Abstract
Purpose
To characterize incidence of low, normal and “supranormal” central venous oxygen saturation (ScvO2) and the relation to markers of tissue hypoxia, course and outcome in cardiac surgery patients.
Methods
Prospective, observational study in a university multidisciplinary 50-bed intensive care unit including 205 consecutive patients undergoing elective cardiac surgery. Data were split into training and test data sets and subjected to 50 replications of fivefold cross-validation to estimate lower and upper bounds of ScvO2 indicative of impaired tissue oxygenation.
Results
Both low (≤60.8%) and supranormal (≥77.4%) ScvO2 were associated with an unfavorable course, while the logistic EuroSCORE for risk adjustment was comparable between groups. Incidences of abnormal ScvO2 were 13.2% low and 30.7% supranormal. Patients with low ScvO2 and an uneventful course initially presented with normal lactate levels, whereas patients with supranormal ScvO2 displayed consistently higher serum lactate levels. High ScvO2 values were associated with the use of β-mimetics and signs of systemic inflammation. Mortality rates were comparable for patient populations presenting either low (14.8%) or supranormal ScvO2 (7.9%) and higher than normals (0%, p < 0.001). Lactate was comparably increased in patients that ultimately died, irrespective whether they had low or supranormal ScvO2 values. In contrast, neither low nor supranormal ScvO2 was associated with altered gastric pCO2.
Conclusions
High ScvO2 is an under-recognized warning sign for impaired tissue oxygenation in the peri-operative period. Including values ≥77.4% as ‘normal’ impaired performance of ScvO2 monitoring to predict a complicated perioperative course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is now well accepted that macrohemodynamic assessment may fail to detect persistent tissue hypoxia, as reflected by increased lactate levels and low central venous oxygen saturation (ScvO2), in a wide range of clinical conditions [1–3]. Signs of persistent tissue hypoxia indicate the need for additional resuscitation, at least in septic patients. The Early Goal-Directed Therapy trial by Rivers and colleagues [3] demonstrated that low ScvO2 was not only associated with high in-hospital mortality, but also that more aggressive therapy to restore ScvO2 could substantially reduce mortality.
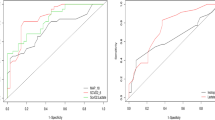
ScvO2-monitoring has been validated against mixed venous saturation and expanded to different patient cohorts as well as clinical conditions [4–7], but with mixed results. In particular, the significance of supply dependency as well as usefulness of ScvO2 monitoring in interdisciplinary ICU-admissions or perioperative patients has been questioned [8]. In a recent study by Bracht et al. [9], the receiver-operating characteristics for ScvO2 to predict 28-day mortality in ‘mixed ICU-admissions’ were very poor, with an area-under-the-curve (AUC) of only 0.53; this was clearly inferior to the SAPS II score with an AUC of 0.89. However, defining cutoff points for ScvO2 in patient cohorts presenting either hypo- or hyperdynamic circulatory failure is problematic. More to the point, efforts to define the significance of “supranormal” ScvO2 are scarce, and including these as ‘normal’ might result in overall poor performance of ScvO2 as a predictor of impaired tissue oxygenation.
Moreover, two components affect the oxygen delivery/uptake relationship (DO2/VO2) as it is reflected in ScvO2. Cardiac output and peripheral cellular oxygen utilization are frequently altered in parallel in individual patients, confounding interpretation of ScvO2 values. Thus, assessment of tissue perfusion typically presents a challenge in patient groups with impaired cardiac function that is complicated by peripheral circulatory and/or mitochondrial failure [10]. Cardiac surgery in patients with impaired left ventricular function reflects such a scenario, as a whole-body inflammatory response capable of initiating peripheral circulatory failure similar to sepsis ensues in up to one-third of patients with need for vasopressors and a characteristic primed phenotype of circulating immune competent cells [11].
We therefore defined lower and upper boundaries and studied incidence of both low as well as “supranormal” ScvO2 prospectively and assessed their relationship to markers of tissue oxygenation in patients undergoing elective cardiac surgery.
Materials and methods
The study was approved by the Institutional Review Board for Human Research of the Friedrich Schiller University, Jena, Germany, which permitted anonymous data analysis, waving informed consent due to the strict observational character and the routine use of central venous lines and gastric tubes in all patients enrolled. A total of 205 patients, age 18 years or older, undergoing cardiac surgery for either coronary artery bypass grafting or valve repair were enrolled between February and November 2004.
