Abstract
The present study aimed to investigate the potential anti-inflammatory and anti-nociceptive activities of glycyrrhizin (GL) in mice and to explore the possible related mechanisms. Xylene-induced ear edema, carrageenan-induced paw edema and acetic acid-induced vascular permeability test were used to investigate the anti-inflammatory activities of GL in mice. Anti-nociceptive effects of GL were assessed by using acetic acid-induced writhing, hot plate test and formalin test, as well as evaluation of spontaneous locomotor activity and motor performance. The mRNA expression of pro-inflammatory cytokines (such as TNF-α, IL-6 and iNOS) and the protein expression of cyclooxygenase-2 (COX-2) were explored by using real-time fluorogenic PCR and Western blot, respectively. The results showed that GL significantly reduced xylene-induced ear edema, carrageenan-induced paw edema, and acetic acid-induced vascular permeation. Additionally, GL significantly inhibited the nociceptions induced by acetic acid and formalin. However, the nociceptions could not be decreased by GL in the hot plate test, and GL did not affect spontaneous locomotor activity and motor performance. The expression levels of TNF-α, IL-6, iNOS and COX-2 were significantly downregulated by GL. In conclusion, GL exerts significant anti-inflammatory and analgesic activities by attenuating the expression levels of TNF-α, IL-6, iNOS and COX-2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Pain, which affects more than 20 % of the population worldwide, is a major public health problem that diminishes quality of life, limits activity, and reduces functional capacity. Pain is generally associated with inflammation caused by tissue trauma, chemical stimuli, and infectious agents. Inflammatory pain is primarily due to the sensitization of specific classes of nociceptive neurons by the direct action of inflammatory mediators [1]. Extensive studies have demonstrated that various pro-inflammatory mediators, including tumor necrosis factor alpha (TNF-α), interleukin-6 (IL-6), and nitric oxide (NO), play an important role in inflammatory pain [2–4]. Additionally, cyclooxygenase-2 (COX-2) contributes to the production of prostaglandin E2 (PGE2) [5], which is a major mediator of inflammatory pain.
While many analgesics and anti-inflammatory drugs are currently available, there is some concern regarding their side effects and low efficacy, making their clinical use problematic. Therefore, the study of novel drugs with greater efficacy and fewer side effects remains a goal of researchers from universities and the pharmaceutical industry.
Licorice, the root of Glycyrrhiza glabra, is one of the oldest and most commonly used herbs in Chinese traditional medicine. Glycyrrhizin (GL), a major active constituent isolated from licorice, possesses a variety of pharmacological activities, including anti-virus activity [6], anti-hepatitis activity [7], and anti-inflammatory activity [8]. Of note, GL is commonly used to treat patients with chronic hepatitis [9]. However, no report has been published to explore its effect on inflammatory pain.
Therefore, in the present study, we investigate the anti-inflammatory and anti-nociceptive effects of GL and explore the possible related mechanisms in experimental models.
MATERIALS AND METHODS
Drugs and Chemicals
Glycyrrhizin (purity > 93.0 %) was purchased from Tokyo Chemical Industry Co. Ltd, Tokyo, Japan. Morphine was provided by General Hospital of Ningxia Medical University. Indometacin, carrageenan, and Evans blue were purchased from Sigma-Aldrich, Steinheim. All compounds were dissolved in normal saline. All other chemicals were of analytical grade and obtained from standard commercial suppliers. NS, indometacin (10 mg/kg), and GL (40, 80, 160 mg/kg) were injected intraperitoneally (i.p.) in an application volume of 0.1 ml/10 g body weight. Morphine (10 mg/kg) was injected subcutaneously (s.c.) in an application volume of 0.1 ml/10 g body weight.
Animals
ICR mice weighing 18–22 g were provided by the Experimental Animal Center of Ningxia Medical University (certificate number was SYXK Ningxia 2005-0001). The mice were housed at 22–24 °C under 12-h light /12-h dark cycles and provided food and water ad libitum. Each animal was used only once in the experiment. The experimental protocol was duly approved by the institutional animal ethics committee of Ningxia Medical University.
Evaluation of Anti-inflammatory Activity
Xylene-Induced Ear Edema Test
Male mice were divided into five groups of 10 animals each: vehicle, vehicle + indometacin (10 mg/kg, i.p.), vehicle + GL (40 mg/kg, i.p.), vehicle + GL (80 mg/kg, i.p.), and vehicle + GL (160 mg/kg, i.p.). Xylene-induced ear edema in mice was initiated according to a method previously described by He et al. [10]. Briefly, each group was pre-treated with the drugs. After 1 h, 20 μl of xylene was administered to the inner surface of the right ear. After 1 h of xylene application, all mice were sacrificed by cervical dislocation and both ears were removed and weighed. The inhibition was calculated as follows: %inhibition = (A − B) × 100/A, where A is the difference in ear weight (control) and B is the difference in ear weight (test).
