Abstract
The objective of the study is to investigate the role and specific molecular mechanism of interleukin-33 (IL-33) acted on acute lung injury (ALI) induced by lipopolysaccharide (LPS). C57BL/6 mice intratracheally instilled LPS to induce ALI model. The mice were randomly divided into three groups: the sham operation group (Sham), ALI group (ALI), and pretreatment with IL-33 of ALI group (IL-33). By observing the survival rate, inflammatory cytokines in bronchoalveolar lavage fluid (BALF), myeloperoxidase (MPO) levels in lung tissue, lung histopathological examination, pulmonary capillary leakage, lung wet/dry (W/D) weight ratio, fibrosis levels in lung tissue, and associated pathways changes among the different groups, comparing to explore the role of IL-33 pretreatment on ALI mice and the possible molecular mechanisms. IL-33 pretreatment overall decreased the survival rate of ALI mice. IL-33 aggravated inflammation reaction showing as increasing the release of proinflammatory cytokines TNF-α and IL-6, increasing MPO levels in lung tissue, and aggravating lung pathology injury. In addition, IL-33 pretreatment further destroyed adherens junctions (AJs) by increasing the phosphorylation of VE-cadherin, resulting in the concomitantly pulmonary capillary barrier damage and pulmonary edema. During this process, mitogen-activated protein kinase (MAPK) pathways further activated. However, IL-33 pretreatment had no significant impact on collagen content of lung tissue. Our results indicated that IL-33 aggravated inflammatory reaction and increased microvascular permeability, but had little effect on pulmonary fibrosis, associated with the further activation of MAPK family proteins in the process. To sum up, IL-33 decreased survival rate and aggravated LPS-induced ALI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) are first described in 1967 and are characterized by the abrupt onset of serious hypoxemia with diffuse alveolar damage and pulmonary infiltrates [1, 2]. ARDS is a more serious state of ALI, and both ALI and ARDS confer a severe illness burden on the individual sufferer and society [3]. Infections, particularly those caused by gram-negative bacteria, are important causes of ALI and ARDS. Extracellular lipopolysaccharide (LPS) of gram-negative bacteria is the promoter of the innate immune response and inflammation, triggering inflammatory cells to produce miscellaneous inflammatory cytokines involved in the control of pathogens [4]. In contrast, desensitization or tolerance to LPS is characterized by a hyporesponsiveness to the subsequent endotoxin challenge due to a prior exposure to a sublethal dose of endotoxin. LPS tolerance produces much lower levels of proinflammatory cytokines such as tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6) than those stimulated with endotoxin for the first time [4]. Exacerbated response to LPS induces an overproduction of proinflammatory cytokines that are responsible for severe systemic dysfunctions. Several mechanisms involved in LPS tolerance have been described: down-regulation Toll-like receptor 4 (TLR-4) and its downstream transcription factors such as nuclear factor-kappa B (NF-κB) and activator protein 1 (AP-1) [5], modification of the myeloid differentiation factor88 (MyD88) or Toll/IL-1R domain-containing adapter inducing interferon-β (IFN-β) signaling pathways, secretion of anti-inflammatory cytokines, and so on [6].
Recent studies summarize the advances in the functional roles of IL-33 in immune regulation, inflammatory and infectious diseases to seek the therapeutic potential of targeting IL-33 [7–13]. It has been reported that the IL-1R-related protein ST2 (also known as IL-1RL1), the natural ligand of interleukin-33 (IL-33), could be involved in LPS tolerance and thus play a protective role in LPS-induced disease [7] while some other studies show an aggravated role of IL-33 in inflammatory disease and have no effect on LPS tolerance [4, 14]. Brint et al. have demonstrated that ST2 knockout (KO) mice could not be desensitized to LPS [7]. Alves-Filho et al. have indicated that IL-33 could attenuate sepsis by enhancing neutrophil influx to the site of infection [9, 10] while some in vitro experiments showed that IL-33 promoted the release of inflammatory cytokines [4, 14].
To sum up, the role of IL-33 on inflammatory diseases is ambiguous. Therefore, in this study, we investigated whether IL-33 triggering of ST2 could play a protective role in LPS-induced disease.
