Abstract
Asthma is the most common chronic illness in children living in developed countries and the leading cause of childhood hospitalization and school absenteeism. Prevalence rates of asthma are increasing and show disparities across gender, geographic regions, and ethnic/racial groups. Common risk factors for developing childhood asthma include exposure to tobacco smoke, previous allergic reactions, a family history of asthma, allergic rhinitis or eczema, living in an urban environment, obesity and lack of physical exercise, severe lower respiratory tract infections, and male gender. Asthma exacerbation in children can be triggered by a variety of factors, including allergens (e.g., pollen, dust mites, and animal dander), viral and bacterial infections, exercise, and exposure to airway irritants. Recent studies have shown that exposure to polycyclic aromatic hydrocarbons (PAHs), a major component of fine particulate matter from combustion sources, is also associated with onset of asthma, and increasing asthmatic symptoms. In this paper, we review sources of childhood PAH exposure and the association between airborne PAH exposure and childhood asthma prevalence and exacerbation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Childhood asthma
Incidence, prevalence, and morbidity
Childhood asthma is a chronic and heterogeneous disease characterized by recurrent airway obstruction, bronchial hyper-responsiveness, and airway inflammation [1]. It is the most common chronic illness in children, affecting approximately one in eight children worldwide, and 9.1 % (6.7 million children) in the United States (US) [2, 3]. Asthma is the leading cause of childhood hospitalization and school absenteeism among children around the world. Only in the US, it causes more than 10.5 million physician visits annually, and is projected to cost over 20 billion dollars in health expenditures and lost productivity [4, 5]. In the United Kingdom, 70 % of parents of asthmatic children take time off from work due to their child’s asthma, while 13 % of them had given up their jobs completely [6].
Prevalence rates of asthma show disparities across gender, regions, and ethnic/racial groups. Asthma is more prevalent in boys, as 2/3 of children with asthma are males [7]. Asthma is most common in developed countries, however, it is becoming increasingly common in developing countries, which is most likely related to the increased urbanization of communities [6]. From 1950 to 2000, the prevalence of childhood asthma increased drastically in Europe, and then decreased during the last decade [8]. It varies across Europe from east to west, which is probably because of simultaneous changes in lifestyle in eastern Europe [8]. The lowest prevalence is reported 1.6 % in Albania and the highest reported 20.7 % in the United Kingdom [9]. Furthermore, racial disparities in childhood asthma are extensive. African American children have 60 % higher asthma prevalence, and children of Native American and Alaskan decent have 25 % higher prevalence than White children. The difference in prevalence between African Americans and Whites has increased since 1980 [10]. Hispanic children have higher rates compared to Whites; and among Hispanics, Puerto Rican children have higher prevalence rates than Mexican–American children [9]. Asian children have the lowest prevalence among races in the US [11]. Regional differences in asthma prevalence in the US are also present. Prevalence is highest in the northeast, and ranges from 4.4 % in Utah and Nevada to 12.1 % in Massachusetts (Fig. 1) [3]. The intersection of socioeconomic status, race and urbanity also influence asthma morbidity, while children who live in low-socioeconomic urban environments experience significantly more asthma-associated morbidity [9].
Asthma prevalence among children 0–17 years old, by state, annual average for the period 2001–2005 [3]
Trends
Globally, childhood asthma prevalence has increased more than twofold, from 3.6 % in 1980 to 7.5 % in 1995 [12]. While some of the global increase may be due to changes in diagnostic practice, there is general agreement that it is a true phenomenon [13]. This trend seems to be associated with changes in lifestyle, which is supported by studies that show an increased prevalence of asthma among those who have moved from a traditional to a more westernized style of living [14, 15]. Between 1980 and 1996, asthma prevalence increased by an average of 4.6 % annually [16, 17]. After a redesign of the National Health Interview Survey (NHIS) in 1997, the trends in annual estimated lifetime asthma, current asthma and asthma attack prevalence level out [17–19]. Childhood asthma prevalence in the US, as estimated in the 2007 NHIS, remains at historically high levels (9.1 %) (Fig. 2). An analysis of the National Health and Nutrition Examination Survey II, has shown asthma to be associated with younger maternal age (relative odds (RO) = 1.4), residence in the city center (RO = 1.6), and family income (lowest vs. highest tertile, RO = 1.7), frequent wheeze associated with low birth weight (RO = 1.4), and skinfold thickness (RO = 1.6) [16]. These factors, however, do not explain racial disparities in asthma prevalence. Even after adjustment for environmental exposures, parental history, and demographic factors, African American children still had 1.6 times higher odds of asthma diagnosis compared to White children and are 2.5 times more likely to experience asthma-related emergency department visits and hospitalizations [3, 16].
Prevalence of asthma among children 0–17 years old in the United States, 1980–2007. In 1997, the NHIS survey was redesigned [17]
Symptoms and mortality
Asthma is characterized by attacks or episodes of inflammation and narrowing of small pulmonary airways [18]. Symptoms can include dyspnea, frequent or intermittent cough (especially at night and after exercise or exposure to cold air), wheezing, and chest congestion or tightness [19]. Expiratory dyspnea is a common symptom characteristic of asthma attacks, however, inspiratory dyspnea may coexist as symptoms progress [20]. In general, asthma severity ranges from mild to severe and life-threatening attacks, with children experiencing more severe symptoms than adults [3].
Asthma deaths among children are rare and potentially avoidable. High risk of asthma death is reported among children with severe, uncontrolled disease, a near-fatal attack of asthma, and a history of recurrent hospitalization or intubation for asthma [21]. Recent data from children aged 0–14 years revealed that mortality is generally very low in Europe, with little difference between countries, implying better control of the condition with improvements in treatment [22]. In 2005, 167 asthma-related deaths were reported among the US children (a mortality rate of 2.3 deaths per 1 million children) [12]. Asthma-related death rates increased by an average of 3.2 % per year from 1980 to 1996, then decreased by an average of 3.9 % per year from 1996 to 2005 [17]. Race and socioeconomic status are factors that confer higher rates of asthma-related mortality. African American children are 5 times more likely to die from asthma than White children [3]. Asthma-related mortality among African American children exceeds the expected difference based on racial disparities in prevalence, and may be related to other factors, such as access to care, exposure to smoking, and non-adherence to treatment among inner-city children [23]. In addition, children from low-socioeconomic families have dramatically higher overall mortality rates, compared to those from moderate/high-socioeconomic families [24].
Risk factors
Several factors have been associated with the development of childhood asthma, but none have proven to be an exclusive causative agent. Common risk factors that may increase the likelihood of developing childhood asthma include exposure to tobacco smoke, previous allergic reactions (allergic skin reactions, food allergies, or allergic rhinitis), a family history of asthma, allergic rhinitis or eczema, living in an urban environment, obesity and lack of physical exercise, severe lower respiratory tract infections (such as pneumonia), small family size, dietary habits, and male gender [25–33]. Other potential risk factors include peripheral blood eosinophilia, lower school-aged lung function, higher levels of airway responsiveness, and breast feeding [34, 35].
