Abstract
Children with autism spectrum disorder (ASD) are at greater risk for experiencing high levels of anxiety symptoms. Recent evidence suggests Cognitive behavioral therapy (CBT) may also be effective for anxiety reduction in some presentations of ASD. This meta-analysis evaluated twenty-three studies. Results yielded a moderate effect size (g = − 0.66) for the reduction of anxiety symptoms. Moderators indicated larger effects for studies were achieved with parental involvement (g = − 0.85, p < .05) than with child-only treatments (g = − 0.34, p < .05). Short-term interventions generated a smaller effect (g = − 0.37 p < .05) than either standard-term (g = − 1.02, p < .05) or long-term interventions (g = − 0.69, p < .05).Implications for children with ASD are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Autism Spectrum Disorder (ASD) is a multifaceted neurodevelopmental disorder characterized by difficulties with social interactions, problems with communication, and restricted and/or repetitive behaviors (American Psychiatric Association (APA) 2013). There is widespread concern regarding the prevalence and incidence of ASD. For example, the Centers for Disease Control and Prevention (CDC 2018) indicated that 1 in 59 children in the United States are identified with ASD, placing the total cost of intervention between $11.5 billion and $60.9 billion.
Comorbidity with other disorders is common among children with ASD. Mental health related disorders include depression, anxiety, attention deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder (Simonoff et al. 2008). In particular, studies have shown children with ASD are at greater risk for experiencing higher levels of anxiety related symptoms when compared to typically developing children (Steensel and Bogels 2015). Up to 80% of children with ASD could meet the diagnostic criteria for an anxiety disorder (Simonoff et al. 2008). Steensel et al. (2011) reported several types of anxiety disorders occurring in children with ASD, including specific phobia (29.8%), obsessive–compulsive disorder (17.4%), and social anxiety disorder (16.6%). The presence of high levels of anxiety in children with ASD can negatively impact social and emotional outcomes, relationships with peers, and educational performance (Fujii et al. 2012; Reaven et al. 2011; Wood et al. 2015). Studies also noted that children with ASD displayed a number of inconsistent fears and anxieties (Kim et al. 2011; White et al. 2009). For example, Kerns and colleagues (2014) assessed anxiety symptoms in children with ASD that are consistent and inconsistent with DSM-5 (APA 2013) criteria in 59 participants. Results indicated that 46% of children showed atypical anxiety symptoms that were not consistent with any DSM-5 criteria. Such symptoms may not be easily captured by these criteria (Kerns et al. 2014). Leaving these children without treatment may cause long-term developmental and psychological problems, such as limited social interactions or rejection, difficulties in a school environment, and underemployment after graduation (Clark et al. 1994). For these reasons, the development of effective interventions for reducing level of anxiety in children with ASD is an important healthcare as well as educational priority (Reaven et al. 2011).
Cognitive Behavior Therapy
Cognitive Behaviour Therapy (CBT) is an evidence-based psychosocial practice originally developed for treatment of adult depression that has been extended to many other areas, including the treatment and primary prevention of anxiety in typically developing children, adolescents, and adults (Chorpita 2007; Kendall 1993). The cognitive-behavioral model was originally developed by Beck (1976) to address the causes of anxiety and depression, and has been improved upon by researchers during the last several decades (Beck 1976; Kendall and Kriss 1983). The primary goal of CBT is to teach individuals to identify irrational beliefs, monitor automatic thoughts, and replace negative automatic thoughts with more realistic and adaptive ones (Kendall and Hedtke 2006). Programs using CBT typically use a structured manual or a modular format involving three features: (1) cognitive restructuring, (2) copings skills, and (3) problem-solving (e.g., Barrett et al. 1996; Chorpita 2007; Kendall and Hedtke 2006). Structured manualized CBTs include explicit cognitive and behavioral techniques with specific sessions and instructions. Examples of structured manualized CBT programs are Coping Cat (Kendall and Hedtke 2006), the Coping Koala (Barrett et al. 1996), and Skills for Academic and Social Success (Warner et al. 2007). While there are benefits to structured manualized programs, they often lack the flexibility to customize interventions for individual needs—such as selecting modules for a particular child. Modular programs, however, allow for more flexibility and provide tailored interventions based on specific individualized needs (Chorpita 2007).
Previous studies have demonstrated the effectiveness of CBTs for children with emotional and behavioral difficulties (Kendall and Hedtke 2006). Although much of the current literature predominantly on CBT involves typically developing children, a growing body of evidence is demonstrating positive outcomes for children with ASD (e.g., Chalfant et al. 2006; White et al. 2012; Wood et al. 2009). Within this emerging evidence, most children with ASD struggle to control and manage their emotions in social communications (Bauminger 2002). As a result, modifications and additions to CBT protocols were recommended for children with ASD (Fujii et al. 2012). Previous CBT protocols have been successfully modified while keeping the core components of CBT intact, demonstrating that modified or modular CBTs may be an effective treatment of anxiety in children with ASD (Chalfant et al. 2006; Reaven et al. 2011; Sofronoff et al. 2005; Sung et al. 2011; Wood et al. 2009). A variety of modified and modular CBT treatments have been evaluated in the research literature with parental involvement and length of the treatment associated with differential treatment outcomes (e.g., Chalfant et al. 2006; Reaven et al. 2011; Storch et al. 2013).
Parental Involvement
Parental involvement in the treatment of anxiety for children with ASD has been a focus of previous studies (Chalfant et al. 2006; Sofronoff et al. 2005). Chalfant et al. (2006) used family-based CBT protocols to reduce anxiety levels in 47 children with comorbid anxiety disorder and high-functioning ASD. Treatment lasted 12 weeks and involved a CBT intervention group and a control group. Therapists saw participants in the CBT intervention group for 2-h weekly sessions. Study findings revealed that 71.4% (20 of 28 children) of the treated participants reduced their anxiety levels under the diagnostic criteria for anxiety disorder. Moreover, Ehrenreich-May et al. (2014) evaluated the effectiveness of parental involvement in managing anxiety. Twenty children (ages 11–14 years) with ASD were selected to take part in an evaluation of the Behavioral Interventions for Anxiety in Children with Autism (BIACA) manualized intervention, where children were treated with their families for the 16-week intervention period. Clinician, child, and parent-rated data were analyzed, and a significant decrease in anxiety was found at post-treatment. Parent-rated externalizing symptoms also showed a statistically significant decrease (g = − 0.91).
