Abstract
Background
The role of mitochondrial dysfunction in the pathogenesis of inflammatory bowel diseases (IBD) is still being investigated. This study evaluated the therapeutic effect of curcumin (Cur), a polyphenolic electrophile in 2,4,6-trinitrobenzene sulfonic acid (TNBS)-induced chronic colitis and mitochondrial dysfunction, in mice.
Methods
Colitis was induced by rectal instillation to mice of 30 mg kg−1 TNBS, alone or followed by daily intraperitoneal injections of Cur 25 mg kg−1. Animals were euthanized at days 3, 7, and 14, post TNBS challenge. Colon mitochondria of control mice were treated with 5 µM Cur, and TNBS (50, 100 µM)-toxicity was evaluated by measuring swelling, respiration, and aconitase and fumarase activities. Redox status was evaluated in colon mucosa and in mitochondria.
Results
In vitro, a short-term Cur treatment controlled the dose and time dependent mitochondrial toxicity induced by TNBS, by collapsing the generation of superoxide anion and hydroperoxy lipids, rebalancing nitric oxide synthase and aconitase activities, and recoupling mitochondria. In vivo, a daily low-dose Cur abolished mice mortality which reached 27% in model group. Cur improved in a time dependent manner mucosal redox homeostasis, cell apoptosis, mucin depleted crypts and crypt abscesses by controlling prooxidant activity of myeloperoxidase and NO synthase associated to phagocytes influx, quenching hydroperoxy lipids, and reboosting GSH levels.
Conclusion
Cur, by quenching intra and extra mitochondrial ROS generation, rebalancing aconitase/fumarase and MDA/GSH ratios, and recoupling mitochondria, may support mithormesis priming and remitting in IBD.
Graphic abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) is a typical inflammatory bowel disease (IBD) affecting sensitive subjects developing chronic intestinal oxidative inflammation associated to imbalanced immune tolerance (Circu and Aw 2011; Novak and Mollen 2015). Mitochondrial stress has been suggested as a predisposing factor initiating intestinal inflammation through increase of epithelial permeability to gut microbiota (Nazli et al. 2004; Lewis and McKay 2009; Wang et al. 2014).
Mitochondria are dynamic autonomous self-replicating organelles, centrally involved in cell redox homeostasis (Murphy 2009; Handy and Loscalzo 2012; Brand 2016; Spinelli and Haigis 2018). One characteristic feature of mitochondria is to provide cells in energy by oxidative phosphorylation (OxPhos), a bioenergetic process coupling electrons transfer through the respirasomes (respiratory complexes I–IV, ETC), with the phosphorylation of ADP to ATP by ATP synthase. Physiologically, few electrons leaked out from respirasomes I and III to reduce oxygen into superoxide anion (O2·−) (Wong et al. 2017). This OxPhos by product may react with nitric oxide (NO) released by matrix NO synthase, to generate various reactive oxygen and nitrogen species (mtROS) (Murphy 2009).
The biphasic discharge of low-dose mtROS involved in eustress conditions and redox signaling pathways and high-dose mtROS causing nitro-oxidative stress, are characteristic features of mithormesis (Brand 2016; Wong et al. 2017).
Abrupt mtROS levels can cause major changes to mitochondria architecture and function (Zorov et al. 2014).
The histones free mtDNA is critically sensitive to nitro-oxidative stress, bringing cell into adaptative response, or apoptosis (Chen et al. 2005; Circu and AW 2011; Izem-Meziane et al. 2012). Also, ROS attack of polyunsaturated fatty acids of phospholipid bilayer generates hydroperoxy lipids, primarily hydroxynonenal (HNE) and malondialdehyde (MDA). These aldehydic adductors exacerbate mitochondrial permeability transition pore (mPTP) opening, leading to mitochondria uncoupling, and the collapse of mitochondrial membrane potential in the expense of ATP synthesis (Chen and Yu 1994; Bernardi et al. 2015). In addition, cardiolipin, a complex phospholipid exclusive to the inner mitochondrial membrane (IMM) leaflet, is intimately associated with respirasomes. Its ROS-dependent oxidation strongly alters the fluidity of lipid bilayer and impairs electrons transfer chain (ETC) activity (Pfeiffer et al. 2003; Yin and Zhu 2012). More, the nitrosation of iron-sulfur (Fe-S)-containing proteins such as aconitase, a redox sensitive enzyme of tri carboxylic acid (TCA) cycle and respirasomes I and III, blocks TCA cycle and respiration, resulting in bioenergetic stress (Chen et al. 2005).
Because of the multifactorial etiology of IBD, and the dose dependent side effects of classical therapies, plant-derived secondary metabolites have been successfully assayed as alternative adjuvant treatments for IBD. They include numerous chemically related compounds polyphenols, flavonoids, terpens, alkaloids, etc.
Inflammation and pain are prominent symptoms associated-disability in Crohn’s disease patients that highly impacts their quality of life (Grossi et al. 2019). Thus, in addition to their controlled use as adjuvant analgesics in chronic pain, the terpenopolyphenolic group of cannabinoids has been shown to be effective on mucosal oxidative inflammation (Millar et al. 2019; Pagano et al. 2016, 2019). They exert their pharmacological effects through the cross talk of various receptors namely, the G protein-coupled cannabinoid (CB1, CB2) receptors, and the transient receptors potential cation channel subfamily V (TRPV) (Zádor and Wollemann 2015). Likewise, curcuminoids was associated with significant reduction in the disease activity index (Szebeni et al. 2019).
Curcumin (Cur) [(1E,6E)-1,7-bis (4-hydroxy-3-methoxyphenyl)-1,6-heptadiene-3,5-dione] is the major curcuminoid antioxidant of Curcuma longa L. This low biovailable lipophilic phytochemical displays multiple molecular pharmacological effects ranging from antioxidant, anti- inflammatory and anti-infectious to sensitizing addicted cancer cells to anticancer therapy (Saha et al. 2012; Heger et al. 2013; Kunnumakkara et al. 2017). The methoxy phenols and α,β-unsaturated carbonyl (enone) electrophile backbone of Cur support its ROS scavenging capacity for superoxide anion, peroxinitrite, hydroperoxy lipids and hydroxyl radical generated by ferrous oxidation in Fenton reaction (Aggarwal et al. 2013, 2015; Kunnumakkara et al. 2017).
Cur can maintain eustress conditions through the reactivation of endogenous antioxidant system, while inhibiting ROS metabolizing enzymes primarily NADPH oxidases, NO synthases, cytochromes P450 and cyclooxygenases (Aggarwal et al. 2013, 2015; Peng et al. 2017).
This polyphenolic electrophile can modulate immune response through inhibition of redox sensitive kinases, and proinflammatory pathways involving the NLRP3 inflammasome and the transcription factorNF-kB (Aggarwal et al. 2013; Heger et al. 2013; Edwards et al. 2017; Luis et al. 2017; Hennig et al. 2018). Cur can restore adaptive cell response to nitro-oxidative stress by thiols modulation of Kelch-like ECH associated protein 1 (Keap1), an endogenous inhibitor of the nuclear factor (erythroid-derived 2)-like 2(Nrf-2). The latter is the master transcription factor of genes for NADPH and GSH biosynthesis and for antioxidant and detoxifying enzymes (Balogun et al. 2003; Li and Kong 2009; Edwards et al. 2017; Luis et al. 2017).
