Abstract
Alteration of tissue perfusion is a main contributor of organ dysfunction. In cardiac surgery, the importance of organ dysfunction is associated with worse outcome. Central venous-arterial difference in CO2 tension (ΔCO2) has been proposed as a global marker of the adequacy of tissue perfusion in shock states. We hypothesized that ΔCO2 could be increased in case of postoperative organ failure or worse outcome. In this monocentric retrospective cohort study, we retrieved, from our database, 220 consecutive patients admitted in intensive care after an elective cardiac surgery. Four time points were formed: ICU admission, and 6, 24 and 48 h after. A ΔCO2 below 6 mmHg defined the normal range values. The SOFA score, intensive care unit and hospital length of stay, hospital and 6-month mortality rate were recorded. We compared patient with low ΔCO2 (<6 mmHg) and high ΔCO2 (≥6 mmHg). We included 55 (25 %) and 165 patients in low and high ΔCO2 groups, respectively. The SOFA score, the hospital and 6 months mortality rate were higher in patients with low ΔCO2. Surprisingly, we did not find results previously published in other surgical settings. In cardiac surgery, ΔCO2 has a low predictive value of outcome.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
In high-risk surgical patients, maintenance of adequate tissue perfusion is associated with less organ failure and may improve patient outcome [1]. In cardiac surgery, the importance of organ dysfunction, evaluated with the SOFA score, is associated with worse outcome [2]. Thus, a better identification of patients at risk of such complications, by bedside easy access marker, is of high clinical significance.
Central venous-arterial difference in CO2 tension (ΔCO2) has been proposed as a global marker of tissue perfusion adequacy in shock states [3, 4]. ΔCO2 increases with low cardiac output or inadequate microcirculatory perfusion [3, 5, 6]. This increase results from blood flow stagnation in the venous compartment [4, 7]. Few studies have challenged the prognostic significance of ΔCO2 in high risk surgical patient. After major abdominal or vascular surgery, ΔCO2 could help to identify patients who would subsequently develop postoperative complications [8, 9]. Several descriptive studies report an increase of ΔCO2 after a cardiac surgery, but its significance remains uncertain [10–15]. To date, only one study reports that high ΔCO2 recorded within 90 min after ICU admission was associated with an increase of postoperative complications [16]. Unfortunately, complications were not clearly defined which limits the impact of that study.
We hypothesized that ΔCO2 could be increased in case of postoperative organ failure after an elective cardiac surgery. We also studied the correlation between ΔCO2 and patient outcome (length of stay and mortality rate).
The main objective of the study was to compare organ dysfunction accessed with the SOFA score between patients with high or low ΔCO2 measured at H6 timepoint. We also compared the length of stay and the mortality rate between both groups.
2 Methods
Ethical approval for this study (Ethical Committee IRB IORG0007394) was provided by the Ethical Committee of Saint Etienne University Hospital, France (Chairperson Dr P. Rusch) on 1st October 2012. Informed consent was deemed not to be required.
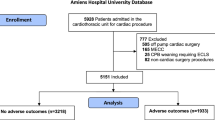
This monocentric retrospective observational study was conducted from November 2012 to April 2013 in an academic postoperative intensive care unit. All consecutive patients admitted after an elective cardiac surgery undergoing cardio pulmonary bypass (CPB) were included. We excluded patients with current infection (e.g. endocarditis) and emergency procedures.
2.1 Study groups and timepoints
We defined two groups, patients with high ΔCO2 (≥6 mmHg) and patients with low ΔCO2 (<6 mmHg) [8, 17].
Four timepoints were formed: ICU admission (admission ICU), and 6 (H6), 24 (H24) and 48 h (H48) thereafter. These timepoints were chosen according to the scheduled routine laboratory tests performed in the unit.
For statistical comparison between groups, ΔCO2 measured at timepoint H6 was taken as reference.
2.2 Anaesthesia and perioperative management
All patients were premedicated with benzodiazepine and hydroxyzine on the night before and 1 h before the surgery. Monitoring consisted of electrocardiography with ST-segment analysis of leads II and V5, pulse oximetry and invasive arterial blood pressure. Induction of anaesthesia was performed with sufentanil (0.3–0.6 µg kg−1) followed by etomidate (0.3 mg kg−1) and cisatracurium (0.15 mg kg−1). After tracheal intubation, a central venous catheter was inserted into the right internal jugular vein. A pulmonary artery catheter was placed for high-risk procedures at the discretion of the anaesthesiologist in charge of the patient. Anaesthesia was maintained by continuous infusion of sufentanil (1–2 µg kg−1 h−1) and desflurane (1 MAC) that was switched to propofol (3–4 mg kg−1 h−1) during CPB.