Acetic Acid-Induced Peritoneal Vascular Permeability Test
Male mice were divided into five groups of 10 animals each as for the xylene-induced ear edema test. The peritoneal vascular permeability test was adapted from the procedure described by Li et al. [11]. Mice were treated with the drugs. One hour later, each animal was given an intraperitoneal injection of 0.7 % acetic acid (10 ml/kg) following an intravenous injection of 0.5 % Evans blue solution (10 ml/kg). After 20 min, all mice were sacrificed by decapitation, and then, the pigment that had leaked into the abdominal cavity of each mouse was rinsed three times with a total of 5 ml normal saline solution. The recovered wash solution was centrifuged at 3000 r/min for 10 min, and the absorbance of the supernatant was measured at a wavelength of 590 nm.
Carrageenan-Induced Paw Edema Test
Male mice were divided into six groups of 10 animals each: control, vehicle, vehicle + indometacin (10 mg/kg, i.p.), vehicle + GL (40 mg/kg, i.p.), vehicle + GL (80 mg/kg, i.p.), and vehicle + GL (160 mg/kg, i.p.). The carrageenan-induced paw edema test employed here was a slight modification of a previously described method [12]. Six groups of mice were treated with the drugs by intraperitoneal administration, respectively. After 1 h, 30 μl NS was injected into the plantar side of the right hind paw of each mouse of the control group and other five groups were treated with 1 % carrageenan (30 μl) in the same region. The paw volume was measured at 1-h interval for 5 h after injection of carrageenan. In addition, the paw volume was measured before administration of any drug as the basal volume of the right hind paw. The paw edema degree is presented as the paw volume changes in relation to the basal values.
Evaluation of Anti-nociceptive Activity
Acetic Acid-Induced Writhing Test
Male mice were divided into five groups of 10 animals each as for the xylene-induced ear edema test. The method of Wang et al. [13] was used for this test. The animals were pre-treated with the drugs 1 h before intraperitoneal administration of acetic acid (0.6 %, 10 ml/kg). The number of constrictions, including abdominal muscle contractions and hind paw extension, was recorded over a period of 20 min, starting 5 min after the acetic acid injection.
Hot Plate Test
Female mice were divided into five groups of 10 animals each: vehicle, vehicle + morphine (10 mg/kg, s.c.), vehicle + GL (40 mg/kg, i.p.), vehicle + GL (80 mg/kg, i.p.), and vehicle + GL (160 mg/kg, i.p.). Mice were treated according to the methods described by Li et al. [14] and Ribeiro et al. [15]. Briefly, mice were placed twice in the YLS-6A hot plate apparatus maintained at a temperature of 55 ± 1 °C, separated by a 20-min interval. Only mice that showed initial nociceptive responses within 5–30 s were selected for the experiment. The latency, defined as the reaction time of each mouse (licking of the hind paws or jumping response) was recorded. Mice were treated with NS (10 ml/kg, i.p.) and GL (40, 80, 160 mg/kg, i.p.) 1 h before the test. Morphine (10 mg/kg, s.c.) was used as a positive control drug, which was administered 30 min before the experiment. The cutoff time was 60 s in order to avoid paw lesions.
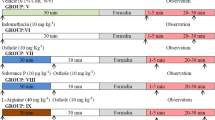
Formalin Test
Male mice were divided into six groups of 10 animals each: vehicle, vehicle + morphine (10 mg/kg, s.c.), vehicle + indometacin (10 mg/kg, i.p.), vehicle + GL (40 mg/kg, i.p.), vehicle + GL (80 mg/kg, i.p.), vehicle + GL (160 mg/kg, i.p.). The test was performed as described by Carballo-Villalobos et al. [16] and Khatun et al. [17]. Sixty minutes after administration for the intraperitoneal route, or 30 min for the subcutaneous route, 2 % formalin (20 μl) was injected subplantar into the right hind paw of each mouse. The accumulated time spent in licking the injected paw was taken as nociceptive response. Furthermore, the nociceptive response was recorded from 0 to 5 min (early phase, neurogenic pain) and 15–30 min (late phase, inflammatory pain) after formalin injection. Morphine and indometacin were used as reference controls.
Spontaneous Locomotor Activity Test
In the locomotor activity test [18, 19], male mice were divided into four groups of 10 animals each: vehicle, vehicle + GL (40 mg/kg, i.p.), vehicle + GL (80 mg/kg, i.p.), and vehicle + GL (160 mg/kg, i.p.). Each group was treated with the drugs 1 h before the test. Each animal was observed for 5 min after a period of 2 min for acclimatization in the YLS-1A spontaneous locomotor activity apparatus. Spontaneous numbers were counted in the experiment.
