Abstract
Vitamin D has an anabolic effect on bone developmental processes and is involved in maintaining skeletal integrity. In recent years, pediatric cases of vitamin D intoxication have attracted attention. Therefore, the aim of this study was to investigate the influence of long-term administration of physiologically-high-dose calcitriol (1,25(OH)2D3) on bone remodeling in young developing rats. Neonatal rats received once-daily subcutaneous injection of calcitriol (250 ng/kg body weight), or PBS only as a control, for 3 weeks. At 1, 2 and 4 weeks’ post-administration, rats were sacrificed and fixed by transcardial perfusion with 4 % paraformaldehyde, following which tibiae were extracted for histochemical analysis. Compared with the control group, the number of tartrate-resistant acid phosphatase- and Cathepsin K-positive osteoclasts were significantly increased, and the expression of alkaline phosphatase in osteoblasts was decreased in trabecular bone of rats administered high-dose 1,25(OH)2D3, leading to decreased trabecular bone volume. In addition, the expression of receptor activator of nuclear factor kappa-B ligand (RANKL) was increased, while that of osteoprotegerin was weaker in osteoblasts in the experimental group compared with the control group. Moreover, there was weaker immunoreactivity for EphrinB2 in osteoclasts and EphB4 in osteoblasts of trabecular bone in the experimental group compared with the control group. These findings suggest that long-term use of physiologically-high dose calcitriol may result in bone loss through RANKL/RANK/osteoprotegerin and EphrinB2–EphB4 signaling pathways, and that these negative effects could continue after drug withdrawal. Therefore, optimal limits for vitamin D administration need to be established for children and adolescents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
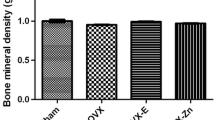
Vitamin D is a hormone involved in calcium homeostasis through its actions on the intestine, kidney, parathyroid gland, and bone (van Leeuwen et al. 2001). It is essential for optimal calcium absorption needed for maintaining normal bone mineral density (BMD) (Woeckel et al. 2010). Calcitriol, also called 1,25-dihydroxy vitamin D3 (1,25(OH)2D3), is the active metabolite of vitamin D3 and is involved in various physiological processes, including calcium homeostasis, bone metabolism and the immune response (Inada et al. 2008). Vitamin D-deficiency, as a greater risk of osteoporosis, results in poorly mineralized bone, with diminished strength and load-bearing capacity, and is linked to rickets in infants and osteomalacia in adults, both of which are skeletal disorders characterized by defective bone mineralization (Suda et al. 2003; Oku et al. 2016). Moreover, the administration of vitamin D to ovariectomized or rachitic animals can relieve impaired bone mineralization (Inada et al. 2008). Therefore, vitamin D is one of the major critical factors involved in bone metabolism.
1,25(OH)2D3 is widely used as an antiresorptive agent for the management of 1,25(OH)2D3 deficiency and secondary hyperparathyroidism in children and adolescents (Ghergherechi et al. 2012; Alshamsan and Bin-Abbas 2016; Dura-Trave and Gallinas-Victoriano 2016). Though vitamin D is necessary for basal bone homeostasis, excessive concentrations may be harmful. Masayoshi et al. demonstrated that high dose 1,25(OH)2D3 inhibits osteoblast mineralization in vitro (Yamaguchi and Weitzmann 2012). And, high dose of 1,25(OH)2D3 acts on the osteoblasts to induce the formation of osteoclasts in a co-culture system in vitro (Takahashi et al. 2014; Cong et al. 2015). Moreover, high-dose maternal 1,25(OH)2D3 can transferred across the placental barrier and injure fetal development or birth (Lieben et al. 2013). In addition, recently, pediatric cases of vitamin D intoxication (VDI) with dietary supplements have drawn our attention. Rajakumar et al. (2013) described a case study of an infant who had hypervitaminosis D caused by a dosing error in an over-the-counter vitamin D supplement. Cengiz et al. reported seven children aged between 0.7 and 4.2 years were admitted with symptoms of hypercalcemia caused by the consumption of a fish oil supplement containing an excessively high dose of vitamin D caused by a manufacturing error (Kara et al. 2014).
To date, though VDI attracted our attention, there is limited data available on the effects of long term administration of high-dose 1,25(OH)2D3 on bone metabolism in children and rodent models in vivo, especially the histological evidence (Fig. 1). Therefore, in the current study, we used neonatal rats administered with physiologically-high-dose 1,25(OH)2D3 to investigate its effects on bone development. Our results indicate that long-term use of high-dose 1,25(OH)2D3, even physiological-high-dose, was harmful to bone, and this negative effects will continue. Therefore, optimal concentrations and protocol for the administration of vitamin D need to be established for humans.