Asthma exacerbation or attacks in children is triggered by a variety of factors including allergens (e.g., pollen, dust mites, and animal dander), viral and bacterial infections, exercise, changes in the weather, and exposure to airway irritants (e.g., tobacco smoke) [36–42]. Recent studies have shown that exposure to polycyclic aromatic hydrocarbons (PAHs), a major component of fine particulate matter from combustion sources, is associated with onset of asthma, and increasing asthmatic symptoms [43, 44]. The aim of this paper is to review sources of childhood PAH exposure and the association between airborne PAH exposure and childhood asthma.
Polycyclic aromatic hydrocarbons (PAHs)
Characteristics
Polycyclic aromatic hydrocarbons (PAHs) are a group of hydrocarbons, defined by two or more fused aromatic rings, that are products of incomplete combustion of tobacco, wood, coal, and fossil fuels [45]. PAHs are one of the most widespread organic pollutants and the widespread environmental distribution of PAHs results in a great deal of human exposure [46, 47]. Due to their lipophilic nature, PAHs are easily absorbed and distributed throughout the human body [48]. PAHs are metabolized by enzymes that convert xenobiotic compounds into more hydrophilic and polar metabolites for easier excretion in human body fluids [49]. There are hundreds of PAHs, which usually occur as complex mixtures rather than as individual compounds (Fig. 3) [50]. Volatile (e.g. naphthalene) and semi-volatile (e.g. phenanthrene and pyrene) PAHs are products of combustion at high temperatures, and can be found in both gas and solid phases [51, 52]. Non-volatile PAHs having 4–6 aromatic rings (e.g. benzo[a]nepyrene, benzo[a]anthracene and idenol[1,2,3,a,b]pyrene) are found as solids bound to particulate matter in air [52].
Sources of exposure
Humans are exposed to PAHs from occupational, environmental, medicinal and dietary sources. Routes of exposure include inhalation, ingestion or percutaneous penetration [53]. Volatile PAHs are primarily inhaled, while semi-volatile and non-volitile PAHs can be inhaled, ingested, and absorbed dermally [51, 52]. After absorption, PAHs distribute to various organs, especially the liver [54]. Initially, they are hydrophobic and relatively inert, but are metabolized within cells to many active forms, including diol-epoxides, quinones, semi-quinones and peroxides [50].
Diet
Diet is the main source of PAH exposure in non-smokers who are not occupationally exposed [55, 56]. The Total Human Environmental Exposure Study in the US estimated that diet accounts for up to 96 % of the daily intake of carcinogenic PAHs in non-smokers [57]. The highest levels of PAHs are found in diets including cereals, meat, and meat products and foods that are smoked, broiled, or grilled. Contamination of foods by PAHs may occur during food processing (e.g., smoking or cooking), or by accidental environmental contamination (e.g., atmospheric pollution of vegetables) [58, 59]. Agricultural crops can be an important source of exposure to PAHs due to the high surface area of some food plants that are exposed to atmospheric deposition of particulate matter containing PAHs [60, 61]. It is believed that the majority of PAH contamination of agricultural crops comes from the air rather than the soil [62].
Tobacco
Smoking tobacco is a major source of exposure to PAHs [63]. Several studies reported a significant positive relationship between urinary levels of the pyrene metabolite, 1-hydroxypyrene-glucuronide (1-OHPG) and smoking [64, 65]. A study by Van Rooij et al. demonstrated that active smoking and PAH-containing food products account for 99 % of urinary excretion of PAH biomarkers in those with no other known exposure to PAHs [66]. Individuals in the US with recent smoking have significantly elevated levels of PAH metabolites in their urine compared to non-smokers [66]. Secondhand tobacco smoke exposure is also correlated with elevated urinary PAH metabolite concentration and children whose parents smoke at home have significantly elevated levels compared to children in non-smoking households [67, 68].
Occupation
Occupation is an important source of exposure to PAHs in a small portion of the population. The level of exposure to PAHs varies widely between occupations with high levels of exposure reported in chimney sweeps, foundry workers, blast furnace and coke-oven workers, vendors of broiled food, waste incineration, and steel plant workers [69–75]. The highest levels of exposure to PAHs occur in coke-oven, asphalt, and diesel workers [76, 77].
Indoor air pollution
Indoor air pollution consists of a complex mixture of agents penetrating from ambient (outdoor) air and agents generated by indoor sources [78]. The main source of indoor air PAHs is the combustion of solid fuels for cooking and heating. Smoking has been consistently described as a major source of indoor air pollution over the last several decades, with more than 30 % of all US children exposed to secondhand smoke [79]. It is estimated that children can spend as much as 90 % of their time indoors making them one of the most vulnerable groups to indoor air pollution exposures [80]. The major source of non-dietary PAH exposure in children is believed to be from indoor sources [81]. In contrast to outdoor environments, modifying indoor air PAHs is more achievable making indoor air pollution an attractive target for childhood asthma prevention [82].
Outdoor air pollution
Motor vehicle engine emissions are a major source of ambient PAHs, particularly in urban areas [83]. The highest PAH emission rates occur in diesel and gasoline engines operated without catalytic converters [84, 85]. In addition, industrial operations, waste incinerators, and residential boilers provide other major sources of ambient PAHs in urban areas [86]. According to the US Agency for Toxic Substances and Disease Registry (ATSDR), background atmospheric concentrations of representative PAHs vary from 0.02 to 1.2 ng/m3 in rural and 0.15–19.3 ng/m3 in urban areas [87]. Regulatory values range from 1 to 10 ng/m3 in different countries, but are frequently exceeded in urban areas [48].
Measurement of PAH dose
A routine method for estimating dietary PAH dose is a combination of usual food intake information obtained from food frequency questionnaires (FFQ) and existing PAH residue databases (RD) containing mean concentrations of PAHs measured in cooked foods (FFQ-RD) [88, 89]. Benzo[a]pyrene is often used as a representative of the class of PAHs due to its carcinogenic potency, prevalence, and correlation with other PAHs [90]. The FFQ-RD method may improve accuracy compared with previously used surrogates of dietary PAH exposure, such as intake of meat or well-done meat [91]. However, there are still some limitations, including inaccurate reporting of usual intake and inadequacies (in completeness and accuracy) of the RD [88]. These limitations can potentially lead to measurement error in the dose and thus limit the power of studies to detect associations [92]. On the other hand, urinary biomarkers of PAH exposure present a practical alternative approach. For example, 1-hydroxypyrene-glucuronide (1-OHPG) is the major urinary metabolite of pyrene, a common PAH, and easily measured in human urine [93]. Since 1-OHPG occurs at higher concentration in urine than most other PAH exposure biomarkers, it has been proposed as a biomarker of exposure to PAHs [53]. The maximum concentration of 1-OHPG in human urine samples is usually found in the evening, suggesting this as a suitable time for sample collection for evaluation of PAHs [94]. Urinary 1-OHPG has also been demonstrated to be significantly higher in individuals exposed to high levels of PAH through their diet [95]. Urinary levels of metabolites of naphthalene (2-naphthol) and phenanthrene (3-hydroxyphenanthrene) have also been shown to be promising surrogates to assess PAH exposure [96]. The major metabolite of naphthalene, 2-naphthol, is primarily found in gas phase and is therefore as a good biomarker to assess airborne and occupational exposures to PAHs [54].