Length of Treatment
Length of treatment may impact treatment outcomes. A review of current CBT protocols shows a variation in the length of time for treatment or “dosage.” Most CBT interventions were 12 weeks in length with weekly sessions (Chalfant et al. 2006; Reaven et al. 2011). Because of the limited time school settings, a few recent studies used a shortened CBT to meet the needs of these children protocol (e.g., Clarke et al. 2016; Luxford et al. 2016; Maskey et al. 2014). McConachie et al. (2013) used a 7-week “Exploring Feelings” intervention for 32 children aged 9–13 years, and found limited reduction in anxiety symptoms of the participants. Some studies have attempted to increase the effectiveness of CBT treatment by increasing the length of the intervention. Fujii et al. (2012) sought to determine if a longer treatment improved the effectiveness of CBT and skill maintenance with treatment lasting 32 weeks. Participants (ages 7–11 years) were randomly selected to participate in the CBT program or a 16-week treatment as usual. Post-treatment results indicated that five of the children in the experimental group no longer met eligibility criteria for an anxiety disorder diagnosis. The effects of factors such as duration, session length and contact time on efficacy of treatment are unclear, as different intervention studies have varied on each of these aspects.
Purpose and Research Questions
Many children with ASD experience high levels of anxiety, especially when compared to typically developing peers. CBT is an anxiety reducing intervention, and emerging evidence suggests CBT may be an effective approach for reducing anxiety for children with high-functioning ASD. We use the term high-functioning ASD to describe individuals with ASD who require supports at level one according to the DSM-5, have sentence-to-conversational-level speech skills, and are of average to above average intelligence. Two meta-analyses have examined the overall effectiveness of CBT as an intervention aimed at anxiety reduction in children with ASD (e.g., Sukhodolsky et al. 2013; Ung et al. 2014). Sukhodolsky et al. (2013) found an overall effect size of d = 1.19, and d = 1.21 for clinical and parent rated outcome measures, respectively, from eight randomized control trail studies (RCTs) without moderator analyses. Ung et al. (2014) reported an overall effect of g = 0.71 from 14 RCTs or open trial studies. Ung and colleagues tested anxiety informant (child, parent or clinician) and treatment modality (group session versus individual sessions), and found that anxiety informant and treatment modality were not significant moderators for CBT treatments. Missing from these earlier meta-analyses were moderator analyses of treatment length or parent involvement. The goal of the current meta-analysis is to update the literature and evaluate the moderators of treatment length and parent involvement. Specific research questions posed were:
-
1.
To what extent can CBT reduce anxiety-related outcomes in children with high-functioning ASD?
-
2.
Does parent involvement in CBT impact anxiety related outcomes in children with high-functioning ASD?
-
3.
Does treatment length impact on the overall effects of CBT in children with high-functioning ASD?
Method
Literature Search and Inclusion Criteria
A search and coding protocol was developed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Moher et al. 2009). First, an electronic search of the literature was conducted to identify studies that examined the effects of CBTs in treating anxiety for children with ASD. The following electronic databases and platforms were searched: (1) Education Full Text, (2) Educational Resources Information Center (ERIC), and (3) PsycINFO. Google Scholar was also searched to help identify as many relevant studies as possible. The search terms used were: “Asperger,” “autism,” “ASD,” “anxiety,” “cognitive behavioral therapy,” and “CBT.” The keywords were used alone and in combination to identify potential studies for inclusion.
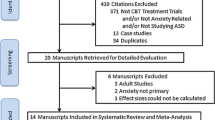
Figure 1 provides an overview of the identification, screening, eligibility, and inclusion steps. Specific criteria for inclusion were: (1) participants were aged 18 years or younger, (2) participants had a primary diagnosis of ASD without an identified intellectual disability, (3) participants had a diagnosis of anxiety disorder or characteristics associated with risk for developing an anxiety disorder, (4) at least one standardized measure of anxiety was reported, (5) a group experimental design was used, (6) a program incorporating CBT for anxiety was implemented, (7) the study was published in a peer-reviewed journal, and (8) the article was written in English. Theses, dissertations, and unpublished reports were not included in this review. Group design studies were included if they: (1) had at least one experimental group that was under the control of experimenter; (2) controlled and systematically manipulated the experimental group; (3) used appropriate typical data analysis methods (t tests, ANOVAs/MANOVAs, ANCOVAs/MANCOVAs, hierarchical linear modeling, structural equation modeling); and, (4) reported at least one appropriate effect size statistic (Cohen’s d, Hedges’ g, Glass’s ∆,; CEC, Cook et al. 2014). Single-case design or qualitative studies were not included for this current study. Initially 633 citations were identified through the database search. Of these, 82 duplicated studies were removed, and 497 were removed after reviewing the abstract because they were either not CBT treatment for ASD or anxiety disorders; 54 articles were then screened for further review. After removing dissertations using single-case designs (n = 7), unpublished reports (n = 5), systematic reviews (n = 4), and meta-analyses (n = 2), 34 articles were assessed for eligibility. From this set of 34, 11 studies were excluded because: raw data were not reported to allow for effect size calculation (n = 2), they were follow-up studies (n = 2), they included individuals older than 18 years of age (n = 2), or they only included participants with non-high-functioning autism (n = 5). As a result, 23 studies were found to have met the initial inclusion criteria.
