Abstract
Background
Ablation of the slow pathway is an established cure for atrioventricular nodal reentrant tachycardia (AVNRT). Periprocedural damage to the conduction system is a major concern during AVNRT ablation, and cryoablation (CRYO) has been suggested to improve the procedural safety compared to standard radiofrequency (RF) ablation, without reducing the procedural success.
Objective
We performed a systematic review and meta-analysis of studies comparing CRYO with RF ablation of AVNRT.
Methods
We searched PubMed, CENTRAL, the BioMed Central, EMBASE, CardioSource, clinicaltrials.gov, and ISI Web of Science (January 1980 to July 2013). No language restriction was applied. Two independent reviewers screened titles and abstracts to identify studies that compared the procedural outcomes of AVNRT ablation with either CRYO or RF energy. Two independent reviewers assessed the risk of bias according to the Cochrane Collaboration, and extracted patient, study characteristics, and procedural outcome data. Results are expressed as odds ratio (OR) or as weighted mean difference (WMD) with their 95 % confidence interval (CI).
Results
Fourteen studies (5 prospective randomized and 9 observational) with 2,340 patients (mean age range 13 to 53 years, 1,522 (65 %) females) were included in the analysis. RF ablation was performed in 1,262 (54 %) patients, while CRYO in 1,078 (46 %) patients. Acute success (abolition of dual atrioventricular node physiology or single echo beats) was achieved in 88 % of patients treated with RF versus 83 % of those treated with CRYO (OR = 0.72, 95 % CI 0.46 to 1.13; P = 0.157). RF ablation was associated with shorter total procedure time (WMD = −13.7 min, 95 % CI −23 to −4.3 min; P = 0.004), but slightly longer fluoroscopy time (WMD = +4.6 min 95 % CI +1.7 to +7.6 min; P = 0.002). Permanent atrioventricular block occurred in 0.87 % RF cases and in no CRYO case (OR = 3.60, 95 % CI 1.09 to 11.81; P = 0.035). Over a median follow-up of 10.5 months (range 6 to 12 months), freedom from recurrent AVNRT was 96.5 % in the RF group versus 90.9 % in the CRYO group (OR = 0.40, 95 % CI 0.28 to 0.58; P < 0.001). At meta-regression analysis, no clinical or procedural variable had a significant interaction with the results above.
Conclusions
In patients undergoing AVNRT ablation, RF significantly reduces the risk of long-term arrhythmia recurrence compared to CRYO, but is associated with a higher risk of permanent atrioventricular block.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Atrioventricular nodal reentrant tachycardia (AVNRT) is one of the most common sustained supraventricular arrhythmias encountered in clinical practice [1]. The overall prevalence of AVNRT is 2–3 cases per 1,000 persons, accounting for nearly 90,000 new cases every year in US alone [2, 3].
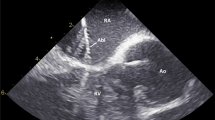
Catheter ablation of the slow pathway provides a lasting cure in a high percentage of patients with AVNRT [4], and represents the first-line therapy for patients with recurrent drug-refractory AVNRT [1]. The major drawback of AVNRT ablation is the risk of periprocedural atrioventricular block (AVB) due to ablation in proximity of the compact AV node. This complication has been reported in up to 1 % of patients treated with radiofrequency (RF) ablation [5, 6]. Cryoablation (CRYO) has been suggested to improve the safety of AVNRT ablation due to the fully reversible tissue injury when applying low-energy lesions (i.e., cryomapping) [7], together with the improved catheter stability due to the adherence of the catheter to the underlying myocardium [8]. Multiple studies have compared the performance of CRYO ablation with standard RF ablation in patients with AVNRT, reporting mixed results [9–22]. To better evaluate the role of CRYO ablation compared to standard RF ablation in AVNRT, we performed a meta-analysis of studies comparing the two ablation energy sources in this setting.
2 Methods
2.1 Data sources and selection
Two trained investigators (R.P, P.S.) independently searched PubMed, CENTRAL, BioMed Central, CardioSource, clinicaltrials.gov, and ISI Web of Science (January 1980 to July 2013). Search keywords included “supraventricular tachycardia AND,” “catheter ablation,” “ablation,” “atrioventricular nodal reentrant tachycardia,” “AVNRT,” “robotic navigation,” “stereotaxis,” “radiofrequency,” “cryoablation,” and “cryo*” (where * denotes a wildcard). No language restriction was used.
