Abstract
A family-based, cognitive behavioural treatment for anxiety in 47 children with comorbid anxiety disorders and High Functioning Autism Spectrum Disorder (HFA) was evaluated. Treatment involved 12 weekly group sessions and was compared with a waiting list condition. Changes between pre- and post-treatment were examined using clinical interviews as well as child-, parent- and teacher-report measures. Following treatment, 71.4% of the treated participants no longer fulfilled diagnostic criteria for an anxiety disorder. Comparisons between the two conditions indicated significant reductions in anxiety symptoms as measured by self-report, parent report and teacher report. Discussion focuses on the implications for the use of cognitive behaviour therapy with HFA children, for theory of mind research and for further research on the treatment components.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is frequently noted that children with a High Functioning Autism Spectrum Disorder (HFA) experience anxiety, where HFA refers collectively to those children who have Autistic Disorder, without intellectual delay, together with those children who have Asperger’s Disorder (American Psychiatric Association, 1994). HFA children have been noted to experience anxiety across their school life, social life and family life (Coupland, 2001; Groden, Cautela, Prince, & Berryman, 1994; Kim, Szatmari, Bryson, Streiner, & Wilson, 2000; Muris, Steerneman, Merckelbach, Holdrinet, & Meesters, 1998; Tonge, Brereton, Gray, & Einfeld, 1999). In fact, anxiety related difficulties are so frequently exhibited in children with Autism Spectrum Disorders (ASDs) that DSM-IV highlights anxiety-like responses as a common, “associated feature” of autism stating that, “there may be excessive fearfulness in response to harmless objects” (American Psychiatric Association, 1994, p. 68).
Prevalence rates of anxiety symptomatology in children with HFA support the argument that anxiety is a core difficulty of many children who suffer with HFA. Several small studies have reported the prevalence of anxiety disorders in ASD children to be between 47 and 84.1% (Gillot, Furniss, & Walter, 2001; Muris et al., 1998; Rumsey, Rapoport, & Sceery, 1985). For example, a study by Muris et al. (1998) found that of 44 children with HFA and families interviewed, 84.1% of the children met DSM-IV criteria for at least one anxiety disorder. Furthermore, within the anxious group, 63.6% met DSM-IV criteria for a specific phobia (SpP) (Muris et al., 1998). More recently, Gillot et al. (2001) found that from a sample of 15 children with high-functioning autism, 47% presented with clinically significant levels of anxiety based on self-report anxiety scales.
Not only is anxiety a frequent difficulty for children with HFA, but also, there is evidence to suggest that anxiety difficulties occur more frequently in ASD children than in other paediatric populations such as children with severe mental retardation and/or epilepsy (Steffenburg, Gillberg, & Steffenburg, 1996) and children who have a language disorder (Gillot et al., 2001).
Similarly children with an ASD have also been found to experience higher rates of anxiety than normally developing children (Achenbach, 1985; Benjamin, Costello, & Warren, 1990; Bird, 1996; Gillot et al., 2001; Matson & Love, 1990). For example, the rates of anxiety symptomatology reported for children with an ASD, i.e. 47–84.1%, are markedly higher than the lifetime prevalence rates reported for typically developing children in DSM-IV [1.5–3.5% Panic Disorder (PD), 3–13% Social Phobia (SP), 3% Generalised Anxiety Disorder (GAD), 11% SpPs; American Psychiatric Association, 1994] or other large epidemiological studies (1% for SP, 1–3.6% for GAD; Bernstein, Costello, & Warren, 1990; Bowen, Offord, & Boyle, 1990; Clark, Smith, Neighbors, Skerlec, & Randall, 1994; Costello et al., 1988; Craske, 1997; Kashani & Ovraschel, 1988, 1990; Kendall, Krain, & Treadwell, 1999). Anxiety prevalence rates are also higher in ASD children than in typically developing children who suffer with chronic medical conditions such as asthma (35%) (Vila, Nollet-Clemencon, de Blic, Mouren-Simeoni, & Scheinmann, 2000).
Despite the strong evidence that anxiety difficulties occur commonly in children with HFA, resulting in marked distress to their families, little research has explored effective treatment options for the anxiety related difficulties of ASD children. Indeed, a review of both the psychological and medical literature between reveals the use of only two forms of intervention to address anxiety in ASD children: psychoanalytic therapy and pharmacotherapy.
In general, psychoanalytic treatments have focused on therapist techniques such as exploring the clients “separation anxiety” from the analyst, exploring anxiety relating to a disturbance in the primary bond between the client and the mother and exploring the client’s “body anxiety” in order to help the client address the physiological component of their anxiety response (Braconnier, 1983; Heinemann, 1999; Schteingart, 1989). However, several methodological and theoretical limitations exist within the psychoanalytic treatments of anxious ASD individuals including small sample sizes (e.g. n = 1) and a lack of quantitative outcome information.
Evidence for the use of medication in the treatment of anxiety in children with an ASD, also seems to be limited. Studies have explored medication regimes for their ability to address the associated features of anxious ASD individuals rather than to specifically target primary anxiety difficulties (Brodkin, McDougle, Naylor, Cohen, & Price, 1997; Kalus et al., 1991; McDougle et al., 1992; Nicolson, Awad, & Sloman, 1998; Tsai, 1999). A further limitation is that most pharmacological investigations have only involved adult participants with Autistic Disorder. Moreover, the effects of medication only appear to last as long as the medication is being consumed with relapse occurring once the medication regime is ceased (Tsai, 1999).
The limitations of the abovementioned interventions for ASD children indicate that researchers need to explore whether other forms of anxiety treatment might be more appropriate for the anxious, ASD population. In particular, it might be important to consider other psychotherapeutic interventions that target the underlying cognitions and behaviours that maintain the ASD individual’s anxiety, for example, cognitive behaviour therapy (CBT).
It has been suggested recently that evidence for the efficacy of CBT in treating childhood anxiety disorders is now strong enough to warrant CBT being considered as a “Probably Efficacious” treatment in accordance with the criteria for “Empirically Supported Treatment” set out by the American Psychological Association’s “Committee on Science and Practice” (Chambless & Hollon, 1998). Specifically, the findings for the use of CBT in treating anxiety disorders in children are considered exemplary in five ways (for recent reviews of the efficacy of CBT in treating anxious children see Albano, Chorpita, & Barlow, 2003; Albano & Kendall, 2002; Alfano, Beidel, & Turner, 2002; Compton, Burns, Egger, & Robertson, 2002; Kashdan & Herbert, 2001; Ollendick & King, 1998; Weisz, Weiss, Han, Granger, & Morton, 1995). First, research has included cases serious enough to warrant formal diagnosis of an anxiety disorder and has employed standardised assessment tools in determining these diagnoses (Barrett, Dadds, & Rapee, 1996; Kendall, 1994; Kendall et al., 1997). Second, randomised control trials have indicated clinical significance of CBT treatments compared with waiting list (WL) control conditions (e.g. Barrett et al., 1996; Kendall, 1994; Kendall et al., 1997; Rapee, 2000; Silverman et al., 1999a, b). For example, Kendall (1994) found that the majority of the 47 children assigned to the treatment condition with an anxiety disorder diagnosis no longer met criteria for an anxiety disorder post-treatment. Moreover, a significant group by time interaction was found with 64% of the treatment group no longer meeting anxiety disorder criteria compared to 5% (one client) in the WL control group. Third, research has indicated that the post-treatment reductions attained from CBT programs have been maintained over long, post-treatment follow-up periods (Barrett, Duffy, Dadds, & Rapee, 2001; Barrett, Rapee, Dadds, & Ryan, 1996; Kendall, Safford, Flannery-Schroeder, & Webb, 2004). Specifically, several recent long-term follow-up studies revealed that CBT treatment gains were maintained as long as 6 years after treatment (Barrett et al., 2001) or 7 years after treatment (Kendall et al., 2004). Fourth, the superiority of CBT as a treatment for anxiety in children has been demonstrated by independent research groups in at least two different countries: the USA (Kendall et al., 1997) and Australia (Barrett et al., 1996). Fifth, most of the CBT programs evaluated have employed treatment manuals and, therefore, have maintained treatment integrity.
Not only has CBT been shown to be effective in treating anxiety symptoms in children, but also, more recently, CBT has been found to be effective in preventing the development of anxiety symptoms in children (see Barrett & Turner, 2004 for a review). For example, Barrett and Turner (2001) developed a 12-session CBT intervention called the “Friends for Children” program that could be incorporated into classroom curriculum as a means of preventing anxiety. They (2001) assessed the efficacy of the preventative intervention using a sample of 489 primary school aged children. The intervention was found to reduce the report of anxiety symptoms (Barrett & Turner, 2001).
