Abstract
Respiratory rate has been shown to be an important predictor of cardiac arrest, respiratory adverse events and intensive care unit admission and has been designated a vital sign. However it is often inadequately monitored in hospitals. We test the hypothesis that RespiraSense, a piezoelectric-based novel respiratory rate (RR) monitor which measures the differential motion of the chest and abdomen during respiratory effort, is not inferior to commonly used methods of respiratory rate measurement. Respiratory rate was compared between the developed RespiraSense device and both electrocardiogram and direct observation by nursing staff. Data was collected from 48 patients admitted to the post-anaesthesia care unit in a tertiary level hospital. The primary outcome measure was difference in average RR calculated over a 15 min interval between (1) RespiraSense and ECG and (2) RespiraSense and nurses’ evaluation. The secondary outcome measure was the correlation between the respiratory rates measured using these three methods. The 95 % confidence interval for the difference in average RR between RespiraSense and ECG was calculated to be [−3.9, 3.1]. The 95 % confidence interval for the difference in average RR between RespiraSense and nurses’ evaluation was [−5.5, 4.3]. We demonstrate a clinically relevant agreement between RR monitored by the RespiraSense device with both ECG-derived and manually observed RR in 48 post-surgical patients in a PACU environment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
The level of documentation of vital signs in many hospitals is poor [1, 2]. Of the four vital signs, respiratory rate (RR) in particular is often not recorded, even when the patient’s primary problem is a respiratory condition [3–6]. This is in spite of the fact that an abnormal respiratory rate has been shown to be an important predictor of serious events such as cardiac arrest and admission to an intensive care unit (ICU) [7–10]. Retrospective studies of charts suggest that recorded respiratory rates are abnormal in about 1 % of patients, but when intensive automatic monitoring is used, abnormalities are noted at least ten times more frequently [11].
Respiratory rate is an important predictor of cardiac arrest [7] and is likely a more useful indicator of critical illness than changes in systolic blood pressure or pulse [9]. Greater than half of all patients suffering a serious adverse event on the general wards had a respiratory rate greater than 24 breaths per minute [10]. These patients could have been identified as high risk up to 24 h before the event with a specificity of over 95 %. Abnormal RR is also an important indicator of sepsis, pneumonia and respiratory depression. Improved detection and treatment of respiratory problems improves long-term outcome [12].
Although the ability to monitor heart rate continuously and effectively has been developed, an effective, reliable RR monitoring sensor has yet to be developed. Two methods of RR measurement are in common clinical use: direct observation and electrocardiogram-derived. A third method, capnography (monitoring of the concentration or partial pressure of carbon dioxide in the respiratory gases) is usually seen as the gold standard in the hospital environment, however it’s use is currently largely restricted to intensive care units and operating theatres, although more widespread use has been recommended [13]. A need for further refinements in capnography technology to decrease false-positive alarms and improve patient comfort has also been identified [14]. As the trials were performed in the PACU ward of the hospital, for the purpose of this paper the PMD RespiraSense will be compared to the respiration monitors currently utilised within the PACU ward.
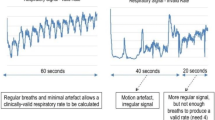
Direct measurement is performed by manual observation of RR by look or touch. However, reproducibility of RR measurement is limited by significant inter-observer variability [15]. Electrocardiogram (ECG) leads are used to measure the change in electrical impedance as the chest wall expands. This may give rise to inaccurate measurements at lower respiratory rates, when there is interference by blood flow, when low skin–electrode impedance is not maintained throughout the monitoring period [16], or when there is excessive subject motion.
Neither clinical measurement by nurses nor electronic measurements, using transthoracic impedance plethysmography, provide accurate measurement of RR in an emergency department setting [17].
We present a pilot study to assess the non-inferiority of the RespiraSense device compared to existing respiratory rate monitoring techniques commonly used in hospital wards, namely ECG-derived respiratory rate and direct manual observation by nursing staff.