Materials and methods
Animal and tissue preparation
All animal experiments in this study were conducted according to the Guidelines for Animal Experimentation of Shandong University. Pregnant rats were obtained from Laboratory Animal Centre of Shandong University (Jinan, China) and kept in plastic cages (1 animal per cage) under standard laboratory. All rats were fed a standard rodent diet ad libitum. Neonatal rats from them were randomly divided into two groups, experimental group and control group (30 rats per group). Calcitriol (Selleck Chemicals, Houston, TX, USA) was dissolved in a small amount of ethanol and diluted with PBS to a final concentration of 1 mg/ml. The newborn rats in the experimental group were further subdivided into three groups (groups A, B, C; ten rats per group), which were then received single, once-daily subcutaneous injections of calcitriol (250 ng/kg body weight) for 1, 2, 3 weeks respectively (group A for 1 week, group B for 2 weeks, group C for 3 weeks). The rats of groups A and B were sacrificed after the indicated administration periods. To determine whether the effects of calcitriol on the development of rats would persist after the drug withdrawal, after 3 weeks of calcitriol administration, the rats of group C were withdrawn from drug treatment and kept for another week followed by execution at the fourth week. The high dose of 1,25(OH)2D3 was utilized as it elicits a maximal physiologic response in normal rats (Ng et al. 2014; Yao et al. 2005). The rats were given only PBS as control (same quantity and frequency with the VD group) and sacrificed at the indicated time points corresponding to their respective experimental groups.
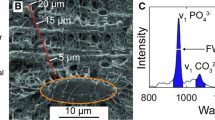
After the above treatment, the rats were anesthetized with an intraperitoneal injection of 10 % chloral hydrate (400 mg/100 g body weight) and fixed with 4 % paraformaldehyde in 0.1 M phosphate buffer (pH 7.4) by transcardial perfusion, respectively. After fixation, tibiae were removed and immersed in the same fixative for additional 24 h. Following that, samples were decalcified with 10 % EDTA–2Na solution for 3 weeks at 4 °C. Then the specimens were dehydrated through an ascending ethanol series and then embedded in paraffin using standard procedures. Serial longitudinal 5-μm-thick sections were prepared for following histological analysis using sliding microtome (LEICA SM 2010R, Heidelberger, German).
Histological examination and image analysis
Hematoxylin and eosin (H&E) staining were performed to identify the morphology of metaphysis in both groups. Stained sections were observed and digital images were taken with a light microscope (Olympus BX-53, Tokyo, Japan). Trabecular bone volume (BV/TV, bone volume/tissue volume × 100 %) were measured by Image-Pro Plus 6.2 software (Media Cybernetics, Silver Spring, MD, USA). Specifically, ten slices of each sample were used for quantitative histomorphometric analysis to get the mean value.
Histochemistry (TRAP staining) for osteoclasts
To evaluate the osteoclasts, tartrate-resistant acid phosphatase (TRAP) staining was performed as previously showed (Li et al. 2013). In brief, dewaxed paraffin sections were submerged in a mixture of 3.0 mg of naphthol AS-BI phosphate, 18 mg of red violet LB salt, and 100 mM l(+) tartaric acid (0.36 g) diluted in 30 ml of 0.1 M sodium acetate buffer (PH 5.0) for 15 min at 37 °C. The sections were then faintly counterstained with methyl green for assessing by light microscopy (Olympus BX-53, Tokyo, Japan). Osteoclasts numbers were counted in three randomly selected non-overlapping microscopic fields in each section by Image-Pro Plus 6.2 software (Media Cybernetics, Silver Spring, MD, USA). At least ten sections from each sample were analyzed.
