Abstract
Interleukin 1β (IL-1β) is a pleiotropic pro-inflammatory cytokine that plays a critical role in the development of osteoarthritis (OA). Coptisine is an isoquinoline alkaloid extracted from Coptidis rhizome and has been reported to possess anti-inflammatory activity. However, the anti-inflammatory effects of coptisine on interleukin-1 beta (IL-1β)-stimulated chondrocytes have not been reported. Therefore, the aim of this study was to investigate the effects of coptisine on IL-1β-induced inflammation in human articular chondrocytes. Our results showed that coptisine greatly inhibited the production of nitric oxide (NO) and prostaglandin E2 (PGE2), as well as suppressed the expression of inducible NO synthase (iNOS) and cyclooxygenase-2 (COX-2) in human OA chondrocytes induced by IL-1β. It also inhibited the expression of matrix metalloproteinase-3 (MMP-3) and MMP-13 in IL-1β-stimulated human OA chondrocytes. Furthermore, coptisine significantly inhibited the IL-1β-induced NF-kB activation in human OA chondrocytes. Taken together, these data suggest that coptisine inhibits the IL-1β-induced inflammatory response by suppressing the NF-kB signaling pathway. Thus, coptisine may be a potential agent in the treatment of OA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Osteoarthritis (OA) is a common degenerative disease, and the prevalence of OA is increased dramatically over the age of 50. It is characterized by self-perpetuating low-grade inflammation and degradative processes within the articular cartilage of affected joints [1]. Currently, although nonsteroidal anti-inflammatory drugs (NSAIDs) have been used clinically for the past few years to treat OA, these agents are only temporarily effective and exhibit numerous side effects [2]. Thus, there is an urgent need for the development of novel, safe, and more effective therapeutic strategies for the treatment of OA.
Interleukin 1β (IL-1β) is a pleiotropic pro-inflammatory cytokine that plays a critical role in the development of OA. Previous reports have indicated that in response to IL-1β, chondrocytes secrete pro-inflammatory cytokines, chemokines, neutral metalloproteinases (MMPs), and nitric oxide (NO). These inflammatory mediators lead to the pathogenesis of OA [3–5]. Thus, the inhibition of these inflammatory mediators will be reasonable therapeutic targets for treating OA.
Coptisine is an isoquinoline alkaloid extracted from Coptidis rhizome. Increasing evidences have reported that coptisine has many biological activities such as antidiabetic, antimicrobial, anti-cancer, and anti-inflammatory properties [6–9]. Previous studies showed that coptisine treatment also attenuated the pro-inflammatory cytokines including interleukin (IL)-1β, IL-6, and tumor necrosis factor-α in heart tissue after myocardial ischemia/reperfusion injury [10]. Meanwhile, coptisine was found to inhibit obesity-related inflammation through LPS/TLR4-mediated signaling pathway in Syrian golden hamsters [11]. However, the anti-inflammatory effects of coptisine on IL-1β-stimulated chondrocytes have not been reported. Therefore, the aim of this study was to investigate the effects of coptisine on IL-1β-induced inflammation in human articular chondrocytes.
MATERIALS AND METHODS
Human Articular Chondrocytes Culture and Treatment
Human OA cartilage was obtained from six females (mean ± SD age 63.7 ± 5.3 years), who had undergone arthroplasty. Informed written permission was obtained from the patients according to the terms of the Ethics Committee of the Chinese Medicine Hospital of Xinjiang Uygur Autonomous Region (China). Primary cultures of human chondrocytes were isolated from articular cartilage as previously described [12]. Cartilage slices were digested with 0.2 % collagenase (Serva, Heidelberg, Germany) for 4 h at 37 °C in a shaker. Primary chondrocytes were cultured in DMEM supplemented with 10 % fetal bovine serum (FBS), 100 U/mL penicillin, and 100 μg/mL streptomycin (Sigma, St. Louis, MO, USA) at 37 °C in a 5 % CO2 incubator. When cells reached 80 % confluence, cells were passaged and chondrocytes of passage one were used for subsequent experiments.