2.2 Study selection
Two independent reviewers (R.P., P.S.) performed study selection. Citations initially selected by systematic search were first retrieved as a title and/or abstract and preliminarily screened. Potentially relevant reports were then retrieved as complete manuscripts and assessed for compliance to inclusion criteria. Studies were included if (1) they were focused on catheter ablation of AVNRT, (2) they were specifically designed to compare the outcomes of CRYO versus RF ablation in patients with AVNRT, and (3) they reported the procedural outcomes data separately for the CRYO and RF ablation groups. No restriction regarding the type of AVNRT (i.e., typical vs. atypical) within the eligible studies was applied.
2.3 Data extraction and quality assessment
Two independent reviewers (R.P., P.S.) evaluated the studies for inclusion in the meta-analysis and extracted the data regarding inclusion and exclusion criteria, the total number of patients included, the number of patients undergoing ablation with CRYO or RF energy, the baseline clinical characteristics of the patients, the length of the follow-up, the acute procedural success (i.e., abolition of dual AV nodal physiology or single echo beats), the occurrence of transient AVB, the occurrence of permanent AVB, the total procedure time, the total fluoroscopy time, and the long-term success (i.e., freedom from recurrent AVNRT). Disagreements between reviewers were resolved by a third blinded reviewer (L.D.B.).
Study quality was evaluated according to the established methods of the Cochrane Collaboration [23]. Specifically, we separately estimated the risk of selection, performance, and detection bias [23]. Since the tested intervention (i.e., catheter ablation of AVNRT) was an invasive procedure, allocation concealment and masking were not possible in the original studies [24, 25]. Therefore, in the present analysis, such items were not considered part of the quality assessment [24, 25].
2.4 Data synthesis and analysis
Data are expressed as odds ratio (OR) with 95 % confidence interval (CI) for binary outcomes, and as weighted mean difference (WMD) and 95 % CI for continuous outcome variables.
Binary outcomes (i.e., acute success, long-term success, transient AVB, permanent AVB) from individual studies were analyzed according to the Mantel–Haenszel model to compute individual ORs with pertinent 95 % CI, and pooled summary effect estimate was calculated by means of a fixed-effect model [23, 24]. Weighted mean differences with pertinent 95 % CI were computed for continuous outcome variables (i.e., total procedural time and fluoroscopy time) by entering the mean and standard deviation of differences between baseline and follow-up, and were combined with a DerSimonian and Laird random-effect method to obtain the summary estimate of the endpoint [23, 24].
The meta-analysis was initially conducted on all the retrieved studies [9–22], and then separately on studies with a randomized [9, 10, 15, 18, 22] and observational [11–14, 16, 17, 19–21] design.
The authors compared the robustness of findings from the meta-analysis through a series of additional sensitivity analyses, including random-effects model analyses, and by withdrawing one study at a time [24, 25]. The presence of heterogeneity among studies was evaluated only qualitatively due to the small number of included studies.
The risk of small study bias (including publication bias) was assessed by visual inspection of the funnel plots [26].
To appraise the impact on procedural success and complications (permanent AVB) of covariates potentially affecting the ablation results with CRYO or RF, such as age, gender (percentage of females), type of CRYO catheter used (i.e., 4-mm tip vs. 6-mm tip cryocatheter), and duration of study follow-up, a meta-regression analysis using inverse-variance-weighting (which weighs each study on the basis of its precision) was performed.
The study followed the preferred reporting items for systematic reviews and meta-analyses statement [27]. Statistical level of significance was defined at a P < 0.05 (two-tailed). Analyses were performed using the STATA 11.2 software package (Stata Corporation, College Station, Texas, USA).
3 Results
3.1 Search results and study selection
The search permitted the retrieval of 378 citations. We identified 42 studies, which were assessed according to compliance to the inclusion criteria. Five studies had a prospective randomized design and compared the outcomes of CRYO versus RF ablation in AVNRT [9, 10, 15, 18, 22]. Nine studies had an observational design (Table 1) [11–14, 16, 17, 19–21]. Other 28 studies were excluded; the reasons for study exclusion are highlighted in Fig. 1. Ultimately, 14 published studies were selected and included in the meta-analysis [9–22]. One study (Ding et al. [19]) was in Chinese language and was appropriately translated in English to allow inclusion in the pooled analysis. A flow diagram showing the selection process is shown in Fig. 1.