Immunohistochemistry for ALP, CK, RANKL, OPG, EphrinB2 and EphB4
To evaluate the activities of osteoblasts and osteoclasts, immunohistochemistry of (alkaline phosphatase) ALP and (Cathepsin K) CK were performed respectively. RANKL/RANK/OPG pathway and EphrinB2/EphB4 pathway are both involved in the normal coupling process between osteoclasts and osteoblasts, thus the sections were examined for RANKL, OPG, EphrinB2 and EphB4 immunohistochemistry staining after calcitriol administered. Briefly, after xylene treatment, dewaxed paraffin sections were pretreated with 0.3 % hydrogen peroxide for 30 min, and then with 1 % bovine serum albumin (BSA; seologicals proteins Inc. Kankakee, IL, USA) in PBS (1 % BSA-PBS) for 20 min to reduce non-specific staining. The sections were then incubated for 2 h at room temperature with: (1) rabbit antiserum against rat tissue nonspecific ALP, generated by Oda et al. (1999) at a dilution of 1:100; (2) anti-CK antibody (Abcam, Cambrige, MA, USA) at a dilution of 1:100; (3) anti-RANKL antibody (Santa Cruz Biotechology, Santa Cruz, CA, USA) at a dilution of 1:50; (4) anti-OPG antibody (Abcam, Cambrige, MA, USA) at a dilution of 1:50; (5) Mouse EphrinB2 antibody (R&D Systems, Minneapolis, MI, USA) at a dilution of 1:25; (6) Mouse EphB4 antibody (R&D systems, Minneapolis, MI, USA) at a dilution of 1:50 in 1 % BSA-PBS. After rinsing with PBS, the sections were incubated with horseradish peroxidase-conjugated swine anti-rabbit IgG (DaKo, Glostrup, Denmark) for ALP, CK, RANKL and OPG; rabbit anti-Goat IgG (Jackson ImmunoResearch Labortories, Inc, Baltimore, MD, USA) for EphrinB2 and EphB4 1 h at room temperature. The immunoreaction was visualized with diaminobenzidine (DAB) (Sigma-Aldrich, St. Louis, MO, USA). All sections were counterstained faintly with methyl green and observed under a light microscope (Olympus BX-53, Tokyo, Japan). Immunostaining intensities (optical density, OD) were also analyzed using Image-Pro Plus 6.2 software. Positive reaction areas of ALP, CK, RANKL, OPG, EphrinB2 and EphB4 were manually selected through color cube based manner. At least ten sections from each sample were analyzed. In addition, metaphysis of each tissue section was selected to be evaluated at 4× magnification, in which the metaphysis was totally included.
Statistical analysis
All statistical analyses were performed using SPSS software. All values are presented as mean ± standard deviation (SD) in the results and scatter plots of individual data points in the figures. The differences between 1,25(OH)2D3 administered group and control were assessed by student’s t test, and considered statistically significant at *p < 0.05 and **p < 0.01.
Results
Histological alterations of tibial metaphysis and statistical analysis
At 1, 2 and 4 weeks after 1,25(OH)2D3 administration, high-dose 1,25(OH)2D3-treated rats showed obvious decreases in trabecular bone volume compared with that of the control group (Fig. 2a–f). Statistical analysis revealed several significant differences between the 1,25(OH)2D3 administration (VD) and control groups regarding trabecular bone volume density (BV/TV; 1 week: 19.22 ± 0.81 % in the VD group vs. 38.71 ± 1.30 % in the control, p < 0.01, 2 weeks: 25.02 ± 1.09 % in the VD group vs.33.38 ± 0.68 % in the control, p < 0.01, 4 week: 19.07 ± 0.71 % in the VD group vs.33.10 ± 1.12 % in the control, p < 0.01, Fig. 2g).
Histological alterations and statistical analysis. Hematoxylin-eosin staining of tibiae shows the differences between the two groups. a–c low magnification of tibiae of control group (a 1 week, b 2 weeks, c 4 weeks); d–f low magnification of tibiae of 1,25(OH)2D3-administered group (d 1 week, e 2 weeks, f 4 weeks). g The mean values of BV/TV were assessed for both groups by using statistics (n = 10; **p < 0.01). At 1, 2, 4 weeks after 1,25(OH)2D3 administration for 3 weeks, tibiae showed obvious histological manifestation of decreased trabecular bone volume. All corresponding numerical information is found in the results section. Error bars indicate ±SD. TB trabecular bone, BV/TV trabecular bone volume/tissue volume. a–f ×40
Tartrate-resistant acid phosphatase (TRAP) staining and Cathepsin K (CK) immunolocalization
Compared with control group, the number of TRAP-positive osteoclasts was significantly increased on the surface of trabecular bone in rats administered with physiologically-high-dose 1,25(OH)2D3. Osteoclasts in the control group were flat and slender with 2–3 nuclei, whereas osteoclasts in the VD group were round or polygonal with many nuclei (Fig. 3a–f). Statistical analysis found a significant difference in the numbers of osteoclasts between the VD and control groups (1 week: 40.00 ± 2.58 in the VD group vs. 26.02 ± 1.32 in the control, p < 0.01, 2 weeks: 75.03 ± 3.61 in the VD group vs. 41.05 ± 2.48 in the control, p < 0.01, 4 weeks: 85.01 ± 3.21 in the VD group vs. 54.04 ± 3.71 in the control, p < 0.01, Fig. 3g). CK staining showed stronger CK expression in the VD group compared with the control (Fig. 4a–f). Statistical analysis revealed significant differences in the optical densities of CK between the VD and control groups (1 week: 0.358 ± 0.005 in the VD group vs. 0.148 ± 0.004 in the control, p < 0.01, 2 weeks: 0.283 ± 0.004 in the VD group vs. 0.156 ± 0.003 in control, p < 0.01, 4 weeks: 0.260 ± 0.005 in the VD group vs. 0.112 ± 0.003 in the control, p < 0.01, Fig. 4g).
