Abstract
Clamping and shunting during carotid endarterectomy (CEA) surgery causes changes in cerebral blood flow. The purpose of this study was to assess and compare, side by side, the cerebral oxygenation (rSO2) and processed electroencephalogram (EEG) response bilaterally to carotid artery clamping and shunting in patients undergoing CEA under general anesthesia. With institutional approval and written informed consent, patients undergoing CEA under general anesthesia and routine carotid artery shunting were recorded bilaterally, simultaneously and continuously with an rSO2 and processed EEG monitor. The response of the monitors during carotid artery clamping and shunting were assessed and compared between monitors and bilaterally within each monitor. Sixty-nine patients were included in the study. At clamping the surgical-side and contralateral-side rSO2 dropped significantly below the baseline incision value (−17.6 and −9.4 % respectively). After shunting, the contralateral-side rSO2 returned to baseline while the surgical-side rSO2 remained significantly below baseline (−9.0 %) until the shunt was removed following surgery. At clamping the surgical-side and contralateral-side processed EEG also dropped below baseline (−19.9 and −20.6 % respectively). However, following shunt activation, the processed EEG returned bilaterally to baseline. During the course of this research, we found the rSO2 monitor to be clinically more robust (4.4 % failure rate) than the processed EEG monitor (20.0 % failure rate). There was no correlation between the rSO2 or processed EEG changes that occurred immediately after clamping and the degree of surgical side stenosis measured pre-operatively. Both rSO2 and processed EEG respond to clamping and shunting during CEA. Cerebral oximetry discriminates between the surgical and contralateral side during surgery. The rSO2 monitor is more reliable in the real-world clinical setting. Future studies should focus on developing algorithms based on these monitors that can predict clamping-induced cerebral ischemia during CEA in order to decide whether carotid artery shunting is worth the associated risks. From the practical point of view, the rSO2 monitor may be the better monitor for this purpose.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
For high-grade carotid stenosis, carotid endarterectomy (CEA) remains the recommended treatment for the prevention of stroke in symptomatic patients [1]. One risk of CEA is intraoperative cerebral ischemia due to the decreased cerebral blood flow (CBF) resulting from carotid artery cross-clamping [2]. A shunt may be placed to maintain adequate perfusion to the ipsilateral hemisphere during surgery [3].
A survey of vascular surgeons indicates that as many as 26 % of respondents utilize a shunt only if cerebral ischemia is suggested [4], based on a trial period of cross-clamping [5, 6]. Selective shunting is sometimes favored over routine shunting to avoid risks associated with shunting, including carotid artery dissection, shunt thrombosis or plaque embolization, inadequate shunt flow and limited exposure of the distal portion of the plaque [7]. However, it has been noted that there is not enough evidence to support or refute the use of routine or selective shunting to achieve superior outcomes during CEA under general anesthesia [8]. Improved selection criteria for shunting may be beneficial. In a patient undergoing an awake CEA, acute cerebral ischemia is detected by changes in neurologic or cognitive function [9]. However, it has been reported that 84.6 % of patients undergo CEA under general anesthesia [10].
Many intraoperative monitoring techniques have been utilized for detecting acute cerebral ischemia. These include stump pressures of the internal carotid artery, somatosensory-evoked potentials, transcranial Doppler, real-time electroencephalographic (EEG) monitoring and jugular venous oxygen saturation [5, 11, 12]. These techniques are complex, may require additional personnel, and/or are not highly sensitive or specific for diagnosing acute cerebral ischemia [13].
A class of processed EEG monitors, often referred to as level-of-consciousness (LOC) or depth-of-anesthesia monitors, now in widespread use in the operating room, may offer a simple, reliable and low-cost alternative to the aforementioned techniques for detecting cerebral ischemia in anesthetized patients undergoing CEA. Studies have suggested that an EEG LOC monitor can play a role in detecting acute cerebral ischemia in these patients [7, 9, 11, 13]. Regional cerebral oximetry (rSO2) by near infrared spectroscopy (NIRS), like the processed EEG LOC monitors, also appears to be a promising, reliable, noninvasive and low-cost method of detecting cerebral ischemia [5, 6, 14, 15]. This monitor has several advantages including ease of application and usefulness in patients who lack a temporal bone window and cannot be monitored with transcranial Doppler [5].
We measured the response to clamping and shunting of a common processed EEG and an rSO2 monitor, bilaterally and simultaneously, in patients undergoing CEA under general anesthesia in order to ferret out any differences between the two monitors in response to changes in CBF during this phase of the surgery.
