Abstract
Interleukin-17A (IL-17A) is involved in multiple inflammatory diseases. Our study was to investigate the role of IL-17A on acute lung injury (ALI) respectively induced by lipopolysaccharide (LPS) and paraquat (PQ) on mice. We built ALI mouse models respectively by single intraperitoneal (i.p.) injection with LPS or single gavage with PQ liquid. Two hours after the models were established, a dosage of neutralizing antibody was used to blockade IL-17A by i.p. injection. At 8, 24, and 48 h, the lung wet-to-dry ratio (W/D) was calculated and total protein in bronchoalveolar lavage fluid (BALF) was measured; hematoxylin-eosin staining was used to observe lung tissue pathological changes; inflammatory cells in BALF were recorded with a hemocytometer; cytokines were measured with enzyme-linked immunosorbent assay kits; immunohistochemistry examined the expression of IL-17A and activation of nuclear factor-κB p65 (NF-κB p65); and qPCR determined the expression of IL-17A mRNA. After being administered with LPS or PQ, all mice presented ALI pathological change; expression of IL-17A increased significantly. When blocking IL-17A with antibody, lung injury in both LPS- and PQ-administrated mice was attenuated. All the above tests decreased. Compared with those in PQ mice, IL-17A levels in LPS mice were higher. IL-17A involves the ALI induced by LPS or PQ and promotes the pathological process by activating NF-κB P65 and recruiting neutrophils, which enlarges the cascade effect of inflammation and injures lung tissues. And when blockading IL-17A with antibody, the ALI is alleviated. The reaction of IL-17A in the ALI induced by LPS is stronger than that by PQ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
As a severe life-threatening disease, acute lung injury (ALI) is characterized by pulmonary edema, hemorrhage, inflammatory cell infiltration, and diffused alveolar capillary injury on pathology [35], and mainly presented as dyspnea, continuous hypoxemia, and tachycardia in the clinics. It is also a leading cause of morbidity and mortality in critically sick patients which can result into persistent respiratory failure or even to death [45, 47]. Multiple factors can induce ALI, such as sepsis, severe pneumonia, trauma, bleomycin (BLM), and acute paraquat (PQ) poisoning [14]. Studies indicated that various inflammatory cells and cytokines were involved in the ALI [37].
IL-17A, also known as IL-17, is a pro-inflammatory cytokine, which is mainly produced by T helper cell 17 (Th17), natural killer cells, and neutrophils [24]. IL-17A has been considered crucial in a multitude of inflammatory diseases, both autoimmune and acquired: rheumatoid arthritis [22], multiple sclerosis [50], psoriasis [20, 43], systemic sclerosis [9, 18], Crohn’s disease [10, 40], systemic lupus erythematosus [34], Behçet’s disease [12], and Job’s syndrome [25]. It has also been thought that IL-17A stimulates epithelial cell secretion of CXCL8, CXCL1, CXCL5, G-CSF, and GM-CSF, which in turn recruit neutrophil to induce asthma [1, 4]. Recent studies found that neutralizing IL-17A with antibody or knockout IL-17A gene can attenuate neutrophil activation in lung early injury induced by silica particles or BLM, which improved the pulmonary fibrosis in the later period [5, 21, 24]. Furthermore, IL-17A aggravates cecal ligation and puncture (CLP)-induced sepsis, and high expression of IL-17A in lung was closely related to lipopolysaccharide (LPS)-induced ALI [36]. The abovementioned prompted us to study the effect of IL-17A on ALI.
Infection and acute PQ poisoning are the most common factors of ALI in our Emergency Intensive Care Unit (EICU); therefore, we used LPS or PQ respectively to build ALI mouse models, then blockade IL-17A with neutralizing antibody in vivo to investigate the effect of IL-17A on ALI induced by different agents.
MATERIALS AND METHODS
Animals
Healthy female Institute of Cancer Research (ICR) mice (SPF grade, 6–8 weeks, 26–30 g in body weight) were purchased from Liaoning Changsheng Biological Technology Company (animal production license no.: SCXK (l) 2015-0001). Mice were kept under a 12-h light/12-h dark cycle with free access to food and water for 1 week prior to the experimental procedures in the Animal Lab of China Medical University Science Experiment Center. Animal experiments were all in accordance with ethical policies of the Institutional Animal Ethics Committee and Animal Care Guidelines of China Medical University.