Practically, the study demonstrated that IL-33 could enhance LPS response with further activating mitogen-activated protein kinase (MAPK) pathways. Therefore, the application of IL-33 in inflammatory disease was controversial.
MATERIALS AND METHOD
Materials
LPS (Escherichia coli O111:B4), formamide, and evans blue were purchased from Sigma-Aldrich (Sigma-Aldrich, Milwaukee, WI, USA). IL-33 was from Enzo Life Sciences (Enzo Life Sciences, Switzerland). Enzyme-linked immunosorbent assay (ELISA) kits were purchased from R & D Systems (R & D Systems, Minneapolis, MN, USA), and myeloperoxidase (MPO) ELISA kit was from Bluegene (Bluegene, China). Sircol Soluble Collagen Assay kits were purchased from Biocolor (Biocolor, British). Abs specific for VE-cadherin, total JNK, phosphorylated JNK (p-JNK), total ERK, phosphorylated ERK (p-ERK), total p38, and phosphorylated p38 (p-p38) were from Cell Signaling Technology (Cell Signaling Technology, Danvers, MA, USA). Anti-phosphotyrosine antibody (4G10) was from Millipore Corporation (Millipore, CA, USA).
Mice
Animal procedures were carried out in compliance with Institutional Standards for Use of Laboratory Animals. Eight- to 12-week-old C57BL/6 mice were purchased from Silaike Experimental Animal Co. Ltd. (Shanghai, China). All the mice were housed in specific pathogen-free laboratory, reared in airconditioned with 6 am to 18 pm light cycle, and fed standard rodent chow ad libitum.
In Vivo Models
Briefly, the mice were randomly divided into three groups respectively. Group 1: the sham operation group (Sham); group 2: ALI group (ALI); and group 3: pretreatment with IL-33 of ALI group (IL-33). The mice in the Sham group received normal saline (NS) intraperitoneally (I.P.) for 6 h then followed by 50 μL of NS intratracheally (I.T.); the mice in the ALI group were given NS I.P. for the same time then followed by instilling of LPS (100 μg/50 μL) I.T.; the mice in the IL-33 group were injected with 1 μg IL-33 I.P. for 6 h, followed by instilling of LPS (100 μg/50 μL) I.T.. For most experiments, the mice were pretreatment with IL-33 for 6 h and stimulated with LPS for 24 h except those of observing survival rate. The dosage and time are based on the published articles [4, 9]. The mice were sacrificed by Chloraldurat, and samples were collected for the following assays. In each group, 18 mice were used to observing the survival rate; 6 mice of their left lungs were collected for histopathological examination and the right lungs were for wet/dry (W/D) weight ratio assay; another 6 mice of their lungs were used to detect alveolar capillary leakage; for the other mice in each group, bronchoalveolar lavage fluid (BALF) samples were collected for ELISA assay, and lung samples were conserved for MPO, collagen content, Western blot, and co-immunoprecipitation (Co-IP) assays.
Survival Rate of 7 Days
Eighteen mice per group were treated as mentioned and followed for 7 days to observe the survival rate. The dose of LPS was determined by preliminary experiments. Survival time was estimated using the Kaplan–Meier method. Log-rank test was used to compare survival times between the groups.
Lung Inflammation Assays
BALF Harvesting
The trachea was exposed and cannulated with a catheter. BALF samples were obtained by lavaging the lungs three times with 1 mL of iced NS. The fluid recovered after lavage was greater than 90% on average. BALF was centrifuged at 3000 rpm for 10 min at 4°C, and the supernatant was stored at −80°C for further assays.
ELISA Assay
The amounts of the cytokines TNF-α and IL-6 in the cell-free BALF were measured respectively with commercially available ELISA kits according to the manufacturer’s instructions. The absorbance values were measured at 450 nm using an ELISA reader (Bio-Rad, USA). These concentrations were interpolated from the standard curves.