Human chondrocytes at a density of 1 × 105 cells/well were pretreated with or without various concentrations (2.5, 5, and 10 μg/ml) of coptisine (Sigma, St. Louis, MO, USA) for 2 h and then co-incubated in the absence or presence of IL-1β (10 ng/ml) for 24 h.
Cell Viability
The 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay was used to detect cell viability. In brief, after treatment, the cells were incubated with MTT solution (5 mg/ml) at 37 °C for 4 h. Then, the culture medium was discarded, and 100 μL DMSO (Sigma, St. Louis, MO, USA) was then added to the plates, shaking for 10 min to solubilize MTT tetrazolium crystal. The spectrophotometric absorbance was measured at 570 nm using a microplate reader (Bio-Rad, Hercules, CA, USA).
NO and PGE2 Measurement
The nitrite levels in the culture medium were evaluated by Griess reaction as previously described [13]. The levels of prostaglandin E2 (PGE2) were investigated using a commercial ELISA kit according to the manufacturer’s protocol (Invitrogen, Carlsbad, CA, USA).
NO and PGE2 Measurement
The nitrite levels in the culture medium were determined by Griess reaction as previously described. The level of PGE2 was analyzed using a commercially available ELISA kit (Yanjin Biotechnology Co., Shanghai, China) according to the manufacturer’s instructions.
qRT-PCR
Total RNA was isolated from chondrocytes using TRIzol (Invitrogen Inc., Carlsbad, CA, USA). Approximately 5-μg total RNA for each sample was reverse transcribed into first-strand complementary DNA (cDNA) for quantitative real-time PCR (qRT-PCR) analysis. RT-PCR was conducted using an ABI Prism 7500 sequence detection system (Applied Biosystems, Foster City, CA, USA) using a SYBR Green Real-Time PCR Master Mix kit (Takara Biotechnology, Dalian, China). The PCR primers for inducible nitric oxide synthase (iNOS) were 5′-TTTCCAAGACACACTTCACCA-3′ (forward) and 5′-ATCTCCTTTGTTACCGCTTCC-3′ (reverse); for cyclooxygenase-2 (COX-2) were 5′-GAGAGATGTATCCTCCCACAGTCA-3′ (forward) and 5′-GACCAGGCACCAGACCAAAG-3′ (reverse); for MMP-3 were 5′-GCATTGGCTGAGTGAAAGAGAC TGTATC-3′ (forward) and 5′-ATGATGAACGATGGACAGATGA-3′; (reverse); for MMP-13 were 5′-AGTAGTTCCAAAGGCTACAACTTGTTT-3′ (forward) and 5′-GGAGTGGTCAAGCCCTAAGGA-3′ (reverse); and for GADPH were 5′-ATGACAACTCCCTCAAGAT-3′ (forward) and 5′-GATCCACAACGGATACATT-3′ (reverse). GADPH was used as a quantitative and qualitative control to normalize gene expression. Data were analyzed using the formula: R = 2−(ΔCt sample − ΔCt control).
Western Blot
Proteins were extracted from chondrocytes with the RIPA lysis buffer (Beyotime Biotechnology, Shanghai, China) and protein concentrations were measured by BCA Protein Assay kit. Equal amounts of protein (30 μg) were separated by SDS-PAGE and transferred onto a nitrocellulose membrane (Amersham, Little Chalfont, UK). After blocking with 2 % nonfat milk in Tris-buffered saline (TBS) with 0.1 % Tween-20 (TBST) at room temperature for 1 h, the membranes were incubated with primary antibodies (anti-iNOS, anti-COX2, anti-MMP-3, anti-MMP-13, anti-phospho-NF-kB p65, anti-IkB and anti-GAPDH) (dilution 1/1000, Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA) overnight at 4 °C. Subsequently, the membranes were incubated with IgG-horseradish peroxidase (HRP)-labeled secondary antibodies (Santa Cruz Biotechnology, Inc., Santa Cruz, CA, USA) at room temperature for 1 h. Blots were visualized using Amersham western blot detection reagent (GE Healthcare, Piscataway, New Jersey, USA).