Health effects of PAHs
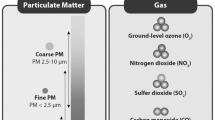
PAHs are significant components of PM2.5 (particulate matter diameter <2.5 μm) and less so of PM10 (<10 μm), both of which have been linked to adverse respiratory health [97]. In recent years, PAHs have received particular attention because of their oxidative potential and related cytotoxicity [98]. Exposure to PAHs has been linked to several adverse outcomes in children, including cognitive development, childhood IQ, and respiratory health [99–101]. The US National Health and Nutrition Examination Survey (NHANES) (1999–2000, 2001–2002, and 2003–2004) provided comprehensive descriptions of reference ranges for a large panel of urinary PAH metabolites collected from a population of children and adults with no suspected occupational exposures [102, 103]. Higher level of PAHs was detected among children, suggesting that they may be at greater risk for adverse health effects [104].
PAHs are the principal carcinogenic chemical constituents in soot and coal tar that are responsible for cancer induction in animal models [50, 105, 106]. The International Agency for Research on Cancer (IARC) and the United States National Toxicology Program (NTP) have classified a number of PAHs as “known human carcinogens”, “probable human carcinogens” or “reasonably anticipated to be a human carcinogen” The NTP lists 12 PAHs as human carcinogen, including benz[a]anthracene, benzo[a]pyrene, benzo[b]fluoranthene, benzo[j]fluoranthene, dibenz[a,h]anthracene, dibenzo[a,h]pyrene, dibenzo[a,i]pyrene, indeno[1,2,3-cd]pyrene, benzo[k]fluoranthene, dibenzo[a,e]pyrene, dibenzo[a,l]pyrene, and 5-methylchrysene [107–109].
PAHs and childhood asthma
Several lines of evidence support an association between fine particulate matter, a major source of airborne PAHs, and childhood asthma. During the 2008 Beijing Olympics, the central government temporarily restricted air pollution emissions in Beijing, greatly reducing ambient pollutant levels. During this period, a statistically significant reduction in the mean concentration of PM2.5 (−27 %) coincided with a decrease in childhood asthma admissions [110]. In a prospective birth cohort study of 3,863 newborn children, outdoor PM2.5 levels were associated with a significant increase in the incidence of asthma (OR 1.28; 95 % CI 1.10–1.49), the prevalence of asthma (OR 1.26; 95 % CI 1.04–1.51), and the prevalence of asthma symptoms (OR 1.15; 95 % CI 1.02–1.28) [111].
Secondhand tobacco smoke is a major route of childhood PAH exposure and has been associated with childhood asthma. A meta-analysis of studies published from 1970 to 2005 showed a positive association between household secondhand tobacco smoke exposure and current childhood asthma (RR 1.25, 95 % CI 1.21–1.30), and incident childhood asthma (RR 1.21, 95 %CI 1.08–1.36) [112]. In addition, maternal tobacco smoking has been associated with an increased incidence of childhood asthma up to age 6 (OR 1.31, 95 %CI 1.22–1.41), but less strongly thereafter (OR 1.13, 95 %CI 1.04–1.22) [113]. Similarly, indoor air pollution has been associated with higher rates of reported childhood asthma; compared with other fuel types, coal was associated with the highest incidence of asthma [114–116].
Further studies suggest that specific components of PM2.5 including, black carbon, transition metals, or PAHs are associated with adverse respiratory outcomes and asthma, particularly in infants and children [101, 117–121]. Annual average particulate PAH exposure, estimated by a land use regression model, was associated with decreased forced expiratory volume (FEV1) in asthmatic children [122]. Miller et al. [123] reported an association between increased urinary PAH metabolites in children and biomarkers of pediatric allergy including anti-mouse IgE and/or anti-cat IgE levels. Subsequent studies investigated the effect of early repeated exposures to PAHs and reported that non-atopic children were susceptible to adverse respiratory effects due to pyrene, but not higher molecular weight (non-volatile) PAHs [123, 124]. In contrast, exposure to non-volatile PAHs enhanced allergic sensitization to cockroach allergen – a strong risk factor for greater asthma morbidity in children [125].
Studies suggest that PAHs may act through immunoglobulin E (IgE) to stimulate inflammatory responses and enhance allergic reactions [126–129]. Experimental evidence indicates that pyrene enhances allergic IgE responses in mice [130, 131]. Adjuvant effects of PAHs on IgE have been demonstrated in human nasal provocation studies. A study by Diaz-Sanchez et al. [133], showed that intranasal instillation of PAH rich diesel exhaust particles increased total IgE production, and acted as an adjuvant for ragweed specific IgE after challenges with both ragweed + DEP compared to ragweed alone [132, 133]. Exposures to PAHs in vivo may also influence B cell and T-helper cell differentiation by skewing immune responses toward a Th2 specific profile, which favors B-cell production of IgE and eosinophils both of which are hallmarks of allergic inflammation and allergic asthma [134]. Recent studies have focused on the role of PAHs on aryl hydrocarbon receptors (AHRs) and induction of Th17 cells. Th17 cells as a source of IL-17 and IL-22 are implicated in the pathogenesis of airway disease and particularly asthma [135, 136].
PAHs have also been linked to asthma through oxidative stress pathways (Fig. 4) [137–140]. PAHs bioactivated by cytochrome P450 generate reactive oxygen species (ROS) (e.g. epoxides, peroxides, semiquinones and quinones) that may enhance asthma morbidity [137]. Li et al. [141] demonstrated that PAHs in diesel exhaust can initiate a cascade of oxidative stress that leads to airway inflammation. In this model, the reactive oxygen species, from redox cycling of PAH intermediates, activate both the anti-inflammatory and the pro-inflammatory signaling pathways, leading to transcriptional upregulation of genes involved in regulating immune response [137, 142–144]. Immune responses include synthesis of cytokines, cell adhesion molecules and chemokines, increases in neutrophils, eosinophils, and macrophage production and activity, resulting in airway inflammation and asthma exacerbation [124, 137, 145]. Other studies suggest that prenatal exposure to PAHs may account for some of the observed increased asthma prevalence [146]. A recent prospective cohort study revealed that prenatal PAH exposure is associated with significant reduction in Forced Expiratory Volume in 0.5 s, Forced Expiratory Volume in 1 s (FEV1), and Forced Expiratory Flow 25–75 % (FEV 25–75 %), suggesting that prenatal PAH exposure inhibits the full development of respiratory airway caliber [147]. A study in northern Moravia region at Czech Republic, a known region with high concentrations of PAHs in Europe, showed an association between prenatal PAH exposure and intrauterine growth retardation (IUGR) and higher prevalence of asthma [148]. Certain PAHs resemble steroid hormones and are considered endocrine disruptors [149]. They are lipid soluble, and are transferred across the placenta and the fetal blood brain barrier [150]. These results collectively demonstrate that there are complex relationships between PAH exposure and asthma development, and multiple potential mechanisms might mediate this web of causation.