Although, CBT has widely demonstrated efficacy among typically developing, anxious children (without intellectual delay), there is no published literature regarding the direct relevance of CBT models to children with an ASD who have age appropriate intellectual functioning. When employed, CBT-like strategies tend to be used indirectly by focusing on the parents. They are used either to teach the parents how to manage their own stress and, in turn, cope more effectively with their child’s anxious behaviours (Verheij & Van Loon, 1993; Wolf, Noh, Fisman, & Speechly, 1989) or to teach the parents anxiety-reducing skills so that they can re-teach the skills to their child, thereby becoming their child’s own therapist (Verheij & Van Loon, 1993). There are documented benefits for including parents in anxiety interventions for children (Mendlowitz et al., 1999; Shortt, Barrett, & Fox, 2001). However, failure to include the child as a direct participant in the intervention might not only hinder the child’s ability to become independently aware of their anxiety difficulties but also, the child’s ability to independently manage their anxiety difficulties (Jackson, 1983; Piacentini & Bergman, 2001).
The paucity of research into CBT as a potential model for treating anxiety in HFA children may be, in part, due to suggestions from research that all children with an ASD have difficulty in identifying emotions and cognitions both in themselves and in others, otherwise known as “Theory of Mind (ToM)” impairment (Baron-Cohen, 2001; Baron-Cohen, Leslie, & Frith, 1985). Based on the ToM hypothesis outlined by Baron-Cohen et al. (1985), an anxious ASD child might not be considered an appropriate candidate for a CBT program because CBT relies on the child’s ability to infer their own emotional states and thoughts in order to shift their cognitive style and, in turn, their anxious behaviour (Beck, 1976; Kendall et al., 1999).
However, while early ToM research suggested ToM impairments to be specific to children with ASD and global across all ASD children (Happé, 1994a; Holroyd & Baron-Cohen, 1993; Kleinman, Marciano, & Ault, 2001), more recent literature has highlighted growing evidence that children with HFA are able to identify both their own and other’s thoughts (Bauminger & Kasari, 1999; Bowler, 1992; Buitelaar, van der Wees, Swaab-Barneveld, & van der Gaag, 1999; Dahlgren, Sandberg, & Hjelmquist, 2003; Dyck, Ferguson, & Shochet, 2001; Happé, 1995; Yirmiya, Erel, Shaked, & Solomonica-Levi, 1998). Given the new ToM findings, it may be plausible to suggest that psychotherapeutic interventions like CBT be explored as a potential treatment for anxious HFA children.
Furthermore, CBT might be appropriate for children with an ASD because of the similarities that seem to exist between their information processing style and that of typically developing anxious children. According to central coherence theory, children with an ASD are argued to be over-selective in their information processing style, focusing on small details rather than scanning the whole context in order to identify what is important to focus on (e.g. Frith, 1989; Happé, 1994a; Happé, Briskman, & Frith, 2001; Morgan, Maybery, & Durkin, 2003; Wing, 1976, 1997). Similarly, typically developing anxious children are argued to have an information processing bias whereby they selectively attend to threat related information resulting in the misinterpretation of ambiguous situations as threatening because of a failure to consider the global context (e.g. Daleiden & Vasey, 1997; Kendall, 1985; Kendall & Ronan, 1990).
The information processing difficulties of both ASD and typically developing anxious children have both been argued to be best addressed by structured cognitive retraining exercises (Frith, 1989; Happé, 1994b; Kendall & Ronan, 1990). It is noteworthy that the structured retraining exercises sound particularly similar to the process that occurs within the cognitive therapy component of a CBT program.
There is now evidence to suggest that anxious HFA children might easily be able to engage in the abovementioned cognitive tasks (Beebe & Risi, 2003; Chalfant, 2004; Chalfant, Franklin, & Rapee, 2004; Lord, 1996). In a recent study, Chalfant et al. (2004) demonstrated that 20 anxious HFA children were as able to identify their anxious thoughts as 600 anxious non-ASD children when asked to complete the Children’s Automatic Thoughts Scale (CATS; Schniering & Rapee, 2002). For example, HFA children who presented with social anxiety selectively endorsed thoughts relating to social anxiety more than any other types of thoughts on the CATS (Chalfant et al., 2004). In other words, anxious HFA children were shown to be able to identify thoughts that reflect their emotional state, one of the main requirements for suitability for a CBT intervention (Chalfant et al., 2004). Consequently, it seems possible that the cognitive components normally associated with CBT anxiety programs would not only suit the learning style of HFA anxious children, but also, these children would be likely to complete the structured cognitive exercises of a manualised CBT program as well as their typically developing anxious peers.
Given the efficacy of manualised CBT interventions and the findings suggesting that HFA children might be appropriate candidates for a CBT intervention, it seems that treatment outcome research using manualised CBT with anxious HFA children could be a sensible starting point in renewing the search for effective anxiety treatments for ASD children. Therefore, the current study is the first clinical trial investigating the effectiveness of CBT for HFA children who have a comorbid anxiety disorder. It was hypothesised that the active treatment condition would produce significantly greater change in the dependent variables than the WL control condition.
Methods
Participants
Forty-seven children aged 8–13 years (35 boys, 12 girls) with a mean age of 10.8 years (SD = 1.35) participated in the treatment study. Children were recruited through referrals from community health centres, mental health professionals, medical practitioners and parents who referred their child after media releases in the Autism Association of NSW (AANSW) quarterly magazine. As a result of the logistics of using a clinical setting rather than a research clinic, four treatment groups were conducted with recruitment for each group occurring for 2 months, and commencing 3 months before the program began. Participants were randomly assigned before each treatment group began to either the CBT (n = 28) or WL condition (n = 19; offered treatment after the WL period, which was approximately 7 months duration). Therefore, the number of children allocated in each group varied according to the number of families that were recruited ahead of any one of the four treatment groups. Treatment occurred in groups of 6–8 children.
In terms of diagnosis of an ASD, 13 (27.7%) of the participants had a documented diagnosis of High Functioning Autistic Disorder and 34 (72.3%) had a documented diagnosis of Asperger’s Disorder. All participants had been diagnosed by a paediatrician, psychiatrist or clinical psychologist. Participants were not accepted into the program without accompanying documentation of their diagnosis. No criteria were set regarding “acceptable” screeners or other instruments for diagnosis of ASD from the outside clinicians. However, clinical observations by the investigators during the pre-treatment assessment process did confirm that the participant’s ASD diagnoses seemed accurate. Accompanying referral documentation from previous assessments by allied health professionals revealed that all of the participants had age appropriate language skills and ranged between borderline to very superior in their level of intellectual functioning.
Participants received a primary anxiety disorder diagnosis [i.e. Separation Anxiety Disorder (SAD), n = 8; GAD, n = 14; SP, n = 20; SpP, n = 3; and PD, n = 2] on the basis of structured clinical interviews conducted with the both the parent and the child using the “Anxiety Disorders Interview Schedule” (ADIS; Albano & Silverman, 1996). When parent and child reports differed, diagnosis was based on parental reports. It is noteworthy that the children selected to participate in the study met criteria for an anxiety disorder beyond their ASD related symptomatology. That is, all children participating in the current study presented with frequent, irrational fears and/or worries that impaired their daily functioning rather than rational concerns about their daily lives. For example, children who presented with frequent, irrational fears and avoidant behaviours, e.g. eating in front of family and peers, and avoiding evening meals with their family on a daily basis, gained entrance to the study. Alternatively, children who presented with rational concerns about being teased at school, when they were experiencing regular teasing at school because of their ASD, did not gain entrance to the study.
Twenty-six (55.3%) of the participants met criteria for two anxiety disorders and 9 (19.1%) met criteria for three anxiety disorders. The percentage frequencies of primary diagnoses of anxiety disorders, as determined using the child version of the “Anxiety Disorders Interview Schedule for DSM-IV” (ADIS-C/P) are represented for each condition in Table 1.
Thirteen (27.7%) of the children presented with a secondary diagnosis of comorbid ADHD. Children who had intellectual delay, physical disability, who were currently taking anti-anxiety or anti-depressant medication, who presented with marked externalising difficulties (e.g. Conduct Disorder or Oppositional Defiant Disorder) or whose parents were experiencing acute marital breakdown (were referred elsewhere) and not included in the study (n = 4).
Therapy was provided to the participants by two registered female clinical psychologists in the School Outreach Service of the AANSW. A third registered female psychologist conducted concurrent parent discussion sessions that were attended by a mix of single parents (both single mothers and single fathers) and parent couples.
Measures
As is recommended in the psychological literature (Kazdin, 1986; Kendall & Morris, 1991; Ollendick, 1986), multi-modal and multi-person assessment was used.