Central venous access was obtained percutaneously via the internal jugular approach using a triple lumen spectrophotometry catheter (PreSepCV, Edwards Lifesciences, Unterschleissheim, Germany) after induction of anesthesia and connected to the optical module of a Vigilance monitor (Edwards Lifesciences). In vivo calibration was performed according to the manufacturer's instruction at least on a 6-hourly basis. All patients routinely received transesophageal echocardiography, which was used in addition to postoperative chest radiography to confirm the position of the fiberoptic catheter in the central vein. Also, a gastric tonometry tube (Tonometrics TM, 14F, Datex Ohmeda) for continuous estimation of gastric CO2 partial pressure (prCO2; Tonocap TC 200, Datex-Engström, Helsinki, Finland) to calculate arterio-intestinal pCO2-gradient (aiDCO2) was placed after intubation.
Upon admission to the ICU, all patients were treated according to standard practice; no specific hemodynamic study protocol was implemented. Values for ScvO2, which are otherwise frequently but not routinely monitored on our ICU, were made available to the physician in charge.
Blood gas analyses and lactate levels were assessed at least every 2–3 h via a bed-side analyzer (Radiometer ABL, Copenhagen, Denmark), which was calibrated on a daily basis and subjected to quality control by the central laboratory for clinical chemistry according to ‘good clinical practice’ criteria.
Patients were monitored as described above until they were hemodynamically stable, extubated and fulfilled criteria for discharge to a step-down unit, but no longer than 24 h.
A “complicated course” was defined prospectively by the end points mortality, need for veno-venous hemofiltration or ventilation for more than 24 h.
Statistical analysis
Determination of lower and upper boundaries for ScvO2
Data at time point h = 0 h were split into training and test sets as recommended [12]. The definition of optimal lower and upper bounds for ScvO2 was solely based on the training set. We used 50 replications of fivefold cross-validation to obtain estimators for the optimal lower and upper bounds for ScvO2. In each cross-validation step, the optimal bounds were computed by a grid search.
Thus, three groups were defined as low, normal and supranormal ScvO2, based on their immediate ScvO2 values upon admission to the ICU. For a more detailed description, see the ESM.
Test statistics and data reporting
Data are presented as median and interquartile range, absolute numbers or percentages. Demographic data, hemoglobin levels, perioperative transfusion requirements, Acute Physiology and Chronic Health Evaluation II (APACHE II), Sepsis-related Organ Failure Assessment (SOFA) and Simplified Acute Physiology Score II (SAPS II) scores, EuroSCORE, laboratory data, dosage of catecholamines and markers of tissue hypoxia at a particular time were compared between the three groups using the Kruskal-Wallis test followed post hoc, if significant, by Mann-Whitney U test with Bonferroni correction. Differences between categorical variables were analyzed applying Fisher's exact test. For serial measurements of markers of tissue hypoxia, the area under the curve normalized for observation periods was calculated and similarly tested by Kruskal-Wallis and post-hoc Mann-Whitney U tests with Bonferroni correction. Changes over time, e.g., for vasoactive drugs, were assessed by Friedman repeated measure on ranks followed if significant by Tukey’s test. A p value less than 0.05 was considered statistically significant. To avoid drop-out bias, the ‘last-observation-carried-forward principle’ was applied.
Data analysis was performed using the SPSS software package, version 15.0, and the software R (R Foundation for statistical computing, Vienna, Austria, http://www.R-project.org).
Results
Incidence of low and supranormal values for ScvO2 upon admission to the ICU
Abnormal values for ScvO2 were observed in over 40% of the patients upon admission to the ICU after elective cardiac surgery. A low ScvO2 (determined as ≤60.8%) was observed less frequently (13.2% of cases) than a supranormal (determined as ≥77.4%) ScvO2 (30.7% of cases). The supranormal ScvO2 group already had higher values during the intraoperative course at some time points. However, intraoperative ScvO2 values were rather high in all groups.
Demographic data
There were no statistically significant differences among the three patient groups in the assessed demographic variables of sex, preoperative left ventricular function, NYHA classification, chronic cardiovascular medication, type and duration of surgery, bypass and ischemia time, and lowest hematocrit and oxygen delivery during cardiopulmonary bypass (Table 1). While heart rates were comparable between groups at all time points, mean arterial pressure was lower in the supranormal ScvO2 group in comparison with the normal ScvO2 group after induction of anesthesia and 3 and 12 h after ICU admission. However, median and interquartile ranges were within normal range (see electronic supplementary material). Patients with either low or supranormal ScvO2 were however on average 2–4 years older, and those with high ScvO2 had a moderately lower body mass index (Table 1). Intra- and postoperative infusion management was comparable among the three patient groups (see electronic supplementary material). Of interest, hemoglobin values were significantly lower upon admission in those patients with a low ScvO2, but this was corrected postoperatively as reflected in higher transfusion requirements. In the low ScvO2 group, patients received more platelet concentrates intraoperatively.