MPO Determination
MPO concentrations in the lung tissues were detected using a MPO ELISA kit according to the manufacturer’s instructions. Briefly, the lung tissues were homogenized and centrifuged at 3000 rpm for 10 min at 4°C. The supernatants and standard sample were added into a microtiter plate (100 μL/well) precoated with a murine anti-MPO mAb. After incubation for 1 h at 37°C, the plate was washed for five times followed by addition of the substrate and stop solution, and was measured using a microplate reader at OD450. All the samples were assayed in triplicate.
Lung Histopathological Examination
The left lungs were fixed immediately in 10% buffered formalin (pH 7.4) for 24 h. Then, they were dehydrated in alcohol, embedded in paraffin (4 μm), and stained with hematoxylin/eosin (HE) for examination under an optical microscope (Olympus BX51, Japan). The lung injury scores were scaled from 1 to 4 and evaluated by two pathologists in a blinded fashion (1 = minimal; 2 = mild and moderate; 3 = severe; and 4 = maximal).
Pulmonary Microvascular Permeability Assays
Alveolar Capillary Leakage
Briefly, 2% evans blue dye (150 mg/kg) was injected into the tail vein and allowed to circulate in the blood vessels for 30 min. Intravascular evans blue was washed by NS perfusing from the right ventricle for 5 min. Then, the lungs were excised, weighed, homogenized, and extracted in 2 mL formamide/100 mg lung at 37°C waterbath for 24 h. Evans blue content was determined by the optical density (OD) at 620 nm of the formamide extract.
Lung W/D Weight Ratio Assay
The right lungs were removed, cleansed and weighed to obtain the wet weight, then dried in an oven at 80°C for 24 h, and weighed the weight in the every following 6 h until the dry weight invariant. The ratio of the W/D weight was calculated to assess the tissue edema.
Co-IP assay
Homogenate was immunoprecipitated with VE-cadherin antibody overnight (4°C) and subsequently incubated with Protein G Agarose beads for 4 h, washed, and resuspended. All steps were carried out at 0 to 4°C. The agarose pellets were stored at −80°C until proteins were analyzed by subsequent experiments. It is followed by immunoblotting analysis, using primary antibody of VE-cadherin and anti-phosphotyrosine antibody (4G10).
Lung Fibrosis Assays
Masson Staining of Collagen
The left lungs were fixed immediately in 10% buffered formalin (pH 7.4), embedded in paraffin, sectioned to 4-μm thick, and stained with standard Masson trichrome staining. Then, they were examined under an optical microscope (Olympus BX51, Japan).
Sircol Soluble Collagen Assay
Collagen content in the lung tissues was detected using a Sircol Soluble Collagen Assay kit according to the manufacturer’s instructions. Briefly, the lung tissues were homogenized and centrifuged at 15,000 rpm for 10 min at 4°C. The supernatants and standard sample were added into a microtiter plate (100 μL/well) followed with collagen-specific Sircol dye reagent (1 mL/well). After shaking for 30 min, the plate was centrifuged for 10 min followed by addition of the alkaline agent, and they were measured using a microplate reader at OD540. All the samples were assayed in triplicate.
Western Blot Assay
Tissues were homogenized in tissue protein extraction solution (TPER; Pierce, Rockford, IL, USA) containing 1% proteinase inhibitor cocktail. After centrifugation, the protein concentration in the supernatant was determined by Bradford assay. Equivalent amount of proteins (30 μg) was individually subjected to gel electrophoresis according to standard procedures. Incubated with relevant primary antibodies at 4°C overnight and then probed with secondary antibodies conjugated with HRP. β-actin was used as a loading control. Antigen-antibody complexes were visualized using the Pierce ECL Western blot substrate (Thermo Fisher Scientific Inc., Waltham, MA, USA). Each experiment was repeated at least three times.
Statistics
Data were showed as mean ± SD. Differences between the two groups were analyzed using one-way ANOVA, followed by Student’s t test with SPSS 16.0 Software (SPSS Inc., Chicago, IL, USA). A probability of P < 0.05 was considered statistically significant (*P < 0.05; **P < 0.01; ***P < 0.001).