Variable Coding and Coding Reliability
Each study was coded independently by two trained researchers for the following information: study name, sample size, participants’ age, gender and ethnicity, type of the intervention, intervention format (i.e., with or without parental involvement), and intervention length (see Table 1 for characteristics of the included studies). Reliability was calculated for 30% of the studies (n = 7). The formula used for inter-coder agreement was the sum of agreement/total number of agreements + disagreements × 100 (House et al. 1981). Inter-coder agreement for study characteristics was 92%.
Potential Moderators
Studies were coded for two possible moderator variables: (1) parental involvement and (2) the length of intervention. Parental involvement was coded as a dichotomous variable (i.e., with parental involvement or without parental involvement). Length of the intervention was coded as short-term (shorter than 12 weeks), standard-term (12 to 15 weeks), and long-term (16 weeks or longer).
Data Analysis
Effect sizes were fitted to the data using standardized mean differences between treatment and comparison group at post-treatment (Cohen 1969). All studies used anxiety related outcomes that reflected more than one type of scale. Therefore, the effect sizes were combined and averaged for each study (as suggested in: Lipsey and Wilson 2001). Only one study (Sofronoff et al. 2005) included more than one experimental group (one with and one without parental involvement). As a result, effect sizes were calculated for each subsample within the study (Sofronoff et al. 2005). A number of included studies reported pre- post- group change findings and did not use control groups. In the absence of a control group or comparison group, mean changes in treatment group scores from pre-treatment and post-treatment were used to determine effect sizes in seven studies (Ehrenreich-May et al. 2014; Maskey et al. 2014; Ooi et al. 2008; Steensel & Bogels 2015; Sung et al. 2011; Thomson et al. 2015; Weiss et al. 2015). Initially, Cohen’s d was calculated using the raw scores from each study (Cohen 1969). In a meta-analysis, it is critically important to consider the possible standard error (Lipsey and Wilson 2001). Therefore, all effect sizes were then converted to Hedges’ g based on the formulas provided by Lipsey and Wilson (2001). The weighted mean estimate of the effect sizes was then calculated with Hedges’ g to demonstrate the overall effectiveness. A random-effects model was used to estimate summary effects in the current study. The random-effects model assumes that each effect size is correlated with the independent variables and is drawn from unique populations (Hedges and Vevea 1998). Because the studies using CBT may vary according to types of the interventions, settings and participant age ranges, etc., the true effect size may vary from study to study. The Q-statistic was used to test both the homogeneity of effect sizes and the possible impact of moderators on this meta-analysis (Hedges 1981). The statistical I2 was also used to demonstrate percentage heterogeneity within in the current study (Higgins and Thompson 2002). For visual demonstration of heterogeneity, forest plots were used (Moher et al. 2009). Because funnel plots of standard error versus standard differences in means may lead to false results, a comparison of the sample sizes by mean differences was used to determine publication bias (Hedges and Vevea 1998).
Results
The 23 studies generated 24 separate effect sizes ranging between g = − 3.4 and − 0.04. The overall weighted effect size of using of the CBTs for anxiety across the 24 effects sizes was moderate, g = − 0.66, 95% CI [− 0.88, − 0.44], z = − 5.83, p < .05, with significant heterogeneity, Q (22) = 62.49, p < .05, I2 = 62.2%. Effects sizes and confidence intervals across all of the studies at 95% CI are reported in Fig. 2. Figures 3 and 4 provide funnel plots of included studies with and without outliers. Visual inspection of the funnel plot identified Chalfant et al. (2006) as an outlier. Results continued to generate a moderate effect size after removing the outlier, g = − 0.56, 95% CI [− 0.71, − 0.42], z = − 7.81, p < .05 but altered the heterogeneity of the studies, Q (21) = 24.78, p = .31, I2 = 11.23%.
Descriptive Characteristics
Participant Characteristics
Table 1 provides an overview of the participant characteristics for the included studies. This meta-analysis included 23 studies with a total of 745 participants (268 controls and 477 treatment subjects). Participants ranged in age from 5 to 18 years old from a variety of locations and settings; a single study involved children younger than 7 years of age (Scarpa and Reyes 2011). Sample sizes varied from 6 to 79 participants. Twenty-two studies reported participant gender, and of these 615, were male (82.6%) and 124 female (17.4%). Of the studies that reported ASD subtype, 258 (43.4%) were diagnosed with Asperger’s syndrome, 179 (30.1%) with autism spectrum disorder, 143 (24.1%) with pervasive developmental disorders-not otherwise specified, and 14 (2.4%) with high-functioning ASD.
Treatment Components
Each study was coded for treatment components. The following types of CBT programs were used with or without adaptations: The Building Confidence program (Wood & McLeod 2008); the Coping Cat program (Kendall and Hedtke 2006); Discussing + Doing = Daring (Steensel & Bogels 2015); Exploring Feelings (Attwood 2004); Fighting Worry and Facing Fears (Reaven et al. 2005); Jr. Detective program (Beaumont and Sofronoff 2008); Multimodal Anxiety and Social Skills Intervention (MASSI; White et al. 2010a); The Cool Kids (Lyneham et al. 2003); The Behavioral Interventions for Anxiety in Children with Autism manual (BIACA: Wood et al. 2008); and Versions of CBT.
Design Characteristics
The design characteristics for each study were also coded. All studies utilized group design research. More specifically, eight studies were randomized controlled trials comparing CBTs to waitlist, four studies were randomized controlled trials comparing CBTs to usual care groups, and two studies were randomized controlled trials comparing CBTs to a delayed treatment group. Sung et al. (2011) compared the CBT intervention group to social, recreational intervention groups. Seven studies did not use control groups (Drmic et al. 2017; Ehrenreich-May et al. 2014; Maskey et al. 2014; Ooi et al. 2008; Sung et al. 2011; Thomson et al. 2015; Weiss et al. 2014).