Motor Activity Test
Male mice were divided into four groups of 10 animals each as for the spontaneous locomotor activity test. The effect of GL on motor coordination performance was tested on the YLS-4C accelerating rota-rod apparatus as described previously [20, 21]. The animals were acclimatized to the revolving drum by training them on different occasions for 3 days before the experiment. Only the animals that could stay on the rotating rod for more than 3 min were selected for the test. On the experimental day, the mice were treated with the drugs, and 1 h later, they were tested. The time required for the mice to stay on the rota-rod was recorded, with a maximum cutoff of 5 min.
Real-Time Fluorogenic PCR Assays
After the carrageenan-induced paw edema test, paw skin tissues were removed, and total RNA was extracted. Total RNA was reverse-transcribed into cDNA by TransScript One-Step gDNA Removal and cDNA Synthesis SuperMix (TransGen Biotech, China) and analyzed by quantitative real-time PCR (Bio-Rad, USA) with TransStart TipTop Green qPCR SuperMix (TransGen Biotech, China). Primers used for the real-time PCR analysis were the following: TNF-α (forward): 5′-CCACCATCAAGGACTCAAATG-3′, (reverse): 5′-GAGACAGAGG CAACCTGACC-3′; IL-6 (forward): 5′-GGACCAAGACCATCCAATTC -3′, (reverse): 5′-ACCACAGTGAGGAATGTCCA-3′; iNOS (forward): 5′-AGCCAAGCCCTCACCTACTT-3′, (reverse): 5′-CTCTGCCTATCCG TCTCGTC-3′; β-actin (forward): 5′-GAGACCTTCAACACCCCAGC-3′, (reverse): 5′-ATGTCACGCACGATTTCCC -3′.
Western Blot Analysis
Western blot analysis was done as previously described [22]. Briefly, after the carrageenan-induced paw edema test, the mice (n = 6, for each group) were decapitated and paw skin tissues were quickly collected. Total proteins were extracted by using protein extraction kits following the manufacturer’s instructions. Protein concentrations were determined using the BCA protein assay kit (Thermo, USA). Protein samples (50 μg) were separated by 10 % sodium dodecyl sulfate-polyacrylamide gel electrophoresis and then transferred onto a nitrocellulose membrane. The membranes were incubated overnight at 4 °C with the primary antibodies (COX-2, 1:1000, Cell Signal, USA; β-actin, 1:1000, Proteintech Group, USA) and washed with 5 % skimmed milk in TBST. Afterwards, the membranes were treated with the secondary antibodies, namely, goat anti-rabbit (1:3000, Proteintech Group, USA) for 2 h at room temperature. Immunoreactive proteins were detected with an enhanced chemiluminescence (ECL), and the signals were quantified by densitometry with Quantity One 1-D Analysis Software (Bio-Rad, USA).
Statistical Analysis
All values were expressed throughout as mean ± S.E.M. Statistical analysis was performed using a one-way analysis of variance (ANOVA) followed by Tukey’s multiple comparison tests. The analyses were carried out using GraphPad Prism version 5.0 software. Values of p < 0.05 were considered to be statistically significant.
RESULTS
Evaluation of Anti-inflammatory Activity
Xylene-Induced Ear Edema Test
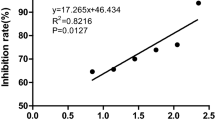
As shown in Fig. 1, GL at 40, 80, and 160 mg/kg significantly decreased xylene-induced ear edema with inhibitory rates of 23.25 % (p < 0.05), 36.07 % (p < 0.01), and 55.67 % (p < 0.01), respectively. Indometacin (10 mg/kg), the reference drug, also manifested a significantly diminished edema with an inhibition rate of 54.91 % (p < 0.01).
Anti-inflammatory effects of GL on xylene-induced ear edema in mice. Mice received NS (10 ml/kg, i.p.), indometacin (10 mg/kg, i.p.), or GL (40, 80, 160 mg/kg, i.p.) 1 h prior to xylene. The vehicle-treated animals are xylene-induced inflammatory mice. Data are expressed as the mean ± S.E.M. of 10 animals for each group. *p < 0.05 and **p < 0.01 compared with the vehicle group.
Acetic Acid-Induced Peritoneal Vascular Permeability Test
Effects of GL on peritoneal vascular permeability induced by acetic acid have been shown in Fig. 2. The administration of GL (80, 160 mg/kg) caused a significant reduction in the dye leakage compared with the vehicle group (p < 0.01), while there was no significant variation after giving GL (40 mg/kg) (p > 0.05). Indometacin (10 mg/kg) also reduced the dye leakage significantly, similar to GL at the dose of 160 mg/kg (p < 0.01).
Anti-inflammatory effects of GL on acetic acid-induced vascular permeability in mice. NS (10 ml/kg, i.p.), GL (40,80,160 mg/kg, i.p.), and indometacin (10 mg/kg, i.p.) were administered 1 h before 0.7 % acetic acid (10 ml/kg, i.p.), which was followed with 0.5 % Evans blue solution (10 ml/kg, i.v.) for each mouse. The vehicle-treated animals are acetic acid-induced inflammatory mice. Data are expressed as the mean ± S.E.M. of 10 animals for each group. **p < 0.01 compared with the vehicle group.