2 Methods
2.1 Study design
This prospective, observational study was approved by our Institutional Review Board (IRB). Patients between the ages of 18 and 85 years, American Society of Anesthesiologists (ASA) class I-IV, who underwent CEA with routine shunting under general anesthesia from June 10, 2011, to July 22, 2013, were included. Patients excluded from this study included prisoners, pregnant women, mentally disabled patients, patients with ASA class V, alcohol or drug abusers, patients being administered drugs, such as ketamine, that may alter the integrity of the EEG or rSO2, or patients not suitable for either processed EEG or rSO2 monitoring as determined by the researcher, surgeon or attending anesthesiologist.
At our institution, the indications for CEA are symptomatic patients with stenosis >50 % and asymptomatic patients with stenosis >80 %. All CEAs performed in this study were primary repairs, utilized routine shunting under general anesthesia, and were completed with patch repair.
2.2 Experimental procedure
The monitors used in this study included the BIS VISTA (Covidien, Manfield, MA USA) processed EEG bilateral LOC monitor and the INVOS 5100c (Covidien) NIRS bilateral cerebral oximeter. The BIS generates a unitless index—the BIS index—that ranges from 0 to 100, with 100 indicating full consciousness. The INVOS generates an index—the rSO2 index—ranging from approximately 15 to 95 that primarily represents the venous oxygen saturation of the tissue underlying the sensor.
Preoperatively, the BIS and INVOS monitors were time-synchronized to each other and to the operating room (OR) clock to establish a common time benchmark. Data storage devices (USB flash drives) were connected to both monitors for real-time data collection and post-processing. The BIS and INVOS electrodes were attached to the patient in the manner specified by the manufacturer. One bilateral BIS electrode was used for sensing the EEG signal from both the surgical side and contralateral side of the brain. Two unilateral INVOS electrodes (one each on the left and right side of the forehead) were used for sensing the rSO2 from the surgical-side and contralateral side of the brain. After confirming that the monitors were functioning properly, but prior to induction, electronic data collection began. Data were recorded simultaneously and continuously beginning just prior to induction of anesthesia to the time the patient was ready for transport from the OR following surgery.
Anesthesia was induced with propofol and maintained with desflurane, sevoflurane or isoflurane per the attending anesthesiologist. Opioid use—either fentanyl or remifentanil—was at the discretion of the anesthesiologist and was generally minimal. The anesthesiologist controlled blood pressure to within 20 % of the baseline (pre-incision) value. He/she treated relative hypotension by decreasing the anesthetic agent, or by treating with phenylephrine or ephedrine. He/she treated hypertension by the increasing the anesthetic level.
During the surgery, the researcher manually recorded the time, systolic and diastolic blood pressure (SAP and DAP), mean arterial pressure (MAP), heart rate (HR), respiratory rate (RR), arterial oxygen saturation (SaO2), inhaled anesthetic concentration, processed EEG index and rSO2 index at the following events:
-
Induction
-
Incision
-
Clamp on
-
Shunt in/clamp off
-
Clamp on/shunt out
-
Clamp off
-
Surgery complete
-
Anesthesia discontinued
-
Patient awake/extubated
Although these parameters were recorded during the surgeries as a matter of course, they were not accounted for in the subsequent rSO2 and processed EEG data analysis because of the observational design of this study.
2.3 Statistical analysis
All inferential statistics assumed an alpha equal to 0.05 for significance. Recorded surgical-side and contralateral-side processed EEG data (recorded electronically once/second) and surgical-side and contralateral-side rSO2 data (recorded electronically approximately once/five seconds) were averaged per minute in boxcar fashion and synchronized in time. We compared the processed EEG index and rSO2 index data separately between the surgical and contralateral sides at each event time point (see Figure Legends for events) with repeated measures ANOVA analysis methods and appropriate post hoc testing. In addition, we identified the minimum processed EEG and rSO2 index value reached immediately following clamping as an indicator of acute decrease in CBF, and compared these values with the degree of carotid stenosis measured preoperatively. We used a multivariate logistical model for this evaluation. Finally, we calculated the five-minute average value of each parameter five minutes after shunting to establish an approximate steady state value following shunt activation. We included all values as events in our statistical analysis.