Statistical Analysis
The data were expressed as mean ± SD of the representative experiment performed in triplicate. One-way ANOVA analysis or Student’s t test was used for the statistical comparison of multiple groups. Results were considered statistically significant at a P value less than 0.05.
RESULTS
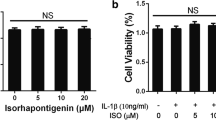
Effect of Coptisine on Human OA Chondrocyte Viability
The cytotoxicity of coptisine on chondrocytes was determined using the MTT assay. The results showed that coptisine at the concentration range of 1–10 μM did not have cytotoxic effects on human OA chondrocytes (Fig. 1a). Moreover, we observed that IL-1β treatment significantly reduced cell viability; however, pretreatment with coptisine reversed this effect, exhibiting a dose-dependent manner (Fig. 1b).
Effect of coptisine on human OA chondrocyte viability. a Human chondrocytes at a density of 1 × 105 cells/well in 96-well plates were pretreated with various concentrations of coptisine (2.5, 5, and 10 μg/ml) for 24 h, and the MTT assay was performed to detect cell viability. b Human OA chondrocytes at a density of 1 × 105 cells/well were pretreated for 2 h with various concentrations of coptisine (2.5, 5, and 10 μg/ml) and then stimulated or not stimulated with IL-1β (10 ng/ml) for 24 h. Then, cell viability was determined using the MTT assay. The values presented are the means ± SD of three independent experiments. *P < 0.05 vs control group; #P < 0.05 vs IL-1β group.
Coptisine Inhibits IL-1β-Induced NO and PGE2 Production in OA Chondrocytes
The effects of coptisine on IL-1β-induced NO and PGE2 production were measured. As shown in Fig. 2, the production of NO and PGE2 was increased greatly in chondrocytes treated with IL-1β. However, treatment of coptisine inhibited IL-1β-induced NO and PGE2 production in a dose-dependent manner.
Coptisine inhibits IL-1β-induced NO and PGE2 production in OA chondrocytes. Human OA chondrocytes at a density of 1 × 105 cells/well were pretreated for 2 h with various concentrations of coptisine (2.5, 5, and 10 μg/ml) and then stimulated or not stimulated with IL-1β (10 ng/ml) for 24 h. a The nitrite levels in the culture medium were assessed by Griess reaction. b The levels of PGE2 were determined using a ELISA kit. The values presented are the means ± SD of three independent experiments. *P < 0.05 vs control group; #P < 0.05 vs IL-1β group.
Coptisine Inhibits IL-1β-Induced iNOS and COX-2 Expression in OA Chondrocytes
Next, we examined the effects of coptisine on IL-1β-induced iNOS and COX-2 expression in human chondrocytes. As shown in Fig. 3a, b, stimulation of human OA primary chondrocytes with 24-h IL-1β treatment showed a significant downregulation of iNOS and COX-2 messenger RNA (mRNA) expression. Treatment of chondrocytes with coptisine significantly reduced both iNOS and COX-2 protein compared to IL-1β treatment alone. In addition, we observed that coptisine remarkably inhibited the protein expression of iNOS and COX-2 in a dose-dependent manner in contrast with chondrocytes stimulated with IL-1β alone (Fig. 3c).
Coptisine inhibits IL-1β-induced iNOS and COX-2 expression in OA chondrocytes. Human OA chondrocytes at a density of 1 × 105 cells/well were pretreated for 2 h with various concentrations of coptisine (2.5, 5, and 10 μg/ml) and then stimulated or not stimulated with IL-1β (10 ng/ml) for 24 h. The mRNA expression levels of iNOS (a) and COX-2 (b) were determined by qRT-PCR. c The protein expression levels of iNOS and COX-2 were assessed by Western blot. The values presented are the means ± SD of three independent experiments. *P < 0.05 vs control group; #P < 0.05 vs IL-1β group.
