Abstract
This study investigated the effects of an instructional package which included the use of custom-made video models together with picture prompts and reinforcement to toilet train a 4-year-old boy diagnosed with autism. Six components of toileting were identified during a task analysis: Walking to the toilet, undressing, sitting on the toilet, eliminating in the toilet, redressing, and flushing. A changing criterion design was employed to assess the effects of the intervention. Results showed that the intervention package was effective in teaching the functional skills of dressing, sitting on the toilet and flushing, skills which generalized to a second setting. However, it did not result in the acquisition of reliable in-toilet voiding. The current study contributes to the small body of research literature regarding toilet training and video modeling, highlighting the attention to detail required when undertaking interventions using custom-made videos to toilet train children with autism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Achieving independent toileting is an essential life skill. Poor toileting skills can cause physical discomfort and negatively impact personal hygiene, self-confidence, social competence and acceptance, thereby resulting in a dependence on caregivers for help. For individuals with autism, toileting acquisition is often delayed, and in some cases never achieved (Sells-Love et al. 2002). Szyndler (1996) found that 82 % of parents of children with autism reported having difficulties over toileting.
Current clinical approaches to toilet training individuals with developmental disabilities are largely based on Azrin and Foxx’s (1971) comprehensive training protocol called the rapid toilet training (RTT) program (Kroeger and Sorensen-Burnworth 2009). The RTT program features scheduled toileting opportunities, increased fluid-intake to increase the operant rate of urinating and positive reinforcement for in-toilet voiding. RTT, in the original and modified versions, has been implemented in numerous studies to toilet train individuals with various disabilities (Didden et al. 2001; Sells-Love et al. 2002).
Although a major element of being toilet trained involves the acquisition of related behaviors (e.g., undressing and flushing the toilet), many toilet training studies have not addressed these. Instead, common dependent variables in such studies have been toilet initiations, dry or wet diapers, frequency of in-toilet urinations, or number of toileting accidents (Bainbridge and Myles 1999; Didden et al. 2001; Sells-Love et al. 2002). The acquisition of these associated behaviors as well as in-toilet voiding is necessary for the increased independence and autonomy of both the children and caregivers concerned.
Despite the extent of toileting difficulties in individuals with autism, little research has been conducted with them (Keen et al. 2007). It has been suggested that current toilet training techniques may not be the best option and that alternative approaches may be needed with this population (Keen et al. 2007). One such alternative is video modeling. Video modeling involves the child observing a video of a model engaging in the target behavior and subsequently imitating it (Charlop-Christy et al. 2000). Video modeling has been shown to be effective in teaching a variety of skills to individuals with autism, including academic (Moore et al. 2013), social (Litras et al. 2010; Tetreault and Lerman 2010) communication (Wert and Neisworth 2003), play (Hine and Wolery 2006) and self-help skills (Rayner 2010).
Video modeling is thought to be particularly suited to children with autism (Delano 2007) and to have several advantages over, for example in vivo modeling. Firstly, video modeling takes advantage of their relative strength in visual processing (see e.g., Bellini and Akullian 2007) and common interest in watching videos, increasing the likelihood of the child attending to the modeled behavior. Secondly, the amount of irrelevant stimuli in the environment can be controlled through the use of video editing thereby compensating for possible over selectivity. Additionally, video modeling is considered cost effective as videos can be used repeatedly without requiring the continued physical presence of the person modeling the behavior (Charlop-Christy et al. 2000).
Despite its success in teaching new skills to children with autism, video modeling alone may not always be effective. Shukla-Mehta et al. (2010) recommended that additional strategies should be used with video modeling to increase acquisition and generalization of target behaviors. Such strategies may include reinforcement (Wert and Neisworth 2003), and live instructional and picture prompting (LeBlanc et al. 2003).