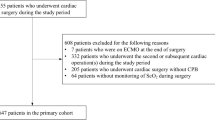
3 Results
Sixty-nine patients were included; data were obtained for 65 patients. Cerebral oxygenation data for three patients were not collected due to monitor malfunction, thus representing a 4.4 % monitor failure rate. One consenting patient was excluded due to an error in the medical records regarding his age (actual age >85 years old). Of the 65 patients for whom rSO2 data were collected, processed EEG data were collected for only 52 patients due to technical problems with the BIS monitor and BIS electrode integrity, thus representing a 20.0 % monitor failure rate. Thirty females and 35 males completed the study. Thirty-five left-sided and 30 right-sided surgeries were performed. Patient demographics are given in Table 1a. Preoperative surgical and contralateral-side stenosis data are provided in Table 1b.
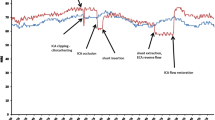
3.1 Typical rSO2 and processed EEG response during CEA surgery
Figure 1 shows a typical cerebral oxygenation and processed EEG versus time response from one patient. At clamping, rSO2 decreased until the shunt was activated and then increased to a relatively steady value during the surgery until the shunt was removed and blood flow was reestablished in the repaired artery. The surgical side rSO2 decreased more than the contralateral side rSO2 and remained lower in comparison throughout surgery. The processed EEG index also decreased following cross-clamping and increased following activation of the shunt. However, there was no clearly discernible difference between the contralateral-side and surgical-side processed EEG response.
a Cerebral oxygenation versus time and b processed EEG index versus time from one patient in this study. Events: 1 = induction; 2 = incision; 3 = clamp on; 4 = shunt in/clamp off (shunt activated); 5 = clamp on/shunt out; 6 = clamp off (blood flow reestablished in repaired artery); 7 = surgery complete; 8 = anesthesia discontinued; 9 = patient awake/extubated
3.2 Overall rSO2 and processed EEG response during CEA surgery
Table 2 and Fig. 2 present the overall rSO2 and processed EEG versus event response for our patient population during CEA surgery. Following clamping the surgical-side rSO2 was significantly lower than contralateral-side oxygenation until the shunt was removed and blood flow was restored in the repaired carotid artery. The processed EEG index decreased bilaterally to a value significantly below baseline following clamping but returned to a value near baseline following shunt activation. There was no significant difference between the contralateral-side and surgical side processed EEG indices within the defined events in this study.
Table 3 shows the significance between incision, considered our baseline event, and the other events in this study, within each group (contralateral and surgical group). Of note, both the rSO2 (surgical-side and contralateral-side) and the processed EEG index decreased significantly below baseline following clamping of the carotid artery. The surgical-side cerebral oxygenation remained statistically lower than baseline through surgery until the shunt was removed and blood flow reestablished in the repaired artery. The processed EEG index returned to the value at incision following shunt activation.
The minimum rSO2 and processed EEG value reached immediately following carotid shunting were not predictive of the degree of carotid stenosis in the diseased artery, as determined preoperatively.
4 Discussion
The risk of acute cerebral ischemia during CEA due to cross clamping of the carotid artery has prompted the interest in monitoring CBF and predicting an ischemic occurrence. When the procedure is performed on awake patients, cerebral ischemia can be effectively assessed with neurologic testing. However, most patients undergo CEA under general anesthesia. As a result, researchers have sought a reliable noninvasive method to detect these ischemic changes when patients are asleep. Our study focuses on rSO2 and processed EEG monitoring as possible methods of tracking changes in cerebral perfusion during CEA. Although these monitors have been studied previously for this purpose, our study is the first to utilize bilateral monitoring with both technologies measured simultaneously in a population of patients undergoing CEA with routine shunting. As a result, we have been able to more clearly demonstrate the response patterns of both monitors to clamping and shunting of the carotid artery and, thus, provide a better comparison of the two monitors.
Cerebral oximetry has shown some promise in tracking changes in CBF during CEA and predicting carotid artery clamping induced cerebral ischemia [5, 6, 14, 16] that would predicate the need for a shunt during surgery. Prediction algorithms have been based on the level of decrease in rSO2 following carotid artery clamping, as compared to indicators such as neurologic testing, transcranial Doppler and real-time EEG analysis. The sensitivity and specificity achieved with these algorithms have suggested a modest usefulness for rSO2 in determining a need for shunt placement.