Animal Grouping and Model Establishment
LPS (L2880-25 mg, Sigma-Aldrich, USA) was dissolved in 0.9% saline solution (0.5 mg/ml), and 25% PQ liquid (Shaanxi Galen, Crop Science Co., Ltd, Xi’an, China) was diluted into 5 mg/ml with 0.9% saline solution. A total of 195 female mice were randomly and evenly divided into 13 groups: NS group, LPS group (3 groups), LPS + Ab group (3 groups), PQ group (3 groups), and PQ + Ab group (3 groups), with 15 mice in each group. Mice in the NS group were treated with equal volume of physiological saline by single gastric gavage. Mice in the LPS group and LPS + Ab group were i.p. injected with LPS solution (20 ml/kg); mice in the PQ group and PQ + Ab group were exposed to PQ solution by single gastric gavage (5 ml/kg). LPS + Ab group and PQ + Ab group mice were i.p. injected with IL-17A-neutralizing antibody (5 mg/kg) (eBiosicence, San Diego, USA) 2 h after LPS and PQ were treated. All of the above managements were one-off and free of contamination.
Specimen Harvest
At 8, 24, and 48 h after being treated with LPS and PQ, living mice from each group were anesthetized with i.p. injection with 10% chloral hydrate (0.3 ml/100 g) (from pharmacy of the emergency department). Peripheral blood was collected to obtain serum for cytokine assay. Six mouse tracheas were cannulated, and each mouse was lavaged with phosphate-buffered saline (PBS) three times immediately after blood was collected. Afterwards, bronchoalveolar lavage fluid (BALF) was collected and the volume was recorded. Then, BALF was mixed well and centrifuged (1500 rpm, 4 °C) for 10 min. Supernatants were stored at −80 °C for total protein analysis and cytokine assay, and pellets were prepared for inflammatory cell counts. The remaining living mice were used for lung tissue detection: right lung tissues for lung wet/dry (W/D) weight ratio calculation, left upper lung tissues for histological study, and left lower lung tissues for qPCR test.
W/D Ratio Calculation
Right lungs were cleared and weighed immediately to obtain the “wet” weight, and then placed in an oven at 60 °C for 72 h to obtain the “dry” weight. The ratio of the wet lung to the dry lung was calculated.
ELISA for Cytokines in Serum and BALF
IL-17A, IL-6, and TNF-α in serum and IL-17A in BALF were detected by enzyme-linked (ELISA) kits (Bioss, Beijing, China) according to the manufacturer’s instructions.
Total Protein Analysis in BALF
Total protein content in BALF was measured by the Bradford method using Coomassie Brilliant Blue G-250 kits (Solarbio, Beijing, China); operations were in accordance with the manufacturer’s instructions.
Inflammatory Cell Counts in BALF
BALF pellets were resuspended in 0.3 ml saline solution. Total number of leukocytes and neutrophils was calculated with a hemocytometer.
Tissue Preparation and Histological Study
Left upper lung tissues were fixed with 10% neutral formalin, embedded in paraffin, and sliced at a thickness of 5 μm.
Histology of lung was examined under the microscope with hematoxylin–eosin staining and then evaluated using a semi-quantitative scoring method. Lung injury was graded from 0 (normal) to 4 (severe) in four categories: interstitial inflammation, inflammatory cell infiltration, congestion, and edema: 0 for no injury, 1 for injury <25%, 2 for injury ranging from 25 to 50%, 3 for 50 to 75%, and 4 for injury >75%. Total score was calculated by adding up the individual score of each category [41].
Immunohistochemistry for IL-17A and NF-κB p65
Lung slides were dewaxed and hydrated. The antigens were repaired in sodium citrate at pH 6.0 by a microwave for 10 min. Endogenous peroxidase was inactivated by 3% H2O2 for 15 min. Goat serum (SL2-10, Solarbio, Beijing, China) was used to block non-specific antigen sites for 15 min. Then, the slides were incubated successionally with diluted primary antibody (IL-17A for 1:50; NF-κB p65 for 1:100) (IL-17A:130-82-1-AP; NF-κB p65:8242P; Proteintech, Wuhan, China) overnight at 4 °C. The sections were then washed with PBS and incubated with biotin-conjugated secondary antibody (1:200 diluted) for 30 min at 37 °C; then, streptavidin/HRP was added and 100 μl diaminobenzidine (DAB) was added until reaction terminated by tap water, with dyeing time controlled under a microscope. Finally, the slides were re-dyed with hematoxylin (Solarbio, Beijing, China), dehydrated, vitrified, and mounted before being observed under a light microscope. Negative controls were generated by omitting the primary antibodies. The results were evaluated semi-quantitatively according to the percentage of positive cells in five randomly selected fields under 400-fold magnification and then pictures were taken, for the score of positive cell ratio; 0–1, 1–10, 10–50, 50–80, and 80–100% were scored as 0, 1, 2, 3, and 4, respectively. For intensity score, negative, weakly positive, positive, and strongly positive were scored as 0, 1, 2, and 3, respectively. IHC score value = positive cell ratio score × intensity score [15].
