Joseph was 7 years, 2 months old and attended a special education school. Joseph had an age-equivalent score of 8 months on the expressive language subdomain, and 1 year on the receptive language subdomain of the VABS-II. He had an age-equivalent score of 1 year 5 months on the personal, 10 months on the domestic, and 11 months on the community daily living subdomains of the VABS-II. Joseph was also receiving approximately 10 h of home-based ABA therapy each week. At commencement of the study, Joseph was not able to urinate or defecate on the toilet and was wearing diapers day and night. Joseph’s parents had unsuccessfully attempted to toilet train Joseph prior to this study. Joseph also did not have any spoken language and communicated basic one-word requests using a SGD. For Joseph chocolate chip cookies, sour gummy candy, and potato chips were high level reinforcers. A giant straw was identified as a moderate level reinforcer and popcorn and raisins were low level reinforcers.
Assessment of Imitation and Visual Discrimination Skills
The imitation and visual performance sections of the ABLLS-R (Partington 2010) were administered to both children in order to assess their imitation and visual discrimination skills and to attempt to account for potential variation between those children who may learn from video modeling and those who may not (Lindsay, Moore, Anderson, and Dillenburger 2013; Rayner 2014). Results of the ABLLS-R indicated Harvey was able to imitate touching his head and touching his mouth. Joseph was able to imitate touching his head, raising his arms up, and tapping the table.
In addition, a video modeling probe was conducted in order to determine whether each child was able to imitate one-step gross motor actions (e.g., clapping hands), one-step actions with objects (e.g., pushing a car), facial expressions (e.g., a surprised face), and single-word utterances (e.g., mumma) from a video model. The following steps were undertaken: (1) the child was seated at a table, (2) the necessary objects were placed within the child’s reach, (3) the child was cued to attend to the video, (4) the child was shown one of the actions and instructed to imitate that action (i.e., Copy me), (5) the video was paused, and the child was allowed 10 s to respond; if the child did not respond, then the next behavior to be imitated was played, (6) responses were recorded as correct, incorrect, or no response. Each behavior to be imitated was shown to the child twice in succession. The entire sequence of video modeling imitation probes was conducted three times. The video modeling probe indicated that both boys could imitate clapping hands and tapping the table.
Overall, the ABLLS-R and the imitation probes suggested that the participants had preliminary imitation skills but might experience some difficulty with an imitation based intervention (Rayner 2014). Therefore, based on previous research (e.g., Drysdale et al. 2014), a video chaining procedure was implemented. This involved showing the toilet training video in segments (as opposed from start to finish) wherein each step of the toileting sequence was shown directly before the child practiced that step. The video was only shown in its entirety after participants had reached acquisition criteria (see Data Collection and Dependent Measures).
Settings and Instructors
Baseline, intervention, follow-up, and all video recording were conducted within the children’s homes. No restriction was placed on the areas of the house that each child was able to roam during any of the study phases. Generalization probes were conducted at the children’s school bathroom. The school bathroom was adjacent to the children’s classroom and contained a toilet, sink, and shower area.
Parent Training
The children were supported to complete the toileting sequence by their parent. Training was provided to each parent before intervention commenced. Training was conducted by providing parents with a manual describing the intervention and data collection procedures. The researcher then explained the intervention in person and modeled procedures for each parent. The procedures were modeled with each child, until the parents demonstrated that they were able to implement each of the steps in the procedure with 100 % accuracy. Parents were able to demonstrate mastery of the procedures after two rehearsals. Generalization probes were completed by the classroom teacher or teacher aide, with guidance from the researchers. The intervention procedures were modeled for the teacher and teacher aide using the method that was followed in order to train the parents.
Materials
Each child used a SGD (Apple iPod TouchFootnote 1 with Proloquo2GoFootnote 2) to communicate. A toilet symbol was added to the home screen display of these SGDs. The device was programmed to produce the synthetically generated word “toilet” when the TOILET symbol was selected.
Video Production and Content
The videos were recorded by the researchers, using an Apple iPad mini. The video was edited using Final Cut ProFootnote 3 software and animations were produced using Adobe PhotoshopFootnote 4 software. The videos were presented to each child using their family’s iPad. Each child’s preferred reinforcers were included in the video in order to demonstrate them being reinforced for elimination. The use of their SGD in order to request use of the toilet, was also included. The video model consisted of a combination of video self-modeling and point-of-view modeling.
Video recordings were completed during one of the baseline sessions. In order to produce the video model, the child was recorded performing each of the steps in the toileting sequence except urination and defecation. Urination and defecation were each added to the video model using animation. Physical, verbal, and gestural prompts were used in order to encourage each child to complete each of the steps in the toileting sequence except voiding. For urination and defecation, no prompting was provided. Any prompting recorded on the video was edited out so that the final video showed the child engaging in the toileting sequence independently. The child was shown to be receiving their preferred reinforcer as well as verbal praise for successfully eliminating on the toilet. Urination and defecation were represented using animations that included sound effects for urination and defecation. Each child’s genitalia were also covered over with an animation of their genitals in order to protect their privacy. All other aspects of the scene, with the exception of genitals, represented the real environment. The resulting videos were approximately 1.5 min in length and began with the written words, and verbal statement It’s time to go to the toilet.