There is some controversy concerning whether observed changes in rSO2 represent true changes in cerebral perfusion or if they are more related to changes in perfusion of superficial tissues. During CEA, the common, internal and external carotid arteries are clamped prior to insertion of the shunt. Once the shunt is placed, the common and internal carotid arteries are unclamped and the shunt is activated. However, the external carotid artery remains clamped during the shunted portion of the procedure, resulting in decreased perfusion of superficial facial tissues. Our results clearly show that rSO2 increases after activation of the shunt while the external carotid artery remains deprived of blood flow, which confirms that rSO2 responds to true changes in CBF. However, the fact that surgical-side rSO2 does not return all the way to baseline during the shunted period could suggest some contamination of the signal by decreased oxygenation of superficial tissues perfused by the external carotid artery.
Processed EEG monitoring has also been studied as a possible method of tracking changes in CBF during CEA. These monitors are widely available in the OR today and are familiar to anesthesiologists and surgeons. The potential utility of these monitors to track and predict CBF changes has been suggested in the literature [7, 9, 11, 13, 17]. As with the rSO2 studies, these works utilize changes in the processed EEG index to predict the need for shunt placement to avoid cerebral ischemia, and the prediction algorithms are derived using the standard accepted monitoring modalities in sensitivity and specificity analyses. Like the rSO2 algorithms, the processed EEG algorithms have had varying degrees of predictive success.
The majority of studies related to the use of rSO2 and processed EEG monitoring during CEA under general anesthesia have been performed in patients undergoing procedures with selective shunting. It is important to point out that our study is unique in that it demonstrates the consistent response to cross-clamping and shunting of the carotid artery in a population of routinely shunted patients, the majority of who would not have met the criteria for shunt insertion in other studies. Our results support the use of rSO2 monitoring to track changes in CBF during CEA under general anesthesia. Our data show that surgical side rSO2 values consistently decrease in response to cross-clamping of the carotid arteries and increase with shunt placement while contralateral-side values remain relatively constant. Furthermore, unlike processed EEG, the rSO2 response discriminates between the surgical- and contralateral-side of the brain during CEA.
From the technical standpoint, we found the INVOS rSO2 monitoring system to be far more robust than the BIS processed EEG system as far as clinical performance is concerned. With the BIS monitor, we encountered numerous issues with electrode integrity and electrode adhesion, which introduced noise and interruptions in the raw EEG signal and its processing. Of course we recognize that this is, in part, an inherent problem when monitoring microvolt-level electrical signals in a noisy OR environment. In contrast, we had virtually no problems with the INVOS monitoring system. The difficulties we did have were all related to data storage issues.
Although we did not find a relationship between the degree of surgical-side stenosis, as assessed preoperatively, and the minimum rSO2 or processed EEG index values reached at clamping during surgery, this relationship should nevertheless be pursued in further studies because of its potential as a preoperative predictor of cerebral ischemia at carotid artery shunting. Our study was observational and, thus, the true minimum level of the parameters may not have been reached by the time the surgeon activated the shunt. Admittedly, evaluating this relationship was an afterthought on our part and not an element of the original study design. An interventional study would need to be conducted to determine if a correlation exists.
Our study had several limitations. First, we did not control for blood pressure. However, general practice at our institution is to maintain blood pressure at or near the patient’s baseline around the time of cross-clamping. In addition, as this was a purely observational study and we did not use either monitoring modality to suggest intra-operative management changes, we can draw no conclusion from our data regarding the possibility of reducing neurologic complications with rSO2 monitoring.
5 Conclusion
Our data supports the use of rSO2 and processed EEG monitoring as methods of tracking changes in CBF during CEA under general anesthesia. Both monitors are widely available, well understood by clinicians and require no additional personnel. Cerebral oxygenation monitoring discriminates between the surgical and contralateral sides, while processed EEG monitoring does not. Further studies are needed to understand the etiology behind this difference. Additionally, rSO2 had a much lower failure rate in our study. Further studies should be performed using both rSO2 and processed EEG to determine the utility of these monitoring modalities in selective shunt placement and other maneuvers to increase CBF compared to the gold standard of full real-time EEG monitoring. Once reliable thresholds are established, it will need to be determined if the use of these monitors can prevent shunting-related complications or reduce costs.
References
Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125:e2–220.
Kofke WA, Brauer P, Policare R, Penthany S, Barker D, Horton J. Middle cerebral artery blood flow velocity and stable xenon-enhanced computed tomographic blood flow during balloon test occlusion of the internal carotid artery. Stroke. 1995;26(9):1603–6.
Bond R, Rerkasem K, Rothwell PM. Routine or selective carotid artery shunting for carotid endarterectomy (and different methods of monitoring in selective shunting). Stroke. 2003;34:824–5.