Carrageenan-Induced Paw Edema Test
Figure 3 shows the swelling of mice paw increased progressively and peaked at the third hour after carrageenan injection. When a GL dose of 160 mg/kg was given, the inhibition ratios of edema at 1, 2, 3, 4, and 5 h were 65.00, 62.96, 71.85, 73.25, and 76.19 %, respectively, as compared to the vehicle group (p < 0.01). Indometacin (10 mg/kg) inhibited the paw edema markedly through the 5 h following the carrageenan injection.
Anti-inflammatory effects of GL on carrageenan-induced paw edema in mice. NS (10 ml/kg, i.p.), indometacin (10 mg/kg, i.p.), and GL (40, 80, 160 mg/kg, i.p.) were administered 1 h before carrageenan injection. The vehicle-treated animals are carrageenan-induced inflammatory mice. Data are expressed as the mean ± S.E.M. of 10 animals for each group. *p < 0.05 and **p < 0.01 compared with the vehicle group; ## p < 0.01 compared with the control group.
Evaluation of Anti-nociceptive Activity
Acetic Acid-Induced Writhing Test
In the writhing test, Fig. 4 shows that GL at 80 and 160 mg/kg markedly decreased the number of writhes, with the inhibition ratios of 35.51 % (p < 0.01) and 54.16 % (p < 0.01), respectively, when compared to the vehicle group. However, the anti-nociceptive effect of GL 40 mg/kg was not significant (p > 0.05). In comparison with the vehicle group, indometacin at 10 mg/kg significantly reduced the number of writhes (p < 0.01) and the inhibition ratio was 51.91 %.
Anti-nociceptive effects of GL on acetic acid-induced writhing responses in mice. Animals were pre-treated with NS (10 ml/kg, i.p.), indometacin (10 mg/kg, i.p.), or GL (40, 80, 160 mg/kg, i.p.) 1 h before 0.6 % acetic acid (10 ml/kg, i.p.). The vehicle-treated animals are acetic acid-induced nociceptive mice. Data are expressed as the mean ± S.E.M. of 10 animals for each group. **p < 0.01 compared with the vehicle group.
Hot Plate Test
The effects of GL in the hot plate test are shown in Fig. 5. In our test, GL (40, 80, 160 mg/kg) had no influence on nociception (p > 0.05), compared with the vehicle group. In contrast, the positive drug morphine (10 mg/kg) showed a notable anti-nociceptive effect (p < 0.01).
Anti-nociceptive effects of GL on reaction times to thermal stimuli in mice. NS (10 ml/kg, i.p.) or GL (40, 80, 160 mg/kg, i.p.) was administered 1 h before thermal stimuli while morphine (10 mg/kg, s.c.) was administered 30 min before. The vehicle-treated animals are thermal stimuli-induced nociceptive mice. Data are expressed as the mean ± S.E.M. of 10 animals for each group. **p < 0.01 compared with the vehicle group.
Formalin Test
As shown in Fig. 6, the formalin test produced a distinct biphasic pain response. In the first phase, only morphine (10 mg/kg) significantly inhibited the biting and licking response, compared with the vehicle group. In contrast, pre-treatment of animals with morphine (10 mg/kg), indometacin (10 mg/kg), and GL (40, 80, 160 mg/kg) inhibited pain response markedly in the second phase with the inhibition ratios of 99.21 % (p < 0.01), 49.30 % (p < 0.01), 28.30 % (p < 0.05), 44.72 % (p < 0.01), and 61.63 %, respectively.
Anti-nociceptive effects of GL on formalin-induced nociception in mice. NS (10 ml/kg, i.p.), indometacin (10 mg/kg, i.p.), or GL (40, 80, 160 mg/kg, i.p.) was administered 1 h before the formalin (2 %, 20 μl) injection while morphine (10 mg/kg, s.c.) was administered 30 min before. The vehicle-treated animals are formalin-induced nociceptive mice. Data are expressed as the mean ± S.E.M. of 10 animals for each group. *p < 0.05 and **p < 0.01 compared with the vehicle group.
Spontaneous Locomotor Activity and Motor Activity Test
As seen in Fig. 7a–b, even after administration of GL (40, 80, 160 mg/kg), both spontaneous locomotor activity and rota-rod performance time were not significantly affected (p > 0.05), as compared with the vehicle group.
Effects of GL on spontaneous locomotor activity and motor coordination in mice. Mice were pre-treated with NS (10 ml/kg, i.p.) or GL (40, 80, 160 mg/kg, i.p.) 1 h before the tests. a Spontaneous locomotor activity. b Motor coordination. Data are expressed as the mean ± S.E.M. of 10 animals for each group.