The complex European System for Cardiac Operative Risk Evaluation (EuroSCORE), a logistic tool assessing 17 individual risk factors, including comorbidities as well as perioperative determinants predictive of 28-day mortality, was comparable among the groups (Table 1).
Time course of ScvO2 and relation to markers of impaired tissue oxygenation
ScvO2 values normalized in both the low and supranormal groups within the first 6–12 h after admission to the ICU (Fig. 1). With respect to detection of tissue hypoxia, two different patterns, most likely relating to either hypo- or hyperdynamic cardiovascular impairment, could be observed. Low ScvO2 values were associated with normal lactate values for the majority of patients. Low ScvO2 associated with lactate production was associated with mortality (Figs. 2, 3).
Time course of ScvO2 in patients classified as low (≤60.8%; filled circle), normal (60.9–77.3%; open circle) and supranormal (≥77.4%; filled diamond) regarding their central venous saturation. Data are medians and interquartile range. *p < 0.05 compared to normal ScvO2; † p < 0.05 compared to low ScvO2; ‡ p < 0.05 compared to respective baseline
Time course of lactate in patients classified as low (≤60.8%; filled circle), normal (60.9–77.3%; open circle) and supranormal (≥77.4%; filled diamond) regarding their central venous saturation. Data are medians and interquartile range. Inset: Area under curve as a measure of lactate production for each individual patient. Box and whisker plots indicate median, interquartile range, 5th and 95th percentile and outliers. *p < 0.05 compared to normal ScvO2; † p < 0.05 compared to low ScvO2; ‡ p < 0.05 compared to respective baseline
Correlation of ScvO2 and lactate production (as reflected in area under the curve of plasma lactate) and their association with mortality. Circles reflect patients with low ScvO2, squares indicate normal ScvO2 and diamonds high ScvO2 upon admission. Empty symbols indicate surviving, filled symbols dying patients
In contrast, supranormal ScvO2 was paralleled by immediate and persistently increased lactate production in all patients, with even higher lactate values in those patients subsequently dying (Figs. 2, 3). Higher lactate values in these patients were detected as early as at the time of protamin bolus intraoperatively, reflecting the end of cardiopulmonary bypass and end of off-pump bypass surgery, respectively.
Thus, the combined analysis of ScvO2 and lactate values as surrogates for oxidative metabolism identified patients with significant tissue hypoxia, whereas aiDCO2 was not associated with unfavorable clinical outcome (Fig. 4).
Time course of arterio-intestinal pCO2-gradient in patients classified as low (≤60.8%; filled circle), normal (60.9–77.3%; open circle) and supranormal (≥77.4%; filled diamond) regarding their central venous saturation. Data are medians and interquartile range. *p < 0.05 compared to normal ScvO2; † p < 0.05 compared to low ScvO2; ‡ p < 0.05 compared to respective baseline
The importance of high ScvO2 levels as a marker of tissue hypoxia is further supported by the association of supranormal values with mortality, which was 14.8% for low, 7.9% for high and 0% for normal ScvO2 (p < 0.001). Surrogates of morbidity, i.e., ventilation >24 h (low ScvO2: 14.8%, normal ScvO2: 6.1%, supranormal ScvO2: 14.3%) and hemodialysis (low ScvO2: 7.4%, normal ScvO2: 3.5%, supranormal ScvO2: 9.5%) displayed a similar trend not reaching significance. Assuming that both low and “supranormal” ScvO2s are indicative of impaired tissue oxygenation, and consequently defining lower and upper boundaries of normal, resulted in a good performance of ScvO2 to predict unfavorable outcome as reflected in a sensitivity of 0.75 and a specificity of 0.69.
Possible factors for impaired oxygen extraction include use of catecholamines as well as initiation of systemic inflammatory response by the surgical insult. Both, use of β-mimetics (see ESM) and increased white blood count and procalcitonin levels as markers of systemic inflammation were associated with a supranormal ScvO2 (Table 2). In addition, there was a trend towards higher blood glucose levels in the supranomal ScvO2 group [blood glucose (AUC) (mmol/h): low 468.2 (406.8/543.3), normal 496.7 (418.7/565.9), supranormal 528.7 (458.6/639.4), p = 0.048 (not significant after post-hoc adjustment for multiple testing)).