This study investigated the potential of Cur in a mice model of 2,4,6-trinitrobenzene sulfonic acid (TNBS)-associated colitis and mitochondrial toxicity.
Materials and methods
Ethics statement
The experiments were performed in accordance with the Ethical Committee for animals’ welfare of University of Science and Technology Houari Boumediene [ATRSS 2011 (ATRSS/PNR 08/N_305)], and with Algerian Legislation for the protection of animal experiments used in scientific purposes [Law No. 12-235/2012; Executive Decrees No. 10-80/10-90].
Adult male NMRI mice from Institut Pasteur (Algiers, Algeria), were kept under controlled conditions, and experienced with chemicals obtained from Sigma Aldrich (St Louis, MO), except otherwise indicated.
Evaluation of low-dose curcumin treatment in TNBS-induced colitis in mice
In vivo protocol
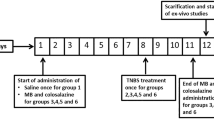
Colitis was induced in 3 model groups of mice (n = 7) instilled rectally with 100 µl TNBS (30 mg kg−1 in 30% ethanol) (Morris et al. 1989). Three additional groups of mice received daily intraperitoneal injections of curcumin (Cur, 25 mg kg−1), according to previous reports (Ukil et al. 2003; Mouzaoui et al. 2012), immediately after TNBS challenge. Mice were observed for mortality and body weight loss, and were serially euthanized by cervical translocation at days 3, 7, and 14 post colitis induction. Mice instilled with 30% ethanol (control group) were sacrificed at day 14 (Fig. 1). Colons were cut opened longitudinally, washed with ice-cold saline and scored for macroscopic damages (Fedorak et al. 1992).
Curcumin prevented TNBS-induced mice mortality and body weight loss. In vivo protocol for colitis induction in mice (n = 7) using the haptenic weak acid 2,4,6 trinitrobenzene sulfonic acid (TNBS) (a). Mice were given 30% ethanol (control), TNBS (30 mg kg−1 in 30% ethanol, intrarectal instillation, ir. (TNBS group), or TNBS + Cur (25 mg kg−1, intraperitoneal, ip; Cur group). Mice were euthanized at days 3, 7 and 14 days post-colitis induction. Evaluation of survival rate (b) and body weight variation (c)
Histological analysis of colonic lesions
Distal and proximal colons samples were fixed overnight in 10% phosphate buffered formalin and processed for histological analysis. Thin sections stained with hematoxylin–eosin (H&E) or periodic-acid-Schiff (PAS), were analyzed for colon architecture and mucus content by light microscopy (Carl Zeiss, Germany), and scored for microscopic damages (Neurath et al. 1995).
Hoechst 33258-stained colon sections were evaluated for apoptosis (Yamaoka et al. 2008). Apoptotic cells displaying high fluorescence intensity due to chromatin condensation and nuclear fragmentation, were counted in 10 fields under fluorescence microscopy (Carl Zeiss inc., Thornwood, NY).
Preparation of colon homogenates
Colonic tissues were homogenized in ice-cold 50 mM phosphate buffer (pH 7.4) containing 0.5%Triton X-100 (Ultra-turrax T25, England). After freeze-thawing three times, homogenates were centrifuged at 10,000g, 15 min at 4 °C. The resulting supernatants were stored at − 40 °C.
Evaluation of short-term curcumin treatment in TNBS-induced mitochondrial toxicity
Isolation of colon mitochondria
Colon mitochondria were isolated according to the method of Towers et al. (1972), with slight modifications. Colons recovered from control mice were homogenized in ice cold 10% (w:v) MOPS (10 mM, pH 7.4) containing 125 mM sucrose and 0.05% BSA (Ultra-turrax T25, England). Unbroken cells and nuclei were pelleted at 800 g, 5 min at 4 °C. Supernatants were further centrifuged at 12,000g, 20 min at 4 °C. Crude mitochondria were washed twice and suspended in ice cold respiratory buffer (pH 7.4), and used within 2 h.
Mitochondrial swelling assay
Swelling was measured as an index of mitochondrial permeability transition pore (mPTP) opening (Masubuchi et al. 2002). Colon mitochondria (0.5 mg prot ml−1) were incubated in 10 mM MOPS buffer (pH 7.4) containing 125 mM sucrose, 5 mM succinate, 20 µM CaCl2 with or without 5 µM Cur (Izem-Meziane et al. 2012), 10 min at 25 °C. The change in matrix volume following 50 and 100 µM TNBS treatment was monitored at 540 nm, 10 min at 25 °C. Results were expressed as ΔOD540nm mg−1 prot.
Mitochondrial complex I assay
The rate of NADH oxidation was used as a measure of complex I activity (Kuznetsov and Gnaiger 2003). Colon mitochondria were disrupted by sonication and complex I activity was measured in 50 mM phosphate buffer (pH 7.4) containing 0.1 mM ubiquinone-1, 1 mM KCN and 2 mM NaN3, with or without 5 µM Cur for 5 min. Complex I activity was monitored in the presence of 50 or 100 µM TNBS at 340 nm for 2 min. Results were expressed as μmol of NADH mg−1 prot.
Determination of respiration and superoxide anion production
Mitochondria (0.5 mg prot ml−1) were incubated in 15 mM MOPS buffer (pH 7.4) containing 200 mM mannitol, 50 mM sucrose, 150 mM KCl, 0.5 mM EDTA, 50 µM KCN, 1 mM potassium ferricyanide [K3Fe(CN)6], with or without 5 µM Cur for 5 min. The respiration was initiated by 5 mM succinate in the presence of 50 or 100 µM TNBS, and followed at 420 nm, 5 min at 25 °C (Forman and Wilson 1982). Results were expressed as μmol of reduced potassium ferricyanide mg−1 prot.
The potential of Cur to scavenge superoxide anion (O2·–) was determined using mitochondria (0.5 mg prot ml−1) incubated in 10 mM Tris buffer (pH 7.4) containing 250 mM sucrose, 100 μM cytochrome c, with or without 5 µM Cur for 5 min. After addition of 50 or 100 µM TNBS, the generation of O2·– was monitored by the reduction of cytochrome c at 550 nm, 2 min at 25 °C. Results were expressed as μM O2·–mg−1 prot.
Determination of mitochondrial aconitase and fumarase activity ratio
Aconitase activity was measured by monitoring the formation of cis-aconitate from isocitrate at 240 nm in 50 mM Tris–HCl buffer (pH 7.4) containing 0.6 mM MnCl2 and 2 mM isocitrate (Hausladen and Firdovich 1996). One unit (U) was defined as the amount of enzyme necessary to produce 1 μmol of cis-aconitate min−1. Fumarase activity was determined by measuring the increase in absorbance at 240 nm in 30 mM potassium phosphate buffer (pH 7.4) and 5 mM succinate (Racker 1950). One unit (U) was defined as the amount of enzyme that produces 1 μmol of fumarate min−1.