Outcome Measures
All studies employed more than one direct measure of children’s anxiety and focused primarily or secondarily on decreasing children anxiety level. Although Scarpe and Reyes (2011) did not include any information related to the name of the measurements, the following standard anxiety measures were used by studies in the current analysis: the Anxiety Disorders Interview Schedule Clinical Severity Rating-Child and Parent Versions (n = 11; Silverman and Albano 1996), the Anxious Self-Statements Questionnaire (n = 1; Kendall and Hollon 1989), the Child and Adolescent Symptom inventory-4 Anxiety Scale (n = 1; Sukhodolsky et al. 2007), the Clinical Global Impression-Severity scale (n = 4; Guy 1976), the Multidimensional Anxiety Scale for Children- Child and Parent Versions (n = 5; March 1997), the Pediatric Anxiety Scale for Children (n = 5; Research Units of Pediatric Psychopharmacology Autism Network 2002), the Revised Children’s Anxiety and Depression Scale-Total Anxiety (n = 3; Chorpita et al. 2000), the Revised Children’s Manifest Anxiety Scale (n = 2; Reynolds and Richmond 1978), the Screen for Child Anxiety Related Disorders (n = 3; Birmaher et al. 1997), the Spence Children’s Anxiety Scale-child and parent versions (n = 16; Spence 1998), the School Anxiety Scale (n = 1; Lyneham et al. 2008).
Potential Moderators
Potential moderators of interest in this study include length of intervention and parental involvement. They were analyzed to address the second purpose of this meta-analysis.
Length of Intervention
The short-term intervention category included eight studies using a CBT protocol less than 12 weeks. Five studies used a CBT protocol of 12 weeks, one additional study was 14-weeks (White et al. 2012) but was categorized as a standard-term intervention category. Finally, the long-term intervention category comprised ten studies with a protocol equal to or greater than16 weeks.
Short-term interventions had smaller effects sizes, g = − 0.37, 95% CI [− 0.60, − 0.14], z = − 3.14, p < .05, than standard-term interventions, g = − 1.02, 95% CI [− 1.67, − 0.37], z = − 3.07, p < .05, or long-term intervention, g = − 0.69, 95% CI [− 0.98, − 0.41], z = − 4.74, p < .05. Removing the outlier did not impact significant differences across categories of short-term intervention, g = − 0.37, 95% CI [− 0.60, − 0.14], z = − 3.14, p < .05, standard-term intervention, g = − 0.67, 95% CI [− 0.91, − 0.44], z = − 5.73, p < .05, and long-term intervention, g = − 0.69, 95% CI [− 0.98, − 0.41], z = − 4.74, p < .05. There was significant heterogeneity between groups, QB (2) = 8.70, p < .05, and within the groups, QW (21) = 53.79, p < .05. Removing the outlier did not significantly alter group heterogeneity, QB (2) = 4.44, p < .05, but it caused significant changes with respect to within group heterogeneity, QW (20) = 20.34, p = .44. See Fig. 5 for the forest plot of effects size by types of programs.
Forest plot of studies included in the meta-analysis by types of involvement. A horizontal line represents the 95% confidence intervals of the each study. Black box represents the effect size of the study. The first two diamonds represent the overall effects across moderator groups. The bottom diamond represents the overall effects across 23 studies. ES effects size, LL lower limit, UL upper limit
Parent Involvement
Two groups were created based on parental involvement: studies with parental involvement (n = 15), and studies without parental involvement (n = 9). Treatments that had parental involvement resulted in a larger overall effect size, g = − 0.85, 95% CI [− 1.16, − 0.54], z = − 5.34, p < .05 than treatments without parental involvement, g = − 0.34, 95% CI [− 0.57, − 0.12], z = − 2.99, p < .05. Removing the outlier (Chalfant et al. 2006) did not significantly change these results. Figure 6 depicts a forest plot of effects size by types of implementer.
Forest plot of studies included in the meta-analysis by length of the intervention. A horizontal line represents the 95% confidence intervals of the each study. Black box represents the effect size of the study. The first three diamonds represent the overall effects across moderator groups. The bottom diamond represents the overall effects across 23 studies. ES effects size, LL lower limit, UL upper limit
Discussion
This meta-analysis reviewed the effects of programs that used CBT on anxiety related outcomes for children with high-functioning ASD across 23 studies. Previous meta-analyses (Sukhodolsky et al. 2013; Ung et al. 2014), assessing work through 2018, included a limited number of studies and did not assess length of treatment or parental involvement as potential moderators. This meta-analysis was the first to examine the potential impact of these two variables. Findings suggest that CBT treatments produced moderate changes in the level of anxiety in children with ASD. Weighted effect sizes with or without the outlier (Chalfant et al. 2006) were within the moderator range (g = 0.5–0.8; Cohen 1981). As such, it appears that CBT may be beneficial for high-functioning children with ASD in managing their thoughts and emotions; primary findings are consistent with the results of previous meta-analyses (Sukhodolsky et al. 2013; Ung et al. 2014).
All studies from two previous meta-analyses were included and examined through this meta-analysis. (See Table 2). Sukhodolsky et al. (2013) found the largest effects sizes across clinical, parent and child reports with eight studies. Ung et al. (2014) also found a statistically significant moderate effect size with 14 studies involving 511 youth. The results of current study also yielded moderate effects, but smaller than previous two meta-analyses, in 23 studies involving 745 youth (See Table 2). In comparison, Hofmann et al. (2012) reviewed 48 studies of CBT treatment for anxiety disorders, and found consistently strong effects sizes for the use of CBT in treating anxiety disorders among typically developing children. The finding that effects for typically developing children were larger than for those with ASD. This particular result may indicate that children with ASD may not respond as well to CBT as their peers. As such, additional types of individualization may be needed in order for children with ASD to fully benefit from treatment (Keefer et al. 2017).