RESULT
Survival Rate of 7 Days
As shown in Fig. 1, the 7-day survival rate of the Sham group was 100%. The ALI group was 50%, while the IL-33 pretreatment group decreased to 16.67%. The survival rate of the ALI group was decreased in comparison with that of the Sham group (***P < 0.001); simultaneously, pretreatment with IL-33 showed a lower survival rate than that of the ALI group (*P < 0.05).
Lung Inflammation
The proinflammatory cytokine tumor necrosis factor-α (TNF-α) and IL-6 in the ALI group were 305.15 ± 15.82 and 865.14 ± 32.65 pg/mL, respectively, while those in the IL-33 pretreatment group were 485.35 ± 22.32 and 1520.22 ± 78.23 pg/mL, respectively. The level of proinflammatory cytokines in the IL-33 pretreatment group significantly increased in comparison with that in the ALI group (***P < 0.001) (Fig. 2a, b). Pulmonary concentration of MPO was a marker of neutrophil infiltration into the lungs. ALI group lung tissue MPO concentration was 1.52 ± 0.19 μ/mg; while it was 2.21 ± 0.21 μ/mg in the IL-33 pretreatment group, IL-33 pretreatment increased lung MPO concentration (***P < 0.001) (Fig. 2c). Under light microscope, HE staining of the Sham group expressed normal lung structures, and no damage was observed. The IL-33 pretreatment caused more extensive morphological damages in the lungs than the ALI group and Sham group, which were manifested by increased alveoli congestion/hemorrhage, leukocytes infiltration, alveoli collapse, and so on. HE staining and lung injury scores results also showed that the IL-33 pretreatment aggravated lung inflammatory reaction (***P < 0.001) (Fig. 2d, e).
a b Proinflammatory factor TNF-α and IL-6 levels in BALF (***P < 0.001) (mean ± SD, n = 6). c MPO concentration in the lung tissues (***P < 0.001) (mean ± SD, n = 6). d HE staining (original magnification: ×400). e The lung injury scores (1 = minimal; 2 = mild and moderate; 3 = severe; and 4 = maximal) (***P < 0.001) (mean ± SD, n = 6).
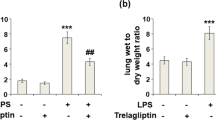
Pulmonary Microvascular Permeability
The critical feature of ALI was the destruction of vascular integrity, and the subsequent upregulated permeability would result in alveolar capillary leakage and pulmonary edema. Evans blue content extracted by formamide was a definite index of alveolar capillary leakage. Pulmonary capillary leakage of the ALI group was 245.68 ± 16.27 μg/g lung tissue while the IL-33 pretreatment group was 385.37 ± 24.35 μg/g lung tissue (***P < 0.001) (Fig. 3a). The ratio of the W/D, a measure of interstitial pulmonary edema, and severity of ALI, showed similar results with that of capillary leakage. The W/D weight ratio of the ALI group was 5.25 ± 0.58, and that of the IL-33 pretreatment group increased to 6.38 ± 0.59 (**P < 0.01) (Fig. 3b). As shown in Fig. 3c, the Sham group had no phosphorylation of adherens junctions (AJs) protein and VE-cadherin protein; the ALI group appeared phosphorylation of VE-cadherin protein; however, the IL-33 pretreatment group had more phosphorylation of VE-cadherin.
Pulmonary Fibrosis Level
Masson staining of collagen showed no collagen in the Sham group, ALI group, and IL-33 pretreatment group, which was visible coloration of collagen (Fig. 4a). The content of collagen of lung tissue in the Sham group was 8.12 ± 1.25 mg/g, while that in the ALI group was 29.25 ± 3.85 mg/g and that in the IL-33 pretreatment group was 32.13 ± 4.45 mg/g. The content of collagen of lung tissue in the ALI group increased significantly compared to that in the Sham group (**P < 0.01) (Fig. 4b), but the IL-33 pretreatment group had no significant difference compared to that in the ALI group (P > 0.05). As evidenced by Masson trichrome staining, along with the content of soluble collagens, the ALI group accompanied with obvious pulmonary tissue fibrosis; however, the IL-33 pretreatment group had no significant effect on pulmonary fibrosis formation.
