Abstract
The current study tested the associations between peer victimization and internalizing symptoms in 54 verbally fluent adolescent males with a diagnosis of autism spectrum disorder. Adolescent- and parent-reports of multiple types of peer victimization and internalizing symptoms were used. First, the validity and reliability of the adolescent-report measure of peer victimization were successfully tested, with some exceptions. Then, structural equation models showed that adolescent-reports of peer victimization were associated with a latent construct of internalizing symptoms even after controlling for parent-reports of peer victimization. Discussion focuses on the importance of considering adolescent-reports of negative peer experience, such as peer victimization, rather than relying exclusively on parent reports.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescents with autism spectrum disorders (ASD) are common targets of peer victimization, with parents reporting rates ranging from 46 to 94 % across studies (Cappadocia et al. 2012; Little 2002; Sterzing et al. 2012). These rates are especially alarming considering that peer victimization has been shown to be clearly related to the development of internalizing symptoms in typically developing adolescents (Reijntjes et al. 2010; Siegel et al. 2009; Sweeting et al. 2006; van der Wal et al. 2003; You and Bellmore 2012). Internalizing symptoms are common in adolescents with ASD (Ghaziuddin et al. 1998, 2002; Hurtig et al. 2009), including lifetime estimates for depression as high as 25 % (Leyfer et al. 2006), as compared to estimated lifetime estimates of depression of 5 % for typical adolescents (Costello et al. 2005). However, research aimed at understanding potential causes of internalizing symptoms in adolescents with ASD is limited.
Internalizing symptoms refer to feelings of “being withdrawn, experiencing somatic complaints, and feeling anxious or depressed” (Ghandour et al. 2010, p. e270). In typically developing adolescents, the association between peer victimization and internalizing symptoms is well-established. Specifically, peer victimization is associated both concurrently and over time with higher levels of internalizing symptoms, including depressive and/or anxiety problems (Reijntjes et al. 2010; Siegel et al. 2009; Sweeting et al. 2006; van der Wal et al. 2003; You & Bellmore 2012). Thus, the high rates of peer victimization reported in adolescents with ASD may help explain elevated rates of internalizing symptoms in this group. Indeed, some recent work has provided support for this hypothesis. For instance, peer teasing has been found to mediate the cross-sectional correlation between autistic traits and depressive/anxiety symptoms in the general population (Rosbrook and Whittingham 2010). In addition, a study of 60 adolescents with ASD and comorbid anxiety disorder found that adolescent-reports of peer victimization were significantly correlated with parent-reported maladjustment across different types of internalizing symptoms (Storch et al. 2012).
Although there is a growing literature on peer victimization in ASD in general, many of these studies have relied primarily on parent reports of victimization. This is problematic because studies of typical adolescents have shown self-reports of peer victimization to be especially important for understanding peer victimization in general, as well as for understanding the links between peer victimization and internalizing symptoms (Hawker & Boulton 2000; Reijntjes et al. 2010; Siegel et al. 2009; Sweeting et al. 2006). This should not be surprising since experiences of peer victimization in adolescence are most likely to occur when the parent is not present to witness it or to protect their child. Thus, it is reasonable to expect that self-reported experiences of peer victimization, separate from what is reported by parents, would also be important for understanding internalizing problems in adolescents with ASD.
To address this limitation of previous studies, the current study used both parent- and adolescent-reports to examine the link between peer victimization and internalizing symptoms. We focused on the specific period of adolescence because this is a time when the social world is changing and the effects of peer victimization become more apparent (Boivin et al. 2010; Nansel et al. 2001). Within this age group, we also chose to limit our sample to individuals with fluent language. The importance of focusing on psychological adjustment is particularly apparent in individuals with fluent language who represent one of the fastest growing sub-groups of individuals with ASD (Lord and Bishop 2010), and for whom comorbid mental health symptoms can sometimes cause as much impairment as other ASD-related difficulties (Raja et al. 2011). These adolescents are thought to be especially vulnerable to the effects of negative peer experiences for two reasons. One, they are more likely to be integrated into larger social networks because of their higher language skills. This in turn makes it less likely that parents are able to observe their child’s social interactions and increases the likelihood that the children will experience negative social interactions due to increased exposure to the peer group. Two, because of their higher cognitive and language abilities, they may be more likely to be able to recognize their difficulties with peers. For example, previous research has shown that, when actually experiencing peer victimization, adolescents with ASD who have average IQ were just as likely to accurately interpret and understand the experience as victimization as adolescents without ASD (van Roekel et al. 2010).
Since there is currently no validated self-report measure of peer victimization for adolescents with ASD, the first goal of the current study was to validate such a measure. To do this, a group of adolescents with ASD who had fluent language abilities completed a validated, self-report measure of peer victimization previously utilized in studies of typically developing adolescents (Schwartz et al. 2002). The original items for the measure covered multiple types of peer victimization, including verbal, relational, and physical found in studies of typical adolescents (Schwartz et al. 2002; You and Bellmore 2012) and in those with ASD (Storch et al. 2012). Verbal victimization involves name-calling, teasing, and saying derogatory things about another person. Examples of relational victimization include gossiping, spreading rumors, and talking about others when they are not around. Physical victimization refers to actions such as hitting, kicking, punching, and shoving. While these studies measure these multiple forms of peer victimization, they often collapse across the types and focus on a total victimization score even though certain types of peer victimization have been shown to be more important for understanding psychological health than other types of victimization. For instance, verbal victimization has been shown to be particularly important for predicting increases in depressive symptoms over time especially in groups that are at risk for experiencing verbal victimization, such as obese and overweight adolescents (Adams and Cantin 2013; Adams and Bukowski 2008).