Data Collection and Dependent Measures
The dependent variables in this study were recorded as the number of steps that were independently completed in the toileting sequence; the percentage of times urination occurred (out of total opportunities); and the frequency of defecation. Data on the toileting sequence were recorded on completion of each step in this process. Completion was defined as independently finishing the steps of the toileting sequence. These steps included: (1) requesting to use the toilet, (2) walking to the toilet, (3) undressing by removing trousers and underwear, (4) sitting down on the toilet, (5) the duration of time that the child remained seated on the toilet, (6) whether the child urinated on the toilet, (7) whether the child defecated on the toilet, (8) dressing by pulling up their underwear and trousers, and (9) flushing the toilet. For steps 1–4, 8, and 9, the parent or researcher recorded whether the child completed each of these steps correctly and independently or whether prompting was required. If prompting was needed an incorrect response was recorded as well as the type of prompt required (verbal, gestural, or physical). For step 5, the length of time the child remained seated on the toilet, without redirection or prompting to do so, was recorded, as rounded up to the nearest minute. Urination and defecation (steps 6 and 7) were also recorded in accordance with whether either of these types of voiding occurred or not, while seated on the toilet. Data were collected by each child’s family member.
During baseline, generalization, and follow-up the percentage of steps independently completed (steps 1–4 and 8–9) for each practice opportunity was calculated. For each day, the percentage of times urination occurred (out of total opportunities) and the frequency of defecation, if any, were also calculated. During intervention (and generalization for Harvey) approximately six (range = 5–7) practice opportunities with each of these steps were implemented per day. At the end of each day the percentage of correct steps across all practice opportunities for that day was calculated. The percentage of times each child urinated out of the total number of opportunities for that day was also calculated. Finally, because participants did not defecate reliably on each practice opportunity (see Elimination schedule) the frequency of defecation for each day was calculated.
Each child was deemed to have mastered the toileting sequence when they were able to independently follow the toileting sequence with 80 % accuracy over three consecutive days. Based on results of the elimination schedule (see Elimination schedule) both participants were considered to have mastered urination when they were able to urinate in the toilet on 80 % of opportunities over three consecutive days. Defecation acquisition criteria were set at defecating in the toilet once per day over three consecutive days for Harvey and twice per day over three consecutive days for Joseph. The variation in acquisition criteria across participants is a reflection of the fact that Joseph defecated more frequently during baseline than Harvey.
Experimental Design
The intervention package used to teach toileting skills was introduced in a staggered fashion across participants (first to Harvey and then Joseph) in line with the requirements of a non-concurrent multiple-baseline across participants design (Kennedy 2005). After intervention short- and long-term follow-up sessions were conducted. Generalization probes in a non-training setting, facilitated by a teacher or teacher aide not involved in the intervention were conducted in baseline and again after acquisition criteria were reached. For Joseph the generalization probes were conducted after mastery of urination skills only as defecation skills did not meet acquisition criteria.
Procedures
Elimination Schedule
Data on each child’s elimination schedule was gathered in order to determine the times of the day in which they were most likely to require the toilet, and therefore, the time of the day during which practice opportunities should be provided. This data was also used to determine acquisition criteria. In order to gather this data, parents checked their child’s diaper at 30 min intervals. Whether the child had urinated or defecated during this 30 min interval was then recorded on the data sheet. Data was collected for 1 week, at which point we were able to determine the intervals during the day in which each child was voiding on a consistent basis (over 50 % of the time). Both participants consistently urinated 5–7 times per day. The percentage of opportunities to urinate in the toilet was therefore used as acquisition criteria. Harvey consistently defecated in the afternoon only, while Joseph consistently defecated in the morning and afternoon each day. The frequency of occurrences of in-toilet defecation was therefore used for the acquisition criterion.
Baseline
A task analysis was completed in order to identify each of the steps in the toileting sequence. The key steps that were identified included participants: (a) requesting to use the toilet, (b) walking to the toilet, (c) undressing by removing their trousers and underwear, (d) sitting on the toilet, (e) urinating or defecating on the toilet, (f) dressing by pulling up their underwear and trousers, (g) flushing the toilet, and (h) walking to the sink to commence washing their hands. In instances of defecation wiping would also be required, though urination was the initial target of intervention. During baseline the child was told It’s time to go to the toilet. The child was then given 10 s in which to respond. If the child did not respond, they were provided with a least-to-most prompting sequence (verbal, gestural, physical) in order to support them to proceed to the next step in the sequence. No reinforcement (verbal or tangible) was provided during baseline and the articipants continued to wear diapers during this phase.
Sitting on the Toilet
If during baseline, the child was not prepared to remain seated on the toilet for a minimum of 2 min, this became the first target of intervention, as it was unlikely that the child would eliminate on the toilet if they were unable to remain seated for this length of time. Each child was provided with verbal praise for remaining seated on the toilet. If the child attempted to get off the toilet, then they were verbally prompted to remain seated (e.g., Let’s try and sit for a little bit longer). If the child attempted to get off the toilet a second time, then the child was allowed to do so.