To date, only two studies have investigated the effectiveness of video modeling in toilet training children with autism. Bainbridge and Myles (1999), used video modeling to teach a 3-year-old boy to initiate toilet use, defined as walking to the toilet. In the second study, Keen et al. (2007) explored the effectiveness of video modeling in teaching day-time urinary control to five children with autism. Their results suggest that video modeling used in conjunction with prompts and reinforcement may improve the achievement of day-time urinary skills in children when compared to prompts and reinforcement alone. Although both of these studies demonstrate some success using video modeling to toilet train children with autism, none of the participants in either study achieved full toilet training nor were they completely independent in performing behaviors associated with toileting (e.g., undressing, sitting on the toilet, in-toilet voiding, redressing, and flushing).
Darden-Brunson et al. (2008) offered a possible explanation for the limited use of video-modeling with toileting. They suggested that video modeling may be unsuitable for teaching some sensitive behaviors because of limitations with explicit visual depiction of personal self-care behaviors. Both Bainbridge and Myles (1999) and Keen et al. (2007) used commercially produced videos. Although insufficient work has been done to date on the relative effects of commercial versus custom-made videos, custom-made videos may prove to be more effective than commercial videos. Two recent studies (Palechka and Mcdonald 2010; Rosenberg et al. 2010) have reported a relatively slower rate of skill acquisition with commercial videos relative to custom-made videos.
The aim of the present study was to investigate the effectiveness of video modeling using a custom-made video to toilet train a child diagnosed with autism. The treatment package included picture prompting, and reinforcement together with the video model. It was predicted that the use of the video modeling intervention would lead to the acquisition of toileting skills that would be maintained at follow up and generalize to other settings.
Method
Participant
The participant (pseudonym Andrew) was 4 years and 6 months of age when the study commenced. He was recruited through the first author’s involvement as a volunteer in a home-based intervention program. Andrew was previously diagnosed with Autism Spectrum Disorder by a psychologist not involved in this project. Andrew attended a special education school, a mainstream preschool, and an early childhood intervention centre, each for one session per week. He also received approximately 4 h of a home-based intervention program weekly. Andrew did not display any toileting skills and was still in diapers, though his mother reported he showed signs of discomfort after soiling. Andrew’s language development was delayed, and he used a very limited vocal expressive repertoire. His psychologist reported that Andrew had recently made substantial gains in non-vocal communication, primarily through the Picture Exchange Communication System with which he had achieved mand sentence construction. Andrew was also reported to enjoy watching videos.
Settings and Materials
Video production, baseline and intervention and follow up sessions were conducted at Andrew’s home. During baseline, intervention and follow up Andrew was usually located in either the playroom or living area with the toilet approximately 5 m away down a short hallway. Typically only his mother was present during these sessions though both his father and twin sister were also generally present in the evenings. The generalization sessions were conducted in the special education school Andrew attended.
A Flip video camera, Apple Macintosh™ computer, toileting picture cue card, blank DVD and food reinforcements were used in the construction of the video. In the training sessions, a television fitted with a DVD player, the custom-made video, a picture cue card depicting a boy sitting on a toilet bowl, observation recording sheets, procedural checklists, and food rewards were used. Social validity was assessed using the Treatment Acceptability Rating Form (TARF-R) (Reimers et al. 1992). The questionnaire contains 20 items rated on a 7-point Likert scale, 17 of which measure a single dimension of acceptability, with the remaining three addressing problem severity as well as understanding of the proposed intervention.
Experimental Design
A changing-criterion design incorporating baseline, a six-step intervention and follow up was used. Though the steps were presented in the correct temporal sequence in the video, steps could be mastered in any sequence during training. Mastery for each step in the changing-criterion sequence was defined as successfully completing the step without prompts on at least three consecutive occasions (Hartmann and Hall 1976).
Dependent Measures and Data Collection
Information regarding Andrew’s current interests was obtained using a reinforcer assessment sheet (Central Region Autism Spectrum Disorders Team 2005). This was used in the selection of potential reinforcers as well as in identifying preferred television shows. Video clips of the latter were incorporated into the video model in an attempt to increase the likelihood of attending.