To ensure that the current study also addressed instances of peer victimization that might be particular to those with ASD, new items were created for the current study to capture aspects of peer victimization thought to be germane to adolescents with ASD. Unlike the items designed to assess relational victimization, these new social victimization items focused on adolescents’ experiences of being victimized for social difficulties that are particular to their disorder, such as being made fun of when trying to talk to a group of peers, or being teased for trying to be friends with someone. These social victimization items are different from relational victimization in that they focus on specific social difficulties that affect most adolescents with ASD. In contrast, relational victimization assesses adolescents’ experiences of damage to or threats to damage their peer reputations, including relationships and acceptance (Crick et al. 1999; Young et al. 2006).
In an additional step of validating the self-report measure of peer victimization while gaining insight into its links to psychological health, we examined the associations between peer victimization and internalizing symptoms. These analyses accounted for both self- and parent-reports of peer victimization and internalizing symptoms to test if self-reports provided additional value above and beyond parent-reports of peer victimization. Finally, a secondary aim of the current study was to examine the associations between specific behavioral characteristics of ASD and peer victimization. In addition to providing information for validating the self-report measure, these analyses represented a first step in understanding what behavioral characteristics might put adolescents with ASD at risk for being peer victimized.
Method
Participants
Participants included 54 adolescent boys and one of their biological parents (N = 52), adoptive parents (N = 1), or grandparents (N = 1). Participants were recruited from existing participant registries (see “Recruitment” section below). The mean age of the sample was 14.62 years (SD = 2.25; range 10.39–17.99 years) and was primarily Caucasian (92.6 % Caucasian, Black 3.7 %, Asian 1.9 %, Bi-racial 1.9 %). Parental reports of family income revealed that 26 % made less than $50,000 a year, 46 % made between $50,000 and $100,000 a year, and 28 % made over $100,000. It should be mentioned that there were no significant correlations between age or income (all rs < .11, p ns) and any study measures and t-tests found no differences between Caucasians and the other ethnicities for any of the study measures (ts < 1.03, p ns).
Parents confirmed diagnoses of autism-related disorders during a telephone pre-screening or background history measure. Frequencies of specific autism-related disorders revealed that 21 (38.9 %) adolescents had been diagnosed with Asperger’s Disorder, 22 (40.7 %) with autism, 9 (16.7 %) with Pervasive Developmental Disorder, Not Otherwise Specified (PDD-NOS), and 2 (3.7 %) with multiple ASD diagnoses. Parents also reported the age at which their adolescent was diagnosed, with the youngest reported age of 1 year and the oldest reported age of 11 years. The average reported age at diagnosis was 6.40 years (SD = 2.55). See Table 1 for description of participant characteristics by diagnosis.
Procedures
Recruitment
The majority of participants were recruited from existing research (50.0 %, n = 27) or clinical (41.7 %, n = 22) registries, which accounted for 90.7 % of the study sample. The individuals recruited from these registries had previously undergone a comprehensive assessment through either a specialty diagnostic clinic in a division of developmental-behavioral pediatrics or an ASD focused research project within a large pediatric hospital. These assessments included a parent interview and questionnaires, as well as cognitive testing, language testing, and the Autism Diagnostic Observation Schedule (ADOS). Diagnoses of ASD were made by a developmental pediatrician or a clinical psychologist on the basis of all information obtained during the evaluation. Potential participants identified from the registries were mailed letters that described the study and instructed families to call project staff if they were interested in participating. Follow-up phone calls were made approximately 2 weeks after the letters were sent. The remaining five participants (9.3 % of the study sample) were recruited via study flyers posted in clinics and treatment areas that served patients with ASD or on the hospital’s research website, or distributed at community events. These participants all had a previous diagnosis of ASD made by a developmental pediatrician or clinical psychologist from the same developmental behavioral pediatric clinic as those recruited from the registries. To confirm diagnoses for the five participants not recruited from one of the registries, scores on the parent-reported Social Communication Questionnaire, Lifetime Version (SCQ; Rutter et al. 2003) were examined. The SCQ is a 40-item survey to which parents respond “yes” or “no” to each item describing a symptom associated with ASD. The suggested cut-off score of 15 on the SCQ total score is used to identify individuals with an ASD. All five participants not recruited from existing registries exceeded cut-offs on the SCQ (M = 21.60, SD = 3.58). Analyses were run only with participants recruited from research registries (and thus were known to have undergone comprehensive diagnostic evaluations) and then with all participants. There were no differences in the findings.
A prescreening interview was conducted to ensure that all adolescent participants met the following inclusion criteria: (a) previous diagnosis of an ASD, including autism, Asperger’s Disorder, or PDD-NOS, (b) English-speaking, (c) fluent language abilities, which was defined as using complex sentences on a daily basis, and (d) between the ages of 10 and 17. Recruited families were excluded from the study if their adolescent met one of the following exclusion criteria: (a) had not previously been diagnosed with ASD, (b) insufficient language abilities (i.e., complex sentences not used on a daily basis), (c) known genetic disorder (e.g., Down Syndrome, Fragile X Syndrome), (d) deafness, (e) blindness, (f) serious motor impairment, or (g) adolescent or parent/guardian did not speak English. During the prescreening interview, seven families were excluded for the following reasons: outside the age range (N = 1); no diagnosis of ASD (N = 2); insufficient language abilities (N = 2); low IQ and parent suspected that he would not be able to understand the questions (N = 1); and could not walk independently (N = 1). In addition, research staff identified two screen fails at the beginning of the study visit; one was determined to not have fluent language and another could not understand the rating scales used in study measures. These seven families and two screen fails are not included in the final study sample of 54 adolescent boys with ASD. Based on direct experiences with the participants, study staff members reported that participants easily completed all study questions and had strong verbal skills, adding further support to the strength of our recruitment and prescreening strategies.