3.2 Qualitative findings
Table 1 reports the baseline characteristics of the 14 studies included in the meta-analysis [9–22]. All studies were designed to compare the outcomes of AVNRT ablation with either CRYO or RF energy, and all used standard manual ablation [9–22]. There was substantial qualitative heterogeneity in the design of studies. As mentioned, five studies had a prospective randomized design [9, 10, 15, 18, 22], and were of comparable quality (Fig. 2). All studies included adult patients with AVNRT and reported detailed data on the procedural outcomes of interest. A 4-mm non-irrigated tip catheter was adopted in the RF arm of all the randomized studies [9, 10, 15, 18, 22]. The type of cryocatheter used was heterogeneous, with a 4-mm tip catheter in two of the randomized studies [9, 10], and a 6-mm tip catheter in the remaining three studies [15, 18, 22]. Cryomapping was performed in all the studies [9, 10, 15, 18, 22]. After ablation, patients were followed-up with scheduled office visits [9, 10, 15, 18, 22], and with ECG and 24-h Holter monitoring [10, 15, 18]. A loop recorder (3 months post-procedure) was used only in the study by Kimman et al. [9]. Overall, the 5 randomized studies included a total of 911 patients (mean age range 46 to 51 years, 559 (61 %) females) with an average follow-up of 7.6 ± 2.6 months (range 6 to 12 months).
Nine studies had an observational design [11–14, 16, 17, 19–21]. Of these, 8 were retrospective [11–14, 17, 19–21], 1 prospective, and included a total of 1,429 patients (67 % females) [16]. Three studies included pediatric population with AVNRT (mean age range 13 to 14.2 years) [11, 13, 17], and the remaining six studies were focused on adults with AVNRT (mean age range 46 to 53 years) [12, 14, 16, 19–21]. The quality of the observational studies were scored at high risk of bias and appeared comparable (Fig. 2). Detailed procedural success and complications data for quantitative analysis were retrievable from all the studies [11–14, 16, 17, 19–21]. Three studies did not report the total procedure and fluoroscopy time [13, 16, 19]. A 4-mm non-irrigated tip catheter was adopted in the RF arm of all the studies. A 4-mm tip cryocatheter was used in four studies [11–13, 20], a 6-mm tip cryocatheter in three [14, 16, 17], and a 8-mm tip cryocatheter in one study [21]. The study by Ding et al. [19] did not report the type of cryocatheter used. Patients were followed-up with scheduled office visits [11–14, 16, 17, 19–21], and with ECG and 24-h Holter monitoring [13, 14, 16, 17, 20, 21]. None of the included studies adopted three-dimensional non-fluoroscopic mapping systems.
The final pooled analysis included a total of 2,340 patients (mean age range 13 to 53 years, 1,522 (65 %) females), of whom 1,262 (54 %) were treated with RF ablation, and 1,078 (46 %) with CRYO ablation.
3.3 Quantitative data synthesis
3.3.1 Acute success
Acute procedural success, defined as elimination of dual AV nodal physiology or single echo beats, was achieved in 1,111/1,262 (88 %) of patients treated with RF and in 896/1,078 (83 %) of those treated with CRYO (OR = 0.72, 95 % CI 0.46 to 1.13, P = 0.157; I 2 = 0 %) (Fig. 3). The same results were obtained when analyzing only studies with a randomized design (OR = 0.71, 95 % CI 0.32 to 1.58; P = 0.404), or with an observational design (OR = 0.73, 95 % CI 0.42 to 1.26; P = 0.252) (Fig. 3). All the other prespecified sensitivity analyses did not affect the results. Meta-regression analysis failed to show a significant interaction between the tested variables and the acute procedural success. There was no evidence of publication bias (bias coefficient = −0.75, P = 0.896).