Structured Diagnostic Measures
The parent interview schedule of the child version of the “Anxiety Disorders Interview Schedule for DMS-IV” (ADIS-C/P) (Albano & Silverman, 1996) was conducted with the child and the parents at AANSW. The ADIS is a structured interview schedule that is consistent with the DSM-IV criteria for diagnosis of childhood anxiety disorders and has sound reliability (Silverman, Saavedra, & Pina, 2001). Use of the schedule allowed the clinicians to determine whether or not the participant’s anxiety related difficulties might be severe enough to warrant a diagnosis of an anxiety disorder, beyond their autism related difficulties and helped screen out other disorders.
Self-report Measures
Revised Children’s Manifest Anxiety Scale
The Revised Children’s Manifest Anxiety Scale (RCMAS) measures the child’s chronic anxiety (trait). The scale consists of 37 items (to which the individual responds “Yes” or “No”) (Reynolds & Richmond, 1978). The scale produces three anxiety factors: Physiological Symptoms (e.g. “Often I feel sick in my stomach”), Worry and Oversensitivity (e.g. “I worry when I go to bed at night”) and Social Concerns/Concentration (e.g. “I feel that others do not like the way I do things”) and have demonstrated validity and reliability (Reynolds & Richmond, 1978). Nine items in the scale compose a Lie Scale (e.g. “I always have good manners”).
Spence Children’s Anxiety Scale
The Spence Children’s Anxiety Scale (SCAS) consists of 44 items of which 38 address specific symptoms of anxiety and 6 are positive, filler items used to reduce the chances of a negative response bias, e.g. “I am proud of my school work” (Spence, 1998). It evaluates symptoms according to six subscales that measure separation anxiety (e.g. “I would feel afraid of being on my own at home”), SP (e.g. “I feel afraid if I have to talk in front of my class”), obsessive-compulsive disorder (e.g. “I have to think of special thoughts to stop bad things from happening”), panic-agoraphobia (e.g. “I suddenly become dizzy or faint when there is no reason for this”), generalised anxiety (“I worry that I will do badly at my school work”) and fears of physical injury (e.g. “I am scared of insects or spiders”) (Spence, 1998). The SCAS was chosen because it has sound validity and reliability and is considered to be significantly correlated with the RCMAS (Spence, 1998; Spence, Barrett, & Turner, 2003).
Children’s Automatic Thoughts Scale
The CATS consists of 40 items that assess a wide range of negative self-statements in children and adolescents (Schniering & Rapee, 2002). The items on the CATS load onto four separate subscales of cognitive content: Physical Threat (e.g. “I’m going to dye”), Social Threat (e.g. “Most people are against me”), Personal Failure (e.g. “I am worthless”) and Hostile Intent (e.g. “I won’t let anyone get away with picking on me”) (Schniering & Rapee, 2002). The CATS was employed as a psychometrically sound tool for examining the negative thoughts of the participants because it is the only child, self-report measure that assesses negative beliefs or thoughts across both internalising and externalising difficulties, including anxiety (Schniering & Rapee, 2002). The items on the CATS have demonstrated developmental sensitivity (Schniering & Rapee, 2002).
Parent-Report Measures
Spence Children’s Anxiety Scale—Parent Report
The parent report of the SCAS is identical to the self-report form except that it evaluates the child’s symptoms of anxiety according to parent perceptions of their child (Nauta, Scholing, Rapee, Abbott, & Spence, 2004). Like the child self-report, it evaluates symptoms according to six subscales that measure separation anxiety, SP, obsessive-compulsive disorder, panic-agoraphobia, generalised anxiety and fears of physical injury (Spence, 1998). The parent form of the SCAS was considered useful in providing a global impression of the child’s anxiety difficulties.
Strengths and Difficulties Questionnaire—Parent Report
The 25 items in the Strengths and Difficulties Questionnaire (SDQ) comprise 5 scales of 5 items each: Emotional Symptoms Scale (e.g. child has “many worries, often seems worried”), Conduct Problems Scale (e.g. child “often lies or cheats”), Hyperactivity Scale (e.g. child is “easily distracted, concentration wanders”), Peer Problems Scale and Prosocial Scale (e.g. child “shares readily with other children”) (Goodman, 1997). Therefore, the SDQ was used as a reliable tool to screen for any internalising and externalising difficulties within the child.
Teacher-Report Measures
Strengths and Difficulties Questionnaire—Teacher Report
The teacher-report form of the SDQ is identical to the parent-report form (Goodman, 1997). It was employed to provide further information about the presentation of any internalising and/or externalising difficulties within the child when at school. Moreover, it was used to help determine whether any differences in behaviour were being observed in the child between the school environment and the home environment.
Procedure
After referral, families were contacted and interviewed briefly over the telephone in order to clarify the child’s anxiety related difficulties and screen for other physical, medical and behavioural disorders. At the completion of the telephone interview, families were mailed the self-, parent- and teacher-report forms outlined above. Upon returning the measures to clinicians, families were then invited to attend a clinical interview at the AANSW. Written informed consent was obtained from families during the clinical interview.
After establishment of a diagnosis, participants were randomly assigned to either the 12-session CBT or the WL condition. Participants in the CBT condition were seen by therapists for weekly sessions of 2 h duration. Participants in the CBT and WL conditions were given the same measures both prior to the treatment and immediately after the 12-session treatment ended (after approximately 5½ months). At the end of the 12-session treatment, parents also completed a short questionnaire regarding consumer satisfaction with the program and any suggestions they might make regarding the improvement of the program. The same clinicians administered the pre- and post-treatment anxiety measures and interviews, and lead the treatment groups.
All the WL participants, their families and their teachers, were informed that data was being collected from them whilst on the WL and that treatment would be offered at the conclusion of the WL period. As expected, since the treatment being offered was the first specialist service of its kind specifically for HFA children, no families sought alternative treatment for their anxiety during the waiting period, although they may have been receiving other therapies to address their ASD related difficulties, e.g. speech pathology, applied behaviour analysis or occupational therapy.
Treatment Materials
The CBT intervention was designed as an HFA adaptation to the Macquarie University, “Cool Kids” program (Lyneham, Abbott, Wignall, & Rapee, 2003) with permission from the authors. The program focuses on treating the main components of anxiety rather than a specific anxiety disorder. The “Cool Kids” program is routinely used as a group treatment program. The adaptation involved nine weekly treatment sessions and three monthly booster sessions. In general, the adapted material covered the recognition of anxious feelings and somatic reactions to anxiety, simplified cognitive restructuring exercises, coping self-talk, exposure to feared stimuli and relapse prevention. The first four sessions were training sessions whereby the therapists introduced and role-played anxiety management procedures, which were then practised by the children. The remaining sessions were practise sessions whereby the children consolidated newly learned skills and planned out their weekly exposure tasks [for more detail on specific treatment procedures see Lyneham et al. (2003)].
The adaptations to the Cool Kids program were made in order to account for the visual and concrete learning style of HFA children (Jackson, 1983). Specifically, the program was extended over a longer period of time (6 months), with the use of more visual aides and structured worksheets than might usually be employed. Moreover, the largest components of the program were devoted to relaxation (three treatment sessions and two booster sessions) and exposure (4½ treatment sessions and all booster sessions) because they involve more concrete exercises and place less emphasis on the children’s communication skills, which, by the nature of their HFA, are markedly impaired. During the exposure sessions families planned out their weekly exposure tasks rather than completing the tasks in the sessions. Therefore, the exposure tasks served as daily homework assignments. No measures were used to evaluate homework compliance. However, families were asked to make a daily diary entry to record the practice and outcomes from their exposure exercises.
While a cognitive therapy component was still included in the program (1½ treatment sessions and 2 booster sessions), the information in the cognitive activities was simplified, as were the tasks involving generating helpful and unhelpful thoughts and thought challenging. The changes to the cognitive component were again made because of the children’s language and/or communication impairments. Therefore, rather than relying on their impaired communication skills when generating their own helpful and unhelpful thoughts, the HFA children identified helpful and unhelpful thoughts from worksheets with large lists of possible alternatives. As a result, the children still required the ability to identify what thoughts they and others might be experiencing.
A parent based group CBT manual was also adapted from the Cool Kids program to use with the families in concurrent sessions to the child program. The parent program addressed anxiety education, relaxation strategies, cognitive restructuring exercises, graded exposure, parent management training and relapse prevention [for more detail on specific treatment procedures see Lyneham et al. (2003)].
Treatment manuals were implemented with flexibility to allow for the individuality of each parent and child.
Results
Pre-treatment Differences
The CBT and WL groups were compared at pre-treatment on several demographic features. Children in the CBT and WL conditions did not differ in their ages t(45) = .975, p > .05, their gender χ 2(1, N = 47) = .01, p > .05 or their school grade χ 2(1, N = 47) = 2.083, p > .05. Similarly, there were no significant differences between conditions for type of ASD χ 2(1, N = 47) = .696, p > .05, level of intellectual functioning χ 2(1, N = 47) = 1.041, p > .05, family makeup χ 2(1, N = 47) = .713, p > .05, number of siblings t(45) = −.909, p > .05 or socioeconomic status (as measured by parent report of the family’s yearly income) χ 2(1, N = 47) = 2.663, p > .05. No significant pre-treatment differences were found between participants in the CBT and WL conditions in their type of primary anxiety disorder diagnosis χ 2(1, N = 47) = 1.093, p > .05.