TRAP staining for osteoclasts in the trabecular bone and statistical analysis. Upper line (a 1 week, b 2 weeks, c 4 weeks) control group; lower line (d 1 week, e 2 weeks, f 4 weeks) 1,25(OH)2D3 administration group. The osteoclasts in control group were flat and slender with 2–3 nuclei (a–c); Whereas in experimental groups the osteoclasts were round and polygon with many nuclei (d–f). g TRAP-positive osteoclasts were counted in the metaphysis of tibiae for both groups (n = 10; **p < 0.01). All corresponding numerical information is found in the results section. Error bars indicate ±SD. SD standard deviation; a–f ×100; cells ×400
Immunolocalization of CK in the trabecular bone and statistical analysis. Upper line (a 1 week, b 2 weeks, c 4 weeks) control group; lower line (d 1 week, e 2 weeks, f 4 weeks) 1,25(OH)2D3 administration group. Weak expression of CK in the control group with flat and slender osteoclasts (a 1 week, b 2 weeks; c 4 weeks), while intense expression of CK in the 1,25(OH)2D3 administration group with round and polygon osteoclasts (d 1 week, e 2 weeks; f 4 weeks). g Mean optical density of CK immunoreactivity were assessed in the trabecular bone for both groups (n = 10; **p < 0.01). All corresponding numerical information is found in the results section. Error bars indicate ±SD. SD standard deviation; a–f ×100; cells ×400
Alkaline phosphatase (ALP), RANKL and osteoprotegerin (OPG) immunolocalization
In the VD group, trabecular bone of the metaphysis showed stronger RANKL expression and weaker ALP and OPG expression than the control at all time points (Figs. 5a–f, 6a–l). Statistical analysis revealed significant differences in ALP-, RANKL-, OPG-immunoreactivity between the VD and control groups (ALP: 1 week: 0.025 ± 0.002 in the VD group vs. 0.056 ± 0.003 in the control, p < 0.01, 2 weeks: 0.010 ± 0.002 in the VD group vs. 0.099 ± 0.004 in the control, p < 0.01, 4 weeks: 0.027 ± 0.002 in the VD group vs. 0.121 ± 0.003 in the control, p < 0.01, Fig. 5g; RANKL: 1 week: 0.149 ± 0.005 in the VD group vs. 0.066 ± 0.003 in the control, p < 0.01, 2 weeks: 0.106 ± 0.002 in the VD group vs. 0.049 ± 0.003 in the control, p < 0.01, 4 weeks: 0.088 ± 0.002 in the VD group vs. 0.051 ± 0.003 in the control, p < 0.01, Fig. 6m; OPG: 1 week: 0.052 ± 0.002 in the VD group vs. 0.110 ± 0.004 in the control, p < 0.01, 2 weeks: 0.027 ± 0.002 in the VD group vs. 0.099 ± 0.003 in the control, p < 0.01, 4 weeks: 0.029 ± 0.002 in the VD group vs. 0.081 ± 0.003 in the control, p < 0.01, Fig. 6n).