All patients received unfractionated heparin to maintain an active clotting time greater than 450 s. The CPB priming solution contained 1000 ml of normal saline solution and 500 ml of 6 % hydroxylethyl starch 130/0.4. Cardiac arrest was induced with a cold crystalloid solution (St Thomas® or Custodiol®). CPB under normal temperature was performed with an open circuit using a membrane oxygenator with a continuous flow of 2.2–2.4 L min−1 m−2. Mean arterial blood pressure was maintained between 50 and 70 mmHg. Anticoagulation was reversed at the end of surgery with protamine to achieve a normal activated clotting time. All patient received tranexamic acid during CPB (10 mg kg−1 at the start of CPB, 10 mg kg−1 h−1 during CPB and 10 mg kg−1 at the end of CPB).
On arrival at the postoperative intensive care unit (ICU) a goal-directed protocol for fluid and vasopressor administration was followed. Normovolemia was indicated by a central venous pressure of 8–12 mmHg at zero positive end expiratory pressure (ZEEP), or a pulmonary artery occlusion pressure (PAOP) of 12–15 mmHg at ZEEP, or pulse pressure variation <15 %. If blood pressure remained under 60 mmHg following fluid challenge, norepinephrine was titrated (by 0.05 µg kg−1 min−1 increments) to achieve a mean arterial pressure of 60–80 mmHg. Dobutamine was titrated (by 2.5 µg kg−1 min−1 increments) to achieve a cardiac index ≥2.5 L min−1 m−2. Transfusion of erythrocytes was started if haemoglobin level fell below 10 g dl−1. Red blood cells transfusion was analysed between groups.
Multimodal analgesia was standardised using paracetamol, tramadol and morphine titration if necessary. The sedation with propofol was continued until achievement of normothermia (>36.5 °C), blood loss through mediastinal drains <50 mL h−1 and hemodynamic stabilization with a urine output exceeding 0.5 mL kg−1. There was no weaning protocol in the unit but patients were then rapidly set to pressure support ventilation to allow spontaneous breathing and extubation. Patients are normally discharged to the surgical ward within 48 postoperative hours.
2.3 Data collection
Age, sex, BMI, EuroSCORE and SAPS II score, significant past medical history, pre-operative left ventricular ejection fraction (LVEF) and type of surgery were collected at baseline.
Blood through the central venous catheter and the arterial line was simultaneously drawn for blood gas analysis. The difference between pcvCO2 and paCO2 defined ΔCO2. For patients with a pulmonary artery catheter, mixed venous blood gas was analysed and thus ΔCO2 was calculated with mixed venous pCO2. For those patients, cardiac index (CI) was recorded. Indexed oxygen consumption was calculated by the Fick equation VO2 = CI × (CaO2–CvO2) × 10 where CaO2 and CvO2 are the arterial and venous oxygen content respectively.
Temperature, arterial blood lactate, central venous oxygen saturation (ScvO2) and haemoglobin level were recorded.
Postoperative organ failure was assessed with the Sequential Organ Failure Assessment (SOFA) score. ICU and hospital length of stay were also gathered. Survival to hospital discharge and 6 months later were obtained from the hospital database or from a phone call to the patient or his general practitioner.
2.4 Statistical analysis
Data are expressed as mean ± standard deviation or absolute number and percentage. Groups were compared with an analysis of variance for quantitative variables, or the Fisher’s exact test qualitative variables. Values at different timepoints were compared with a repeated-measure ANOVA and Scheffe post hoc analysis. A curvilinear regression was performed to compare pooled data of ΔCO2 with cardiac index, and linear regression to compare pooled data of ΔCO2 with ScvO2, temperature, haemoglobin and lactate. Statistical analysis was performed with SAS 9.3. Probability values less than 0.05 were considered statistically significant.
3 Results
During the study period, 220 patients were retrieved from our database, 55 (25 %) and 165 were included in low and high ΔCO2 groups, respectively. Eighteen patients (8 %) were discharged before 48 h (15 and 3 in high and low ΔCO2 groups, respectively; p = 0.6). Information on 6-month survival status could not be obtained in 10 patients (5 in both groups).