Real-Time Fluorogenic PCR Assays
To further investigate the mechanisms of anti-inflammatory effects of GL, the expression levels of major cytokines found in carrageenan-induced paw skin tissue, namely, TNF-α, IL-6, and iNOS mRNA, were assessed. The results showed that TNF-α, IL-6, and iNOS mRNA expressions in vehicle group increased significantly as compared with those of the control group (p < 0.01). However, with GL 160 mg/kg treatment, the mRNA expression levels of TNF-α (p < 0.01), IL-6 (p < 0.05), and iNOS (p < 0.05) were suppressed markedly, compared with those of the vehicle group (Fig. 8a–c).
Effects of GL on TNF-α, IL-6, and iNOS mRNA expression in carrageenan-induced mice paw edema tissue. a–c TNF-α, IL-6, and iNOS mRNA expressions in paw edema tissue of mice were measured by quantitation real-time PCR. Mice were treated with NS (10 ml/kg, i.p.) or GL (160 mg/kg). Data are expressed as the mean ± S.E.M. of six animals for each group. *p < 0.05 and **p < 0.01 compared with the vehicle group; # p < 0.05 and ## p < 0.01 compared with the control group.
Western Blot Analysis
In our experiment, there was an increase in the expression of COX-2 in the vehicle group, compared with the control group (p < 0.01). When GL 160 mg/kg was given to the mice, the protein expression level of COX-2 markedly decreased, in comparison with the vehicle group (p < 0.05) (Fig. 9a, b).
Effects of GL on COX-2 expression in carrageenan-induced mice paw edema tissue. a Representative Western blotting bands of COX-2 expression in carrageenan-induced paw edema tissue. b Effect of GL (160 mg/kg) on the COX-2 expression in carrageenan-induced paw edema tissue. Data are expressed as the mean ± S.E.M. of six animals for each group. *p < 0.05 compared with the vehicle group; ## p < 0.01 compared with the control group.
DISCUSSION
Currently, available therapy for the management of inflammatory pain is inadequate in most cases. Furthermore, the usual treatment drugs of inflammatory pain, nonsteroidal anti-inflammatory drugs (NSAIDs), ultimately lead to severe toxicities including gastrointestinal ulceration, bronchospasm, and kidney dysfunction, when they are used for long time. Therefore, the search for new and safe drugs that effectively interfere with pain and inflammatory processes is urgently needed [23]. In our present study, we evaluated the potential anti-inflammatory and anti-nociceptive effects of glycyrrhizin using several pharmacological tools.
The anti-inflammatory activities of GL were assessed using xylene-induced ear edema test, carrageenan-induced paw edema test, and acetic acid-induced vascular permeability test. The xylene-induced ear edema in mice is a preliminary and simple model for screening potential anti-inflammatory drugs [10]. The results of xylene-induced ear edema showed that GL had a significant anti-inflammatory activity. To further demonstrate the anti-inflammatory activity of GL, vascular permeability test and carrageenan-induced paw edema test were performed. Increased vascular permeability is an early and major vascular event in the inflammatory response [24, 25]. The vascular permeability induced by acetic acid causes an increase in the peritoneal fluids of prostaglandin, serotonin, and histamine. Our results showed that GL significantly inhibited the acetic acid-induced increased vascular permeability in mice. The carrageenan-induced paw edema is a useful model to investigate the anti-inflammatory effect of plant extracts and natural products [26]. Carrageenan-induced inflammation consists of two phases [27]: the early phase (first 2 h after carrageenan injection) is attributed to the release of pro-inflammatory mediators, such as histamine and serotonin [28], and the second phase (3–5 h after carrageenan injection) is mainly mediated by kinins, prostaglandin, nitric oxide, cyclooxygenase [28], cytokines, and neutrophil-derived free radicals [29]. In the present study, we observed that GL caused significant reduction of edema in the both phases, revealing that its anti-inflammatory effect is most likely due to the inhibition of different aspects and mediators of inflammation.
NF-κB is the main intracellular pathway involved in the inflammatory response. Some studies demonstrated that inflammatory cytokines (such as TNF-α, IL-6, and iNOS) and inducible enzymes such as COX-2 are both induced through the NF-κB pathway [30, 31]. Excess amount of NO plays an important role in the aggravation of inflammatory diseases; thus, NO production and iNOS expression are considered pharmacologic targets for anti-inflammatory drugs. TNF-α is considered a major initiator of inflammatory responses, which play a vital role in triggering the activation of other cytokines [32], and IL-6 is a pro-inflammatory cytokine, a potent mediator of inflammatory processes [33]. Additionally, some studies demonstrated that various cytokine antagonists were able to reduce inflammatory hyperalgesia, suggesting that cytokine activation is an important step in the inflammatory processes [34]. In our study, the treatment with GL markedly reduced the mRNA expression of TNF-α, IL-6, and iNOS, which demonstrates that the anti-inflammatory effects of GL are likely due to the reduction in the mRNA expression of TNF-α, IL-6, and iNOS.