Pre-treatment dependent measures, i.e. the self-report measures for the children, parents and teachers, were also compared across the CBT and WL conditions. For the child self-report measures, there were no significant differences between the CBT and WL conditions at pre-treatment on the CATS, RCMAS or SCAS, F(1,45) = 3.254, p > .05; F(1,45) = 2.508, p > .05; F(1,45) = .153, p > .05, respectively. Both the CBT and WL groups scored in the clinically significant range at pre-treatment. Similarly there were no significant pre-treatment differences between the CBT and WL conditions on the CATS Hostile Intent Scale; the child-report measure of externalising thoughts, F(1,45) = 2.471, p > .05. There were no significant differences between the CBT and WL groups on the parent form of the SCAS, the parent form of the SDQ Emotional Scale or the parent form of the SDQ Externalising Scale, F(1,45) = .235, p > .05; F(1,45) = .035, p > .05; F(1,45) = .532, p > .05, respectively. For the teacher-report measures, no significant pre-treatment differences were found between the CBT and WL groups on the SDQ Emotional or Externalising Scales, F(1,45) = 1.355, p > .05; F(1,45) = .537, p > .05, respectively.
During treatment there were four dropouts in the CBT condition (completers = 28). Participants were considered to have dropped out of the CBT program if they attended up to the first two sessions and then discontinued from the program. Two of the participants dropped out because their parents work schedules did not permit regular attendance, one of the participants dropped out because they moved out of area of the treatment centre and one of the participants dropped out because they felt the group was of no benefit to them. The number of dropouts was small, and there seemed to be no marked pre-treatment differences between the completers and the dropouts across any of the variables. For example, in both groups the majority of participants were male, had a diagnosis of Asperger’s disorder and were of average intellectual functioning. Consequently, no statistical comparisons were made between the two groups. Pre-treatment means for the completers and dropouts are presented in Table 2 for participant’s age and the self-report measures.
Diagnostic Status
At post-treatment, the percentage of children who no longer met DSM-IV criteria for a current primary anxiety disorder was significantly more for the CBT condition (20 of 28 children or 71.4%) than for the WL (0 out of 19 children or 0%), χ 2(1, N = 47) = 24.889, p < .05.
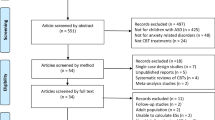
A repeated measures analysis of variance (ANOVA) was used to compare the number of anxiety disorder diagnoses between the CBT and WL conditions at pre- and post-treatment. A significant main effect was found for Time F(1,45) = 73.661, p < .001, η 2 = .621 indicating an overall reduction in the number of anxiety disorder diagnoses across the CBT and WL conditions. A significant Group × Time interaction F(1,45) = 63.792, p < .001, η 2 = .586 was also found indicating a significantly greater reduction between pre- and post-treatment in the number of anxiety disorder diagnoses for participants in the CBT condition than for those on the WL. Figure 1 represents the Group × Time interaction. Follow-up paired t-tests indicated a significant difference between the number of pre- and post-treatment anxiety diagnoses for the CBT group but no significant differences between the number of pre- and post-treatment anxiety diagnoses for the WL, t(1,27) = 10.408, p < .01 and t(1,18) = 1.000, p > .05, respectively. Independent sample t-tests revealed no significant difference between the CBT and WL groups in their number of pre-treatment anxiety diagnoses t(1,45) = −1.230, p > .05. However, a significant difference was found between the CBT and WL groups in their number of post-treatment anxiety diagnoses, t(1,45) = 5.074, p < .01. That is, the CBT group had a significantly smaller number of anxiety diagnoses at post-treatment than the WL group.
Self-report Measures
Tables 3, 4 and 5 show means and standard deviations for the child, parent and teacher self-report measures, respectively, at pre- and post-treatment for the CBT and WL conditions. Three of the measures, the CATS, the SDQ Parent and the SDQ Teacher, contain scales that assess both internalising and externalising difficulties. Therefore, separate totals were calculated for the internalising and externalising scales within these three measures. For the CATS, a total was calculated for the three internalising thoughts scales (Physical Threat, Social Threat, Personal Failure), and a separate total was calculated for the one externalising thoughts scale (Hostile Intent). For the SDQ parent and teacher forms, a total was calculated for the two externalising scales (Hyperactivity and Conduct Problems), and a separate total was calculated from the one internalising scale (Emotional Symptoms Scale). Results for all the self-report measures were analysed using 2 (Condition: CBT and WL) × 2 (Time: Pre-treatment vs Post-treatment) repeated measures ANOVAs to examine immediate treatment effects. Since nine tests were conducted, the critical alpha was set at p < .005.
On the CATS Internalising Thoughts Scales, there was a significant main effect for time, F(1,45) = 37.583, p < .005, η 2 = .455, showing an overall reduction in self-reported internalising thoughts about worries and self-esteem for both the CBT and WL condition. A significant Group × Time interaction, F(1,45) = 24.451, p < .005, η 2 = .352, indicated a significantly greater reduction between pre- and post-treatment in the number of internalising thoughts for participants in the CBT condition than for those on the WL. Follow-up paired t-tests indicated a significant difference in CATS internalising scores for the CBT group between pre- and post-treatment, t(1,27) = 7.848, p < .01. There was no significant difference in CATS internalising scores for the WL between pre- and post-treatment, t(1,18) = .951, p > .05. Independent samples t-tests revealed no significant difference between the CBT and WL groups in their pre-treatment scores on the CATS Internalising Scales, but a significant difference between the CBT and WL groups in their post-treatment scores, t(1,45) = 1.804, p > .05 and t(1,45) = 15.781, p < .01, respectively. That is, at post-treatment, the CBT group reported significantly less internalising thoughts about anxiety and self-esteem than the WL group.
Similarly, for the RCMAS, the ANOVA revealed a significant main effect for time, F(1,45) = 96.888, p < .005, η 2 = .683, demonstrating an overall reduction of self-reported anxiety for both CBT and WL conditions and a significant Group × Time interaction, F(1,45) = 71.145, p < .005, η 2 = .613, showing a significantly greater reduction between pre- and post-treatment in self-reported anxiety for participants in the CBT condition than for those in the WL. Follow-up paired t-tests indicated a significant difference in RCMAS scores for the CBT group between pre- and post-treatment, t(1,27) = 14.879, p < .01. That is, the CBT group showed a significant reduction in self-reported anxiety from pre- to post-treatment. However, there was no significant difference in RCMAS scores for the WL between pre- and post-treatment, t(1,18) = .870, p > .05. Independent samples t-tests revealed no significant difference between the CBT and WL groups in their pre-treatment scores on the RCMAS, t(1,45) = 1.584, p > .05. However, a significant difference was found between the CBT and WL groups in their post-treatment scores on the RCMAS, t(1,45) = 11.246, p < .01. That is, at post-treatment, the CBT group reported significantly less anxiety symptoms on the RCMAS than the WL group.
From pre- to post-treatment for the SCAS, the ANOVA revealed significant main and interaction effects, F(1,45) = 58.127, p < .005, η 2 = .564, and F(1,45) = 51.544, p < .005, η 2 = .534, respectively. The main effect for time revealed an overall reduction of self-reported anxiety symptoms for all the conditions. The significant interaction demonstrated a significantly greater reduction between pre- and post-treatment in the anxiety symptoms for the CBT condition than for the WL. Follow-up paired t-tests indicated a significant difference in SCAS scores for the CBT group between pre- and post-treatment, t(1,27) = 10.914, p < .01. That is, the CBT group showed a significant reduction in self-reported anxiety symptomatology between pre- and post-treatment. However, there was no significant difference in SCAS scores for the WL group between pre- and post-treatment, t(1,18) = .323, p > .05. Independent samples t-tests revealed no significant difference between the CBT and WL groups in their pre-treatment scores on the SCAS, t(1,45) = −.391, p > .05. However, a significant difference was revealed between the CBT and WL groups in their post-treatment scores on the SCAS, t(1,45) = 9.048, p < .01. That is, at post-treatment, the CBT group reported significantly less anxiety symptoms on the SCAS than the WL group.
Finally, in terms of externalising difficulties, as measured by the CATS Hostile Intent Scale, from pre- to post-treatment, the ANOVA showed neither a significant main effect nor a significant interaction, F(1,45) = 6.281, p > .01, η 2 = .122 and F(1,45) = 7.091, p > .01, η 2 = .136, respectively. That is, there was no demonstrated change over time in externalising thoughts across conditions nor a greater reduction in externalising thoughts for one condition more than the other between pre- and post-treatment.