Coptisine Inhibits IL-1β-Induced MMP-3 and MMP-13 Expression in OA Chondrocytes
MMPs play critical roles in degrading cartilage. Thus, we investigated the effects of coptisine on MMP-3 and MMP-13 expression in IL-1β-induced chondrocytes using qRT-PCR and Western blot. The results of qRT-PCR analysis demonstrated that IL-1β significantly induced the mRNA expression of MMP-3 and MMP-13 compared to untreated chondrocytes. Treatment with coptisine for 24 h in human chondrocytes caused a significant reduction in gene expression in a dose-dependent manner compared with chondrocytes stimulated with IL-1β (Fig. 4a, b). Similarly, Western blot analysis also showed that coptisine suppressed IL-1β-induced protein expression of MMP-3 and MMP-13 in human chondrocytes (Fig. 4c).
Coptisine inhibits IL-1β-induced MMP-3 and MMP-13 expression in OA chondrocytes. Human OA chondrocytes at a density of 1 × 105 cells/well were pretreated for 2 h with various concentrations of coptisine (2.5, 5, and 10 μg/ml) and then stimulated or not stimulated with IL-1β (10 ng/ml) for 24 h. The mRNA expression levels of MMP-3 (a) and MMP-13 (b) were assayed by qRT-PCR. c The protein expression levels of MMP-3 and MMP-13 were determined by Western blot. The values presented are the means ± SD of three independent experiments. *P < 0.05 vs control group; #P < 0.05 vs IL-1β group.
Coptisine Inhibits IL-1β-Induced NF-kB Activation in OA Chondrocytes
To investigate the anti-inflammatory mechanism of coptisine, the effects of coptisine on IL-1β-induced NF-kB activation were detected by Western blot. As shown in Fig. 5, IL-1β stimulation significantly induced NF-kB activation and IkBα degradation in chondrocytes. However, treatment of coptisine inhibited IL-1β-induced NF-kB activation in chondrocytes.
Coptisine inhibits IL-1β-induced NF-kB activation in OA chondrocytes. Human OA chondrocytes at a density of 1 × 105 cells/well were pretreated for 2 h with 10 μg/ml coptisine and then stimulated or not stimulated with IL-1β (10 ng/ml) for 1 h. a The protein levels of p-NF-kB p65 and IkB-α were assessed by western blot analysis. b, c The densitometry data was also assessed. The values presented are the means ± SD of three independent experiments. *P < 0.05 vs control group; #P < 0.05 vs IL-1β group.
DISCUSSION
Pro-inflammatory cytokines such as IL-1β produced by activated chondrocytes are believed to play important roles in the initiation and development of OA [14]. In this study, we investigated the effects of coptisine on IL-1β-induced inflammation in chondrocytes. The results demonstrated that the effects of coptisine (0-10 μg/ml) on chondrocytes were not attributable to cytotoxic effects. Coptisine exhibited an ability to inhibit the IL-1β-dependent upregulation of the production of NO and PGE2, and the expression of iNOS, COX-2, MMP-3, and MMP-13 in chondrocytes. Treatment of coptisine suppressed IL-1β-induced NF-kB activation in chondrocytes.
A growing body of evidence indicates that inflammatory insults can lead to iNOS overexpression in chondrocytes [12, 15, 16]. It was reported that OA chondrocytes overexpress iNOS and its product NO [17]. Moreover, COX-2 is an important mediator of pain and inflammation in osteoarthritic joints, mainly stimulated by IL-1β. After induction, COX-2 participates in the sequential enzymatic reactions that lead to the synthesis of PGE2, which plays a critical role in the pathophysiology of OA [18, 19]. In line with the previous studies, in the present study, we observed that IL-1β treatment significantly increased the production of NO and PGE2, as well as induced the expression of iNOS and COX-2 in chondrocytes. However, coptisine inhibited the IL-1β-dependent upregulation of the production of NO and PGE2, and the expression of iNOS and COX-2 in chondrocytes. These data suggest that coptisine may exert anti-inflammatory effects on cartilage protection by inhibiting the expression of inflammatory mediators induced by IL-1β in the pathogenesis of OA.