Study Visit
Adolescents who met the prescreening criteria listed above (see “Recruitment” section) were invited to the research laboratory along with at least one parent or legal guardian, for a one-hour study visit; this included all 54 families for the study sample. All visits took place in hospital clinic space. With the parent present, a trained research assistant explained the study, including issues of privacy and confidentiality of responses, and that participation was voluntary. A consent form was signed by the parent or legal guardian and an assent form was signed by the adolescent. The parent or legal guardian completed a set of surveys (see “Parent measures” below) in a separate room from the adolescent. For the adolescent, a research assistant was present to read each item on every measure (see “Adolescent measures” below), and the adolescent made his chosen response by marking it on the paper or indicating which response he wanted the research assistant to mark. Eight of the participants (15 %) asked to not have the items read to them and completed the surveys successfully on their own. Because there was concern that some adolescents might have difficulty completing the surveys, those helping the adolescent complete the surveys were instructed to note any questions or confusion that adolescents expressed while completing study measures. Upon completion of the adolescent and parent surveys, each family received a $20 gift card as a token of appreciation.
Measures
Adolescent Measures
Adolescents completed three surveys about peer victimization and psychosocial difficulties. Except for the one adolescent who was excluded due to lack of understanding of the ratings scales (see “Recruitment” section), study staff reported that participants generally understood the instructions and rating scales for each survey. On average, adolescents took approximately 50 min to complete the surveys.
The Self-report of Peer Victimization is a 12-item scale containing several types of overt and indirect peer victimization, modified from the Schwartz Peer Victimization Scale (SPVS; Schwartz et al., 2002). Adolescents indicated how often they had experienced each type of victimization using a seven-point scale, where a 1 = “Never happens to me”, 2 = “Happens to me once a year”, 3 = “Happens to me 2 or 3 times a year”, 4 = “Happens to me 4–6 times a year”, 5 = “Happens once or twice a month”, 6 = “Happens to me once or twice a week”, and 7 = “Happens to me almost every day.” Four subscales were created by summing and averaging scores for completed items. The Verbal victimization subscale comprised four items (e.g., “How often do other kids call you names that hurt his feelings?”), the Relational victimization subscale consisted of two items (e.g., “How often do other kids gossip or say mean things about you?”), and the Physical victimization subscale comprised two items (e.g., “How often do other kids hit or push you?”). Three items were added for the current study to assess peer victimization in social situations thought to be particularly relevant to adolescents with ASD (e.g., How often do you get teased or made fun of when you try to hang out with other kids?; How often do other kids say mean things to you when you try to be their friend?; How often do other kids make fun of or tease you when you talk to them?). More information about this scale is detailed in the “Results” section.
The Youth Self-Report (YSR; Achenbach 2001a) is a 112-item self-report measure designed to assess social and behavioral competencies and difficulties. Due to their sensitive nature, four items about suicidal ideation and sexuality were not included in the present study. Thus, adolescents responded to a total of 108 items indicating how true each statement was for them over the past six months using a three-point scale ranging from 0 = “Not true” to 2 = “Very true or often true”.
For this study, we were interested in the broad-band raw score of Internalizing Problems, which was created by summing and averaging relevant items, so scores could range from 0 to 2. The Internalizing Problems score comprised 30 items covering self-ratings of anxious/depressed, withdrawn, and somatic symptoms. Internal consistency estimates for the Internalizing Problems raw score (α = 0.90) was good. Study staff reported that adolescents did not have difficulty understanding any of the items on the YSR.
The Children’s Depression Inventory (CDI; Kovacs 1992) is a 27-item self-report survey, used to assess cognitive and behavioral symptoms of depression. The suicidal ideation item was not included in the present study due to the sensitive nature of the item. For the remaining 26 items, participants were presented with a set of three statements and asked to select which described them best over the past 2 months. Chosen responses were coded as a 0, 1, or 2, with a higher score indicating higher depressive symptomatology. Scores were summed and averaged across the 26 items to create a total score, which could range from 0 to 2, reflecting overall depressive symptoms. Internal consistency of the total score was good (α = 0.88). Study staff reported that adolescents did not have difficulty understanding any of the items on the CDI.
Parent Measures
Parents completed a background history form, which included age, ethnicity and race of the adolescent and biological parents/primary caregivers, as well as educational level, occupation(s), and income of the primary caregiver(s). Several items also asked about the previous ASD diagnosis the adolescent had received.
The Parent-Report of Peer Victimization scale is a 12-item measure with items identical to the previously described Self-report of Peer Victimization scale completed by the adolescent. All items were re-worded such that parents reported about their child’s victimization experiences. Parents indicated how often their adolescent experienced each type of victimization using the same seven-point scale as the adolescent measure, which ranged from 1 = “Never happens to my child” to 7 = “Happens to my child almost every day”.
To maintain consistency with the adolescent reported victimization survey, subscales similar to those created for the adolescent self-report survey were created for the parent-reported victimization survey. Verbal victimization comprised four items (e.g., “How often do other kids call your child names that hurt your feelings?”), whereas Relational victimization consisted of two items (e.g., “How often do other kids gossip or say mean things about your child?”). Physical victimization comprised two items (e.g., “How often do other kids hit or push your child?”), and Social victimization comprised the three new items that were specific to social behaviors (e.g., How often do other kids make fun of the way your child acts?). All subscales demonstrated adequate internal consistency; Cronbach α’s ranged from 0.78 to 0.95.
The Child Behavior Checklist (CBCL; Achenbach 2001b) is a 113-item parent-report measure designed to assess social and behavioral competencies and difficulties. Parents responded to all items indicating how true each statement was for their adolescent over the past 6 months using a three-point scale ranging from 0 = “Not true” to 2 = “Very true or often true”.