Intervention
The purpose of intervention was to teach each child to independently follow each of the steps in the toileting sequence, and to learn to eliminate on the toilet. Therefore the children did not wear diapers during intervention, except to bed at night. Because intervention was not targeted at school, diapers were worn over the child’s undies (in an attempt to reinforce awareness of urination and defecation). The initial target of intervention was urination, and the urination process was modeled on the video. Upon mastery of urination, defecation was targeted. This is because urination occurs a lot more frequently, thus allowing for a greater number of practice opportunities and for reinforcement of the desired behavior.
Based on the elimination schedule approximately six practice opportunities (range = 5–7) were provided per day for each child. Immediately prior to a scheduled toileting time, the child was shown the video model depicting the first step of the toileting sequence (i.e., requesting to use the toilet). Upon watching the first video segment, the child was told It’s time to go to the toilet. The child’s SGD was available within their reach, with the symbol for requesting use of the toilet visible. The child was allowed 10 s in which to respond to the step in the toileting sequence. If the child did not respond, responded incorrectly, or went off-task, then he was prompted to complete that step using a least-to-most prompting procedure (verbal, gestural, physical). This process of watching the video model for each step in the toileting sequence followed by practicing that step was repeated until the child had watched each step of the process and completed the entire toileting sequence. While seated on the toilet, the child was verbally reminded to void in the toilet (e.g., You can go wees on the toilet). If the child did not eliminate on the toilet after a maximum of 10 min seated on the toilet, then they were told it was time to stand up. After participants had reached acquisition criterion for completing the steps of the toileting routine, the entire video model was shown at the beginning of a practice opportunity, rather than in segments.
Reinforcement
The child was praised for successfully completing each step. If verbal praise seemed insufficient to motivate the child to complete the step (i.e., we were unable to reduce our prompting after 6 days), then tangible reinforcement (e.g., an edible) was introduced. Each child was differentially reinforced for completing steps in the toileting sequence, and for eliminating in the toilet. As determined by the results of the preference assessment, participants were provided with the highest level of reinforcement when they successfully voided in the toilet (i.e., jelly beans, chocolate chips, or pebbles candy for Harvey and sour gummy candy, chocolate chip cookies, or potato chips for Joseph). The child was not provided with access to these reinforcers outside of toilet training sessions. This reward was provided to the child immediately following elimination on the toilet and was accompanied by descriptive verbal praise (e.g., Good job, you went wees on the toilet).
Each child was also rewarded with moderate level reinforcement (i.e., talking puzzle for Harvey and giant straw for Joseph) for successfully completing all of the steps in the toileting sequence. Reinforcement was provided for prompted and unprompted responses, and regardless of whether the child successfully eliminated in the toilet. This was provided upon completing all of the steps in the toileting sequence.
Low level reinforcement (i.e., nuts or crackers for Harvey and popcorn or raisins for Joseph) was used to reinforce each child for sitting on the toilet and for compliance with instructions (if needed). If the child demonstrated some resistance to following any of the steps in the toileting sequence or was unmotivated to do so, then the child was reinforced for following each step in the toileting sequence, using these low level reinforcers. Both participants required such reinforcement for walking to the toilet and for sitting on the toilet.
Procedural Modifications
In order to address challenging behavior and excessive accidents, several modifications were made to the original procedures. For Harvey, aggressive behavior (e.g., attempting to bite others) was observed in baseline. Therefore, in an attempt to reduce any challenging behavior, verbal praise was given after he completed each step in the toileting sequence.
For both children dry checks were added to the toileting routine. These were added during the 17th intervention session for Harvey and the 40th intervention session for Joseph. This procedural modification was implemented in an attempt to decrease the frequency of accidents by creating an incompatible behavior (e.g., being dry). Initially dry checks occurred every 15 min. These were faded after three consecutive days without accidents. Fading involved a variable schedule of dry checks, which was thinned (by increasing the amount of time between dry checks every 3 days) until no dry checks were implemented. For each dry check the parent approached their child, gained their attention, and said, Are you dry? The child was then prompted to touch the area to feel wet or dry. If the child was dry they were given low level reinforcement (i.e., nuts or crackers for Harvey and popcorn or raisins for Joseph). If the child was wet his parent said, You are wet. We need to do wees in the toilet. The parent then assisted their child in changing his clothing.
Lastly, for Joseph additional modifications were implemented on the 78th intervention session. These included an increase in the number of opportunities to go to the toilet from 5 to 7 in an attempt to reduce accidents, as well as reinforcing (by providing access to music) quiet hands while sitting on the toilet in an attempt to decrease his stimulatory behavior (e.g., tapping his hands on the wall or toilet and touching self).
Generalization
Generalization probes for the toileting sequence and urination followed the same procedure that was used during baseline, except they were implemented in each child’s school and facilitated by their teacher or teacher aide. For Harvey, post-acquisition generalization probes were conducted 1 week following mastery of urination. Due to inconsistent responding nine generalization probes were conducted. For Joseph, two post-acquisition generalization probes were conducted during the first long-term follow-up. One of these probes was conducted in a second novel environment (University Clinic) and facilitated by the researcher. Because the children typically only defecated before and/or after school time, generalization for defecation was not assessed.