Biochemical evaluation of colon mucosa and mitochondria redox status
The level of reduced glutathione (GSH) was measured as a marker of antioxidant potential in colon homogenates and mitochondria (nmol of GSH mg−1 prot) (Ellman 1959). Nitric oxide (NO) synthase activity was measured by nitrites content, the stable nitric oxide metabolite (Green et al. 1982), and expressed in μM nitrites mg−1 prot, using a sodium nitrite curve as standard. The level of malondialdehyde (MDA), a marker of lipid peroxides (nmol of MDA mg−1 prot) was measured as described (Ohkawa et al. 1979). Neutrophils recruitment into inflamed colons was determined by myeloperoxidase (MPO) activity (μM H2O2 consumed min−1 mg−1 prot) according to Krawisz et al. (1984). Biochemical values were normalized to samples protein concentration (Bradford 1976).
Statistical analysis
Data were expressed as mean ± SEM. Statistical analysis was performed using the Student’s t-test, p < 0.001, 0.05 and 0.01 differences between groups were considered significant. Histological damage scores were analyzed by Mann–Whitney’s U test.
Results
Low-dose Cur treatment erased TNBS-induced chronic nitro-oxidative colitis in mice
The protective effect of low dose Cur in TNBS-induced drastic mice mortality and chronic colitis scores, was checked at three end points (3, 7 and 14 days), post colitis induction.
Cur suppressed mice mortality by reducing colitis and histological scores
TNBS-colitis is an hapten sensitizer-based model mimicking the colonic immune dependent symptoms of Crohn’s disease (Morris et al. 1989; Hölttä et al. 2008; Tu et al. 2017).
Our results show that TNBS induced 20–30% mice mortality, at the 2nd week post colitis induction. The surviving mice showed a time dependent increase in colitis scores (Table 1, Fig. 1).
TNBS-treated colons revealed hemorrhagic edemas in mucosa and submucosa infiltrated by mixte inflammatory cells. The early disruption of colon architecture, was associated with mucin depleted foci (MDF) as attested by the low number of alcian blue (AB) positive goblet cells. Crypt abscesses highly invaded by neutrophils occurred at the 2nd week, primarily in distal colon (Fig. 2A, B).
Curcumin improved TNBS-induced macroscopic and microscopic colon lesions. Mice receiving vehicle (control group), TNBS (30 mg kg−1, ir; TNBS group) alone (A) or followed by daily treatment of Cur (25 mg kg−1, ip; Cur group) (B) were sacrificed at days 3, 7 and 14 post colitis induction. Specimens of distal and proximal colons were submitted to histological analysis as described in materials and methods section. Hematoxylin and eosin (H&E)-stained colon sections of control (a) and TNBS-treated mice for 3 (b), 7 (c), 14 (d) days in distal and proximal colon were analyzed by light microscopy (400 ×). Representative H&E-stained colon sections of luminal wall of colon mucosa showing foci of hemorrhages (arrowhead), inflamed areas (arrow). Microscopic damage were assessed according to Neurath et al. (1995)
Daily low-dose Cur suppressed mortality and improved the hallmarks of chronic colitis, including crypt architecture, goblet cells number and mucin content more efficiently in proximal colon, compared with the damaged distal colon (Table 1; Figs. 2, 3).
Curcumin attenuated cell apoptosis and goblet cells loss related to oxidative stress in TNBS-colitis. Sections of distal (A) and proximal (B) colons were obtained as described in Fig. 2. Representative Alcian blue (AB) and Hoechst 33258-stained distal (A) and proximal (B) colon sections, of TNBS-treated for 3 (b), 7 (c), 14 (d) days followed (+ Cur) or not (− Cur) by Cur treatment were analyzed by light microscopy (400x), and assessed for microscopic damages (Neurath et al. 1995)
Cur prevented phagocytes influx and redox imbalance in distal colon
One hallmark of IBD is the transmural infiltration of primed neutrophils and macrophages where they accumulate substantial ROS amounts generating persistent oxidative stress (Circu and Aw 2011; Mouzaoui et al. 2012; Aviello and Knaus 2016; Peng et al. 2017).
Compared with control, nitrites level enhanced by three- to fourfold, while MPO activity rapidly increased by seven-fold (p < 0.001) to stabilise at 3.5-fold of control at day 14, in inflamed distal colon (p < 0.001), indicating phagocytes dependent oxidative activity. MDA levels increased by three- to fivefold (p < 0.01), while GSH levels decreased by 62%, 83% and 52% (p < 0.001), respectively, compared to control.
Cell apoptosis increased by 3- (p < 0.01), 5- (p < 0.001) and 2.5-fold (p < 0.01) at days 3, 7 and 14, respectively, post colitis induction.
Low-dose Cur reduced progressively nitrite level by 55% (p < 0.01) and 70% (p < 0.001), and MPO activity by 70% and 85% (p < 0.01), compared to model group. It blocked cell apoptosis by 60% (p < 0.01), 58% (p < 0.001), 40% (p < 0.05), and MDA levels by 67%, 66% and 62% (p < 0.001), while restoring GSH content by 34% and 25% (p < 0.01) in inflamed distal colon, compared to TNBS-treated group (Tables 2, 3; Fig. 3A, B).
Protective effect of Cur in inflamed proximal colon
As predicted by the differences in genetic profile, metabolism and interactions with gut microbiota, the proximal and distal colon display specific sensitivity to oxidative inflammation and cancer (Glebov et al. 2003; Sun et al. 2020).
We show that TNBS-associated inflammation and nitro-oxidative stress extended progressively to proximal colon (Table 1). Nitrites level doubled (p < 0.01) after 3 days to reach fivefold increase (p < 0.001) at week 2. MPO activity rapidly doubled (p < 0.01) to stabilize at fourfold increase (p < 0.001) at day 14 (Table 2).
TNBS enhanced MDA level by three- (p < 0.01), five- and eightfold (p < 0.001), and cell apoptosis by four-, five- (p < 0.001) and threefold (p < 0.01), respectively, 3, 7 and 14 days post TNBS challenge (Tables 3, 4).
Cur lowered time dependently nitrites levels by 80% (p < 0.001) and 70% (p < 0.001) and MPO activity by 25% (p < 0.05), 57% (p < 0.01) and 75% (p < 0.001), respectively, at days 7 and 14. Cur improved cell apoptosis by 30% (p < 0.05), 35% (p < 0.01) and 10% (p > 0.05), and MDA levels by 11%, 65% and 73% (p < 0.001), compared with model group.
TNBS depressed GSH level by about tenfold (p < 0.001) which was fully restored by Cur supplementation.
Short-term Cur treatment improved TNBS-induced mitochondrial toxicity in vitro
Recently, mitochondrial dysfunction in IBD has been associated to nitro-oxidative stress (Wang et al. 2014; Zorov et al. 2014; Packiriswamy et al. 2017; Wong et al. 2017).
To furher explore the role of mitochodrial stress in the severity of colitis, the protective effect of short term Cur treatment was analyzed on TNBS-inflamed mitochondria isolated from control mice and from in vivo protocol.