A task analysis of Andrew’s toileting identified six steps: walking to the toilet, undressing, sitting on the toilet, eliminating in the toilet, redressing, and flushing. Unprompted completion of these steps were the dependent measures in this study. To simplify the task processes of urination and defecation were both modeled in a seated position.
Throughout all phases of the study Andrew was provided free access to liquids to optimize the frequency of urination and practice opportunities. All sessions were conducted either by the first author or Andrew’s mother.
Procedure
Before the study, approval was obtained from the State Department of Education and Early Childhood Development and the University Human Ethics Committee. Andrew’s parents, school principal, and teacher provided written informed consent for the study. Written permission was also obtained for the use of footage from the copyright holders of Andrew’s favorite television program.
Video Production and Content
Video production occurred during the baseline phase. This enabled examination of data to assess any possible effects the video production process may have had on the target behavior. The video contained two types of video modeling: video self-modeling and point-of-view video modeling. Video self-modeling involves learners watching recorded and edited videos of themselves performing the targeted behaviours (Mechling et al. 2005). Point-of-view video modeling (PVM) involves the use of video filmed from the learner’s perspective and can involve both close up shots of e.g., hands performing a fine motor task or a broader scene shot from the learner’s eye level (Rayner et al. 2009).
PVM was used to capture footage of behaviors that required fine motor skills such as flushing the toilet. To produce the self-modeling segments of the video, Andrew was prompted physically and verbally to perform the behaviors and rewarded for attempts. Footage of Andrew walking to the toilet, pulling down his pants and sitting on the toilet bowl was captured in this way. The clip of Andrew pulling down his pants was reversed to construct one of him pulling up his pants. Camera positioning ensured that the footage did not depict genitalia during the dressing stages and a soft toy was used to cover exposed genitals when Andrew was seated on the toilet bowl. The footage was edited to remove unwanted behaviors and prompts. Sound effects of in-toilet urination and defecation were added to the video.
Clips from Andrew’s favorite television program, which was identified during the reinforcement assessment, were inserted into the beginning middle and end of the video to maintain interest when watching, for durations of 40 s, 10 s, and 65 s respectively. The final edited video was 3 min and 15 s in duration. The video was burned onto a Digital Video Disk (DVD) so that it could be played on the computer.
The beginning of the video showed, in order, a title frame, a hand holding the picture cue card, the card being handed to Andrew’s mother, followed by her saying “Let’s go to the toilet”. The video then depicted Andrew walking to the toilet with his mother. Once there he pulled down his pants and sat on the toilet bowl. Sound effects of voiding into the toilet followed. The video then showed Andrew getting off the toilet and pulling up his pants. A finger was then shown pressing the flush button of the toilet bowl and feces in the toilet being flushed away. The video ended with his mother saying “Good job, Andrew!”
Identifying Elimination Schedule
Pre-baseline observation data were collected on Andrew’s elimination schedule between 8 am and 6 pm across 7 days. His nappy was checked every 30 min for urine or feces and their presence or absence was recorded. Using these data the probability of Andrew eliminating during each 30 min interval was calculated. Eight 30 min intervals throughout the day were identified as having a 50 % or greater probability of soiling having occurred: 8:00, 9:30, 11:00, 12:30, 14:00, 15:00, 16:30, 18:00. These times were selected as optimal observation and toilet training opportunities for use in the subsequent Baseline and Intervention phases.
Baseline
Andrew was prompted to use the toilet eight times per day, during the times previously identified. Andrew was shown the picture cue card and verbally prompted, “It’s time to go to the toilet.” If he did not initiate the appropriate behaviors in the toileting chain within 10 s he would then be prompted, using a standard least-to-most prompting procedure, to perform each of the toileting behaviors.