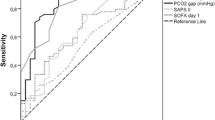
The peak value of ΔCO2 (7.3 ± 2.7 mmHg) was observed 6 h after ICU admission, this timepoint corresponded also to the highest rate of patients with ΔCO2 ≥ 6 mmHg (Fig. 1). Patients’ characteristic did not differ significantly between patients with low or high ΔCO2 (Table 1). Baseline left ventricular ejection fraction was slightly but significantly lower in patients with low ΔCO2. Type of surgical procedure was not significantly different between groups (Table 2). CPB duration but not cross clamping was significantly increased in low ΔCO2 patients. Volume of fluids administrated or number of red blood cells units transfused were not different between groups.
Unexpectedly, we recorded worse outcome for patients with low ΔCO2, as shown with significantly higher SOFA score and mortality rate in this group (Table 3). ICU and hospital length of stay were similar between groups.
Cardiac index was measured in 44 patients. ΔCO2 was weakly correlated with cardiac index or ScvO2 or temperature (Fig. 2). Patients who required dobutamine (whatever the dose) had significantly higher ΔCO2 than those who did not (7 ± 2.6 vs 5.5 ± 2.6 p < 0.0001). We found no correlation between ΔCO2 and lactate (Fig. 2) or haemoglobin (data not shown).
4 Discussion
In cardiac surgery, several mechanisms can lead to an organ dysfunction, alteration of tissue perfusion is an important contributor [18–20]. In that context, evaluation of bedside easy access markers of tissue perfusion is a matter of importance. The difference in CO2 pressure between the vein and the artery (ΔCO2) is one of those. Indeed, ΔCO2 is influenced by both cardiac output and regional blood flow [3, 6]. In this large retrospective study we report, surprisingly, that patients with low ΔCO2 had worse outcome.
Nowadays, mortality after an elective cardiac surgery is low [2]. Organ dysfunction is more frequent and extends hospital length of stay and cost [2]. Organ dysfunction evaluation using the SOFA score has been shown to predict outcome in cardiac surgery patients [2]. This is the first study showing worse outcomes in patients with low ΔCO2. Other studies gave, indirectly, conflicting results in cardiac surgery patients. Studies on early goal-directed hemodynamic therapy demonstrated a significant reduction of complications and length of stay in the hemodynamic optimization group compare to the standard care [13, 21]. Interestingly, patients from both groups exhibited similar ΔCO2 kinetic while outcomes were improved in the intervention group [13]. In another study on regional perfusion in cardiac surgery patients, ΔCO2 was not significantly different between patients who required catecholamine compared to those who did not [12]. These studies are in opposition with Cavaliere et al.’s [16] one. Indeed, the authors reported 52 % of complications for patients with high ΔCO2 compared to 11 % for patients with normal ΔCO2 [16]. But, as already mentioned, hemodynamic and respiratory complications were not clearly defined compromising a clear interpretation of the study. Predictive value of high ΔCO2 has been demonstrated in recently in high risk surgical patients (mainly major elective abdominal surgery) [8, 9]. Indeed, ΔCO2 higher than 6 mmHg, measured during the surgery or within the first 12 post-operative hours, could help to identify patients who would develop subsequently postoperative infections or organ dysfunction [8, 9]. High ΔCO2 was even independently associated with such complications [9]. It is impossible to compare studies carried out in different settings, but mean SOFA score were higher than those reported here. One can argue that with much severe patients we could obtain different results. Nevertheless this hypothesis does not explain why highest SOFA score was observed in low ΔCO2 group.
As others, we found that widening of ΔCO2 is frequent after cardiac surgery [12, 15, 16]. ΔCO2 is a marker of adequacy of venous blood flow to remove the total amount of CO2 produced by the tissues but not a marker of tissue hypoxia [6, 7]. In an isolated hind limb model, lowering oxygen delivery (DO2) by decreasing flow, resulted in an increased of ΔCO2, whereas lowering DO2 by decreasing blood oxygenation did not affect ΔCO2 [7]. These results were confirmed in cardiac surgery by a study performed in 43 patients [14]. The authors measured regional blood flow as well as lactate production, a surrogate for tissue hypoxia. They report a weak correlation between ΔCO2 and blood flow and no correlation with lactate. Similar findings are reported by Jacob et al. [11]. Altered tissue perfusion is common after cardiac surgery but is resolved early without inducing any significant organ dysfunction in most cases [22]. This could explain the high incidence of elevated ΔCO2 but also its lack of correlation with SOFA or lactate. The cardiac output is the other major contributor of ΔCO2. According to the modified Fick equation, the ΔCO2/cardiac output relationship is curvilinear. At low values of cardiac output, changes in cardiac output result in large changes in ΔCO2. Several authors have confirmed this relation in critical care patients [5, 23]. We found only a weak correlation between ΔCO2 and cardiac index, however in agreement with previously published data [10, 14–16].