Parent-Report Measures
Regarding the parent-report measures, from pre- to post-treatment for the SCAS-P, a significant main effect for Time, F(1,45) = 74.259, p < .005, η 2 = .623 and a significant Group × Time interaction, F(1,45) = 52.835, p < .005, η 2 = .540 were found. The main effect indicated an overall reduction in parent-reported anxiety symptoms for both conditions. The interaction effect indicated that the parents of children in the CBT condition reported a significantly greater reduction in their child’s anxiety symptoms between pre- and post-treatment than the parents of children in the WL condition. Follow-up paired t-tests indicated a significant difference in SCAS-P scores for the CBT group between the pre- and post-treatment, t(1,27) = 11.483, p < .01. However, there was no significant difference in SCAS-P scores for the WL between pre- and post-treatment, t(1,18) = 1.026, p > .05. Independent samples t-tests revealed no significant difference between the CBT and WL groups in their pre-treatment scores on the SCAS-P, t(1,45) = .485, p > .05. However, a significant difference was found between the CBT and WL groups in their post-treatment scores on the SCAS-P, t(1,45) = 14.610, p < .01. That is, at post-treatment, parents of children in the CBT group reported significantly less anxiety symptoms in their child than parents of children in the WL group.
In support of the SCAS parent-report results, a significant main effect for Time, F(1,45) = 25.475, p < .005, η 2 = .361, and a significant Group × Time interaction, F(1,45) = 54.336, p < .005, η 2 = .547 were found for the parent form of the SDQ Emotional Symptoms Scale. Follow-up paired t-tests indicated a significant difference in parent SDQ Emotional scores for the CBT group between pre- and post-treatment, t(1,27) = 10.275, p < .01. That is, parents of children in the CBT group showed a significant reduction in their reports of emotional difficulties within their child between pre- and post-treatment. However, there was no significant difference in parent SDQ Emotional scores for the WL between pre- and post-treatment, t(1,18) = −1.407, p > .05. Independent samples t-tests revealed no significant difference between the CBT and WL groups in their pre-treatment scores on the parent SDQ Emotional Scale, t(1,45) = .186, p > .05. However, there was a significant difference between the CBT and WL groups in their post-treatment scores on the scale, t(1,45) = 14.687, p < .01. That is, at post-treatment, parents of children in the CBT group reported significantly less emotional difficulties for their child than parents of children in the WL group.
In terms of externalising difficulties, as measured by the parent report SDQ Externalising Scales, from pre- to post-treatment, the ANOVA showed a significant main effect and a significant interaction, F(1,45) = 10.057, p < .005, η 2 = .183 and F(1,45) = 16.109, p < .005, η 2 = .264, respectively. That is, there was both an overall reduction in parent-reported externalising difficulties across conditions and a significantly greater reduction in parent-reported externalising difficulties for children in the CBT condition than for children in the WL condition, between pre- and post-treatment. Follow-up paired t-tests indicated a significant difference in parent SDQ Externalising scores for the CBT Group between pre- and post-treatment, t(1,27) = 5.226, p < .01. However, there was no significant difference in the parent SDQ Externalising scores for the WL between pre- and post-treatment, t(1,18) = −.631, p > .05. Independent samples t-tests revealed no significant differences between the CBT and WL groups in either their pre- or post-treatment scores on the parent SDQ Externalising Scale, t(1,45) = −.729, p > .05 and t(1,45) = 2.130, p > .01, respectively. However, there did appear to be a trend in the scores such that parents of the CBT group tended to have lower scores at post-treatment than the parents of the WL group.
Teacher-Report Measures
Regarding the teacher-report measures, from pre- to post-treatment for the teacher SDQ Emotional Scale, a significant main effect for Time, F(1,45) = 13.854, p < .005, η 2 = .235 and a significant Group × Time interaction, F(1,45) = 28.702, p < .005, η 2 = .389 were found. The main effect indicated an overall reduction of teacher-reported emotional symptoms for both conditions. The interaction effect indicated that teachers of children in the CBT condition reported a significantly greater reduction in the child’s emotional symptoms between pre- and post-treatment than teachers of children in the WL condition. Follow-up paired t-tests indicated a significant difference in the teacher SDQ Emotional scores for the CBT group between pre- and post-treatment, t(1,27) = 8.252, p < .01. However, there was no significant difference in teacher SDQ Emotional scores for the WL between pre- and post-treatment, t(1,18) = −.903, p > .05. Independent samples t-tests revealed no significant difference between the CBT and WL groups in their pre-treatment scores on the teacher SDQ Emotional Scale, t(1,45) = 1.164, p > .05. However, there was significant difference between the CBT and WL groups in their post-treatment scores on the scale, t(1,45) = 9.415, p < .01. That is, at post-treatment, teachers of children in the CBT group reported significantly less emotional difficulties for the children than did teachers of children in the WL group.
In terms of externalising difficulties, as measured by the teacher report SDQ Externalising Scales, from pre- to post-treatment, the ANOVA showed a significant main effect and a significant interaction, F(1,45) = 10.861, p < .005, η 2 = .194 and F(1,45) = 12.477, p < .005, η 2 = .217, respectively. That is, there was both an overall reduction in teacher-reported externalising difficulties across conditions and a significantly greater reduction in teacher-reported externalising difficulties for children in the CBT condition than for children in the WL condition, between pre- and post-treatment. Follow-up paired t-tests indicated a significant difference in teacher SDQ Externalising scores for the CBT group between pre- and post-treatment, t(1,27) = 4.997, p < .01. However, there was no significant difference in teacher SDQ Externalising scores for the WL group between pre- and post-treatment, t(1,18) = −.175, p > .05. Independent samples t-tests revealed no significant difference between the CBT and WL groups in either their pre- or post-treatment scores on the teacher SDQ Externalising Scales, t(1,45) = −.733, p > .05 and t(1,45) = 2.117, p > .01, respectively. However, there did appear to be a trend in the scores such that teachers for the CBT group tended to have lower scores at post-treatment than the teachers for the WL group.
Discussion
The current study represents the first report on the efficacy of a cognitive–behavioural intervention for the treatment of anxiety disorders in children with a HFA. Overall, the results indicate that the active CBT treatment condition produced significant change in the dependent variables in contrast to the WL control condition. Since all the child-, parent- and teacher-report data supported the beneficial effects of the CBT intervention, it could be concluded that the efficacy of the treatment extended to both the children’s home and school settings. Moreover, given that the completers did not seem to differ from the dropouts, and that no significant differences were found between the CBT and WL groups in gender, type of ASD, level of intellectual functioning, family makeup or socioeconomic status, it seems reasonable to conclude that the primary source of change was the CBT treatment.
The current findings are comparable to previous studies that have tested the efficacy of CBT in treating anxiety disorders among typically developing children and their families (Albano et al., 2003; Albano & Kendall, 2002; Barrett et al., 1996; Compton et al., 2002; Flannery-Schroeder & Kendall, 2000; Kashdan & Herbert, 2001; Kendall, 1994; Kendall et al., 1997; Ollendick & King, 1998; Weisz et al., 1995). Specifically, the incidence of treated HFA children who were anxiety diagnosis free at post-treatment, 71.4%, is comparable to the range, 54–73%, reported across studies with typically developing children, where no adjunctive family intervention has been used (e.g. Flannery-Schroeder & Kendall, 2000; Kendall, 1994). Moreover, the incidence is comparable to the range, 64–84%, reported across studies where, similar to the current CBT intervention, an adjunctive family intervention has been used (e.g. Barrett et al., 1996; Silverman et al., 1999a, b).
The current results could be argued to fill a gap in the level of knowledge about the treatment of anxiety in HFA children. Until now, cognitive–behavioural interventions have never been empirically evaluated with a HFA population. In fact, to date there has been little empirical research on any treatment models for the anxiety of HFA children beyond pharmacotherapy. Consequently, the present findings highlight that CBT could be an effective treatment model for the anxiety difficulties commonly associated with HFA children. Further treatment-outcome studies would be beneficial in order to replicate the current findings and, in turn, confirm support for the use of CBT as a treatment for anxious HFA children.
The present findings support Chalfant et al.’s (2004) conclusions that HFA children seem to be able to identify their thoughts using the CATS and, therefore, may have some ToM ability. The CATS scales were included in the current study to measure cognitive shift in the participants. The internalising thought scores of the CBT group differed significantly between pre- and post-treatment and were significantly lower at post-treatment than the scores of the WL group. Consequently, the results suggest that the CBT participants not only benefited from the intervention in terms of experiencing less internalising thoughts about anxiety and self-esteem, but also, that they were able to demonstrate this cognitive shift by accurately completing the CATS. Specific evidence that CBT participants accurately quantified their cognitive shift using the CATS, can be seen in the level of accordance between their lower scores on the CATS at post-treatment and their lower scores on other self- and parent-report measures of anxiety symptomatology. Therefore, if the HFA participants demonstrated an intact ability to identify their thoughts, then it seems plausible to suggest that they, in turn, may have demonstrated some ToM ability. As a result, the findings also provide further support for Chalfant et al.’s (2004) suggestion that HFA children may be considered appropriate candidates for CBT interventions.