Forest plot showing the individual and pooled odds ratio (OR) of acute procedural success (abolition of dual atrioventricular node physiology or single echo beats) comparing radiofrequency (RF) with cryoenergy (CRYO) across observational and randomized studies. Square boxes denote OR; horizontal lines represent 95 % confidence interval (CI)
3.3.2 Procedural time and fluoroscopy time
RF ablation was associated with a significantly shorter total procedure time as compared to CRYO (WMD = −13.7 min, 95 % CI −23 to −4.3 min, P = 0.004; I 2 = 78 %) (Fig. 4). This result was driven by the inclusion of data from randomized trials (WMD = −13.3 min, 95 % CI −23.3 to −3.3 min; P = 0.009), as it was not confirmed when restricting the analysis only to observational studies (WMD = −15.1 min, 95 % CI −34.9 to +4.8 min; P = 0.137) (Fig. 4).
Forest plot showing the individual and pooled weighted mean differences (WMD) of total procedural time comparing radiofrequency (RF) versus cryoenergy (CRYO). Square boxes denote WMD. The dimension of each square box denotes the weight from random effect analysis. Horizontal lines represent 95 % confidence interval (CI)
On the other side, fluoroscopy time was slightly longer with RF (WMD = +4.6 min, 95 % CI +1.7 to +7.6 min, P = 0.002; I 2 = 88 %) (Fig. 5). This result appeared consistent in both randomized (WMD = +5 min, 95 % CI +0.3 to +9.7 min; P = 0.036) and observational studies (WMD = +4.4 min, 95 % CI +0.3 to +8.4 min; P = 0.033) (Fig. 5).
Forest plot showing the individual and pooled weighted mean differences (WMD) of fluoroscopy time comparing radiofrequency (RF) versus cryoenergy (CRYO). Square boxes denote WMD. The dimension of each square box denotes the weight from random effect analysis. Horizontal lines represent 95 % confidence interval (CI)
3.3.3 Periprocedural atrioventricular block
Data on periprocedural transient AVB were retrievable from 11 studies [9–13, 16–18, 20–22]. Transient AVB occurred in 29/687 (4.2 %) patients in the RF group compared to 59/680 (8.7 %) in the CRYO group (OR = 0.49, 95 % CI 0.31 to 0.76; P = 0.001) (Fig. 6). In the CRYO group, none of these events translated into permanent AVB. On the other side, permanent AVB occurred in 0.87 % of patients treated with RF (OR = 3.60, 95 % CI 1.09 to 11.81; P = 0.035).
3.3.4 Long-term success
After a median follow-up of 10.5 months (range 6 to 12 months), freedom from recurrent AVNRT was achieved in 96.5 % in the RF group, and in 90.9 % in the CRYO group (OR = 0.40, 95 % CI 0.28 to 0.58, P < 0.001; I 2 = 0.5 %) (Fig. 7). The same results were obtained when analyzing only studies with a randomized design (OR = 0.38, 95 % CI 0.22 to 0.68; P = 0.001) or with an observational design (OR = 0.41, 95 % CI 0.25 to 0.67; P < 0.001) (Fig. 7). All the other prespecified sensitivity analyses did not affect the results. Indeed, point estimates and 95 % CIs for ORs all remained >1.0 when sequentially excluding each study in turn. Meta-regression analysis failed to show a significant interaction between the tested variables and the long-term procedural success. There was no evidence of publication bias (bias coefficient = −0.17, P = 0.816).
3.3.5 Combined endpoint: procedural failure and AVNRT recurrence
When analyzing the combined endpoint of procedural failure (including permanent AVB) and arrhythmia recurrence, RF was associated with a significant lower risk of the composite endpoint compared to CRYO (OR = 0.47, 95 % CI 0.33 to 0.67, P < 0.001; I 2 = 0 %). These results were highly consistent, as they were not affected by any of the prespecified sensitivity analyses. Meta-regression analysis also failed to show an interaction between the tested covariates and the composite endpoint of procedural failure and AVNRT recurrence.
4 Discussion
This systematic review was designed to compare the outcomes of CRYO versus standard RF ablation for the treatment of AVNRT, and is based on the statistical pooling of 14 studies enrolling more than 2,300 patients [9–22]. The present analysis includes a large AVNRT cohort in which the two energy sources have been formally compared, and mainly shows that RF is associated with a significantly higher long-term success as compared to CRYO, but also with a slightly increased risk of periprocedural permanent AVB.