As with the YSR, we were interested in the Internalizing Problems raw scale score, which could range from 0 to 2. The Internalizing Problems scale included 32 items covering parent-ratings of anxious/depressed, withdrawn, and somatic symptoms, which were summed and averaged. Internal consistency estimate for the Internalizing Problems raw score (α = 0.86) was excellent.
The Social Responsiveness Scale (SRS; Constantino and Gruber 2005) is a 65-item survey designed as a continuous measure of ASD symptomatology. Parents rated how well each symptom described their child using a four-point Likert scale ranging from 0 = “not true” to 3 = “almost always true”. All items were summed to create a total score. Internal consistency across the items for the total score was excellent (α = 0.95). In addition, T-scores were computed and ranged from 55 to greater than 95.
Parents completed the Repetitive Behavior Scale—Revised (RBS-R; Bodfish et al. 2000) with regard to the frequency and severity of their child’s restricted and repetitive behaviors. The RBS-R consists of 43 items on which parents rated their child using a four-point Likert scale ranging from 0 = “behavior does not occur” to 3 = “behavior occurs and is a severe problem”. All items were summed to create a total score. Internal consistency for total score was excellent (α = 0.94.).
Results
Validating the Self-Report Measure of Peer Victimization
To validate the self-report measure of peer victimization, the inter-item reliabilities were tested for each subscale and the notes from study staff concerning participants’ responses to the items were reviewed. Next, principal components analysis was conducted to determine if the original factor structures could be replicated, and then inter-rater reliability was examined by running correlations between self-reports and parent-reports for each subscale. Finally, to measure convergent validity, correlations were tested within each reporter across subscales and across reporter across each subscale.
As seen in Table 2, the Cronbach’s alphas suggest that the subscales were reliable in this sample with the exception of the adolescent-reported physical victimization subscale. In addition, study staff found that adolescents had difficulty with an item in the relational victimization subscale. Though the internal consistency for this subscale was adequate, adolescents frequently expressed confusion about the item, “How often do other kids gossip or say mean things about you when you are not around?” Specifically, adolescents asked for clarification about how they were supposed to know if other kids said things behind their backs given that they were not there to hear what the other kids were saying. Also, it should be mentioned that the low Cronbach’s alpha for the physical victimization subscale is most likely due to adolescents reporting very low rates of this type of victimization (66 % reported physical victimization never happened).
Next, principal components analysis for the 12 items replicated the measure’s original three factors and the new social factor with the varimax rotation resulting in all loadings for each factor to be above 0.64 with no cross-loadings across factors above 0.42. In addition, all eigenvalues were over one and explained 78.1 % of the total variance.
Correlations in Table 2 were examined between all of the peer victimization subscales for both adolescent- and parent-reports as an indication of inter-rater reliability and convergent validity. Inter-rater reliability was found for most of the subscales. Across the two reporters for the same types of peer victimization, verbal, physical, and social victimization were significantly correlated (e.g., adolescent-reported verbal victimization was correlated with parent-reported verbal victimization), but relational victimization was not. Convergent validity was also found across the subscales with the exception of physical victimization. Within each reporter, each type of peer victimization was significantly correlated with each of the other types of peer victimization (e.g., for the adolescent-reports, verbal victimization was associated with each of the other three types of adolescent-reported peer victimization). Across the two reporters for different types of peer victimization, all types of peer victimization were correlated with each other except for adolescent-reports of physical victimization. Adolescent-reports of physical victimization were not correlated with parent reports of verbal, relational, or social peer victimization.
Preliminary Analyses
Descriptive statistics are presented for all study measures in Table 3. All measures reflected a normal distribution (skewness < 1.70; kurtosis < 2.07). Preliminary analyses examined the means and standard deviations for the adolescent- and parent- reports of peer victimization. Paired samples t-tests examined differences between adolescent-reports and parent-reports for each type of peer victimization (See Table 4). These analyses found that for verbal, relational, and social types of peer victimization, parents reported higher rates of victimization than adolescents. There were no differences found between the two reporters for physical victimization. Next, repeated measures ANOVAs examined differences in rates between each type of victimization within each reporter (See Table 4). For both adolescent- and parent-reports the same pattern emerged. Higher rates were reported for verbal and relational victimization than for physical and social victimization, and higher rates were reported for social victimization than for physical victimization. There were no differences between reported rates of verbal and relational victimization.
Associations Between Peer Victimization and Internalizing Symptoms
Before the associations were examined between peer victimization and internalizing symptoms, a basic measurement model was used to create a latent variable for internalizing symptoms. For the latent variable, the CDI, the YSR internalizing scale, and the CBCL internalizing scale were used as indicators. This basic measurement model was found to have a good fit (χ2 = 67.20, p < .01; CFI = 0.99; TLI = 0.98; RMESA 90 % CI [0.01–0.02]). Standardized loadings for each of the three indicators were all significant (p > .001) and above 0.40. This latent variable was used in the models that follow.
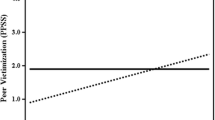
Adolescent-Reports of Peer Victimization
Four SEM models examined the associations between adolescent-reports of peer victimization and the latent measure of internalizing symptoms for each type of peer victimization. For each of the models (See Fig. 1), the effect of one of the types of victimization on the latent factor of internalizing symptoms was tested while controlling for the effects of age, family income, and SRS total scores. The SRS total score was included as a measure of parent-reported ASD symptoms, a possible confounding variable since it could be associated with both peer victimization and internalizing symptoms. The RBS-R total score was also examined as a control measure of parent-reported ASD symptoms, but preliminary models found that the RBS-R was not associated with the internalizing latent construct in any of the adolescent- or parent-report models. Thus, it was not entered into the final models. All models were found to fit the data (χ2 > 105.73, p < .01; CFIs > 0.92; TLIs > 0.91; RMESA 90 % CI [0.07–0.09]). As seen in Fig. 1, all four types of adolescent-reported peer victimization had strong associations with the internalizing symptoms latent factor (standardized coefficients ranged from 0.50 to 0.68).