PAH and asthma pathogenesis/exacerbation pathways. CYP450 cytochrome P450, GSH glutathione, HO-1 heme oxygenase 1, IgE immunoglobulin E, IL interleukin, NO 2 nitrogen dioxide, Nrf2 nuclear factor (erythroid derived-2) like 2, PM particulate matter, RANTES regulated on activation, normal T cell expressed and secreted, ROS reactive oxygen species, RSV respiratory syncytial virus, SOD superoxide dismutase
Future directions
The underlying cause of the association between air PM exposure and childhood asthma is unclear. A variety of constituents of PM are potential candidates for contributing to asthma initiation, exacerbation and progression. These include common allergens, microbial products, irritants, PAHs, carbon black, and sensitizing agents. Research is needed to clarify the associations between these constituents of PM and childhood asthma in order to focus efforts to develop effective prevention measures. This approach could lead to direct pollutant-control strategies toward those sources or constituents responsible for the greatest burden of risk for childhood asthma development and morbidity [151]. Further investigation of the interactions between multiple potential causative agents is needed to clarify potential mechanisms underlying these associations in order to enhance our ability to understand the pathogenesis of this disease and its treatment.
References
Bousquet J, Jeffery PK, Busse WW, Johnson M, Vignola AM. Asthma from bronchoconstriction to airways inflammation and remodeling. Am J Respir Crit Care Med. 2000;161:1720–45.
Lai C, Beasley R, Crane J, Foliaki S, Shah J, Weiland S. Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2009;64:476–83.
Akinbami LJ. The Stat of childhood asthma, United States, 1980–2005. Advance data from vita and health statistics; no 381. Hyattsville, MD: National Center for Health Statistics; 2006.
Moorman JE, Rudd RA, Johnson CA, King M, Minor P, Bailey C, Scalia MS, Akinbami LJ. National surveillance for asthma—United States, 1980–2004. Department of Health and Human Services, Centers for Disease Control and Prevention; 2007.
National Heart, Lung, and Blood Institute. Morbidity and mortality: chart book on cardiovascular, lung, and blood diseases. Bethesda, Md: National Institutes of Health; 2009.
Braman SS. The global burden of asthma. Chest. 2006;130(1 Suppl):4S–12S.
Almqvist C, Worm M, Leynaert B. Impact of gender on asthma in childhood and adolescence: a GA2LEN review. Allergy. 2008;63:47–57.
Rabe KF, Adachi M, Lai CK, Soriano JB, Vermeire PA, Weiss KB, Weiss ST. Worldwide severity and control of asthma in children and adults: the global asthma insights and reality surveys. J Allergy Clin Immunol. 2004;114:40–70.
Smyth RL. Asthma: a major pediatric health issue. Respir Res. 2002;3(Suppl 1):S3–7.
Measuring childhood asthma prevalence before and after the 1997 redesign of the National Health Interview Survey—United States. MMWR Morb Mortal Wkly Rep. 2000;49:908–11.
Bryant-Stephens T. Asthma disparities in urban environments. J Allergy Clin Immunol. 2009;123:1199–206.
Akinbami LJ, Schoendorf KC. Trends in childhood asthma: prevalence, health care utilization, and mortality. Pediatrics. 2002;110:315–22.
Britton J. Asthma’s changing prevalence. BMJ. 1992;304:857–8.
Woolcock AJ. Asthma-disease of a modern lifestyle. Med J Aust. 1996;165:358–9.
Cookson J. Prevalence rates of asthma in developing countries and their comparison with those in Europe and North America. Chest. 1987;91:97S–103S.
Gupta RS, Carrión-Carire V, Weiss KB. The widening black/white gap in asthma hospitalizations and mortality. J Allergy Clin Immunol. 2006;117:351–8.
Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123:S131–45.
Cairns CB. Acute asthma exacerbations: phenotypes and management. Clin Chest Med. 2006;27:99–108.
Calamelli E, Ricci G, Pession A. Recent advances in diagnosis and therapy of allergic rhinitis and asthma in childhood. Eur Ann Allergy Clin Immunol. 2012;44:215–24.
Nishimuta T, Kondo N, Hamasaki Y, Morikawa A, Nishima S. Childhood asthma. Allergol Int. 2011;60:147–69.
McFadden E, Warren EL. Observations on asthma mortality. Ann Intern Med. 1997;127(2):142–7.
Anderson HR, Gupta R, Kapetanakis V, Asher MI, Clayton T, Robertson CF, Strachan DP. ISAAC streeting committee. International correlations between indicators of prevalence, hospital admissions and mortality for asthma in children. Int J Epidemiol. 2008;37(3):573–82.
Herzog R, Cunningham-Rundles S. Pediatric asthma: natural history, assessment, and treatment. Mt Sinai J Med. 2011;78:645–60.
Miller JE. The effects of race/ethnicity and income on early childhood asthma prevalence and health care use. Am J Public Health. 2000;90:428–30.
Salam MT, Li YF, Langholz B, Gilliland FD. Early-life environmental risk factors for asthma: findings from the Children’s Health Study. Environ Health Perspect. 2004;112:760–5.
Sears MR, Holdaway MD, Flannery EM, Herbison GP, Silva PA. Parental and neonatal risk factors for atopy, airway hyper-responsiveness, and asthma. Arch Dis Child. 1996;75:392–8.
Aligne CA, Auinger P, Byrd RS, Weitzman M. Risk factors for pediatric asthma. Contributions of poverty, race, and urban residence. Am J Respir Crit Care Med. 2000;162:873–7.
MacDowell AL, Bacharier LB. Infectious triggers of asthma. Immunol Allergy Clin North Am. 2005;25:45–66.
Shaheen SO. Obesity and asthma: cause for concern? Clin Exp Allergy. 1999;29:291–3.
Infante-Rivard C, Amre D, Gautrin D, Malo JL. Family size, day-care attendance, and breastfeeding in relation to the incidence of childhood asthma. Am J Epidemiol. 2001;153:653–8.
Devereux G, Seaton A. Diet as a risk factor for atopy and asthma. J Allergy Clin Immunol. 2005;115:1109–17.
Guilbert TW, Morgan WJ, Zeiger RS, Bacharier LB, Boehmer SJ, Krawiec M, Larsen G, Lemanske RF, Liu A, Mauger DT, Sorkness C, Szefler SJ, Strunk RC, Taussig LM, Martinez FD. Atopic characteristics of children with recurrent wheezing at high risk for the development of childhood asthma. J Allergy Clin Immunol. 2004;114:1282–7.