Immunolocalization of ALP in the trabecular bone and statistical analysis. Upper line (a 1 week, b 2 weeks, c 4 weeks) control group; lower line (d 1 week, e 2 weeks, f 4 weeks) 1,25(OH)2D3 administration group. Comparing to the control group (a 1 week, b 2 weeks, c 4 weeks), weaker expressions of ALP were showed in the 1,25(OH)2D3 administration group (d 1 week, e 2 weeks, f 4 weeks). g Mean optical density of ALP immunoreactivity were assessed in the trabecular bone for both groups (n = 10; **p < 0.01). All corresponding numerical information is found in the results section. Error bars indicate ±SD. SD standard deviation; a–f ×200
Immunolocalization of RANKL and OPG in the trabecular bone and statistical analysis. Upper line (a 1 week, b 2 weeks, c 4 weeks, g 1 week, h 2 weeks, i 4 weeks) control group; lower line (d 1 week, e 2 weeks, f 4 weeks, j 1 week, k 2 weeks, l 4 weeks) 1,25(OH)2D3 administration group. Weak expression of RANKL in the control group (a 1 week, b 2 weeks, c 4 weeks), while stronger expression of RANKL were showed in the 1,25(OH)2D3 administration group (d 1 week, e 2 weeks, f 4 weeks). Comparing to the control group (g 1 week, h 2 weeks, i 4 weeks), weaker expression of OPG were observed in the 1,25(OH)2D3 administration group (j 1 week, k 2 weeks, l 4 weeks). M and N: mean optical density of RANKL and OPG immunoreactivity were assessed in the trabecular bone for both groups, respectively (n = 10; **p < 0.01). All corresponding numerical information is found in the results section. Error bars indicate ±SD. SD standard deviation. a–l ×200
EphrinB2 and EphB4 immunolocalization
In the VD group, trabecular bone of the metaphysis showed weaker EphrinB2 expression in osteoclasts and EphB4 in osteoblasts at all time points compared with the control group (Fig. 7a–l). Statistical analysis revealed significant differences in EphrinB2- and EphB4-immunoreactivity between the VD and control groups (EphrinB2, 1 week: 0.071 ± 0.002 in the VD group vs. 0.117 ± 0.004 in the control, p < 0.01, 2 weeks: 0.038 ± 0.002 in the VD group vs. 0.098 ± 0.003 in the control, p < 0.01, 4 weeks: 0.040 ± 0.003 in the VD group vs. 0.126 ± 0.003 in the control, p < 0.01, Fig. 7m; EphB4, 1 week: 0.078 ± 0.003 in the VD group vs. 0.104 ± 0.003 in control, p < 0.01, 2 weeks: 0.062 ± 0.002 in the VD group vs. 0.091 ± 0.004 in the control, p < 0.01, 4 weeks: 0.052 ± 0.002 in the VD group vs. 0.110 ± 0.003 in the control, p < 0.01, Fig. 7n).
Immunolocalization of EphrinB2 and EphB4 in the trabecular bone and statistical analysis. Upper line (a 1 week, b 2 weeks, c 4 weeks, g 1 week, h 2 weeks, i 4 weeks) control group; lower line (d 1 week, e 2 weeks, f 4 weeks, j 1 week, k 2 weeks, l 4 weeks) 1,25(OH)2D3 administration group. Intense expression of EphrinB2 of the control group (a 1 week, b 2 weeks, c 4 weeks), while weak expression of EphrinB2 (d 1 week, e 2 weeks, f 4 weeks) in the 1,25(OH)2D3 administration group. Intense expression of EphB4 of the control group (g 1 week, h 2 weeks, i 4 weeks), while weak expression of EphB4 (j 1 week, k 2 weeks, l 4 weeks) in the 1,25(OH)2D3 administration group. M and N: mean optical density of EphrinB2 and EphB4 immunoreactivity were assessed in the trabecular bone for both groups, respectively (n = 10; **p < 0.01). All corresponding numerical information is found in the results section. Error bars indicate ±SD. SD standard deviation. a–l ×200
Discussion
In this study, 3-week-continuous administration of high-dose 1,25(OH)2D3 stimulated osteoclastogenesis and inhibited the activity of osteoblasts, which resulted in decreased trabecular bone volume (Fig. 8). In addition, these negative effects could continuously affect bone metabolism after drug withdrawal.
1,25(OH)2D3 has been shown to affect certain bone cells, targeting each of the major bone cell types either directly or indirectly to influence the anabolic and catabolic processes of bone remodeling. Calcitriol, the activated form of vitamin D3, has opposing effects on osteoblast differentiation (Hicok et al. 1998; Lohmann et al. 2000; Li et al. 2008). Furthermore, supraphysiological doses of 1,25(OH)2D3 inhibit cancellous bone formation, exerting a negative influence on bone quality, beginning from 1-week post-administration and intensifying after 1 month of exposure (Idelevich et al. 2011). In the present study, we noticed that even at a physiologically-high dose, 1,25(OH)2D3 inhibited osteogenesis, inhibited the activity of osteoblasts and reduced bone formation in vivo.
TRAP, a histochemical and biochemical marker for osteoclasts, allows for the examination of osteoclastic differentiation and function (Cole and Walters 1987). Regarding osteoclastogenesis, our results revealing that high-dose calcitriol increased the number of TRAP-positive osteoclasts are consistent with some previous studies, in which calcitriol strongly stimulated the formation of osteoclasts and induced the expression of RANKL and macrophage colony-stimulating factor (M-CSF), both in vitro and in vivo, leading to bone resorption (Suda et al. 1999; Sato et al. 2007). However, other studies have shown that calcitriol inhibited osteoclast formation. Specifically, calcitriol was reported to inhibit the induction of c-fos and nuclear factor of activated T cells c1 (NFATc1) and upregulated the expression of interferon-beta (IFN-beta), which are key regulators of osteoclast formation (Takasu et al. 2006; Sakai et al. 2009). In addition, our previous studies reported that local administration of calcitriol promoted osteogenesis and mineralization, which could be promising for the restoration of mandibular bone defects (Feng et al. 2015; Liu et al. 2015). More interestingly, in thyroparathyroidectomized rats infused with parathyroid hormone (PTH), systemically administered calcitriol inhibited PTH-induced bone resorption at a physiological dose and stimulated bone resorption at a toxic dose (Ueno et al. 2003). Overall, these results indicate that calcitriol may function by stimulating or inhibiting bone resorption, depending on the dose and route of administration.