Standardized coefficients for models testing the separate associations of self-reported and parent-reported peer victimization with a latent construct of internalizing symptoms. *p < .05. **p < .01. ***p < .001. The internalizing symptoms latent variable is comprised of the CDI total score, YSR internalizing score, and CBCL internalizing score. None of the control variables were significant across all models (all ps > .11). Across the four models, the ranges of the standardized coefficients for each control variable are as follows: Age 0.01–0.03, Family Income −10 to −05, and SRS 0.18 to 0.22
Parent-Reports of Peer Victimization
Four SEM models examined the associations between parent-reports of peer victimization and the latent measure of internalizing symptoms for each type of peer victimization. For each of the models (See Fig. 1), the effect of one of the types of victimization on the latent factor of internalizing symptoms was tested while controlling for the effects of age, family income, and SRS total score. As in the adolescent- report model, the SRS was included as a measure of parent-reported ASD symptoms, a possible confounding variable since it could be associated with both peer victimization and internalizing symptoms. All models were found to fit the data (χ2 > 85.73, p < .01; CFIs > 0.94; TLIs > 0.93; RMESA 90 % CI [0.05–0.07]). As seen in Fig. 1, only the parent-report of physical victimization was significantly associated with the internalizing latent factor.
Adolescent- and Parent-Reports of Peer Victimization Examined Simultaneously
Four SEM models examined the associations of both adolescent- and parent-reports of peer victimization and the latent measure of internalizing symptoms for each type of peer victimization. For each of the models (See Fig. 2), the effects of both adolescent- and parent-reports of one of the types of victimization simultaneously on the latent factor of internalizing symptoms were tested while controlling for the effects of age, family income, and SRS total score. In addition, the adolescent- and parent-reports of peer victimization were correlated in each model. All models were found to fit the data (χ2 > 108.72, p < .01; CFIs > 0.95; TLIs > 0.95; RMESA 90 % CI [0.06–0.10]). For each of the four types of peer victimization (See Fig. 2), the adolescent-reports of peer victimization were significantly associated with the internalizing latent factor, but the parent-reports of victimization were not when simultaneously accounting for both reporters.
Standardized coefficients for models testing the associations of self-reported and parent-reported peer victimization with a latent construct of internalizing symptoms. *p < .05. **p < .01. ***p < .001. The internalizing symptoms latent variable is comprised of the CDI total score, YSR internalizing score, and CBCL internalizing score. None of the control variables were significant across all models (all ps > .09). Across the four models, the ranges of the standardized coefficients for each control variable are as follows: Age 0.02–0.04, Family Income −11 to −04, and SRS 0.14 to 0.23
Associations Between Behavioral Characteristics and Peer Victimization
Partial correlations were conducted to examine the associations between behavioral characteristics and peer victimization. Specifically, partial correlations were run between each of the four types of victimization for each reporter and scores on the SRS and RBS-R, while controlling for age and family income (See Table 5). SRS total score was associated with parent-reports of all four types of victimization and only adolescent-reports of verbal and social victimization. The RBS-R was associated with parent-reports of all four types of victimization, but not with any types of adolescent-reported peer victimization.
Discussion
The current study examined the relationship between peer victimization and internalizing symptoms in adolescents with ASD using both parent- and adolescent-reports. Peer victimization is known to be important in predicting internalizing symptoms in typically developing adolescents, and recent evidence suggests that this association holds true in adolescents with ASD, as well. However, previous studies of adolescents with ASD have relied primarily on parent-report, which limits our understanding of how the actual experiences of adolescents are related to internalizing symptoms.
To address this problem, the first objective of the current study was to explore the validity of self-reports of peer victimization in verbally fluent adolescents with ASD. The results were mixed depending on the type of peer victimization examined. First, parents reported higher rates of verbal, relational, and social victimization than did adolescents. Comparing these means to the actual scale for peer victimization, the mean for adolescents falls in the range of peer victimization happening to them once to 2–3 times a year while the parent mean falls in the range of happening 2–3 times to 4–6 times a year, which translates to higher rates than found from self-reports in the general population (Nansel et al. 2001). While this suggests the rates are higher for those with ASD, future studies will need to directly test differences in peer victimization rates using both typical adolescents and adolescents with ASD as participants to draw firmer conclusions. In addition, for verbal and social types of victimization, there was clear evidence to support that this group of adolescents can indeed provide valid reports about their perceptions of experiences of peer victimization. For both of these types of victimization, there was high internal consistency across the items for each scale, there were no reports of the adolescent having difficulty completing the items on either scale, the self-reports were correlated with parent reports of the same type of victimization, and the self-reports demonstrated associations with other variables similar to those reported in previous studies with typical adolescents (e.g., internalizing symptoms).
On the other hand, there were some concerns with respect to the validity of adolescent-reports of relational and physical victimization. Though adolescents did not report having difficulty with the items on the physical victimization scale, and this scale was correlated with parent-reports of physical victimization, the internal consistency across the items on this scale was low, and it was not correlated with parent-reports of verbal, relational, or social victimization (all other types of victimization were associated across reporters). For relational victimization, the internal consistency across the items was adequate and the construct was associated with other variables shown to be important in previous studies of typical adolescents, but study staff reported that some adolescents had difficulty conceptually understanding certain items, and self-reports of relational victimization were not correlated with parent-reports of relational victimization. Together, these findings suggest that there should be more confidence in interpreting the findings for adolescent-reports of verbal and social victimization than relational or physical victimization in terms of null effects and the relative size of the effects across the types of peer victimization for both the correlations and the SEM findings. It should be mentioned that the minimal ratio of number of subjects to number of items considered ideal for a principal components analysis (5:1) was not met for the met for the current study (4.5:1). While there was other support for the validity of the peer victimization scale (e.g., adequate internal reliability among the items), future studies will need to ensure a higher ratio when testing the factor structure of this scale. Along the same line, one should consider the relatively small sample when interpreting the findings in general, especially in terms of the statistical power for the study.