Bacharier LB, Guilbert TW. Diagnosis and management of early asthma in preschool-aged children. J Allergy Clin Immunol. 2012;130:287–96.
Oddy WH, Holt PG, Sly PD, Read AW, Landau LI, Stanley FJ, Kendall GE, Burton PR. Association between breast feeding and asthma in 6 year old children: findings of a prospective birth cohort study. BMJ. 1999;319:815–9.
Peat JK, Allen J, Oddy W, Webb K. Breastfeeding and asthma: appraising the controversy. Pediatr Pulmonol. 2003;35:331–4.
Karimi P, Shahrokni A, Moradi S. Evidence for US Preventive Services Task Force (USPSTF) Recommendations against routine mammography for females between 40–49 years of age. Asian Pac J Cancer Prev. 2013;14:2137–9.
Green RM, Custovic A, Sanderson G, Hunter J, Johnston SL, Woodcock A. Synergism between allergens and viruses and risk of hospital admission with asthma: case-control study. BMJ. 2002;324:763.
Gern JE. Viral and bacterial infections in the development and progression of asthma. J Allergy Clin Immunol. 2000;105:S497–502.
Massie J. Exercise-induced asthma in children. Pediatric Drugs. 2002;4:267–78.
Mireku N, Wang Y, Ager J, Reddy RC, Baptist AP. Changes in weather and the effects on pediatric asthma exacerbations. Ann Allergy Asthma Immunol. 2009;103:220–4.
Wu F, Takaro TK. Childhood asthma and environmental interventions. Environ Health Perspect. 2007;115:971–5.
Rumchev K, Spickett J, Bulsara M, Phillips M, Stick S. Association of domestic exposure to volatile organic compounds with asthma in young children. Thorax. 2004;59:746–51.
Burton A. Children’s health: methylation links prenatal PAH exposure to asthma. Environ Health Perspect. 2009;117:A195.
Delfino RJ. Epidemiologic evidence for asthma and exposure to air toxics: linkages between occupational, indoor, and community air pollution research. Environ Health Perspect. 2002;110:573.
Cerniglia CE. Biodegradation of polycyclic aromatic hydrocarbons. Curr Opin Biotechnol. 1993;4:331–8.
Connell DW, Hawker DW, Warne MJ, Vowles PP. Polycyclic aromatic hydrocarbons (PAHs). In: Connell DW, editor. Basic concepts of environmental chemistry. Boca Raton, FL: CRC Press; 1997. p. 205–17.
Srogi K. Monitoring of environmental exposure to polycyclic aromatic hydrocarbons: a review. Environ Chem Lett. 2007;5:169–95.
Franco SS, Nardocci AC, Günther WMR. PAH biomarkers for human health risk assessment: a review of the state-of-the-art. Cad Saude Publica. 2008;24:S569–80.
Shimada T. Xenobiotic-metabolizing enzymes involved in activation and detoxification of carcinogenic polycyclic aromatic hydrocarbons. Drug Metab Pharmacokinet. 2006;21:257–76.
Baird WM, Hooven LA, Mahadevan B. Carcinogenic polycyclic aromatic hydrocarbon-DNA adducts and mechanism of action. Environ Mol Mutagen. 2005;45:106–14.
Jongeneelen FJ. Benchmark guideline for urinary 1-hydroxypyrene as biomarker of occupational exposure to polycyclic aromatic hydrocarbons. Ann Occup Hyg. 2001;45:3–13.
Chuang JC, Callahan PJ, Lyu CW, Wilson NK. Polycyclic aromatic hydrocarbon exposures of children in low-income families. J Expo Anal Environ Epidemiol. 1999;9:85–98.
Strickland P, Kang D. Urinary 1-hydroxypyrene and other PAH metabolites as biomarkers of exposure to environmental PAH in air particulate matter. Toxicol Lett. 1999;108:191–9.
Rappaport SM, Waidyanatha S, Serdar B. Naphthalene and its biomarkers as measures of occupational exposure to polycyclic aromatic hydrocarbons. J Environ Monit. 2004;6:413–6.
Ramesh A, Walker SA, Hood DB, Guillén MD, Schneider K, Weyand EH. Bioavailability and risk assessment of orally ingested polycyclic aromatic hydrocarbons. Int J Toxicol. 2004;23:301–33.
Kamangar F, Karimi P. The state of nutritional epidemiology: why we are still unsure of what we should eat? Arch Iran Med. 2013;16:483–6.
Lioy PL, Waldman JM, Greenberg A, Harkov R, Pietarinen C. The Total Human Environmental Exposure Study (THEES) to benzo (a) pyrene: comparison of the inhalation and food pathways. Arch Environ Health. 1998;43:304–12.
Falco G, Domingo JL, Llobet JM, Teixido A, Casas C, Muller L. Polycyclic aromatic hydrocarbons in foods: human exposure through the diet in Catalonia, Spain. J Food Prot. 2003;66:2325–31.
Wenzl T, Simon R, Anklam E, Kleiner J. Analytical methods for polycyclic aromatic hydrocarbons (PAHs) in food and the environment needed for new food legislation in the European Union. Trends Analyt Chem. 2006;25:716–25.
Kobayashi R, Okamoto RA, Maddalena RL, Kado NY. Polycyclic aromatic hydrocarbons in edible grain: a pilot study of agricultural crops as a human exposure pathway for environmental contaminants using wheat as a model crop. Environ Res. 2008;107:145–51.
Gadde B, Bonnet S, Menke C, Garivait S. Air pollutant emissions from rice straw open field burning in India, Thailand and the Philippines. Environ Pollut. 2009;157:1554–8.
Nam JJ, Thomas GO, Jaward FM, Steinnes E, Gustafsson O, Jones KC. PAHs in background soils from Western Europe: influence of atmospheric deposition and soil organic matter. Chemosphere. 2008;70:1596–602.
Pufulete M, Battershill J, Boobis A, Fielder R. Approaches to carcinogenic risk assessment for polycyclic aromatic hydrocarbons: a UK perspective. Regul Toxicol Pharmacol. 2004;40:54–66.
Fagundes RB, Abnet CC, Strickland PT, Kamangar F, Roth MJ, Taylor PR, Dawsey SM. Higher urine 1-hydroxy pyrene glucuronide (1-OHPG) is associated with tobacco smoke exposure and drinking mate in healthy subjects from Rio Grande do Sul, Brazil. BMC Cancer. 2006;6:139.
Kang D, Rothman N, Cho SH, Lim HS, Kwon HJ, Kim SM, Schwartz B, Strickland PT. Association of exposure to polycyclic aromatic hydrocarbons (estimated from job category) with concentration of 1-hydroxypyrene glucuronide in urine from workers at a steel plant. Occup Environ Med. 1995;52:593–9.
Van Rooij JG, Veeger MM, Bodelier-Bade MM, Scheepers PT, Jongeneelen FJ. Smoking and dietary intake of polycyclic aromatic hydrocarbons as sources of interindividual variability in the baseline excretion of 1-hydroxypyrene in urine. Int Arch Occup Environ Health. 1994;66:55–65.