Long-Term Follow-Up
Long-term follow-up sessions were conducted in order to measure whether each child had maintained the toileting skills that they had learned. These sessions followed the same procedures that were used during baseline. For Harvey, two long-term follow-up sessions were conducted 2 months after intervention targeting defecation ceased. These were conducted following the steps of the toileting sequence and elimination. For Joseph one session was conducted 3 months following intervention. A second round of long-term follow-up was collected 1 month later (3 months after the last intervention session for Harvey and 4 months for Joseph) with three sessions for each child. Because Joseph did not reach acquisition criterion, follow-up for defecation was not assessed.
Social Validity
The Treatment Acceptability Rating Form-Revised (TARF-R, Reimers, Wacker, and Cooper 1991) Pre-intervention and Post-intervention forms were administered by the researchers. The TARF-R is a 20-item parent rating questionnaire in which responses are rated using a 7-point Likert scale. Seventeen of these questions measure parent ratings of the acceptability of the treatment approach, while three questions focus on the severity of the problem and the parents’ understanding of the intervention approach. Administration prior to and after intervention was implemented in order to assess any changes in perceived acceptability and understanding of the intervention. These forms were administered to Harvey and Joseph’s parents at baseline and upon conclusion of involvement in the study.
Interobserver Agreement
The parents collected data on the steps that the child completed in the toileting sequence, as well as elimination (see Data Collection and Dependent Measures). An independent observer (the researcher or trained family member) recorded the same data within the practice opportunities in order to determine the reliability of the parent’s data collection. In each of these cases the trained family member collecting data was the child’s father. To help to ensure accurate intervention implementation and data collection, the researcher also collected inter-observer agreement (IOA) data weekly. Any errors in treatment fidelity or data collection were discussed with parents following each session.
Interobserver agreement data was collected on 24 % of practice opportunities for Harvey, and 30 % of practice opportunities for Joseph. The percentage of agreement between the instructor and independent observer was calculated for each practice opportunity using the formula: [Agreements/(Agreements + Disagreements)] × 100. This resulted in 99 % agreement for Harvey and 93.5 % agreement for Joseph.
Procedural Integrity
To assess procedural integrity the same independent observer had a checklist of the procedural steps and recorded whether or not the instructor had correctly implemented each procedural step in its proper sequence. Procedural integrity data was collected on 23 % of practice opportunities for Harvey with 100 % correct implementation of the procedural steps. This data was also collected on 28 % of practice opportunities for Joseph with 99 % correct implementation. To help to ensure accurate intervention implementation and data collection, the researcher also collected inter-observer agreement (IOA) and procedural integrity (PI) data weekly.
Results
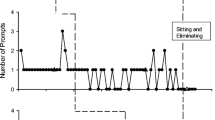
Figure 1 displays the percentage of steps completed independently in practice sessions across days of the study for Harvey and Joseph. Figure 2 displays the percentage of times each participant urinated in the toilet in practice sessions across days of the study. Figure 3 displays the frequency of in-toilet defecation for each participant in practice sessions across days of the study.
Harvey
During the first two baseline sessions, as well as the generalization session, Harvey did not complete any of the toileting steps independently. By the third baseline session he was sitting independently on the toilet, resulting in 16 % of steps in the toileting sequence completed. This might be explained by a procedural modification in which he was given verbal praise for sitting appropriately on the toilet in an attempt to reduce biting his parents and the researcher. Harvey did not demonstrate in-toilet voiding (urination and defecation) during baseline.
With the introduction of the intervention package Harvey steadily increased in the percentage of toileting steps completed independently (Fig. 1). He reached acquisition criterion by the 12th day of intervention. He continued to perform at an average of 90 % (range = 63–100 %) independent toileting steps as he mastered in-toilet voiding. Generalization of toileting steps was evident with 43 to 89 % of steps completed independently at school. Variation in performance was observed across all of the steps. At the first long-term follow-up independent toileting steps maintained at 100 %, but dropped slightly at the second long-term follow-up (79–86 %).
The first video model with animation of in-toilet urination combined with prompting and reinforcement led to urination in some (0–40 %) practice sessions (Fig. 2). With the introduction of dry checks this steadily increased until Harvey reached acquisition criterion by the 39th day of intervention. As Harvey learned in-toilet defecation, he continued to urinate in the toilet on 100 % of opportunities during most days, with a few days at 0 to 50 %. On the first day of generalization to school Harvey urinated in the toilet on 100 % of practice opportunities. This decreased in subsequent probes (to 25 % on 1 day) and then increased to 100 %. During both phases of follow-up Harvey maintained in-toilet urination on 100 % of opportunities.
Harvey demonstrated in-toilet defecation on 4 days during the intervention phase that was targeting urination (Fig. 3). The second video containing animation of in-toilet defecation was introduced after acquisition criteria were met and generalization probes for toileting steps and in-toilet urination were conducted. On the first day of intervention targeting defecation, Harvey defecated in the toilet twice and reached acquisition criterion by the third day. Because the mastery criterion for defecation was set at only one elimination per day for three consecutive days, intervention continued to ensure learning had occurred. Harvey defecated in the toilet 1 to 4 times per day on 78 % (n = 18) of the days for which intervention continued. In-toilet defecation also maintained in 4 of the 5 follow-up sessions.