2 Materials and methods
Permission was obtained from the Cork Research Ethics Committee to recruit adult patients scheduled for non-urgent surgery at a tertiary hospital (Cork University Hospital). Inclusion criteria were: age greater than 18 years, scheduled for admission to the post anaesthesia care unit (PACU) following surgery under general, regional or local anaesthesia. Exclusion criteria were: patients with diagnosed respiratory disorders (chronic obstructive pulmonary disease, asthma, pulmonary fibrosis), a history of allergy to medical grade skin adhesive or latex, planned postoperative ventilation, pregnancy, patients requiring legally authorized representatives.
The RespiraSense respiratory rate monitor is based upon piezoelectric technology. This technology is in the form of films of an ultra-flat laminated layer of piezo material. This material, when bent or strained, produces a small varying voltage difference. This monitor measures the differential motion of the chest and abdomen during respiratory effort to derive a respiratory rate. The housing for the piezo material was made out of a silicone material and can be seen in Fig. 1. The housing was attached to the patient using 3M medical grade adhesive tape. A Shimmer Research Platform unit (Fig. 2) was used to acquire the data from the sensor at a sampling rate of 20.1 Hz and wirelessly transmitted the data to the external tablet device (Fig. 3). Wireless transmission of information conforms to standard Bluetooth communication protocols as currently used in clinical settings. The received data was stored on the tablet for the duration of the trial and post-processing was performed using Octave on a desktop computer. The dimensions of the RespiraSense sensor unit are: length 80 mm, width 50 mm, depth 15 mm, weight 50 g.
On admission to the PACU standard monitoring (pulse oximetry, electrocardiography, non-invasive arterial blood pressure (Datex AS/3 monitor; Datex Corp., Helsinki, Finland) was attached by the PACU nursing staff. Institutional standard monitoring procedures were commenced, including recording of RR as observed by the attending nurse every 5 min. The upper limb of the RespiraSense monitor was attached along the chest wall overlying the 10th rib, the lower limb was placed over the abdomen and the shimmer unit attached in the mid-axillary line (Fig. 4). A wireless Bluetooth connection was then established with the computer tablet to record RR from the RespiraSense device. The attending nurse and principal investigator were both blind to the RespiraSense reading.
During each trial, the following measurements were obtained by the principal investigator:
-
subject age, mode of anaesthesia, surgery type
-
RR as observed by attending PACU nurse every 5 min
-
patient rating of comfort of device using 11 point verbal rating scale (VRS; 0 = least comfort imaginable, 10 = most comfort imaginable)
-
attending PACU nurse rating of ease of device use, using 11 point VRS (0 = least difficulty imaginable to use, 10 = most difficulty imaginable to use)
-
adverse respiratory events (RR < 5 or >25 breaths per minute, hypoxaemia <92 %, airway obstruction requiring at least jaw thrust or chin lift manoeuvre).
The following measurements were recorded electronically:
-
ECG-derived RR, recorded on Dell Laptop connected to Datex monitor
-
RespiraSense derived RR, recorded on Panasonic ToughPad tablet.
Patients were considered fit for discharge from PACU as per institutional protocol. The RespiraSense monitor was removed immediately prior to discharge from PACU.
2.1 Statistical analysis
The primary outcome measure for the study was mean difference in average RR between (1) RespiraSense and ECG and (2) RespiraSense and nurses’ evaluation. Each RR point was output for a non-overlapping 15 min interval. The secondary outcome was the correlation between the respiratory rates measured for (1) RespiraSense versus ECG and (2) RespiraSense versus nurses’ evaluation.
The difference in average RR between monitoring techniques over this 15 min interval was summarised using the mean, standard deviation, median and range. The effectiveness of the RespiraSense monitor versus nurse observation of RR and ECG-derived RR was determined by 95 % confidence intervals for the mean difference in average RR between techniques. A difference of three breaths per minute (bpm) was considered of minimum clinical relevance. This was chosen from the early warning system (EWS) which identifies a score difference of 3 bpm to be meaningful by defining the respiration scores in steps of 3 bpm.