Vitamin D is a moderator of osteoclastic activity and not just an inducer of osteoclastogenesis. The effects of vitamin D on osteoclastic activity has largely been established to be mediated via 1,25(OH)2D3 activity on osteoblasts, which regulates the secretion of the key osteoclastogenesis factor, RANKL. RANKL/OPG ratio is an index of osteoclastogenic stimulation (Tanaka et al. 2011) and plays a key role in the regulation of bone metabolism (Martin 2013). In this study, we found that high-dose 1,25(OH)2D3 obviously increased the expression of RANKL and decreased the expression of OPG. This change in RANKL/OPG ratio resulted in augmented osteoclast numbers and activities, accelerating trabecular bone remodeling. Such metabolic effects of active vitamin D were in line with a previous report that 1,25(OH)2D3 promoted the expression of RANKL in osteoblasts in vitro (Takahashi et al. 2014).
Recent studies revealed the importance of EphB4 and EphrinB2 during the “coupling” of osteoblast and osteoclast function in bone remodeling. Activation of EphB receptors by the ephrinB ligands is referred to as “forward signaling,” whereas activation of the ephrinB ligands by the EphB receptors is designated “reverse signaling.” (Zhao et al. 2006; Allan et al. 2008; Irie et al. 2009). The osteogenic potential of osteoblasts was enhanced by forward signaling via EphB4, while the differentiation and function of osteoclasts was inhibited by reverse signaling through EphrinB2 (Zhao et al. 2006). In the present study, we demonstrated that the expressions of both EphrinB2 and EphB4 were downregulated in tibia of the VD group, with decreased bone mass and increased osteoclastic activities compared with the control group. Supportive studies demonstrated that inhibition of EphrinB2/EphB4 signaling using a blocking peptide (TNYL) or a decoy soluble form of EphB4 (sEphB4) caused the inhibition of mineralization of human mesenchymal stem cells (Arthur et al. 2011) and mouse bone marrow stromal cells (Allan et al. 2008; Martin et al. 2010) in vitro. Moreover, increased expressions of EphB4 and EphrinB2 by genistein, an isoflavone that can bind to and activate estrogen receptors, improved glucocorticoid-induced osteoporosis (Cheng et al. 2015). Taken together, EphrinB2/EphB4 signaling may play an important role in the reduction of bone mass associated with high dose of vitamin D administration.
In conclusion, our results suggest that long-term administration of high-dose 1,25(OH)2D3 during bone development, even a maximal physiological dose, can increase osteoclast numbers and activities, and decrease bone formation through the RANKL/RANK/OPG and EphrinB2/EphB4 signaling pathways, subsequently impairing bone metabolism. Optimal dosages for vitamin D supplementation for its positive effects on bone metabolism, without causing side effects, need to be determined.
References
Allan EH, Häusler KD, Wei T, Gooi JH, Quinn JM, Crimeen-Irwin B, Pompolo S, Sims NA, Gillespie MT, Onyia JE, Martin TJ (2008) EphrinB2 regulation by PTH and PTHrP revealed by molecular profiling in differentiating osteoblasts. J Bone Miner Res 23:1170–1181
Alshamsan FM, Bin-Abbas BS (2016) Knowledge, awareness, attitudes and sources of vitamin D deficiency and sufficiency in Saudi children. Saudi Med J 37:579–583
Arthur A, Zannettino A, Panagopoulos R, Koblar SA, Sims NA, Stylianou C, Matsuo K, Gronthos S (2011) EphB/ephrin-B interactions mediate human MSC attachment, migration and osteochondral differentiation. Bone 48:533–542
Cheng Y, Wang WL, Liang JJ (2015) Genistein attenuates glucocorticoid-induced bone deleterious effects through regulation Eph/ephrin expression in aged mice. Int J Clin Exp Pathol 8:394–403
Cole AA, Walters LM (1987) Tartrate-resistant acid phosphatase in bone and cartilage following decalcification and cold-embedding in plastic. J Histochem Cytochem: Off J Histochem Soc 35:203–206