Another goal of the current study was to examine the link between peer victimization and internalizing symptoms in verbally fluent adolescents with ASD. In general, it was found that adolescent-reports of peer victimization were associated with internalizing symptoms, whereas parent-reports were not (with the exception of physical victimization). The pattern of findings for the adolescent-reports was the same before and after accounting for the parent-reports. This is not to say that parent-reports of peer victimization are not important, but rather that adolescents’ perceptions of these peer experiences seem to be more closely related to internalizing symptoms. Indeed, studies in typically developing adolescents have shown that self-reports, in contrast to other reports, are particularly important for predicting internalizing problems (Hawker and Boulton 2000). It has been suggested that rather than viewing multiple reporters as one being better than the other, it might be better to think of each reporter as having their own separate predictive validity in terms of different outcomes, since each reporter observes or experiences the behavior in different contexts (Achenbach et al. 1987). In any case, it is not constructive to try to interpret null effects; so it will be more fruitful to focus on the adolescent-report findings in the current study rather than on the parent-report null effects.
In this respect, the findings where both types of reports were examined simultaneously show that experiences of peer victimization that are uniquely perceived by the adolescent, separate from those perceived by the parent, are especially important for understanding the relationship between peer victimization and internalizing symptoms. This suggests that there is a need to understand and focus on reducing peer victimization that occurs outside the purview of parents. This may be especially the case for adolescents with ASD with higher language abilities who are more likely to be integrated into larger social networks where parents are not necessarily able to observe social interactions. To measure these types of experiences and other experiences where parents may not have direct access future studies will not only want to use self-reports but will also want to use teachers and peers as reporters. There is a long line of research with typically developing adolescents that has found peer reports to be particularly important in understanding the adolescent social world (Rubin et al. 2006). Furthermore, adolescents with ASD tend to have higher rates of depression and anxiety compared to typical adolescents (Leyfer et al. 2006; van Steensel et al. 2011). The results of the current study suggest that self-reported experiences of peer victimization may help to explain the higher rates of internalizing difficulties in adolescents with ASD. Thus, a greater understanding of the adolescent’s own perspective could provide insights about how to refine interventions and treatments for adolescents who are most risk for developing depression and/or anxiety in this group.
When interpreting the relationships between peer victimization and internalizing symptoms in this sample, it is important to consider that the cross-sectional design of this study does not allow one to know the direction of association. This is especially important considering that internalizing symptoms have also been shown to predict peer victimization (Reijntjes et al. 2010). In other words, it is not known if victimization leads to internalizing symptoms or if internalizing symptoms leads to victimization. In typically developing adolescents, both have been shown to be true. Future studies will need to employ longitudinal designs to be able to better elucidate the nature of this association. Cross-sectional designs can also lead to issues of shared-method variance, which is a concern for those partial correlations conducted between measures completed by the same person, but not for the associations found with the latent variable for internalizing symptoms. The latent construct of internalizing symptoms was composed of both adolescent- and parent-reports of internalizing symptoms and thus can be interpreted as the overlap of the perceptions of the adolescent’s internalizing symptoms between both reporters. Special attention should also be given to the strength of the associations. Since previous studies have found high rates of peer victimization in adolescents with ASD (Cappadocia et al. 2012; Little 2002), the strong effects between self-reports of peer victimization and internalizing symptoms and the weak effects of parent-reports of peer victimization on internalizing symptoms reported here suggest that it is those adolescents who are actually aware of these negative experiences who are most at risk. In other words, it is clear that this group is often targeted for peer victimization, but peer victimization is only associated with internalizing symptoms when adolescents actually perceive that they are being targeted. While this may seem intuitive, it suggests that interventions that focus on internalizing issues in this group may want to focus their efforts on adolescents’ perceptions of peer experiences, both negative and positive. It also underscores the importance of gathering information about perceptions of peer experiences directly from the adolescent, as well as investigating processes, such as self-esteem and the hypothalamic–pituitary–adrenal axis, that may help to explain the importance of self-perceptions of these experiences found in other studies of adolescents without ASD (Adams and Bukowski 2008; Adams et al. 2011).
In terms of individual characteristics and the relationship with peer victimization, there were different patterns depending on the reporter. Adolescent- and parent-reports of verbal and social victimization were most consistently associated with SRS total scores. This suggests that adolescents who are reported to exhibit higher levels of ASD-related symptoms and behaviors on the SRS may be particularly likely to be victimized by their peers. On the other hand, restricted and repetitive behaviors on the RBS-R were only associated with parent-reports of peer victimization. Importantly, as mentioned above, one must be cautious of issues of shared-method variance when interpreting the findings from the partial correlations in those cases where the partial correlation is between two variables reported by the same person. Thus, in order to better understand how individual characteristics of adolescents with ASD, such as ASD symptom severity or behavior problems, are related to peer victimization, future studies should employ other reporters such as teachers or peers in the classroom. Not only would teacher- and peer-reports of experiences and behaviors be important to combat issues of shared-method variance, but teachers and peers also have access to different peer contexts than parents, resulting in a more complete view of the adolescent’s social world.