Cur prevented TNBS-induced mitochondrial swelling
Compared with control, 50 and 100 µM TNBS enhanced mitochondrial swelling by 3.5- and 3.8-fold (p < 0.001), and by 3.7- and 4.2-fold (p < 0.001), respectively after 5 and 10 min, suggesting that this haptenic sensitizer induced a dose and time dependent uncoupling of colon mitochondria. Short-term Cur attenuated mitochondrial swelling by 77% (p < 0.001) and 68% (p < 0.01), and by 67% and 68% (p < 0.01), respectively, compared to the respective controls (Fig. 4).
Curcumin improved the opening of mitochondrial permeability transition pore (mPTP) induced by TNBS. Control colon mitochondria were incubated in swelling buffer as described in materials and methods section. Mitochondrial swelling was initiated by the addition of TNBS 50 (a) or 100 μM (b, c) in the presence or absence of 5 µM Cur for 10 min at 25 °C. Data are means ± SEM. n = 5 for controls; n = 5 for TNBS. *p < 0.05, **p < 0.01 and ***p < 0.001 vs. control; #p < 0.05, ##p < 0.01 and ###p < 0.001 vs. TNBS treated mitochondria
Cur prevented inhibition of mitochondrial respiration by TNBS
Compared with control, 50 and 100 µM TNBS (5 min) decreased respiration by 50% and 65% (p < 0.001), and electron transfer through complex I by 38% (p < 0.05) and 65% (p < 0.01), respectively. Cur restored mitochondrial respiration by 30% (p < 0.05) and 26% (p < 0.05), and complex I activity by 33% and 9% (p < 0.05), respectively, in TNBS-treated mitochondria (Fig. 5a, b).
Curcumin ameliorated TNBS-induced colon mitochondria toxicity in vitro. Colon mitochondria (0.5 mg prot−1) were incubated with 100 µM TNBS in the presence or absence of 5 µM Cur as described in materials and methods section and assayed for respiration (a), complex I activity (b) and superoxide (c) and nitric oxide (d) production. Data are means ± SEM. n = 5 for controls; n = 5 for TNBS. *p < 0.05, **p < 0.01 and ***p < 0.001 vs. control; #p < 0.05, ##p < 0.01 and ###p < 0.001 vs. TNBS treated mitochondria
Cur quenched matrix superoxide anion and restored aconitase activity
To further explore the mechanism of mitochondria dysfunction attested by uncoupling, inhibition of respiration, complex I and aconitase activity, we evaluated the impact of Cur in TNBS-induced mtROS generation.
Superoxide generation was amplified by two- (p < 0.05) and fourfold (p < 0.001), whereas aconitase activity was depressed by 50% (p < 0.05) and 77% (p < 0.01) in colon mitochondria exposed to 50 µM and 100 µM TNBS, respectively, compared to control.
Cur quenched TNBS-generated superoxide anion by 55% (p < 0.05) and 60% (p < 0.001), (Fig. 5c), and restored aconitase activity by 50% (p < 0.05), and 70% (p < 0.01), respectively. In contrast, TNBS and Cur had no effect on fumarase activity (Fig. 6a, b).
Curcumin prevented TNBS-collapsing redox sensor activities. (0.5 mg prot−1) were incubated with 100 µM TNBS in the presence or absence of 5 µM Cur as described in materials and methods section and assayed for aconitase activity (a), fumarase activity (b). Evaluation of aconitase/fumarase ratio (c). Data are means ± SEM. n = 5 for controls; n = 5 for TNBS. *p < 0.05, **p < 0.01 and ***p < 0.001 vs. control; #p < 0.05, ##p < 0.01 and ###p < 0.001 vs. TNBS treated mitochondria
Cur prevented TNBS-induced mitochondrial redox imbalance
Cur can restore mitochondrial redox balance through its ability to scavenge mtnitrites, to inhibit lipids peroxidation and to restore mtGSH stores.
The level of mtnitrites and mtMDA increased by 1.2- (p > 0.05) and 1.5-fold (p < 0.05), and by 1.3- (p < 0.05) and 1.8-fold (p < 0.01), in response to 50 and 100 µM TNBS (5 min), respectively. Whereas the level of mtGSH was lowered by 10% (p > 0.05) and 30% (p < 0.05), indicating that TNBS-toxicity is related to the dose dependent mitochondrial redox imbalance.
Cur fully restored mtGSH level and dropped mtMDA by 36% (p < 0.05) and 45% (p < 0.01) in colon mitochondria exposed to 50 and 100 µM TNBS, thus rebalancing mtMDA/mtGSH ratio, while mtnitrites level were slightly restored (19% and 1%; p > 0.05), in 50 and 100 µM TNBS-treated mitochondria (Figs. 5d, 7).
Curcumin prevented TNBS-induced mitochondria redox imbalance. Colon mitochondria (0.5 mg prot−1) were incubated with 100 µM TNBS in the presence or absence of 5 µM Cur as described in materials and methods section and assayed for MDA (a) and GSH (b) levels. Evaluation of colon mitochondria MDA/GSH ratio (c). Data are means ± SEM. n = 5 for controls; n = 5 for TNBS. *p < 0.05, **p < 0.01 and ***p < 0.001 vs. control; #p < 0.05, ##p < 0.01 and ###p < 0.001 vs. TNBS treated mitochondria
Discussion
This study reports the pharmacological effect of Cur in TNBS-mediated mitochondria toxicity and colitis.
As a weak acid, TNBS accumulated within matrix can collapse pH gradient (mtΔpH) and disrupt inner membrane potential (mtΔΨ), which uncouples ETC activity from ATP synthesis (Fig. 4). In addition to sulphite-peroxyl and sulphate radicals generated by oxidative metabolism of TNBS, intestinal nitro-reductases accumulate nitro and superoxide radicals, in vivo. More, mucosal oxidative damages are amplified by TNBS redox cycling and its toxicogenic potential on mitochondria enriched colon epithelial cells (Grisham et al. 1991; Chamulitrat 1999).
TNBS-stressed mitochondria show hallmark features of a ROS dependent dysfunction. The half and two third decrease in respiration and respirasome I activity may be related to the drop in aconitase activity, the redox check point of TCA cycle (Titov et al. 2016). A mitochondrial NO synthase (mtNOS) has been convincingly identified as a variant of constitutive neuronal NOS (Kanai et al. 2001). Low-dose NO is protective to respirasome I by neutralizing superoxide to nitrate (Figs. 5, 6) (Sharpley et al. 2006). At higher doses, NO cross reaction with superoxide releases the highly reactive peroxynitrite (ONOO-), which covalently binds to Fe-S-containing respirasomes I, III, triggering a reverse electron transfer flow and mitochondria uncoupling (Brown and Borutaite 2004; Ohtani et al. 2012). Mitochondria uncoupling is a physiological adaptive response to mild oxidative stress (Fig. 4). mtROS and lipid peroxides can induce antioxidant activity of uncoupling protein 2 (UCP2), an ubiquitous mitochondrial carrier associated to inner mitochondrial membrane, which catalyzes protons re entry into matrix and energy dissipation in the expense of ATP synthesis (Houten and Wanders 2010; Chen et al. 2018; Huang et al. 2019). Also, UCP2 blocks fatty acids entry, while exporting various TCA cycle metabolites to the cytoplasm. This limits NADH and FADH2 generation, the electron donors for mtROS-releasing respiration (Vozza et al. 2014).