In surgical context and particularly in cardiac surgery, the sudden variation in temperature observed in the perioperative period is a potential confounding factor. Indeed, temperature may impact cellular respiration and therefore CO2 production [24]. Our results also illustrate the difficulties of assessing the tissue perfusion in cardiac surgery. Indeed, haemodilution, anaemia, haemodynamic alterations, and use of vasoactive and ionotropic drugs are factors that, in addition to CPB, likely result in tissue perfusion changes, and sometimes in the opposite direction [25].
Our study has some limitations. First, high ΔCO2 associated with high ScvO2 could identify patients who could still remain inadequately resuscitated [8, 17]. This hypothesis has not been studied here, but both low and high ScvO2 are markers of tissue hypoxia in cardiac surgery patients [26]. Secondly, we focused on postoperative ΔCO2; we cannot exclude that perioperative ΔCO2 could be predictive of outcome. Third, both groups were formed with the values of ΔCO2 measured at H6. Similar trend was observed with other time points. As shown on Fig. 1, patients with abnormal ΔCO2 were significantly more represented at H6 than all others timepoints. Forth, we plotted measurements from mixed and central venous CO2. A strong agreement between p(mixed v-a)CO2 and p(central v-a)CO2 measurements has been shown in a heterogeneous group of critically ill patients [5]. Due to the specificities of cardiac surgery patients, we analysed our data according to the location of sampling (mixed venous or central venous). We obtained exactly the same trend but statistical significance was lost when samples came from mixed venous blood. At least our study is probably not powered for our objectives. Indeed, the retrospective power calculation is 0.71 and 0.59 to detect a difference for H6 SOFA score and 6 months mortality, respectively.
In this large retrospective cohort, we showed that high ΔCO2 did not predict post-operative complications after cardiac surgery. ΔCO2 is probably difficult to interpret in a cardiac surgery setting mainly due to the sudden variation of many parameters interfering with tissue perfusion.
References
Shoemaker WC, Appel PL, Kram HB. Role of oxygen debt in the development of organ failure sepsis, and death in high-risk surgical patients. Chest. 1992;102(1):208–15.
Patila T, Kukkonen S, Vento A, Pettila V, Suojaranta-Ylinen R. Relation of the Sequential Organ Failure Assessment score to morbidity and mortality after cardiac surgery. Ann Thorac Surg. 2006;82(6):2072–8.
Dres M, Monnet X, Teboul JL. Hemodynamic management of cardiovascular failure by using PCO(2) venous-arterial difference. J Clin Monit Comput. 2012;26(5):367–74. doi:10.1007/s10877-012-9381-x.
Danin PE, Siegenthaler N, Levraut J, Bernardin G, Dellamonica J, Bendjelid K. Monitoring CO2 in shock states. J Clin Monit Comput. 2015;29(5):591–600. doi:10.1007/s10877-014-9638-7.
Cuschieri J, Rivers EP, Donnino MW, Katilius M, Jacobsen G, Nguyen HB, Pamukov N, Horst HM. Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med. 2005;31(6):818–22.
Lamia B, Monnet X, Teboul JL. Meaning of arterio-venous PCO2 difference in circulatory shock. Minerva Anestesiol. 2006;72(6):597–604.
Vallet B, Teboul JL, Cain S, Curtis S. Venoarterial CO(2) difference during regional ischemic or hypoxic hypoxia. J Appl Physiol. 2000;89(4):1317–21.
Futier E, Robin E, Jabaudon M, Guerin R, Petit A, Bazin JE, Constantin JM, Vallet B. Central venous O(2) saturation and venous-to-arterial CO(2) difference as complementary tools for goal-directed therapy during high-risk surgery. Crit Care. 2010;14(5):R193. doi:10.1186/cc9310.
Robin E, Futier E, Pires O, Fleyfel M, Tavernier B, Lebuffe G, Vallet B. Central venous-to-arterial carbon dioxide difference as a prognostic tool in high-risk surgical patients. Crit Care. 2015;19:227. doi:10.1186/s13054-015-0917-6.
Ariza M, Gothard JW, Macnaughton P, Hooper J, Morgan CJ, Evans TW. Blood lactate and mixed venous-arterial PCO2 gradient as indices of poor peripheral perfusion following cardiopulmonary bypass surgery. Intensive Care Med. 1991;17(6):320–4.