Discussion
In this study, we assessed the incidence of abnormal values for ScvO2 and their relation to global as well as regional markers of impaired tissue oxygenation (i.e., serum lactate and gastric tonometry) in patients undergoing elective cardiac surgery. Our data confirm that a low ScvO2 (≤60.8%) occurred in approximately 13% of patients, but was associated with an unfavorable course only if paralleled by increased lactate production. However, a supranormal ScvO2 (≥77.4%) was observed even more frequently, i.e., in approximately one-third of patients, and appeared to be a hitherto under-recognized warning sign of impaired tissue oxygenation in the same patient population. ScvO2, in particular the combined use of ScvO2 and lactate levels together, was better than gastric tonometry to identify patients at risk.
Mixed and central venous O2 saturations are influenced by arterial oxygen saturation (SaO2) and by the balance between VO2 and cardiac output and hemoglobin concentration. If, as is usually the case in the ICU setting, SaO2 is normal, then ScvO2 reflects the global oxygen supply-demand ratio of the tissues. Additional surrogates of impaired oxygen supply to peripheral tissues, such as serum lactate [13–15], or markers of regional perfusion, such as gastric tonometry, have been proposed as supplementary parameters to unravel persistent tissue hypoxia, though with mixed results [16–18].
The concept of consistent changes of the various surrogates for tissue hypoxia is not supported by the present data. In patients with low ScvO2, lactate levels failed to provide additional information, as lactate only rose upon recovery of circulatory function in parallel with an increase in ScvO2 and presumably cardiac index. On the other hand, many patients with initial low ScvO2 had an uneventful course, which might reflect a compensated state of chronic congestive heart failure in the absence of other signs of tissue hypoxia. Moreover, gastric tonometry (aiDCO2), unlike ScvO2, failed to detect persistent tissue hypoxia. This suggests either impaired tissue oxygenation in regions other than the gut, or points to limitations of gut tonometry [17, 19, 20] and serum lactate [21]. Our results lend support to the recommendation that regional or micro-circulation assessment, e.g., with gastric tonometry, should not be used routinely [22].
A similar observation pointing towards a high sensitivity of ScvO2 to identify patients at risk has been reported by Pearse et al. [23] recently for a mixed sample of patients undergoing major surgery, although the authors limited their definition of abnormal to <65% to detect cardiocirculatory compromise.
Thus, the new information that our data show is that the sensitivity of ScvO2 to detect tissue hypoxia also held true for supranormal values. More to the point, lactate production was even higher in these patients. Mixed or central venous oxygen saturation has traditionally been regarded as an end point of low impact on clinical decision making in “hyperdynamic” shock where high venous saturation is common. Two mechanisms are likely responsible for the supranormal ScvO2 in our population: (1) a systemic inflammatory response (SIRS) to cardiopulmonary bypass or off-pump surgery with concomitant mitochondrial dysfunction [24, 25] or (2) therapeutic measures to increase DO2, most notably β-mimetics. SIRS as the underlying cause is supported by higher white cell counts and markers of inflammation, most notably procalcitonin on day 1, in the present subset of patients. However, higher white cell counts can also reflect β-stimulation [26]; consistent with this notion, a higher share of patients in the subgroup with supranormal ScvO2 received β-mimetics. Another facet might be a higher lactate production due to a metabolic adjustment in consequence of the use of β-mimetics [27]. This would be consistent with the tendency to higher blood glucose values in the supranormal ScvO2 group. However, in pediatric cardiac surgery a raised lactate:pyruvate ratio was detected in 50% of patients with hyperlactatemia, but on the other hand the median lactate value in patients with a high lactate:pyruvate ratio was only 2.1 mmol/l (IQR 1.2/3.2), and only lactate, but not lactate:pyruvate ratio was associated with prolongation of ICU support [28]. High lactate values might also be due to cytokine mediation, correlating with pronounced SIRS, and other non-anaerobic mechanisms [21].