The drastic consumption of GSH and sustained accumulation of MDA, a marker of electrophilic hydroperoxy lipids, exacerbates MDA/GSH ratios in stressed mitochondria, and in inflamed distal and proximal colon, suggesting MDA/GSH ratio as a potential index of nitro-oxidative stress at tissular and subcellular level. The nitro-oxidative process in proximal colon reached threefold the level of distal colon, and may account for colon epithelial cell apoptosis (Tables 3, 4; Fig. 7).
Superoxide dismutases (SOD) block propagating oxidative chain reactions through dismutation of superoxide into hydrogen peroxide (H2O2) in matrix (MnSOD) and cytosol (Cu/Zn SOD) (Murphy 2009). Then, glutathione reductase (GSH/GS-SG)/glutathione peroxidase shuttle takes up H2O2 and oxidizes NADPH (H+) through the thiol redox chain thioredoxin (TrxR)/TRX/Peroxiredoxin/catalase, facilitating the reduction of hydroperoxy lipids and H2O2 (Awasthi et al. 2000; Cox et al. 2009; Handy and Loscalzo 2012).
By restoring GSH stores, Cur can restart this ROS-detoxifying machinery (Table 4; Fig. 7).
By quenching TNBS-generated mtROS and trapping hydroperoxy lipids around respirasomes (Fig. 8), Cur can support mitochondria recoupling through the fine modulation of mPTP opening, inner mitochondrial membrane fluidity and physiological electrons transfer by respirasomes. The powerful antioxidant and metal chelating capacity are supported by the redox activity of methoxyphenols and α,β-unsaturated carbonyl (enone) electrophile backbone of Cur (Priyadarsini et al. 2003; Jiao et al. 2006; Wei et al. 2006; Aggarwal et al. 2015).
Recoupling of TNBS-stressed mitochondria by curcumin. TNBS induced mitochondrial stress, and sustained reactive oxygen and nitrogen species (mtROS) levels. The mtROS dependent oxidation of polyunsaturated fatty acids of phospholipid bilayer generates hydroperoxy lipids adductors which leads to mitochondria uncoupling, and the collapse of mitochondrial membrane potential. In addition, the nitrosation of iron-sulfur (Fe-S)-clusters of respirasomes I and III, and the redox sensitive aconitase, blocks tri carboxylic acid (TCA) cycle and respiration, resulting in bioenergetic stress. Curcumin (Cur) as a lipophilic phytochemical can insert into lipid bilayer which ii interfers with lipids and proteins oxidation by scavenging superoxide anion, peroxinitrite, hydroperoxy lipids and hydroxyl radical. Cur can also reactivate endogenous antioxidant system and restore adaptive cell response to nitro-oxidative stress by thiols modulation of (Keap1), an endogenous inhibitor of the transcription nuclear factor (erythroid-derived 2)-like 2(Nrf-2) of genes for NADPH and GSH biosynthesis and for antioxidant and detoxifying enzymes. In addition, matrix superoxide dismutase (MnSOD) block propagating oxidative chain reactions through dismutation of superoxide into hydrogen peroxide (H2O2). Then, glutathione reductase (GSH/GS-SG)/glutathione peroxidase shuttle takes up H2O2 and oxidizes NADPH (H+) through the thiol redox chain thioredoxin (TrxR)/TRX/Peroxiredoxin/catalase, then facilitating the reduction of hydroperoxy lipids and H2O2
Cur may prime mithormesis, the adaptive mitochondrial response to nitro-oxidative stress, by up-regulating genes involved in GSH and NADPH neosynthsesis through NRF2-EpRE pathway (Aggarwal et al. 2013; Forman et al. 2014).
Mitochondrial stress has been evidenced in intestinal epithelium of IBD patients, and ultrastructural changes of colon mitochondria have been earlier attributed to deficient fatty acid β-oxidation (Houten and Wanders 2010; Sifroni et al. 2010; Packiriswamy et al. 2017).
Besides, the uncontrolled immune response of CD mimicked by TNBS is sustained by Th1 and Th7 dependent pro inflammatory cytokines IFN-γ, IL-1β, TNF-α resulting from the massive influx of inflammatory Th1/Th17 cells and neutrophils (Hölttä et al. 2008; Beltrán et al. 2010).
Macrophages accumulated in luminal epithelium, while neutrophils invaded crypt pits, forming abscesses in distal colon (Figs. 2, 3). The respiratory burst and NO synthase activity of phagocytes infiltrating colon mucosa are significant sources of extracellular ROS. The coupling of phagocytes NADPH oxidase (NOX2)-derived superoxide anion (ROS precursor), NO and MPO activity concentrate mixed reactive nitrogen and oxygen species in distal and proximal colon at days 3, 7 and 14 days of TNBS-colitis (Tables 2, 4). Active inflammatory foci are maintained in intestinal mucosa by the persistent flow of mitochondria and NOXs-derived ROS, fuelled by inducible colonic NOX1, uncoupled endothelial NOS activity and various oxidative metabolic activities (Beltrán et al. 2010; Mouzaoui et al. 2012; Aviello and Knaus 2016). NO-related colonic damages have been attributed to macrophage 1 (M1) subset. The alternative activation of macrophages 2 (M2) with up regulated arginase activity is involved in epithelia cells proliferation and mucosa healing (Tu et al. 2017).
Importantly, low-dose Cur abolished the drastic mortality in mice, and improved in a time dependent manner macroscopic and histological scores including crypts disruption, intestinal fibrosis and hemorrhagic edema, while restoring mucosal function by progressive recovery of mucin-producing crypts (Table 1; Figs. 2, 3), intestinal permeability and gut microbiota (Nazli et al. 2004; Kaulmann and Bohn 2016). Mucin depleted foci (MDF) with β catenin mutations are preneoplastic formations. They are identified in animal models of colon carcinogenesis and in humans with CRC. They are emerging as biomarkers of colon carcinogenesis (Femia et al. 2005; Sakai et al. 2012).
Low-dose Cur attenuated TNBS-oxidative bowel inflammation by inhibiting the prooxidant activity of myeloperoxidase and NO synthase associated to phagocytes influx, primarily through the blockade of adhesion to vascular endothelium (Table 2; Fig. 5) (Kunnumakkara et al. 2017; Luis et al. 2017). Cur reboosted catalase activity in colon mucosa (data not shown), indicating that oxidative lesions and mitochondrial damages also results from inefficient antioxidant system.
Phytochemicals encomprise a wide set of electrophilic adductors of the cytoplasmic Keap1/Cul3-NRF2 redox sensor. Keap1 is a zinc metalloprotein wearing critical 25–27 Cys residues (Dinkova-Kostova et al. 2005). Among them, Cys 151,257, 273, 288, and 297 of BTB/ERV domains can finely appreciate electrophile and oxidative stress. Various electrophiles and oxidants including TNBS, lipid peroxides, and reactive oxygen and nitrogen species can interact with Keap1 to weaken interactions with DLG and ETGE binding domains of NRF2.