Intervention
Immediately prior to the designated training times Andrew was asked to watch the toileting video. He was then prompted with the same verbal phrase and picture cue card as those used in baseline and the video. As in the baseline phase, if he did not initiate the appropriate behaviors in the toileting chain within 10 s Andrew was prompted (least-to-most) to complete the next step. If Andrew did not emit the step in the toileting chain after a physical prompt was given, the step was completed for him. Andrew was required to sit on the toilet bowl for a minimum of 2 min and verbally prompted “pee-pee/poo-poo”) to eliminate in the toilet. Across the intervention phase the time Andrew spent sitting on the toilet bowl was increased in 1 min increments up to 15 min. If he did not eliminate by the end of the time period sitting on the toilet bowl, he was asked to stand up. On those occasions in which the current criterion level had been reached Andrew was reinforced through the provision of preferred edibles or access to preferred toys at the end of the entire behavior chain. To limit inconvenience for the family, Andrew’s diapers were only removed during scheduled toileting sessions.
In-Vivo Modeling
Because in-bowl elimination had still not occurred by session 89, in vivo modeling of voiding in the toilet bowl (father as model) was introduced. These in-vivo modeling sessions occurred approximately once every 2 days for the next 25 days at times when Andrew’s father was available.
Generalization of Toileting
On four occasions, twice during the intervention phase and twice in follow-up, Andrew was prompted to use the toilet using the picture cue card and prompt phrase at the special education school he attended. No further prompting was given and no reinforcement provided other than verbal praise offered by the care giver.
Follow Up
Follow up data were gathered 5 days after the conclusion of the intervention. Procedures were as described in baseline; Andrew was prompted with the verbal phrase and cue card to go to the toilet. He had not been shown the video since the intervention phase ended.
Interobserver Agreement
To determine the reliability of observations, 20 % of the sessions, distributed approximately equally across baseline, intervention phases, and follow up, were observed in vivo by both the first author and Andrew’s mother. Interobserver agreement was calculated by dividing the number of items that were agreed upon by the total number of items, and multiplying that number by 100 (Cooper et al. 2007). This yielded 100 % agreement overall.
Treatment Fidelity
A procedural checklist incorporated into the observation recording sheet was used to ensure consistent and accurate delivery of all sessions. One hundred percent compliance was observed with all prompting, time on toilet seat, and reinforcement procedures for each training session observed. However, typically only four or five training sessions occurred per day and the video was shown only two or three times each day.
Social Validity
To minimize the demand characteristics, social validity was assessed by a doctoral student not otherwise associated with the project. She had knowledge of the treatment procedure but had no vested interest in the research outcomes. The (TARF-R) (Reimers et al. 1992) was completed by Andrew’s mother pre- and post- intervention. Retrospective interviews were also conducted with both Andrew’s mother and classroom teacher on completion of the intervention to discuss what worked well and what could be improved.
Results
Baseline and Intervention
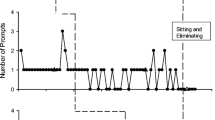
Figure 1 shows the number of steps in a toileting chain Andrew completed without prompts across each phase of the study including generalization probes.
During baseline, the behavior of walking to the toilet was already present in Andrew’s repertoire. No other steps were emitted independently. With the introduction of the video modeling intervention, immediate improvements in the performance of target behaviors were evident. Andrew reached the criterion of two completed steps (walking to the toilet and sitting on the toilet bowl) without prompts on the third intervention session. After four sessions with the video Andrew flushed the toilet successfully without prompts, although this behavior (Step 3) did not occur reliably for another seven sessions.
At Session 41 Andrew completed pulling up his pants without prompts (Step 4) and continued this behavior on all subsequent trials, achieving criterion by Session 43. On Session 45 Andrew also undressed himself successfully and without prompting for the first time, reaching criterion for this behavior two sessions later.
Andrew continued to display the target behaviors of walking to the toilet, undressing, sitting on the toilet, redressing and flushing, but without any instances of in-bowl voiding. Consequently an in vivo modeling element was added to the intervention at Session 87. Seven days after the introduction of in-vivo modeling, Andrew successfully urinated in the toilet bowl but only did so twice more during sessions 128 and 129. No further instances of elimination in the toilet occurred. The intervention was terminated after session 135 due to time constraints.