Cong L, Zhang C, Tu G (2015) Osteoblastic NF-kappaB pathway is involved in 1alpha, 25(OH)2D3-induced osteoclast-like cells formation in vitro. Int J Clin Exp Pathol 8:5988–5996
Dura-Trave T, Gallinas-Victoriano F (2016) Seasonal variations in calcidiol and parathyroid hormone levels in healthy children and adolescents in Navarre, Spain: a cross-sectional study. JRSM Open 7:2054270416632704
Feng W, Lv S, Cui J, Han X, Du J, Sun J, Wang K, Wang Z, Lu X, Guo J, Oda K, Amizuka N, Xu X, Li M (2015) Histochemical examination of adipose derived stem cells combined with beta-TCP for bone defects restoration under systemic administration of 1alpha,25(OH)2D3. Mater Sci Eng C Mater Biol Appl 54:133–141
Ghergherechi R, Hazhir N, Tabrizi A (2012) Comparison of vitamin D deficiency and secondary hyperparathyroidism in obese and non-obese children and adolescents. Pak J Biol Sci 15:147–151
Hicok KC, Thomas T, Gori F, Rickard DJ, Spelsberg TC, Riggs BL (1998) Development and characterization of conditionally immortalized osteoblast precursor cell lines from human bone marrow stroma. J Bone Miner Res: Off J Am Soc Bone Miner Res 13:205–217
Idelevich A, Kerschnitzki M, Shahar R, Monsonego-Ornan E (2011) 1,25(OH)2D3 alters growth plate maturation and bone architecture in young rats with normal renal function. PLoS One 6:e20772
Inada M, Tsukamoto K, Hirata M, Takita M, Nagasawa K, Miyaura C (2008) Novel vitamin D3 analogs, 1alpha, 25(OH)2D(3)-26, 23-lactam (DLAMs), antagonize bone resorption via suppressing RANKL expression in osteoblasts. Biochem Biophys Res Commun 372:434–439
Irie N, Takada Y, Watanabe Y, Matsuzaki Y, Naruse C, Asano M, Iwakura Y, Suda T, Matsuo K (2009) Bidirectional signaling through ephrinA2–EphA2 enhances osteoclastogenesis and suppresses osteoblastogenesis. J Biol Chem 284:14637–14644
Kara C, Gunindi F, Ustyol A, Aydin M (2014) Vitamin D intoxication due to an erroneously manufactured dietary supplement in seven children. Pediatrics 133:e240–244
Li Y, Bäckesjö CM, Haldosén LA, Lindgren U (2008) Species difference exists in the effects of 1 alpha, 25(oh)(2)d(3) and its analogue 2-methylene-19-nor-(20 s)-1,25-dihydroxy vitamin d(3) (2md) on osteoblastic cells. J Steroid Biochem 112:110–116 (Lieben)
Li M, Hasegawa T, Hogo H, Tatsumi S, Liu Z, Guo Y, Sasaki M, Tabata C, Yamamoto T, Ikeda K, Amizuka N (2013) Histological examination on osteoblastic activities in the alveolar bone of transgenic mice with induced ablation of osteocytes. Histol Histopathol 28:327–335
Lieben L, Stockmans I, Moermans K, Carmeliet G (2013) Maternal hypervitaminosis D reduces fetal bone mass and mineral acquisition and leads to neonatal lethality. Bone 57:123–131
Liu HR, Cui J, Feng W, Lv SY, Du J, Sun J, Han XC, Wang ZM, Lu X, Yimin Oda K, Amizuka N, Li MQ (2015) Local administration of calcitriol positively influences bone remodeling and maturation during restoration of mandibular bone defects in rats. Mater Sci Eng C 49:14–24
Lohmann CH, Bonewald LF, Sisk MA, Sylvia VL, Cochran DL, Dean DD, Boyan BD, Schwartz Z (2000) Maturation state determines the response of osteogenic cells to surface roughness and 1,25-dihydroxy vitamin D3. J Bone Miner Res 15:1169–1180
Martin TJ (2013) Historically significant events in the discovery of RANK/RANKL/OPG. World J Orthop 4:186–197
Martin TJ, Allan EH, Ho PW, Gooi JH, Quinn JM, Gillespie MT, Krasnoperov V, Sims NA (2010) Communication between ephrinB2 and EphB4 within the osteoblast lineage. Adv Exp Med Biol 658:51–60
Ng AH, Frick KK, Krieger NS, Asplin JR, Cohen-McFarlane M, Culbertson CD, Kyker-Snowman K, Grynpas MD, Bushinsky DA (2014) 1,25(OH)(2)D(3) induces a mineralization defect and loss of bone mineral density in genetic hypercalciuric stone-forming rats. Calcifi Tissue Int 94:531–543