The electrophilic capacity of Cur is associated to α,β-unsaturated carbonyl (enone) moiety. Its cytoprotective effect is potentiated by auto-oxidation and oxidative metabolism which generate more efficient derived electrophiles with enhanced nucleophile binding sites (Priyadarsini et al. 2003; Edwards et al. 2017; Luis et al. 2017).
Cur and its oxidized derivatives can adduct Keap1 through oxidation of its most reactive Cys151 and polyphenols sensitive Cys of BTB/ERV domain, to induce conformational change. This releases a stabilized form of NRF2 which translocates to the nucleus where it adapts on Maf protein to lock the antioxidant/electrophile response element (ARE/EpRE) on DNA, and triggers the transcription of a network of cytoprotective genes, such as heme-oxygenase-1, NADP(H) quinine oxidorectase 1, thioredoxin…, which restores redox homeostasis at systemic and cellular level (Wang et al. 1997; Edwards et al. 2017).
Complex interplay between NLRP3 inflammasome, NFKB and NRF2, modulating pro- and anti inflammatory pathways is potentially mastered by the regulatory protein p62 (Hennig et al. 2018).
Taken together, our results indicate that short term Cur, restore primary mitochondrial architecture and function through the modulation of mPTP opening (swelling), ROS leakage by the redox loops of the electron transfer chain (ROS generation). This critical property is likely related to its lipophilic nature, allowing spontaneous “vectorization” to the mitochondria. Cur can collapse the mtROS gradient, by quenching superoxide, nitrites and hydroxyl radical. This ROS-detoxifiyng capacity sustains mitochondria recoupling and colon epithelium healing.
Herbal medicine is growing, worldwide. Despite its low bioavailability, Cur, a phytochemical electrophile with high safety and tolerability is promising as mitochondrial targeted antioxidant, for IBD.
Abbreviations
- CD:
-
Crohn’s disease
- Cul3:
-
Cullin3-based Cullin-RING E3 ubiquitin ligase
- Cur:
-
Curcumin
- ARE/EpRE:
-
Antioxidant response element/electrophile response element
- ETC:
-
Electron transfer chain; GSH, reduced glutathione
- IBD:
-
Inflammatory bowel diseases
- I(O)MM:
-
Inner (outer) mitochondrial membrane
- iNOS:
-
Inducible NO synthase
- Keap1:
-
Kelch-like ECH associated protein 1
- MDA:
-
Malondialdehyde
- MPO:
-
Myeloperoxidase
- mPTP:
-
Mitochondrial permeability transition pore
- NO:
-
Nitric oxide
- NOX2:
-
NADPH Oxidase2
- O2·− :
-
Superoxide anion
- NRF2:
-
Nuclear factor (erythroid-derived 2)-like 2
- OxPhos:
-
Oxidative phosphorylation
- mt:
-
Mitochondria
- PN:
-
Neutrophils
- ROS:
-
Reactive oxygen species
- TNBS:
-
2,4,6-Trinitrobenzene sulfonic acid
References
Aggarwal BB, Gupta SC, Sung B (2013) Curcumin: an orally bioavailable blocker of TNF and other pro-inflammatory biomarkers. Br J Pharmacol 169:1672–1692
Aggarwal BB, Deb L, Prasad S (2015) Curcumin differs from tetrahydrocurcumin for molecular targets, signaling pathways and cellular responses. Molecules 20:185–205
Aviello G, Knaus UG (2016) ROS in gastrointestinal inflammation: rescue ? Br J Pharmacol 174:1704–1718
Awasthi S, Pandya U, Singhal SS, Lin JT, Thiviyanathan V, Seifert WE et al (2000) Curcumin-glutathione interactions and the role of human glutathione S-transferase P1–1. Chem-Biol Interact 128:19–38
Balogun E, Hoque M, Gong P, Killeen E, Green CJ, Foresti R et al (2003) Curcumin activates the haemoxygenase-1gene via regulation of Nrf2 and the antioxidant-responsive element. Biochem J 371:887–895
Beltrán B, Nos P, Dasi F, Iborra M, Bastida G, Martínez M et al (2010) Mitochondrial dysfunction, persistent oxidative damage, and catalase inhibition in immune cells of naïve and treated Crohn’s disease. Inflamm Bowel Dis 16:76–86
Bernardi P, Rasola A, Forte M, Lippe G (2015) The mitochondrial permeability transition pore: channel formation by F-ATP synthase, integration in signal transduction, and role in pathophysiology. Physiol Rev 95(4):1111–1155
Bradford MM (1976) A rapid and sensitive method for the quantification of microgram quantities of proteins utilizing the protein-dye binding. Anal Biochem 72:248–252
Brand MD (2016) Mitochondrial generation of superoxide and hydrogen peroxide as the source of mitochondrial redox signaling. Free Radic Biol Med 100:14–31
Brown GC, Borutaite V (2004) Inhibition of mitochondrial respiratory complex I by nitricoxide, peroxynitrite and S-nitrosothiols. Biochim Biophys Acta 1658:44–54
Capasso R, Borrelli F, Cascio MG, Aviello G, Huben K, Zjawiony JK et al (2008) Inhibitory effect of salvinorin A, from Salvia divinorum, on ileitis-induced hypermotility: cross-talk between kappa-opioid and cannabinoid CB(1) receptors. Br J Pharmacol. 155(5):681–689
Capasso R, Orlando P, Pagano E, Aveta T, Buono L, Borrelli F et al (2014) Palmitoylethanolamide normalizes intestinal motility in a model of post-inflammatory accelerated transit: involvement of CB1 receptors and TRPV1 channels. Br J Pharmacol 171(17):4026–4037
Chamulitrat W (1999) Desulfonation of a colitis inducer 2,4,6-trinitrobenzene sulfonic acid produces sulfite radical. Biochim Biophys Acta 1472(1–2):368–375
Chen JJ, Yu BP (1994) Alterations in mitochondrial membrane fluidity by lipid peroxidation products. Free Radic Biol Med 17:411–418
Chen XJ, Wang X, Kaufman BA, Butow RA (2005) Aconitase couples metabolic regulation to mitochondrial DNA maintenance. Science 307:714–717
Chen W, Luo S, Xie P, Hou T, Yu T, Fu X (2018) Overexpressed UCP2 regulates mitochondrial flashes and reverses lipopolysaccharide-induced cardiomyocytes injury. Am J Transl Res 10(5):1347–1356
Circu ML, Aw TY (2011) Redox biology of the intestine. Free Radic Res 45:1245–1266
Cox AG, Winterbourn CC, Hampton MB (2009) Mitochondrial peroxiredoxin involvement in antioxidant defence and redox signalling. Biochem J 425:313–325
Dinkova-Kostova AT, Holtzclaw WD, Wakabayashi N (2005) Keap1, the sensor for electrophiles and oxidants that regulates the phase 2 response, is a zinc metalloprotein. Biochemistry 44:6889–6899