The results of our study may have important clinical implications. After the first description by Jackman et al. of the feasibility and safety of slow pathway ablation in a consecutive series of patients [4], catheter ablation has been consistently implemented as a curative approach in patients with AVNRT, and is nowadays included among the first-line treatments for this arrhythmia [1]. The risk of permanent damage to the compact AV node, with resulting permanent AVB, still represents a major concern during RF ablation in the slow pathway region. In a prospective registry including 1,197 patients undergoing RF ablation of AVNRT, advanced AVB (second or third degree) was reported in 1 % of patients [6]. A recent systematic review reported an overall incidence of AVB of 1.7 % [28], with a long-term arrhythmia-free survival of 94.3 %. In an effort to improve the safety of AVNRT ablation, CRYO has been introduced as an alternative treatment option to standard RF for slow pathway ablation. The possible benefits of CRYO compared to RF include increased catheter stability and lower risk of catheter dislodgment during ablation due to cryoadherence to the underlying myocardium [29], the creation of more homogeneous and sharply demarcated lesions [30], and the fact that cryoablation is virtually painless, possibly reducing the need for anesthesia and minimizing patients' movements and respiratory excursions. In addition, CRYO offers the unique possibility of cryomapping, that is, delivering a lesion above the target temperature for irreversible tissue necrosis (typically at −30 °C) to evaluate the effect of ablation and to prove that no collateral damage is occurring. Although some authors have questioned the complete irreversibility of lesions during cryomapping, no permanent lesion has ever been convincingly demonstrated with such an approach. To the best of our knowledge, no case of permanent AVB requiring pacemaker implant has ever been reported with CRYO ablation of AVNRT.
The results of our analysis largely confirm the higher safety profile of CRYO over RF in the setting of AVNRT. Indeed, no permanent AVB was reported in the CRYO group, compared to an overall rate of 0.87 % in the RF group. These results are in line with a recently published pooled analysis by Hanninen et al. [31]. At variance with Hanninen et al. [31], we performed a formal meta-regression analysis to appraise the impact of different covariates, including age, gender, type of cryocatheter used, and duration of study follow-up on the risk of periprocedural AVB with RF. Of note, meta-regression analysis failed to disclose a significant interaction between baseline clinical or procedural variables and the risk of permanent injury to the AV node with RF. On the other hand, the absolute rate of this complication was small, and even our meta-analysis might be underpowered to fully evaluate for predictors of AVB. In addition, it is possible that longer follow-up periods might result in increased number of late AVB, which represent a limitation of the studies included in the pooled analysis.
It is worth emphasizing the finding of an increased risk of transient and reversible AVB in the CRYO group (8.7 vs. 4.2 %, P = 0.001), which might be related to the more anterior approach used during AVNRT ablation with CRYO [32]. Nonetheless, as mentioned, none of these patients eventually developed complete AVB, which further highlights the safety of CRYO for AVNRT ablation.
Fluoroscopy times were also lower in the CRYO group. This finding can be explained by the increased stability of the cryocatheter during ablation, which reduces the necessity of a constant monitoring of the catheter position with fluoroscopy.
Finally, with regard to long-term arrhythmia-free survival, RF was associated with a significantly lower rate of AVNRT recurrence over long-term follow-up (3.5 vs. 9.1 %, P < 0.001). The finding was consistent across all the included studies, and was further confirmed when analyzing the composite endpoint of procedural failure (including permanent AVB) and AVNRT recurrence. In addition, no interaction was found between different clinical and procedural variables and the better long-term procedural success with RF at meta-regression analysis. In this regard, it is important to emphasize that lack of statistical significance at meta-regression analysis should not be conclusively viewed as lack of clinical effect, given the well-known limitations in statistical power of meta-regression [33].
Furthermore, some important variables, such as the number of cryoablation cycles, were not consistently retrievable from all the included studies. Therefore, we were not able to fully evaluate the impact of such confounders on the results of our pooled analysis.
5 Conclusions
This review presents a meta-analysis of data from 14 studies comparing CRYO with RF for the catheter ablation of AVNRT, and shows a significantly increased long-term arrhythmia-free survival with RF, although with a higher risk of permanent AVB. Given the substantial higher impact of permanent AVB compared to recurrent AVNRT, physicians or patients might opt for CRYO energy instead of RF when procedural safety is preferred to long-term arrhythmia-free survival.