Any observational trial such as this study can provide only limited mechanistic information regarding therapeutic interventions. Why patients received β-mimetics in the present study remains speculative. Supranormal ScvO2 would be consistent with the notion that epinephrine was started, e.g., to improve contractility rather than to normalize tissue perfusion, as use of transesophageal echocardiography is standard in our department and may lead in the light of ScvO2 monitoring to an “overuse” of inotropic substances. “Adequacy” of cardiac function and output was thus achieved more or less irrespective of ScvO2 as a surrogate for the DO2/VO2 relationship. However, this poses important concerns, since the use of epinephrine or dobutamine might worsen outcome if used liberally, i.e., to increase DO2 above the actual need of peripheral tissues. This is consistent with data obtained in congestive (chronic) heart failure where—despite improved cardiac function—excess mortality accompanies the use of β-mimetics [11, 29, 30], and with a recent study in cardiac surgery patients, where use of dobutamine based solely on clinical judgment was associated with increased cardiac morbidity [31].
In conclusion, our data indicate that ScvO2 monitoring, in particular if used along with lactate as a systemic marker of tissue hypoxia, is superior to gastric tonometry, a supposedly sensitive marker of regional flow, to detect both low output syndrome and hyperdynamic shock early in the postoperative cardiac surgery phase.
Supranormal values of ScvO2, which are traditionally considered to be of limited clinical value, turned out to be under-recognized warning signs of impaired tissue oxygenation in cardiac surgery patients. Thus, our data lend support to the concept of a rather narrow corridor of safety for ScvO2, e.g., as used here between 60 and 75%. The association of high ScvO2 with both use of β-mimetics and unfavorable outcome raises the question as to whether the use of β-mimetics might have been too liberal in our cohourt of patients, e.g., triggered by echocardiographic estimates.
In any case, we propose that combined analysis of ScvO2 and lactate levels may be used to identify patients at risk, and a high ScvO2 might reflect an underrecognized warning sign in this context. Additional studies are warranted to test these results in an independent data set.
Abbreviations
- aiDCO2 :
-
Arterio-intestinal pCO2-gradient
- AUC:
-
Area under the curve
- CABG:
-
Coronary artery bypass graft
- DO2 :
-
Oxygen delivery
- pCO2 :
-
Partial pressure of carbon dioxide
- SAPS II:
-
Simplified Acute Physiology Score II
- ScvO2 :
-
Central venous oxygen saturation
- SaO2 :
-
Arterial oxygen saturation
- SIRS:
-
Systemic inflammatory response syndrome
- SOFA:
-
Sepsis-related Organ Failure Assessment
- VO2 :
-
Oxygen uptake
References
Ander DS, Jaggi M, Rivers E, Rady My, Levine TB, Barry Levine AB, Masura J, Gryzbowski M (1998) Undetected cardiogenic shock in patients with congestive heart failure presenting to the emergency department. Am J Cardiol 82:888–891
Rady MY, Rivers EP, Nowak RM (1996) Resuscitation of the critically ill in the ED: responses of blood pressure, heart rate, shock index, central venous oxygen saturation, and lactate. Am J Emerg Med 14:218–225
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M (2001) Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med 345:1368–1377
Kortgen A, Niederprüm P, Bauer M (2006) Implementation of an evidence-based “standard operating procedure” and outcome in septic shock. Crit Care Med 34:943–949
Reinhart K, Rudolph T, Bredle DL, Hannemann L, Cain SM (1989) Comparison of central-venous to mixed-venous oxygen saturation during changes in oxygen supply/demand. Chest 95:1216–1221
Ladakis C, Myrianthefs P, Karabinis A, Karatzas G, Dosios D, Fildissis G, Gogas J, Baltopoulos G (2001) Central venous and mixed venous oxygen saturation in critically ill patients. Respiration 68:279–285
Chawla LS, Zia H, Gutierrez G, Katz NM, Seneff MG, Shah M (2004) Lack of equivalence between central and mixed venous oxygen saturation. Chest 126:1891–1896
Bellomo R, Reade MC, Warrillow SJ (2008) The pursuit of a high central venous oxygen saturation in sepsis: growing concerns. Crit Care 12:130
Bracht H, Hänggi M, Jeker B, Wegmüller N, Porta F, Tüller D, Takala J, Jakob SM (2007) Incidence of low central venous oxygen saturation during unplanned admission in a multidisciplinary intensive care unit: an observational study. Crit Care 11:R2