Edwards RL, Luis PB, Varuzza PV, Joseph AI, Presley SH, Chaturvedi R, Schneider C (2017) The anti-inflammatory activity of curcumin is mediated by its oxidative metabolites. J Biol Chem 292:21243–21252
Ellman G (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82(1):70–77
Fedorak R, Empey L, Walker K (1992) Verapamil alters eicosanoid synthesis and accelerates healing during experimental colitis in rats. Gastroenterology 102:1229–1235
Femia AP, Bendinelli B, Giannini A, Salvadori M, Pinzani P, Dolara P, Caderni G (2005) Mucin-depleted foci have b-catenin genes mutations, altered expression of its protein and are dose-and time-dependent in the colon of 1,2-dimethylhydrazine-treated rats. Int J Cancer 116(1):9–15
Forman N, Wilson D (1982) Energetics and stoichiometry of oxidative phosphorylation from NADH to cytochrome c in isolated rat liver mitochondria. J Biol Chem 25:12908–12915
Forman HJ, Davies KJA, Fulvio Ursini F (2014) How do nutritional antioxidants really work: nucleophilic tone and para-hormesis versus free radical scavenging in vivo. Free Radic Biol Med 66:24–25
Glebov OK, Rodriguez LM, Nakahara K, Jenkins J, Cliatt J, Humbyrd CJ et al (2003) Distinguishing right from left colon by the pattern of gene expression. Cancer Epidemiol Biomarkers Prev 12:755–762
Green LC, Wagner DA, Glogowski J, Skiper PL, Wishnock JS, Tannenbaum SR (1982) Analysis of nitrate, nitrite and [15 N] nitrate in biological fluids. Anal Biochem 126:131–138
Grisham MB, Volkmer C, Tso P, Yamada T (1991) Metabolism of trinitrobenzene sulfonic acid by the rat colon produces reactive oxygen species. Gastroenterology 101:540–547
Grossi V, Hyams JS, Glidden NC, Knight BE, Young EE (2019) Characterizing clinical features and creating a gene expression profile associated with pain burden in children with inflammatory bowel disease. Inflamm Bowel Dis. https://doi.org/10.1093/ibd/izz240
Handy DE, Loscalzo J (2012) Redox regulation of mitochondrial function. Antioxid Redox Signal 16(11):1323–1367
Hausladen A, Firdovich I (1996) Measuring nitric oxide and superoxide: rate constants for aconitase reactivity. Met Enzymol 269:37–41
Heger M, van Golen RF, Broekgaarden M, Michel MC (2013) The molecular basis for the pharmacokinetics and pharmacodynamics of curcumin and its metabolites in relation to cancer. Pharmacol Rev 66:222–307
Hennig P, Garstkiewicz M, Grossi S, Michela Di Filippo M, French LE, Beer HD (2018) The crosstalk between Nrf2 and inflammasomes. Int J Mol Sci 19:562
Hölttä V, Klemetti P, Sipponen T, Westerholm-Ormio M, Kociubinski G, Salo H et al (2008) IL-23/IL-17 immunity as a hallmark of Crohn's disease. Inflamm Bowel Dis 14(9):1175–1184
Houten SM, Wanders RJA (2010) A general introduction to the biochemistry of mitochondrial fatty acid β-oxidation. J Inherit Metab Dis 33:469–477
Huang J, Peng W, Zheng Y, Hao H, Li S, Yao Y, et al (2019) Upregulation of UCP2 expression protects against lps-induced oxidative stress and apoptosis in cardiomyocytes. Oxidat Med Cellular Longev 2019:articleID 2758262
Izem-Meziane I, Djerdjouri B, Rimbaud S, Caffin F, Fortin D, Garnier A et al (2012) Catecholamine-induced cardiac mitochondrial dysfunction and mPTP opening: protective effect of curcumin. Am J Physiol Heart Circ Physiol 302:H665–H674
Jiao Y, Wilkinson J, Pietsch CE, BussJ L, Wang W, Planalp R et al (2006) Iron chelation in the biological activity of curcumin. Free Radic Biol Med 40:1152–1160
Kanai AJ, Pearce LL, Clemens PR, Birder LA, Van Bibber MM, Choi SY et al (2001) Identification of a neuronal nitric oxide synthase in isolated cardiac mitochondria using electrochemical detection. Proc Natl Acad Sci USA 98(24):14126–14131
Kaulmann A, Bohn T (2016) Bioactivity of polyphenols: preventive and adjuvant strategies toward reducing inflammatory bowel diseases-promises, perspectives and pitfalls. Oxid Med Cell Longev 2016:9346470
Krawisz JE, Sharon P, Stenson WF (1984) Quantification assay for acute intestinal inflammation based on myeloperoxidase activity. Gastroenterology 87:1344–1350
Kunnumakkara AB, Bordoloi D, Padmavathi G, Monisha J, Roy NK, Prasad S, Aggarwal BB (2017) Curcumin, the golden nutraceutical: multi targeting for multiple chronic diseases. Br J Pharmacol 174(11):1325–1348
Kuznetsov A, Gnaiger E (2003) Complex I (NADH: Ubiquinone oxidoreductase, EC 1.6.5.3) mitochondrial membrane enzyme. MiT Net 8(15):1–8
Lewis K, McKay DM (2009) Metabolic stress evokes decreases in epithelial barrier function. Ann NY Acad Sci USA 1165:327–337
Li W, Kong AN (2009) Molecular mechanisms of Nrf2-mediated antioxidant response. Mol Carcinog 48:91–104
Luis PB, Gordon ON, Nakashima F, Joseph AI, Shibata T, Uchida K et al (2017) Oxidative metabolism of curcumin-glucuronide by peroxidases and isolated human leukocytes. Biochem. Pharmacol 132:143–149
Masubuchi Y, Nakayama S, Horie T (2002) Role of mitochondrial permeability transition in diclofenac–induced hepatocyte injury in rats. Hepatology 35:544–551
Millar SA, Stone NL, Bellman ZD, Yates AS, England TJ, O'Sullivan SE (2019) A systematic review of cannabidiol dosing in clinical populations. Br J Clin Pharmacol 85:1888–1900
Morris GP, Beck PL, Herridge MS, Depew WT, Szewczuk MR, Wallace JL (1989) Hapten-induced model of chronic inflammation and ulceration in the rat colon. Gastroenterology 96:795–803
Mouzaoui S, Rahim I, Djerdjouri B (2012) Aminoguanidine and curcumin attenuated tumor necrosis factor (TNF)-α-induced oxidative stress, colitis and hepatotoxicity in mice. Int Immunopharmacol 12:302–311
Murphy MP (2009) How mitochondria produce reactive oxygen species. Biochem J 417(1):1–13
Nazli A, Yang PC, Jury J, Howe K, Watson JL, Söderholm JD et al (2004) Epithelia under metabolic stress perceive commensal bacteria as a threat. Am J Pathol 164:947–957
Neurath M, Fuss I, Kelasall B, Stuber E, Strober W (1995) Antibodies to interleukin-12 abrogate established experimental colitis in mice. J Exp Med 182:1281–1290
Novak EA, Mollen KP (2015) Mitochondrial dysfunction in inflammatory bowel disease. Front Cell Dev Biol 3:62