The secondary analysis was to assess the direct relationship or correlation between the average measured respiratory rate for the RespiraSense device and each of the examined measuring techniques. A Pearson’s Product-Moment correlation analysis was performed.
The RespiraSense monitor would be considered effective in detecting changes in RR comparable to nurse evaluation if a correlation coefficient greater than 0.6 was achieved. The RespiraSense monitor would be considered effective in detecting changes in RR comparable to ECG if a correlation coefficient greater than 0.7 was achieved. Correlations greater than 0.6 identify strong relationships between datasets where the datasets demonstrate similar and simultaneous increases and decreases in measurements. The expected correlation with ECG-derived RR was set at 0.7 because the continuous nature of both the PMD and ECG-derived monitoring could be expected to result in a closer correlation. Bland–Altman analysis was used to present the results graphically.
Using an estimated standard deviation of 6 bpm based on the range of possible values for RR, a sample size of 31 subjects was calculated to be sufficient to estimate a two-sided 95 % confidence interval of width length 6 bpm for the difference between techniques in average RR, assuming at least one evaluable 15 min interval per patient. A 95 % confidence interval of width 6 bpm was chosen to reflect a clinically relevant difference of 3 bpm in either direction, that is [−3, +3].
3 Results
48 patients who presented for non-urgent surgical intervention at our hospital and who did not violate exclusion criteria were enrolled in the trial. No patient declined to enrol in the trial.
The mean age of subjects was 51.5 (median 53, standard deviation 17.7, range 20–83) years. 28 male and 20 female subjects were enlisted. 40 patients underwent general anaesthesia, 6 patients regional anaesthesia and 2 patients sedation. The mean time spent by the patients in the PACU was 59.5 (median 58, standard deviation 15.8, range 34–98) min. No patients suffered an adverse respiratory event during the trial. In terms of comfort, 48 patients (100 %) rated the RespiraSense device as 10 on a VRS for comfort while 12 nursing staff (100 %) rated the RespiraSense device as 10 on a VRS for ease of use (application of device only).
Of the total 144 recorded data points, 115 time points were available for analysis (see Appendix). The remaining 29 time points were lost due to: delays in connecting ECG monitoring (2 patients), laptop shut down (2 patients), disconnection of the RespiraSense device (1 patient) and failure of ECG to generate meaningful RR data (i.e. RR < 1 bpm) (nine 15 minute intervals across multiple patients). Non-overlapping data was required to ensure variable independence in Bland–Altman analysis.
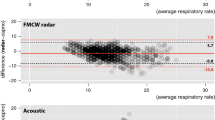
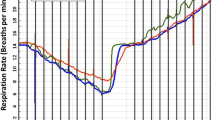
Comparisons of the RespiraSense with ECG-derived RR (column 1) and with nurse monitored RR (column 2) are presented in Table 1. Figure 5 summarises the data from the utilized 115 epochs for ECG versus RespiraSense in the form of a Bland–Altman plot. The direction of difference is: (ECG–RespiraSense). The solid line represents the bias of the differences. Dashed lines represent the 95 % confidence limits for the differences. The mean difference for average RR between RespiraSense and ECG is less than 1 bpm, mean (SD) = −0.41 (1.79). The 95 % confidence interval (CI) for the difference in average RR is calculated to be [−3.9, 3.1], which does not exclude the clinically relevant difference of 3 bpm. However, the difference was greater than 3 bpm in the case of just nine intervals (7.8 % of intervals).