The ability of the children in the current study to both engage in and benefit from the CBT intervention also has indirect implications for broader ToM research. Since the intervention was found to be effective, it could be inferred that the treated participants were able to engage in the cognitive therapy component of the program. It is acknowledged that the cognitive tasks in the current program were modified such that children did not need to generate their own helpful and unhelpful thoughts, but rather, could pick these thoughts out from written lists of alternatives. In modifying the program, emphasis was taken away from the HFA children’s primary communication impairments. However, while the cognitive therapy component was altered in its delivery it was not removed from the program. The children did not need to use their expressive communication skills, but they did need to identify worrying thoughts in themselves and in others; to identify emotional states; to understand and to explain how particular thoughts affect emotions; and to generate helpful and/or brave thoughts in order to change emotional states. As a result, since the treated HFA children were able to complete the cognitive tasks, it seems plausible to argue that they may have indirectly been demonstrating ToM ability. Therefore, the present findings seem to challenge the suggestion in the literature that all children with an ASD have no ToM ability (Baron-Cohen et al., 1985; Holroyd & Baron-Cohen, 1993; Kleinman et al., 2001). Rather, the results support the growing argument that ToM impairment is neither specific to children with autism nor globally impaired across all types of ASDs (Bauminger & Kasari, 1999; Bowler & Strom, 1999; Buitelaar et al., 1999; Yirmiya, Solomonica-Levi, Shulman, & Pilowsky, 1996). Moreover, the results support the suggestion that HFA children may have ToM ability (Bauminger & Kasari, 1999; Bowler & Strom, 1999; Buitelaar et al., 1999; Yirmiya et al., 1996). Future research could explore what is the optimal degree of modification that needs to be made to the cognitive components of the program in order for the children to engage in the cognitive tasks without relying on their impaired communication skills.
Given that the children in the CBT group were successful in completing the simplified cognitive tasks, it is possible that similar cognitive tasks could be developed in order to teach complex ToM skills to children, both with an ASD and typically developing. For example, children could be provided pictures of facial expressions representing a range of emotional states with an accompanying list of potential thoughts and asked to try and match the thought to the facial expression. It seems plausible that making ToM and empathy tasks concrete in the abovementioned way could be beneficial for any child with information processing and/or abstract reasoning difficulties, not only ASD children. Again, for a child with an ASD, the ability to pick the correct answer from a range of provided alternatives rather than generate their own response avoids heavy reliance on their primary communication impairments.
Long-term follow-up data is not yet available from the present study. Clearly, it will be beneficial to monitor the CBT participants over a follow-up period of 6, 12 and 24 months in order to determine whether their treatment gains are maintained. Although ethical considerations could arise, future treatment outcome research might compare the CBT and WL conditions at pre-, post-treatment and at follow-up, such that the length of time spent on the WL is extended to the follow-up period.
It is unclear whether the adapted CBT program for the HFA children made the intervention more effective than using the standard Cool Kids intervention (Lyneham et al., 2003) without adaptation. Future treatment outcome research could compare the standard Cool Kids program (Lyneham et al., 2003), the current adaptation and the WL in order to clarify the impact of the adapted components in the HFA program.
A similar issue relates to the treatment’s cost-effectiveness. That is, it is unclear whether the length and number of the therapeutic sessions (2 h duration and 12 sessions, respectively) were more than what might be necessary for successful treatment outcomes. Perhaps future research could further examine the issue of optimum session time and intervention length for anxious HFA children.
The broader impact of the CBT intervention on the child and family’s quality of life was not measured in the current study. There is evidence in the literature to suggest that structured, intense interventions like the CBT group program cannot only improve the main presenting difficulty, but also, can improve other aspects of the participant’s functioning such as their peer relationships (Hirshfeld-Becker & Biederman, 2002; Kendall, 2000). Future studies involving CBT and HFA children could include measures of family quality of life and perhaps, more importantly for ASD children, measures of social skills and/or social functioning.
Several methodological issues could be associated with the current investigation. It is recognised that the current sample of HFA children was small in size. Accordingly, the data may not be reflective of the wider anxious HFA population. The participant’s formal ASD diagnostic assessment was not completed by the investigating clinicians. Consequently, the validity of the participants’ diagnostic status could be questioned. However, although not formally assessed by the investigators, behavioural observations of the participants over the 6-month period confirmed that all participants did seem to meet the DSM-IV criteria for either Autistic Disorder or Asperger’s Disorder.
Given that the study was conducted in a natural clinical setting, with limited resources, rather than a designated research clinic, several other methodological issues arise. First, treatment integrity was not formally measured by the investigators. The benefits of the current CBT intervention could be interpreted with greater confidence if audio-taped therapy sessions were checked for integrity by clinicians who were blind to the study’s aims. Second, no therapist time was spent with the WL control group. Spending an equivalent amount of time with the treatment and control groups could help ensure that the benefits of the treatment could be attributed to the treatment alone and not to time spent with a therapist. Third, it is possible that knowledge of the treatment program might have impacted on the way the WL participants completed their measures. For example, knowledge of the future treatment might have helped to attenuate some of their anxiety. This could, in turn, have resulted in slightly lower scores on measures of anxiety symptomatology at post-test. Fourth, the clinicians who implemented the CBT groups and collected the relevant pre- and post-treatment data were not blind to the study’s aims. Again, greater conviction in the current results could be achieved if a larger number of clinicians could be involved in either blindly running the CBT groups and/or blindly collecting the pre- and post-treatment data. Nevertheless, the consistent pattern of results across several information sources seems to provide added confidence to the findings.
Regardless, the current findings provide the first evidence for the benefit of a CBT anxiety intervention for anxious, HFA children. Future research is needed to replicate and, therefore, confirm the findings regarding the efficacy of the CBT approach with anxious HFA children. Future investigations could also begin to explore whether a more simplified version of the current program could be used to address the anxiety related difficulties of children with lower functioning forms of autism, including children with intellectual impairment.
References
Achenbach, T. M. (1985). Assessment of anxiety in children. In H. A. Tuma, & J. D. Maser (Eds.), Anxiety and the anxiety disorders (pp. 707–734). Hillsdale: Lawrence Erlbaum.
Albano, A. M., Chorpita, B. F., & Barlow, D. H. (2003). Childhood anxiety disorders. In E. J. Marsh, & R. A. Russell (Eds.), Child psychopathology (2nd ed., pp. 279–329). New York: Guildford.
Albano, A. M., & Kendall, P. C. (2002). Cognitive behavioural therapy for children and adolescents with anxiety disorders: Clinical research advances. International Review of Psychiatry, 14, 129–134.
Albano, A. M., & Silverman, W. K. (1996). Anxiety Disorders Interview Schedule for DSM-IV: Child version. Clinical manual. San Antonio: Psychological Corporation.
Alfano, C. A., Beidel, D. C., & Turner, S. M. (2002). Cognition in childhood anxiety: Conceptual methodological and developmental issues. Clinical Psychology Review, 22, 1209–1238.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington: Author.
Baron-Cohen, S. (2001). Theory of mind and autism: A review. In L. M. Glidden (Eds.), International review of research in mental retardation: Autism (pp. 169–184). San Diego: Academic.
Baron-Cohen, S., Leslie, A. M., & Frith, U. (1985). Does the autistic child have a theory of mind? Cognition, 21, 37–46.
Barrett, P. M., Dadds, M. R., & Rapee R. M. (1996). Family treatment of childhood anxiety: A controlled trial. Journal of Consulting and Clinical Psychology, 64, 333–342.
Barrett, P. M., Duffy, A. L., Dadds, M. R., & Rapee, R. M. (2001). Cognitive-behavioral treatment of anxiety disorders in children: Long-term (6 year) follow-up. Journal of Consulting and Clinical Psychology, 69, 135–141.
Barrett, P. M., Rapee, R. M., Dadds, M. R., & Ryan, S. M. (1996). Family enhancement of cognitive style in anxious and aggressive children. Journal of Abnormal Child Psychology, 24, 187–203.
Barrett, P. M., & Turner, C. M. (2001). Prevention of anxiety symptoms in primary school children: Preliminary results from a universal school-based trial. British Journal of Clinical Psychology, 40, 399–410.
Barrett, P. M., & Turner, C. M. (2004). Prevention strategies. In T. L. Morris, & J. S. March (Eds.), Anxiety disorders in children and adolescents (pp. 371–387). New York: Guilford.