Table 1 displays results of the TARF-R administered to Harvey’s parents pre- and post-intervention. Results suggest that both parents’ perceived acceptability of the program increased from pre- to post-intervention. Specifically, they indicated an improvement in scores for reasonableness and effectiveness of the procedure. While the rest of the acceptability variables remained stable over time for Harvey’s father, Harvey’s mother also reported a slight increase in willingness post-intervention. An increased post-intervention score for side-effects indicated Harvey’s mother reported fewer side-effects than she had originally anticipated. A decreased post-intervention score for disruption/time indicated that she perceived the intervention to cause more disruption and time to implement than expected, reporting that it did not fit well into the family routine.
Joseph
Baseline performance for independently completing each step of the toileting sequence dropped from 16 to 0 % for Joseph. During the generalization probe he did not complete any of the toileting steps independently. Joseph did not demonstrate in-toilet voiding (urination and defecation) throughout baseline.
Joseph commenced intervention after Harvey had reached acquisition criteria for the toileting sequence and in-toilet urination. With the introduction of the intervention package he gradually developed independence in completing the steps of the toileting sequence until he reached acquisition criterion on the 29th day of intervention (Fig. 1). As he mastered in-toilet voiding he continued to perform the toileting steps at high levels of independence (M = 86 %, range = 53–100 %). Throughout both phases of follow-up Joseph maintained independent toileting (100 % for each session) and this generalized to his school and the University Clinic.
Initially in-toilet urination was variable (M = 6 %, range = 0–60 % of opportunities) and progress was slow (Fig. 2). With the introduction of dry checks Joseph reached acquisition criterion on the 54th day of intervention. However, in-toilet urination subsequently dropped. With the introduction of a second procedural modification this plateaued at an average of 37 % (range = 0–100 %). At follow-up in toilet urination increased to 100 % and this generalized to his school and the University Clinic.
With the introduction of the video model containing animation of in-toilet defecation Joseph defecated in the toilet three times out of the 19 days (16 %) of intervention targeting defecation (Fig. 3). He did not reach mastery criterion for in-toilet defecation.
Pre- and post-intervention results of the TARF-R for Joseph’s parents are reported in Table 2. While perceived acceptability of the program increased slightly from pre- to post-intervention for Joseph’s father, acceptability decreased over time for his mother. For both parents perceived reasonableness of the intervention declined and decreased scores for disruption/time indicated that they felt the intervention caused more disruption and time to implement than they had expected. On the other hand, increased post-intervention scores for side-effects indicated both parents reported fewer side-effects than they had originally anticipated. For Joseph’s father perceived effectiveness and affordability of the intervention increased from pre- to post-intervention. However, Joseph’s mother indicated that the intervention was less affordable than she had initially anticipated.
Discussion
The current study investigated the effectiveness of an intervention package that was used to teach toileting skills to two children with autism. Specifically, the efficacy of video modeling, including animation to depict in-toilet voiding, combined with behavioral prompting and reinforcement procedures were evaluated. Results suggest that the intervention was effective in teaching toileting skills, as illustrated by an increase in both the percentage of steps in the toileting sequence completed independently and in-toilet voiding (urination). These toileting skills maintained over a 3 to 4 month period after the intervention ended and generalized to the school setting for both boys. The intervention also led to mastery of in-toilet defecation for 1 of the 2 children.
The current study incorporated evidence-based toilet training procedures that were derived from the RTT model (Azrin and Foxx 1971); specifically the use of prompting and reinforcement techniques. This study extended previous research into RTT, however, by eliminating the use of punishment procedures, incorporating a schedule-based toileting routine, and investigating collateral behaviors associated with the toileting sequence, including communicating the need to use the toilet. It is noted, that while these collateral behaviors are receiving increasing attention, they are not usually included in the description of toileting protocols (Kroeger and Sorensen-Burnworth 2009).
In addition to these modified RTT techniques, the current study extended the work of Drysdale et al. (2014) and Lee et al. (2014) who investigated the use of custom-made video models in order to teach children with autism the steps in the toileting sequence and in-toilet urination. To our knowledge, this study is the first to use animation to depict defecation as well as urination. Initially the video model targeted in-toilet urination and once this skill was mastered a second video model depicting in-toilet defecation was introduced. This allowed for the depiction of sensitive behaviors (urination and defecation) whilst maintaining privacy (of genitalia), which has been hypothesized to assist skill acquisition (Drysdale et al. 2014; Lee et al. 2014). While both participants in the current study mastered urination after introduction of the intervention, Joseph did not master defecation and Harvey demonstrated some in-toilet defecation before the video depicting defecation was introduced. Consequently, while these findings show promise, further research needs to be conducted in order to determine the utility of videos incorporating animation of voiding.