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Ohtani H, Katoh H, Tanaka T, Saotome M, Urushida T, Satoh H et al (2012) Effects of nitric oxide on mitochondrial permeability transition pore and thiol mediated responses in cardiac myocytes. Nitric Oxide 26:95–101
Packiriswamy N, Coulson KF, Holcombe SJ, Sordillo LM (2017) Oxidative stress-induced mitochondrial dysfunction in a normal colon epithelial cell line. World J Gastroenterol 23(19):3427–3439
Pagano E, Capasso R, Piscitelli F, Romano B, Parisi OA, Finizio S et al (2016) An orally active cannabis extract with high content in cannabidiol attenuates chemically-induced intestinal inflammation and hypermotility in the mouse. Front Pharmacol 4(7):341
Pagano E, Romano B, Iannotti FA, Parisi OA, D'Armiento M, Pignatiello S et al (2019) The non-euphoric phytocannabinoid cannabidivarin counteracts intestinal inflammation in mice and cytokine expression in biopsies from UC pediatric patients. Pharmacol Res 22:104464
Peng Y, Junliang PuJ, Tang C, Wu Z (2017) Curcumin inhibits heat-induced apoptosis by suppressing NADPH oxidase 2 and activating the Akt/mTOR signaling pathway in bronchial epithelial cells. Cell Physiol Biochem 41:2091–2103
Pfeiffer K, Gohil V, Stuart RA, Hunte C, Brandt U, Greenberg ML, Schagger H (2003) Cardiolipin stabilizes respiratory chain supercomplexes. J Biol Chem 278:52873–52880
Priyadarsini KI, Maity DK, Naik GH, Kumar MS, Unnikrishnan MK, Satav JG, Mohan H (2003) Role of phenolic OH and methylene hydrogen on the free radical reactions and antioxidant activity of curcumin. Free Radic Biol Med 35:475–484
Racker E (1950) Spectrophotometric measurements of the enzymatic formation of fumaric and cis-aconitic acids. Biochim Biophys Acta 4(1–3):211–214
Saha S, Adhikarya A, Bhattacharyya P, Das T, Sa G (2012) Death by design: where curcumin sensitizes drug-resistant tumours. Anticancer Res 32(7):2567–2584
Sakai E, Morioka T, Yamada E, Ohkubo H, Higurashi T, Hosono K et al (2012) Identification of preneoplastic lesions as mucin-depleted foci in patients with sporadic colorectal cancer. Cancer Sci 103:144–149
Sharpley MS, Shannon RJ, Draghi F, Hirst J (2006) Interactions between phospholipids and NADH:ubiquinone oxidoreductase (complex I) from bovine mitochondria. Biochemistry 45:241–248
Sifroni KG, Damiani CR, Stoffel C, Cardoso MR, Ferreira IC, Rezin GT et al (2010) Mitochondrial respiratory chain in the colonic mucosal of patients with ulcerative colitis. Mol Cell Biochem 342:111–115
Spinelli JB, Haigis MC (2018) The multifaceted contributions of mitochondria to cellular metabolism. Nat Cell Biol 20(7):745–754
Sun Y, Mironova V, Chen Y, Lundh EPF, Zhang Q, Cai Y, et al (2020) Molecular pathway analysis indicates a distinct metabolic phenotype in women with right-sided colon cancer. Trans Onc 13(1):42–56
Szebeni GJ, Nagy LI, Berkó A, Hoffmann A, Fehér LZ, Bagyánszki M et al (2019) The anti-inflammatory role of mannich curcuminoids: special focus on colitis. Molecules 24:1546. https://doi.org/10.3390/molecules24081546beni
Titov DV, Cracan V, Goodman RP, Peng J, Grabarek Z, Mootha VK (2016) Complementation of mitochondrial electron transport chain by manipulation of the NAD+/NADH ratio. Science 352:231–235
Towers N, Dixon H, Kellerman G, Linnane A (1972) Biogenesis of mitochondria. The sensitivity of rat liver mitochondria to antibiotics; a phylogenetics difference between a mammalian system and yeast. Anal Biochem Biophys 151:361–369
Tu L, Chen J, Xu D, Xie Z, Yu B, Tao Y, Shi G, Duan L (2017) IL-33-induced alternatively activated macrophage attenuates the development of TNBS-induced colitis. Oncotarget 8(17):27704–27714
Ukil A, Maity S, Karmakar S, Datta N, Vedasiromoni JR, Das PK (2003) Curcumin, the major component of food flavour turmeric, reduces mucosal injury in trinitrobenzene sulphonic acid-induced colitis. Br J Pharm 139:209–218
Vozza A, Parisi G, De Leonardis F et al (2014) UCP2 transports C4 metabolites out of mitochondria, regulating glucose and glutamine oxidation. Proc Nat Acad Sci USA 111(3):960–965
Wang J, Pan MH, Cheng AL, Lin LI, Ho YS, Hsieh CY, Lin JK (1997) Stability of curcumin in buffer solutions and characterization of its degradation products. J Pharm Biomed Anal 15:1867–1876
Wang A, Keita AV, Phan V, McKay CM, Schoultz I, Lee J et al (2014) Targeting mitochondria-derived reactive oxygen species to reduce epithelial barrier dysfunction and colitis. Am J Pathol 184:2516–2527
Wei QY, Chen WF, Zhou B, YangL LZL (2006) Inhibition of lipid peroxidation and protein oxidation in rat liver mitochondria by curcumin and its analogues. Biochim Biophys Acta 1760:70–77
Wong HS, Dighe PA, Mezera V, Monternier PA, Brand MD (2017) Production of superoxide and hydrogen peroxide from specific mitochondrial sites under different bioenergetic conditions. J Biol Chem 292:16804–16809
Yamaoka T, Yan F, Hanwei C, Hobbs S, Dise RS, Tong W, Polik DB (2008) Transactivation of EGF receptor and ErbB2 protects intestinal epithelial cells from TNF-induced apoptosis. Proc Natl Acad Sci USA 105:11772–11777
Yin H, Zhu M (2012) Free radical oxidation of cardiolipin: chemical mechanisms, detection and implication in apoptosis, mitochondrial dysfunction and human diseases. Free Radic Res 46(8):959–974
Zádor F, Wollemann M (2015) Receptome: interactions between three pain-related receptors or the “Triumvirate” of cannabinoid, opioid and TRPV1 receptors. Pharmacol Res 102:254–263
Zorov DB, Juhaszova M, Sollott SJ (2014) Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol Rev 94(3):909–950
Acknowledgements
We are grateful to Dr Dang MC and Dr El Benna J from “the Laboratoire d'Excellence Inflamex”, Faculté de Médecine, Site Xavier Bichat, Paris, France, for the kind gift of TNBS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mouzaoui, S., Banerjee, S. & Djerdjouri, B. Low-dose curcumin reduced TNBS-associated mucin depleted foci in mice by scavenging superoxide anion and lipid peroxides, rebalancing matrix NO synthase and aconitase activities, and recoupling mitochondria. Inflammopharmacol 28, 949–965 (2020). https://doi.org/10.1007/s10787-019-00684-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10787-019-00684-4