As COX-2, an inducible cyclooxygenase isoform, plays an important role in the inflammatory responses of a number of inflammatory cells and tissues, inhibition of COX-2 exerted potent anti-inflammatory effects. [35]. Therefore, the level of COX-2 protein expression was further evaluated in our experiments. GL markedly inhibited COX-2 expression in the carrageenan-induced paw edema model. Thus, the results from this study indicated that the anti-inflammatory effect of GL may be associated with inhibiting COX-2 protein expression.
There is a connection between the nociception and the inflammatory response. To estimate the analgesic property of GL, the acetic acid-induced writhing test, the formalin-induced hind paw licking test, and the hot plate test were performed. The acetic acid-induced writhing in mice is the most useful model for preliminary studies of analgesic activity because of its high sensitivity [18]. Our results demonstrated that GL could markedly reduce the number of writhes, suggesting that GL possessed anti-nociceptive effects. However, acetic acid-induced constriction is regarded as a non-selective anti-nociceptive model [36]. Therefore, it is not possible to ascertain whether the anti-nociception was the central or the peripheral effect by using this test alone. The hot plate test is a well-validated model for evaluating centrally acting analgesic drugs [37, 38]. The results of our hot plate test suggested that GL is not a centrally acting analgesic. To ascertain whether the effects of GL were due to a peripheral mechanism, the formalin test was performed. The formalin test, a valid model for analgesic study in vivo, has been reported to produce distinct biphasic pain response [39]. The early phase (0 to 5 min) is associated with the activation of nociceptive neurons by the direct action of formalin [40], and the second phase (15 to 30 min) is thought to be an inflammatory pain response involving the release of many mediators such as histamine, serotonin, prostaglandins, bradykinin, and cytokines [41]. Studies have shown that drugs that act primarily on the central nervous system inhibit both phases, while others that act peripherally, such as anti-inflammatory and nonsteroidal agents, predominantly inhibit the second phase [15, 42]. In our study, GL (similar to anti-inflammatory and nonsteroidal agents) only suppressed the second phase of the formalin-induced nociception, indicating that the analgesic effect of GL is likely due to its peripheral anti-nociceptive mechanisms. It should be noted that GL affected neither the spontaneous locomotor activity in mice nor the motor activity. These results indicated the improbability of the anti-nociceptive effect of GL being due to any degree of motor impairment or sedation.
In conclusion, results of the present study indicated that GL possessed anti-inflammatory and anti-nociceptive effects. They also suggested that the mechanisms of anti-inflammatory and anti-nociceptive effects of GL may be attributed to the inhibition of expression levels of TNF-α, IL-6, iNOS, and COX-2. In addition, the anti-nociceptive action of GL may be dependent on peripheral mechanisms. Based on these results, GL may serve as a useful therapeutic agent for the treatment of painful conditions and inflammatory diseases. However, the optimal therapeutic dose of GL against inflammatory pain was not fully elucidated. A major limitation of the present study is that the exact mechanisms of GL against inflammatory pain have not been identified and need further research.
References
Julius, D., and A.I. Basbaum. 2001. Molecular mechanisms of nociception. Nature 413: 203–210.
Chiu, Y.J., T.H. Huang, C.S. Chiu, T.C. Lu, and W.H. Peng. 2012. Analgesic and anti-inflammatory activities of the aqueous extract from Plectranthus amboinicus (Lour.) Spreng. Both in vitro and in vivo. Evidence-Based Complementary and Alternative Medicine 2012: 508137.
Huang, G.J., B.S. Wang, W.C. Lin, S.S. Huang, and C.Y. Lee. 2012. Antioxidant and anti-inflammatory properties of Longan (Dimocarpus longan Lour.) Pericarp. Evidence-Based Complementary and Alternative Medicine 2012: 709483.
Bogdan, C. 2001. Nitric oxide and the immune response. Nature Immunology 2: 907–916.
Niu, X., H. Zhang, W. Li, Q. Mu, H. Yao, and Y. Wang. 2015. Anti-inflammatory effects of cavidine in vitro and in vivo, a selective COX-2 inhibitor in LPS-induced peritoneal macrophages of mouse. Inflammation 38(2): 923–933.
Utsunomiya, T., M. Kobayashi, R.B. Pollard, and F. Suzuki. 1997. Glycyrrhizin, an active component of licorice roots, reduces morbidity and mortality of mice infected with lethal dose of influenza virus. Antimicrobial Agents and Chemotherapy 41: 551–556.
Okamoto, T. 2000. The protective effect of glycyrrhizin on anti-Fas antibody-induced hepatitis in mice. European Journal of Pharmacology 387: 229–232.
Ohuchi, K., Y. Kamada, S. Tsurufuji, and S. Tsurufuji. 1981. Glycyrrhizin inhibits prostaglandin E2 production by activated peritoneal macrophages from rats. Prostaglandins and Medicine 7: 457–463.