The two previous meta-analyses reported significant heterogeneity in effects sizes. Because Chalfant et al. (2006) had large effect sizes with their large sample sizes; this study had greater weight in the calculation of the Q-statistics to determine heterogeneity of the effect sizes. As a result, with limited studies, it is possible that Q-statistics led to errors in determining heterogeneity of the effect sizes either with or without an outlier. For instance, heterogeneity that included the outlier (Chalfant et al. 2006) found significant dispersion across the effect sizes. This finding suggested that dispersion across the effect sizes is not due to random errors and, there are significant differences across the studies. The heterogeneity within the current studies may support Kerns and her colleagues’ hypotheses related to atypical anxiety symptoms in children with ASD.
Recently, studies have examined factors associated with the wide range of effects reported. For example, Boulter at al. (2014) and Wigham et al. (2015) found intolerance of uncertainty in ASD to be greater than in typically anxious children. Furthermore, Keefer et al. (2017) examined the effects of intolerance of uncertainty on anxiety outcomes following modified CBT. They found that intolerance of uncertainty was correlated with high levels of anxiety and worry post-intervention. More studies are needed to determine specific symptoms of anxiety in children with ASD (Kerns et al. 2014). If this atypical presentation is shown to be a common phenomenon in ASD, then the components of CBT treatment may need to be developed or modified based on these specific atypical symptoms in order to address the unique aspects and needs of anxiety in children with ASD.
Moderator analysis of parental involvement demonstrated that children benefited most from CBTs when parents were involved in the intervention. This finding points to the impact of parental involvement on the efficacy of CBT for treatment of anxiety in this population. The interventions with parental involvement resulted in a large treatment effect size, while the treatment with the child only yielded a small effect size. After removing Chalfant et al. (2006), the results of the homogeneity test were also consistent with this observation. The results revealed a substantial variation between studies with and without parental involvement. Treatment effects in the studies were greater with parental involvement than without. This finding provides some support for the hypothesis that family participation plays a significant role in the efficacy of CBT in this group. Several of the studies reviewed demonstrated a beneficial relationship between parental involvement and effectiveness of CBT (Chalfant et al. 2006; Sofronoff et al. 2005; Weiss et al. 2014). Moreover, several recent studies have shown that parents of children with ASD are likely to have higher levels of stress and lower levels of educational opportunities to decrease parental stress while improving parental behaviors for children with ASD (Hassall et al. 2005). Although the findings are not conclusive, they show the importance of further research to consider the potential impact of parental involvement on the effects of CBT.
The results also presented some differences based on intervention length. For instance, some studies (e.g., Clarke et al. 2016; Luxford et al. 2016) included only a few 1-h sessions to work with children in developing cognitive skills within the short-term intervention format. As a result, treatment effects associated with short-term interventions were significantly weaker than those obtained in standard-term and long-term interventions. Clarke et al. (2016) mentioned that the main reason for these differences may be that using cognitive skills takes time for children with ASD. Likewise, children may need extended time to understand and apply newly learned cognitive strategies for coping with their feelings. Some studies have also aimed to increase the efficacy of interventions in a short period of time (e.g., one week) by extending the contact time with clients. McConachie et al. (2013) increased the length of sessions up to two-hours to maximize contact time while they decreased weekly sessions to four weeks. The results of the study, suggest that extended time rather than more contact time is required to learn and administer cognitive strategies implemented. It is thus likely that children need extended time rather than more contact time to learn and administer cognitive strategies for coping with their anxieties. One unexpected finding from this particular moderator analysis is that no statistically significance difference in intervention effect sizes between standard-term and long-term interventions was obtained. Only Fujii et al. (2012) had a larger effect than the other studies. It is possible that Fujii et al. (2012) were more effective because this study administrated a 32-week intervention, which was a significantly longer duration than other long-term interventions. Fujii et al. (2012) incorporated 16 weekly 90-min CBT sessions for a total of 32 sessions for developing cognitive skills to explore feelings and modify automatic thoughts with enough time, and found a significant impact on reducing the level of anxiety for participants.
Limitations and Future Research
Several limitations need to be taken into consideration in interpreting the findings of this meta-analysis. Most notable is the smaller number of studies identified for inclusion. This may cause variability in obtained weighted mean effect sizes, and affect the results of homogeneity testing. Because of the limited number of studies, the results of the heterogeneity test between or within the moderator groups could not be adequately analyzed. The paucity of information reported on participants was the second limitation. Previous studies have demonstrated that a strong relationship existed between parental stress and anxiety in children. Relatives can cause children to develop and maintain anxiety under some circumstances (Ginsburg and Schlossberg 2002; Rapee et al. 2001). A majority of the included studies failed to provide sufficient information related to family characteristics, such as level of parental anxiety or which parent was involved in the intervention (mother or father). Although parental involvement is generally found beneficial, the unexamined role of parental stress should be considered. Future studies should examine the impact of parental behaviors on CBT efficacy. The third limitation was the variation in CBT treatments. These variations need to be tested and shown to be effective and reliable in reducing anxiety symptoms in children with ASD.
In sum, children with high-functioning ASD are more likely to struggle with high levels of anxiety, and CBT for children with ASD is an emerging treatment option in the literature to date. This meta-analysis explored the overall efficacy of CBT treatments on anxiety levels in children with ASD. The results suggest that CBTs have the potential to be an effective component for addressing anxiety-related symptoms for children with ASD. Moreover, the results of the moderator analyses demonstrated the importance of treatment length and parental involvement. The evidence to date is broadly supportive of the approach although more research is needed to better tailor and adapt CBT to meet the unique needs of individuals with ASD. Future research is also needed to evaluate CBTs in order to address atypical anxiety symptoms that were associated more with ASD. These symptoms (such as novelty and restricted interests, unusual specific fear; Kerns et al. 2014) do not reflect the traditional anxiety disorders. Thus, future studies are need to identify atypical anxiety symptoms more clearly and comprehensively to evaluate the efficacy of cognitive behavioral treatments for both traditional and atypical anxiety symptoms.