An important limitation of the current study is lack of access to more comprehensive, current phenotypic data, such as IQ or ADOS scores or information about psychiatric comorbidities. Although all of the adolescents in the current study had been previously diagnosed with ASD by a developmental pediatrician or a psychologist, it would have been preferable to conduct updated diagnostic evaluations of adolescents upon entry to this study. This would allow for more detailed examinations of the associations between individual adolescent characteristics, peer victimization, and internalizing symptoms. In addition, ensuring that all participants met a minimum IQ cut-off would increase confidence that they were able to comprehend the questionnaires, though comprehension did not appear to be an issue for participants included in the current study based on the observations of the examiners. Future studies will want to include current ADOS and IQ scores to have a better understanding of the participants as well as to determine whether higher functioning adolescents with ASD are worse off when it comes to internalizing problems. In addition, items of a sexual nature and items concerning suicide were removed from some of the internalizing scales for the current study. Schools asked for these items to be removed as a condition of a future data collection for the current larger project. Overall, the findings should be interpreted in light of these omitted items as the inclusion of these items could help to further identify those adolescents who are most at risk for suicidal thoughts and would need to be referred to an appropriate clinical resource. The findings in terms of internalizing symptoms should also be interpreted in the context of the large age range of the participants given that internalizing problems may manifest differently across this age range.
Conclusion
The vast majority of individuals diagnosed with ASD in childhood continue to experience substantial ASD-related impairments throughout their lives (Howlin et al. 2004; Seltzer et al. 2003). Therefore, in order to meet the needs of individuals with ASD into adolescence and adulthood, it is necessary to consider ways of promoting psychological adjustment and well-being even in the presence of continued social-communication challenges. Importantly, the current study found evidence that peer victimization may be an important factor in understanding psychological health for adolescents with ASD and that it is especially important to account for the adolescent’s perceptions of these negative events when exploring links with internalizing symptoms.
References
Achenbach, T. M. (2001a). Youth self report (YSR). Burlington, VT: University of Vermont Department of Psychiatry.
Achenbach, T. M. (2001b). The child behavior checklist (CBCL). Burlington, VT: University of Vermont Department of Psychiatry.
Achenbach, T. M., McConaughy, S. H., & Howell, C. T. (1987). Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin, 101, 213–232. doi:10.1037/0033-2909.101.2.213.
Adams, R. E., & Bukowski, W. M. (2008). Peer victimization as a predictor of depression and body mass index in obese and non-obese adolescents. Journal of Child Psychology and Psychiatry, 49, 858–866. doi:10.1111/j.1469-7610.2008.01886.x.
Adams, R. E., & Cantin, S. (2013). Self-disclosure in friendships as the moderator of the association between peer victimization and depressive symptoms in overweight adolescents. Journal of Early Adolescence, 33, 341–362. doi:10.1177/0272431612441068.
Adams, R. E., Santo, J. B., & Bukowski, W. M. (2011). The presence of a best friend buffers the effects of negative experiences. Developmental Psychology, 47, 1786–1791. doi:10.1037/a0025401.
Bodfish, J. W., Symons, F. J., Parker, D. E., & Lewis, M. H. (2000). Varieties of repetitive behavior in autism: Comparisons to mental retardation. Journal of Autism and Developmental Disorders, 30, 237–243. doi:10.1023/A:1005596502855.
Boivin, M., Petitclerc, A., Feng, B., & Barker, E. D. (2010). The developmental trajectories of peer victimization in middle to late childhood and the changing nature of their behavioral correlates. Merrill-Palmer Quarterly, 56, 231–260.
Cappadocia, M. C., Weiss, J. A., & Pepler, D. (2012). Bullying experiences among children and youth with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42, 266–277. doi:10.1007/s10803-011-1241-x.
Constantino, J. N., & Gruber, C. P. (2005). Social responsiveness scale (SRS). Los Angeles, CA: Western Psychological Services.
Costello, E. J., Egger, H., & Angold, A. (2005). 10-year research update review: The epidemiology of child and adolescent psychiatric disorders: I. Methods and Public Health Burden. Journal of the American Academy of Child and Adolescent Psychiatry, 44, 972–986. doi:10.1097/01.chi.0000172552.415969.6f.
Crick, N. R., Wellman, N. E., Casas, J. F., O’Brien, K. M., Nelson, D. A., Grotpeter, J. K., et al. (1999). Childhood aggression and gender: A new look at an old problem. In D. Bernstein (Ed.), Nebraska symposium on motivation (pp. 75–141). Lincoln, NE: University of Nebraska Press.
Ghandour, R. M., Kogan, M. D., Blumberg, S. J., & Perry, D. G. (2010). Prevalence and correlates of internalizing mental health symptoms among CSHCN. Pediatrics, 125, e269–e277. doi:10.1542/peds.2009-0622.
Ghaziuddin, M., Ghaziuddin, N., & Greden, J. (2002). Depression in persons with autism: Implications for research and clinical care. Journal of Autism and Developmental Disorders, 32(4), 299–306. doi:10.1023/a:1016330802348.
Ghaziuddin, M., Weidmer-Mikhail, E., & Ghaziuddin, N. (1998). Comorbidity of Asperger syndrome: A preliminary report. Journal of Intellectual Disability Research, 42(4), 279–283. doi:10.1046/j.1365-2788.1998.00065.x.
Hawker, D. S. J., & Boulton, M. J. (2000). Twenty years’ research on peer victimization and psychosocial maladjustment: A meta-analytic review of cross-sectional studies. Journal of Child Psychology and Psychiatry, 41, 441–455. doi:10.1111/1469-7610.00629.
Howlin, P., Goode, S., Hutton, J., & Rutter, M. (2004). Adult outcome for children with autism. Journal of Child Psychology and Psychiatry, 45(2), 212–229. doi:10.1111/j.1469-7610.2004.00215.x.
Hurtig, T., Kuusikko, S., Mattila, M., Haapsamo, H., Ebeling, H., Jussila, K., et al. (2009). Multi-informant reports of psychiatric symptoms among high-functioning adolescents with Asperger syndrome or autism. Autism, 13(6), 583–598. doi:10.1177/1362361309335719.