Van Rossum, T.G., A.G. Vulto, W.C. Hop, and S.W. Schalm. 2001. Glycyrrhizin-induced reduction of ALT in European patients with chronic hepatitis C. American Journal of Gastroenterology 96: 2432–2437.
He, X.Y., Q.C. Liu, W. Peng, Y.L. Huang, Y.L. Huang, and C.J. Wu. 2013. Bioactivities and serum pharmacochemistry of Qi-Wei-Xiao-Yan-Tang. Pharmaceutical Biology 51: 629–634.
Li, C.Q., L.C. He, H.Y. Dong, and J.Q. Jin. 2007. Screening for the anti-inflammatory activity of fractions and compounds from Atractylodes macrocephala koidz. Journal of Ethnopharmacology 114: 212–217.
Wang, J.P., Y.M. Zhou, Y.J. Ye, X.M. Shang, and Y.L. Cai. 2011. Topical anti-inflammatory and analgesic activity of kirenol isolated from Siegesbeckia orientalis. Journal of Ethnopharmacology 137: 1089–1094.
Wang, Q.S., L. Yang, W.Y. Cui, L. Chen, and Y.H. Jiang. 2014. Anti-Inflammatory and anti-nociceptive activities of methanol extract from aerial part of Phlomis younghusbandii Mukerjee. Plos One 9(3), e89149.
Li, M.X., X.F. Shang, Z.P. Jia, and R.X. Zhang. 2010. Phytochemical and biological studies of plants from the genus Phlomis. Chemistry & Biodiversity 7: 283–301.
Ribeiro, N.A., T.M. Abreu, H.V. Chaves, M.M. Bezerra, H.S. Monteiro, and R.J. Jorge. 2014. Sulfated polysaccharides isolated from the green seaweed Caulerpa racemosa plays antinociceptive and anti-inflammatory activities in a way dependent on HO-1 pathway activation. Inflammation Research 63: 569–580.
Carballo-Villalobos, A.I., M.E. González-Trujano, and F.J. López-Muñoz. 2014. Evidence of mechanism of action of anti-inflammatory/antinociceptive activities of acacetin. European Journal of Pain 18: 396–405.
Khatun, A., M.Z. Imam, and M.S. Rana. 2015. Antinociceptive effect of methanol extract of leaves of Persicaria hydropiper in mice. BMC Complementary and Alternative Medicine 15: 63–71.
Chen, Y.F., Y. Haung, W.Z. Tang, L.P. Qin, and H.C. Zheng. 2009. Antinociceptive activity of Paederosidic Acid Methyl Ester (PAME) from the n-butanol fraction of Paederia scandens in mice. Pharmacology Biochemistry and Behavior 93: 97–104.
Wang, H.Y., Y.X. Li, L.L. Dun, and T.T. Xu. 2013. Antinociceptive effects of matrine on neuropathic pain induced by chronic constriction injury. Pharmaceutical Biology 7: 844–850.
Soares, D.G., A.M. Godin, R.R. Menezes, R.D. Nogueira, and A.M. Brito. 2014. Anti-inflammatory and antinociceptive activities of Azadirachtin in mice. Planta Medica 80: 630–636.
de Oliveira, A.M., A.F. de Araújo, R.P. Lyra Lemos, L.M. Conserva, J.N. de Souza Ferro, and E. Barreto. 2015. Antinociceptive and anti-inflammatory activity of the siaresinolic acid, a triterpene isolated from the leaves of Sabicea grisea Cham. & Schltdl. var. grisea. Journal of Natural Medicines 69: 232–240.
Fang, J.Q., J.Y. Du, Y. Liang, and J.F. Fang. 2013. Intervention of electroacupuncture on spinal p38 MAPK/ATF-2/VR-1 pathway in treating inflammatory pain induced by CFA in rats. Molecular Pain 9: 1–14.
da Silva, K.A., M.N. Manjavachi, A.F. Paszcuk, M. Pivatto, and C. Viegas Jr. 2012. Plant derived alkaloid (-)-cassine induces anti-inflammatory and anti-hyperalgesics effects in both acute and chronic inflammatory and neuropathic pain models. Neuropharmacology 62: 967–977.
Khor, Y.H., A.K. Teoh, S.M. Lam, D.C. Mo, and S. Weston. 2009. Increased vascular permeability precedes cellular inflammation as asthma control deteriorates. Clinical and Experimental Allergy 39: 1659–1667.
Wilhelm, D.L., and B. Mason. 1960. Vascular permeability changes in inflammation: the role of endogenous permeability factors in mild thermal injury. British Journal of Experimental Pathology 41: 487–506.
Chang, T.N., J.S. Deng, Y.C. Chang, C.Y. Lee, and L. Jung-Chun. 2012. Ameliorative effects of Scopoletin from Crossostephium chinensis against inflammation pain and its mechanisms in mice. Evidence-Based Complementary and Alternative Medicine 2012: 595603.