References
*References marked with an asterisk indicate studies included in the meta-analysis
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th edn.). Washington, DC: Author.
Attwood, T. (2004). Exploring feelings: Cognitive behavioural therapy to manage anxiety. Arlington: Future Horizons.
Barrett, P. M., Dadds, M. R., & Rapee, R. M. (1996). Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology, 64(2), 333–342. https://doi.org/10.1037/0022-006x.64.2.333.
Bauminger, N. (2002). The facilitation of social-emotional understanding and social interaction in high-functioning children with autism: Intervention outcomes. Journal of autism and developmental disorders, 32(4), 283–298.
Beaumont, R., & Sofronoff, K. (2008). A multi-component social skills intervention for children with Asperger syndrome: The Junior Detective Training Program. Journal of Child Psychology and Psychiatry, 49(7), 743–753.
Beck, A. T. (1976). Cognitive therapy and the emotional disorders. New York: International Universities Press.
Birmaher, B., Khetarpal, S., Brent, D., Cully, M., Balach, L., Kaufman, J., & Neer, S. M. (1997). The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child & Adolescent Psychiatry, 36(4), 545–553. https://doi.org/10.1097/00004583-199704000-00018.
Boulter, C., Freeston, M., South, M., & Rodgers, J. (2014). Intolerance of uncertainty as a framework for understanding anxiety in children and adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44(6), 1391–1402.
Centers for Disease Control and Prevention. (2018, April 26). Retrieved October 17, 2017, from https://www.cdc.gov/.
*Chalfant, A. M., Rapee, R., & Carroll, L. (2006). Treating anxiety disorders in children with high functioning autism spectrum disorders: A controlled trial. Journal of Autism and Developmental Disorders, 37(10), 1842–1857. https://doi.org/10.1007/s10803-006-0318-4.
Chorpita, B. F. (2007). Modular cognitive-behavioral therapy for childhood anxiety disorders. New York: Guilford Press.
Chorpita, B. F., Yim, L. M., Moffitt, C. E., Umemoto, L. A., & Francis, S. E. (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A Revised Child Anxiety and Depression Scale. Behaviour Research and Therapy, 38, 835–855. https://doi.org/10.1016/S0005-7967(99)00130-8.
Clark, D. B., Smith, M. G., Neighbors, B. D., Skerlec, L. M., & Randall, J. (1994). Anxiety disorders in adolescence: Characteristics, prevalence, and comorbidities. Clinical Psychology Review, 14(2), 113–137. https://doi.org/10.1016/0272-7358(94)90012-4.
*Clarke, C., Hill, V., & Charman, T. (2016). School based cognitive behavioural therapy targeting anxiety in children with autistic spectrum disorder: a quasi-experimental randomised controlled trail incorporating a mixed methods approach. Journal of Autism and Developmental Disorders, 47(12), 3883–3895. https://doi.org/10.1007/s10803-016-2801-x.
Cohen, J. (1969). Statistical power analysis for the behavioral sciences. New York: Academic Press.
Cook, B., Buysse, V., Klingner, J., Landrum, T., McWilliam, R., Tankersley, M., & Test, D. (2014). Council for Exceptional Children: Standards for evidence-based practices in special education. Teaching Exceptional Children, 46(6), 206.
*Drmic, I. E., Aljunied, M., & Reaven, J. (2017). Feasibility, acceptability and preliminary treatment outcomes in a school-based CBT intervention program for adolescents with ASD and anxiety in Singapore. Journal of Autism and Developmental Disorders, 47(12), 3909–3929.
*Ehrenreich-May, J., Storch, E. A., Queen, A. H., Rodriguez, J. H., Ghilain, C. S., Alessandri, M.,.. . Wood, J. J. (2014). An open trial of cognitive-behavioral therapy for anxiety disorders in adolescents with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 29(3), 145–155. https://doi.org/10.1177/1088357614533381.
*Fujii, C., Renno, P., Mcleod, B. D., Lin, C. E., Decker, K., Zielinski, K., & Wood, J. J. (2012). Intensive cognitive behavioral therapy for anxiety disorders in school-aged children with autism: A Preliminary comparison with treatment-as-usual. School Mental Health, 5(1), 25–37. https://doi.org/10.1007/s12310-012-9090-0.
Ginsburg, G. S., & Schlossberg, M. C. (2002). Family-based treatment of childhood anxiety disorders. International Review of Psychiatry, 14(2), 143–154. https://doi.org/10.1080/09540260220132662.
Guy, W. (1976). ECDEU assessment manual for psychopharmacology. US Dept Health, Education, and Welfare publication; ADM No. 76–338 (pp. 218–222). Rockville: National Institute of Mental Health.
Hassall, R., Rose, J., & Mcdonald, J. (2005). Parenting stress in mothers of children with an intellectual disability: the effects of parental cognitions in relation to child characteristics and family support. Journal of Intellectual Disability Research, 49(6), 405–418. https://doi.org/10.1111/j.1365-2788.2005.00673.x.
Hedges, L. V. (1981). Distribution theory for glass estimator of effect size and related estimators. Journal of Educational and Behavioral Statistics, 6(2), 107–128. https://doi.org/10.3102/10769986006002107.
Hedges, L. V., & Vevea, J. L. (1998). Fixed- and random-effects models in meta-analysis. Psychological Methods, 3(4), 486–504. https://doi.org/10.1037/1082-989x.3.4.486.
Higgins, J. P., & Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21(11), 1539–1558. https://doi.org/10.1002/sim.1186.
Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36(5), 427–440.
House, A. E., House, B. J., & Campbell, M. B. (1981). Measures of interobserver agreement: Calculation formulas and distribution effects. Journal of Behavioral Assessment, 3(1), 37–57. https://doi.org/10.1007/bf01321350.