Follow Up
Results from the three maintenance probes in the 5-day follow-up period indicated that the five toileting skills acquired during the intervention were maintained over this time without prompting other than display of the initial cue card. Andrew performed the behaviors successfully and in sequence without the use of any prompts on each occasion. However, no elimination in the toilet occurred.
Generalization
Andrew’s teacher reported that he did not display any of the target toileting behaviors in school during the baseline phase. During the generalization probes in the intervention and in the follow-up phase, results indicate that Andrew successfully displayed all acquired toileting behaviors in the school setting without the use of prompts or reinforcement.
Social Validity
The results of the TARF-R questionnaire administered to Andrew’s mother pre- and post-intervention are presented in Table 1. Overall, the video modeling intervention was seen as being acceptable, appropriate, fair and reasonable for the task. However changes in scores suggest that her experience with the intervention resulted in a decrease in her perception of the acceptability of the program; in particular scores for disruptiveness, and effectiveness of the program deteriorated and the mother considered there to be more negative side-effects on completion of the project. Her stated willingness to participate in the project also clearly dropped as a result of the experience. Scores remained consistent for severity, understanding and affordability of the intervention.
A follow up interview conducted with Andrew’s mother 6 months after intervention revealed that by this time Andrew had been fully toilet trained. He was reported to be initiating toileting through picture exchange and performing all toileting behaviors successfully. Interestingly, despite the reduced program acceptability evident in the TARF-R results presented above, the mother reported that after the study ended she incorporated video footage of in-toilet voiding (performed by a similar aged peer who was a friend of the family) into the video used in the intervention and showed this modified video to Andrew. Andrew’s mother also reported that at that time she also stopped putting diapers on Andrew during the day. His mother reported that on the third day of watching the modified video and not wearing diapers in the day Andrew performed two instances of in-toilet voiding with the number of such events increasing rapidly thereafter.
Discussion
The current study examined the effectiveness of a video modeling intervention using a custom-made video in conjunction with prompting and reinforcement to toilet train a child with autism. The predictions that the use of the video modeling intervention would lead to the acquisition of toileting skills and that the new toileting skills would be maintained at follow up and generalized to other settings were partially supported.
The intervention was effective in teaching all toileting behaviors that were clearly depicted in the video model (i.e., undressing, sitting on the toilet bowl, redressing, and flushing). Further, these behaviors were maintained over a 5-day period after termination of the intervention and some evidence is present of generalization to a school setting. Despite these outcomes, the intervention was ineffective in teaching the behavior of in-toilet voiding, arguably the most important step in toileting. Because in-toilet voiding was not actually shown in the modeling video, it could be argued therefore that this component of the intervention lacked integrity. Although an in-vivo modeling component was added to the intervention to aid in the acquisition of this final step, it also proved unsuccessful. This may have been a result of limited exposure to this model. Because in vivo modeling requires the person modeling the behavior to be physically present, the live model (the father) was only available once every second day.
Darden-Brunson et al. (2008) suggested that video modeling may not be suited for some sensitive behaviors (e.g., bathing) due to privacy issues and current social expectations regarding the explicit depiction of genitalia and excretion. However, the results from our follow up interview with the mother indicate that, with Andrew, successful in-toilet voiding was accomplished in short order following a combination of such explicit video depiction together with removal of his diapers through the day. Of course, even if data were available to support this informal report, it would not be possible to separate out the differential contributions of video depiction and the removal of diapers in this case. Further research exploring this appears justified. Presumably some of the practical limitations of video depiction concerning Darden-Brunson et al. (2008) and restricting the video depictions we provided in this study could be overcome by the use of cartoons or avatars as video models. A clear visual demonstration of in bowl voiding might assist skill acquisition.
The present study provides valuable information regarding the use of video modeling in toilet training children with autism. A particular strength of the procedure appears to be its acceptability, illustrated in this case by the fact that – despite a reduction in reported acceptability of the intervention over time - the mother at her own initiative extended our video modeling procedure without input from the research team.