Microscopic observation was performed by two experienced pathologists who were blinded to the treatment group.
Expression of IL-17A mRNA in Lung Tissues
The expression of IL-17A messenger RNA (mRNA) in lung tissues was assayed by qPCR. Lung tissues used for qPCR were stored at −80 °C, and total RNA was isolated from lung homogenates with TRIzol reagent (15596026, Invitrogen, San Diego, CA, USA), then RT Kit (TaKaRa, Dalian, CHN) was used to perform the reverse transcription (RT) reaction in the 20 μl system. qPCR reaction was performed in the 20 μl system containing 10 μl SYBR® Premix Ex Taq™, 0.8 μl forward primer (10 μM), 0.8 μl reverse primer (10 μM), 1.6 μl cDNA template, and 6.8 μl distilled H2O (dH2O). The PCR program was as follows: 37 °C reverse transcription for 15 min, 85 °C pre-denaturation for 2 min, 95 °C denaturation for 30 s, 40 °C annealing for 30s, and 40 cycles on 96 Real-Time Quantitative LightCycler 480 Instrument II (Roche, Switzerland/ Germany). GAPDH was used for an internal control, and relative gene expression was calculated using the IL-17A/GAPDH ratios. IL-17A and GAPDH mRNA sequences were referred from PubMed database. All the primers (Sangon, Shanghai, China) were designed with Primer 5.0. A solubility curve was drawn at the same time to ensure the specificity of fluorescent qPCR. The primers used were listed as follows: IL-17A (344 bp), forward 5′-TGTCAATGCGGAGGGAAAG-3′, reverse 5′-GCAGTTTGGGACCCCTTTAC-3′; GAPDH (183 bp), forward 5′-GGTTGTCTCCTGCGACTTCA-3′, reverse 5′-TGGTCCAGGGTTTCTTACTC-3′.
STATISTICAL ANALYSIS
All data were following a normal distribution and expressed as means ± standard deviation (SD). Statistical analysis was performed with SPSS 22.0 version (SPSS, Chicago, IL), statistical differences were determined by one-way analysis of variance (one-way ANOVA), followed by least significant difference test (LSD-t) or Games-Howell test for multiple comparisons, and P < 0.05 was considered to be statistically significant.
RESULTS
Symptoms on Mice
There were no evident symptoms on mice in the NS group. The LPS group, LPS + Ab group, PQ group, and PQ + Ab group mice showed a series of symptoms such as listlessness, decreased activity, sluggishness, tachypnea, and an increase in oral secretions. Symptoms on the LPS + Ab group and PQ + Ab group mice were milder than those on the LPS group and PQ group; there was no significant difference between the LPS group and PQ group.
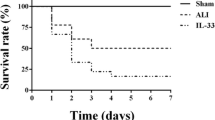
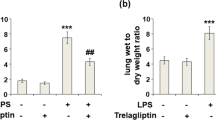
Lung Wet/Dry Weight Ratio
Lung W/D increased gradually in the LPS group, LPS + Ab group, PQ group, and PQ + Ab group. Compared with the LPS group, lung W/D in the LPS + Ab group decreased (P < 0.05). Compared with the PQ group, lung W/D in the PQ + Ab group decreased (P < 0.05). There was no difference between the LPS and PQ groups (P > 0.05) (Fig. 1a).
Total Protein in BALF
Compared with the NS group, total protein in BALF of the LPS group, LPS + Ab group, PQ group, and PQ + Ab group increased (P < 0.01). Compared with the LPS group, BALF protein in the LPS + Ab group decreased (P < 0.01). Compared with the PQ group, BALF protein in the PQ + Ab group decreased (P < 0.01). BALF protein in the PQ group approximated that in the LPS group (Fig. 1b).
Lung Pathological Change
Serious pulmonary hemorrhage and swelling were observed in the LPS group, LPS + Ab group, PQ group, and PQ + Ab group mice. Compared with the LPS and PQ groups, pulmonary hemorrhage and swelling from the LPS + Ab group and PQ + Ab group looked milder. There was no significant difference between the LPS group and the PQ group. The NS group showed no change (Fig. 2).
Observed under a light microscope, lung tissues of mice from the NS group showed a normal structure. While in the LPS group, LPS + Ab group, PQ group, and PQ + Ab group, there were great changes in the alveolar structure with inflammatory cell infiltration, and it was full of fluid in the thickened alveolar walls (Fig. 3a, b). Compared with the LPS group and PQ group, the changes in the LPS + Ab group and PQ + Ab group became milder. There was no difference in the changes between the LPS group and PQ group. Lung injury score is shown in Fig. 3c.