Keefer, A., Kreiser, N. L., Singh, V., Blakeley-Smith, A., Duncan, A., Johnson, C., … Vasa, R. A. (2017). Intolerance of uncertainty predicts anxiety outcomes following CBT in youth with ASD. Journal of Autism and Developmental Disorders, 47(12), 3949–3958.
*Keehn, R. H., Lincoln, A. J., Brown, M. Z., & Chavira, D. A. (2012). The coping cat program for children with anxiety and autism spectrum disorder: A pilot randomized controlled trial. Journal of Autism and Developmental Disorders, 43(1), 57–67. https://doi.org/10.1007/s10803-012-1541-9.
Kendall, P. C. (1993). Cognitive-behavioral therapies with youth: Guiding theory, current status, and emerging developments. Journal of Consulting and Clinical Psychology, 61(2), 235–247. https://doi.org/10.1037//0022-006x.61.2.235.
Kendall, P. C., & Hedtke, K. (2006). Cognitive-behavioral therapy for anxious children: Therapist manual (3rd edn.). Ardmore: Workbook Publishing.
Kendall, P. C., & Hollon, S. D. (1989). Anxious self-talk: development of the anxious self-statements questionnaire (ASSQ). Cognitive Therapy and Research, 13, 81–93.
Kendall, P. C., & Kriss, M. R. (1983). Cognitive-behavioral interventions. In C. E. Walker (Ed.), The handbook of clinical psychology: theory, research and practice (pp. 770–819). Homewood: Dow Jones-Irwin.
Kerns, C. M., Kendall, P. C., Berry, L., Souders, M. C., Franklin, M. E., Schultz, R. T., … Herrington, J. (2014). Traditional and atypical presentations of anxiety in youth with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44(11), 2851–2861.
Kim, Y. S., Leventhal, B. L., Koh, Y. J., Fombonne, E., Laska, E., Lim, E. C., … Grinker, R. R. (2011). Prevalence of autism spectrum disorders in a total population sample. American Journal of Psychiatry, 168(9), 904–912. https://doi.org/10.1176/appi.ajp.2011.10101532.
Lipsey, M. W., & Wilson, D. B. (2001). Practical meta-analysis. Thousand Oaks: Sage.
*Luxford, S., Hadwin, J. A., & Kovshoff, H. (2016). Evaluating the effectiveness of a school-based cognitive behavioural therapy intervention for anxiety in adolescents diagnosed with autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(12), 3896–3908. https://doi.org/10.1007/s10803-016-2857-7.
Lyneham, H. J., Abbott, M. J., Wignall, A., & Rapee, R. M. (2003). The Cool Kids Family Program—Therapist Manual. Sydney: Macquarie University.
Lyneham, H. J., Street, A. K., Abbott, M. J., & Rapee, R. M. (2008). Psychometric properties of the school anxiety scale—Teacher reported (SAS-TR). Journal of Anxiety Disorders, 22(2), 292–300. https://doi.org/10.1016/j.janxdis.2007.02.001.
March, J. S. (1997). Multidimensional anxiety scale for children. North Tonawanda: Multi-Health Systems.
*Maskey, M., Lowry, J., Rodgers, J., McConachie, H., & Parr, J. R. (2014). Reducing specific phobia/fear in young people with autism spectrum disorders (ASDs) through a virtual reality environment intervention. PloS One, 9(7), e100374.
*Mcconachie, H., Mclaughlin, E., Grahame, V., Taylor, H., Honey, E., Tavernor, L.,.. . Couteur, A. L. (2013). Group therapy for anxiety in children with autism spectrum disorder. Autism, 18(6), 723–732. https://doi.org/10.1177/1362361313488839.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269.
*Ooi, Y. P., Lam, C. M., Sung, M., Tan, W. T. S., Goh, T. J., Fung, D. S. S., … Chua, A. (2008). Effects of cognitive-behavioural therapy on anxiety for children with high-functioning autistic spectrum disorders. Singapore Medical Journal, 49(3), 215.
*Reaven, J., Blakeley-Smith, A., Culhane-Shelburne, K., & Hepburn, S. (2011). Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: A randomized trial. Journal of Child Psychology and Psychiatry, 53(4), 410–419. https://doi.org/10.1111/j.1469-7610.2011.02486.x.
Reaven, J., Hepburn, S., Nichols, S., Blakely-Smith, A., & Dasari, M. (2005). Coping group: Fighting worry and facing fears: an unpublished treatment manual for children with ASD and anxiety disorder. Denver: University of Colorado at Denver and Health Sciences Center.
*Reaven, J. A., Blakeley-Smith, A., Nichols, S., Dasari, M., Flanigan, E., & Hepburn, S. (2008). Cognitive-behavioral group treatment for anxiety symptoms in children with high-functioning autism spectrum disorders. Focus on Autism and Other Developmental Disabilities, 24(1), 27–37. https://doi.org/10.1177/1088357608327666.
Research Units on Pediatric Psychopharmacology Autism Network. (2002). Risperidone in children with autism and serious behavioral problems. New England Journal of Medicine, 347, 314–321.
Reynolds, C. R., & Richmond, B. O. (1978). What I think and feel: A revised measure of child’s manifest anxiety. Journal of Abnormal Child Psychology, 6(2), 271–280. https://doi.org/10.1007/bf00919131.
*Scarpa, A., & Reyes, N. M. (2011). Improving emotion regulation with CBT in young children with high functioning autism spectrum disorders: A pilot study. Behavioural and Cognitive Psychotherapy, 39(04), 495–500. https://doi.org/10.1017/s1352465811000063.
Silverman, W. K., & Albano, A. M. (1996). The anxiety disorders interview schedule for DSM IV-Child and parent versions. SanAntonio: Graywind.
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of Child & Adolescent Psychiatry, 47(8), 921–929. https://doi.org/10.1097/chi.0b013e318179964f.