In addition to the treatment fidelity issue mentioned above, there are some additional limitations to the present study. Ill health during the study, affecting both Andrew and his mother, and uncontrollable changes to Andrew’s schooling routine during the intervention phase both may have impacted his toileting schedule as well as the acquisition of toileting skills. Also, though some generalization data were obtained, including baseline generalization probes in the school would have strengthened the study. Future research should extend the time interval between the intervention and follow-up phases as well as conduct generalization probes in all phases of the study. Furthermore, as with all single-subject design case studies the external validity of these results requires verification through systematic replication.
In summary, the present research aimed to extend our understanding of the effects of video modeling in toilet training children with autism. The study showed this procedure to be effective in the acquisition of a number of toileting skills beyond those reported previously (Bainbridge and Myles 1999; Keen et al. 2007) though not in the promotion of non-visually depicted toileting behaviors. Reinforcement and prompting were used in conjunction with video modeling. Tentative conclusions regarding the effectiveness of the video modeling intervention in toilet training individuals with autism can be drawn. The data suggest that such custom-made videos are promising techniques in teaching these skills. The intervention package appears to have been acceptable to the parents and was associated with good generalization of the skills that were acquired. Future research exploring the effects of explicit portrayals of the process of elimination in the toilet, possibly through depiction of avatar models is warranted.
References
Azrin, N. H., & Foxx, R. M. (1971). A rapid method of toilet training the institutionalized retarded. Journal of Applied Behavior Analysis, 4, 89–99. doi:10.1901/jaba.1971.4-89.
Bainbridge, N., & Myles, B. S. (1999). The use of priming to introduce toilet training to a child with autism. Focus on Autism and Other Developmental Disabilities, 14, 106–109. doi:10.1177/108835769901400206.
Bellini, S., & Akullian, J. (2007). A meta-analysis of video modeling and video self-modeling interventions for children and adolescents with Autism Spectrum Disorders. Exceptional Children, 73, 264–287.
Central Region Autism Spectrum Disorders (2005). Reinforcer assessment. Retrieved from http://162.127.6.150/esu6/Gems/seautism/REINFORCERASSESSMENT.pdf.
Charlop-Christy, M. H., Le, L., & Freeman, K. A. (2000). A comparison of video modeling with in vivo modeling for teaching children with autism. Autism and Developmental Disorders, 30, 535–552. doi:10.1023/A:1005635326276.
Cooper, J. O., Heron, T. E., & Heward, W. L. (2007). Applied behavior analysis (2nd ed.). New Jersey: Pearson Education Inc.
Darden-Brunson, F., Green, A., & Goldstein, H. (2008). Video-based instruction for children with autism. In J. K. Luiselli, D. C. Russo, W. P. Christian, & S. M. Wilczynski (Eds.), Effective practices for children with autism: educational and behavioral support interventions that work (pp. 241–268). USA: Oxford University Press.
Delano, M. (2007). Video modeling interventions for children with autism. Remedial and Special Education, 28, 33–42.
Didden, R., Sikkema, S. P., Bosman, I. T., Duker, P. C., & Curfs, L. M. (2001). Use of a modified Azrin-Foxx toilet training procedure with individuals with Angelman-Syndrome. Journal of Applied Research in Intellectual Disabilities, 14, 64–70. doi:10.1046/j.1468-3148.2001.00047.x.
Hartmann, D., & Hall, R. (1976). The changing criterion design. Journal of Applied Behavior Analysis, 9, 527–532.
Hine, J. F., & Wolery, M. (2006). Using point-of-view video modeling to teach play to preschoolers with autism. Topics in Early Childhood Special Education, 26, 83–93. doi:10.1177/02711214060260020301.
Keen, D., Brannigan, K. L., & Cuskelly, M. (2007). Toilet training for children with autism: the effects of video modeling. Journal of Developmental and Physical Disabilities, 19, 291–303. doi:10.1007/s10882-007-9044-x.
Kroeger, K. A., & Sorensen-Burnworth, R. (2009). Toilet training individuals with autism and other developmental disabilities: a critical review. Research in Autism Spectrum Disorders, 3, 607–618.