Cytokine Change
Compared with the NS group, both IL-17A in BALF and IL-17A, IL-6, and TNF-α in serum from the LPS group, LPS + Ab group, PQ group, and PQ + Ab group increased significantly (P < 0.01); TNF-α in serum peaked at 24 h. Compared with the LPS group and PQ group, levels of IL-17A, IL-6, and TNF-α in the LPS + Ab group and PQ + Ab group decreased, respectively (P < 0.01); the level of IL-17A in BALF in the LPS group was higher than that in the PQ group (P < 0.01). For the levels of IL-6 and TNF-α in serum, there was no significant difference between the LPS group and PQ group (P > 0.05) (Fig. 4).
Expression of IL-17A and NF-κB p65 by IHC
IL-17A-positive cells were stained brown or dark brown mainly in the cytoplasm (Fig. 5). As for NF-κB p65, in the NS group, brown granules were mainly in the cytoplasm, but in the LPS group, LPS + Ab group, PQ group, and PQ + Ab group, brown granules were mainly in the cell nucleus (Fig. 6). The IHC scores are shown in Fig. 7.
Inflammatory Cell Counts in BALF
Compared with the NS group, BALF leucocytes and neutrophils in the LPS group, LPS + Ab group, PQ group, and PQ + Ab group significantly increased (P < 0.01). Compared with the LPS group and PQ group, leucocytes and neutrophils in the LPS + Ab group and PQ + Ab group decreased (P < 0.05). There was no significant difference between the LPS group and PQ group (P > 0.05) (Fig. 8).
Expression of IL-17A mRNA in Lung Tissues
As is shown in Fig. 9, expression of lung tissue IL-17A mRNA in the LPS group, LPS + Ab group, PQ group, and PQ + Ab group was higher than that in the NS group (P < 0.01). Compared with the LPS group and PQ group, expression of IL-17A mRNA in the LPS + Ab group and PQ + Ab group decreased (P < 0.05). IL-17A mRNA expression in the LPS group was higher than that in the PQ group (P < 0.05).
DISCUSSION
Our experiments indicated that mice showed symptoms of ALI in succession such as sluggishness, less activity, tachypnea, increased oral secretions, and lip cyanosis after administration with LPS or PQ. Meanwhile, serious pulmonary congestion and edema were observed on the mice. As is well known to all, being a component of the gram-negative bacteria wall, LPS is a primary cause of ALI induced by sepsis which can prompt inflammatory cell activation and cytokine secretion [37, 38]. As a highly efficient vegetative herbicide, PQ is also highly toxic to humans that mainly damages lungs once taken in by the human body. It also can lead to alveolar epithelial cell disruption, alveolar edema, hemorrhage, and infiltration of inflammatory cells [38]. A large number of studies revealed that inflammatory mediators infiltrated and accumulated in the alveolar space leading to the destruction of alveoli which is the main pathology change of ALI [8, 38, 46, 49, 51]. In our experiments, mice which were treated with LPS and PQ presented an increase in lung W/D ratios and BALF proteins. Furthermore, disruption of alveolar structure and infiltration of inflammatory cells were observed under the microscope, and the alveolar space was full of fluids along with alveolar septa thickening. The ALI changes were consistent with previous researches [7, 46].
Previous studies confirmed that LPS can not only damage the alveolar endothelial cells in a direct way but also activate inflammatory cells to release cytokines to injury lung tissues indirectly, such as IL-6 and TNF-α [16, 23, 26, 49]. Meanwhile, studies on ALI induced by PQ poisoning indicate that oxygen free radicals trigger the release of inflammatory mediators to aggravate lung tissue injury [19]. IL-6 and TNF-α have been demonstrated to magnify and maintain inflammatory response in the process of ALI by many researches [13, 23, 26]. In our experiments, IL-6 and TNF-α increased significantly after administration with LPS and PQ. Moreover, along with the increased expression of IL-17A in lung tissues, the content of IL-17A in serum and BALF elevated markedly. Blockading IL-17A with antibody decreased the levels of IL-17A in serum and BALF, and the lung tissue injury attenuated evidently; meanwhile, the W/D ratio and BALF content declined. However, IL-17A continuously elevated at the observation time which was different from TNF-α, which may be related to the role of IL-17A in maintaining the inflammatory response.