Girn HR, Dellagrammaticas D, Laughlan K, Gough MJ. Carotid endarterectomy: technical practices of surgeons participating in the GALA trial. Eur J Vasc Endovasc Surg. 2008;36:385–9.
Pennekamp CW, Bots ML, Kapelle LJ, Moll FL, de Borst GJ. The value of near-infrared spectroscopy measured cerebral oximetry during carotid endarterectomy in perioperative stroke prevention. A review. Eur J Vasc Endovasc Surg. 2009;38(5):539–45.
Pennekamp CW, Immink RV, den Ruijter HM, Kappelle LJ, Bots ML, Buhre WF, et al. Near-infrared spectroscopy to indicate selective shunt use during carotid endarterectomy. Eur J Vasc Endovasc Surg. 2013;46(4):397–403.
Dahaba AA, Xue JX, Hua Y, Liu QH, Xu GX, Liu YM, et al. The utility of using the bispectral Index–Vista for detecting cross-clamping decline in cerebral blood flow velocity. Neurosurgery 2010; 67(3 Suppl Operative):ons102–7; discussion ons107. doi: 10.1227/01.NEU.0000383152.50183.81.
Rerkasem K, Rothwell PM. Routine or selective carotid artery shunting for carotid endarterectomy (and different methods of monitoring in selective shunting). Stroke. 2010;41:e53–4.
Kodaka MK, Nishikawa Y, Suzuki T, Asano K, Maeyama A, Miyao H. Does bilateral bispectral index monitoring (BIS) detect the discrepancy of cerebral reperfusion during carotid endarterectomy? J Clin Anesth. 2009;21:431–4.
Leichtle SW, Mouawad NJ, Welch K, Lampman R, Whitehouse WM Jr, Heidenreich M. Outcomes of carotid endarterectomy under general and regional anesthesia from the American College of Surgeons’ National Surgical Quality Improvement Program. J Vasc Surg. 2012;56(1):81–8.
Skordilis M, Rich N, Viloria A, Dimitrova G, Bergese S, Dzwonczyk R. Electroencephalogram response of patients undergoing carotid endarterectomy: a pilot study. Ann Vasc Surg. 2011;25:909–12.
Samra SK, Dy EA, Welch K, Dorje P, Zelenock GB, Stanley JC. Evaluation of a cerebral oximeter as a monitor of cerebral ischemia during carotid endarterectomy. Anesthesiology. 2000;93:964–70.
Estruch-Perez MJ, Ausina-Aguilar A, Barbera-Alacreu M, Sanchez-Morillo J, Solaz-Roldan C, Morales-Suarez-Varela MM. Bispectral index changes in carotid surgery. Ann Vasc Surg. 2010;24:393–9.
Stilo F, Spinelli F, Martelli E, Pipitó N, Barillà D, De Caridi G, et al. The sensibility and specificity of cerebral oximetry, measured by INVOS 4100, in patients undergoing carotid endarterectomy compared with awake testing. Minerva Anestesiol. 2012;78(10):1126–35.
Pedrini L, Magnoni F, Sensi L, Pisano E, Ballestrazzi M, Cirelli M, et al. Is near-infrared spectroscopy a reliable method to evaluate clamping ischemia during carotid surgery? Stroke Res Treat. 2012:156975. doi: 10.1155/2012/156975. (Epub 2011 Nov 9).
Zogogiannis ID, Iatrou CA, Lazarides MK, Vogiatzaki TD, Wachtel MS, Chatzigakis PK, et al. Evaluation of an intraoperative algorithm based on near-infrared refracted spectroscopy monitoring, in the intraoperative decision for shunt placement, in patients undergoing carotid endarterectomy. Middle East J Anesthesiol. 2011;21(3):367–73.
Heller H, Hatami R, Mullin P, Sciacca RR, Khandji AG, Hamberger M, et al. Bilateral bispectral index monitoring during suppression of unilateral hemispheric function. Anesth Analg. 2005;101(1):235–41.
Conflict of interest
This research was funded internally by The Ohio State University Department of Anesthesiology, and not by the manufacturer of the monitors studied, Covidien. The authors have no conflict of interest with the manufacturer. The authors are compensated by the academic/medical institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Perez, W., Dukatz, C., El-Dalati, S. et al. Cerebral oxygenation and processed EEG response to clamping and shunting during carotid endarterectomy under general anesthesia. J Clin Monit Comput 29, 713–720 (2015). https://doi.org/10.1007/s10877-014-9657-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9657-4