Lee KH, Vermeulen R, Lenters V, Cho SH, Strickland PT, Kang D. Determinants of urinary 1-hydroxypyrene glucuronide in South Korean children. Int Arch Occup Environ Health. 2009;82:961–8.
Taioli E, Sram RJ, Garte S, Kalina I, Popov TA, Farmer PB. Effects of polycyclic aromatic hydrocarbons (PAHs) in environmental pollution on exogenous and oxidative DNA damage (EXPAH project): description of the population under study. Muta Res. 2007;620:1–6.
Horwood L, Fergusson D, Shannon F. Social and familial factors in the development of early childhood asthma. Pediatrics. 1985;75:859–68.
Hogstedt C, Jansson C, Hugosson M, Tinnerberg H, Gustavsson P. Cancer incidence in a cohort of Swedish chimney sweeps, 1958–2006. Am J Public Health. 2013;103:1708–14.
Liu HH, Lin MH, Chan CI, Chen HL. Oxidative damage in foundry workers occupationally co-exposed to PAHs and metals. Int J Hyg Environ Health. 2010;213:93–8.
Campo L, Fustinoni S, Consonni D, Pavanello S, Kapka L, Siwinska E, Mielzynska D, Bertazzi P. Urinary carcinogenic 4–6 ring polycyclic aromatic hydrocarbons in coke oven workers and in subjects belonging to the general population: Role of occupational and environmental exposure. Int J Hyg Environ Health. 2014;217:231–8.
Kuo CY, Chang SH, Chien YC, Chiang FY, Wei YC. Exposure to carcinogenic PAHs for the vendors of broiled food. J Exp Sci Environ Epidemiol. 2005;16:410–6.
Oh E, Lee E, Im H, Kang HS, Jung WW, Won NH, Kim EM, Sul D. Evaluation of immuno-and reproductive toxicities and association between immunotoxicological and genotoxicological parameters in waste incineration workers. Toxicoloxy. 2005;210:65–80.
Yang HH, Lai SO, Hsieh LT, Hsueh HJ, Chi TW. Profiles of PAH emission from steel and iron industries. Chemosphere. 2002;48:1061–74.
Unwin J, Cocker J, Scobbie E, Chambers H. An assessment of occupational exposure to polycyclic aromatic hydrocarbons in the UK. Ann Occup Hygiene. 2006;50:395–403.
Godschalk RW, Van Schooten FJ, Bartsch H. A critical evaluation of DNA adducts as biological markers for human exposure to polycyclic aromatic compounds. J Biochem Mol Biol. 2003;36:1–11.
Breysse PN, Diette GB, Matsui EC, Butz AM, Hansel NN, McCormack MC. Indoor air pollution and asthma in children. Proc Am Thorac Soc. 2010;7:102–6.
Matsui EC, Hansel NN, McCormack MC, Rusher R, Breysse PN, Diette GB. Asthma in the inner city and the indoor environment. Immunol Allergy Clin North Am. 2008;28:665–86.
Klepeis NE, Nelson WC, Ott WR, Robinson JP, Tsang AM, Switzer P, Behar JV, Hern SC, Engelmann WH. The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Expo Anal Environ Epidemiol. 2001;11:231–52.
Fiala Z, Vyskocil A, Krajak V, Viau C, Ettlerova E, Bukac J, Fialova D, Emminger S. Environmental exposure of small children to polycyclic aromatic hydrocarbons. Int Arch Occup Environ Health. 2001;74:411–20.
McCormack MC, Breysse PN, Matsui EC, Hansel NN, Williams D, Curtin-Brosnan J, Eggleston P, Dietter GB, Center for Childhood Asthma in Urban Envirnment. In-home particle concentrations and childhood asthma morbidity. Environ Health Perspect. 2009;117:294–98.
Diette GB, McCormack MC, Hansel NN, Breysse PN, Matsui EC. Environmental issues in managing asthma. Resp Care. 2008;53:602–17.
Murugesan A, Umarani C, Subramanian R, Nedunchezhian N. Biodiesel as an alternative fuel for diesel engines—a review. Renew Sust Energy Rev. 2009;13:653–62.
Karavalakis G, Boutsika V, Stournas S, Bakeas E. Biodiesel emissions profile in modern diesel vehicles. Part 2: Effect of biodiesel origin on carbonyl, PAH, nitro-PAH and oxy-PAH emissions. Sci Total Environ. 2011;409:738–47.
Wu S, Tao S, Liu W. Particle size distributions of polycyclic aromatic hydrocarbons in rural and urban atmosphere of Tianjin, China. Chemosphere. 2006;62:357–67.
Agency for Toxic Substances and Disease Registry. Toxicological profile for polycyclic aromatic hydrocarbons. Atlanta: Agency for Toxic Substances and Disease Registry; 1995.
Sinha R, Cross A, Curtin J, Zimmerman T, McNutt S, Risch A, Holden J. Development of a food frequency questionnaire module and databases for compounds in cooked and processed meats. Mol Nutr Food Res. 2005;49:648–55.
Keating GA, Bogen KT, Chan JM. Development of a meat frequency questionnaire for use in diet and cancer studies. J Am Diet Assoc. 2007;107:1356–62.
Deziel NC, Strickland PT, Platz EA, Abubaker S, Buckley TJ. Comparison of standard methods for assessing dietary intake of benzo [a] pyrene. Cancer Epidemiol Biomark Prev. 2011;20:962–70.
Sinha R, Cross AJ, Graubard BI, Leitzmann MF, Schatzkin A. Meat intake and mortality: a prospective study of over half a million people. Arch Intern Med. 2009;169:562–71.
Spiegelman D. Approaches to uncertainty in exposure assessment in environmental epidemiology. Ann Rev Public Health. 2010;31:149–63.
Strickland P, Kang D, Sithisarankul P. Polycyclic aromatic hydrocarbon metabolites in urine as biomarkers of exposure and effect. Environ Health Perspect. 1996;104:927.
Zhao ZH, Quan WY, Tian DH. Experiments on the effects of several factors on the 1-hydroxypyrene level in human urine as an indicator of exposure to polycyclic aromatic hydrocarbons. Sci Total Environ. 1992;113:197–207.
Kang D, Rothman N, Cho SH, Lim HS, Kwon HJ, Kim SM, Schwartz B, Strickland PT. Association of exposure to polycyclic aromatic hydrocarbons (estimated from job category) with concentration of 1-hydroxypyrene glucuronide in urine from workers at a steel plant. Occup Environ Med. 1995;52:593–9.
Sobus JR, Waidyanatha S, McClean MD, Herrick RF, Smith TJ, Garshick E, Ladan F, Hart JE, Zheng Y, Rappaport SM. Urinary naphthalene and phenanthrene as biomarkers of occupational exposure to polycyclic aromatic hydrocarbons. Occup Environ Med. 2009;66:99–104.