IL-17A regulates innate responses of various cells including neutrophils and macrophages to prompt the local inflammation [33]. It is also involved in the neutrophil recruitment to the airway and the induction of pro-inflammatory cytokines from pulmonary capillaries to alveoli [32]. Our experiments show that neutrophils in BALF increased after the mice were administered with LPS and PQ; neutralizing IL-17A with antibody decreased neutrophils in BALF, which was consistent with a previous study [21]. IL-17A recruits neutrophils to participate in the ALI process on LPS and PQ mice.
As a nuclear transcription factor, NF-κB plays a crucial role in regulating gene transcription in inflammatory response [6]. p65 protein is a subunit of NF-κB which activates cytokines to enlarge the cascade effect in the response by promoting related gene transcription [2]. While being stimulated by infection or cytokines, free p65 transferred quickly to the nucleus and bonded the specificity of gene sequences into the NF-κB, which prompts the cytokine release [2, 28]. IL-17A has been reported to activate p65 in mouse lung which results into the large secretion of TNF-α to damage the lung [29, 42]. In our experiments, activated NF-κB p65 increased in LPS and PQ poisoning mouse lung tissues. Blockading IL-17A reduced the activation of NF-κB p65, meanwhile the levels of IL-6 and TNF-α decreased. IL-17A has been reported to induce respiratory epithelial cells to secrete IL-6 [27, 31], but other reports said IL-6 induces T cells to differentiate into Th17 cells to excrete IL-17A [30]. On all accounts, in our experiments, blockade with IL-17A antibody reduced cells which produce IL-17A and decreased the expression of IL-17A mRNA while it reduced IL-6 and TNF-α in serum.
Comparing the difference of IL-17A between LPS and PQ mice, we found that levels of IL-17A in LPS mice were higher than those in PQ poisoning mice in both serum and BALF, and the expression of IL-17A in LPS mouse lung was higher than that in PQ poisoning mice. This may be due to the different mechanisms between LPS and PQ induced to ALI: On the one hand, LPS directly stimulates the γδT cell secretion of IL-17A [39]; on the other hand, LPS bonding to toll-like receptor-4 (TLR-4) prompts the nuclear transcription factor to produce IL-17A indirectly. Meanwhile, IL-17A upregulates the endoplasmic reticulum stress (ER stress) to activate the NF-κB, and then increase IL-17A in a positive feedback way [17, 44] (Fig. 10a). However, a large amount of active oxygen (reactive oxygen species, ROS) was produced to activate oxidative stress which causes cell lipid peroxidation injury and apoptosis in the lung tissues after PQ intoxication [3]. ROS can activate the NF-κB nuclear transfer to increase the IL-17A production [11, 17]. Meanwhile, cells produce IL-6 and TNF-α which can not only prompt T cells to differentiate to γδT cells but also activate NF-κB to produce IL-17A [48] (Fig. 10b). It has been confirmed that ROS plays a pivotal role in the PQ poisoning lung injury although inflammatory injury plays an important role in the development of ALI [16, 19].
In conclusion, IL-17A is involved in the ALI process induced by LPS or PQ, and promotes the pathological process by activating NF-κB p65 and recruiting neutrophils to enlarge the cascade effect of inflammation to injure lung tissues. Blockading IL-17A with antibody can alleviate the ALI process. But the reaction of IL-17A in the ALI induced by LPS is stronger than that by PQ.
References
Afzali, B., P. Mitchell, R.I. Lechler, S. John, and G. Lombardi. 2010. Translational mini-review series on Th17 cells: induction of interleukin-17 production by regulatory T cells. Clinical and Experimental Immunology 159 (2): 11.
Baeuerle, P.A., and D. Baltimore. 1989. A 65-kappaD subunit of active NF-kappaB is required for inhibition of NF-kappaB by I kappaB. Genes & Development 3 (11): 10.
Black, A.T., J.P. Gray, M.P. Shakarjian, D.L. Laskin, D.E. Heck, and J.D. Laskin. 2008. Increased oxidative stress and antioxidant expression in mouse keratinocytes following exposure to paraquat. Toxicology and Applied Pharmacology 231 (3): 9.
Brandt, E.B., M.B. Kovacic, G.B. Lee, A.M. Gibson, T.H. Acciani, T.D. Le Cras, P.H. Ryan, A.L. Budelsky, and G.K. Khurana Hershey. 2013. Diesel exhaust particle induction of IL-17A contributes to severe asthma. The Journal of Allergy and Clinical Immunology 132 (5): 11.
Braun, R.K., C. Ferrick, P. Neubauer, M. Sjoding, A. Sterner-Kock, M. Kock, L. Putney, D.A. Ferrick, D.M. Hyde, and R.B. Love. 2008. IL-17 producing gammadelta T cells are required for a controlled inflammatory response after bleomycin-induced lung injury. Inflammation 31 (3): 13.