Similar to Fig. 5, Fig. 6 summarises the data for Nurse Evaluation versus RespiraSense, with the direction of difference (Nurse–RespiraSense). The mean difference for average RR between RespiraSense and the Nurse Evaluation is also less than 1 bpm, mean (SD) = −0.58 (2.50). The 95 % CI for the difference in average RR is calculated to be [−5.5, 4.3], which also does not exclude the clinically relevant difference of 3 bpm. The difference was greater than 3 bpm in the case of 23 intervals (20 % of intervals). However, only three of the 23 intervals also showed a difference of greater than 3 bpm in average RR for RespiraSense versus ECG.
The Pearson Product-Moment Correlation Coefficient (PMMCC) of 0.84 demonstrates a very strong relationship between RespiraSense and ECG in monitoring RR. Similarly, the PMMCC of 0.78 demonstrates a slightly weaker, but still strong, relationship between RespiraSense and the nurse’s evaluation in monitoring RR.
4 Discussion
In this paper we have shown that in a clinical setting the RespiraSense device can measure RR, with values which show a clinically relevant agreement with those derived from ECG and from direct measurement by nursing staff.
Patients in the PACU have a wide variety of breathing patterns due to different types of anaesthesia used, varying use of opioid drugs and different body habitus and airway types such as those associated with obstructive sleep apnoea. In addition, postoperative patients are at risk for adverse respiratory events [18, 19]. Both of these factors make the results presented herein relevant and externally valid.
We chose to compare the RespiraSense to two commonly used methods: ECG-derived and direct measurement. Although both of these techniques have been shown to be either inconsistent or unreliable, they remain the most commonly used techniques at our institution and many other institutions worldwide. ECG-derived RR monitoring is restricted to patients attached to ECG monitors at our institution and thus occurs only in PACU, monitored emergency room beds, the intensive care and coronary care units; the majority of patients will only have RR monitoring performed at fixed time intervals by manual observation.
Respiratory rate measurement derived from capnography is likely the nearest to a gold standard but is currently used only in intubated patients and is thus even more restricted in use. While the use of capnography in non-intubated patients is increasing, it’s use remains largely confined to the operating room, perhaps because of perceived problems with equipment and patient comfort [13, 14] as well as accuracy [20]. Future analysis of the RespiraSense device will compare it to capnography outside the PACU ward.
In addition to the quantitative results, it has also been shown that patients consistently rate the device as the most comfortable imaginable while nursing staff in a busy tertiary PACU find the RespiraSense device to be very easy to use.
Limitations of the study include the absence of blinding and the lack of a ‘gold standard’ for RR monitoring for comparison. Both ECG-derived RR monitoring and manual observation are suboptimal techniques. We used these techniques as comparison because they are the most commonly used non-invasive monitoring techniques in our hospital, and thus may reflect current ‘real life’ clinical practice. Comparing the RespiraSense monitor to these controls may have underestimated the accuracy of the RespiraSense device. This study was not powered to the incidence of postoperative obstructive apnoea and no such clinically significant apnoea occurred. As a result it is unclear whether the RespiraSense device would detect obstructive apnoea as well as clinical observation or capnography. A larger study powered to the incidence of such obstructive apnoea is planned. As the average recording time for the current trial was 59.5 min, a study with extended observational periods is required to investigate the trending capability of the RespiraSense. Similarly further trials are required to demonstrate the practical aspects of device use in different types of surgery, e.g. thoracic or paediatric surgery. Finally, patients with a history of respiratory disease were excluded from this study in order to demonstrate safety in a lower risk population—a further study investigating utility in patients with respiratory disease will be required. Strengths of the study include the use of patients with a broad range of ages, anaesthetic techniques and levels of sedation and the use of patient and nurse assessments of comfort and ease of use.
5 Conclusion
We demonstrate a clinically relevant agreement between RR monitored by the RespiraSense device with both ECG-derived and manually observed RR in 48 post-surgical patients.
References
Hillman K, Chen J, Cretikos M, et al. MERIT study investigators. Introduction of the medical emergency team (MET) system: a cluster randomised controlled trial. Lancet. 2005;365:2091–7.