*Sofronoff, K., Attwood, T., & Hinton, S. (2005). A randomised controlled trial of a CBT intervention for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry, 46(11), 1152–1160. https://doi.org/10.1111/j.1469-7610.2005.00411.x.
Spence, S. H. (1998). A measure of anxiety symptoms among children. Behaviour Research and Therapy, 36(5), 545–566. https://doi.org/10.1016/s0005-7967(98)00034-5.
*Steensel, F. J., & Bögels, S. M. (2015). Cbt for anxiety disorders in children with and without autism spectrum disorders. Journal of Consulting and Clinical Psychology, 83(3), 512–523. https://doi.org/10.1037/a0039108.
Steensel, F. J., Bögels, S. M., & Perrin, S. (2011). Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clinical Child and Family Psychology Review, 14(3), 302.
*Storch, E. A., Arnold, E. B., Lewin, A. B., Nadeau, J. M., Jones, A. M., Nadai, A. S.,.. . Murphy, T. K. (2013). The effect of cognitive-behavioral therapy versus treatment as usual for anxiety in children with autism spectrum disorders: A randomized, controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 52(2). https://doi.org/10.1016/j.jaac.2012.11.007.
*Storch, E. A., Lewin, A. B., Collier, A. B., Arnold, E., Nadai, A. S., Dane, B. F.,.. . Murphy, T. K. (2014). A randomized controlled trial of cognitive-behavioral therapy versus treatment as usual for adolescents with autism spectrum disorders and comorbid anxiety. Depression and Anxiety, 32(3), 174–181. https://doi.org/10.1002/da.22332.
Sukhodolsky, D. G., Bloch, M. H., Panza, K. E., & Reichow, B. (2013). Cognitive-behavioral therapy for anxiety in children with high-functioning autism: A Meta-analysis. Pediatrics, 132(5). https://doi.org/10.1542/peds.2013-1193.
Sukhodolsky, D. G., Scahill, L., Gadow, K. D., Arnold, L. E., Aman, M. G., Mcdougle, C. J.,.. . Vitiello, B. (2007). Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. Journal of Abnormal Child Psychology, 36(1), 117–128. https://doi.org/10.1007/s10802-007-9165-9.
*Sung, M., Ooi, Y. P., Goh, T. J., Pathy, P., Fung, D. S., Ang, R. P.,.. . Lam, C. M. (2011). Effects of cognitive-behavioral therapy on anxiety in children with autism spectrum disorders: A randomized controlled trial. Child Psychiatry & Human Development, 42(6), 634–649. https://doi.org/10.1007/s10578-011-0238-1.
*Thomson, K., Riosa, P. B., & Weiss, J. A. (2015). Brief report of preliminary outcomes of an emotion regulation intervention for children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(11), 3487–3495. https://doi.org/10.1007/s10803-015-2446-1.
Ung, D., Selles, R., Small, B. J., & Storch, E. A. (2014). A systematic review and meta-analysis of cognitive-behavioral therapy for anxiety in youth with high-functioning autism spectrum disorders. Child Psychiatry & Human Development, 46(4), 533–547. https://doi.org/10.1007/s10578-014-0494-y.
Warner, C. M., Warner, C. M., Fisher, P. H., & Klein, R. G. (2007). School-based behavioral intervention for social anxiety disorder in adolescents: Results of an attention control trial and implementation issues. PsycEXTRA Dataset. https://doi.org/10.1037/e533832007-001.
*Weiss, J. A., Viecili, M. A., & Bohr, Y. (2014). Parenting stress as a correlate of cognitive behavior therapy responsiveness in children with autism spectrum disorders and anxiety. Focus on Autism and Other Developmental Disabilities, 30(3), 154–164. https://doi.org/10.1177/1088357614547808.
White, S. W., Albano, A., Johnson, C., Kasari, C., Ollendick, T., Klin, A., et al. (2010a). Development of a cognitive-behavioral intervention program to treat anxiety and social deficits in teens with high-functioning autism. Clinical Child and Family Psychology Review, 13(1), 77–90. https://doi.org/10.1007/s10567-009-0062-3.
*White, S. W., Ollendick, T., Albano, A. M., Oswald, D., Johnson, C., Southam-Gerow, M. A.,.. . Scahill, L. (2012). Randomized controlled trial: multimodal anxiety and social skill intervention for adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 43(2), 382–394. https://doi.org/10.1007/s10803-012-1577-x.
Wigham, S., Rodgers, J., South, M., McConachie, H., & Freeston, M. (2015). The interplay between sensory processing abnormalities, intolerance of uncertainty, anxiety and restricted and repetitive behaviours in autism spectrum disorder. Journal of Autism and Developmental Disorders, 45(4), 943–952.
*Wood, J. J., Drahota, A., Sze, K., Har, K., Chiu, A., & Langer, D. A. (2009). Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of Child Psychology and Psychiatry, 50(3), 224–234. https://doi.org/10.1111/j.1469-7610.2008.01948.x.
*Wood, J. J., Ehrenreich-May, J., Alessandri, M., Fujii, C., Renno, P., Laugeson, E.,.. . Storch, E. A. (2015). Cognitive behavioral therapy for early adolescents with autism spectrum disorders and clinical anxiety: A randomized, controlled trial. Behavior Therapy, 46(1), 7–19. https://doi.org/10.1016/j.beth.2014.01.002.
Wood, J. J., McLeod, B. D., Hiruma, L. S., & Phan, A. Q. (2008). Child anxiety disorders: A family-based treatment manual for practitioners. New York: WW Norton & Co.
Funding
The authors received no financial support for the research and publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Perihan, C., Burke, M., Bowman-Perrott, L. et al. Effects of Cognitive Behavioral Therapy for Reducing Anxiety in Children with High Functioning ASD: A Systematic Review and Meta-Analysis. J Autism Dev Disord 50, 1958–1972 (2020). https://doi.org/10.1007/s10803-019-03949-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-019-03949-7