References
Blomstrom-Lundqvist, C., Scheinman, M. M., Aliot, E. M., et al. (2003). ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias–executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias). Circulation, 108, 1871–1909.
Goyal, R., Zivin, A., Souza, J., et al. (1996). Comparison of the ages of tachycardia onset in patients with atrioventricular nodal reentrant tachycardia and accessory pathway-mediated tachycardia. American Heart Journal, 132, 765–767.
Lee, K. W., Badhwar, N., & Scheinman, M. M. (2008). Supraventricular tachycardia–part I. Current Problems in Cardiology, 33, 467–546.
Jackman, W. M., Beckman, K. J., McClelland, J. H., et al. (1992). Treatment of supraventricular tachycardia due to atrioventricular nodal reentry by radiofrequency catheter ablation of slow-pathway conduction. New England Journal of Medicine, 327, 313–318.
Calkins, H., Yong, P., Miller, J. M., et al. (1999). Catheter ablation of accessory pathways, atrioventricular nodal reentrant tachycardia, and the atrioventricular junction: final results of a prospective, multicenter clinical trial. The Atakr Multicenter Investigators Group. Circulation, 99, 262–270.
Scheinman, M. M., & Huang, S. (2000). The 1998 NASPE prospective catheter ablation registry. Pacing and Clinical Electrophysiology, 23, 1020–1028.
Baust, J. G., & Gage, A. A. (2005). The molecular basis of cryosurgery. BJU International, 95, 1187–1191.
Jentzer, J. H., Goyal, R., Williamson, B. D., et al. (1994). Analysis of junctional ectopy during radiofrequency ablation of the slow pathway in patients with atrioventricular nodal reentrant tachycardia. Circulation, 90, 2820–2826.
Kimman, G. P., Theuns, D. A., Szili-Torok, T., et al. (2004). CRAVT: a prospective, randomized study comparing transvenous cryothermal and radiofrequency ablation in atrioventricular nodal reentrant tachycardia. European Heart Journal, 25, 2232–2237.
Zrenner, B., Dong, J., Schreieck, J., et al. (2004). Transvenous cryoablation versus radiofrequency ablation of the slow pathway for the treatment of atrioventricular nodal reentrant tachycardia: a prospective randomized pilot study. European Heart Journal, 25, 2226–2231.
Collins, K. K., Dubin, A. M., Chiesa, N. A., Avasarala, K., & Van Hare, G. F. (2006). Cryoablation versus radiofrequency ablation for treatment of pediatric atrioventricular nodal reentrant tachycardia: initial experience with 4-mm cryocatheter. Heart Rhythm, 3, 564–570.
Gupta, D., Al-Lamee, R. K., Earley, M. J., et al. (2006). Cryoablation compared with radiofrequency ablation for atrioventricular nodal reentrant tachycardia: analysis of factors contributing to acute and follow-up outcome. Europace, 8, 1022–1026.
Avari, J. N., Jay, K. S., & Rhee, E. K. (2008). Experience and results during transition from radiofrequency ablation to cryoablation for treatment of pediatric atrioventricular nodal reentrant tachycardia. Pacing and Clinical Electrophysiology, 31, 454–460.
Chan, N. Y., Mok, N. S., Lau, C. L., et al. (2009). Treatment of atrioventricular nodal reentrant tachycardia by cryoablation with a 6-mm-tip catheter versus radiofrequency ablation. Europace, 11, 1065–1070.
Deisenhofer, I., Zrenner, B., Yin, Y. H., et al. (2010). Cryoablation versus radiofrequency energy for the ablation of atrioventricular nodal reentrant tachycardia (the CYRANO Study): results from a large multicenter prospective randomized trial. Circulation, 122, 2239–2245.
Opel, A., Murray, S., Kamath, N., et al. (2010). Cryoablation versus radiofrequency ablation for treatment of atrioventricular nodal reentrant tachycardia: cryoablation with 6-mm-tip catheters is still less effective than radiofrequency ablation. Heart Rhythm, 7, 340–343.