Findings from the present study should be interpreted in light of the potential differential contributions of the intervention package. The present study incorporated well-established behavioral instructional strategies, in addition to the video model. As these procedures were used simultaneously within the intervention, it is not possible to differentiate between the effects of the video model versus prompting and reinforcement procedures. Drysdale et al. (2014) reported acquisition of toileting skills prior to introduction of the video model, suggesting that the use of social praise alone could be sufficient to teach toileting skills to children with autism. Furthermore, there is debate about whether video modeling is more effective for children with ASD when used alone or in conjunction with additional prompting and reinforcement procedures (Wang and Koyama 2014). It has been suggested that it is difficult to determine which independent variable (video modeling, prompting, or reinforcement) is able to account for skill acquisition when video modeling interventions consist of multiple components (Rayner, Denholm, and Sigafoos 2009; Shukla-Mehta, Miller, and Callahan 2009).
Although it is difficult to determine which of the independent variables can explain intervention effects, it is possible that the use of video modeling in conjunction with prompting and reinforcement might be more effective than prompting and reinforcement alone. Murzynski and Bourret (2007), for example, found that the participants acquired skills taught with video modeling plus least-to-most prompting procedures in fewer trials and with fewer prompts than skills taught with least-to-most prompting alone. It is therefore, important that further research is conducted to determine the impact of video modeling on toilet training, when used in isolation or as part of a multi-component intervention. If reinforcement and prompting procedures alone are sufficient, the time and cost of video production and viewing might be saved. By contrast, the use of video modeling in conjunction with behavioral teaching techniques may enhance the efficiency with which we are able to teach toileting skills.
Given the delay in acquisition of toileting skills for many children with autism (Szyndler 1996), it is important that we understand how to increase the efficiency with which we can facilitate toilet use. In the current study, the acquisition of toileting skills took a relatively long time, particularly for Joseph who took a total of 54 days to acquire in-toilet urination skills. This is considerably longer than the time taken by participants in previous research, in which in-toilet urination was acquired in as few as 6–8 days (Drysdale et al. 2014). There are several possible explanations for these differences in acquisition rates. Notably, the participants in the Drysdale et al. (2014) study were 4 and 5 years of age. By contrast the participants in the current study were between 7 and 8 years of age. It is possible that toileting skills are acquired more quickly when introduced at a younger age as there is less established history of diaper use and/or toileting accidents. Equally, because both Joseph and Harvey had previous failed attempts at toilet training, they may have had negative prior experience or a negative reinforcement history associated with toilet use. The fact that intervention was solely conducted within the home environment may also explain the time taken for acquisition of independent toileting. Intervention did not occur in the school setting and diapers were worn in that environment, thereby allowing each child to avoid toilet use. Given that a substantial period of time is spent in the school setting it would seem reasonable to hypothesize that if intervention had been conducted across settings, it would have supported faster acquisition of toileting skills. Further research might evaluate the impact of intervention that is targeted in all environments.
Another possible explanation for the time taken to acquire toileting skills, is that neither child had well established imitation skills prior to intervention. Each child was unable to imitate the actions presented using a video model within the initial assessment of imitation skills, with the exception of two actions (clapping hands and tapping the table). It is possible to conclude that learning via a video model may have been more efficient if these children had more advanced imitation skills and a history of imitating actions presented via this modality (Rayner 2014). Equally, this may have allowed the researchers to present the video model as a chain of steps as opposed to presenting each step in isolation.
Research has also recommended that challenging behavior, which might impede compliance or skill acquisition, is addressed prior to intervention (Nikopoulos, Canavan, and Nickpoulou-Smyrni 2009). Self-stimulatory behavior (hand tapping and touching self) appeared to be interfering with Joseph’s ability to complete the steps in the toileting sequence, as well as voiding. Therefore, commencement of defecation intervention was delayed while we attempted to decrease his levels of challenging behavior. This delay meant that intervention was prolonged. It is recommended that future research, and the clinical use of video modeling to support toilet training, ensures that challenging behaviors (e.g., compliance with instructions, self-stimulatory behavior, and aggression) are controlled prior to commencing intervention. Finally, it is noteworthy, that other studies did not continue intervention for as long as the present study. This may explain why in-toilet voiding was not accomplished in previous research (e.g., Bainbridge and Myles 1999; Keen et al. 2007; Lee et al. 2014) and also suggests that intervention may need to be sustained for several weeks before progress is observed. This may be the case particularly for children with challenging behaviors that interfere with toilet use and/or who have a history of failed toilet training attempts.
Based on recommendations from a review of the literature by Kroeger and Sorensen-Burnworth (2009), the present study made two further important contributions to the literature. First, parent training was provided in order to support the family to implement the intervention. This involved both face-to-face training and a written manual. It is thought that the video models themselves may also have supported this process because they may have prompted the parents to follow each step in the toileting behavior chain. In order to ensure that the procedures were implemented with a high degree of consistency and accuracy interobserver agreement and procedural integrity data were collected by the researcher. When procedures were not followed correctly, and procedural integrity was low, the researcher was able to provide additional feedback and training for the parents. The use of these parent training procedures, and the embedded prompts associated with using video modeling, have important clinical implications.