LeBlanc, L., Coates, A., Daneshvar, S., Charlop-Christy, M., Morris, C., & Lancaster, B. (2003). Using video modeling and reinforcement to teach perspective-taking skills to children with autism. Journal of Applied Behavior Analysis, 36, 253–257. doi:10.1901/jaba.2003.36-253.
Litras, S., Moore, D. W., & Anderson, A. (2010) Using video self-modeled social stories to teach social skills to a young child with autism. Autism Research and Treatment, vol. 2010, Article ID 834979. doi:10.1155/2010/834979.
Mechling, L. C., Pridgen, L. S., & Cronin, B. A. (2005). Computer-based video instruction to teach students with intellectual disabilities to verbally respond to questions and make purchases in fast food restaurants. Education and Training in Developmental Disabilities, 40, 47–59.
Moore, D. W., Anderson, A., Treccase, F., Deppeler, J., Furlonger, B., & Didden, R. (2013). A video-based package to teach a child with ASD to write her name. Journal of Developmental and Physical Disabilities. doi:10.1007/s10882-012-9325-x. Published online.
Palechka, G., & McDonald, R. (2010). A comparison of the acquisition of play skills using instructor-created video models and commercially available videos. Education and Treatment of Children, 33, 457–474. doi:10.1353/etc.0.0100.
Rayner, C. S. (2010). Video-modeling to improve task completion in a child with autism. Developmental Neurorehabilitation, 13, 225–230. doi:10.3109/17518421003801489.
Rayner, C., Denholm, C., & Sigafoos, J. (2009). Video-based intervention for individuals with autism: key questions that remain unanswered. Research in Autism Spectrum Disorders, 3, 291–303. doi:10.1016/j.rasd.2008.09.001.
Reimers, T. M., Wacker, D. P., Cooper, L. J., & De Raad, A. O. (1992). Acceptability of behavioral treatments for children: analog and naturalistic evaluations by parents. School Psychology Review, 21, 628–643. Retrieved from http://www.nasponline.org/publications/spr/index-list.aspx.
Rosenberg, N. E., Schwartz, I. S., & Davis, C. A. (2010). Evaluating the utility of commercial videotapes for teaching hand washing to children with autism. Education and Treatment of Children, 33, 443–455. doi:10.1353/etc.0.0098.
Sells-Love, D., Rinaldi, L. M., & McLaughlin, T. F. (2002). Toilet training an adolescent with severe mental retardation in the classroom: a case study. Journal of Developmental and Physical Disabilities, 14, 111–118. doi:10.1023/A:1015272212804.
Shukla-Mehta, S., Miller, T., & Callahan, K. J. (2010). Evaluating the effectiveness of video instruction on social and communication skills training for children with autism spectrum disorders: a review of the literature. Focus on Autism and Other Developmental Disabilities, 25, 23–36. doi:10.1177/1088357609352901.
Szyndler, J. (1996). Toileting problems in a group of children with autism. Child and Adolescent Mental Health, 1, 19–25. doi:10.1111/j.1475-3588.1996.tb00004.x.
Tetreault, A. S., & Lerman, D. C. (2010). Teaching social skills to children with autism using point-of-view video modeling. Education and Treatment of Children, 33, 395–419. doi:10.1353/etc.0.0105.
Wert, B. Y., & Neisworth, J. T. (2003). Effects of video self-modeling on spontaneous requesting in children with autism. Journal of Positive Behavior Interventions, 5, 30–34. doi:10.1177/10983007030050010501.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was completed in partial fulfilment of the requirements for the Post Graduate Diploma in Psychology for the first author. We wish to acknowledge the contribution of Catriona de Bruin in collecting the social validity data.
Rights and permissions
About this article
Cite this article
Lee, C.Y.Q., Anderson, A. & Moore, D.W. Using Video Modeling to Toilet Train a Child with Autism. J Dev Phys Disabil 26, 123–134 (2014). https://doi.org/10.1007/s10882-013-9348-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10882-013-9348-y