Krewski D, Jerrett M, Burnett RT, Ma R, Hughes E, Shi Y, Turner MC, Pope CA III, Thurston G, Calle EE, Thun MJ, Beckerman B, DeLUnca P, Finkelstein N, Ito K, Moore DK, Newbold KB, Ramsay T, Rozz Z, SHin H, Tempalski. Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Res Rep Health Eff Inst. 2009;140:5–114.
Garza KM, Soto KF, Murr LE. Cytotoxicity and reactive oxygen species generation from aggregated carbon and carbonaceous nanoparticulate materials. Int J Nanomedicine. 2008;3:83–94.
Perera FP, Rauh V, Whyatt RM, Tsai WY, Tang D, Diaz D, Hoepner L, Barr D, Tu YH, Camann D, Kinney P. Effect of prenatal exposure to airborne polycyclic aromatic hydrocarbons on neurodevelopment in the first 3 years of life among inner-city children. Environ Health Perspect. 2006;114:1287–92.
Perera FP, Li Z, Whyatt R, Hoepner L, Wang S, Camann D, Rauh V. Prenatal airborne polycyclic aromatic hydrocarbon exposure and child IQ at age 5 years. Pediatrics. 2009;124:e195–202.
Jedrychowski W, Galas A, Pac A, Flak E, Camman D, Rauh V, Perera F. Prenatal ambient air exposure to polycyclic aromatic hydrocarbons and the occurrence of respiratory symptoms over the first year of life. Eur J Epidemiol. 2005;20:775–82.
Li Z, Sandau CD, Romanoff LC, Caudill SP, Sjodin A, Needham LL, Patterson DG Jr. Concentration and profile of 22 urinary polycyclic aromatic hydrocarbon metabolites in the US population. Environ Res. 2008;107:320–31.
Grainger J, Huang W, Patterson DG, Turner WE, Pirkle J, Caudill SP, Wang RY, Needham LL, Sampson EJ. Reference range levels of polycyclic aromatic hydrocarbons in the US population by measurement of urinary monohydroxy metabolites. Environ Res. 2006;100:394–423.
Al-Daghri NM, Alokail MS, Abd-Alrahman SH, Draz HM, Yakout SM, Clerici M. Polycyclic aromatic hydrocarbon exposure and pediatric asthma in children: a case-control study. Environ Health. 2013;12:1.
Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomark Prev. 2014;23:700–13.
Karimi P, Shahrokni A, Ranjbar MR. Implementation of proteomics for cancer research: past, present, and future. Asian Pac J Cancer Prev. 2014;15:2433–8.
IARC. Polynuclear aromatic compounds. Part I: chemical, environmental and experimental data; 1983. Lyon: International Agency for Research on Cancer.
National Toxicology Program. Public Health Service, US Department of Health and Human Services, 12th report on carcinogens. Research Triangle Park, NC; 2011. p. 353–61.
NTP 12th report on carcinogens. Rep Carcinog. 2011;12(499):iii-499.
Jia Y, Stone D, Wang W, Schrlau J, Tao S, Simonich SL. Estimated reduction in cancer risk due to PAH exposures if source control measures during the 2008 Beijing Olympics were sustained. Environ Health Perspect. 2011;119:815–20.
Brauer M, Hoek G, Van Vliet P, Meliefste K, Fischer PH, Wijga A, Koopman LP, Gerritsen J, Kerkhof M, Heinrish J, Bellander T, Brunekreef B. Air pollution from traffic and the development of respiratory infections and asthmatic and allergic symptoms in children. Am J Respi Crit Care Med. 2002;166:1092–8.
Vork K, Broadwin R, Blaisdell R. Developing asthma in childhood from exposure to secondhand tobacco smoke: insights from a meta-regression. Cien Saude Colet. 2008;13:1313–25.
Strachan DP, Cook DG. Parental smoking and childhood asthma: longitudinal and case-control studies. Thorax. 1998;53:204–12.
Qian Z, Zhang J, Korn LR, Wei F, Chapman RS. Factor analysis of household factors: are they associated with respiratory conditions in Chinese children? Int J Epidemiol. 2004;33:582–8.
Burr M, Anderson H, Austin J, Harkins L, Kaur B, Strachan D, Warner JO. Respiratory symptoms and home environment in children: a national survey. Thorax. 1999;54:27–32.
Peabody JW, Riddell TJ, Smith KR, Liu Y, Zhao Y, Gong J, Milet M, Sinton JE. Indoor air pollution in rural China: cooking fuels, stoves, and health status. Arch Environ Occup Health. 2005;60:86–95.
Spira-Cohen A, Chen LC, Kendall M, Lall R, Thurston GD. Personal exposures to traffic-related air pollution and acute respiratory health among Bronx schoolchildren with asthma. Environ Health Perspect. 2011;119:559–65.
Patel MM, Miller RL. Air pollution and childhood asthma: recent advances and future directions. Curr Opin Pediatr. 2009;21:235–42.
Bell ML, Ebisu K, Peng RD, Dominici F. Adverse health effects of particulate air pollution: modification by air conditioning. Epidemiology. 2009;20:682–6.
Miller RL, Garfinkel R, Horton M, Camann D, Perera FP, Whyatt RM, Kinney PL. Polycyclic aromatic hydrocarbons, environmental tobacco smoke, and respiratory symptoms in an inner-city birth cohort. Chest. 2004;126:1071–8.
Rosa MJ, Jung KH, Perzanowski MS, Kelvin EA, Darling KW, Camann DE, Chillrud SN, Whyatt RM, Kinney PL, Perera FP, Miller RL. Prenatal exposure to polycyclic aromatic hydrocarbons, environmental tobacco smoke and asthma. Respir Med. 2011;105:869–76.
Nadeau K, McDonald-Hyman C, Noth EM, Pratt B, Hammond SK, Balmes J, Tager I. Ambient air pollution impairs regulatory T-cell function in asthma. J. Allergy Clin Immunol. 2010;126:845–52.
Miller RL, Garfinkel R, Lendor C, Hoepner L, Li Z, Romanoff L, Sjodin A, Needham L, Perera FP, Whayatt RM. Polycyclic aromatic hydrocarbon metabolite levels and pediatric allergy and asthma in an inner-city cohort. Pediatr Allergy Immunol. 2010;21:260–7.
Karimi P, Modarresi SZ, Sahraian MA, Shoormasti RS, Mahlooji M, Kazemnejad A, Pourpak Z. The relation of multiple sclerosis with allergy and atopy: a case control study. Iran J Allergy Asthma Immunol. 2013;12:182–9.
Perzanowski MS, Chew GL, Divjan A, Jung KH, Ridder R, Tang D, Diaz D, Goldstein IF, Kinney PL, Rundle AG, Camann DE, Perera FP, Miller RL. Early-life cockroach allergen and polycyclic aromatic hydrocarbon exposures predict cockroach sensitization among inner-city children. J Allergy Clin Immunol. 2013;131:886–93.