Bauminger, N., & Kasari, C. (1999). Brief report: Theory of mind in high-functioning children with autism. Journal of Autism and Developmental Disorders, 29, 81–86.
Beck, A. T. (1976). Cognitive therapy and the emotional disorders. New York: International Universities Press.
Beebe, D. W., & Risi, S. (2003). Treatment of adolescents and young adults with high-functioning autism or Asperger syndrome. In M. A. Reinecke, F. M. Dattilio, & A. Freeman (Eds.), Cognitive therapy with children and adolescents: A casebook for clinical practice (2nd ed., pp. 369–401). New York: Guilford.
Benjamin, R. S., Costello, E. J., & Warren, M. (1990). Anxiety disorders in a paediatric sample. Journal of Anxiety Disorders, 4, 851–855.
Bernstein, R. S., Costello, E. J., & Warren, M. (1990). Anxiety disorders in paediatric sample. Journal of Anxiety Disorders, 4, 293–316.
Bird, H. R. (1996). Epidemiology of childhood disorders in a cross-cultural context. Journal of Child Psychology and Psychiatry and Allied Disciplines, 37, 35–49.
Bowen, R. C., Offord, D. R., & Boyle, M. H. (1990). The prevalence of overanxious disorder and separation anxiety disorder: Results from the Ontario Child Health Study. Journal of the American Academy of Child and Adolescent Psychiatry, 29, 753–758.
Bowler, D. M. (1992). “Theory of Mind” in Asperger’s syndrome. Journal of Child Psychology and Psychiatry, 33, 877–893.
Bowler, D. M., & Strom, E. (1999). Elicitation of first-order “theory of mind” in children with autism. Autism, 2, 33–44.
Braconnier, A. (1983). Autistic anxiety: Psychoanalytic approach. Neuropsychiatrie de L’Enfance et de L’Adolescence, 31, 255–256.
Brodkin, E. S., McDougle, C. J., Naylor, S. T., Cohen, D. J., & Price, L. H. (1997). Clomipramine in adults with pervasive developmental disorders: A prospective open-label investigation. Journal of Child and Adolescent Psychopharmacology, 7, 109–121.
Buitelaar, J. K., van der Wees, M., Swaab-Barneveld, H., & van der Gaag, J. R. (1999). Theory of mind and emotion-recognition functioning in autistic spectrum disorders and in psychiatric control and normal children. Development and Psychopathology, 11, 39–58.
Chalfant, A. M. (2004). Anxiety in children with High Functioning Autism Spectrum Disorders: Theoretical issues and treatment implications. Manuscript submitted for publication.
Chalfant, A. M., Franklin, J., & Rapee, R. M. (2004). The perception of anxious thoughts in children with an Autism Spectrum Disorder. Manuscript submitted for publication.
Chambless, D. L., & Hollon, S. D. (1998). Defining empirically supported therapies. Journal of Consulting and Clinical Psychology, 6, 7–18.
Clark, D. B., Smith, M. G., Neighbors, B. D., Skerlec, L. M., & Randall, J. (1994). Anxiety disorders in adolescence: Characteristics, prevalence, and co morbidities. Clinical Psychology Review, 14, 113–137.
Compton, S. N., Burns, B. J., Egger, H. L., & Robertson, E. (2002). Review of the evidence base for treatment of childhood psychopathology: Internalizing disorders. Journal of Consulting and Clinical Psychology, 70, 1240–1266.
Costello, E. J., Costello, A. J., Edelbrock, C., Burns, B. J., Dulcan M. K., Brent D., et al. (1988). Psychiatric disorders in paediatric primary care. Archives of General Psychiatry, 45, 1107–1116.
Coupland, N. J. (2001). Social phobia: Etiology, neurobiology and treatment. Journal of Clinical Psychiatry, 62(Suppl. 1), 25–35.
Craske, M. G. (1997). Fear and anxiety in children and adolescents. Bulletin of the Menninger Clinic, 61(Suppl. A), 4–36.
Dahlgren, S., Sandberg, A. D., & Hjelmquist, E. (2003). The non-specificity of theory of mind deficits: Evidence from children with communicative disabilities. European Journal of Cognitive Psychology, 15, 129–155.
Daleiden, E. L., & Vasey, M. W. (1997). An information-processing perspective on childhood anxiety. Clinical Psychology Review, 17, 407–429.
Dyck, M. J., Ferguson, K., & Shochet, I. M. (2001). Do autism spectrum disorders differ from each other and from non-spectrum disorders on emotion recognition tests? European Child and Adolescent Psychiatry, 10, 105–116.
Flannery-Schroeder, E. C., & Kendall, P. C. (2000). Group and individual cognitive-behavioral treatments for youth with anxiety disorders: A randomized clinical trial. Cognitive Therapy and Research, 24, 251–278.
Frith, U. (1989). Autism: Explaining the enigma. Oxford: Blackwell.
Gillot, A., Furniss, F., & Walter, A. (2001). Anxiety in high-functioning children with autism. Autism, 5, 277–286.
Goodman, R. (1997). The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38, 581–586.
Groden, J., Cautela, J., Prince, S., & Berryman, J. (1994). The impact of stress and anxiety on individuals with autism and developmental disabilities. In E. Schopler, & G. B. Mesibov (Eds.), Behavioral issues in autism. Current issues in autism (pp. 177–194). New York: Plenum.
Happé, F. G. E. (1994a). An advanced test of Theory of Mind: Understanding of story characters’ thoughts and feelings by able autistic, mentally handicapped, and normal children and adults. Journal of Autism and Developmental Disorders, 24, 129–154.
Happé, F. G. E. (1994b). Annotation: Current psychological theories of autism: The “Theory of Mind” account and rival theories. Journal of Child Psychology and Psychiatry, 35, 215–229.
Happé, F. G. E. (1995). The role of age and verbal ability in the theory of mind task performance of subjects with autism. Child Development, 66, 843–855.
Happé, F. G. E., Briskman, J., & Frith, U. (2001). Exploring the cognitive phenotype of autism: Weak “central coherence” in parents and siblings of children with autism: I. Experimental tests. Journal of Child Psychology and Psychiatry and Allied Disciplines, 42, 299–307.
Heinemann, E. (1999). Psychoanalytic therapy with an autistic young man: A discussion of Frances Tustin’s theories. In J. De Groef, & E. Heinemann (Eds.), Psychoanalysis and mental handicap (pp. 23–40). London: Free Association Books.
Hirshfeld-Becker, D. R., & Biederman, J. (2002). Rationale and principles for early intervention with young children at risk for anxiety disorders. Clinical Child and Family Psychology Review, 5, 161–172.
Holroyd, S., & Baron-Cohen, S. (1993). Brief report: How far can people with autism go in developing a theory of mind? Journal of Autism and Developmental Disorders, 23, 379–385.
Jackson, H. J. (1983). Current trends in the treatment of phobias in autistic and mentally retarded persons. Australia and New Zealand Journal of Developmental Disabilities, 9, 191–208.
Kalus, O., Asnis, G. M., Ribinson, E., Kahn, R., Friedman, J. M. H., Iqbal, N., et al. (1991). Desipramine treatment in panic disorder. Journal of Affective Disorders, 21, 239–244.
Kashani, J. H., & Ovraschel, H. (1988). Anxiety disorders in mid-adolescence: A community sample. American Journal of Psychiatry, 145, 960–964.
Kashani, J. H., & Ovraschel, H. (1990). A community study of anxiety in children and adolescents. American Journal of Psychiatry, 147, 313–318.
Kashdan, T. B., & Herbert, J. D. (2001). Social anxiety disorder in childhood and adolescence: Current status and future directions. Clinical Child and Family Psychology Review, 4, 37–61.
Kazdin, A. E. (1986). Research designs and methodology. In S. L. Garfield, & A. E. Bergin (Eds.), Handbook of psychotherapy and behaviour change (3rd ed., pp. 23–69). New York: Wiley.
Kendall, P. C. (1985). Toward a cognitive-behavioural model of child psychopathology and a critique of related interventions. Journal of Abnormal Child Psychology, 13, 357–372.
Kendall, P. C. (1994). Treating anxiety disorders in children: Results of a randomised clinical trial. Journal of Consulting and Clinical Psychology, 62, 100–110.
Kendall, P. C. (2000). Child and adolescent therapy: Cognitive-behavioral procedures (2nd ed.). New York: Guilford.
Kendall, P. C., Flannery-Schroeder, E., Panichelli-Mindel, S., Southam-Gerow, M., Henin, A., & Warman, M. (1997). Therapy for youths with anxiety disorders: A second randomized clinical trial. Journal of Consulting and Clinical Psychology, 65, 366–380.
Kendall, P. C., Krain, A., & Treadwell, K. R. H. (1999). Generalized anxiety disorders. In R. T. Ammerman, M. Hersen, & C. G. Last (Eds.), Handbook of prescriptive treatments for children and adolescents (pp. 155–171). Needham Heights: Allyn & Bacon.