Brennenstuhl, H., A. Armento, A.K. Braczysnki, M. Mittelbronn, and U. Naumann. 2015. IκBζ, an atypical member of the inhibitor of nuclear factor kappa B family, is induced by γ-irradiation in glioma cells, regulating cytokine secretion and associated with poor prognosis. International Journal of Oncology 47 (5): 10.
Chen, D., T. Ma, X.W. Liu, C. Yang, and Z. Liu. 2015. Rapamycin Reverses Paraquat-Induced Acute Lung Injury in a Rat Model through Inhibition of NFkB Activation. International Journal of Clinical and Experimental Pathology 8 (5): 12.
Crimi, E., and A.S. Slutsky. 2004. Inflammation and the acute respiratory distress syndrome. Best Practice & Research. Clinical Anaesthesiology 18 (3): 16.
Dańczak-Pazdrowska, A., M. Kowalczyk, B. Szramka-Pawlak, J. Gornowicz-Porowska, A. Szewczyk, W. Silny, A. Olewicz-Gawlik, M. Molińska-Glura, R. Zaba, and P. Hrycaj. 2012. Interleukin-17A and interleukin-23 in morphea. Archives of Medical Science 8 (6): 7.
Dige, A., S. Støy, T.K. Rasmussen, J. Kelsen, C.L. Hvas, T.D. Sandahl, J.F. Dahlerup, B. Deleuran, and J. Agnholt. 2013. Increased levels of circulating Th17 cells in quiescent versus active Crohn’s disease. Journal of Crohn’s & Colitis 7 (3): 8.
Gawarammana, I.B., and N.A. Buckley. 2011. Medical management of paraquat ingestion. British Journal of Clinical Pharmacology 72 (5): 13.
Geri, G., B. Terrier, M. Rosenzwajg, B. Wechsler, M. Touzot, D. Seilhean, T.A. Tran, B. Bodaghi, L. Musset, V. Soumelis, D. Klatzmann, P. Cacoub, and D. Saadoun. 2011. Critical role of IL-21 in modulating TH17 and regulatory T cells in Behçet disease. The Journal of Allergy and Clinical Immunology 128 (3): 10. doi:10.1016/j.jaci.2011.05.029.
Hemmati, A.A., Z. Nazari, M.E. Motlagh, and S. Goldasteh. 2002. The role of sodium cromolyn in treatment of paraquat-induced pulmonary fibrosis in rat. Pharmacological Research 46 (3): 6.
Jones, R., A.M. Baetjer, and L. Reid. 1971. Effect of extremes of temperature and humidity on the goblet cell count in the rat airway epithelium. British Journal of Industrial Medicine 28 (4): 5.
Kaemmerer, D., L. Peter, A. Lupp, S. Schulz, J. Sänger, R.P. Baum, V. Prasad, and M. Hommann. 2012. Comparing of IRS and Her2 as immunohistochemical scoring schemes in gastroenteropancreatic neuroendocrine tumors. International Journal of Clinical and Experimental Pathology 5 (3): 8.
Kim, J.H., H.W. Gil, J.O. Yang, E.Y. Lee, and S.Y. Hong. 2010. Effect of glutathione administration on serum levels of reactive oxygen metabolites in patients with paraquat intoxication: a pilot study. The Korean Journal of Internal Medicine 25 (3): 6.
Kim, S.R., H.J. Kim, D.I. Kim, K.B. Lee, H.J. Park, J.S. Jeong, S.H. Cho, and Y.C. Lee. 2015. Blockade of Interplay between IL-17A and Endoplasmic Reticulum Stress Attenuates LPS-Induced Lung Injury. Theranostics 5 (12): 20.
Kurasawa, K., K. Hirose, H. Sano, H. Endo, H. Shinkai, Y. Nawata, K. Takabayashi, and I. Iwamoto. 2000. Increased interleukin-17 production in patients with systemic sclerosis. Arthritis and Rheumatism 43 (11): 9.
Frank, L. 1981. Prolonged survival after paraquat. Role of the lung antioxidant enzyme systems. Biochemical Pharmacology 30 (16): 6.
Li, J., X. Chen, Z. Liu, Q. Yue, and H. Liu. 2007. Expression of Th17 cytokines in skin lesions of patients with psoriasis. Journal of Huazhong University of Science and Technology. Medical Sciences 27 (3): 3.