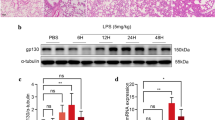
The Activation of MAPK Pathways
As shown in Fig. 5, the expression levels of p-ERK, p-JNK, and p-p38 were upregulated both in the ALI group and IL-33 group while a more remarkable upregulation was observed in the IL-33 group. The result suggested a potential role of MAPK pathways in the enhanced response to LPS after injection with IL-33.
DISCUSSION
ALI and ARDS are the pulmonary reflections of a serious systemic inflammatory characterized pathologically by diffuse alveolar damage, alveolar capillary leakage, oedema, hypoxemia, poor lung compliance, bilateral infiltrates, and so on [2, 3]. Optimal treatment involves suitable fluid management, protective lung ventilation, multiple organ support, and treatment of possible underlying cause [15, 16]. However, abundant epidemiological surveys suggest ALI/ARDS remain a significant health burden with high morbidity and mortality. A recent systematic review shows that the mortality for ARDS is between 36 and 44%, with little change over the two decades [15]. Thus, there is heightened interest in more accurate and complete characterization of high-risk populations and therapy of the patients with ALI/ARDS.
IL-33 has recently identified as the ligand for the orphan receptor ST2 [17]. ST2 is a member of the IL-1 receptor (IL-1R) family, which belongs to the Toll-like receptor (TLR)/IL-1R (TIR) superfamily [17, 18]. IL-33, with dual functions, can behave as inflammatory cytokines and transcription factors [4].
Therefore, we investigated the role of IL-33 with a common inflammation model ALI. In this study, it was demonstrated that IL-33 could not relieve ALI, instead aggravating LPS-induced ALI. IL-33 enhanced the effect in response to LPS, totally showing as decrease the survival rate.
Vascular endothelial barrier dysfunction, a hallmark of several disease states including ALI, was a mainly cause of the destruction of vascular integrity. Vascular endothelial barrier was comprised of tight junctions (TJs) and AJs at the interendothelial junction (IEJ). The AJs were formed via VE-cadherin-mediated interactions between neighboring endothelial cells (ECs) [19]. Enhanced phosphorylation of VE-cadherin, blocked AJ formation, resulted in defective AJs, thus increased EC permeability concomitant with TJ disorganization [19, 20]. Therefore, VE-cadherin, the major AJs component in ECs, was vital to preserve vascular barrier function [21, 22]. Pretreatment with IL-33 could enhance phosphorylation of VE-cadherin, thus destroying vascular integrity to aggravate ALI. The critical feature of ALI was the destruction of vascular integrity, and the subsequent upregulated permeability would result in alveolar capillary leakage and pulmonary edema [23]. Pretreatment with IL-33 increased evans blue content and W/D weight ratio, which were definite indicators of alveolar capillary leakage and pulmonary edema, respectively.
Taken together, these results suggested that IL-33 specifically targeted the AJs in endothelial cells (ECs) by increasing membrane phosphorylation of VE-cadherin. These findings demonstrated that IL-33, in part, destroyed vascular endothelial barrier through the resultant VE-cadherin phosphorylation.
TNF-α and IL-6 were important cytokines in recruitment of leukocytes into the lungs in LPS-induced ALI [24]. Pulmonary concentration of MPO was a marker of neutrophil infiltration into the lungs. Pretreatment with IL-33 increased the levels of proinflammatory cytokines (TNF-α and IL-6) and MPO concentration, which meant a more severe inflammation and leukocyte infiltration. TLR4 was the receptor of LPS and LPS/TLR4/MAPK was involved in a variety of inflammatory reactions [25–28]. Although the signaling pathways activated by IL-33 remain poorly understood, it was reported that IL-33-enhancing effect of LPS response targeted the MyD88-dependent pathway of TLR-4 and IL-33-mediated cytokines production by human mast cells was mediated by a signaling pathway involving MAPK. The activation of MAPK family molecules in turn promotes the production of many proinflammatory proteins and enhances immune reactivity [4, 7, 29]. The members of MAPK family, including JNKs, ERKs, and p38 MAPK, were activated by phosphorylation on threonine and tyrosine residues by upstream dual-specificity kinases [5, 30]. Our study demonstrated that the enhancement of LPS response with the IL-33 pretreatment was coupled with an increase of MAPK phosphorylation. Therefore, IL-33 might further increase the activation of MAPK pathways to enhance the release of inflammatory cytokines to aggravate ALI.