MMPs are important regulators in the progression of OA. Among the MMPs, MMP-3 and MMP-13 are important for degrading collagens, proteoglycans, and other extracellular matrix macromolecules in cartilage [20]. There is substantial evidence that inhibition of MMP production could inhibit the progression of OA [21–23]. In addition, IL-1β stimulates chondrocytes to release proteolytic enzymes and MMPs, which are key regulators of cartilage destruction [24]. Herein, we found that coptisine inhibited the IL-1β-dependent upregulation of the expression of MMP-3 and MMP-13 in chondrocytes. These results suggest that coptisine controlled cartilage loss by downregulating MMP-3 and MMP-13 in IL-1β-treated chondrocytes.
Emerging studies have indicated that NF-kB signaling pathway was essential for the chondrocytes to express inflammation-related genes, including MMP-1, 3, and 13, iNOS, IL-1, IL-6, TNF-α, COX-2, and a disintegrin and metalloproteinase (ADAM) with thrombospondin-1 domains (ADAMTS) -4 and -5, which play important roles in the pathophysiology of OA [4, 25–27]. Both subunits (p50 and p65) of NF-kB are abundant in OA and in synovitis. IL-1β can induce NF-kB activation in chondrocytes. Indeed, it is well known that IkBα-phosphorylation by IL-1β leads to ubiquitination and degradation of IkBα. In response to IL-1β, NF-kB p65 dissociates from IkB and translocates into the nucleus to regulate the expression of inflammatory mediators, including NO and PGE2. Furthermore, the NF-kB inhibitor reduces IL-1β-induced MMP-3 and MMP-13 production in human chondrocytes [28]; NF-kB p65-specific siRNA also inhibited the expression of NF-kB p65 and activation of NF-kB, reducing the expression of COX-2, NOS-2, and MMP-9 induced by IL-1β in cultured chondrocytes [29]. Recent evidence has shown that coptisine inhibited NF-kB p65 phosphorylation, which is regulated in response to receptor activator of NF-kB ligand (RANKL) in bone marrow macrophages (BMMs) [30]. In this study, we found that coptisine dose-dependently inhibited IL-1β-induced NF-kB activation in chondrocytes. These data suggested that coptisine inhibited IL-1β-induced inflammatory mediators expression by inhibiting NF-kB activation.
In conclusion, our results showed that coptisine inhibits IL-1β-induced expression of inflammatory mediators through suppressing NF-kB activation in chondrocytes. Thus, coptisine may serve as a potential anti-inflammatory agent in the treatment of OA.
References
Pelletier, J.P., J. Martel‐Pelletier, and S.B. Abramson. 2001. Osteoarthritis, an inflammatory disease: potential implication for the selection of new therapeutic targets. Arthritis and Rheumatism 44: 1237–1247.
Ding, C. 2002. Do NSAIDs affect the progression of osteoarthritis? Inflammation 26: 139–142.
Li, X., M. Ellman, P. Muddasani, J.H.C. Wang, G. Cs‐Szabo, A.J. van Wijnen, et al. 2009. Prostaglandin E2 and its cognate EP receptors control human adult articular cartilage homeostasis and are linked to the pathophysiology of osteoarthritis. Arthritis and Rheumatism 60: 513–523.
Goldring, M.B., and M. Otero. 2011. Inflammation in osteoarthritis. Current Opinion in Rheumatology 23: 471–478.