Vinegar, R., W. Schreiber, and R. Hugo. 1969. Biphasic development of carrageenan oedema in rats. Journal of Pharmacology and Experimental Therapeutics 166: 96–103.
Niu, X., Y. Li, W. Li, H. Hu, H. Yao, and H. Li. 2014. The anti-inflammatory effects of Caragana tangutica ethyl acetate extract. Journal of Ethnopharmacology 152: 99–105.
Ishola, I.O., E.O. Agbaje, O.O. Adeyemi, and R. Shukla. 2014. Analgesic and anti-inflammatory effects of the methanol root extracts of some selected Nigerian medicinal plants. Pharmaceutical Biology 52: 1208–1216.
Cunha, T.M., G.R. Souza, A.C. Domingues, E.U. Carreira, and C.M. Lotufo. 2012. Stimulation of peripheral Kappa opioid receptors inhibits inflammatory hyperalgesia via activation of the PI3Kγ/AKT/nNOS/NO signaling pathway. Molecular Pain 8: 1–10.
Wang, J., X.W. Wang, Y. Zhang, C.P. Yin, and S.W. Yue. 2011. Nuclear factor-κB mediates TRPV4-NO pathway involved in thermal hyperalgesia following chronic compression of the dorsal root ganglion in rats. Behavioural Brain Research 221: 19–24.
Xu, Y.Q., S.J. Jin, N. Liu, Y.X. Li, and J. Zheng. 2014. Aloperine attenuated neuropathic pain induced by chronic constriction injury via anti-oxidation activity and suppression of the nuclear factor kappa B pathway. Biochemical and Biophysical Research Communications 451: 568–573.
Erchler, W.B., and E.T. Keller. 2000. Age-associated increased interleukin-6 gene expression, late-life diseases, and frailty. Annual Review of Medicine 51: 245–270.
Khan, S., O. Shehzad, J. Chun, and Y.S. Kim. 2013. Mechanism underlying anti-hyperalgesic and anti-allodynic properties of anomalin in both acute and chronic inflammatory pain models in mice through inhibition of NF-κB, MAPKs and CREB signaling cascades. European Journal of Pharmacology 718: 448–458.
Smith, W.L., D.L. DeWitt, and R.M. Garavito. 2000. Cyclooxygenases: structural, cellular and molecular biology. Annual Review of Biochemistry 69: 145–182.
Collier, H.O.J., L.C. Dinneen, C.A. Johnson, and C. Schneider. 1968. The abdominal constriction response and its suppression by analgesic drugs in the mouse. British Journal of Pharmacology 32: 295–310.
Damasceno, S.R., F.R. Oliveira, N.S. Carvalho, C.F. Brito, and I.S. Silva. 2014. Carvacryl acetate, a derivative of carvacrol, reduces nociceptive and inflammatory response in mice. Life Sciences 94: 58–66.
Afsar, T., M.R. Khan, S. Razak, S. Ullah, and B. Mirza. 2015. Antipyretic, anti-inflammatory and analgesic activity of Acacia hydaspica R. Parker and its phytochemical analysis. BMC Complementary and Alternative Medicine 15: 136–148.
Xu, Q., Y. Wang, S. Guo, Z. Shen, Y. Wang, and L. Yang. 2014. Anti-inflammatory and analgesic activity of aqueous extract of Flos populi. Journal of Ethnopharmacology 152: 540–545.
Devaraj, S., A.S. Esfahani, S. Ismail, S. Ramanathan, and M.F. Yam. 2010. Evaluation of the anti-nociceptive activity and acute oral toxicity of standardized ethanolic extract of the rhizome of Curcuma xanthorrhiza Roxb. Molecules 15: 2925–2934.
Sani, M.H., Z.A. Zakaria, T. Balan, L.K. Teh, and M.Z. Salleh. 2012. Antinociceptive activity of methanol extract of Muntingia calabura leaves and the mechanisms of action involved. Evidence-Based Complementary and Alternative Medicine 2012: 89361.
Tsai, D.S., M.H. Huang, J.C. Tsai, Y.S. Chang, and Y.J. Chiu. 2015. Analgesic and anti-inflammatory activities of Rosa taiwanensis nakai in mice. Journal of Medicinal Food 18: 592–600.
Acknowledgments
This research was supported by Natural Science Foundation of Ningxia (Grant No. Nz13227). We thank Dr. Margaret for editing our manuscript.
Conflict of Interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
Hong-Ling Wang and Yu-Xiang Li contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, HL., Li, YX., Niu, YT. et al. Observing Anti-inflammatory and Anti-nociceptive Activities of Glycyrrhizin Through Regulating COX-2 and Pro-inflammatory Cytokines Expressions in Mice. Inflammation 38, 2269–2278 (2015). https://doi.org/10.1007/s10753-015-0212-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-015-0212-3