Oda K, Amaya Y, Fukushi-Irie M, Kinameri Y, Ohsuye K, Kubota I, Fujimura S, Kobayashi J (1999) A general method for rapid purification of soluble versions of glycosylphosphatidylinositol-anchored proteins expressed in insect cells: an application for human tissue-nonspecific alkaline phosphatase. J Biochem 126:694–699
Oku Y, Tanabe R, Nakaoka K, Yamada A, Noda S, Hoshino A, Haraikawa M, Goseki-Sone M (2016) Influences of dietary vitamin D restriction on bone strength, body composition and muscle in rats fed a high-fat diet: involvement of mRNA expression of MyoD in skeletal muscle. J Nutr Biochem 32:85–90
Rajakumar K, Reis EC, Holick MF (2013) Dosing error with over-the-counter vitamin D supplement: a risk for vitamin D toxicity in infants. Clin Pediatr 52:82–85
Sakai S, Takaishi H, Matsuzaki K, Kaneko H, Furukawa M, Miyauchi Y, Shiraishi A, Saito K, Tanaka A, Taniguchi T, Suda T, Miyamoto T, Toyama Y (2009) 1-Alpha, 25-dihydroxy vitamin D3 inhibits osteoclastogenesis through IFN-beta-dependent NFATc1 suppression. J Bone Miner Metab 27:643–652
Sato M, Nakamichi Y, Nakamura M, Sato N, Ninomiya T, Muto A, Nakamura H, Ozawa H, Iwasaki Y, Kobayashi E, Shimizu M, DeLuca HF, Takahashi N, Udagawa N (2007) New 19-nor-(20S)-1alpha,25-dihydroxy vitamin D3 analogs strongly stimulate osteoclast formation both in vivo and in vitro. Bone 40:293–304
Suda T, Takahashi N, Udagawa N, Jimi E, Gillespie MT, Martin TJ (1999) Modulation of osteoclast differentiation and function by the new members of the tumor necrosis factor receptor and ligand families. Endocr Rev 20:345–357
Suda T, Ueno Y, Fujii K, Shinki T (2003) Vitamin D and bone. J Cell Biochem 88:259–266
Takahashi N, Udagawa N, Suda T (2014) Vitamin D endocrine system and osteoclasts. Bonekey Rep 3:495
Takasu H, Sugita A, Uchiyama Y, Katagiri N, Okazaki M, Ogata E, Ikeda K (2006) c-Fos protein as a target of anti-osteoclastogenic action of vitamin D, and synthesis of new analogs. J Clin investig 116:528–535
Tanaka H, Mine T, Ogasa H, Taguchi T, Liang CT (2011) Expression of RANKL/OPG during bone remodeling in vivo. Biochem Biophys Res Commun 411:690–694
Ueno Y, Shinki T, Nagai Y, Murayama H, Fujii K, Suda T (2003) In vivo administration of 1,25-dihydroxy vitamin D3 suppresses the expression of RANKL mRNA in bone of thyroparathyroidectomized rats constantly infused with PTH. J Cell Biochem 90:267–277
van Leeuwen JP, van Driel M, van den Bemd GJ, Pols HA (2001) Vitamin D control of osteoblast function and bone extracellular matrix mineralization. Crit Rev Eukaryot Gene Expr 11:199–226
Woeckel VJ, Alves RD, Swagemakers SM, Eijken M, Chiba H, van der Eerden BC, van Leeuwen JP (2010) 1Alpha,25-(OH)2D3 acts in the early phase of osteoblast differentiation to enhance mineralization via accelerated production of mature matrix vesicles. J Cell Physiol 225:593–600
Yamaguchi M, Weitzmann MN (2012) High dose 1,25(OH)2D3 inhibits osteoblast mineralization in vitro. Int J Mol Med 29:934–938
Yao JJ, Bai S, Karnauskas AJ, Bushinsky DA, Favus MJ (2005) Regulation of renal calcium receptor gene expression by 1,25-dihydroxy vitamin D3 in genetic hypercalciuric stone-forming rats. J Am Soc Nephrol 16:1300–1308
Zhao C, Irie N, Takada Y, Shimoda K, Miyamoto T, Nishiwaki T, Suda T, Matsuo K (2006) Bidirectional ephrinB2–EphB4 signaling controls bone homeostasis. Cell Metab 4:111–121
Acknowledgments
This study was partially supported by the National Nature Science Foundation of China (Grant Nos. 81271965; 81470719; 8151101150) to Li M.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
We declare that we have no conflict of interest.
Additional information
Jing Sun and Bao Sun have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Sun, J., Sun, B., Wang, W. et al. Histochemical examination of the effects of high-dose 1,25(OH)2D3 on bone remodeling in young growing rats. J Mol Hist 47, 389–399 (2016). https://doi.org/10.1007/s10735-016-9681-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10735-016-9681-4