Kendall, P. C., & Morris, R. (1991). Child therapy: Issues and recommendations. Journal of Consulting and Clinical Psychology, 59, 777–784.
Kendall, P. C., & Ronan, K. R. (1990). Assessment of children’s anxieties, fears and phobias: Cognitive-behavioural models and methods. In C. R. Reynolds, & K. W. Kamphaus (Eds.), Handbook of psychological and educational assessment of children (pp. 223–244). New York: Guilford.
Kendall, P. C., Safford, S., Flannery-Schroeder, E., & Webb, A. (2004). Child anxiety treatment: Outcomes in adolescence and impact on substance use and depression at 7.4 year follow-up. Journal of Consulting and Clinical Psychology, 72, 276–287.
Kim, J. A., Szatmari, P., Bryson, S. E., Streiner, D. L., & Wilson, F. J. (2000). The prevalence of anxiety and mood problems among children with autism and Asperger syndrome. Autism, 4, 117–132.
Kleinman, J., Marciano, P. L., & Ault, R. L. (2001). Advanced theory of mind in high-functioning adults with autism. Journal of Autism and Developmental Disorders, 31, 29–36.
Lord, C. (1996). Treatment of a high-functioning adolescent with autism: A cognitive-behavioral approach. In M. A. Reinecke, F. M. Dattilio, & A. Freeman (Eds.), Cognitive therapy with children and adolescents: A casebook for clinical practice (pp. 394–404). New York: Guilford.
Lyneham, H. J., Abbott, M. J., Wignall, A., & Rapee, R. M. (2003). The Cool Kids family program—therapist manual. Sydney: Macquarie University.
Matson, J. L., & Love, S. R. (1990). A comparison of parent-reported fear for autistic and nonhandicapped age-matched children and youth. Australia and New Zealand Journal of Developmental Disabilities, 16, 349–357.
McDougle, C. J., Price, L. H., Volkmar, F. R., Goodman, W. K., Ward-O’Brien, D., Nielsen, J., et al. (1992). Clomipramine in autism: Preliminary evidence of efficacy. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 746–750.
Mendlowitz, S. L., Manassis, K., Bradley, S., Scapillato, D., Miezitis, S., & Shaw, B. F. (1999). Cognitive-behavioral group treatments in childhood anxiety disorders: The role of parental involvement. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1223–1229.
Morgan, B., Maybery, M., & Durkin, K. (2003). Weak central coherence, poor joint attention, and low verbal ability: Independent deficits in early autism. Developmental Psychology, 39, 646–656.
Muris, P., Steerneman, P., Merckelbach, H., Holdrinet, I., & Meesters, C. (1998). Comorbid anxiety symptoms in children with pervasive developmental disorders. Journal of Anxiety Disorders, 12, 387–393.
Nauta, M., Scholing, A., Rapee, R., Abbott, M., & Spence, S. (2004). Development of a parent report measure of children’s anxiety: Psychometric properties and comparison with child report in a clinic and normal sample. Behaviour Research and Therapy, 42, 813–839.
Nicolson, R., Awad, G., & Sloman, L. (1998). An open trial of risperidone in young autistic children. Journal of the American Academy of Child and Adolescent Psychiatry, 37, 372–376.
Ollendick, T. H. (1986). Behaviour therapy with children and adolescents. In S. Garfield, & A. Bergin (Eds.), Handbook of psychotherapy and behaviour change (3rd ed., pp. 525–565). New York: Wiley.
Ollendick, T. H., & King, N. J. (1998). Empirically supported treatments for children with phobic and anxiety disorders: Current status. Journal of Clinical Child Psychology, 27, 156–167.
Piacentini, J., & Bergman, R. L. (2001). Developmental issues in cognitive therapy for childhood anxiety disorders. Journal of Cognitive Psychotherapy, 15, 165–182.
Rapee, R. M. (2000). Group treatment of children with anxiety disorders: Outcome and predictors of treatment response. Australian Journal of Psychology, 52, 125–129.
Reynolds, C. R., & Richmond, B. O. (1978). What I think and feel: A revised measure of child’s manifest anxiety. Journal of Abnormal Child Psychology, 6, 271–280.
Rumsey, J. M., Rapoport, J. L., & Sceery, W. R. (1985). Autistic children as adults: Psychiatric social, and behavioral outcomes. Journal of the American Academy of Child and Adolescent Psychiatry, 24, 465–473.
Schniering, C. A., & Rapee, R. M. (2002). Development and validation of a measure of children’s automatic thoughts: The children’s automatic thoughts scale. Behaviour Research and Therapy, 40, 1091–1109.
Schteingart, A. (1989). Autism and separation anxiety. Revue Francaise de Psychanalyse, 53, 291–296.
Shortt, A. L., Barrett, P. M., & Fox, T. L. (2001). Evaluating the FRIENDS program: A cognitive-behavioural group treatment for anxious children and their parents. Journal of Clinical Child and Adolescent Psychology, 30, 525–535.
Silverman, W. K., Kurtines, W. M., Ginsburg, G. S., Weems, C. F., Lumpkin, P. W., & Carmichael, D. H. (1999a). Treating anxiety disorders in children with group cognitive–behavioral therapy: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 67, 995–1003.
Silverman, W. K., Kurtines, W. M., Ginsburg, G. S., Weems, C. F., Rabian, B., & Serafini, L. T. (1999b). Contingency management, self-control, and education support in the treatment of childhood phobic disorders: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 67, 675–687.
Silverman, W. K., Saavedra, L. M., & Pina, A. A. (2001). Test–retest reliability of anxiety symptoms and diagnoses with the anxiety disorders interview schedule for DSM-IV: Child and parent versions. Journal of American Academy of Child and Adolescent Psychiatry, 40, 937–943.
Spence, S. H. (1998). A measure of anxiety symptoms among children. Behaviour Research and Therapy, 36, 545–566.
Spence, S. H., Barrett, P. M., & Turner, C. M. (2003). Psychometric properties of the Spence Children’s Anxiety Scale with young adolescents. Journal of Anxiety Disorders, 17, 605–625.
Steffenburg, S., Gillberg, C., & Steffenburg, U. (1996). Psychiatric disorders in children and adolescents with mental retardation and active epilepsy. Archives of Neurology, 53, 904–912.
Tonge, B. J., Brereton, A. V., Gray, K. M., & Einfeld, S. L. (1999). Behavioural and emotional disturbance in high-functioning autism and Asperger syndrome. Autism, 3, 117–130.
Tsai, L. Y. (1999). Pharmacology in autism. Psychosomatic Medicine, 61, 651–665.
Verheij, F., & Van Loon, H. (1993). Pervasive developmental disorders not otherwise specified: A developmental-psychopathological approach for the development of made-to-measure treatment planning. European Journal of Child and Adolescent Psychiatry: Acta Paedopsychiatrica, 55, 235–242.
Vila, G., Nollet-Clemencon, C., de Blic, J., Mouren-Simeoni, M., & Scheinmann, P. (2000). Prevalence of DSM-IV anxiety and affective disorders in a paediatric population of asthmatic children and adolescents. Journal of Affective Disorders, 58, 223–231.
Weisz, J. R., Weiss, B., Han, S. S., Granger, D. A., & Morton, T. (1995). Effects of psychotherapy with children and adolescents revisited: A meta-analysis of treatment outcome studies. Psychological Bulletin, 117, 450–468.
Wing, L. (1976). Early Childhood Autism. London: Pergamon.
Wing, L. (1997). The history of ideas on autism. Autism, 1, 13–23.
Wolf, L. C., Noh, S., Fisman, S. N., & Speechly, M. (1989). Psychological effects of parenting stress on parents of autistic children. Journal of Autism and Developmental Disorders, 19, 157–166.
Yirmiya, N., Erel, O., Shaked, M., & Solomonica-Levi, D. (1998). Meta-analysis comparing theory of mind abilities of individuals with autism, individuals with mental retardation, and normally developing individuals. Psychological Bulletin, 124, 283–307.
Yirmiya, N., Solomonica-Levi, D., Shulman, C., & Pilowsky, T. (1996). Theory of mind abilities in individuals with autism, down syndrome, and mental retardation of unknown etiology: The role of age and intelligence. Journal of Child Psychology and Psychiatry, 37, 1003–1014.
Acknowledgments
The authors gratefully acknowledge the financial support from Autism Spectrum Australia (“Aspect”) and the St George Foundation. Also, thanks go to all the children and parents who made the research possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chalfant, A.M., Rapee, R. & Carroll, L. Treating Anxiety Disorders in Children with High Functioning Autism Spectrum Disorders: A Controlled Trial. J Autism Dev Disord 37, 1842–1857 (2007). https://doi.org/10.1007/s10803-006-0318-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-006-0318-4