Li, J., Y. Zhang, J. Lou, J. Zhu, M. He, X. Deng, and Z. Cai. 2012. Neutralisation of peritoneal IL-17A markedly improves the prognosis of severe septic mice by decreasing neutrophil infiltration and proinflammatory cytokines. Plos One 7(10): e46506.
Li, N., J.C. Wang, T.H. Liang, M.H. Zhu, J.Y. Wang, X.L. Fu, J.R. Zhou, S.G. Zheng, P. Chan, and J. Han. 2013. Pathologic finding of increased expression of interleukin-17 in the synovial tissues of rheumatoid arthritis patients. International Journal of Clinical and Experimental Pathology 6 (7): 5.
Liu, W., L.P. Shan, X.S. Dong, X.W. Liu, T. Ma, and Z. Liu. 2013. Effect of early fluid resuscitation on the lung in a rat model of lipopolysaccharide-induced septic shock. European Review for Medical and Pharmacological Sciences 17 (2): 9.
Lo Re, S., L. Dumoutier, I. Couillin, C. Van Vyve, Y. Yakoub, F. Uwambayinema, B. Marien, S. van den Brûle, J. Van Snick, C. Uyttenhove, B. Ryffel, J.C. Renauld, D. Lison, and F. Huaux. 2010. IL-17A-producing gammadelta T and Th17 lymphocytes mediate lung inflammation but not fibrosis in experimental silicosis. Journal of Immunology 184 (11): 11.
Ma, C.S., G.Y. Chew, N. Simpson, A. Priyadarshi, M. Wong, B. Grimbacher, D.A. Fulcher, S.G. Tangye, and M.C. Cook. 2008. Deficiency of Th17 cells in hyper IgE syndrome due to mutations in STAT3. The Journal of Experimental Medicine 205 (7): 7.
Ma, T., and Z. Liu. 2013. Functions of aquaporin 1 and α-epithelial Na+ channel in rat acute lung injury induced by acute ischemic kidney injury. International Urology and Nephrology 45 (4): 10. doi:10.1007/s11255-012-0355-1.
McAllister, F., A. Henry, J.L. Kreindler, P.J. Dubin, L. Ulrich, C. Steele, J.D. Finder, J.M. Pilewski, B.M. Carreno, S.J. Goldman, J. Pirhonen, and J.K. Kolls. 2005. Role of IL-17A, IL-17F, and the IL-17 receptor in regulating growth-related oncogene-alpha and granulocyte colony-stimulating factor in bronchial epithelium: implications for airway inflammation in cystic fibrosis. Journal of Immunology 175 (1): 9.
Metelev, V.G., E.A. Kubareva, and T.S. Oretskaya. 2013. Regulation of activity of transcription factor NF-κB by synthetic oligonucleotides. Biochemistry (Mosc) 78 (8): 12.
Mi, S., Z. Li, H. Liu, Z.W. Hu, and F. Hua. 2012. Blocking IL-17A protects against lung injury-induced pulmonary fibrosis through promoting the activation of p50NF-kappaB. Yao Xue Xue Bao 47 (6): 6.
Mi, S., Z. Li, H.Z. Yang, H. Liu, J.P. Wang, Y.G. Ma, X.X. Wang, H.Z. Liu, W. Sun, and Z.W. Hu. 2011. Blocking IL-17A promotes the resolution of pulmonary inflammation and fibrosis via TGF-beta1-dependent and -independent mechanisms. Journal of Immunology 187 (6): 12.
Nembrini, C., B.J. Marsland, and M. Kopf. 2009. IL-17-producing T cells in lung immunity and inflammation. The Journal of Allergy and Clinical Immunology 123 (5): 9.
Numasaki, M., H. Takahashi, Y. Tomioka, and H. Sasaki. 2004. Regulatory roles of IL-17 and IL-17F in G-CSF production by lung microvascular endothelial cells stimulated with IL-1beta and/or TNF-alpha. Immunology Letters 95 (1): 8.
Peck, A., and E.D. Mellins. 2009. Breaking old paradigms: Th17 cells in autoimmune arthritis. Clinical Immunology 132 (3): 10.
Perry D, Peck AB, Carcamo WC, Morel L, Nguyen CQ. 2011. The current concept of T (h) 17 cells and their expanding role in systemic lupus erythematosus. Arthritis.
Pugin, J., G. Verghese, M.C. Widmer, and M.A. Matthay. 1999. The alveolar space is the site of intense inflammatory and profibrotic reactions in the early phase of acute respiratory distress syndrome. Critical Care Medicine 27 (2): 9.