Kovacs, M. (1992). Children’s depression inventory manual. Los Angeles: Western Psychological Services.
Leyfer, O. T., Folstein, S. E., Bacalman, S., Davis, N. O., Dinh, E., Morgan, J., et al. (2006). Comorbid psychiatric disorders in children with Autism: Interview development and rates of disorders. Journal of Autism and Developmental Disorders, 36(7), 849–861. doi:10.1007/s10803-006-0123-0.
Little, L. (2002). Middle-class mothers’ perceptions of peer and sibling victimization among children with Asperger’s syndrome and nonverbal learning disorders. Issues in Comprehensive Pediatric Nursing, 25, 43–57. doi:10.1080/014608602753504847.
Lord, C., & Bishop, S. L. (2010). Autism spectrum disorders: Diagnosis, prevalence, and services for children and families. Society for Research in Child Development Social Policy Report, 24(2), 1–27.
Nansel, T. R., Overpeck, M., Pilla, R. S., Ruan, J., Simons-Morton, B., & Scheidt, P. (2001). Bullying behaviors among US youth: Prevalence and association with psychosocial adjustment. Journal of American Medical Association, 285, 2094–2100. doi:10.1001/jama.285.16.2094.
Raja, M., Azzoni, A., & Frustaci, A. (2011). Autism spectrum disorders and suicidality. Clinical Practice and Epidemiology in Mental Health, 7. doi:10.2174/1745017901107010097.
Reijntjes, A., Kamphuis, J. H., Prinzie, P., & Telch, M. J. (2010). Peer victimization and internalizing problems in children: A meta-analysis of longitudinal studies. Child Abuse and Neglect, 34, 244–252. doi:10.1019/j.chiabu.2009.07.009.
Rosbrook, A., & Whittingham, K. (2010). Autistic traits in the general population: What mediates the link with depressive and anxious symptomatology? Research in Autism Spectrum Disorders, 4(3), 415–424. doi:10.1016/j.rasd.2009.10.012.
Rubin, K. H., Bukowski, W. M., & Parker, J. G. (2006). Peer interactions, relationships, and groups. In W. Damon, R. M., Lerner, & N. Eisenberg (Eds.,) Handbook of child psychology: Vol. 3. Social, emotional, and personality development, 6th ed (pp. 571–645). New York: Wiley.
Rutter, M., Bailey, A., & Lord, C. (2003). The social communication questionnaire: Manual. Los Angeles, CA: Western Psychological Services.
Schwartz, D., Farver, J. M., Chang, L., & Lee-Shin, Y. (2002). Victimization in South Korean children’s peer groups. Journal of Abnormal Child Psychology, 30, 113–125. doi:10.1023/A:1014749131245.
Seltzer, M. M., Krauss, M. W., Shattuck, P. T., Orsmond, G., Swe, A., & Lord, C. (2003). The symptoms of autism spectrum disorders in adolescence and adulthood. Journal of Autism and Developmental Disorders, 33(6), 565–581.
Siegel, R. S., La Greca, A. M., & Harrison, H. M. (2009). Peer victimization and social anxiety in adolescents: Prospective and reciprocal relationships. Journal of Youth and Adolescence, 38, 1096–1109. doi:10.1007/s10964-009-9392-1.
Sterzing, P. R., Shattuck, P. T., Narendorf, S. C., Wagner, M., & Cooper, B. P. (2012). Bullying involvement and autism spectrum disorders. Archives of Pediatrics and Adolescent Medicine, 166, 1058–1064. doi:10.1001/archpediatrics.2012.790.
Storch, E. A., Larson, M. J., Ehrenreich-May, J., Arnold, E. B., Jones, A. M., Renno, P., et al. (2012). Peer victimization in youth with autism spectrum disorders and co-occurring anxiety: Relations with psychopathology and loneliness. Journal of Developmental and Physical Disabilities, 24, 575–590. doi:10.1007/s10882-012-9290-4.
Sweeting, H., Young, R., West, P., & Der, G. (2006). Peer victimization and depression in early-mid adolescence: A longitudinal study. British Journal of Educational Psychology, 76, 577–594. doi:10.1348/000709905X49890.
van der Wal, M. F., deWit, C. A. M., & Hirasing, R. A. (2003). Psychosocial health among young victims and offenders of direct and indirect bullying. Pediatrics, 111, 1312–1317.
van Roekel, E., Scholte, R. H., & Didden, R. (2010). Bullying among adolescents with autism spectrum disorders: Prevalence and perception. Journal of Autism and Developmental Disorders, 40, 63–73. doi:10.1007/s10803-009-0832-2.
van Steensel, F. J. A., Bogels, S. M., & Perrin, S. (2011). Anxiety disorders in children and adolescents with autistic spectrum disorders: A meta-analysis. Clinical Child and Family Psychology Review, 14, 302–317. doi:10.1007/s10567-011-0097-0.
You, J., & Bellmore, A. (2012). Relational peer victimization and psychosocial adjustment: The mediating role of best friendship qualities. Personal Relationships, 19, 340–353. doi:10.1111/j.1475-6811.2011.01365.x.
Young, E. L., Boye, A. E., & Nelson, D. A. (2006). Relational aggression: Understanding, identifying, and responding in schools. Psychology in the Schools, 43, 297–312. doi:10.1002/pits.20148.
Acknowledgments
The authors would like to thank Carrie Thomas and Alyssa Wendling for their assistance in recruitment and data collection.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Adams, R.E., Fredstrom, B.K., Duncan, A.W. et al. Using Self- and Parent-Reports to Test the Association Between Peer Victimization and Internalizing Symptoms in Verbally Fluent Adolescents with ASD. J Autism Dev Disord 44, 861–872 (2014). https://doi.org/10.1007/s10803-013-1938-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10803-013-1938-0