Goldring, M.B., M. Otero, D.A. Plumb, C. Dragomir, M. Favero, K. El Hachem, et al. 2011. Roles of inflammatory and anabolic cytokines in cartilage metabolism: signals and multiple effectors converge upon MMP-13 regulation in osteoarthritis. European Cells & Materials 21: 202–220.
Yuan, L., D. Tu, X. Ye, and J. Wu. 2006. Hypoglycemic and hypocholesterolemic effects of Coptis chinensis franch inflorescence. Plant Foods for Human Nutrition 61: 139–144.
Zhen, Z., B. Chang, M. Li, F.-M. Lian, L. Chen, L. Dong, et al. 2011. Anti-diabetic effects of a Coptis chinensis containing new traditional Chinese medicine formula in type 2 diabetic rats. The American Journal of Chinese Medicine 39: 53–63.
Yan, D., C. Jin, X.-H. Xiao, and X.-P. Dong. 2008. Antimicrobial properties of berberines alkaloids in Coptis chinensis Franch by microcalorimetry. Journal of Biochemical and Biophysical Methods 70: 845–849.
Li, J., D.-M. Qiu, S.-H. Chen, S.-P. Cao, and X.-L. Xia. 2013. Suppression of human breast cancer cell metastasis by coptisine in vitro. Asian Pacific Journal of Cancer Prevention 15: 5747–5751.
Guo, J., S.-B. Wang, T.-Y. Yuan, Y.-J. Wu, Y. Yan, L. Li, et al. 2013. Coptisine protects rat heart against myocardial ischemia/reperfusion injury by suppressing myocardial apoptosis and inflammation. Atherosclerosis 231: 384–391.
Zou, Z.-Y., Y.-R. Hu, H. Ma, Y.-Z. Wang, K. He, S. Xia, et al. 2015. Coptisine attenuates obesity-related inflammation through LPS/TLR-4-mediated signaling pathway in Syrian golden hamsters. Fitoterapia 105: 139–146.
Cheng, A.W.M., T.V. Stabler, M. Bolognesi, and V.B. Kraus. 2011. Selenomethionine inhibits IL-1β inducible nitric oxide synthase (iNOS) and cyclooxygenase 2 (COX2) expression in primary human chondrocytes. Osteoarthritis and Cartilage 19: 118–125.
Au, R., T. Al-Talib, A. Au, P. Phan, and C. Frondoza. 2007. Avocado soybean unsaponifiables (ASU) suppress TNF-α, IL-1β, COX-2, iNOS gene expression, and prostaglandin E 2 and nitric oxide production in articular chondrocytes and monocyte/macrophages. Osteoarthritis and Cartilage 15: 1249–1255.
Moos, V., M. Rudwaleit, V. Herzog, K. Höhlig, J. Sieper, and B. Müller. 2000. Association of genotypes affecting the expression of interleukin‐1β or interleukin‐1 receptor antagonist with osteoarthritis. Arthritis and Rheumatism 43: 2417–2422.
Ahmed, S., A. Rahman, A. Hasnain, M. Lalonde, V.M. Goldberg, and T.M. Haqqi. 2002. Green tea polyphenol epigallocatechin-3-gallate inhibits the IL-1β-induced activity and expression of cyclooxygenase-2 and nitric oxide synthase-2 in human chondrocytes. Free Radical Biology and Medicine 33: 1097–1105.
Abramson, S.B. 2008. Nitric oxide in inflammation and pain associated with osteoarthritis. Arthritis Research & Therapy 10: 1–7.
Amin, A.R., P. Di Cesare, P. Vyas, M. Attur, E. Tzeng, T.R. Billiar, et al. 1995. The expression and regulation of nitric oxide synthase in human osteoarthritis-affected chondrocytes: evidence for up-regulated neuronal nitric oxide synthase. The Journal of Experimental Medicine 182: 2097–2102.
Kojima, F., H. Naraba, S. Miyamoto, M. Beppu, H. Aoki, and S. Kawai. 2004. Membrane-associated prostaglandin E synthase-1 is upregulated by proinflammatory cytokines in chondrocytes from patients with osteoarthritis. Arthritis Research & Therapy 6: R355–R365.