Second, using the TARF-R (Reimers et al. 1991), the social validity of the intervention package was measured. Findings indicated Harvey’s parents reported an increase in acceptability, while Joseph’s parents reported a reduction in acceptability of the intervention over time. This discrepancy might be explained by the fact that Harvey acquired skills associated with toileting as well as in-toilet urination and defecation, while Joseph took considerably longer to master toileting skills and urination and did not learn in-toilet defecation. For Harvey, there were also additional collateral benefits of intervention reported. Anecdotally, Harvey’s parents reported that they were able to remove his jumpsuit following intervention as fecal smearing subsided, he began to sleep through the night as he did not wake due to voiding, and there were decreased costs as they no longer needed to buy diapers. These additional benefits may also explain Harvey’s parents perceived acceptability of the intervention package.
There are a number of limitations to the present study that should be noted. Firstly, each of the children in the current study wore diapers during baseline. Though the potential effect of this is difficult to determine, it is possible that the removal of the diapers during intervention may have impacted upon each child’s acquisition of voiding skills. Secondly, no data was collected on the number of accidents that each child had during intervention. Although this was attempted, parents reported that it was too challenging to collect this data in addition to the other intervention requirements. In future, it is a recommendation of the researchers that the frequency of accidents is recorded in order to determine continence outside of scheduled toileting times. Thirdly, procedural integrity data was not completed for the implementation of the dry checks. While parents did have an interval timer set on their phones to remind them to implement the dry checks, this was not monitored. Finally, as discussed, the combination of video modeling with prompting and reinforcement procedures during intervention means it is difficult to conclude whether video modeling in isolation is sufficient to teach toileting skills.
In summary, the current study aimed to increase our understanding of the impact of a video modeling intervention package in toilet training children with autism. The use of animation to depict both in-toilet urination and defecation was novel, with little research to date establishing successful techniques for promoting this skill. Results suggest that the use of animation is promising for facilitating elimination in the toilet, which is arguably the most important step in toileting. Future research exploring the differential effects of this video modeling technique and behavioral instructional strategies is warranted.
Notes
Apple iPod/iPad is a registered trademark of the Apple Corporation, Cupertino California, www.apple.com
Proloquo2Go is a registered trademark of AssistiveWare B.V., Amsterdam the Netherlands, www.assistiveware.com
Final Cut Pro is a registered trademark of the Apple Corporation, Cupertino California, www.apple.com
Adobe Photoshop is a registered trademark of Adobe Systems Incorporated, San Jose California, www.adobe.com
References
Azrin, N. H., & Foxx, R. M. (1971). A rapid method of toilet training the institutionalized retarded. Journal of Applied Behavior Analysis, 4, 89–99.
Bainbridge, N., & Myles, B. S. (1999). The use of priming to introduce toilet training to a child with autism. Focus on Autism & Other Developmental Disabilities, 14, 106–109.
Baker, S. D., O'Reilly, M., & Lang, R. (2009). Review of video modeling with students with emotional and behavioral disorders. Education and Treatment of Children, 32, 403–420.
Cicero, F. R., & Pfadt, A. (2002). Investigation of a reinforcement-based toilet training procedure for children with autism. Research in Developmental Disabilities, 23, 319–331. doi:10.1016/S0891-4222(02)00136-1.
Darden-Brunson, F., Green, A., & Goldstein, H. (2008). Video-based instruction for children with autism. In J. K. Luiselli, D. C. Russo, W. P. Christian, & S. M. Wilczynki (Eds.), Effective practices for children with autism: Educational and behavioral support interventions that work (pp. 241–268). USA: Oxford University Press.
Drysdale, B., Lee, C. Y. Q., Anderson, A., & Moore, D. W. (2014). Using video modeling incorporating video modeling to teach toileting to two children with autism spectrum disorder. Journal of Developmental and Physical Disabilities. doi:10.1007/s10882-014-9405-1.
Green, V., Sigafoos, J., Didden, R., O’Reilly, M., Lancioni, G., Ollington, N., & Payne, D. (2008). Validity of a structured interview protocol for assessing children’s preferences. In P. Grotewell & Y. Burton (Eds.), Early childhood education: Issues and developments (pp. 87–103). New York: Nova.
Keen, D., Brannigan, K. L., & Cuskelly, M. (2007). Toilet training for children with autism: the effects of video modeling. Journal of Developmental and Physical Disabilities, 19, 291–303. doi:10.1007/s10882-007-9044-x.
Kennedy, C. (2005). Single-case designs for educational research. Boston: Pearson Education Inc.
Kroeger, K. A., & Sorensen-Burnworth, R. (2009). Toilet training individuals with autism and other developmental disabilities: a critical review. Research in Autism Spectrum Disorders, 3, 607–618. doi:10.1016/j.rasd.2009.01.005.
Lang, R., Shogren, K., Machalicek, W., Rispoli, M., O'Reilly, M. F., Regester, A., & Baker, S. (2009). Use of video self-modeling to teach classroom rules to two children with Asperger’s syndrome. Research in Autism Spectrum Disorders, 3, 483–488.
Lang, R., Ramdoss, S., Raulston, T., Carnett, A., Sigafoos, J., Didden, R., et al. (2014). Assistive technology for people with autism spectrum disorders. In G. E. Lancioni & N. N. Singh (Eds.), Assistive technology for people with diverse abilities (pp. 157–191). New York: Springer.