To sum up, we found that IL-33 could not relieve inflammation, instead aggravating LPS-induced ALI. IL-33 enhanced the effect in response to LPS, showing as decreased the survival rate, infiltrated of inflammatory cells, secreted more proinflammatory cytokines, diffused alveolar damage, and exacerbated vascular permeability, but had little effect on pulmonary fibrosis. The effect of IL-33 might act through activating MAPK pathways.
However, there are still some problems to be solved. IL-33 is selectively expressed on T helper type 2 (Th2) cells but not Th1 cells. IL-33 drives production of Th2-associated cytokines and thereby promotes defense and pathology in tissues and organs [31–33]. The influence of IL-33 on immune balance and immune deviation has not yet been identified. For example, in severe systemic reactions, such as experimental sepsis from cecal ligation and puncture (CLP), the bodies are in a state of immunosuppression and IL-33 plays a protective role [9], while in our study, the mice are in a state of immune hyperfunction in early period of inflammation and IL-33 aggravates damage. Accordingly, we guess it may be because of the distinct immune states for that IL-33 has different roles in inflammatory disease. Besides, in these two models, the importance of injured organs is different to life activities. In CLP model, cecal inflammation makes the activation of defense system and thus, plays a protective effect on the body, while in ALI model, lung inflammation also activates the defense system and thus, aggravates lung injury inducing the increase of death. Another possible reason is that we use different pretreatment times; CLP models were pretreated 1 and 24 h, while we pretreat 6 h. Besides, the role of ST2 in LPS tolerance diverges. Brint et al. have demonstrated that ST2 KO mice could not be desensitized to LPS whereas another report shows that IL-33 enhances LPS-induced inflammatory cytokine production by regulating LPS receptor complex in LPS tolerance model [4, 7]. The conclusion that IL-33/ST2 was involved in LPS tolerance has gotten with ST2 KO mice; it might in part affect the role of IL-33/ST2 pathways.
In summary, IL-33 has different functions in various inflammatory diseases and states. Until now, the mechanism of IL-33 on Th1/Th2 type cytokine balance and inflammatory disease is unknown, and many issues need to be resolved. Therefore, in follow-up experiments, we will further explore the effect of IL-33 on immune balance and Th1 to Th2 shift, in order to better understand the role of IL-33 in different inflammatory states, and will further investigate whether IL-33 is involved in LPS tolerance. Thus, the potential therapeutic efficacy of IL-33 against sepsis and other inflammatory disease is controversial, and its clinical application is ambiguous.
CONCLUSION
Our results indicate that IL-33 enhances LPS response accompanying with the further activation of MAPK family proteins in the process. IL-33 enhances LPS-induced ALI mainly in aggravation inflammatory reaction and increases microvascular permeability, but has little effect on pulmonary fibrosis. To sum up, IL-33 decreased survival rate and aggravated LPS-induced ALI. The therapeutic effect of IL-33 against sepsis and other inflammatory diseases is closely related to the overall situation of the body.
References
Wheeler, A.P., and G.R. Bernard. 2007. Acute lung injury and the acute respiratory distress syndrome: A clinical review. Lancet 369: 1553–1564.
Matthay, M.A., L.B. Ware, and G.A. Zimmerman. 2012. The acute respiratory distress syndrome. The Journal of Clinical Investigation 122: 2731–2740.
Parekh, D., R.C. Dancer, and D.R. Thickett. 2011. Acute lung injury. Clinical Medicine (Lond) 11: 615–618.