Hardy, M.M., K. Seibert, P.T. Manning, M.G. Currie, B.M. Woerner, D. Edwards, et al. 2002. Cyclooxygenase 2‐dependent prostaglandin E2 modulates cartilage proteoglycan degradation in human osteoarthritis explants. Arthritis and Rheumatism 46: 1789–1803.
Brinckerhoff, C.E., and L.M. Matrisian. 2002. Matrix metalloproteinases: a tail of a frog that became a prince. Nature Reviews Molecular Cell Biology 3: 207–214.
Wang, X., P.A. Manner, A. Horner, L. Shum, R.S. Tuan, and G.H. Nuckolls. 2004. Regulation of MMP-13 expression by RUNX2 and FGF2 in osteoarthritic cartilage. Osteoarthritis and Cartilage 12: 963–973.
Yoshihara, Y., H. Nakamura, Ki Obata, H. Yamada, T. Hayakawa, K. Fujikawa, et al. 2000. Matrix metalloproteinases and tissue inhibitors of metalloproteinases in synovial fluids from patients with rheumatoid arthritis or osteoarthritis. Annals of the Rheumatic Diseases 59: 455–461.
Piecha, D., J. Weik, H. Kheil, G. Becher, A. Timmermann, A. Jaworski, et al. 2010. Novel selective MMP-13 inhibitors reduce collagen degradation in bovine articular and human osteoarthritis cartilage explants. Inflammation Research 59: 379–389.
Klatt, A.R., B. Paul‐Klausch, G. Klinger, G. Kühn, J.H. Renno, M. Banerjee, et al. 2009. A critical role for collagen II in cartilage matrix degradation: collagen II induces pro‐inflammatory cytokines and MMPs in primary human chondrocytes. Journal of Orthopaedic Research 27: 65–70.
Pulai, J.I., H. Chen, H.-J. Im, S. Kumar, C. Hanning, P.S. Hegde, et al. 2005. NF-kB mediates the stimulation of cytokine and chemokine expression by human articular chondrocytes in response to fibronectin fragments. The Journal of Immunology 174: 5781–5788.
Roman-Blas, J., and S. Jimenez. 2006. NF-kB as a potential therapeutic target in osteoarthritis and rheumatoid arthritis. Osteoarthritis and Cartilage 14: 839–848.
Marcu, K.B., M. Otero, E. Olivotto, R.M. Borzí, and M.B. Goldring. 2010. NF-kB signaling: multiple angles to target OA. Current Drug Targets 11: 599–613.
Liacini, A., J. Sylvester, W.Q. Li, and M. Zafarullah. 2002. Inhibition of interleukin-1-stimulated MAP kinases, activating protein-1 (AP-1) and nuclear factor kappa B (NF-kB) transcription factors down-regulates matrix metalloproteinase gene expression in articular chondrocytes. Matrix Biology 21: 251–262.
Lianxu, C., J. Hongti, and Y. Changlong. 2006. NF-kBp65-specific siRNA inhibits expression of genes of COX-2, NOS-2 and MMP-9 in rat IL-1β-induced and TNF-α-induced chondrocytes. Osteoarthritis and Cartilage 14: 367–376.
Lee, J.-W., A. Iwahashi, S.-i. Hasegawa, T. Yonezawa, W.B. Jeon, B.-Y. Cha, et al. 2012. Coptisine inhibits RANKL-induced NF-kB phosphorylation in osteoclast precursors and suppresses function through the regulation of RANKL and OPG gene expression in osteoblastic cells. Journal of Natural Medicines 66: 8–16.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors have no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Zhou, K., Hu, L., Liao, W. et al. Coptisine Prevented IL-β-Induced Expression of Inflammatory Mediators in Chondrocytes. Inflammation 39, 1558–1565 (2016). https://doi.org/10.1007/s10753-016-0391-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-016-0391-6