National confidential enquiry into patient outcome and death. An acute problem? London: NCEPOD. http://www.ncepod.org.uk/2005.htm (2005). Accessed 22 June 2014.
Hodgetts TJ, Kenward G, Vlachonikalis IG, et al. The identification of risk factors for cardiac arrest and formulation of activation criteria to alert a medical emergency team. Resuscitation. 2002;54:125–31.
McBride J, Knight D, Piper J, et al. Long-term effect of introducing an early warning score on respiratory rate charting on general wards. Resuscitation. 2005;65:41–4.
Ryan H, Cadman C, Hann L. Setting standards for assessment of ward patients at risk of deterioration. Br J Nurs. 2004;13:1186–90.
Hogan J. Why don’t nurses monitor the respiratory rates of patients? Br J Nurs. 2006;15:489–92.
Fieselmann JF, Hendryx MS, Helms CM, et al. Respiratory rate predicts cardiopulmonary arrest for internal medicine patients. J Gen Intern Med. 1993;8:354–60.
Goldhill DR, McNarry AF, Mandersloot G, et al. A physiologically-based early warning score for ward patients: the association between score and outcome. Anaesthesia. 2005;60:547–53.
Subbe CP, Davies RG, Williams E, et al. Effect of introducing the Modified Early Warning score on clinical outcomes, cardio-pulmonary arrests and intensive care utilisation in acute medical admissions. Anaesthesia. 2003;58:797–802.
Cretikos M, Chen J, Hillman K, et al. The objective medical emergency team activation criteria: a case–control study. Resuscitation. 2007;73:62–72.
Overdyk FJ, Carter R, Maddox RR, et al. Continuous oximetry/capnometry monitoring reveals frequent desaturation and bradypnea during patient-controlled analgesia. Anesth Analg. 2007;105:412–8.
Taenzer AH, Pyke JB, McGrath SP, et al. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers: a before-and-after concurrence study. Anesthesiology. 2010;112:282–7.
Whitaker DK. Time for capnography–everywhere. Anaesthesia. 2011;66(7):544–9.
Kodali BS. Capnography outside the operating rooms. Anesthesiology. 2013;118(1):192–201.
Edmonds ZV, Mower WR, Lovato LM, et al. The reliability of vital sign measurements. Ann Emerg Med. 2002;39:233–7.
Folke M, Cernerud L, Ekström M, et al. Critical review of non-invasive respiratory monitoring in medical care. Med Biol Eng Comput. 2003;41:377–83.
Lovett PB, Buchwald JM, Stürman K, et al. The vexatious vital: neither clinical measurements by nurses nor an electronic monitor provides accurate assessments of respiratory rate in triage. Ann Emerg Med. 2005;45:68–76.
Ouchterlony J, Arvidsson S, Sjöstedt L, et al. Peroperative and immediate postoperative adverse events in patients undergoing elective general and orthopaedic surgery: the Gothenburg study of perioperative risk (PROPER). Part II. Acta Anaesthesiol Scand. 1995;39:643–52.
Rose D, Cohen M, Wigglesworth D, et al. Critical respiratory events in the postanesthesia care unit: patient, surgical, and anesthetic factors. Anesthesiology. 1994;81:410–8.
Friesen RH, Alswang M. End-tidal PCO2 monitoring via nasal cannulae in pediatric patients: accuracy and sources of error. J Clin Monit. 1996;12:155–9.
Acknowledgments
The research project would not have occurred without the patient and professional assistance of the nursing staff in the post anaesthesia care unit of Cork University Hospital. This work was funded by PMD Solutions.
Conflict of interest
P.L. has no financial interest in the RespiraSense device or PMD Solutions.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Lee, P.J. Clinical evaluation of a novel respiratory rate monitor. J Clin Monit Comput 30, 175–183 (2016). https://doi.org/10.1007/s10877-015-9697-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9697-4