Papagiannis, J., Papadopoulou, K., Rammos, S., & Katritsis, D. (2010). Cryoablation versus radiofrequency ablation for atrioventricular nodal reentrant tachycardia in children: long-term results. Hellenic journal of cardiology. Hellenic journal of cardiology, 51, 122–126.
Chan, N. Y., Choy, C. C., Lau, C. L., et al. (2011). Cryoablation versus radiofrequency ablation for atrioventricular nodal reentrant tachycardia: patient pain perception and operator stress. Pacing and Clinical Electrophysiology, 34, 2–7.
Ding, Y. H., Qu, B. M., Che, X. D., et al. (2011). [Comparison of cryoablation and radiofrequency ablation for treating atrioventricular nodal reentrant tachycardia]. Zhonghua xin xue guan bing za zhi, 39, 625–627.
Schwagten, B., Knops, P., Janse, P., et al. (2011). Long-term follow-up after catheter ablation for atrioventricular nodal reentrant tachycardia: a comparison of cryothermal and radiofrequency energy in a large series of patients. Journal of interventional cardiac electrophysiology, 30, 55–61.
Chan, N. Y., Mok, N. S., Choy, C. C., et al. (2012). Treatment of atrioventricular nodal reentrant tachycardia by cryoablation with an 8-mm-tip catheter versus radiofrequency ablation. Journal of interventional cardiac electrophysiology, 34, 295–301.
Rodriguez-Entem, F. J., Exposito, V., Gonzalez-Enriquez, S., & Olalla-Antolin, J. J. (2013). Cryoablation versus radiofrequency ablation for the treatment of atrioventricular nodal reentrant tachycardia: results of a prospective randomized study. Journal of interventional cardiac electrophysiology, 36, 41–45. discussion 45.
Cochrane Handbook for systematic reviews of interventions, Version 5.1.0. Updated March 2011, The Cochrane Collaboration, available from ≤http://www.cochrane-handbook.org/%3E.
Santangeli, P., Di Biase, L., Pelargonio, G., et al. (2011). Cardiac resynchronization therapy in patients with mild heart failure: a systematic review and meta-analysis. Journal of interventional cardiac electrophysiology: an international journal of arrhythmias and pacing, 32, 125–135.
Santangeli, P., Di Biase, L., Dello Russo, A., et al. (2010). Meta-analysis: age and effectiveness of prophylactic implantable cardioverter-defibrillators. Annals of Internal Medicine, 153, 592–599.
Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315, 629–634.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of Internal Medicine, 151, 264–269. W64.
Spector, P., Reynolds, M. R., Calkins, H., et al. (2009). Meta-analysis of ablation of atrial flutter and supraventricular tachycardia. American Journal of Cardiology, 104, 671–677.
Lustgarten, D. L., Keane, D., & Ruskin, J. (1999). Cryothermal ablation: mechanism of tissue injury and current experience in the treatment of tachyarrhythmias. Progress in Cardiovascular Diseases, 41, 481–498.
Mikat, E. M., Hackel, D. B., Harrison, L., Gallagher, J. J., & Wallace, A. G. (1977). Reaction of the myocardium and coronary arteries to cryosurgery. Laboratory Investigation, 37, 632–641.
Hanninen, M., Yeung-Lai-Wah, N., Massel, D., et al. (2013). Cryoablation versus RF ablation for AVNRT: a meta-analysis and systematic review. Journal of cardiovascular electrophysiology; In press.
De Sisti, A., Tonet, J., Gueffaf, F., et al. (2008). Effects of inadvertent atrioventricular block on clinical outcomes during cryoablation of the slow pathway in the treatment of atrioventricular nodal reentrant tachycardia. Europace, 10, 1421–1427.
Doughty, R. N., Whalley, G. A., Gamble, G., MacMahon, S., & Sharpe, N. (1997). Left ventricular remodeling with carvedilol in patients with congestive heart failure due to ischemic heart disease. Australia–New Zealand Heart Failure Research Collaborative Group. Journal of the American College of Cardiology, 29, 1060–1066.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Santangeli, P., Proietti, R., Di Biase, L. et al. Cryoablation versus radiofrequency ablation of atrioventricular nodal reentrant tachycardia. J Interv Card Electrophysiol 39, 111–119 (2014). https://doi.org/10.1007/s10840-013-9842-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-013-9842-2