Espinassous, Q., E. Garcia-de-Paco, I. Garcia-Verdugo, M. Synguelakis, S. von Aulock, J.M. Sallenave, et al. 2009. IL-33 enhances lipopolysaccharide-induced inflammatory cytokine production from mouse macrophages by regulating lipopolysaccharide receptor complex. Journal of Immunology (Baltimore, Md. : 1950) 183: 1446–1455.
Tian, J., Y. Wang, Z. He, Y. Gao, J.E. Rundhaug, and X. Wang. 2011. Hydroxyethyl starch (130 kD) inhibits Toll-like receptor 4 signaling pathways in rat lungs challenged with lipopolysaccharide. Anesthesia and Analgesia 113: 112–119.
Biswas, S.K., P. Bist, M.K. Dhillon, T. Kajiji, C. Del Fresno, M. Yamamoto, et al. 2007. Role for MyD88-independent, TRIF pathway in lipid A/TLR4-induced endotoxin tolerance. Journal of Immunology (Baltimore, Md. : 1950) 179: 4083–4092.
Brint, E.K., D. Xu, H. Liu, A. Dunne, A.N. McKenzie, L.A. O’Neill, et al. 2004. ST2 is an inhibitor of interleukin 1 receptor and Toll-like receptor 4 signaling and maintains endotoxin tolerance. Nature Immunology 5: 373–379.
Schmitz, J., A. Owyang, E. Oldham, Y. Song, E. Murphy, T.K. McClanahan, et al. 2005. IL-33, an interleukin-1-like cytokine that signals via the IL-1 receptor-related protein ST2 and induces T helper type 2-associated cytokines. Immunity 23: 479–490.
Alves-Filho, J.C., F. Sonego, F.O. Souto, A. Freitas, W.A. Verri Jr., M. Auxiliadora-Martins, et al. 2010. Interleukin-33 attenuates sepsis by enhancing neutrophil influx to the site of infection. Nature Medicine 16: 708–712.
Roger, T., and T. Calandra. 2010. Interleukin-33 safeguards neutrophils in sepsis. Nature Medicine 16: 638–639.
Oboki, K., T. Ohno, N. Kajiwara, K. Arae, H. Morita, A. Ishii, et al. 2010. IL-33 is a crucial amplifier of innate rather than acquired immunity. Proceedings of the National Academy of Sciences of the United States of America 107: 18581–18586.
Lu, J., J. Kang, C. Zhang, and X. Zhang. 2015. The role of IL-33/ST2L signals in the immune cells. Immunology Letters 164: 11–17.
Nabe, T. 2014. Interleukin (IL)-33: New therapeutic target for atopic diseases. Journal of Pharmacological Sciences 126: 85–91.
Yagami, A., K. Orihara, H. Morita, K. Futamura, N. Hashimoto, K. Matsumoto, et al. 2010. IL-33 mediates inflammatory responses in human lung tissue cells. Journal of Immunology (Baltimore, Md. : 1950) 185: 5743–5750.
Dushianthan, A., M.P. Grocott, A.D. Postle, and R. Cusack. 2011. Acute respiratory distress syndrome and acute lung injury. Postgraduate Medical Journal 87: 612–622.
Piper, A., Y. Song, N.D. Eves, and T.M. Maher. 2014. Year in review 2013: Acute lung injury, interstitial lung diseases, sleep and physiology. Respirology (Carlton, Vic) 19: 428–437.
Liew, F.Y., N.I. Pitman, and I.B. McInnes. 2010. Disease-associated functions of IL-33: The new kid in the IL-1 family. Nature Reviews Immunology 10: 103–110.
Lingel, A., T.M. Weiss, M. Niebuhr, B. Pan, B.A. Appleton, C. Wiesmann, et al. 2009. Structure of IL-33 and its interaction with the ST2 and IL-1RAcP receptors—Insight into heterotrimeric IL-1 signaling complexes. Structure 17: 1398–1410.
Chichger, H., H. Duong, J. Braza, and E.O. Harrington. 2015. p18, a novel adaptor protein, regulates pulmonary endothelial barrier function via enhanced endocytic recycling of VE-cadherin. FASEB Journal 29: 868–881.