Hochman JS (2003) Cardiogenic shock complicating acute myocardial infarction. Expanding the paradigm. Circulation 107:2998–3002
Tomic V, Russwurm S, Möller E, Claus RA, Blaess M, Brunkhorst F, Bruegel M, Bode K, Bloos F, Wippermann J, Wahlers T, Deigner HP, Thiery J, Reinhart K, Bauer M (2005) Transcriptomic and proteomic patterns of systemic inflammation in on-pump and off-pump coronary artery bypass grafting. Circulation 112:2912–2920
Steckel JH (1993) Cross validating regression models in marketing research. Mark Sci 12:412–427
Maillet JM, Le Besnerais P, Cantoni M, Nataf P, Ruffenach A, Lessana A, Brodaty D (2003) Frequency risk factors and outcome of hyperlactatatemia after cardiac surgery. Chest 123:1361–1366
Pölönen P, Ruokonen E, Hippeläinen M, Pöyhönen M, Takala J (2000) A prospective, randomized study of goal–oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg 90:1052–1059
Smith I, Kumar P, Molloy S, Rhodes A, Newman PJ, Grounds RM, Bennet ED (2001) Base excess and lactate as a prognostic indicators for patients admitted to intensive care. Intensive Care Med 27:74–83
Kavarana MN, Frumento RJ, Hirsch AL, Oz MC, Lee DC, Bennet-Guerrero E (2003) Gastric hypercarbia and adverse outcome after cardiac surgery. Intensive Care Med 29:742–748
Bams JL, Mariani MA, Groeneveld AB (1999) Predicting outcome after cardiac surgery comparison of global hemodynamic and tonometric variables. Br J Anaesth 82:33–37
Lebuffe G, Decoene C, Pol A, Prat A, Vallet B (1999) Regional capnometry with air-automated tonometry detects circulatory failure earlier than conventional hemodynamics after cardiac surgery. Anesth Analg 89:1084–1090
Hameed SM, Cohn SM (2003) Gastric tonometry. The role of mucosal pH measurement in the management of trauma. Chest 123:475S–481S
Hamilton MA, Mythen MG (2001) Gastric tonometry: were do we stand? Curr Opin Crit Care 7:122–127
Bakker J (2001) Lactate: may I have your votes please. Intensive Care Med 27:6–11
Antonelli M, Levy M, Andrews PJD, Chastre J, Hudson LD, Manthous C, Meduri GU, Moreno RP, Putensen C, Stewart T, Torres A (2007) Hemodynamic monitoring in shock and implications for management. International consensus conference, Paris, France, 27–28. April 2006. Intensive Care Med 33:575–590
Pearse R, Dawson D, Fawcett J, Rhodes A, Grounds RM, Bennnet ED (2005) Changes in central venous saturation after major surgery, and association with outcome. Crit Care 9:694–699
Ince C, Sinaasappel M (1999) Microcirculatory oxygenation and shunting in sepsis and shock. Crit Care Med 27:1369–1377
Crouser ED (2004) Mitochondrial dysfunction in septic shock and multiple organ dysfunction syndrome. Mitochondrion 4:729–741
Burns AM, Keogan M, Donaldson M, Brown DL, Park GR (1997) Effects of inotropes on human leucocyte numbers, neutrophil function and lymphocyte subtypes. Br J Anaesth 78:530–535
Levy B (2006) Lactate and the shock state: the metabolic view. Curr Opin Crit Care 12:315–321
Hatherill M, Salie S, Waggie Z, Lawrenson J, Hewitson J, Reynolds L, Argent A (2007) The lactate: pyruvate ratio following open cardiac surgery in children. Intensive Care Med 33:822–829
Thackray S, Easthaugh J, Freemantle N, Cleland JG (2002) The effectiveness and relative effectiveness of intravenous inotropic drugs acting through the adrenergic pathway in patients with heart failure—a meta—regression analysis. Eur J Heart Fail 4:515–529
Follath F, Cleland JG, Just H, Papp JG, Scholz H, Peuhkurinen K, Harjola VP, Mitrovic V, Abdalla M, Sandell EP, Lehtonen L (2002) Efficacy and safety of intravenous levosimendan compared with dobutamine in severe low-output heart failure (the LIDO study): a randomised double-blind trial. Lancet 360:196–202
Fellahi JL, Parienti JJ, Hanouz JL, Plaud B, Riou B, Ouattara A (2008) Perioperative use of dobutamine in cardiac surgery and adverse cardiac outcome: propensity-adjusted analyses. Anesthesiology 108:979–987
Author information
Authors and Affiliations
Corresponding author
Additional information
The study was performed at the Department of Anesthesiology and Critical Care Therapy, Jena University Hospital, Jena, Germany.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Perz, S., Uhlig, T., Kohl, M. et al. Low and “supranormal” central venous oxygen saturation and markers of tissue hypoxia in cardiac surgery patients: a prospective observational study. Intensive Care Med 37, 52–59 (2011). https://doi.org/10.1007/s00134-010-1980-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1980-8