Ran, W.Z., L. Dong, C.Y. Tang, Y. Zhou, G.Y. Sun, T. Liu, Y.P. Liu, and C.X. Guan. 2015. Vasoactive intestinal peptide suppresses macrophage-mediated inflammation by downregulating interleukin-17A expression via PKA- and PKC-dependent pathways. International Journal of Experimental Pathology 96 (4): 7.
Rittirsch, D., M.A. Flierl, D.E. Day, B.A. Nadeau, S.R. McGuire, L.M. Hoesel, K. Ipaktchi, F.S. Zetoune, J.V. Sarma, L. Leng, M.S. Huber-Lang, T.A. Neff, R. Bucala, and P.A. Ward. 2008. Acute lung injury induced by lipopolysaccharide is independent of complement activation. Journal of Immunology 180 (11): 9.
Rose, M.S., L.L. Smith, and I. Wyatt. 1974. Evidence for energy-dependent accumulation of paraquat into rat lung. Nature 252 (5481): 2.
Sakaguchi, R., S. Chikuma, T. Shichita, R. Morita, T. Sekiya, W. Ouyang, T. Ueda, H. Seki, H. Morisaki, and A. Yoshimura. 2016. Innate-like function of memory Th17 cells for enhancing endotoxin-induced acute lung inflammation through IL-22. International Immunology 28 (5): 11.
Siakavellas, S.I., and G. Bamias. 2012. Role of the IL-23/IL-17 axis in Crohn’s disease. Discovery Medicine 14 (77): 10.
Smith, K.M., J.D. Mrozek, S.C. Simonton, D.R. Bing, P.A. Meyers, J.E. Connett, and M.C. Mammel. 1997. Prolonged partial liquid ventilation using conventional and high-frequency ventilatory techniques: gas exchange and lung pathology in an animal model of respiratory distress syndrome. Critical Care Medicine 25 (11): 10.
Song, X., and Y. Qian. 2013. IL-17 family cytokines mediated signaling in the pathogenesis of inflammatory diseases. Cellular Signalling 25 (12): 13.
Raychaudhuri, S.P. 2013. Role of IL-17 in psoriasis and psoriatic arthritis. Clinical Reviews in Allergy & Immunology 44 (2): 11.
Togbe, D., S. Schnyder-Candrian, B. Schnyder, I. Couillin, I. Maillet, F. Bihl, D. Malo, B. Ryffel, and V.F. Quesniaux. 2006. TLR4 gene dosage contributes to endotoxin-induced acute respiratory inflammation. Journal of Leukocyte Biology 80 (3): 7.
Vadász, I., and J.I. Sznajder. 2011. Update in acute lung injury and critical care 2010. American Journal of Respiratory and Critical Care Medicine 183 (9): 6.
Wang, X.Q., X. Zhou, Y. Zhou, L. Rong, L. Gao, and W. Xu. 2008. Low-dose dexamethasone alleviates lipopolysaccharide-induced acute lung injury in rats and upregulates pulmonary glucocorticoid receptors. Respirology 13 (6): 9.
Ware, L.B., and M.A. Matthay. 2000. The acute respiratory distress syndrome. The New England Journal of Medicine 342 (18): 16.
Wing, K., Z. Fehérvári, and S. Sakaguchi. 2006. Emerging possibilities in the development and function of regulatory T cells. International Immunology 18 (7): 10.
Worthen, G.S., C. Haslett, A.J. Rees, R.S. Gumbay, J.E. Henson, and P.M. Henson. 1987. Neutrophil-mediated pulmonary vascular injury. Synergistic effect of trace amounts of lipopolysaccharide and neutrophil stimuli on vascular permeability and neutrophil sequestration in the lung. The American Review of Respiratory Disease 136 (1): 10.
Zepp, J., L. Wu, and X. Li. 2011. IL-17 receptor signaling and T helper 17-mediated autoimmune demyelinating disease. Trends in Immunology 32 (5): 8.
Zhang, H., and G.Y. Sun. 2005. LPS induces permeability injury in lung microvascular endothelium via AT(1) receptor. Archives of Biochemistry and Biophysics 441 (1): 9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Animal experiments were all in accordance with ethical policies of the Institutional Animal Ethics Committee and Animal Care Guidelines of China Medical University.
Funding
This study was funded by the Science and Technology Program of Liaoning Province (Grant Number 2013225303) and Natural Science Foundation of China (Grant Number 81571882).
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Song, Hw., Yang, C., Liu, W. et al. Interleukin-17A Plays the Same Role on Mice Acute Lung Injury Respectively Induced by Lipopolysaccharide and Paraquat. Inflammation 40, 1509–1519 (2017). https://doi.org/10.1007/s10753-017-0592-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-017-0592-7