Fainaru, O., I. Adini, O. Benny, L. Bazinet, E. Pravda, R. D’Amato, et al. 2008. Doxycycline induces membrane expression of VE-cadherin on endothelial cells and prevents vascular hyperpermeability. FASEB Journal 22: 3728–3735.
Gong, H., J. Rehman, H. Tang, K. Wary, M. Mittal, P. Chaturvedi, et al. 2015. HIF2alpha signaling inhibits adherens junctional disruption in acute lung injury. The Journal of Clinical Investigation 125: 652–664.
Semina, E.V., K.A. Rubina, V.Y. Sysoeva, P.N. Rutkevich, N.M. Kashirina, and V.A. Tkachuk. 2014. Novel mechanism regulating endothelial permeability via T-cadherin-dependent VE-cadherin phosphorylation and clathrin-mediated endocytosis. Molecular and Cellular Biochemistry 387: 39–53.
Li, Y.C., C.H. Yeh, M.L. Yang, and Y.H. Kuan. 2012. Luteolin suppresses inflammatory mediator expression by blocking the Akt/NFkappaB pathway in acute lung injury induced by lipopolysaccharide in mice. Evidence-based Complementary and Alternative Medicine 2012: 383608.
Reutershan, J., M.A. Morris, T.L. Burcin, D.F. Smith, D. Chang, M.S. Saprito, et al. 2006. Critical role of endothelial CXCR2 in LPS-induced neutrophil migration into the lung. The Journal of Clinical Investigation 116: 695–702.
Liu, G., Y.J. Park, Y. Tsuruta, E. Lorne, and E. Abraham. 2009. p53 Attenuates lipopolysaccharide-induced NF-kappaB activation and acute lung injury. Journal of Immunology (Baltimore, Md. : 1950) 182: 5063–5071.
Antonov, A., C. Snead, B. Gorshkov, G.N. Antonova, A.D. Verin, and J.D. Catravas. 2008. Heat shock protein 90 inhibitors protect and restore pulmonary endothelial barrier function. American Journal of Respiratory Cell and Molecular Biology 39: 551–559.
Okutani, D. 2006. Src protein tyrosine kinase family and acute lung injury. Nihon Rinsho Men’eki Gakkai kaishi = Japanese journal of clinical immunology 29: 334–341.
Gong, P., D.J. Angelini, S. Yang, G. Xia, A.S. Cross, D. Mann, et al. 2008. TLR4 signaling is coupled to SRC family kinase activation, tyrosine phosphorylation of zonula adherens proteins, and opening of the paracellular pathway in human lung microvascular endothelia. The Journal of Biological Chemistry 283: 13437–13449.
Iikura, M., H. Suto, N. Kajiwara, K. Oboki, T. Ohno, Y. Okayama, et al. 2007. IL-33 can promote survival, adhesion and cytokine production in human mast cells. Laboratory Investigation 87: 971–978.
Sui, X., N. Kong, L. Ye, W. Han, J. Zhou, Q. Zhang, et al. 2014. p38 and JNK MAPK pathways control the balance of apoptosis and autophagy in response to chemotherapeutic agents. Cancer Letters 344: 174–179.
Komai-Koma, M., D. Xu, Y. Li, A.N. McKenzie, I.B. McInnes, and F.Y. Liew. 2007. IL-33 is a chemoattractant for human Th2 cells. European Journal of Immunology 37: 2779–2786.
Xu, D., W.L. Chan, B.P. Leung, F. Huang, R. Wheeler, D. Piedrafita, et al. 1998. Selective expression of a stable cell surface molecule on type 2 but not type 1 helper T cells. The Journal of Experimental Medicine 187: 787–794.
Smith, D.E. 2011. The biological paths of IL-1 family members IL-18 and IL-33. Journal of Leukocyte Biology 89: 383–392.
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (81171639) and Provincial Natural Science Foundation of Zhejiang (LQ16H150001).
Authors’ Contributions
Junran Xie and Ran Lv conceived and designed the experiments and supervised the project. Yaping Zhang performed experiments and interpreted the data. All the authors participated in manuscript writing and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare they have no conflict of interest.