Tsien A, Diaz-Sanchez D, Ma J, Saxon A. The organic component of diesel exhaust particles and phenanthrene, a major polyaromatic hydrocarbon constituent, enhances IgE production by IgE-secreting EBV-transformed human B cells in vitro. Toxicol Appl Pharmacol. 1997;142:256–63.
Nel AE, Diaz-Sanchez D, Ng D, Hiura T, Saxon A. Enhancement of allergic inflammation by the interaction between diesel exhaust particles and the immune system. J Allergy Clin Immunol. 1998;102:539–54.
Lubitz S, Schober W, Pusch G, Effner R, Klopp N, Behrendt H, Buters JT. Polycyclic aromatic hydrocarbons from diesel emissions exert proallergic effects in birch pollen allergic individuals through enhanced mediator release from basophils. Environ Toxicol. 2010;25:188–97.
Xiao GG, Nel AE, Loo JA. Nitrotyrosine-modified proteins and oxidative stress induced by diesel exhaust particles. Electrophoresis. 2005;26:280–92.
Kanoh T, Suzuki T, Ishimori M, Ikeda S, Ohasawa M, Ohkuni H, Tunetoshi Y. Adjuvant activities of pyrene, anthracene, fluoranthene and benzo(a)pyrene in production of anti-IgE antibody to Japanese cedar pollen allergen in mice. J Clin Lab Immunol. 1996;48:133–47.
Bommel H, Li-Weber M, Serfling E, Duschl A. The environmental pollutant pyrene induces the production of IL-4. J Allergy Clin Immunol. 2000;105:796–802.
Cao Y, DePinho RA, Ernst M, Vousden K. Cancer research: past, present and future. Nat Rev Cancer. 2011;11:749–54.
Diaz-Sanchez D, Dotson AR, Takenaka H, Saxon A. Diesel exhaust particles induce local IgE production in vivo and alter the pattern of IgE messenger RNA isoforms. J Clin Invest. 1994;94:1417–25.
Riedl MA, Nel AE. Importance of oxidative stress in the pathogenesis and treatment of asthma. Curr Opin Allergy Clin Immunol. 2008;8:49–56.
van Voorhis M, Knopp S, Julliard W, Fechner JH, Zhang X, Schauer JJ, Mezrich JD. Exposure to atmospheric particulate matter enhances Th17 polarization through the aryl hydrocarbon receptor. PLoS ONE. 2013;8:e82545.
Brandt EB, Kovacic MB, Lee GB, Gibson AM, Acciani TH, Le Cras TD, Ryan PH, Budelsky AL, Khurana Hershey GK. Diesel exhaust particle induction of IL-17A contributes to severe asthma. J Allergy Clin Immunol. 2013;132:1194–204.
Li N, Wang M, Bramble LA, Schmitz DA, Schauer JJ, Sioutas C, Harkema JR, Nel AE. The adjuvant effect of ambient particulate matter is closely reflected by the particulate oxidant potential. Environ Health Perspect. 2009;117:1116–23.
Mastrangelo G, Clonfero E, Pavanello S, Fedeli U, Fadda E, Turato A, Piccinni S, Montagnani R, Marcer G. Exposure to diesel exhaust enhances total IgE in non-atopic dockers. Int Arch Occup Environ Health. 2003;76:63–8.
Pandya RJ, Solomon G, Kinner A, Balmes JR. Diesel exhaust and asthma: Hypotheses and molecular mechanisms of action. Environ Health Perspect. 2002;110:103–12.
Cho YS, Moon HB. The role of oxidative stress in the pathogenesis of asthma. Allergy Asthma Immunol Res. 2010;2(3):183–7.
Li N, Sioutas C, Cho A, Schmitz D, Misra C, Sempf J, Wang M, Oberley T, Froines J, Nel A. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ Health Perspect. 2003;111:455–60.
Nel AE, Diaz-Sanchez D, Li N. The role of particulate pollutants in pulmonary inflammation and asthma: evidence for the involvement of organic chemicals and oxidative stress. Curr Opin Pulm Med. 2001;7:20–6.
Ghabaee M, Bayati A. Saroukolaei SA, Sahraian MA, Sanaati MH, Karimi P, Houshmand M, Sadeghian H, Hashemi Chelavi L. Analysis of HLA DR2&DQ6 (DRB1* 1501, DQA1* 0102, DQB1* 0602) haplotypes in Iranian patients with multiple sclerosis. Cell Mol Neurobiol. 2009;29:109–14.
Rezaee AR, Azadi A, Houshmand M, Mahmoodi F, Purpak Z, Safaei S, Karimi P, Ghabaee M, Sahraian MA. Mitochondrial and nuclear genes as the cause of complex I deficiency. Genet Mol Res. 2012;12:3551–4.
Vattanasit U, Navasumrit P, Khadka MB, Kanitwithayanun J, Promvijit J, Autrup H, Ruchirawat M. Oxidative DNA damage and inflammatory responses in cultured human cells and in humans exposed to traffic-related particles. Int J Hyg Environ Health. 2014;217:23–33.
Chu S, Zhang H, Maher C, McDonald JD, Zhang X, Ho SM, Yan B, Chillrud S, Perera F, Factor P, Miller RL. Prenatal and postnatal polycyclic aromatic hydrocarbon exposure, airway hyperreactivity, and Beta-2 adrenergic receptor function in sensitized mouse offspring. J Toxicol. 2013. doi:10.1155/2013/603581.
Jedrychowski WA, Perera FP, Maugeri U, Majewska R, Mroz E, Flak E, Camann D, Sowa A, Jacek R. Long term effects of prenatal and postnatal airborne PAH exposures on ventilatory lung function of non-asthmatic preadolescent children. Prospective birth cohort study in Krakow. Sci Total Environ. 2015;502:502–9.
Sram RJ, Binkova B, Dostal M, Merkerova-Dostalova M, Libalova H, Milcova A, Rossner P Jr, Rossnerova A, Schmuczerova J, Svecova V, Topinka J, Votavova H. Health impact of air pollution to children. Int J Hyg Environ Health. 2013;216:533–40.
Perera F, Herbstman J. Prenatal environmental exposures, epigenetics, and disease. Reprod Toxicol. 2011;31:363–73.
Brown LNA, Khousbouei H, Goodwin JS, Irvin-Wilson CV, Ramesh A, Sheng L, McCallister MM, Jiang GC, Aschner M, Hood DB. Down-regulation of early ionotrophic glutamate receptor subunit developmental expression as a mechanism for observed plasticity deficits following gestational exposure to benzo pyrene. Neurotoxicology. 2007;28:965–78.
Rusling JF, Kumar CV, Gutkind JS, Patel V. Measurement of biomarker proteins for point-of-care early detection and monitoring of cancer. Analyst. 2010;135:2496–511.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karimi, P., Peters, K.O., Bidad, K. et al. Polycyclic aromatic hydrocarbons and childhood asthma. Eur J Epidemiol 30, 91–101 (2015). https://doi.org/10.1007/s10654-015-9988-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-015-9988-6