Jakob SM, Ruokonen E, Takala J. Assessment of the adequacy of systemic and regional perfusion after cardiac surgery. Br J Anaesth. 2000;84(5):571–7.
Lebuffe G, Decoene C, Pol A, Prat A, Vallet B. Regional capnometry with air-automated tonometry detects circulatory failure earlier than conventional hemodynamics after cardiac surgery. Anesth Analg. 1999;89(5):1084–90.
Polonen P, Ruokonen E, Hippelainen M, Poyhonen M, Takala J. A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg. 2000;90(5):1052–9.
Ruokonen E, Soini HO, Parviainen I, Kosonen P, Takala J. Venoarterial CO2 gradient after cardiac surgery: relation to systemic and regional perfusion and oxygen transport. Shock. 1997;8(5):335–40.
Takami Y, Masumoto H. Mixed venous-arterial CO2 tension gradient after cardiopulmonary bypass. Asian Cardiovasc Thorac Ann. 2005;13(3):255–60.
Cavaliere F, Martinelli L, Guarneri S, Varano C, Rossi M, Schiavello R. Arterial-venous PCO2 gradient in early postoperative hours following myocardial revascularization. J Cardiovasc Surg (Torino). 1996;37(5):499–503.
Vallee F, Vallet B, Mathe O, Parraguette J, Mari A, Silva S, Samii K, Fourcade O, Genestal M. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intensive Care Med. 2008;34(12):2218–25.
Hein OV, Birnbaum J, Wernecke K, England M, Konertz W, Spies C. Prolonged intensive care unit stay in cardiac surgery: risk factors and long-term-survival. Ann Thorac Surg. 2006;81(3):880–5. doi:10.1016/j.athoracsur.2005.09.077.
De Backer D, Dubois MJ, Schmartz D, Koch M, Ducart A, Barvais L, Vincent JL. Microcirculatory alterations in cardiac surgery: effects of cardiopulmonary bypass and anesthesia. Ann Thorac Surg. 2009;88(5):1396–403.
De Somer F. End-organ protection in cardiac surgery. Minerva Anestesiol. 2013;79(3):285–93.
Goepfert MS, Richter HP, Zu Eulenburg C, Gruetzmacher J, Rafflenbeul E, Roeher K, von Sandersleben A, Diedrichs S, Reichenspurner H, Goetz AE, Reuter DA. Individually optimized hemodynamic therapy reduces complications and length of stay in the intensive care unit: a prospective, randomized controlled trial. Anesthesiology. 2013;119(4):824–36. doi:10.1097/ALN.0b013e31829bd770.
Morel J, Bouchet JB, Vola M, Beraud AM, Clerc M, Awad S, Auboyer C, Molliex S. Tissue near infra red spectroscopy change is not correlated with patients’ outcome in elective cardiac surgery. Acta Anaesthesiol Scand. 2014;58(7):835–42. doi:10.1111/aas.12329.
Teboul JL, Mercat A, Lenique F, Berton C, Richard C. Value of the venous-arterial PCO2 gradient to reflect the oxygen supply to demand in humans: effects of dobutamine. Crit Care Med. 1998;26(6):1007–10.
Ralley FE, Wynands JE, Ramsay JG, Carli F, MacSullivan R. The effects of shivering on oxygen consumption and carbon dioxide production in patients rewarming from hypothermic cardiopulmonary bypass. Can J Anaesth. 1988;35(4):332–7. doi:10.1007/bf03010851.
De Blasi RA, Tonelli E, Arcioni R, Mercieri M, Cigognetti L, Romano R, Pinto G. In vivo effects on human skeletal muscle oxygen delivery and metabolism of cardiopulmonary bypass and perioperative hemodilution. Intensive Care Med. 2012;38(3):413–21. doi:10.1007/s00134-011-2404-0.
Perz S, Uhlig T, Kohl M, Bredle DL, Reinhart K, Bauer M, Kortgen A. Low and “supranormal” central venous oxygen saturation and markers of tissue hypoxia in cardiac surgery patients: a prospective observational study. Intensive Care Med. 2011;37(1):52–9. doi:10.1007/s00134-010-1980-8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None declared.
Rights and permissions
About this article
Cite this article
Morel, J., Grand, N., Axiotis, G. et al. High veno-arterial carbon dioxide gradient is not predictive of worst outcome after an elective cardiac surgery: a retrospective cohort study. J Clin Monit Comput 30, 783–789 (2016). https://doi.org/10.1007/s10877-016-9855-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9855-3