Lee, C. Y. Q., Anderson, A., & Moore, D. W. (2014). Using video modeling to toilet train a child with autism. Journal of Developmental and Physical Disabilities, 26, 123–134. doi:10.1007/s10882-013-9348-y.
Lindsay, C. J., Moore, D., Anderson, A., & Dillenburger, K. (2013). The role of imitation in video-based interventions for children with autism. Developmental Neurorehabilitation, 16, 283–289. doi:10.3109/17518423.2012.758185.
Lott, J. D., & Kroeger, K. A. (2004). Self-help skills in persons with mental retardation. In J. L. Matson, R. B. Laud, & M. L. Matson (Eds.), Behavior modification for persons with developmental disabilities: Treatment and supports (Vol. 2). New York: National Association for the Dually Diagnosed.
McCoy, K., & Hermansen, E. (2007). Video modeling for individuals with autism: a review of model types and effects. Education and Treatment of Children, 30, 183–213.
Murzynski, N. T., & Bourret, J. C. (2007). Combining video modeling and least-to-most prompting for establishing response chains. Behavioral Interventions, 22, 147–152. doi:10.1002/bin.224.
Nikopoulos, C. K., Canavan, C., & Nickpoulou-Smyrni, P. (2009). Generalized effects of video modeling on establishing instructional stimulus control in children with autism. Journal of Positive Behavior Interventions, 11, 198–207. doi:10.1177/1098300708325263.
Palechka, G., & MacDonald, R. (2010). A comparison of the acquisition of play skills using instructor-created video models and commercially available videos. Education and Treatment of Children, 33, 457–474. doi:10.1353/etc.0.0100.
Partington, J. W. (2010). The Assessment of Basic Language and Learning Skills Revised (The ABLLS-R). Pleasant Hill: Behavior Analysts, Inc.
Radstaake, M., Didden, R., Peters-Scheffers, N., Moore, D. W., Anderson, A., & Curfs, L. M. G. (2014). Toilet training in individuals with Angelman syndrome: a case series. Developmental Neurorehabilitation, 17, 243–250.
Rayner, C. (2014). Video-based intervention for children with autism: Towards improved assessment of pre-requisite imitation skills. Developmental Neurorehabilitation. doi:10.3109/17518423.2014.890959.
Rayner, C., Denholm, C., & Sigafoos, J. (2009). Video-based intervention for individuals with autism: key questions that remain unanswered. Research in Autism Spectrum Disorders, 3, 291–303. doi:10.1016/j.rasd.2008.09.001.
Reimers, T., Wacker, D., & Cooper, L. (1991). Evaluation of the acceptability of treatments for children’s behavioral difficulties. Child and Family Behavior Therapy, 13, 53–71.
Rinald, K., & Mirenda, P. (2012). Effectiveness of a modified rapid toilet training workshop for parents of children with developmental disabilities. Research in Developmental Disabilities, 33, 933–943.
Rosenberg, N. E., Schwartz, I. S., & Davis, C. A. (2010). Evaluating the utility of commercial videotapes for teaching hand washing to children with autism. Education and Treatment of Children, 33, 443–455. doi:10.1353/etc.0.0098.
Shukla-Mehta, S., Miller, T., & Callahan, K. J. (2009). Evaluating the effectiveness of video instruction on social and communication skills training for children with autism spectrum disorders: a review of the literature. Focus on Autism & Other Developmental Disabilities. doi:10.1177/1088357609352901.
Sparrow, S. S., Cicchetti, D., & Balla, D. A. (2005). Vineland Adaptive Behavior Scales (2nd ed.). Minneapolis, MN: Pearson Assessment, Inc.
Szyndler, J. (1996). Toileting problems in a group of children with autism. Child and Adolescent Mental Health, 1, 19–25.
Tereshko, L., MacDonald, R., & Ahearn, W. H. (2010). Strategies for teaching children with autism to imitate response chains using video modeling. Research in Autism Spectrum Disorders, 4, 479–489.
Vermandel, A., Van Kampen, M., Van Gorp, C., & Wyndaele, J. (2007). How to toilet train healthy children? A review of the literature. Neurology and Urodynamics, 27, 162–166. doi:10.1002/nau.20490.
Wang, H.-T., & Koyama, T. (2014). An analysis and review of the literature and a three-tier video modeling intervention model. Research in Autism Spectrum Disorders, 8, 746–758. doi:10.1016/j.rasd.2014.03.0101.
Whiteley, P. (2004). Developmental, behavioural and somatic factors in pervasive developmental disorders: preliminary analysis. Child: Care, Health and Development, 30, 5–11.
Acknowledgments
We acknowledge and appreciate all the time and energy contributed by the children, their families, and school staff who participated in this study.
Conflict of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McLay, L., Carnett, A., van der Meer, L. et al. Using a Video Modeling-Based Intervention Package to Toilet Train Two Children with Autism. J Dev Phys Disabil 27, 431–451 (2015). https://doi.org/10.1007/s10882-015-9426-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10882-015-9426-4